1. Introduction
Microglial cells, the brain-resident immune cells, play a pivotal role in regulating the cellular processes involved in the development of neuronal networks and the homeostasis maintenance of the central nervous system (CNS) [
1]. Notably, in response to abnormal microenvironment factors, including for example stress, aging, injuries, infections, and hypoxia-ischemia, microglia can assume different activation states, from neuroprotective to neurodestructive, the equilibrium of which may contribute to the onset and outcome of neuroinflammatory and neurodegenerative mechanisms [
2]. Indeed, dysfunction of microglia is one of the hallmarks and leading causes of common neurodegenerative diseases (NDDs), such as Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and amyotrophic lateral sclerosis (ALS) [
3,
4,
5,
6,
7]. All these pathologies are characterized by aberrant aggregation of disease-causing proteins in the brain [
8], which can directly activate microglia, trigger microglia-mediated neuroinflammation, and increase oxidative stress [
9].
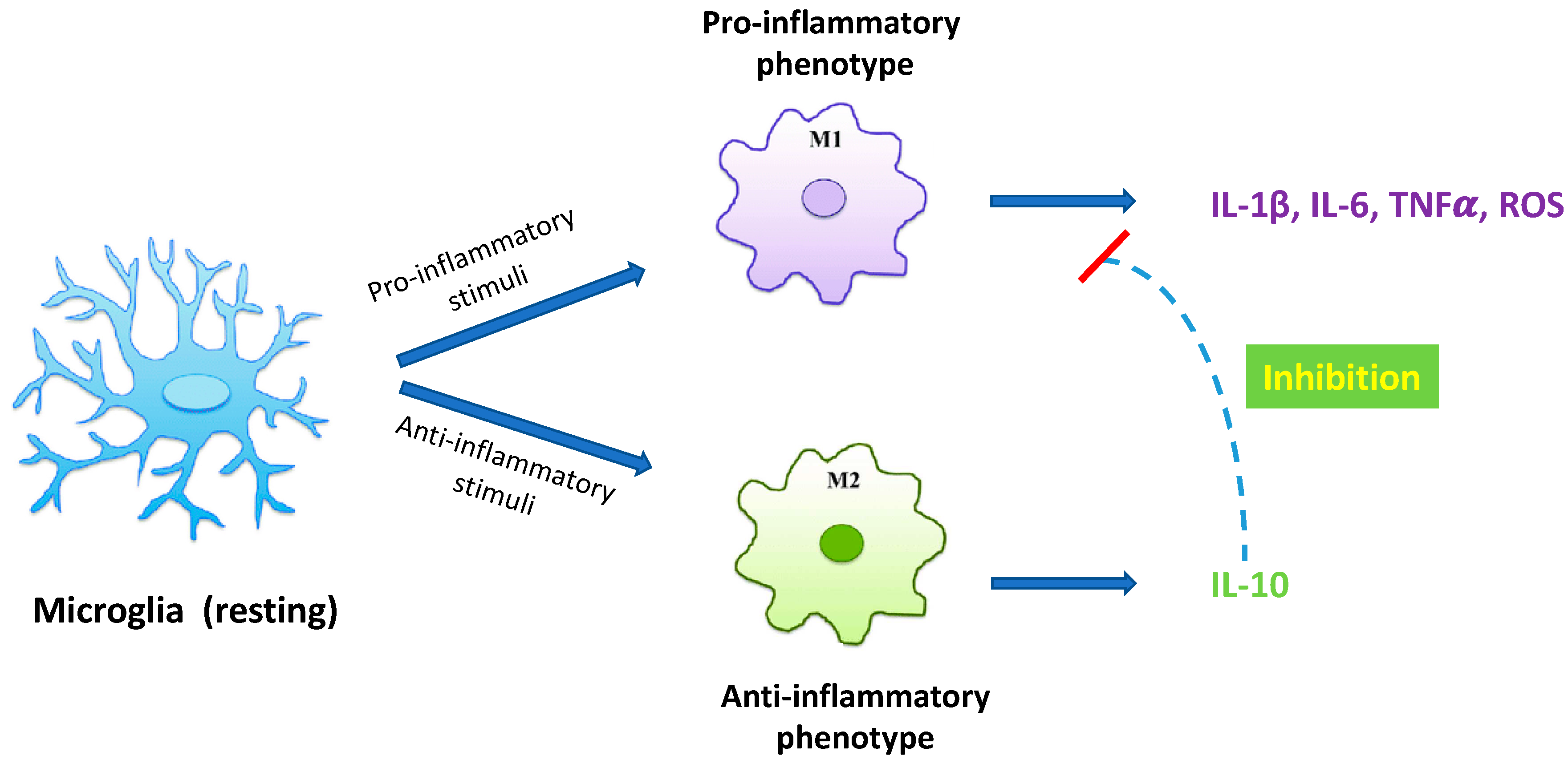
Under physiological conditions microglial cells maintain a ramified cell shape, defined “resting state” (
Figure 1), and vigilantly monitor and protect neuronal function. In the event of brain injury, infection or neurodegeneration, microglia adopt a phagocytic phenotype, defined “M1 state”, in which the cell attains an amoeboid morphology, and may secrete a wide variety of neurotoxic factors, including pro-inflammatory cytokines, proteinases, and reactive oxygen species (ROS), leading to exacerbate damage and neuronal death [
10]. Accumulating evidence suggests that the initial classical activation of microglia is followed by a secondary alternative activation, defined “M2 state”, which is important for neuronal cell repair, tissue remodeling, and suppression of inflammation [
11] (
Figure 1). Since chronic inflammatory activation of microglia is correlated with common NDDs, functional modulation of microglial phenotypes could represent a valid therapeutic strategy [
10,
12,
13].
Recently, 3-iodothyronamine (T1AM), an endogenous thyroid hormone (TH) derivative, able to interact directly with a specific G-protein coupled receptor known as trace amine-associated receptor 1 (TAAR1) [
14], gained interest for its ability to promote neuroprotective effects in several models, including seizure-related excitotoxic damage, altered autophagy, amyloidosis and OGD-induced synaptic dysfunction [
15,
16,
17,
18], and to efficiently cross the blood brain barrier (BBB) [
19]. However, the potential for T1AM to regulate brain neuroinflammatory responses has not yet been explored.
In this study we demonstrated, for the first time, that T1AM inhibits LPS/TNFα-induced inflammatory response in HMC3 human microglial cells through the activation of TAAR1 [
20]. Since it is well known that fibrillar amyloid-β (Aβ) peptides play an important role in microglial activation in AD [
21], we also showed that T1AM-TAAR1 signalling pathway was able to protect against Aβ-induced cytotoxic and inflammatory responses in HMC3 cells, and that TAAR1 stimulation can inactivate microglial NF-κB signalling.
Even though still at a preliminary level, the results of our study highlight the ability of T1AM to extensively modulate microglia-mediated neuroinflammation, providing further insight into its possible therapeutic application for the prevention of neurodegeneration.
2. Results
2.1. T1AM decreased the inflammatory phenotype of LPS/TNFα-stimulated HMC3 human microglial cells.
As previously reported [
22,
23,
24], exposure of human microglial clone 3 (HMC3) cells to LPS/TNFα stimulus for 24 h resulted in a significant increase of pro-inflammatory IL-6 release in cell culture media, while no effect on anti-inflammatory IL-10 levels was observed as compared with control cells. In the present study, HMC3 microglial cell line was used as
in vitro model to investigate the ability of T1AM to prevent neuroinflammation.
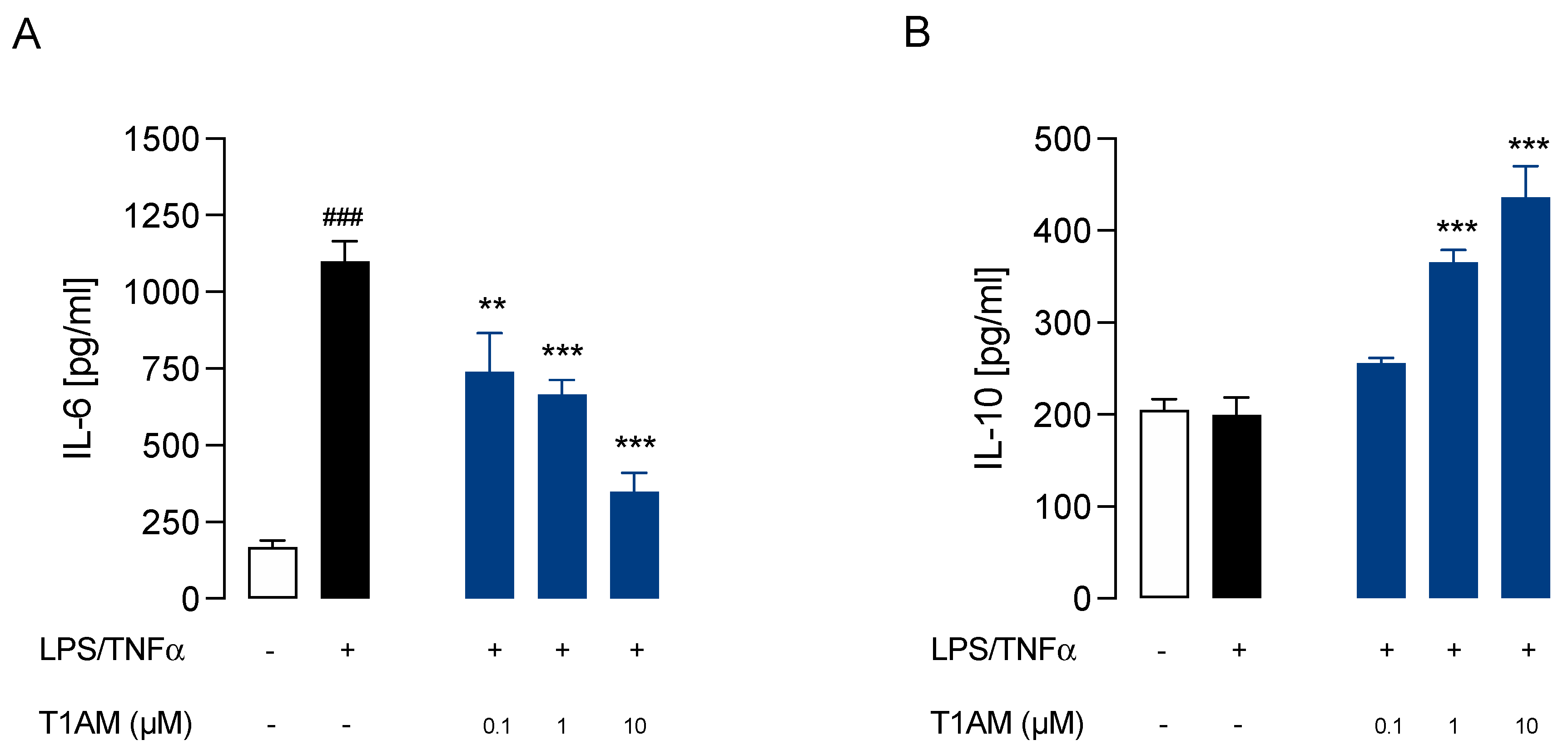
Dose-response experiments were carried out by exposing HMC3 cells to pretreatment with increasing concentrations (0.1, 1, and 10 μM) of T1AM for 1 h, followed by LPS/TNFα treatment for 24 h. ELISA assays on cell culture media, revealed that T1AM causes a significant (p<0.05) dose-dependent reduction of IL-6 levels as compared to LPS/TNFα treated cells (
Figure 2A). A significant (p<0.05) dose-dependent increase in IL-10 levels was also observed in the same set of experiments (
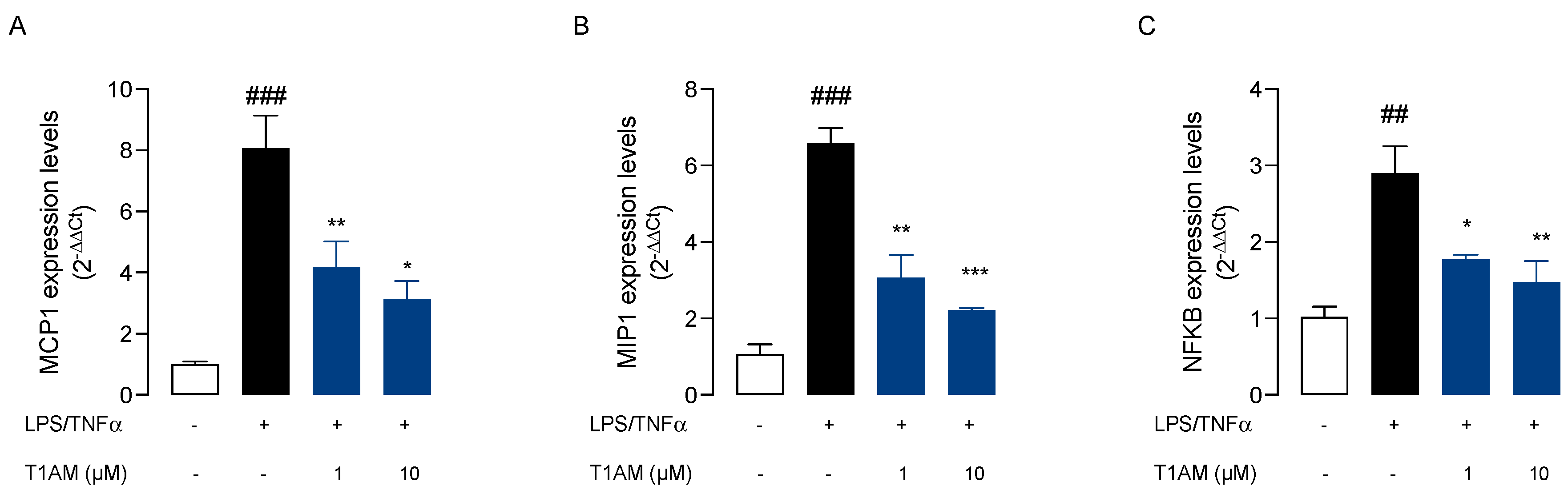
Figure 2B), suggesting that T1AM pretreatment may temper hyperinflammation. Moreover, gene expression analysis revealed that pre-treatment with 1 or 10 μM T1AM significantly decreases the expression of inflammatory response-related genes in LPS/TNFα treated cells, including the monocyte chemoattract protein-1 (MCP1), the macrophage inflammatory protein-1 (MIP1), and the transcription factor NF-kB (
Figure 3).
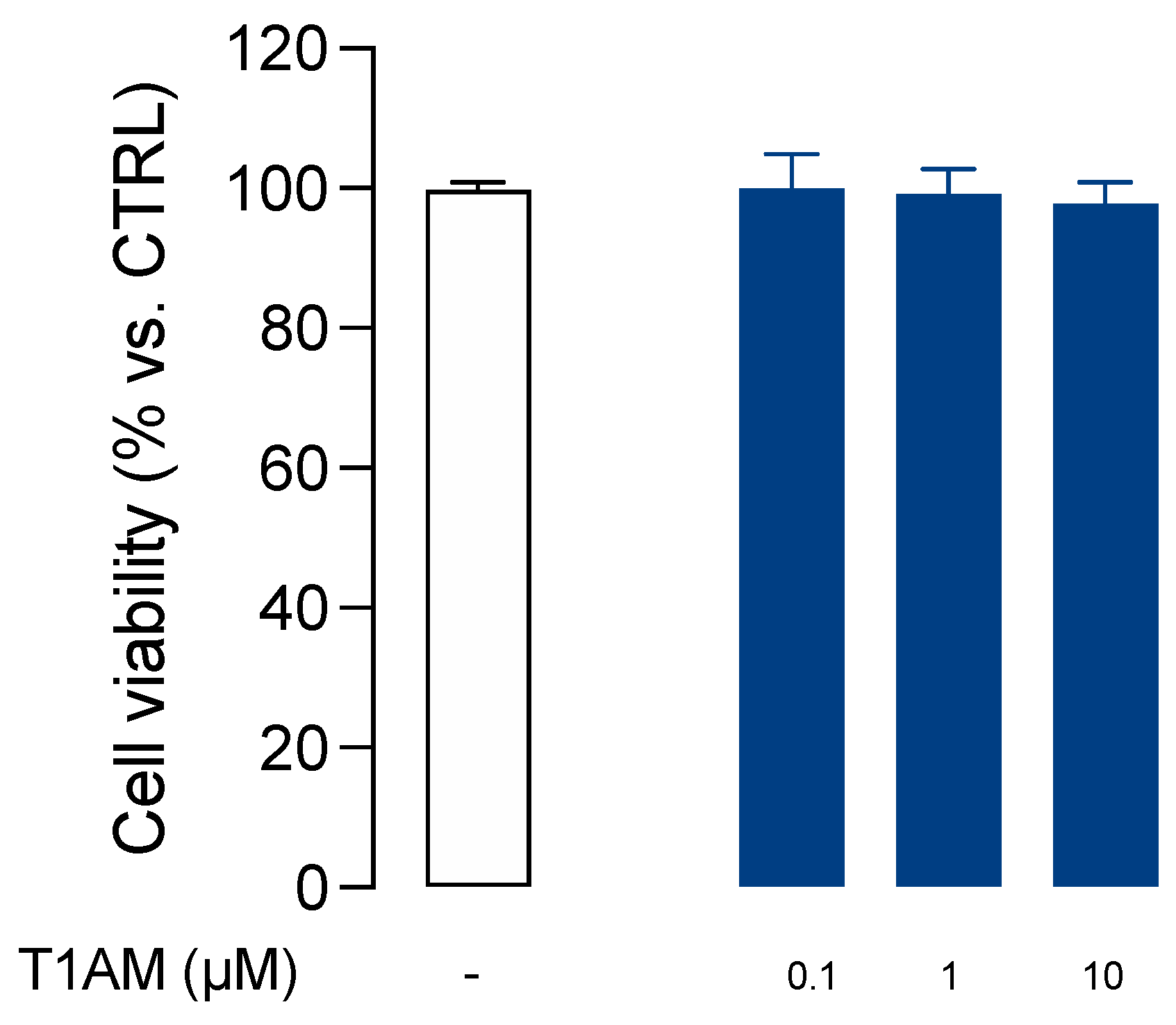
In addition, T1AM was nontoxic to microglial cells when used at 0.1, 1, and 10μM concentrations for 24h (
Figure 4).
2.2. T1AM up-take and metabolism in HMC3 human microglial cells.
T1AM is known to be transported inside cells and rapidly transformed into 3-iodothyroacetic acid (TA1) [
19,
25,
26].
Liquid Chromatography with tandem mass spectrometry (LC-MS/MS) was used to measure T1AM and TA1 levels in HMC3 cells. After incubating HMC3 cell preparations with 0.1 µM T1AM for 5, 15, 30 and 60 min at 37 °C, the cell culture media were collected, and cell lysates were prepared according to a previously reported procedure [
27].
As shown in
Table 1, T1AM was rapidly taken up by HMC3 cells and catabolized to TA1, indicating that in HMC3 cells, amine oxidases were metabolically active. Notably, the product of T1AM catabolism, TA1, after forming was released from cells, and detected into the collected cell culture media showing increasing concentrations over time. In HMC3 cell lysates, the concentration of T1AM appeared to remain constant over time at values corresponding to approximately 25% of the administered dose, whereas only a negligible amount of TA1 was found.
2.3. Trace amine associated receptor TAAR1 is involved in T1AM-mediated anti-inflammatory response of microglial cells.
The evidence that T1AM was able to suppress the response of microglia cells to inflammatory stress, prompted us to extend our investigation to its mechanism of action.
It is known from the literature that T1AM is a high-affinity ligand for TAAR1 [
14], and TAAR1 was demonstrated to mediate T1AM protective effect against synaptic plasticity abnormalities in a mouse model of AD [
28]. Therefore, we explored whether TAAR1 could also be involved in T
1AM-mediated anti-inflammatory response of HMC3 cells.
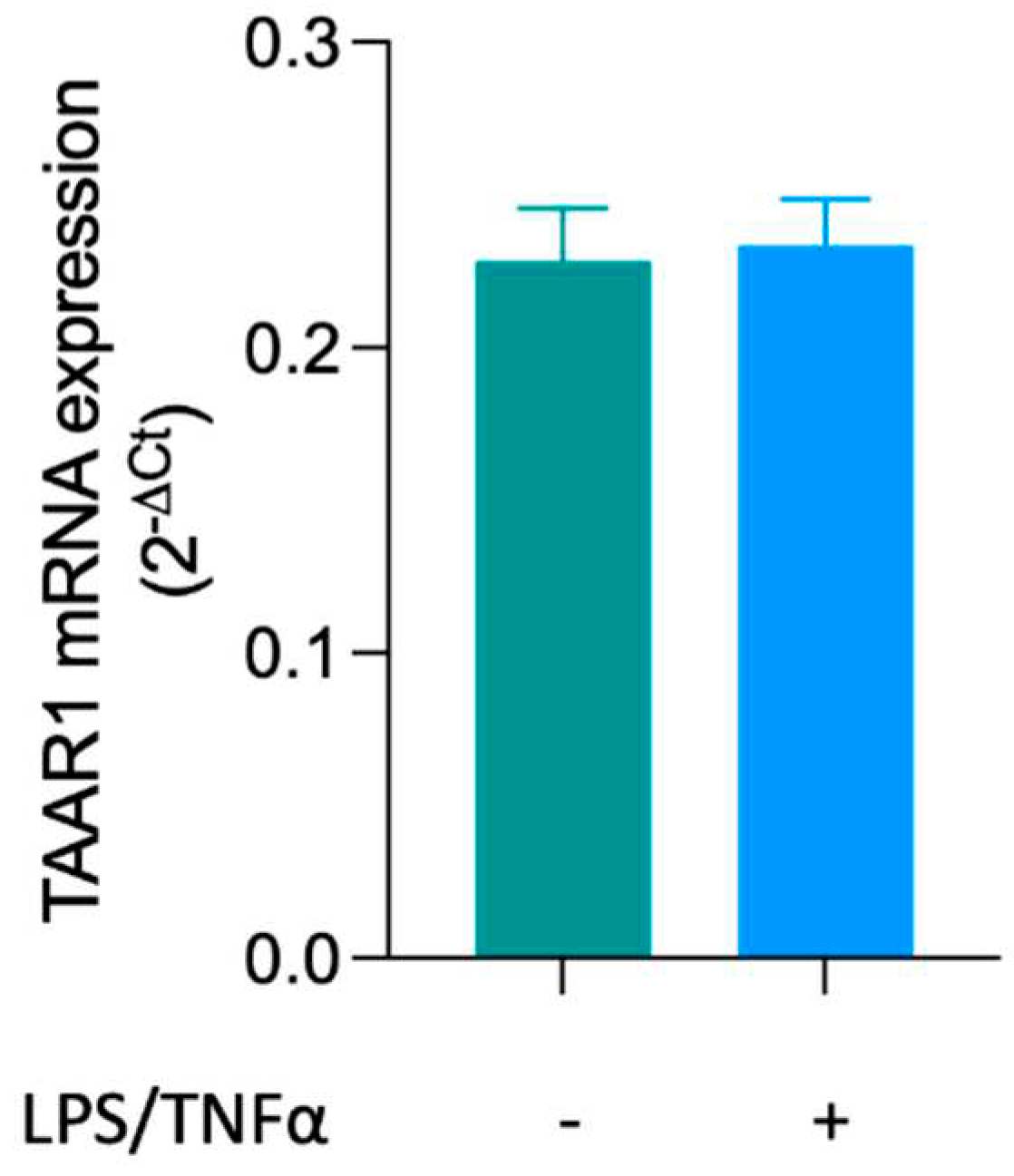
First, expression of TAAR1 in HMC3 microglial cells was assessed by qPCR analysis. As shown in
Figure 5, resting microglial cells showed TAAR1 expression, and no changes were observed after 24 h treatment with LPS/TNFα.
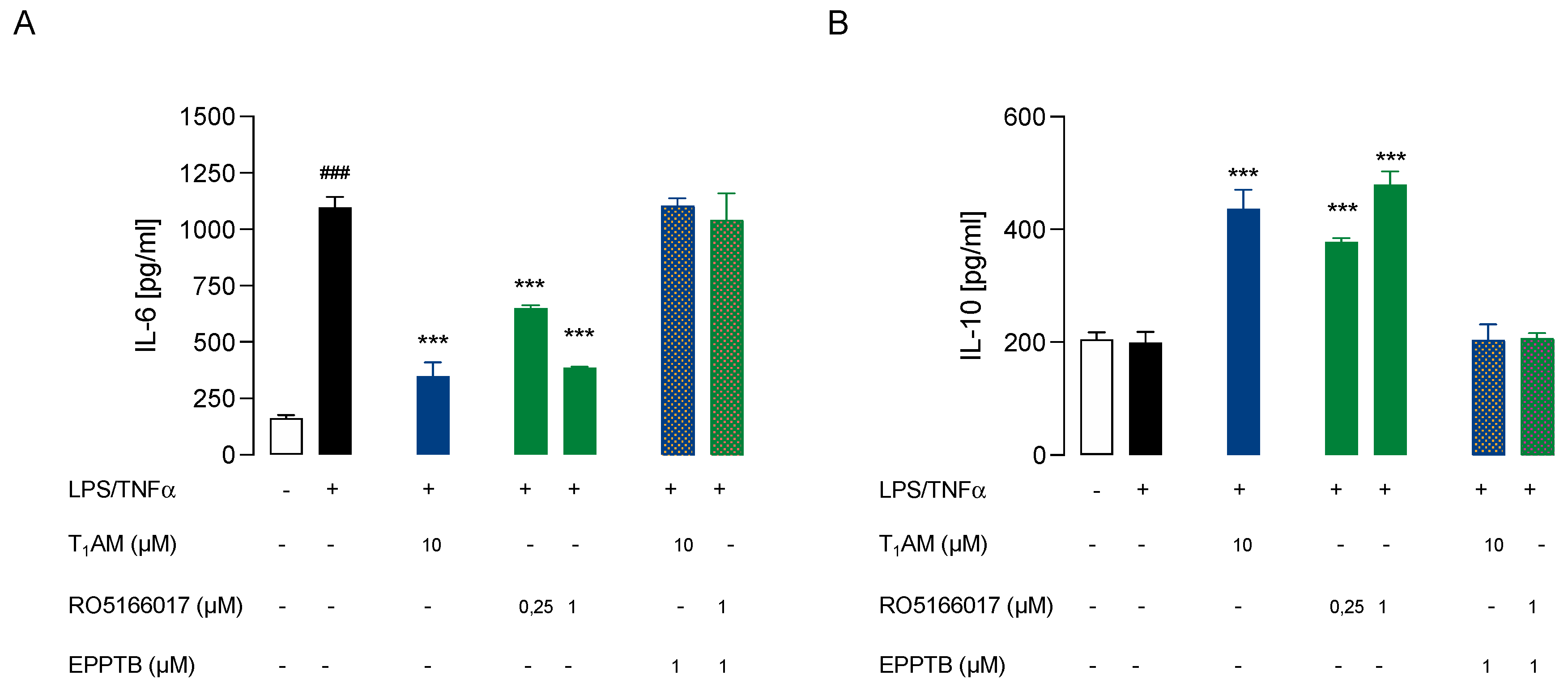
Then, we investigated whether TAAR1 could play a role in our model of inflamed microglia by using a TAAR1 selective antagonist (EPPTB) and a selective agonist (RO5166017) [
29].
We observed that T
1AM protective effect against microglia-activation was abolished by co-administration of TAAR1 selective antagonist EPPTB (5 nM) (
Figure 6A,B). Conversely, the administration of the TAAR1 agonist RO5166017 (1 μM) to LPS/TNFα-stimulated HMC3 cells mimicked the effects on the release of both IL-6 and IL-10 previously observed after administering T1AM (10 μM) (
Figure 6A,B).
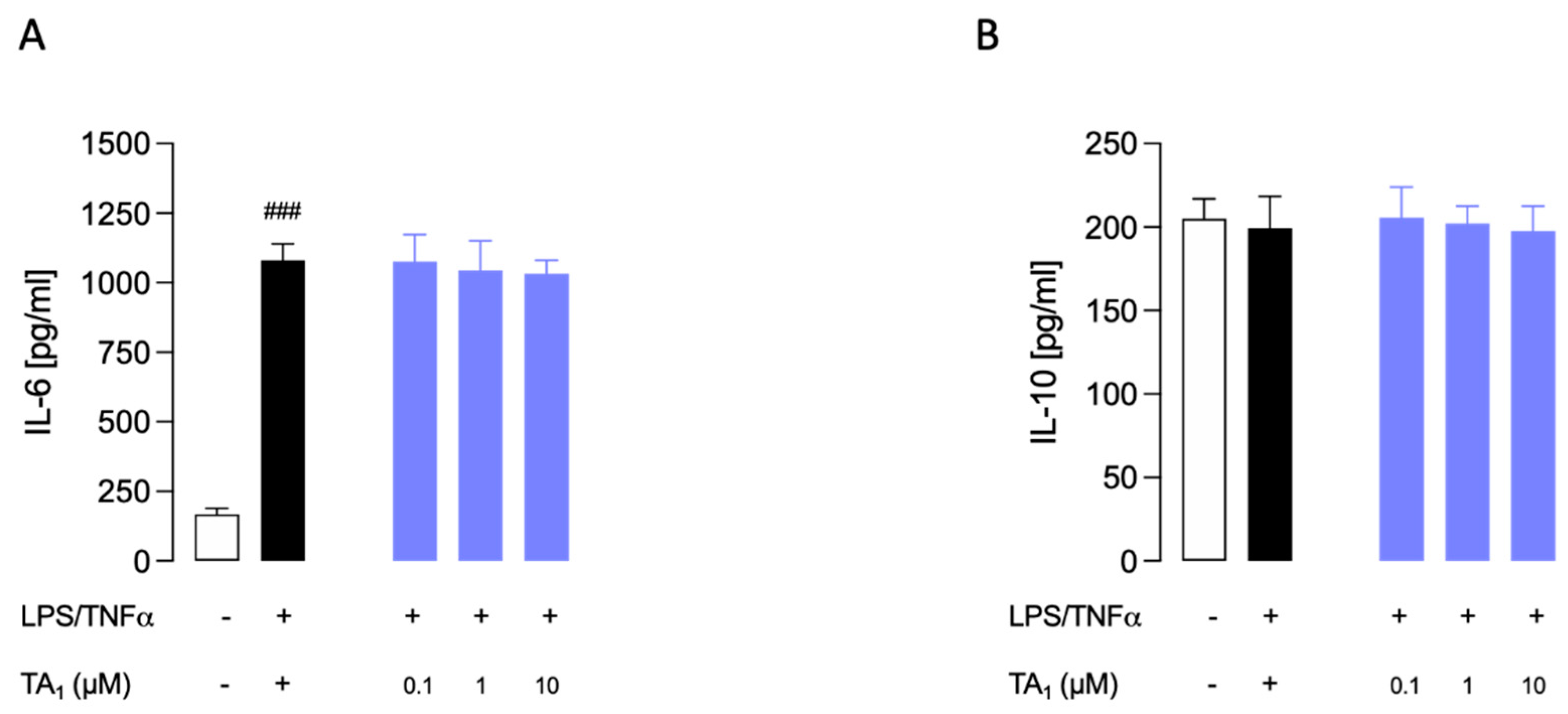
2.4. 3-iodothyroacetic acid (TA1) was not able to decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 human microglial cells.
Since 3-iodothyroacetic acid (TA1), the major catabolite of T1AM [
30,
31,
32], has been reported to be responsible for some effects elicited after the administration of exogenous T1AM, we checked whether TA1 administration could also decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells. We observed that administration of TA1 (0.1, 1, and 10 μM) to LPS/TNFα-stimulated HMC3 cells was not able to produce any significant effect on both IL-6 and IL-10 release from cells (
Figure 7), suggesting that the decreased activation of microglia is exclusively due to the action of T1AM through the interaction with the TAAR1 receptor.
2.5. T1AM-TAAR1 system protects against Aβ25-35-mediated release of proinflammatory factors in HMC3 cells.
Studies have revealed that A
β oligomers activate microglia to secrete proinflammatory factors, including cytokines, chemokines, complements factors, and a large variety of free radicals [
33,
34]. Suppressing the response of microglia cells to inflammatory stress may attenuate AD pathology and lessen the disease progression [
35,
36].
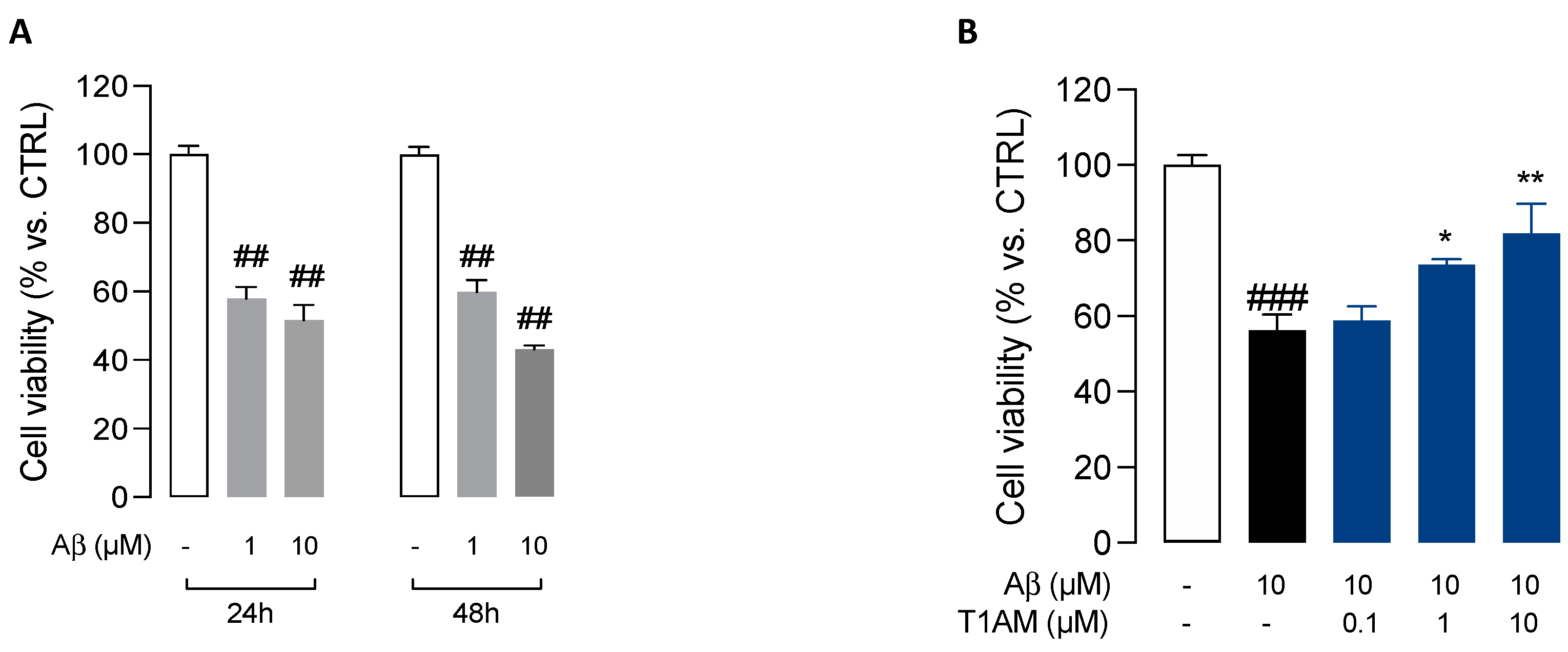
We initially assessed the effects of β-amyloid peptide 25-35 (Aβ25-35) [
37] on HMC3 cells viability. The cells were treated with two different concentrations (1 and 10 μM) of Aβ25-35 for 24 or 48h. Aβ25-35 was found to induce cytotoxicity in HMC3 cells in a concentration- and time-dependent manner, with a 10μM concentration promoting a 50% reduction in cell viability after 24 h (
Figure 8A). We thus used this condition to evaluate the modulation of Aβ25-35 cytotoxicity in further experiments. HMC3 cells were treated with 10 μM Aβ25-35 in the presence of different concentrations (0.1, 1 and 10μM) of T1AM for 24 h to determine the effects of T1AM on β-amyloid-induced cytotoxicity. In line with expectations, MTT assays indicated that T1AM was able to protect cells from Aβ-induced cytotoxicity in a concentration-dependent manner, with the identified best concentrations of 1 and 10μM being used in further experiments (
Figure 8B).
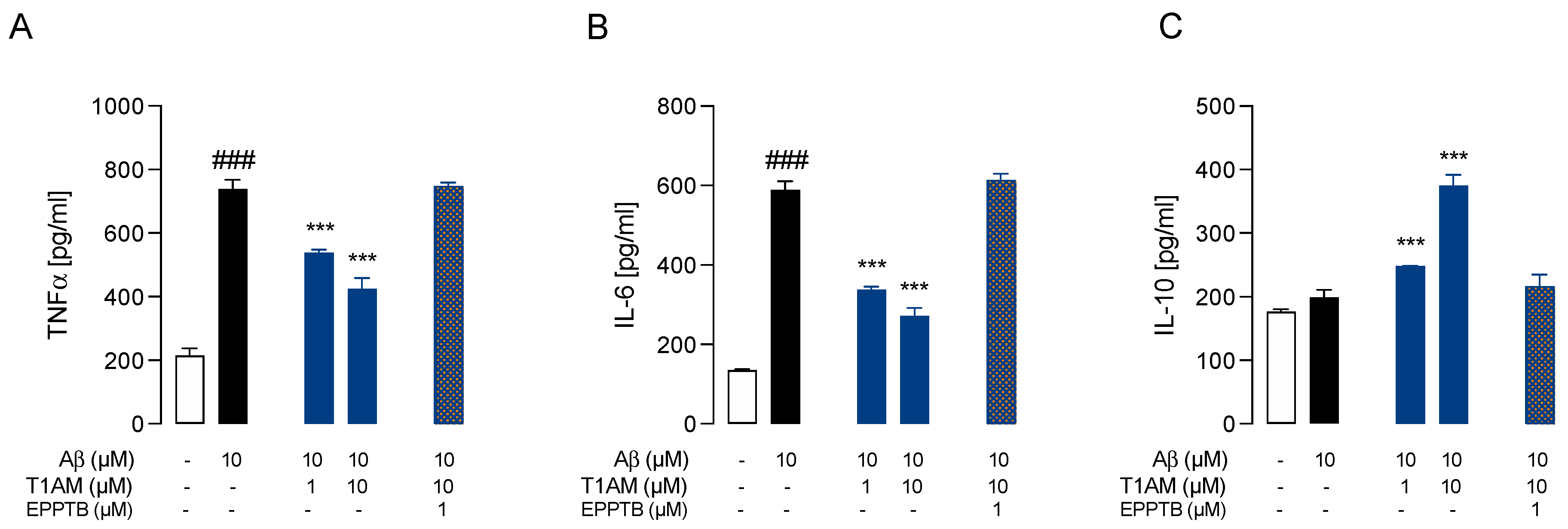
Having assessed the cytoprotective effects of T1AM, we went on to examine the ability of T1AM to suppress β-amyloid induced upregulation of proinflammatory cytokines production. Exposure of HMC3 cells to 10 μM Aβ25-35 for 24h promoted a significant increase in the secretion of common pro-inflammatory cytokines (TNF-α and IL-6), and no effect on the release of anti-inflammatory cytokine IL-10 (
Figure 9A-C). Then, we repeated the experiment exposing HMC3 cells to pretreatment with 1 and 10μM T1AM. Compared with the Aβ-treated group, the levels of TNF-α and IL-6 were found to show a significant return to normal levels in the group receiving the combined Aβ25-35 and T1AM treatment (
Figure 9AB). In addition, pretreatment with T1AM significantly increased the secretion of anti-inflammatory cytokine IL-10 (
Figure 9C). Taken together, these findings indicated the potential of T1AM to inhibit Aβ-induced microglia activation. Since TAAR1 has previously been found to mediate the beneficial effects of T1AM on the inflammatory response of LPS/TNFα treated HMC3 cells, we subsequently proceeded to examine the role of TAAR1 in mediating the anti-inflammatory effects of T1AM in β-amyloid-induced HMC3 cells.
We observed that T
1AM protective effect against Aβ-induced microglia-activation was abolished by co-administration of TAAR1 selective antagonist EPPTB (1μM) (
Figure 9A-C).
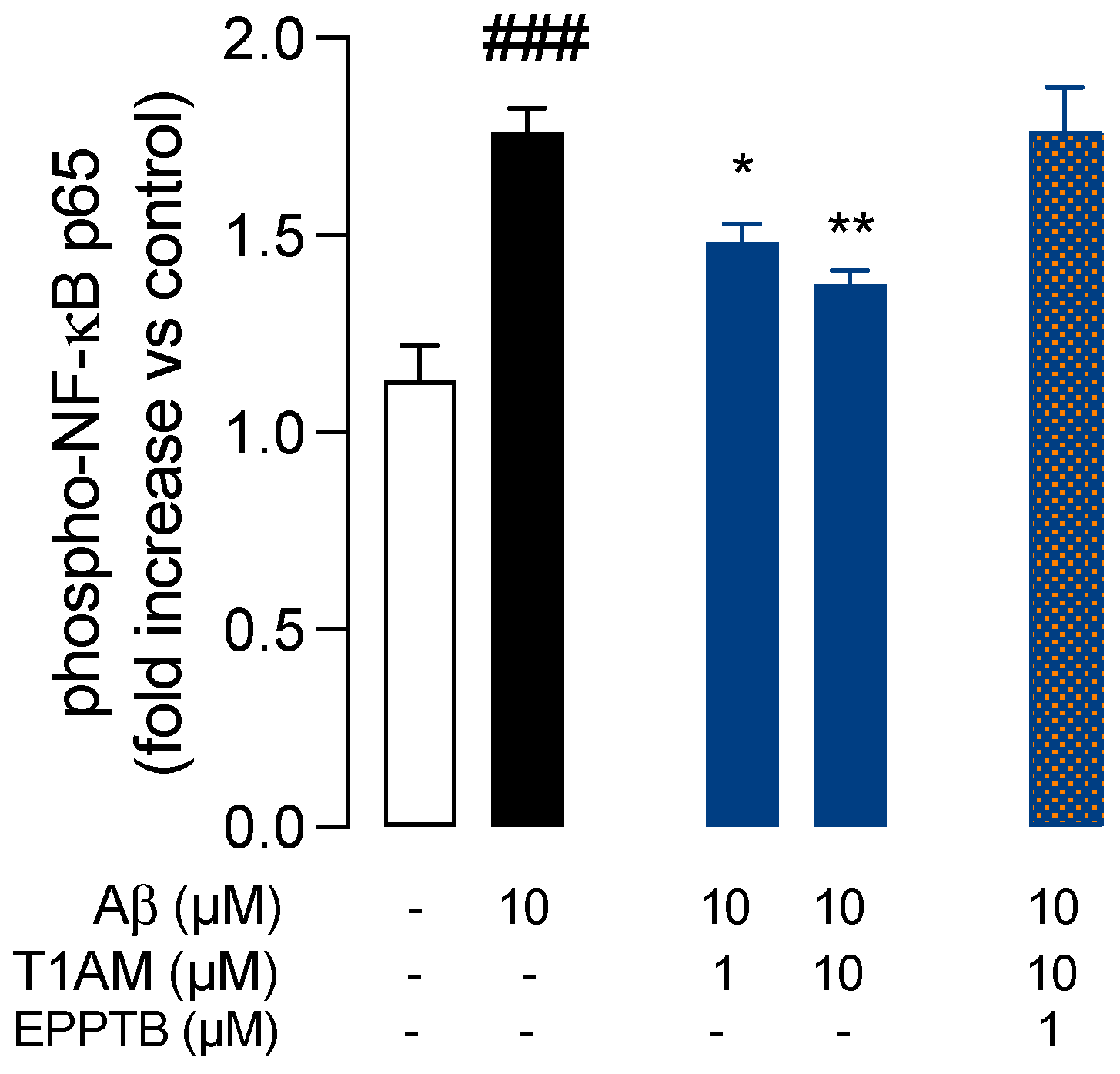
Dysregulation of the transcription factor NF-κB has been widely associated with AD, leading to glial cells activation and neuroinflammation [
38]. More importantly, the inactivation of microglial NF-κB has been shown to restore cognitive deficits and helped to reestablish a homeostatic phenotype in microglia [
39].
Therefore, we decided to evaluate the involvement of NF-κB signalling pathway in the beneficial effects observed with T
1AM in β-amyloid-induced HMC3 cells. Therefore, we repeated key Aβ25-35 and T1AM co-treatment experiments and evaluated NF-κB activity. The cells were then collected, and phospho- NF-κB P65 (p-P65) was detected in the cell lysates (
Figure 10). The results showed that Aβ25-35 treatment increased the phosphorylation level of P65 to activate the NF-κB pathway, and T1AM suppressed this response (
Figure 10). Notably, in the presence of TAAR1 selective antagonist EPPTB (1μM) the effect of T1AM on NF-κB activation was completely abolished (
Figure 10).
3. Discussion
Increasing evidence supports the concept that T1AM and TAAR1 signalling are part of an endogenous system that can be modulated to prevent neurodegeneration [
15,
17,
28,
40,
41,
42]. AD is the most frequent neurodegenerative disorder in the elderly, usually characterized by memory deficits and cognitive decline. Several studies have revealed that dysregulated microglial activation plays pivotal roles in the pathogenesis of AD. Therefore, ascertaining the ability of T1AM and other highly selective TAAR1 agonists to normalize factors that regulate microglia-mediated neuroinflammation would be a considerable advantage in the management of AD.
We have shown here that T1AM was able to reduce LPS/TNFα induced IL-6 in HMC3 human microglial cells, while increasing the production of anti-inflammatory interleukin IL-10, without affecting the cells’ viability. In addition, in LPS/TNFα induced HMC3 cells, treatment with T1AM was observed to decrease the expression of inflammatory response-related genes, including the monocyte chemoattract protein-1 (MCP1), the macrophage inflammatory protein-1 (MIP1), and the transcription factor NF-kB.
Regarding the mechanism of action, T1AM does not bind the nuclear thyroid hormone receptors (TRs) but it stimulates with nanomolar affinity TAAR1, a G protein-coupled receptor that recently emerged to have a role in immunomodulation [
41] and neuroinflammation [
40]. Nevertheless, there is currently not much information regarding TAAR1 expression in microglia [
43]. In the present study, by performing quantitative real time PCR analysis (qPCR) we demonstrated that TAAR1 is expressed in human microglial HMC3 cell line, and we found that after LPS/TNFα stimulation no changing levels of TAAR1 expression were observed in HMC3 cells.
Using a pharmacological approach, we demonstrated that inhibition of TAAR1 was sufficient to prevent T1AM anti-inflammatory effect on HMC3 cells, and conversely the stimulation of TAAR1 in the absence of T1AM was able to attenuate the LPS/TNFα-induced release of pro-inflammatory cytokines, as observed in T1AM-treated cells.
In this investigation, the pharmacokinetics results showed that T1AM was rapidly taken up by HMC3 cells and catabolized to TA1 by oxidative deamination. Since previous works have reported that TA1 may contribute, at least in part, to some effects elicited after the administration of exogenous T1AM [
28,
30,
32,
44], we checked whether TA1 administration could also decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells, but obtained negative results, confirming the specific anti-inflammatory effect of T1AM.
A great number of studies have documented the ability of Aβ fibrils to directly stimulate microglia in vitro to assume a neurotoxic phenotype characterized by secretion of a plethora of proinflammatory molecules, ultimately leading to neuron loss [
45,
46]. We found that aggregated Aβ25–35 peptide (10 μM, 24 h) significantly decreased viability of HMC3 microglial cells. This was concentration-dependently attenuated by T1AM (0.1–10 μM). Pretreatment with T1AM also suppressed the release of TNFα and pro-inflammatory IL-6, while increasing anti-inflammatory IL-10 levels. These effects were almost completely abolished by treatment with the TAAR1 antagonist EPPTB. In addition, Aβ induced activation of microglial NF-κB by phosphorylation. Application of T1AM attenuated this effect via TAAR1 activation, suggesting that the T1AM/TAAR1 system may protect microglial cells against Aβ-induced cell injury by inhibition of inflammation.
In summary, we provided for the first-time preliminary evidence that the T1AM-TAAR1 signalling pathway has the potential to normalize factors that regulate microglia-mediated neuroinflammation, further increasing the relevance of this system in the pathophysiology of AD. Nevertheless, additional investigations will be necessary to confirm the present findings and to evaluate whether they can be reproduced in vivo.
4. Materials and Methods
4.1. Drugs
T1AM and the TAAR1 antagonist N-(3-ethoxyphenyl)-4-(pyrrolidin-1-yl)-3-trifluoromethyl-benzamide (EPPTB) were purchased from Sigma-Aldrich (Milan, Italy); the TAAR1 agonist (S)-4-[(ethylphenylamino) methyl]-4,5-dihydrooxazol-2-ylamine (RO5166017) was kindly provided by Dr. Gainetdinov. T1AM metabolite 3-iodothyroacetic acid (TA1) was kindly provided by Dr. Scanlan. Aliquots were stored at −20 °C in DMSO as a 200 mM stock solution and diluted to the desired final concentration in culture media.
4.2. Analysis of T1AM and TA1
T1AM and its metabolite 3-iodothyroacetic acid (TA1) were assayed in samples by tandem mass spectrometry coupled to liquid chromatography (LC-MS/MS) by using a previously established procedure that allows the simultaneous detection of T1AM and TA1 in each sample [
19,
27]. T1AM and TA1 intracellular concentrations were also assayed by exposing cell lysate samples to the same LC-MS/MS procedure.
Briefly, aliquots (0.1 mL) from each sample collection were spiked with 10 μL of a suitable mixture of internal standards (deuterated T1AM and TA1). After adding methanol (0.4 mL), the samples were shaken for 10 min and centrifuged at 22780 ×g for 10 min. The supernatant was dried under a gentle stream of nitrogen, reconstituted with water/methanol mixture (70/30 by volume) and injected into the LC-MS-MS system. The latter included an Agilent 1290 UHPLC system (Santa Clara, CA, USA) coupled to an AB-Sciex API 4000 triple quadrupole mass spectrometer (Concord, ON, Canada).
4.3. Cell cultures and reagents
The human microglial clone 3 cell line (HMC3) (ATCC® CRL-3304™) was cultured in high glucose DMEM supplemented with 10% FBS, streptomycin (100 g/ml) and penicillin (100 U/mL) (Sigma-Aldrich, Milan, Italy).
LPS (Escherichia coli 0111:B4), TNFα, and Amyloid β-Peptide 25–35 (Aβ25-35) were purchased from Sigma-Aldrich (Milan, Italy).
4.4. MTT (Cell Viability Assay)
HMC3 cells were exposed to cell viability assays by using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) reagent. Briefly, HMC3 cells were exposed to increasing concentrations of T1AM (0.1 - 10 µM) and incubated at 37 °C for 24 h. Then, 0.5 mg/mL MTT reagent was added to each well, and the cells were incubated for 3 h at 37 °C. Next, 25 µL of the medium was removed from the wells, and 50 µL of DMSO was added. After incubating for 10 min at 37 °C, absorbance at 540 nm was determined with an automated microplate reader (BIO-TEK, Winooski, VT, USA). The percentage of cell viability was calculated as a percentage of vehicle-treated cells used as control. The same procedure was also followed to detect the cytotoxic effect produced in HMC3 cells after incubation with Aβ25-35 (1 and 10 µM, for 24 or 48 h) in the absence and presence of increasing concentrations of T1AM (0.1, 1 and 10μM).
4.5. Release of inflammatory molecules from LPS/TNFα-induced HMC3 Cells
Pro-inflammatory IL-6 and anti-inflammatory IL-10 levels were evaluated by specific ELISA assays [RAB0306 (IL-6) and RAB0244 (IL-10), Sigma-Aldrich, Milan, Italy] on collected culture media. Briefly, HMC3 cells were exposed to pretreatment with each of the compounds under investigation (i.e. T1AM, TA1 or RO51660170) for 1h followed by LPS (10 μg/mL)/TNFα (50 ng/mL) for 24 h, used as pro-inflammatory stimuli. Vehicle-treated cells were used as control. In competition experiments, the TAAR1 antagonist EPPTB (1 μM) was administered 15 min before proceeding with the administration of the selected TAAR1 agonist, namely T1AM or RO5166017.
4.6. Release of inflammatory molecules from Aβ25-35 -induced HMC3 Cells
The inflammatory response of HMC3 cells to Aβ25-35 exposure (10µM, 24h) was evaluated by performing specific ELISA assays. In addition to IL-6 and IL-10 measurements, performed as described above, the levels of tumor necrosis factor TNFα (RAB1089, Sigma-Aldrich, Milan, Italy), and nuclear factor kB (NF-kB) (85-86082-11, ThermoFisher Scientific, Carlsbad CA, USA) were also evaluated in collected culture media and in cell lysates, respectively, following the corresponding manufacturer’s instructions. Briefly, HMC3 cells were exposed to pretreatment with T1AM (1 or 10µM) for 1h followed by Aβ25-35 (10µM for 24 h), used as pro-inflammatory stimuli. Vehicle-treated cells were used as control. In competition experiments, the TAAR1 antagonist EPPTB (1 μM) was administered 15 min before proceeding with the administration of T1AM (10µM).
4.7. Gene Expression Analysis
Total RNA was extracted from HMC3 cells using the RNeasy Mini kit (74104, Qiagen, Hilden, Germany) following manufacturer protocol. RNA concentration and purity were determined by Nanodrop-1000 spectrophotometer and Qubit v.1 fluorometer plus Qubit RNA HS Assay Kit (Thermo Fisher Scientific, Wilmington, DE, USA).
Total RNA (1 μg) was retrotranscribed into first-strand cDNA by using by iScriptTM gDNA Clear cDNA Synthesis Kit (Bio-Rad, Milan, Italy) following manual protocol indications.
Relative quantity of gene transcripts was measured by real-time PCR on samples’cDNA using a SYBRGreen chemistry and an CFX Connect Real-Time PCR Detection System (Bio-Rad, Milan, Italy). The PCR cycle program consisted of an initial 30 s denaturation at 95 °C followed by 40 cycles of 5 s denaturation at 95 °C and 15 sec annealing/extension at 60 °C. A final melting protocol with ramping from 65 °C to 95 °C with 0.5 °C increments of 5 s was performed for verification of amplicon specificity and primer dimer formation.
Primers were designed with Beacon Designer Software v.8.0 (Premier Biosoft International, Palo Alto, CA, USA) with a junction primer strategy, whenever possible. In any case, negative control of retro-transcription was performed to exclude any interference from residual genomic DNA contamination. The primer sequences for RealTime-PCR are reported in
Table 2.
All reactions were done in triplicate and the amount of mRNA was calculated by the comparative critical threshold (CT) method. To account for possible variations related to cDNA input or the presence of PCR inhibitors, the endogenous reference gene GAPDH was simultaneously quantified for each sample, and data normalized accordingly.
Author Contributions
B.P. and G.C. designed the study and wrote the manuscript. C.R. and B. P. performed ELISA tests and collected biochemical data. B.P. and V.C. conducted gene expression studies. A.B. and C.R. carried out LC/MS-MS data collection. G.R., F.S., and R.Z. analyzed the data and discussed the results. All authors contributed to the final manuscript and approved the final version. The authors would like to thank the CISUP–Centre for Instrumentation Sharing–University of Pisa for having placed the Sciex QTrap 6500+ mass spectrometer, which was used for the T1AM assays, at the disposal of the authors.
Acknowledgments
This work was supported by a grant Pfizer (Project ID: 67562227; G.C.) and a grant from ETA (Project ID: 549901 to G.R.).
Conflicts of Interest
The authors declare no conflict of interest. The authors declare no competing financial interests.
References
- Li, Q.; Barres, B.A. Microglia and Macrophages in Brain Homeostasis and Disease. Nat Rev Immunol 2018, 18, 225–242. [Google Scholar] [CrossRef] [PubMed]
- Mecha, M.; Feliú, A.; Carrillo-Salinas, F.J.; Rueda-Zubiaurre, A.; Ortega-Gutiérrez, S.; de Sola, R.G.; Guaza, C. Endocannabinoids Drive the Acquisition of an Alternative Phenotype in Microglia. Brain, Behavior, and Immunity 2015, 49, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Reith, W. Neurodegenerative Erkrankungen. Radiologe 2018, 58, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; He, D.; Bai, Y. Microglia-Mediated Inflammation and Neurodegenerative Disease. Mol Neurobiol 2016, 53, 6709–6715. [Google Scholar] [CrossRef]
- Subhramanyam, C.S.; Wang, C.; Hu, Q.; Dheen, S.T. Microglia-Mediated Neuroinflammation in Neurodegenerative Diseases. Seminars in Cell & Developmental Biology 2019, 94, 112–120. [Google Scholar] [CrossRef]
- Chen, W.-W.; Zhang, X.; Huang, W.-J. Role of Neuroinflammation in Neurodegenerative Diseases (Review). Molecular Medicine Reports 2016, 13, 3391–3396. [Google Scholar] [CrossRef]
- Leng, F.; Edison, P. Neuroinflammation and Microglial Activation in Alzheimer Disease: Where Do We Go from Here? Nat Rev Neurol 2021, 17, 157–172. [Google Scholar] [CrossRef]
- Jucker, M.; Walker, L.C. Self-Propagation of Pathogenic Protein Aggregates in Neurodegenerative Diseases. Nature 2013, 501, 45–51. [Google Scholar] [CrossRef]
- Jellinger, K.A. Basic Mechanisms of Neurodegeneration: A Critical Update. Journal of Cellular and Molecular Medicine 2010. [Google Scholar] [CrossRef]
- Glass, C.K.; Saijo, K.; Winner, B.; Marchetto, M.C.; Gage, F.H. Mechanisms Underlying Inflammation in Neurodegeneration. Cell 2010, 140, 918–934. [Google Scholar] [CrossRef]
- Mosser, D.M.; Edwards, J.P. Exploring the Full Spectrum of Macrophage Activation. Nat Rev Immunol 2008, 8, 958–969. [Google Scholar] [CrossRef] [PubMed]
- Thameem Dheen, S.; Kaur, C.; Ling, E.-A. Microglial Activation and Its Implications in the Brain Diseases. CMC 2007, 14, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Lull, M.E.; Block, M.L. Microglial Activation and Chronic Neurodegeneration. Neurotherapeutics 2010, 7, 354–365. [Google Scholar] [CrossRef]
- Scanlan, T.S.; Suchland, K.L.; Hart, M.E.; Chiellini, G.; Huang, Y.; Kruzich, P.J.; Frascarelli, S.; Crossley, D.A.; Bunzow, J.R.; Ronca-Testoni, S.; et al. 3-Iodothyronamine Is an Endogenous and Rapid-Acting Derivative of Thyroid Hormone. Nature Medicine 2004, 10, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Bellusci, L.; Laurino, A.; Sabatini, M.; Sestito, S.; Lenzi, P.; Raimondi, L.; Rapposelli, S.; Biagioni, F.; Fornai, F.; Salvetti, A.; et al. New Insights into the Potential Roles of 3-Iodothyronamine (T1AM) and Newly Developed Thyronamine-Like TAAR1 Agonists in Neuroprotection. Frontiers in Pharmacology 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Bellusci, L.; Runfola, M.; Carnicelli, V.; Sestito, S.; Fulceri, F.; Santucci, F.; Lenzi, P.; Fornai, F.; Rapposelli, S.; Origlia, N.; et al. Endogenous 3-Iodothyronamine (T1AM) and Synthetic Thyronamine-Like Analog SG-2 Act as Novel Pleiotropic Neuroprotective Agents through the Modulation of SIRT6. Molecules 2020, 25, 1054. [Google Scholar] [CrossRef] [PubMed]
- Tozzi, F.; Rutigliano, G.; Borsò, M.; Falcicchia, C.; Zucchi, R.; Origlia, N. T1AM-TAAR1 Signalling Protects against OGD-Induced Synaptic Dysfunction in the Entorhinal Cortex. Neurobiology of Disease 2021, 151, 105271. [Google Scholar] [CrossRef] [PubMed]
- Landucci, E.; Gencarelli, M.; Mazzantini, C.; Laurino, A.; Pellegrini-Giampietro, D.E.; Raimondi, L. N-(3-Ethoxy-Phenyl)-4-Pyrrolidin-1-Yl-3-Trifluoromethyl-Benzamide (EPPTB) Prevents 3-Iodothyronamine (T1AM)-Induced Neuroprotection against Kainic Acid Toxicity. Neurochemistry International 2019, 129, 104460. [Google Scholar] [CrossRef]
- di Leo, N.; Moscato, S.; Borso’, M.; Sestito, S.; Polini, B.; Bandini, L.; Grillone, A.; Battaglini, M.; Saba, A.; Mattii, L.; et al. Delivery of Thyronamines (TAMs) to the Brain: A Preliminary Study. Molecules 2021, 26, 1616. [Google Scholar] [CrossRef]
- Dello Russo, C.; Cappoli, N.; Coletta, I.; Mezzogori, D.; Paciello, F.; Pozzoli, G.; Navarra, P.; Battaglia, A. The Human Microglial HMC3 Cell Line: Where Do We Stand? A Systematic Literature Review. J Neuroinflammation 2018, 15, 259. [Google Scholar] [CrossRef]
- Merighi, S.; Nigro, M.; Travagli, A.; Gessi, S. Microglia and Alzheimer’s Disease. IJMS 2022, 23, 12990. [Google Scholar] [CrossRef] [PubMed]
- Gado, F.; Ferrisi, R.; Polini, B.; Mohamed, K.A.; Ricardi, C.; Lucarini, E.; Carpi, S.; Domenichini, F.; Stevenson, L.A.; Rapposelli, S.; et al. Design, Synthesis, and Biological Activity of New CB2 Receptor Ligands: From Orthosteric and Allosteric Modulators to Dualsteric/Bitopic Ligands. J. Med. Chem. 2022, 65, 9918–9938. [Google Scholar] [CrossRef] [PubMed]
- Ferrisi, R.; Gado, F.; Polini, B.; Ricardi, C.; Mohamed, K.A.; Stevenson, L.A.; Ortore, G.; Rapposelli, S.; Saccomanni, G.; Pertwee, R.G.; et al. Design, Synthesis and Biological Evaluation of Novel Orthosteric-Allosteric Ligands of the Cannabinoid Receptor Type 2 (CB2R). Front. Chem. 2022, 10, 984069. [Google Scholar] [CrossRef] [PubMed]
- Ferrisi, R.; Polini, B.; Ricardi, C.; Gado, F.; Mohamed, K.A.; Baron, G.; Faiella, S.; Poli, G.; Rapposelli, S.; Saccomanni, G.; et al. New Insights into Bitopic Orthosteric/Allosteric Ligands of Cannabinoid Receptor Type 2. IJMS 2023, 24, 2135. [Google Scholar] [CrossRef] [PubMed]
- Ghelardoni, S.; Chiellini, G.; Frascarelli, S.; Saba, A.; Zucchi, R. Uptake and Metabolic Effects of 3-Iodothyronamine in Hepatocytes. Journal of Endocrinology 2014, 221, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Assadi-Porter, F.; Reiland, H.; Sabatini, M.; Lorenzini, L.; Carnicelli, V.; Rogowski, M.; Selen Alpergin, E.; Tonelli, M.; Ghelardoni, S.; Saba, A.; et al. Metabolic Reprogramming by 3-Iodothyronamine (T1AM): A New Perspective to Reverse Obesity through Co-Regulation of Sirtuin 4 and 6 Expression. International Journal of Molecular Sciences 2018, 19, 1535. [Google Scholar] [CrossRef] [PubMed]
- Saba, A.; Chiellini, G.; Frascarelli, S.; Marchini, M.; Ghelardoni, S.; Raffaelli, A.; Tonacchera, M.; Vitti, P.; Scanlan, T.S.; Zucchi, R. Tissue Distribution and Cardiac Metabolism of 3-Iodothyronamine. Endocrinology 2010, 151, 5063–5073. [Google Scholar] [CrossRef]
- Accorroni, A.; Rutigliano, G.; Sabatini, M.; Frascarelli, S.; Borsò, M.; Novelli, E.; Bandini, L.; Ghelardoni, S.; Saba, A.; Zucchi, R.; et al. Exogenous 3-Iodothyronamine Rescues the Entorhinal Cortex from β-Amyloid Toxicity. Thyroid 2020, 30, 147–160. [Google Scholar] [CrossRef]
- Siemian, J.N.; Zhang, Y.; Li, J.-X. Trace Amine-Associated Receptor 1 Agonists RO5263397 and RO5166017 Attenuate Quinpirole-Induced Yawning but Not Hypothermia in Rats. Behavioural Pharmacology 2017, 28, 590–593. [Google Scholar] [CrossRef]
- Laurino, A.; Landucci, E.; Raimondi, L. Central Effects of 3-Iodothyronamine Reveal a Novel Role for Mitochondrial Monoamine Oxidases. Front. Endocrinol. 2018, 9, 290. [Google Scholar] [CrossRef]
- Laurino, A.; De Siena, G.; Saba, A.; Chiellini, G.; Landucci, E.; Zucchi, R.; Raimondi, L. In the Brain of Mice, 3-Iodothyronamine (T1AM) Is Converted into 3-Iodothyroacetic Acid (TA1) and It Is Included within the Signaling Network Connecting Thyroid Hormone Metabolites with Histamine. European Journal of Pharmacology 2015, 761, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Musilli, C.; De Siena, G.; Manni, M.E.; Logli, A.; Landucci, E.; Zucchi, R.; Saba, A.; Donzelli, R.; Passani, M.B.; Provensi, G.; et al. Histamine Mediates Behavioural and Metabolic Effects of 3-Iodothyroacetic Acid, an Endogenous End Product of Thyroid Hormone Metabolism: A Novel Link between Thyroid and Histamine. Br J Pharmacol 2014, 171, 3476–3484. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Liang, D.; Chen, Y.; Xie, Y.; Wang, Y.; Wang, L.; Wang, Z.; Qiao, Z. Gx-50 Reduces β-Amyloid-Induced TNF-α, IL-1β, NO, and PGE 2 Expression and Inhibits NF-ΚB Signaling in a Mouse Model of Alzheimer’s Disease. Eur. J. Immunol. 2016, 46, 665–676. [Google Scholar] [CrossRef]
- Cisbani, G.; Rivest, S. Targeting Innate Immunity to Protect and Cure Alzheimer’s Disease: Opportunities and Pitfalls. Mol Psychiatry 2021, 26, 5504–5515. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-Y.; Bian, J.-S. Hydrogen Sulfide Protects Amyloid-β Induced Cell Toxicity in Microglia. JAD 2011, 22, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Ranaivo, H.R.; Craft, J.M.; Hu, W.; Guo, L.; Wing, L.K.; Van Eldik, L.J.; Watterson, D.M. Glia as a Therapeutic Target: Selective Suppression of Human Amyloid-β-Induced Upregulation of Brain Proinflammatory Cytokine Production Attenuates Neurodegeneration. J. Neurosci. 2006, 26, 662–670. [Google Scholar] [CrossRef]
- Naldi, M.; Fiori, J.; Pistolozzi, M.; Drake, A.F.; Bertucci, C.; Wu, R.; Mlynarczyk, K.; Filipek, S.; De Simone, A.; Andrisano, V. Amyloid β-Peptide 25–35 Self-Assembly and Its Inhibition: A Model Undecapeptide System to Gain Atomistic and Secondary Structure Details of the Alzheimer’s Disease Process and Treatment. ACS Chem. Neurosci. 2012, 3, 952–962. [Google Scholar] [CrossRef]
- Mattson, M.P.; Camandola, S. NF-ΚB in Neuronal Plasticity and Neurodegenerative Disorders. J. Clin. Invest. 2001, 107, 247–254. [Google Scholar] [CrossRef]
- Wang, Chao; Fan, Li; Khawaja, Rabia; Liu, Bangyan; Zhan, Lihong; Kodama, Lay; Chin, Marcus; Li, Yaqiao; Le, David; Zhou, Yungui; et al. Data from: Microglial NF-ΚB Drives Tau Spreading and Toxicity in a Mouse Model of Tauopathy. 2022. [CrossRef]
- Barnes, D.A.; Galloway, D.A.; Hoener, M.C.; Berry, M.D.; Moore, C.S. TAAR1 Expression in Human Macrophages and Brain Tissue: A Potential Novel Facet of MS Neuroinflammation. IJMS 2021, 22, 11576. [Google Scholar] [CrossRef]
- Christian, S.L.; Berry, M.D. Trace Amine-Associated Receptors as Novel Therapeutic Targets for Immunomodulatory Disorders. Front. Pharmacol. 2018, 9, 680. [Google Scholar] [CrossRef]
- Rutigliano, G.; Accorroni, A.; Zucchi, R. The Case for TAAR1 as a Modulator of Central Nervous System Function. Front. Pharmacol. 2018, 8, 987. [Google Scholar] [CrossRef] [PubMed]
- Fleischer, L.M.; Somaiya, R.D.; Miller, G.M. Review and Meta-Analyses of TAAR1 Expression in the Immune System and Cancers. Front. Pharmacol. 2018, 9, 683. [Google Scholar] [CrossRef] [PubMed]
- Laurino, A.; Gencarelli, M.; Raimondi, L. The 3-Iodothyronamine (T1AM) and the 3-Iodothyroacetic Acid (TA1) Indicate a Novel Connection with the Histamine System for Neuroprotection. European Journal of Pharmacology 2021, 912, 174606. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, H.; Arai, T.; Kondo, H.; Tanno, E.; Haga, C.; Ikeda, K. Cell Mediators of Inflammation in the Alzheimer Disease Brain: Alzheimer Disease and Associated Disorders 2000, 14, S47–S53. 14. [CrossRef]
- Gabrielli, M.; Prada, I.; Joshi, P.; Falcicchia, C.; D’Arrigo, G.; Rutigliano, G.; Battocchio, E.; Zenatelli, R.; Tozzi, F.; Radeghieri, A.; et al. Microglial Large Extracellular Vesicles Propagate Early Synaptic Dysfunction in Alzheimer’s Disease. Brain 2022, 145, 2849–2868. [Google Scholar] [CrossRef]
Figure 1.
Diagram of microglia activation.Resting microglia may turn into distinct phenotypes, namely, M1 phenotype and M2 phenotype. M1 classical state releases pro-inflammatory cytokines and cytotoxic substances, including IL-1ß, IL-6, TNFα and ROS, inducing neurological damage. On the other hand, the M2 alternative state produces anti-inflammatory cytokines, such as IL-10, able to inhibit the production of pro-inflammatory cytokines by microglia, thus exerting a neuroprotective role in the CNS.
Figure 1.
Diagram of microglia activation.Resting microglia may turn into distinct phenotypes, namely, M1 phenotype and M2 phenotype. M1 classical state releases pro-inflammatory cytokines and cytotoxic substances, including IL-1ß, IL-6, TNFα and ROS, inducing neurological damage. On the other hand, the M2 alternative state produces anti-inflammatory cytokines, such as IL-10, able to inhibit the production of pro-inflammatory cytokines by microglia, thus exerting a neuroprotective role in the CNS.
Figure 2.
Release of pro- and anti-inflammatory interleukins, IL-6 (A) and IL-10 (B), induced by different concentrations of T1AM. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. **p < 0.01 and ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Figure 2.
Release of pro- and anti-inflammatory interleukins, IL-6 (A) and IL-10 (B), induced by different concentrations of T1AM. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. **p < 0.01 and ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Figure 3.
T1AM decreases the expression of inflammatory response-related genes stimulated by LPS/TNFα treatment in HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05, **p < 0.01 and ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ##p <0.01 and ###p <0.005 compared to vehicle treated cells used as control.
Figure 3.
T1AM decreases the expression of inflammatory response-related genes stimulated by LPS/TNFα treatment in HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05, **p < 0.01 and ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ##p <0.01 and ###p <0.005 compared to vehicle treated cells used as control.
Figure 4.
MTT assay performed with different concentrations of T1AM. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test.
Figure 4.
MTT assay performed with different concentrations of T1AM. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test.
Figure 5.
Real time quantification of TAAR1 expression in HMC3 cells before and after exposure to LPS (10 μg/mL)/TNFα (50ng/ml) treatment for 24 h. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary Student t test.
Figure 5.
Real time quantification of TAAR1 expression in HMC3 cells before and after exposure to LPS (10 μg/mL)/TNFα (50ng/ml) treatment for 24 h. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary Student t test.
Figure 6.
Ability of T1AM to decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells by the modulation of TAAR1. Bars represent the release (pg/mL) of IL-6 (A) and IL-10 (B) in the presence of the drugs at the indicated concentrations. Data represent means ± S.E.M. from independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ###p < 0.005 compared to vehicle treated cells used as control.
Figure 6.
Ability of T1AM to decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells by the modulation of TAAR1. Bars represent the release (pg/mL) of IL-6 (A) and IL-10 (B) in the presence of the drugs at the indicated concentrations. Data represent means ± S.E.M. from independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ***p < 0.005 compared to cells treated with LPS (10 μg/mL)/TNFα (50ng/ml) for 24 h; ###p < 0.005 compared to vehicle treated cells used as control.
Figure 7.
3-iodothyroacetic acid TA1 does not decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ###p < 0.005 compared to vehicle treated cells used as control.
Figure 7.
3-iodothyroacetic acid TA1 does not decrease the inflammatory phenotype of LPS/TNFα-stimulated HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ###p < 0.005 compared to vehicle treated cells used as control.
Figure 8.
MTT assays in HMC3 cells exposed to Aβ. (A) Effects on HMC3 cells viability of treatment with β-amyloid peptide 25-35 (Aβ) at 1 and 10 μM for 24 or 48h. (B) Effects on HMC3 cells viability of pretreatment with T1AM at 0.1, 1 and 10μM, followed by exposure to 10µM Aβ for 24 h. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05, **p < 0.01 compared to cells treated with 10µM Aβ for 24 h; ##p < 0.01; ###p < 0.005 compared to vehicle treated cells used as control.
Figure 8.
MTT assays in HMC3 cells exposed to Aβ. (A) Effects on HMC3 cells viability of treatment with β-amyloid peptide 25-35 (Aβ) at 1 and 10 μM for 24 or 48h. (B) Effects on HMC3 cells viability of pretreatment with T1AM at 0.1, 1 and 10μM, followed by exposure to 10µM Aβ for 24 h. Data represent means ± S.E.M. from three independent experiments, performed in triplicate (n=3). Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05, **p < 0.01 compared to cells treated with 10µM Aβ for 24 h; ##p < 0.01; ###p < 0.005 compared to vehicle treated cells used as control.
Figure 9.
T1AM pretreatment modulate the release of pro-inflammatory (TNF-α, IL-6) and anti-inflammatory (IL-10) interleukins in Aβ-induced HMC3 cells. Bars represent the release (pg/mL) of TNF-α (A), IL-6 (B) and IL-10 (C) in the presence of the drugs at the indicated concentrations. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ***p < 0.005 compared to cells exposed to Aβ 10 µM for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Figure 9.
T1AM pretreatment modulate the release of pro-inflammatory (TNF-α, IL-6) and anti-inflammatory (IL-10) interleukins in Aβ-induced HMC3 cells. Bars represent the release (pg/mL) of TNF-α (A), IL-6 (B) and IL-10 (C) in the presence of the drugs at the indicated concentrations. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. ***p < 0.005 compared to cells exposed to Aβ 10 µM for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Figure 10.
TAAR1 activation modulate the phosphorylation of NF-kB (NF-kB p65) in Aβ-induced HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05 and **p < 0.01 compared to cells exposed to Aβ 10 µM for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Figure 10.
TAAR1 activation modulate the phosphorylation of NF-kB (NF-kB p65) in Aβ-induced HMC3 cells. Data represent means ± S.E.M. from three independent experiments (n=3), performed in duplicate. Statistical analysis was performed by ordinary one-way ANOVA followed by Tukey’s multiple comparison test. *p < 0.05 and **p < 0.01 compared to cells exposed to Aβ 10 µM for 24 h; ###p <0.005 compared to vehicle treated cells used as control.
Table 1.
| Time (min) |
Medium |
Cell Lisates |
| T1AM (nM) |
TA1 (nM) |
T1AM (nM) |
TA1 (nM) |
| 0 |
N.D. |
N.D. |
N.D. |
N.D. |
| 5 |
64.1 ± 2.70 |
0.31 ± 0.02 |
26.0 ± 0.28 |
0.06 ± 0.01 |
| 15 |
57.2 ± 5.40 |
0.66 ± 0.20 |
24.9 ± 0.74 |
0.12 ± 0.02 |
| 30 |
56.7 ± 8.10 |
1.33 ± 0.15 |
27.0 ± 0.30 |
0.14 ± 0.02 |
| 60 |
53.4 ± 3.60 |
3.81 ± 0.80 |
24.46 ± 0.81 |
0.23 ± 0.04 |
Table 2.
Primer sequences of target genes.
Table 2.
Primer sequences of target genes.
Reference Sequence
(RefSeq) RNA |
Gene Symbol |
Primer Sequences |
| NM_002046 |
GAPDH |
F) 5’-CCCTTCATTGACCTCAACTACATG |
| R) 5’-TGGGATTTCCATTGATGACAAGC |
| NM_002982.4 |
MCP1 |
F) 5’-GAGAGGCTGAGACTAACC |
| R) 5’-TGATTGCATCTGGCTGAG |
| NM_002983 |
MIP1 |
F) 5’- ACTTTGAGACGAGCAGCCAGTG |
| R) 5’- TTTCTGGACCCACTCCTCACTG |
| NM_001404662 |
NFKB |
F) 5’-CCTTTCTCATCCCATCTTT |
| R) 5’-CCTCAATGTCCTCTTTCTG |
| NM_138327 |
TAAR1 |
F) 5’- GAGATCTGCTGAGCACTGTTGG |
| R) 5’- CAGCATAGTAGCGGTCAATGGAG |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).