1. Introduction
Asthma is defined as the chronic inflammation of the airways in which mast cell, eosinophils, T-lymphocytes, macrophages, neutrophils and the epithelial cells play a decisive role. This inflammatory disorder may intensify it hyperreactivity of the bronchi, which can cause episodes of wheezing, apnea, tight chest pain and cough. These episodes often are associated with obstruction of the respiratory airflow, a condition that becomes reversible either automatically or after pharmaceutical intervention (1).
The most common chronic disease in children is bronchial asthma, in which an increase in its frequency worldwide has been detected in recent years (2). Moreover, bronchial asthma is one of the most frequent causes of children's absence from school but also visits to the Emergency Department of hospitals. In addition, the disease is more common in boys before puberty whereas in girls it is more common during adolescence (3). The global incidence of asthma is estimated at around 7.2%. From this percentage, 6% concerns adults and 10% children, making the conclusion that asthma is now more common in children than in adults (4).
After the completion of a large international epidemiological study (ISAAC) on the asthma and allergic diseases in children, it was observed that its frequency varies significantly from country to country but also in the different regions of the same state. In countries where the western way of life prevails, such as Great Britain, Australia, New Zealand and the United States, asthma occurs with a significantly high frequency (20 - 35%), in contrast to countries in Eastern Europe and Asia that have less development and lower frequencies (3-5%) are recorded (5). The change of the environment and the modern way of living of urban societies, with the galloping production of pollutants but also with the way it is configured interior of houses, enhance the accumulation of allergenic stimuli within its space (6). In Great Britain, where high rates are observed of bronchial asthma, it has been estimated that around fifteen children die annually from the disease. Based on the epidemiological data available for Greece, childhood asthma appears with a percentage of 11% having an upward course and the maximum frequency is observed most commonly at the age of five on average (3).
According to a large epidemiological study that took place in 155 sample clinics, the amount of 463,800 children, which came from six different countries, showed that the asthma rate is between 20 and 30% of the child population. In Greece, three studies have been conducted by Priftis and his colleagues in 1978, 1991, 1998 to investigate the incidence of childhood asthma, which took place in schools of Patras and it was discovered that 6% of this population suffered from the disease. More recent surveys carried out in the Greek territory prove an upward trend course in terms of the frequency of the disease and especially in school-age children (4).
The purpose of this systematic review is to investigate quality of life of children with bronchial asthma and to what extent the disease affects their everyday life. The objectives of the study are the following:
2. Methods
In order to carry out the study, an extensive search was carried out in Greek and international scientific bibliography guided by basic search principles (7). Specifically, a search was made in international and Greek scientific journals, the period of the last 12 years (2010 – 2022), in electronic PubMed, Google Scholar and Scopus with Greek authors or a Greek sample population, likewise and international authors in the English language the above periodical space. The online search included combinations of the following terms/keywords:
a. in the Greek language: "children", "adolescents", "pediatric patients", "asthma", "pediatric asthma", "bronchial asthma", "quality of life", "health",
b. in the English language: “kids”, “children”, “adolescents”, “pediatric patients”, "asthma", "pediatric asthma", "bronchial asthma", "quality of life (QOL)", "health". The international terms were also consistent with those found absent from the catalogs MeSH (Medical Subject Headings,
http://www.ncbi.nlm.nih.gov/mesh).
3. Results
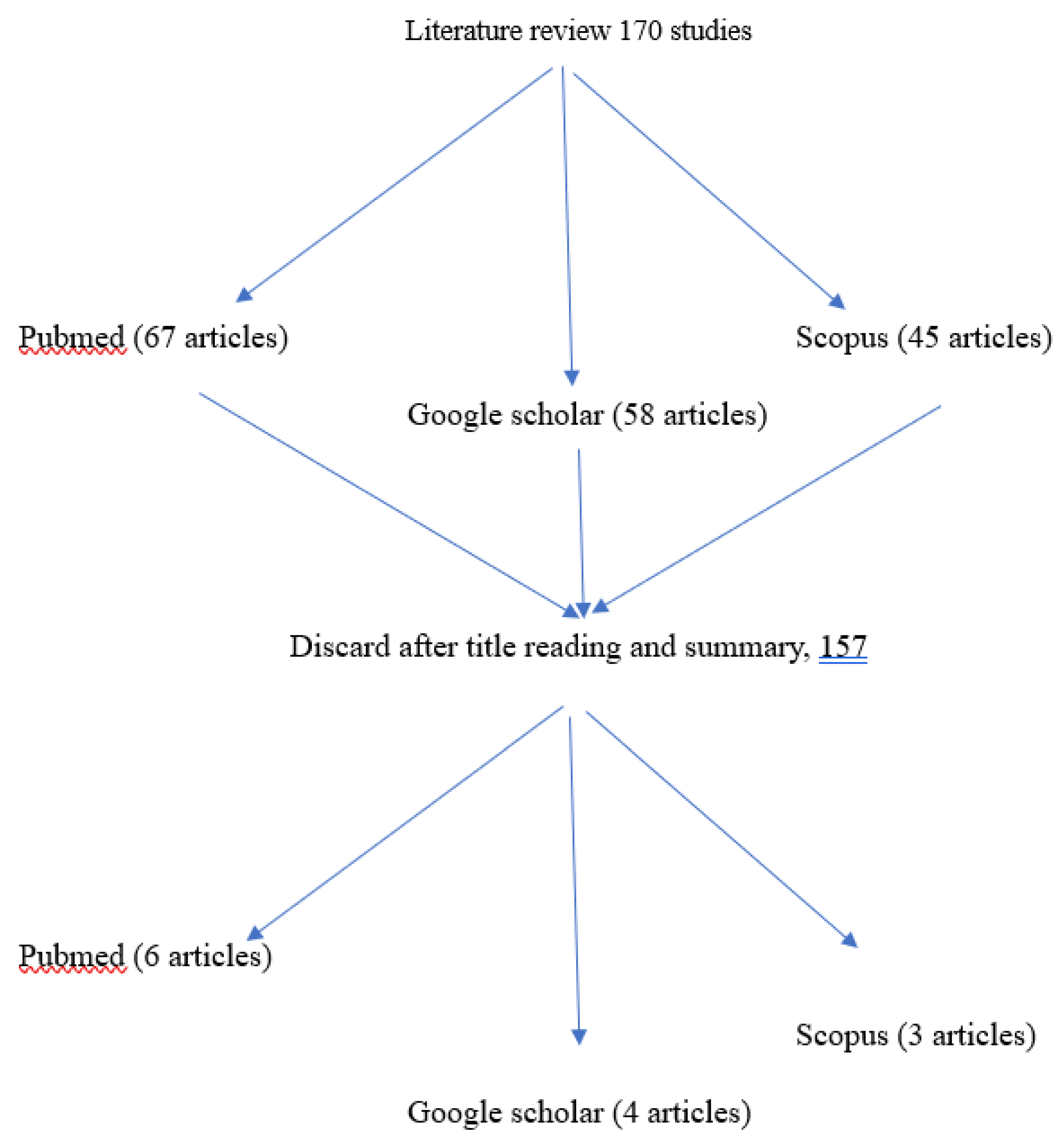
Figure 1 shows the flow chart of the international literature review to investigate the quality of life of children with bronchial asthma. From the international ones PubMed, Google Scholar and Scopus databases were identified, by combination of lemmas (per 2 or 3), a large number of researches of the last five years. Specifically, 67 studies were identified from PubMed, 58 from Google Scholar and 42 from Scopus. Of these, 50 met the special selection criteria with a result after common decision of the researchers of the present study to accept only 13 studies.
In the study of Maher Khdour et al. (8), quality of life (QoL) was assessed and potential risk factors for poor QoL were analyzed among asthmatic children and adolescents. One hundred and thirty-two patients were recruited. It was found that 47 patients (35.6%) had controlled asthma and 85 patients (64.3%) had uncontrolled asthma. When compared to uncontrolled asthma individuals, participants with controlled asthma had improved QoL and scored significantly higher in the symptom domain (P = 0.002), activity domain (P = 0.004), emotional domain (P = 0.002), and overall PAQoL scores (P = 0.002). In general, the results of the present study showed that in children and adolescents, uncontrolled asthma, disease severity, and previously hospitalized patients were associated with poor QoL.
The research by Agrawal et al. (9) aimed to discover any correlation between presence and severity of asthma and the quality of life of African American children origin of low socio-economic level. The study was conducted at the National Children's Hospital of Washington (CNH), in which 66 children, aged 9 – 12. The sample was divided into two groups, one consisted of 36 children who had asthma and in the other 30 who may have suffered from some other disease. The conclusions from this research was that children with asthma and their parents presented lower quality of life compared to the rest. In addition, children with mild asthma, as well as children with university graduate parents had a higher quality of life.
Through the clinical trial they conducted, Montalbano et al. (10) wanted to see if educational programs through a phone application can improve the quality of life of children with asthma. The sample consisted of 47 children aged 6 – 11 years with moderate asthma. The researchers were able to prove their theory, as the results showed that applying such educational program, the children's quality of life improves.
Banjari et al. (11) through their research sought to evaluate the level management of asthma and distinguishing its relationship with quality-of-life suffering children. The study took place in the city of Jeddah, Saudi Arabia and the sample consisted of 106 children diagnosed with bronchial asthma. The research showed that the quality of life of children with uncontrolled asthma was significantly lower as all the psychosocial domains of their lives (activity, symptoms, emotional function) were equally affected. Furtado et al. (12) through their research attempted to verify the anti how there is a correlation between quality of life, severity of asthma, sleep disorders and physical activity in 48 children with asthma aged 7-12 years old from Natal, Brazil. The results of the research showed that the disease severity, sleep quality and shortness of breath after exercise affect the quality of life of children with asthma.
The research of Hallit et al. (13) focused on highlighting the factors that likely to affect the quality of life of children with asthma. They participated in the study 300 children aged 7-16 from a clinic exclusively for pediatric asthmatics patients and from schools of various cities in Lebanon. The researchers concluded that conclusion that the main factor affecting the quality of life of these children is disease management. Other risk factors for low quality of life were seen what it's like to have pets at home and to be infected by some other respiratory disease diseases at the age of less than 5 years.
Kouzegaran et al. (14) investigated the various dimensions of the quality of life of children with asthma in the city of Mashhad, Iran. The sample of 200 children, age range 8-12 years old, were divided into two equal groups. In one group belonged healthy children and on the other children who suffered from bronchial asthma. The comparison of the two groups showed that children with asthma had poor quality of life compared to physically healthy children activity, psychological status and school performance.
Stridsman et al. (15) investigated differences in asthma and quality of life of adolescents depending on the management and severity of the disease between the two genders. The sample consisted of children aged 14-15 years from Northern Sweden which were divided into two groups. One had 128 girls and the other had 119 boys. The comparison of the two groups made it clear that uncontrolled asthma as well as bad quality of life are found in a higher percentage in girls than in boys.
In the study conducted by Kalyva et al. (16) an attempt was made to investigate the vs how age, sex, severity and duration of asthma as well as exposure to parental smoking affects the quality of life of children with asthma. In the study 173 children aged 8-12 years participated, where they were selected by the Pediatric Asthma Unit of the AHEPA University General Hospital of Thessaloniki and the rest from 10 private clinics in Northern Greece. After analyzing the results, the researchers concluded that the severity of asthma is negatively correlated with children's quality of life. Finally, the report in parental smoking is associated with an increase in asthma symptoms, problems in treatment and with more anxiety.
Manion & Velsor – Friedrich (17) in a study they conducted in 2017 in Chicago wanted to compared pediatric asthmatic patients by body weight in order to examine whether obesity may affect quality their lives. Of the 90 children who made up the sample, aged 9 to 14, 36 were overweight or obese based on their Body Mass Index (BMI). During the conduct of the study, it appeared that obese children suffered from severe asthma and were those with the highest number of hospital admissions. Finally, despite everything argued the researchers, what was identified was that obesity combined with asthma did not affect the quality of life of these children until disease severity was taken into account. It appeared, that is, that his seriousness of asthma affects the quality of life of obese asthmatic children just as well and in those with normal weight.
In the longitudinal study by Li et al. (18) in Florida, USA. examined whether the quality of a night's sleep affects asthma control and quality of life asthmatic children, aged 8 – 17.9 years. After extensive analysis of the results obtained, the researchers concluded that its insufficient control disease is associated with poor sleep quality, poor quality of life and severe sleepiness during the day. Poor night sleep quality, individually, was not seen to affect the quality of life of asthmatic children.
Miadich et al. (19) investigated the possibility of differences in quality of life of children with asthma by age. The children who participated were 215, aged from 5 – 12 years old. The results showed that the severity of asthma affects the child's everyday life, and therefore his quality of life, as he grows older of. Specifically, of all the children who suffered from severe asthma, the older ones had lower quality of life compared to the younger ones.
Taminskie et al. (20) in their cross-sectional study, considering as given that asthma control significantly affects their quality of life of afflicted children, attempted to investigate the negative effect of others as well factors such as passive smoking, humidity, children's contact with domestic animals (dogs, cats) etc. The sample of 553 children, aged 2 – 16 years, was selected from various primary and secondary health care structures in Scotland. The main finding of the research was that the factors that made it more difficult for her quality of life of the children in the sample concerned either factors that could easily avoidable (e.g., passive smoking) or treatable coexisting diseases (e.g., allergic rhinitis).
Tools for measuring the quality of life of children with bronchial asthma
In the analysis of the selected review studies, it was realized by the female researchers that many of them used various research tools. This it is clear from the fact that most of them were aimed at his investigation level of quality of life of asthmatic children in relation to someone specific factor such as, for example, the quality of sleep, body weight, physical activity etc.
Table 1 presents the research tools that were used by the authors of the selected studies which, however, concern exclusively measuring quality of life.
4. Discussion
The thorough analysis of the research articles selected for its processing present thesis in order to investigate the level of quality of life of children suffering from bronchial asthma led the researchers to the conclusion that the general level of quality of life of these children appeared to be relatively low. In summary, the quality of life of children with asthma was assessed in terms of physical activity, emotional state, school performance, social life and the quality of sleep.
According to Agrawal et al. (9), the quality of physical activity appears to be significantly lower in children with asthma. This may be due to cases of no controlled (11) and/or severe asthma (14). Also, Furtado et al. (12) observed that low quality of life is directly related with the occurrence of episodes of shortness of breath after exercise. According to the same research, the activities that cause more discomfort in children are running, climbing and football. Finally, many children wanted to participate in above activities but avoided it because of their parents' fear of possible paroxysms.
Regarding the emotional state of children with asthma, Kouzegaran et al. (14) concluded that it was correlated with their quality of life and lower in compared to that of healthy children. On the other hand, Banjari et al. (11) did not detect differences comparing asthmatic and healthy children.
The social life of children with asthma and how much it is affected by the disease seems to have been investigated by Banjari et al. (11), Kouzegaran et al. (14) and Agrawal et al. (9), who concluded that one does not affect the other.
Asthma does not appear to have a negative impact on the school performance of children who are sick, according to Agrawal et al. (9). In contrast, Kouzegaran et al. (14) concluded that children with asthma struggled in school compared to healthy children.
Regarding sleep quality, there is agreement between the researches of Furtado et al. (12) and Li et al. (18). Specifically, the two studies argue that the existence of sleep disorders cannot individually disturb the general quality of life but only when combined with other factors such as asthma management etc.
The main factors that affect either positively or negatively on the quality-of-life asthmatic children are asthma management, asthma severity and various environmental factors, without, however, being the only ones.
The quality of life of children with asthma is understood to be significantly affected by the management of the disease as seen in the studies of Hallit et al. (13), by Taminskiene et al. (20), by Furtado et al. (12) and Banjari et al (11). That is, the better the asthma management, the higher the level of quality of life.
The severity of asthma is perhaps the most important factor affecting quality of life, as can be seen from the conclusions of those studies that dealt with him specific factor. Specifically, Hallit et al. (13) concluded that the asthma symptoms and the emotional state of asthmatic children are directly affected by the severity of the disease. Still, they concluded that the more the milder the asthma, the better the child's quality of life, as well as the reverse. This finding is in agreement with the results of Agrawal et al. (9), by Furtado et al. (12) and Kalyva et al. (16).
According to Taminskiene et al. (20) and Montalbano et al. (10) the systematic exposure of asthmatic children to a smoke environment negatively affects the quality their lives.
Regarding the gender of the children, there was a big dichotomy. Hallit et al. (13) and Taminskiene et al. (20) argued that gender did not appear to play a role in level of quality of life. On the other hand, Kouzegaran et al. (14) observed that the girls with asthma had a better quality of life than boys. However, the research of Stridsman et al. (15), which involved only adolescent subjects, concluded that the girls of this age group had a worse quality of life than boys.
The children's age did not appear to affect their quality of life according to Hallit et al. (13) and Kalyva et al. (16). In contrast, in the research of Miadich et al. (19) observed that older children with severe asthma had worse quality of life from the smallest as her obligations and obstacles multiplied their daily life.
In the research of Taminskiene et al. (20) found obesity to be a neg quality of life factor in children with asthma. However, Manion & Velsor–Friedrich, (17) failed to demonstrate a correlation between the quality of life of children with asthma and their weight.
Moreover, in the study of Taminskiene et al. (20) how many children suffered from coexisting rhinitis presented a decline in their quality of life due to worsening of symptoms and emotional breakdown.
The investigations of Hallit et al. (13), by Banjari et al. (11), by Agrawal et al. (9) and of Li et al. (18) came to the same conclusion regarding the effect of the formative level of parents in the quality of life of their asthmatic children. Specifically, parents with a high level of education may positively influence his quality of life their sick child.
Finally, as a positive factor influencing the level of quality of life of children with asthma appeared to be the socio-economic well-being of their families, according to studies by Taminskiene et al. (20) and Banjari et al. (11).
Finally, the better management and as a result the improvement of the quality of life of children with asthma was demonstrated by Mondalbano et al. (10), using teachers programs provided by a phone application.
5. Conclusions
In conclusion, the results of the present study demonstrated that its level quality of children suffering from bronchial asthma is affected by both factors concerning the disease as well as from their environment. Objective of the medical nurse staff should be the guidance of asthmatic children and families them towards achieving a carefree and productive everyday life. the realization, however, this goal requires the acquisition of complete knowledge regarding who areas of the quality of life of these children are affected and by what factors, in what grade etc.
The contrasts presented in the analysis of the studies under study provide food for further research to clarify what ultimately constitutes the general rule. Still, the complete absence of relevant studies in the Greek area gives another motivation search for answers to the specific research question.
With in-depth quality of life information in mind, the health professionals can join the medical nursing care of children with asthma methods of achieving and maintaining a good level of physical fitness activity, sleep, emotional state, social life, etc. with remotes purposes the best outcome of the disease but mainly the conquest of a full way life that does not differ in any way from that of healthy children.
References
- Cohn, L.; Elias, J.A.; Chupp, G.L. Asthma: Mechanisms of disease persistence and progression. Annu. Rev. Immunol. 2004, 22, 789–815. [Google Scholar] [CrossRef] [PubMed]
- Luxner, K.L. Asthma, Pediatric Nursing Athens: Publications Paschalidis. 2001; pp. 112–119.
- Ferrante, G.; La Grutta, S. The burden of pediatric asthma. Front. Pediatr. 2018, 6, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Priftis, K. Childhood Asthma: Increasingly common, Society and Health; 2002; pp. 157–171.
- Luxner, K.L. Asthma, Pediatric Nursing Athens: Publications Paschalidis. 2011; pp. 112–119.
- Tsanakas, I. Asthma. Basic Pediatrics. Athens: GM Design. 2005.
- Patelarou, E.; Brokalaki, H. Methodology of the systematic review and meta-analysis. Nursing 2010, 49, 122–130. [Google Scholar]
- Khdour, M.; Abu Ghayyadeh, M.; Al-Hamed, D.; Alzeerelhouseini, H.; Awadallah, H. Assessment of quality of life in asthmatic children and adolescents: A cross sectional study in West Bank, Palestine. PLoS ONE 2022, 17, e0270680. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, S.; Iqbal, S.; Patel, S.J.; Freishtat, R.; Kochhar-Bryant, C. Quality of life in at—Risk school-aged children with asthma. J. Asthma 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Montalbano, L. , Ferrante, G., Cilluffo, G., Gentile, M., Arrigo, M., La Guardia, D., Allegra, M., Malizia, V., Gagliardo, R.P., Bonini, M., et al.Targeting quality of life in asthmatic children: The MyTEP pilot randomized trial. Respir. Med. 2019, 53, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Banjari, M.; Kano, Y.; Almadani, S.; Basakran, A.; Al-Hindi, M.; Alahmadi, T. The Relation between Asthma Control and Quality of Life in Children. Int. J. Pediatr. 2018, 2018, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Furtado, P.R.; Maciel, Á.C.C.; Barbosa, R.R.T.; Silva AAM da Freitas DA, d.e.; Mendonça, K.M.P.P. Association between quality of life, severity of asthma, sleep disorders and exercise capacity in children with asthma: A cross-sectional study. Braz. J. Phys. Ther. 2019, 23, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Hallit, S.; Raherison, C.; Waked, M.; Hallit, R.; Layoun, N.; Salameh, P. Validation of the mini pediatric asthma quality of life questionnaire and identification of risk factors affecting quality of life among Lebanese children. J. Asthma 2019, 56, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Kouzegaran, S.; Samimi, P.; Ahanchian, H.; Khoshkhui, M.; Behmanesh, F. Quality of life in children with asthma versus healthy children. Open Access Maced. J. Med. Sci. 2018, 6, 1413–1418. [Google Scholar] [CrossRef] [PubMed]
- Stridsman, C.; Backman, H.; Eklund, B.M.; Rönmark, E.; Hedman, L. Adolescent girls with asthma have worse asthma control and health-related quality of life than boys—A population based study. Pediatr. Pulmonol. 2017, 52, 866–872. [Google Scholar] [CrossRef] [PubMed]
- Kalyva, E.; Eiser, C.; Papathanasiou, A. Health-Related Quality of Life of Children with Asthma: Self and Parental Perceptions. Int. J. Behav. Med. 2016, 23, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Manion, A.B.; Velsor-Friedrich, B. Quality of Life and Health Outcomes in Overweight and Non-Overweight Children With Asthma. J. Pediatr. Health Care 2017, 31, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Thompson, L.A.; Gross, H.E.; Shenkman, E.A.; Reeve, B.B.; DeWalt, D.A.; Huang, I.C. Longitudinal associations among asthma control, sleep problems, and healthrelated quality of life in children with asthma: A report from the PROMIS® Pediatric Asthma Study. Sleep Med. 2016, 20, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Miadich, S.A.; Everhart, R.S.; Borschuk, A.P.; Winter, M.A.; Fiese, B.H. Quality of Life in Children with Asthma: A Developmental Perspective. J. Pediatr. Psychol. 2015, 40, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Taminskiene, V.; Mukhopadhyay, S.; Palmer, C.; Mehta, A.; Ayres, J.; Valiulis, A.; Turner, S.W. Factors associated with quality of life in children with asthma living in Scotland. Pediatr. Pulmonol. 2016, 51, 484–490. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).