Chondrosarcoma, represents approximately 0.1% of all neoplasms of the head and neck, being considered a rare disease but with a relatively good prognosis. The 5-year overall survival (OS) rate is estimated at 70-80%, being considered a disease with a low growth rate. 1–3% of all cases of chondrosarcoma, are located in the region of the head and neck. Chondrosarcoma has the highest incidence between the third and fourth decade of life and cartilaginous neoplasms may have histological patterns ranging from benign chondroid tumors to undifferentiated un-differentiated tumors.
WHO classified chondrosarcomas in 3 degrees, cell density, differentiation and nucleus size being the factors considered in the classification but a simpler classification divides this type of tumors into two classes (low and high grade). Low grade tumors usually have a favorable prognosis and are well differentiated, being associated with a low number of pleomorphisms and cellular atypia [
1,
2].
Low-grade tumors are usually well differentiated with moderate cellularity and very few cellular pleomorphisms or atypia. All chondrosarcomas, regardless of grade, have histological features of hypercellularity, pleomorphism, mitotic activity, mixed intercellular matrix and cellular atypia. Surgical treatment is considered the backbone of the multidisciplinary approach, but the recurrence rate is relatively high for grade II and III tumors compared to low grade tumors (80% vs. 17%), even after optimal surgical treatment. Although chondrosarcoma is considered a radio-resistant tumor, high-dose adjuvant irradiation is recommended in cases with positive surgical margins [
1,
3,
4].
Clinical case
We present a 30-year-old patient without a significant medical history addressed to a ENT department, in july 2012, with dysphagia, swallowing difficulty, foreign body sensation and dysphonia, the onset being insidious apparently following an episode of upper respiratory tract infection (URTI). Hypo-pharyngoscopy and direct laryngoscopy identify a valecular cyst, which is subsequently removed, the evolution being favorable.
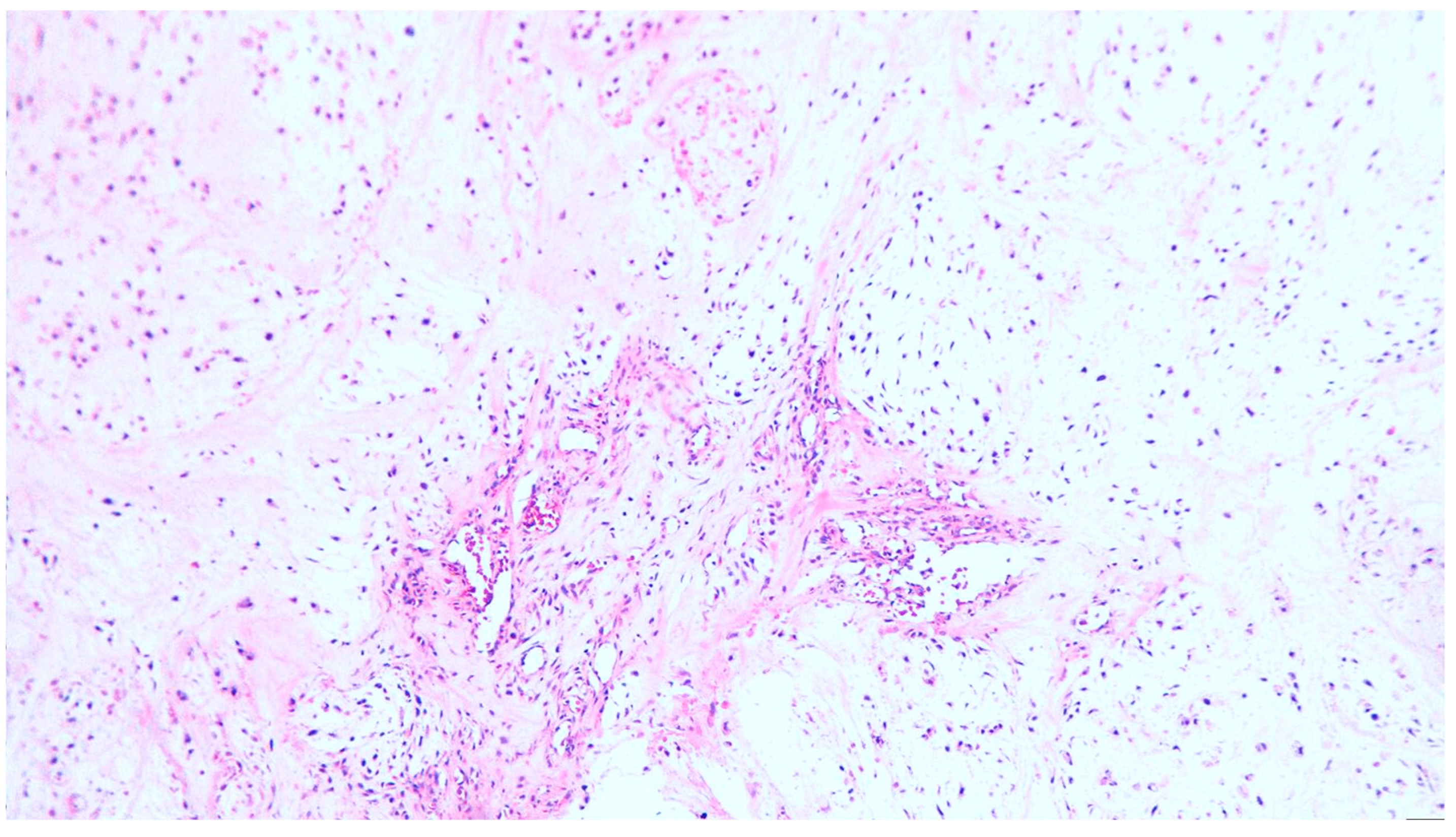
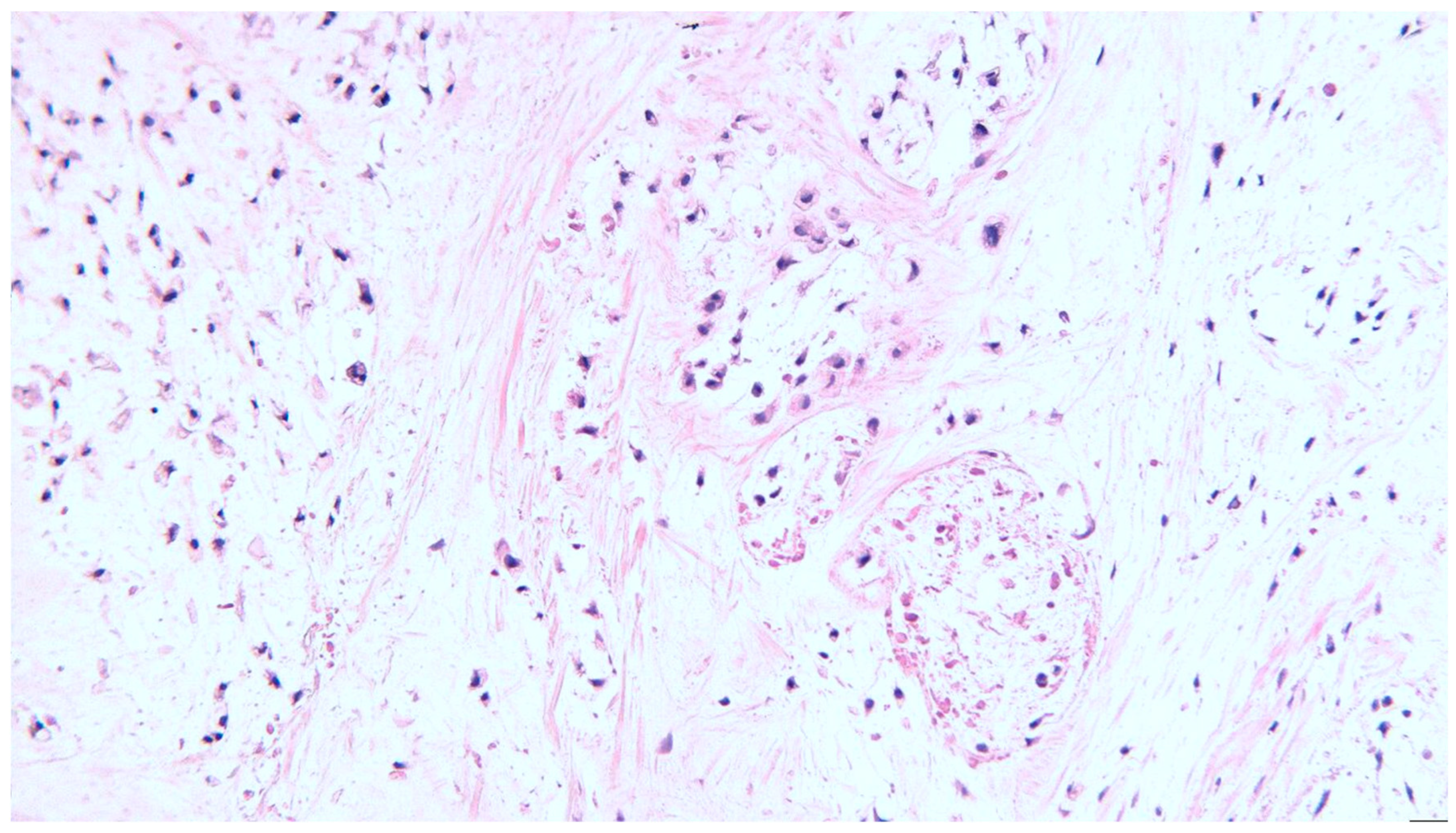
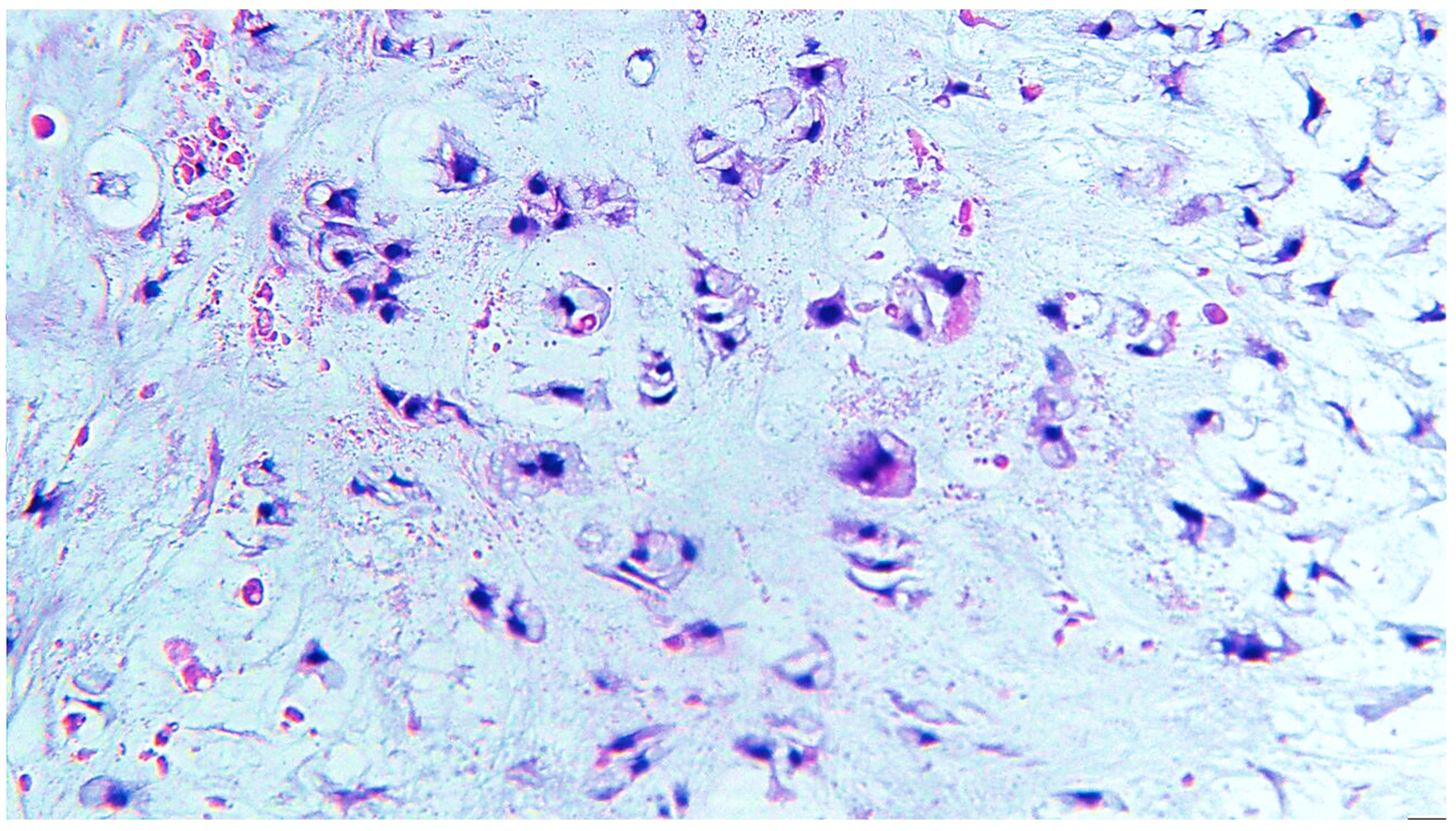
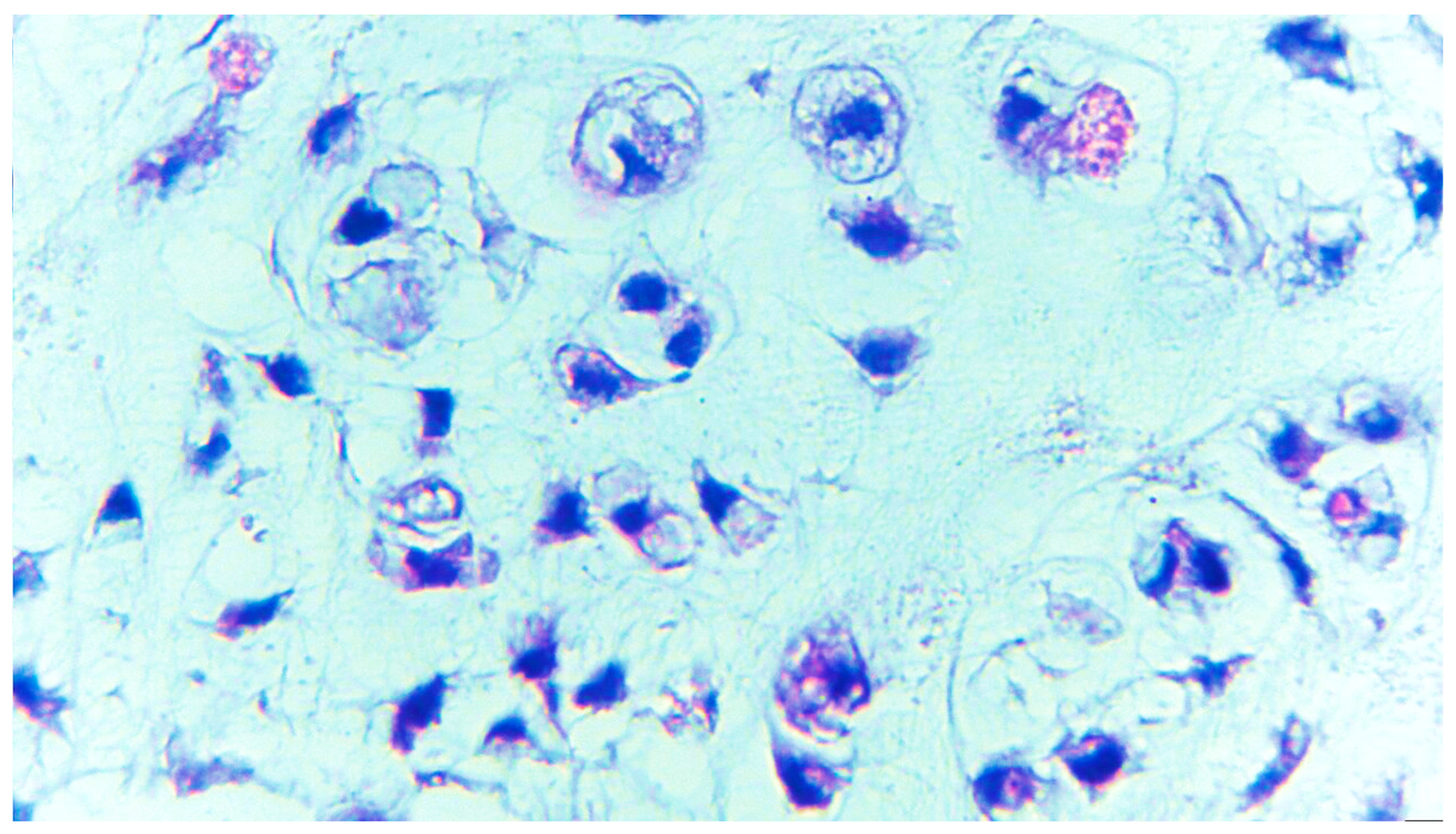
In January 2013 the patient return with inspiratory dyspnea, dysphagia, stomatolalia and fever with progressive evolution. ENT clinical examination highlights a dyspneic patient, with more pronounced inspiratory stridor, multiform tumor process on the right valecula, which dislocates the suprahyoid epiglota on which it orients with concavity towards the left hypopharyngeal lateral wall, deforming it and leaving the triangular slit equilateral with the side of approx. 5 cm. Chest X-ray does not show pathological pleuro-pulmonary aspects. The computer tomography (CT) exam reveals a polycystic-looking tumor formation with multiple septa inside and calcifications with 3-4 mm diameter that interest the right valecula, an aspect that suggests a possible chondrome. Under local anesthesia, tracheotomy is performed, followed by tumor excision, after hyoidectomy by transvalecular approach. Hystopathology reveals a polylobate and polycyclic structure, with relatively smooth capsule, firm consistency, through the transparency of the capsule brindle-like aspect red-violet areas, alternating with light areas. Tumor diameters are 105/65/85 mm. On the section, brindle-like, hard appearance of the whitish areas, the size of a rice grain, non-confluent, separated by areas with a purple, fleshy, firm tint. Epiglotopexy, laryngo-pharyngography, nasal-gastric feeding tube and Portex tracheal cannula were performed simultaneously. Histoplatological examination revealed nodular mycho-chondroid proliferation, delimited by collagen fibrosis with reduced xanthomatous inflammation and chondrocytes. Cartilaginous tissue consists of chondrocytes with irregular hyperchromic nuclei, rarely being binucleate, reduced mitotic activity and areas of bone metaplasia. In the periphery of the myxochondrroid areas, striated muscle tissue is noticeable. The appearance of histo-pathological examination suggests a hamartoma tumor (choristoma) requiring a second opinion to differentiate from a low-grade chondrosarcoma (
Figure 1,
Figure 2,
Figure 3 and
Figure 4). Postoperative evolution is marked by the development of a base of the tongue hematoma, surgical evacuation being performed. Favorable postoperative evolution is mentioned (at 4 days postoperatively, the tracheal cannula is suppressed and the patient breathing normally). Immunohistochemistry confirms the diagnosis of low-grade chondrosarcoma, p53 positive in tumor cells, Ki67 positive in <5%.
In March 2013, the patient addresses to ENT department with swelling, hyperemia and pain at the lower pole of the cervical flap, dysphagia and dehiscence of the wound on 1.5 cm with permanent bleeding. The ENT examination highlights extensive valecular swelling in the suprahyoid epiglottis, the diagnosis being suppurative cervical cellulitis and acute epiglottitis. Subsequently, the patient adress to another ENT department and lingual tonsillectomy is performed. The histopathological examination reveals - Piece 1 chistic wall - Macroscopic evaluation: - Multiple small tissue fragments of 4x3x1rnm and 2x1xlmin and fragments of mucus ; - Microscopy: - Fragments of the mucosa lined by a non-keratinized. stratified squamous epithelium, intact, without atypia, underlying the edematous chorion and a reduced chronic inflammatory infiltrate. Fragments of mucus are observed. - Piece 2 lingual tonsil : Fragment of the mucous membrane lined with squamous epithelium without atypia and fragments of mucus ; Fragment of wallpapered mucosa : - Macroscopic evaluation: 3 whitish tissue fragments elastic gray, dimensions between 5x3x21irn and 3x2xl mm.- Piece 2 lingual tonsil : - Fragment of the mucous membrane lined with squamous epithelium without atypia and fragments of mucus; Fragment of wall-papered mucosa ; - Macroscopic evaluation: 3 whitish tissue fragments, dimensions between 5x3x21mm and 3x2xl mm ; - Microscopy: Fragments of mucosa lined by a non-catenating stratified squamous epithelium, intact, without atypia, underlying the edematous chorion being present lymphatic tissue on allocular follicular architecture with genninal centers.
5 cycles Epirubucine+Cisplatin were performed between April-July 2013, than patient received external beam radiation (cobalt) in a total dose of 50Gy/25 fractions/5weeks/5days per week between August and September. The patient was evaluated periodically in the oncology and ENT department, presenting a performance index ECOG 2 (Eastern Cooperative Oncology Group), dysphagia for solids and liquids, with no significant loco-regional recurrence, until March 2014, when he was lost from evidence.
Discussions
Representing approximately 11% of all primary malignant bone tumors and the second most common sarcoma subtype after osteosarcoma, chondrosarcoma of the head and neck region is rare. The base of the skull, the sinonasal tract, the jaw and the larynx are anatomical locations reported to be associated with the occurrence of chondrosarcoma. Differential diagnosis with chondroblastic osteosarcoma and chondroid chordoma is considered difficult. With an overall survival (OS) estimated at 5 years of 80%, surgery as a single method or followed by adjuvant radiotherapy is considered the optimal approach. For cases not eligible for surgery or associated with cosmetically mutilating effects, radiotherapy has been reported to be effective [
5].
Horta et al. reports a case of chondrosarcoma of the hyoid bone, a very rare subtype, 20 cases being identified at that time in the literature. To be noted in this case is the value of the computer tompgraphy examination which highlights chondroid like calcification originating from the hyoid bone, although previously cytology suggested pleomorphic adenoma. Prior to this case report, analyzing 19 cases of chondrosarcoma of the hyoid bone Zhang et al. also mentions the role of CT imaging and Magnetic Resonance Imaging (MRI) in the diagnostic stage and of surgery followed by radiotherapy as backbone treatment [
6,
7]. Retrospectively reviewing 8 cases of chondrosarcoma of the head and neck region, the Yonsei University Medical College identified radiation therapy as delivered in 50% of cases as an adjuvant after surgery. The case in which complete excision could not be performed was associated with early death, and in 3 cases out of 8 relapse was diagnosed, this being treated successfully in 2 cases [
8].
Vučković mentions a case operated on 14 years after the diagnosis of chondrosarcoma, diagnosed at that time with a chondroma. The authors draw attention to the differential diagnosis of chondrosarcoma, a subtype of tumor characterized by mesenchymal transformation originating in hyaline cartilage, but also to the possibility of transforming a chondroma into a low-grade chondrosarcoma. In all cases of head and neck submucosal tumors, chondrosarcoma should be considered as a differential diagnosis. After the left partial vertical laryngectomy treatment, no local recurrence or distant metastasis was reported in a 12-month follow-up. In a case of right maxillary sinus tumor, grade III chondrosarcoma with skin and bone infiltration of the maxillary sinus and orbital floor was identified. Despite an aggressive adjuvant treatment, a higher tumor grade associated with extreme chromosomal instability was also associated with local recurrence. Sprekelsen et al. mentions the tumor grade as being associated with the risk of recurrence and with the profile of therapeutic failure. In the case of low grade tumors, local growth is predominant, and for high grade head and neck chondrosarcoma, distant metastasis becomes the predominant pattern of failure, even after years from the initial treatment [
9,
10].
Clear cell chondrosarcoma, which usually involves the end of long bones, was reported in nine cases in the head and neck, including 4 cases of tumors of the larynx, the nasal septum of the jaw and the skull. Clear cell chondrosarcoma was associated with septal bulging, and the maxillary tumor did not involve the mucosa. In the case of laryngeal tumors, a tendency of recurrence was observed. Being a rare and slow-growing tumor, a long follow-up and a diagnosis based on immunohistochemical tests is necessary. An unusual onset through 12 days of vomiting is reported in the case of a low grade right cricoid chondrosarcoma with intraluminal and extraluminal extension. 18 months after the resection of the trachea with end to end anastomosis, the patient was alive with no signs of recurrence. And in this case, a resection with margins free of tumor is considered sufficient, radiotherapy being recommended to prevent local recurrence in case of incomplete resection [
11,
12]. Rivero et al. mentions an increased incidence in the 6th and 7th decade of life of laryngeal chondrosarcoma, being 3 times more frequent in men than in women. 70-75% are located on the cricoid and only 10-20% are located on the thyroid cartilage. More than 30 years ago, Burkey remarca a worst outcome asoociated with condrosarcoma of paranasal sinuses [
13,
14].
Tejani et al. considers that tumor size and resection quality are the main risk factors associated with an unfavorable prognosis in head and neck sarcomas. A size of 5cm is considered the cutoff value for the prognosis. Although in most studies they consider the histological degree as an essential prognostic factor, associating therapeutic failure and the increased rate of recurrences and metastases with higher degrees of sarcomas, the authors do not identify the histological tumor degree as a prognostic and predictive factor. Adjuvant radiotherapy is usually administered for cases with high histological grade chondrosarcoma and R1 resections at a dose between 50Gy and 66Gy, in a standard fractionation regimen. The intensity modulated radiation therapy (IMRT) technique and the weekly low dose Cisplatin (30mg/m2) and Ifosfamide-based chemotherapy is generally preferred for high grade tumors. In the case of low-grade chondrosarcoma, the rate of distant metastases is relatively low (1.9%), but the analyzed group included only low-grade chondrosarcoma larynx [
15,
16].
In a systematic review that included only 9 cases reported from 1946 to 2019, Jones and collaborators found a relatively low rate of loco-regional recurrences, with only one of these cases recurring 4 years after surgical treatment. The authors also mention a relatively low rate of adjuvant treatment (2 out of 9 cases) and no case of distant metastasis. The study demonstrates the value of surgical treatment as the basis of the curative approach of head and neck chondrosarcoma. Both wound dehiscence and hematoma are major complications that require surgery, being reported with an incidence of 5.9% respectively 4.2%. Among the risk factors associated with these complications, neck dissection and neo-adjuvant chemo-radiotherapy are considered the most important [
17,
18,
19]. A summary of the main articles on head and neck chondrosarcoma is included in
Table 1. We present the objective and type of study, results and conclusions [
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
16,
17,
18]
Eisbruch analyzed almost 20 years ago the anatomical strictures involved in late dysphagia/aspiration (DARS) in the case of HNC patients treated with chemotherapy based on Gemcitabine and high doses of concurrent radiotherapy for curative purposes. Coreland evaluation of swallowing and structural changes, videofluoroscopy, direct endoscopy and CT with radiotherapy plans obtained with the 3D-conformal technique (3D-CRT), intensity modulated radiotherapy (IMRT) and IMRT optimized for dysphagia reduction. A Cisplatin-based chemotherapy regimen was also proposed to evaluate the specificity of the changes associated with the treatment compared to a certain chemotherapy regimen. Prolongation of pharyngeal transit time, posterior tongue base weakness, lack of coordination between swallowing phases and limited laryngeal elevation, reduction of laryngeal closure and epigotic inversion were identified in the case of both regimens and were associated with a high aspiration rate. The study identifies the laryngeal constrictors, the glottic and supragotic larynx as risk organs associated with dysphagia after radiochemotherapy treatment. The authors demonstrated a moderate benefit of the IMRT technique in limiting the risk of late dysphagia, but by optimizing the IMRT plans related to dysphagia and reducing the radiation doses received by these structures, an additional benefit can be brought in limiting toxicities. Petkar et al. exploits this concept in a phase III randomized trial and evaluates whether sparing pharyngeal constrictor muscle and supraglottic larynx translates into the limitation of late dysphagia. The DARS trial (CRUK/14/014) assessed dysphagia according to the MD Anderson Dysphagia Inventory (MDADI) scale 12 months after treatment. The trial divides the cases of T1-4, N0-3, M0 pharyngeal cancers into two equal groups that are treated by chemo-radiotherapy, using the IMRT technique for the delivery of radiotherapy and the IMRT technique optimized to limit dysphagia [
20,
21,
22].
Dysphagia is one of the most serious tardive complications associated with an aggressive multimodal treatment including radiation therapy and chemotherapy, being a predictor for the risk of aspiration. Oropharynx and hypo-pharynx cancers, but also the stage and size of the tumor are predictive factors of the risk of aspiration. Elderly patients and concurrent chemo-radiotherapy are also associated with an increased risk of late dysphagia and aspiration. Madan and collaborators report aspiration pneumonia as the cause for a 60% death rate in a group of 85 patients with head and neck cancers followed for a period of 12 years. The radio-biological model proposed by Christianen et al, identify the radiation dose received by the pharyngeal constrictor muscles and the supraglottic larynx as predictors for late severe dysphagia. The authors mention the impossibility of using a single dose-volume correlation to predict dysphagia. If in the case of liquids, the mean dose received by the supraglottic larynx is predictive, in the case of dysphagia for soft foods, both the radiation dose received by the superior pharyngeal constrictor muscle, the supraglottic larynx, but also the age with a cutoff value of 65 years are associated with late toxicity. In this context, the use of a modern radiotherapy technique reduce the doses received by these anatomical structures can significantly reduce the risk of late dysphagia and having as a consequence the reduction of the risk for aspiration pneumonia [
23,
24,
25,
26]. Normal tissue complication probability (NTCP) models based on a specific end-point related to the risk of severe toxicity can be the basis of a decision algorithm between delivering the radiation dose treatment to the patient with the IMRT technique or proton beam therapy [
27].
Although it is one of the most serious side effects of HNC treatment, even associating the risk of mortality, aspiration pneumonia associated with chemoradiotherapy and bioradiotherapy with Cetuximab is little investigated. Analyzing retrospectively the data obtained from 374 patients, of which 95 cases (25.4%) had associated aspiration pneumonia, the authors identified a correlation between aspiration pneumonia with treatment response and overall survival. Hospital treatment, hypoalbuminemia before treatment, N classification and oral hygiene were factors associated with the risk of aspiration pneumonia. Neck dissection and accelerated fractionation regimen are also considered risk factors for aspiration [
28,
29].
After an analysis of data from 3513 patients with HNC, aspiration pneumonia was identified in the history in 801 cases 5 months after the initiation of treatment. Hypopharyngeal tumors, male sex, advanced age, comorbidities, lack of surgical treatment before radio-chemotherapy were identified as risk factors for aspiration pneumonia in multivariate analysis. The hospitalization rate for patients with aspiration pneumonia is considered to be 84%, of which 45% are admitted to intensive care units. With a thirty-day mortality of 32.5% and a general risk of death of 45%, aspiration pneumonia must be considered as a possible late complication after radiochemotherapy, especially in elderly patients. Xu et al. mentions that 5 years after the end of the treatment, a quarter of this category of patients will be affected by aspiration pneumonia. Tumor stage are identified as risk factors by Liu et al., patients with ≥ 2 risk factors have a risk of 2,5 times more to aspire after the completion of radiotherapy treatment [
30,
31,
32].
Conclusions
The early loss from the oncological follow-up programs of patients with a low degree of aggression tumor, without evidence of a recurrence or metastasis can be the consequence of a major complication among which we can assume an aspiration pneumonia secondary to a dysphagia, associated with an aggressive multidisciplinary treatment. Large tumor size and positive resection margins (R1 resection) are risk factors that support a intensive adjuvant approach to reduce the risk of recurrence but the low degree of tumor, associating a lower risk of recurrence as well as the adverse effects of adjuvant radiotherapy and chemotherapy are arguments that argue for a intensification of therapy. Given the long life expectancy of these patients, it is recommended to use an irradiation technique to reduce doses to radiosensitive structures as well as to omit elective neck irradiation, taking into account the reduced risk of lymph node involvement. The lack of guidelines that include very rare tumors including low grade chondrosarcoma of head and neck make a unified approach difficult, but the data presented even in case reports could contribute to choosing the regimen that offers the best therapeutic ratio.
References
- FC Quevedo, FB Quevedo, JC Barauna, et al. Case report: Chondrosarcoma of the head and neck Human Pathology: Case Reports Volume 7, March 2017, Pages 4-7.
- HL Evans, AG Ayala, MM Romsdahl, et al. Prognostic factors in chondrosarcoma of bone. A clinic-pathologic analysis with emphasis on histologic grading. Cancer, 40 (1977), pp. 818-831. [CrossRef]
- S Obesoab JL Llorenteab JP Díaz-Molinaab, et al. Surgical treatment of head and neck chondrosarcomas.Tratamiento quirúrgico de los condrosarcomas de cabeza y cuello. Acta Otorrinolaringologica (English Edition) Volume 61, Issue 4, 2010, Pages 262-271.
- AA Catanzano, DL Kerr, AL Lazarides, et al. "Revisiting the Role of Radiation Therapy in Chondrosarcoma: A National Cancer Database Study", Sarcoma, vol. 2019, Article ID 4878512, 9 pages, 2019. [CrossRef]
- Coca-Pelaz A, Rodrigo JP, Triantafyllou A, Hunt JL, Fernández-Miranda JC, Strojan P, de Bree R, Rinaldo A, Takes RP, Ferlito A. Chondrosarcomas of the head and neck. Eur Arch Otorhinolaryngol. 2014 Oct;271(10):2601-9. [CrossRef]
- Horta M, Fernandes L, Borges A. Chondrosarcoma of the hyoid bone: an atypical site of a sarcoma of the head and the neck. BMJ Case Rep. 2015 Nov 5;2015:bcr2015212291. [CrossRef]
- Zhang I, Zaorsky NG, Abraham JA, Tuluc M, Curry JM, Bar-Ad V. Chondrosarcoma of the hyoid bone: case report and review of current management options. Head Neck. 2014 Jul;36(7):E65-72. [CrossRef]
- Lee SY, Lim YC, Song MH, Seok JY, Lee WS, Choi EC. Chondrosarcoma of the head and neck. Yonsei Med J. 2005 Apr 30;46(2):228-32. [CrossRef]
- Vučković L, Klisic A, Filipović A, Popović M, Ćulafić T. Low-grade chondrosarcoma of the larynx: A case report. World J Clin Cases. 2021 Sep 16;9(26):7805-7810. [CrossRef]
- Quevedo, Francisco Carlos, Fernando Quevedo, José Carlos Barauna Neto, Elisa Napolitano e Ferreira, Dirce Maria Carraro and Fernando Augusto Soares. “Case report: Chondrosarcoma of the head and neck.” Human Pathology: Case Reports 7 (2017): 4-7. [CrossRef]
- Mokhtari S, Mirafsharieh A. Clear cell chondrosarcoma of the head and neck. Head Neck Oncol. 2012 Apr 20;4:13. [CrossRef]
- Gao CP, Liu JH, Hou F, Liu H, Xu WJ. Low-grade chondrosarcoma of the cricoid cartilage: a case report and review of the literature. Skeletal Radiol. 2017 Nov;46(11):1597-1601. [CrossRef]
- Pino Rivero V, Keituqwa Yáñez T, González Palomino A, Trinidad Ramos G, Marqués Rebollo L, Gómez de Tejadae Romero R, Blasco Huelva A. Condrosarcoma laríngeo de bajo grado de malignidad. A propósito de un caso localizado en cartílago tiroides [Laryngeal chondrosarcoma of low grade of malignancy. Report of a case located on thyroid cartilage]. An Otorrinolaringol Ibero Am. 2006;33(3):249-56. Spanish.
- Burkey BB, Hoffman HT, Baker SR, Thornton AF, McClatchey KD. Chondrosarcoma of the head and neck. Laryngoscope. 1990 Dec;100(12):1301-5. [CrossRef]
- MA Tejani, TJ Galloway, M Lango, et al. Head and Neck Sarcomas: A Comprehensive Cancer Center Experience. Cancers (Basel). 2013 Sep; 5(3): 890–900. [CrossRef]
- Elktaibi A, Rharrassi I, Hammoune N, Darouassi Y, Hanine MA, Ammar H. A Rare Case of Malignant Tumor of the Larynx with Good Prognosis: Laryngeal Chondrosarcoma. Case Rep Oncol Med. 2019 May 5;2019:9468194. [CrossRef]
- Jones AJ, Alwani M Summerlin D-J, et al. Head and Neck Juxtacortical Chondrosarcoma: A Systematic Review. Archives of Otorhinolaryngology-Head & Neck Surgery. 2019;3(1):4. [CrossRef]
- Finn DG, Goepfert H, Batsakis JG. Chondrosarcoma of the head and neck. Laryngoscope. 1984 Dec;94(12 Pt 1):1539-44. [CrossRef]
- R. Pellini, G. Mercante, C. Marchese,et al. Predictive factors for postoperative wound complications after neck dissection. Acta Otorhinolaryngol Ital. 2013 Feb; 33(1): 16–22. Christianen M.E., Verdonck-de Leeuw I.M., Doornaert P. et al., Patterns of Long-Term Swallowing Dysfunction after Definitive Radiotherapy or Chemoradiation, Radiother. Oncol., Oct., 117, 1, 139-144 (2015). [CrossRef]
- Eisbruch A, Schwartz M, Rasch C, Vineberg K, Damen E, Van As CJ, Marsh R, Pameijer FA, Balm AJ. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys. 2004 Dec 1;60(5):1425-39. [CrossRef]
- Petkar I, Rooney K, Roe JW, Patterson JM, Bernstein D, Tyler JM, Emson MA, Morden JP, Mertens K, Miles E, Beasley M, Roques T, Bhide SA, Newbold KL, Harrington KJ, Hall E, Nutting CM. DARS: a phase III randomised multicentre study of dysphagia- optimised intensity- modulated radiotherapy (Do-IMRT) versus standard intensity- modulated radiotherapy (S-IMRT) in head and neck cancer. BMC Cancer. 2016 Oct 6;16(1):770. [CrossRef]
- Upadhyay P Sr, Kumar P, Chauhan AK, Kumar P, Nigam J, S N. Comparison of Dosimetric Parameters in Dysphagia Aspiration-Related Structures and Clinical Correlation in Head and Neck Cancer Patients Treated With Radiotherapy. Cureus. 2022 Jul 11;14(7):e26765. [CrossRef]
- Upadhyay P Sr, Kumar P, Chauhan AK, Kumar P, Nigam J, S N. Comparison of Dosimetric Parameters in Dysphagia Aspiration-Related Structures and Clinical Correlation in Head and Neck Cancer Patients Treated With Radiotherapy. Cureus. 2022 Jul 11;14(7):e26765. [CrossRef]
- Denaro N., Merlano M.C., Russi E.G., Dysphagia in Head and Neck Cancer Patients: Pretreatment Evaluation, Predictive Factors, and Assessment during RadioChemotherapy, Recommendations., Clin. Exp. Otorhinolaryngol., Sep., 6, 3, 117-126 (2013). [CrossRef]
- Madan R, Kairo AK, Sharma A, et al. Aspiration pneumonia related deaths in head and neck cancer patients: a retrospective analysis of risk factors from a tertiary care centre in North India. J Laryngol Otol. 2015;129(7):710-714. [CrossRef]
- Christianen ME, Schilstra C, Beetz I, Muijs CT, Chouvalova O, Burlage FR, Doornaert P, Koken PW, Leemans CR, Rinkel RN, de Bruijn MJ, de Bock GH, Roodenburg JL, van der Laan BF, Slotman BJ, Verdonck-de Leeuw IM, Bijl HP, Langendijk JA. Predictive modelling for swallowing dysfunction after primary (chemo)radiation: results of a prospective observational study. Radiother Oncol. 2012 Oct;105(1):107-14. [CrossRef]
- Stieb S, Lee A, van Dijk LV, Frank S, Fuller CD, Blanchard P. NTCP Modeling of Late Effects for Head and Neck Cancer: A Systematic Review. Int J Part Ther. 2021 Jun 25;8(1):95-107. [CrossRef]
- Upadhyay P Sr, Kumar P, Chauhan AK, Kumar P, Nigam J, S N. Comparison of Dosimetric Parameters in Dysphagia Aspiration-Related Structures and Clinical Correlation in Head and Neck Cancer Patients Treated With Radiotherapy. Cureus. 2022 Jul 11;14(7):e26765. [CrossRef]
- Lindblom U, Nilsson P, Gärskog O, Kjellen E, Laurell G, Wahlberg P, Zackrisson B, Levring Jäghagen E. Aspiration as a late complication after accelerated versus conventional radiotherapy in patients with head and neck cancer. Acta Otolaryngol. 2016;136(3):304-11. [CrossRef]
- Xu B, Boero IJ, Hwang L, Le QT, Moiseenko V, Sanghvi PR, Cohen EE, Mell LK, Murphy JD. Aspiration pneumonia after concurrent chemoradiotherapy for head and neck cancer. Cancer. 2015 Apr 15;121(8):1303-11. [CrossRef]
- Liu HC, Williamson CW, Zou J, Todd JR, Nelson TJ, Hill LM, Linnemeyer KE, Henderson G, Madgula P, Faung B, Sacco AG, Vitzthum LK, Weissbrod PA, Blumenfeld LS, Mell LK. Quantitative prediction of aspiration risk in head and neck cancer patients treated with radiation therapy. Oral Oncol. 2023 Jan;136:106247. [CrossRef]
- Zaheen A, Stanbrook MB. Accidental barium bronchography. CMAJ. 2017 May 8;189(18):E670. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).