Background
Peripheral venous catheters are the most widely used invasive devices in hospitals, with a prevalence rate of 66% among patients admitted to Catalan hospitals [1-2]. However, they are often used excessively and inappropriately, particularly when the peripheral intravenous line is not the preferred treatment option [
3]. Furthermore, peripheral venous catheters are associated with a high incidence of minor local complications, resulting in additional costs for both patients and healthcare providers [
4]. Research indicates that over 73% of patients may contract a healthcare-associated infection due to the presence of a peripheral venous catheter [
5]. Additionally, some studies suggest that retaining an unused catheter in a patient may increase the risk of developing potentially avoidable complications by more than 25% [
6]. The most relevant complications that require catheter replacement include phlebitis, obstruction, infiltration and extravasation [
4,
7].
On the other hand, the use of peripherally inserted central catheters and midline catheters is growing due to the numerous benefits they offer to patients and healthcare providers. In the first case, they increase patient safety and satisfaction by preserving venous capital and eliminating the discomfort caused by multiple venous punctures [8-9]. In the second case, they could optimize the use of resources if a peripherally inserted central catheter or a midline catheter could replace various peripheral venous catheters.
Due to the numerous benefits of using peripherally inserted central catheters and midline catheters, as well as the drawbacks associated with peripheral venous catheters, more hospitals are creating vascular access specialist teams. These teams are formed by nurses who are specially trained in the insertion and maintenance of peripherally inserted central catheters and midline catheters, utilizing ultrasound support during insertion [
10]. Several studies suggest that this method is more cost-effective [11-12]: on one hand, it offers greater accuracy during insertion and a higher success rate of venipunctures, which eliminates the need of an X-ray to confirm correct catheter placement [
13]; on the other hand, patients are less likely to develop healthcare-associated infections [
5]. In addition, it increases patient satisfaction due to greater comfort, reduced pain sensation, greater patient mobility and decreased length of hospital stay [
11,
13,
14]. Nevertheless, the Cochrane Library conducted a systematic review to compare the effectiveness of the vascular access specialist team with the generalist model commonly used in hospitals and other medical centers, concluding that there is currently insufficient high-quality evidence to either support or reject the implementation of a vascular access specialist team [
15].
Healthcare-associated infections affect 5-10% of patients admitted to a hospital [
13] and are a major burden on the healthcare system, as when they occur they lead to a 77% increase in cost per patient (31% of this increase caused by pharmacy costs, 31% by materials and services, 24% by increased hospital stay and 14% by laboratory costs) [
16]. In addition, healthcare-associated infections are associated with additional complications, which in the worst-case scenario can result in the death of the patient. Some studies estimate that 6% of patients with healthcare-associated infections eventually die from it [
17]. The most common healthcare-associated infections associated with catheter use are bacteremia and phlebitis of infectious origin [
13]. In the case of bacteremia, an episode due to a peripheral venous catheter infection, might increase hospital costs by €18,078 [
18] and the patient's stay tends to be longer and much more expensive [
19]. Moreover, if it happens, the probability of mortality rises to 1.7% [
20,
21]. In case of infectious phlebitis due to peripheral venous catheters, several studies report a prevalence between 3% and 12% [
3,
22].
Despite the economic impact of healthcare-associated infections on the healthcare system, there is a lack of up-to-date data in Catalonia that can accurately determine the direct and indirect costs of this type of infections. In 2015, it was estimated that the cost represented by peripheral venous catheter bacteremia in Catalan hospitals was above 12 million euros, a cost that had already been reduced by approximately 10 million euros during the 2008-2013 period thanks to the implementation of healthcare-associated infection surveillance initiatives such as the VINCat Programme, the Bacteremia Zero Programme and the local programmes initiated by care teams [
23].
The Germans Trias i Pujol University Hospital is a public healthcare center that provides highly complex medical care to a reference population of 800,000 inhabitants in the Northern Metropolitan Health Region of Barcelona. The hospital is part of the Catalan Health Institute, which is the largest provider of healthcare services in Catalonia. In 2019, the hospital had an annual activity that included 37,000 discharges, 426,000 outpatient consultations, 17,000 major surgical interventions and 146,000 emergency visits. Despite the frequent use of venous catheters (approximately 80% of its patients carry one at some point during their hospital stay), in 2022, the hospital had not yet established a vascular access specialist team. A survey conducted in 2019 by the hospital's Infection Control Unit indicated that 71% of nurses do not use peripherally inserted central catheters and midline catheters when they are indicated, despite their potential benefits to patients and the hospital. Nurses cited a lack of skills and the pressure of care as the main reasons for not using these devices.
In this context, given the potential benefits of using an ultrasound-guided technique for the insertion of peripherally inserted central catheters and midline catheters, the hospital is considering adopting a vascular access specialist team. The aim of this study is to conduct a cost-benefit analysis of the substitution of the catheters currently used in the hospital by ultrasound-guided catheters, in order to demonstrate the important economic impact of this measure before implementing it.
Methods
Description of the intervention
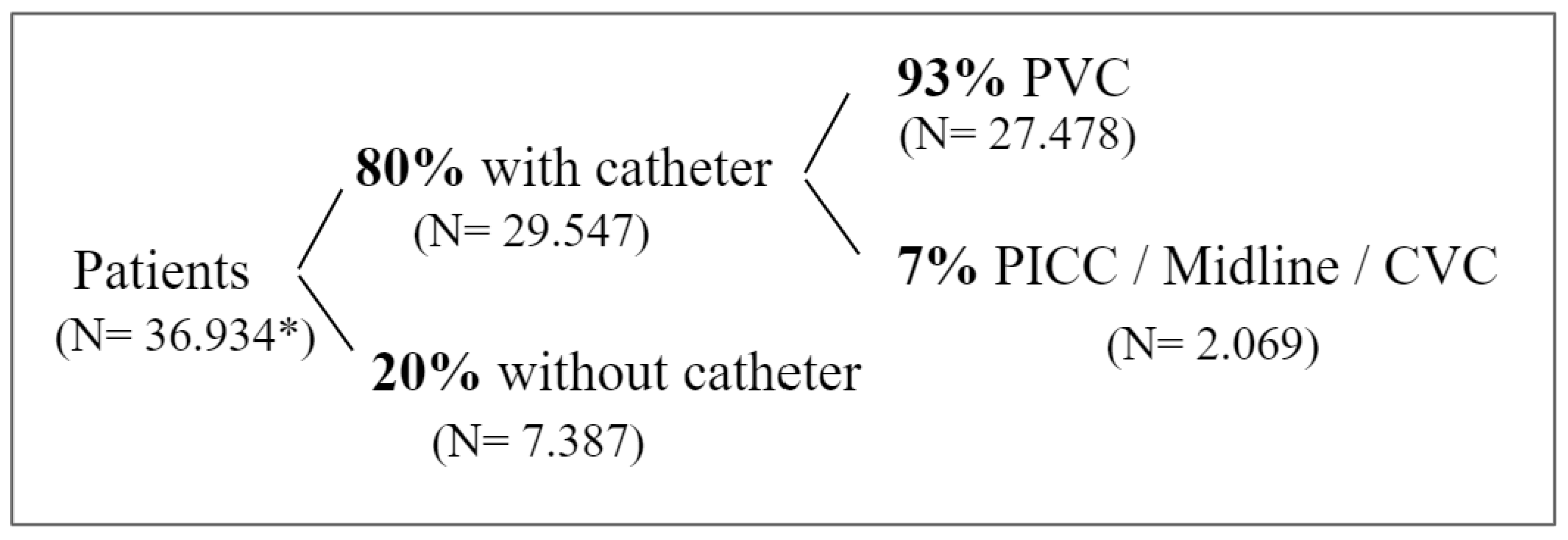
According to venous catheter prevalence data, approximately 80% of the patients hospitalized in the hospital carry a venous catheter at some point during their stay (
Figure 1). Among this proportion, the most frequently used type of catheters are peripheral venous catheters (93%) while other types such as peripherally inserted central catheters, midline catheters and central venous catheters are used in a smaller proportion of cases. The implementation of a vascular access specialist team aims to reduce the use of peripheral venous catheters, peripherally inserted central catheters and midline catheters and increase the use of ultrasound-guided peripherally inserted central catheters and midline catheters in those patients whose clinical characteristics require it. The team will work in collaboration with the Healthcare-associated infections Infection Control Nursing Team to develop and evaluate protocols related to the correct use of the different types of catheter and will monitor the evolution of clinical evidence and implement changes in practice accordingly.
The team will attend patients who are hospitalized in the semi-critical and acute care units, as well as those receiving care at home or in the emergency room. Patients admitted to critical care units will not be attended by the team, as the nursing professionals in those units are already experienced in ultrasound-guided insertion of this type of catheter. Moreover, as most of the central venous catheters are only used in this unit, the new team will not replace this type of catheter. The decision regarding the most suitable type of catheter for a patient is determined by a hospital-implemented decision algorithm. Factors such as medication pH and osmolarity levels, potential damage to the vein’s intimal layer, type and duration of treatment and the patient's clinical history are taken into consideration by the algorithm to determine the appropriate type of catheter and the need for team intervention.
The team will initially consist of two nursing professionals which will be substituted in case of illness or absence due to incapacity or during vacation periods, following the implementation model of other hospitals that already have a vascular access specialist team. Their work schedule does not include night or weekend shifts, so if the algorithm indicates the need for the team’s intervention for patients hospitalized during these time slots, an alternative type of catheter will be placed until the team returns and performs the assessment.
Based on estimations provided by the hospital’s nursing staff and taking into consideration the time required to insert each catheter, the working day and experiences from other hospitals, it is expected that each member of the team can insert an average of five catheters per day. With two team members and assuming 250 working days in a year, the hospital’s annual capacity for catheter insertions would be 2,500. As
Figure 1 shows, the number of patients needing catheters is higher. However, it will be the algorithm that specifies the exact number of catheters the team should insert. Depending on the team’s performance and capacity to attend all patients indicated by the algorithm, the number of team members could be increased.
Study design
An ex ante cost-benefit analysis was conducted from the healthcare provider perspective. On one hand, it has been estimated the reduction in resources used when replacing peripherally inserted central catheters, midline catheters and peripheral venous catheters with the ultrasound-guided peripherally inserted central catheters and midline catheters. On the other hand, the additional resources required for the use of the ultrasound-guided peripherally inserted central catheters and midline catheters have also been studied.
Data
The total costs of the ultrasound-guided peripherally inserted central catheters and midline catheters placement were calculated by quantifying the material costs and the practitioner’s time burden associated with catheter placement, assuming a peripherally inserted central catheter or a midline catheter could can replace an average of three peripheral venous catheters. In contrast, the total benefits were calculated by quantifying the reduction in resources used from eliminating confirmatory radiography and peripheral venous catheters material, as well as the reduction in staff burden. Additionally, the reduction of bacteremia and hospital stay due to the elimination of phlebitis was also quantified. The costs were obtained from the hospital administrative database and were measured in monetary units (euros 2021). No discount rate was used.
Outcome measures
Benefits and costs have been classified into the following categories: personnel, material, confirmatory radiographies and possible complications (
Table 1).
On one hand, in terms of personnel costs, the cost of hiring each nursing professional for the vascular access specialist team is estimated at approximately €53,583 (annual cost to the company). The monetary value of workload relief for the nursing staff provided by the new team was calculated by multiplying company’s hourly cost supported for each worker (€32.63 per hour) by the time required for professionals to perform the insertion of different catheters: approximately 60 minutes for peripherally inserted central catheter, 40 minutes for ultrasound-guided peripherally inserted central catheter, 40 minutes for a midline catheter, 20 minutes for an ultrasound-guided midline catheter and 22.5 minutes (7.5 minutes multiplied by an average of 3 peripheral venous catheters insertions per episode) in the case of peripheral venous catheter. The result of the quantification of the workload relief is €32.63 per intervention for a peripherally inserted central catheter, €21.75 per intervention for an ultrasound-guided peripherally inserted central catheter, €21.75 per intervention for a midline catheter, €10.88 per intervention for an ultrasound-guided midline catheter and €12.24 per 3 peripheral venous catheters insertions.
On the other hand, the cost of peripherally inserted central catheters material is close to €56.31, which is calculated as the weighted average of the prices of different types of peripherally inserted central catheters used in the hospital in 2021. The cost of materials for an ultrasound-guided peripherally inserted central catheter is the same. Similarly, the material cost for a midline catheter is approximately €34, which is the same as the material cost for an ultrasound-guided midline catheter. The cost of the peripheral venous catheters is approximately €0.68 (€2.06 for three units). The cost of the ultrasound scanner used for ultrasound-guided insertion is not included, as it is accounted for in the cost of the material used for each catheter placement. The cost of the X-ray required to verify the correct placement of the peripherally inserted central catheters is estimated to be around €15 [
24].
Finally, it has been taken into account the potential benefits resulting from the reduction of complications and infections through the incorporation of trained professionals for the introduction of ultrasound-guided peripherally inserted central catheters and midline catheters. Firstly, replacing peripheral venous catheters with peripherally inserted central catheters or midline catheters may lead to a reduction in the length of hospital stay due to decreased infections and complications. The value of this reduction in length of stay was estimated by multiplying the probability of phlebitis occurring with peripheral venous catheters (12% according to our own data) with the average cost of increased length of stay (€674 per 24-hour stay [
24], for an estimated increase of 1.5 days, based on our own data). Secondly, the decrease in the number of bacteremias associated with both peripheral venous catheters and peripherally inserted central/midline catheters implies a reduction in resource utilization. This value was calculated by multiplying the number of episodes of bacteremias related to the selection and insertion of peripheral venous catheters and peripherally inserted central/midline catheters at the Germans Trias i Pujol University Hospital (9 in 2021, according to our own data) with the cost associated with a patient developing this infection (€18,078) [
18], and then dividing this value by the total number of patients with any type of catheter (29,547). Therefore, the reduction in the number of bacteremias derived from replacing every three peripheral venous catheters or one peripherally inserted central catheter with an ultrasound-guided peripherally inserted central catheter, or every three peripheral venous catheters or one midline catheter with an ultrasound-guided midline catheter, represents a quantifiable reduction in resources of approximately €5.50.
Discussion
The economic analysis of implementing a vascular access specialist team at the Germans Trias i Pujol University Hospital suggests that it can result in significant resource savings by replacing catheters, while concurrently improving patient safety and well-being by reducing the risk of phlebitis and bacteremia. The replacement of peripheral venous catheters with peripherally inserted central catheters or midline catheters yields the highest reduction in resources, especially in the second case. Moreover, in both cases, the primary driver of cost reduction is the potential decrease in hospital stay due to lower risk of phlebitis. These findings suggest that prioritizing the replacement of peripheral venous catheters, rather than peripherally inserted central catheters or midline catheters inserted without ultrasound guidance, is more beneficial for both patients and the hospital.
Previous studies have concluded that the replacement of catheters with ultrasound-guided peripherally inserted central catheters is cost-effective [
8,
9,
10]. However, to our knowledge, there is no evidence of studies analyzing the cost-benefit of the implantation of a vascular access specialist team that replaces catheters with peripherally inserted central catheters and midline catheters. Gosselin et al [
25] analyzed the cost-effectiveness of the introduction of a vascular access specialist team specialized in the insertion of ultrasound-guided peripherally inserted central catheters, and found that the reduction in resources derived from peripherally inserted central catheters replacement was approximately double from our study (€65 vs. €31). Although this reduction is similar in terms of material resources, in contrast to our study, they considered the cost of disinfecting the room and patient transport, but did not incorporate the increase in resources derived from healthcare-associated infections. Tan et al [
11] have also analyzed the cost-effectiveness of peripherally inserted central catheters replacement. They suggested that the benefits become visible six months after introducing the team in the hospital. They also highlighted the greater comfort for patients and the reduced time for catheter insertion and complications associated with the new catheters. In this sense, a study carried out in Catalonia has estimated the cost of a patient with bacteremia, suggesting an increase in resources of €18,078 [
18], although other studies indicate a potentially higher cost of €21,506 [
26]. These findings suggest that the cost savings associated with introducing the team in our study may be conservative, and the actual cost benefits could potentially be even greater.
In the case of midline catheters, a study comparing their effectiveness with that of peripheral venous catheters demonstrates that midline catheters significantly reduce complications associated with peripheral venous catheters, such as phlebitis, infiltrations, asymptomatic thrombosis, occlusions and accidental removals. The study supports our conclusion and suggests that although midline catheters may have higher costs, these are compensated by the complications prevented, and that patients also prefer midline catheters [
27]. A study conducted by Moulin et al [
28] proposes that ultrasound-guided midline catheters are a good alternative to peripheral venous catheters in cases of prolonged treatment when peripherally inserted central catheters placement is not feasible. Moreover, the study adds that, in addition to the reduction in the risk of healthcare-associated infections, the main benefits for patients with this type of catheter are that it can be inserted at the patient's bedside, does not require a confirmatory X-ray and allows to obtain repeated blood samples without additional punctures.
The hospital’s guidelines are in line with the recommendations of the Catalan Agency for Health Quality and Evaluation [
1], which emphasize the appropriate use of catheters in clinical practice to reduce healthcare-associated infections and improve patient satisfaction. According to this study, implementing a vascular access specialist team could be a positive step towards achieving these goals. Future studies should estimate the impact of this change in the venous access device usage model on clinical variables and user satisfaction, as well as determine the number of catheters of each type that can be replaced by the team based on its size and decision algorithm. With this data, it will be possible to further evaluate the effectiveness of the introduction of the team, including whether the benefits achieved from replacing the catheters outweighs the cost of hiring the team’s professionals.
Limitations
This study has several limitations. First, some of the impacts of implementing a vascular access specialist team are not easily quantifiable and are not accounted for in the calculation. In the case of peripheral venous catheters replacement, these are reflected in the improvement in patient experience and well-being due to the easier catheter insertion, which preserves venous access and increases safety [
14,
29]. In the case of peripherally inserted central catheters and midline catheters substitution, the time to start the treatment is reduced and communication between the nurse and the patient is improved. Previous studies suggested that 83% of patients with the ultrasound catheters rate the change positively and 63% of patients highlight increased comfort with peripherally inserted central catheters [
30].
Secondly, in the absence of specific costs for the device placement procedure, it was assumed to be the same for peripheral venous catheters, peripherally inserted central catheters and midline catheters. Additionally, the costs of the utensils used for insertion, maintenance and replacement of catheters, were not considered, assuming that they could be similar between the compared models. Moreover, the cost of the catheter tip verification system was also not taken into account. Furthermore, the introduction of a vascular access specialist team requires a cultural change and recognition of its activity by all professionals in the institution. Future studies could also incorporate costs associated with materials, communication and dissemination of corresponding information sessions.
Thirdly, it has been assumed that the productive capacity of the team corresponds to a 3:1 ratio in the peripheral venous catheter replacement and that the time required for catheter insertion in the hospital is comparable to the evidence shown by other hospitals. Future research should assess the reliability of these assumptions.
Conclusion
The economic impact of catheter replacement resulting from the implementation of a vascular access specialist team has been analyzed and quantified, concluding that the monetary benefits outweigh the costs. Furthermore, the results suggest that prioritizing the replacement of peripheral venous catheters, rather than peripherally inserted central catheters and midline catheters inserted without ultrasound-guided technique, is more beneficial for both the patient and the hospital, mainly because decrease in hospital stay due to the lowered risk of healthcare-associated infections.
This study is the first to quantify the economic impact of catheter replacement resulting from the implementation of a specialized team in our setting. It provides an estimation of the costs and benefits of implementing such a team, while also establishing a conceptual and reference framework for evaluating the post-implementation results.