1. Introduction
The use of acellular dermal matrix (ADM) allograft for coverage of recession defects does not require a second surgical site to obtain donor tissue [
1,
2,
3,
4,
5]. This means less postoperative morbidity for the patient and less clinical time for the surgeon. Also, particularly advantageous for both the patient and the surgeon is the ability to treat as many sites as desired since the supply of ADM is essentially unlimited [
2,
3,
5,
6]. Initially ADM for root coverage was used in conjunction with a coronally positioned flap (CPF). This approach was highly successful and achieved mean root coverage similar to connective tissue graft procedures with comparable predictability [
3,
4,
6,
7]. Another technique for the use of ADM, the coronally positioned tunnel (CPT) approach, has been recently described [
8]. This is a minimally invasive technique that has no visible incisions and provides the advantage of minimizing flap retraction since the papillae are maintained intact [
9,
10].
Originally the suturing techniques recommended for the CPT were either a subpapillary single tooth sling or a continuous sling. Both of these techniques involved suturing the ADM and the soft tissue separately [
8]. In other words, the operator had to do a sling for the ADM and then an additional sling suture was needed for the soft tissue. Recently another suturing approach has been described whereby the ADM and the soft tissue are sutured simultaneously and only one sling suture is needed [
11]. This technique has the promise of making the CPT procedure more efficient by saving a substantial amount of suturing time, which would benefit both the patient and the surgeon. At this point there are no studies that have compared the suturing techniques to determine if they are equally effective.
The primary objective of this randomized, controlled, blinded clinical pilot study is to compare the double continuous sling technique with the soft tissue and the ADM sutured separately to the single continuous sling technique where they are sutured together using recession defect coverage as the primary outcome variable.
2. Materials and Methods
2.1. Study Design
Sixteen patients who had at least one site with a Miller Class I or II recession defect ≥ 3 mm received treatment with root coverage surgery and were followed for 6 months. Eight patients in the positive control group were treated with a coronally positioned tunnel technique (CPT) plus acellular dermal matrix (ADM; Alloderm, BioHorizons, Birmingham, AL) using two independent continuous sling sutures to secure the graft and the soft tissue separately (SEP group). The test group consisted of 8 patients who were treated with CPT plus ADM using a single continuous sling suture to secure both the graft and the flap simultaneously (TOG group). Patients were randomly selected to receive either the test or control treatment using a coin toss. One operator (DX) performed all surgical procedures under the directions of a mentor (HG). Clinical examinations were performed by a masked examiner (VP) who was unaware of the treatment assignment at all times. The mentor (HG) verified the measurements taken by the blinded examiner. All patients signed an informed consent approved by the University of Louisville Institutional Review Board. The study was conducted between July 17, 2013 and July 17, 2014 in the Graduate Periodontics clinic at the University of Louisville.
2.2. Patient Selection
The inclusion criteria were: 1) at least one Miller Class I or II recession defect ≥ 3 mm; 2) the mucogingival defect must be on a non-molar tooth; and 3) patients must be ≥ 18 years of age. Patients were excluded for the following reasons: 1) presence of debilitating systemic disease or any disease that significantly affects the periodontium; 2) a known allergy to any of the materials used in the study; 3) requirement for antibiotic prophylaxis; 4) root surface restorations at the site of recession; 5) cemento-enamel junction (CEJ) not identifiable; 6) failure to maintain oral hygiene levels of at least 80% plaque-free surfaces; 7) pregnancy or lactation; 8) use of tobacco products; 9) alcohol abuse problems; 10) long-term steroid therapy; 11) history of a previous root coverage procedure at the site; and 12) failure to complete the informed consent form. Patients were given oral hygiene instructions and an adult prophylaxis prior to inclusion in the study.
2.3. Baseline Data
Baseline data included the following: Miller classification of the recession defect; Plaque Index; Gingival Index, bleeding on probing using dichotomous scoring; gingival margin levels; width of keratinized tissue; clinical attachment level; tooth mobility; creeping attachment measured from the 8-week post-surgery until the final evaluation; tooth vitality tested using an electric pulp tester and a cold test; paralleling radiographic examination; patient models; and clinical photos [
12,
13,
14].
2.4. Surgical Treatment
The surgical procedure for both test and control sites consisted of a coronally positioned tunnel preparation as described by Allen and Cummings [
8]. Split-thickness dissection beyond the mucogingival junction was made to elevate the tissue and allow adequate coronal positioning. The tunnel was dissected using a specialized microsurgical kit (Dr. Allen Oral Plastic Surgery Kit, Hu-Friedy, Chicago, IL). The tunnel and ADM were extended at least one tooth mesial and distal to the recession site. Interproximal papillae were completely elevated off the osseous crest from the buccal and lingual sides so that the whole tissue complex was mobile and could be coronally positioned without tension. In one case in the TOG group where access was difficult, an incision was made to release a papilla to prevent tearing the tissue during the tunnel preparation. The hydrated ADM was placed positioned against the root surface 1.0 mm apical to the CEJ to completely cover the defect. The inferior and lateral borders extended at least 3.0 mm beyond margin of the osseous defect.
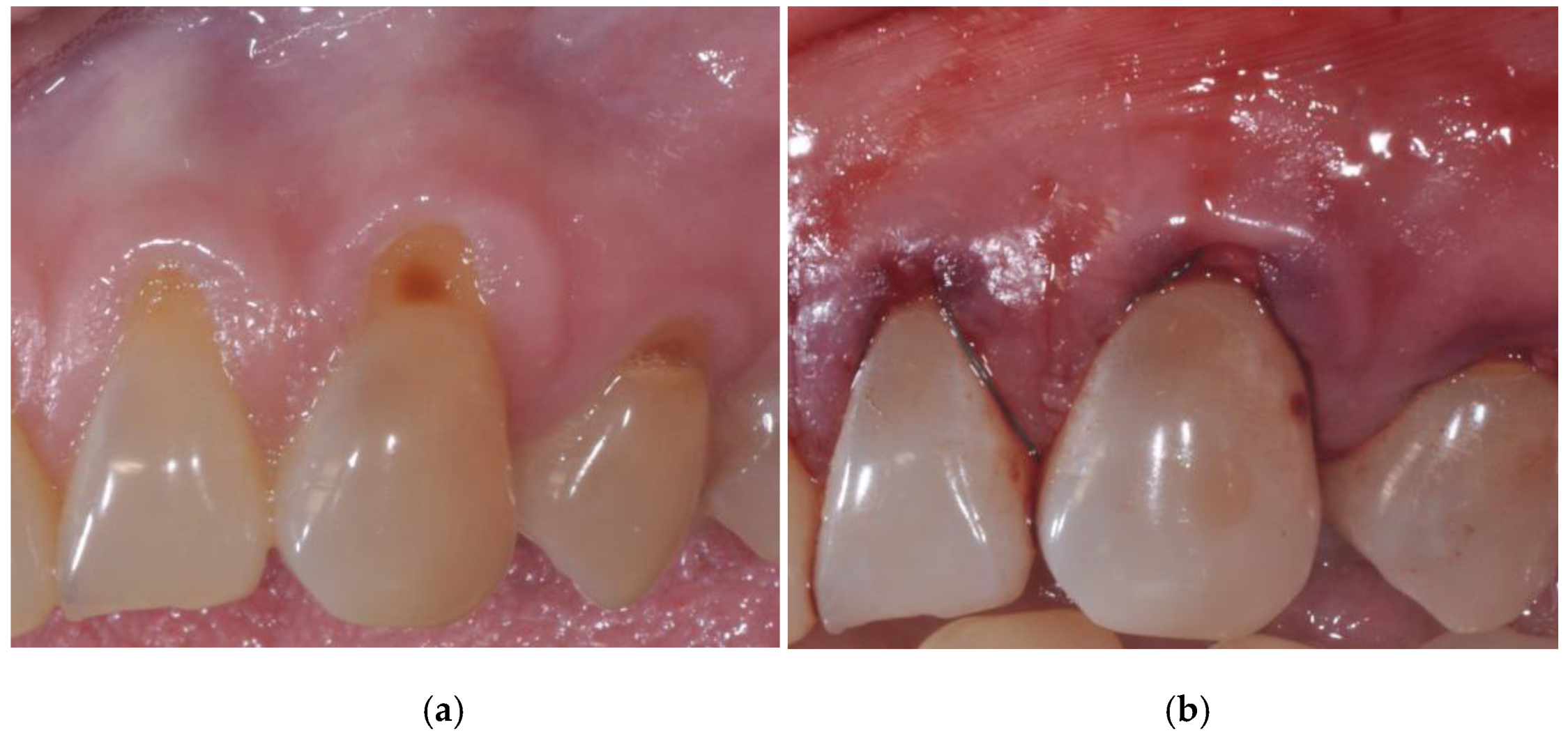
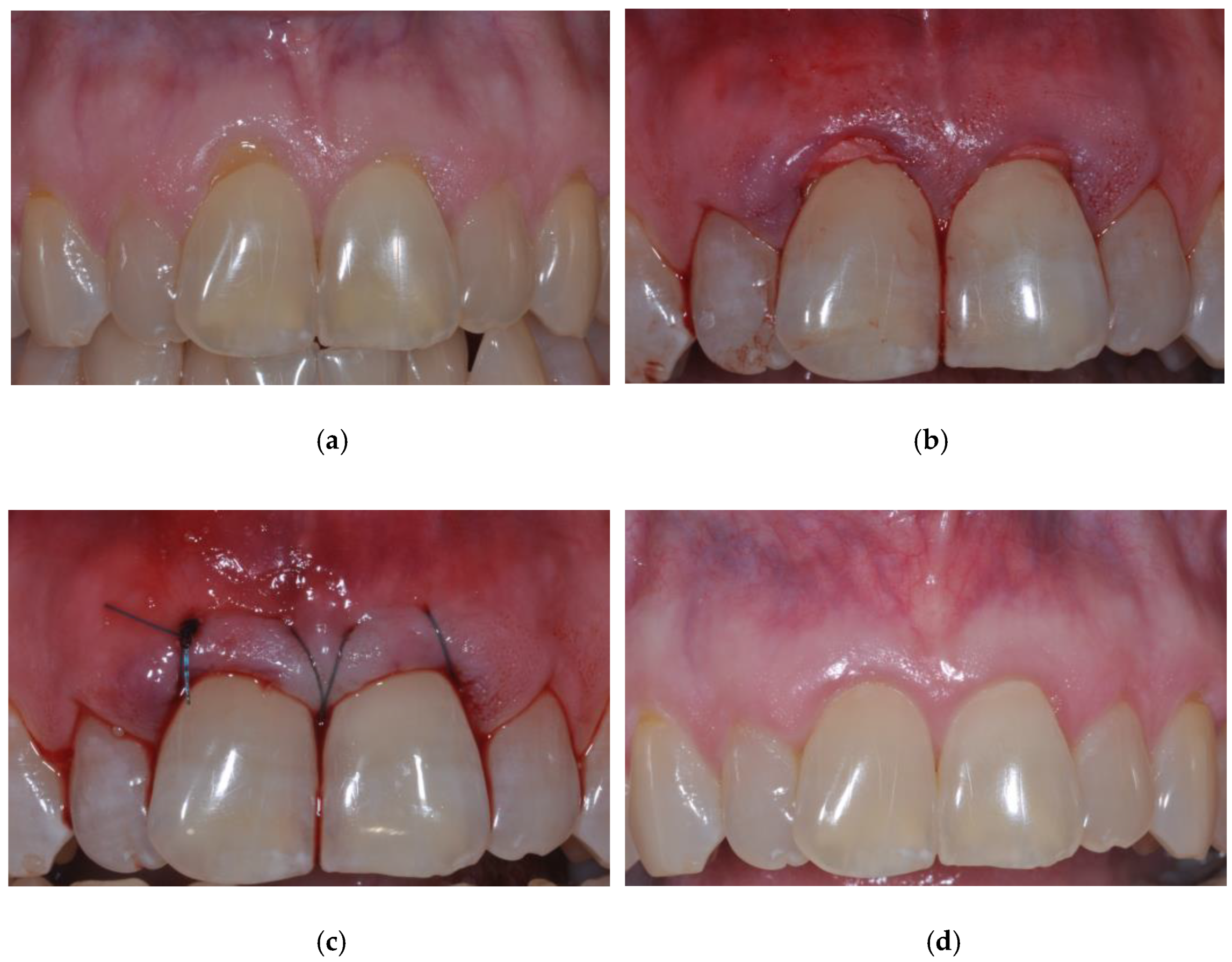
For the suturing of both test and control groups, a monofilament polyglyconate 5-0 suture (Maxon, Kendall Healthcare, Mansfield, MA) that maintains its tensile strength for ≥ 6 weeks was used. In the control group, the ADM was sutured first and separately from the soft tissues using a continuous sling suture technique. Then, the soft tissues were coronally positioned and sutured separately using a continuous sling suture technique at the line angles of the teeth (
Figure 1). In the test group, both the ADM and the soft tissues were coronally positioned and sutured together using a continuous sling suture technique at the line angles of the teeth. The ADM was positioned about 1 mm apical to the CEJ (
Figure 2). The suturing technique deviated from the original description of the CPT technique in that the sutures were not subpapillary [
8].
Post-operative instructions were given to the patients along with the following prescriptions: systemic doxycycline hyclate 50 mg once a day for 14 days; hydrocodone bitartrate 7.5 mg with acetaminophen 300 mg every 6-8 hours as needed for pain; a dose pack of 21 tablets of methylprednisolone.
2.5. Post-surgical Management
All patients were seen at week 1-2, 3-4, 7-8, 16 and 24 postoperatively. The final evaluation was performed at the 24-week exam. Sutures were removed at the 7-8-week postoperative exam. All visits consisted of supragingival plaque removal and oral hygiene reinforcement. Any patient who developed any adverse reaction to the materials used or showed attachment loss ≥ 2.0 mm was exited from the study and received the appropriate treatment. The 8-week postoperative exam was the baseline for the measurement of creeping attachment, and mid-facial recession was recorded. All baseline clinical measurements were repeated at the last exam, 6 months postoperatively.
2.6. Statistical analysis
Mean and standard deviations were calculated for all parameters. The statistical significance of the data for each parameter was analyzed using paired t-test to evaluate changes from initial to final and unpaired t-test to evaluate between group differences.
3. Results
Twelve females and four males with a mean age of 40 ± 10 years (range 18 to 58 years) were included in the study. The SEP group consisted of five maxillary and three mandibular teeth: one maxillary incisor, four maxillary canines, one mandibular canine, and two mandibular premolars. The TOG group consisted of three maxillary and five mandibular teeth made up of the following tooth types: one maxillary incisor, two maxillary canines, two mandibular incisors and three mandibular premolars. There were no adverse reactions and no subjects were exited from the study.
3.1. Clinical Indices
The results for the mean plaque index, the gingival index, bleeding on probing, and mobility at baseline were low, ranging from 0.1 to 0.4, and were further reduced by the 6-month exam when most scores were either 0.0 or 0.1. There were no statistically significant changes from initial to final exam (p > 0.05) except for the mean gingival index in the TOG group, which was reduced by 0.3 (p < 0.05). There were no statistically significant differences between groups at any time (p > 0.05).
3.2. Gingival Recession
The mean recession defect at the initial examination for the SEP group was 3.1 ± 1.0 mm, which was reduced to 0.5 ± 0.8 mm at 6 months, for a defect coverage of 2.6 ± 0.5 mm or 85% (p < 0.05;
Table 1). For the TOG group, the mean initial recession was 3.5 ± 1.0 mm, which was reduced to 0.8 ± 1.2 mm at 6 months, for a defect coverage of 2.8 ± 0.5 mm or 83% (p < 0.05;
Table 2). Frequency data indicated that the predictability of obtaining complete root coverage was 63% (five of eight sites) in both groups (
Table 1 and
Table 2).
3.3. Probing Measurements
The results of the mean probing depth, the clinical attachment level, and keratinized tissue at the initial and the 6-month examinations are shown in
Table 3. There was a significant gain in clinical attachment level (p < 0.05) for both groups. For keratinized tissue there was a significant gain for the TOG group only (p < 0.05).
3.4. Creeping Attachment
Creeping attachment, or the mean change in gingival margin position, from 2 to 6 months, increased from 0.7 ± 1.2 mm to 0.8 ± 1.0 mm, for a mean change of 0.1 ± 1.2 mm for the TOG group (p > 0.05). The SEP group recession increased from 0.2 ± 0.4 mm to 0.5 ± 0.8 mm for a mean change of 0.3 ± 0.7 mm. There were no statistically significant differences between the groups (p > 0.05).
4. Discussion
This 6-month randomized, controlled, blinded pilot study compared two different suturing techniques for the coronally positioned tunnel (CPT) plus acellular dermal matrix (ADM) root coverage procedure. For the control group the ADM was sutured separately from the soft tissues (SEP group) i.e. two separate sling sutures were used, one for the ADM and one for the soft tissues. For the test group a single sling suture was used and the ADM and the soft tissues were sutured together (TOG group).
The mean percent recession defect coverage was 85% for the SEP group and 83% for the TOG group. The difference between groups was not statistically significant although both groups achieved a statistically significant amount of mean root coverage, 2.6 and 2.8 mm for the SEP and TOG groups respectively. This indicates that both techniques worked equally well in achieving recession defect coverage. The primary advantage for the TOG group was reduced operative time. The authors estimate that suturing time was reduced by at least 50%. This makes sense considering the SEP group required two slings, or double the amount of suturing. Actual timing of the suturing was not done since a variable amount of teeth were included for each patient, which precluded a time comparison.
There was a statistically significant gain (p < 0.05) of mean keratinized tissue (KT) for the TOG group, 1.1 ± 0.9 mm, while the SEP group gained only a minimal amount 0.2 ± 0.8 mm (p > 0.05). The reason for this was not clear. The authors speculate that the position of the ADM may have had an influence. For the SEP group the ADM was positioned 1 mm apical to the CEJ while the soft tissue was positioned 2 mm coronal to the CEJ. For the TOG group the ADM was positioned 1 mm apical to the soft tissue margin, while the soft tissue margin was placed 2 mm coronal to the CEJ. This means that for the TOG group the ADM was 1 mm coronal to the CEJ, while for the SEP group the ADM was 1 mm apical to the CEJ. There may be other factors that influenced this result that are not accounted for. In a previous study at our institution there was a 2 mm gain of KT using ADM plus a coronally positioned flap. [
15] This amount of gain was attributed to the inclusion of some clefting type recession defects. While these defects had minimal KT initially the zone of KT was fully restored following the root coverage procedure. In the present study there was no clear difference between the groups except the ADM positioning.
Since the SEP and TOG groups had similar results the data was combined and sorted by arch. This yielded 8 maxillary sites and 8 mandibular sites. The percent of mean defect coverage was 100% in the maxillary arch, in other words complete defect coverage was achieved 100% of the time. For the mandibular arch 69% defect coverage was achieved and complete coverage was obtained in 2 of 8 or 25% of the sites. This may be attributable to a shallow vestibule and muscle pull in the mandibular sites although the dissection was split thickness in an attempt to release the muscle fibers and prevent any muscle pull during the healing period. Another consideration is that the maxillary sites initially had a mean of 2.1 ± 1.1 mm of KT vs. a mean of 0.8 ± 0.6 mm for mandibular sites. Both of these factors may contribute to the slightly compromised result in the mandibular sites. For mandibular sites the amount of defect coverage achieved was 2.4 ± 0.6 mm, while for maxillary sites the amount was 3.0 ± 0.0 mm. Thus, substantial coverage was achieved for mandibular sites and the treatment was considered successful. None of the sites were considered candidates for additional treatment.
The surgical technique used was modeled after the CPT described by Allen and co-workers [
8,
11]. The suturing technique used was previously described by Dodge and differs slightly from the Allen technique in that it is not subpapillary as recommended by Allen [
1,
8,
11]. This clearly made no difference for maxillary sites, however, further study is needed to determine if use of the Allen technique would have improved the mandibular result. A previous study at this institution indicated that the use of platelet-rich plasma (PRP) did improve the result for mandibular sites [
10]. Based on the outcome of the data analysis by arch the use of PRP for mandibular sites is recommended and may favor an improved amount of recession defect coverage.
5. Conclusions
Within the limitation of the design of this randomized, controlled, blinded pilot study the TOG suturing technique produced results similar to the SEP method. This means the TOG technique is recommended due to the substantial saving of suturing time, about 50%, which benefits both the patient and the surgeon. In addition, the TOG technique resulted in greater gain of keratinized tissue than the SEP method.
Author Contributions
Conceptualization, D.X. and H.G.; methodology, H.G.; software, H.G.; validation, H.G.; formal analysis, H.G., M.H, D.K.; investigation, H.G. and V.P.; resources, H.G.; data curation, H.G.; writing—original draft preparation, D.X.; writing—review and editing, H.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of UNIVERSITY OF LOUISVILLE (protocol code # 13.0332 and 7/18/2013 date of approval).” for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All additional data can be found at the University of Louisville Dental School, Department of Periodontics.
Acknowledgments
This research earned the third prize in the Southern Academy of Periodontology clinical research competition in June 2014 Annual Meeting in Hilton Head Island, South Carolina.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dodge JR, Henderson R, Greenwell H. Root coverage without a palatal donor site using an acellular dermal graft. Periodontal Insights 1998;5:5-8.
- Aichelmann-Reidy ME, Yukna RA, Evans GH, et al. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol 2001;72:998-1005. [CrossRef]
- Henderson RD, Greenwell H, Drisko C, et al. Predictable multiple site root coverage using an acellular dermal matrix allograft. J Periodontol 2001;72;571-582. [CrossRef]
- Hirsch A, Goldstein M, Goultschin J, et al. A 2-year follow-up of root coverage using subpedicle acellular dermal matrix allografts and subepithelial connective tissue autografts. J Periodontol 2005;76:1323-1328. [CrossRef]
- Modarressi M, Wang HL. Tunneling procedure for root coverage using acellular dermal matrix: a case series. Int J Periodontics Restorative Dent 2009;29:395-403.
- Woodyard JG, Greenwell H, Hill M, et al. The clinical effect of acellular dermal matrix on gingival thickness and root coverage compared to coronally positioned flap alone. J Periodontol 2004;75:44-56. [CrossRef]
- Harris RJ. A short-term and long-term comparison of root coverage with an acellular dermal matrix and a subepithelial graft. J Periodontol 2004;75:734-743. [CrossRef]
- Allen EP, Cummings LC. Esthetics and regeneration: Acellular dermal matrix (Alloderm). In: Yoshie H, Miyamoto Y (eds). Technique and Science of Regeneration. Tokyo: Quintessence 2005:124-131.
- Papageorgakopoulos G, Greenwell H, Hill M, et al. Root coverage using an acellular dermal matrix and comparing a coronally positioned tunnel to a coronally positioned flap approach. J Periodontol 2008;79:1022-1030. [CrossRef]
- Shepherd N, Greenwell H, Hill M, et al. Root coverage using acellular dermal matrix and comparing a coronally positioned tunnel with and without platelet-rich plasma: a pilot study in humans. J Periodontol 2009;80:397-404. [CrossRef]
- Allen EP. Subpapillary continuous sling suturing method for soft tissue grafting with the tunneling technique. Int J Periodontics Restorative Dent 2010;30:479-485.
- Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal conditions. Acta Odontol Scand 1964;22:121-135.
- Lobene RR, Weatherford T, Ross NM, et al. A modified gingival index for use in clinical trials. Clin Prev Dent 1986;8:3-6.
- Laster L, Laudenbach K, Stoller N. An evaluation of clinical tooth mobility measurements. J Periodontol 1975;46:603-607. [CrossRef]
- Mehlbauer MJ, Greenwell H. Complete root coverage at multiple sites using an acellular dermal matrix allograft. Compend Contin Educ Dent 2005;26:727-733.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).