1. Introduction
Important dento-alveolar, occlusal and skeletal changes occur and are diagnosed during the mixed dentition. Some of them require early treatment (interceptive) in order to prevent aggravation of the problem during the active growth period. The main clinical problem, that often arises, is the provision of an anchorage zone with included permanent tooth. This may be provided by usage of personal rigid grid which connected these teeth. Orthodontic mini-implants are not applicable in vestibular areas with developing tooth germs. The available stable permanent teeth in the early mixed dentition are often an insufficient support unit, which is placed in distance of the active area. Use of metal orthodontic grids designed and printed digitally has expanded the limits of orthodontic treatment, especially in its interceptive phase.
Advances in digitization have created many possibilities for customizing orthodontic appliances. CAD-CAM technologies allow to make a momentary intraoral scan of both tooth rows and their occlusal relationships, digital analysis of all paraclinical studies, but also to make computerized individual design of appliance or additional auxiliary devices [1-4]. In orthodontics most of the printed devices are from biocompatible composites or metal. Today, 3D printing of laser-sintered metal orthodontic grids is the basis for the development of modern orthodontics [5, 6]. The reduction of the stages of appliance’s production (intraoral scanning – computer design – printing) occur combined with minimization of the human errors and without heavy physical activity [7, 8]. The modern laser-sintered orthodontic appliances provide exceptional detail precision [9-13] and have predictable geometry of tooth movements [
8]. The construction of the appliances can be tailored to the geometry of the forces for biomechanical action and moments produced by it. The extreme accuracy of the devices does not allow the generation of residual tensions voltages. There is already a lot of research on the topic in regards to their mechanical properties, electrochemical behaviour and biocompatibility. Most often, the printed devices are made of cobalt-chromium (Co-Cr) alloys [
10], which are strong. Their mechanical properties such as hardness, strength and modulus of elasticity must be known, because it is necessary to guarantee their wear and, at the same time, the printed devices should not be dangerous to the hard tissues (teeth) on which they are placed and debonded, therefore they also can undergo deformation [
14]. The appliances must be strong enough to withstand masticatory forces during chewing without any permanent deformation, maximum accuracy and reduced risk of human error and deviation in geometry [15, 16]. They increase the predictability of the result, but require the orthodontist's technical preparation and financing [17, 18].
As every orthodontic force produces a reactive force of equal magnitude, the success of the orthodontic treatment depends on the anchorage and the elimination of side effects, including the unwanted teeth movement or tooth segments.
Our aim is to describe a fully digital model for providing anchorage during orthodontic-surgical traction of impacted teeth in the mixed dentition’s period. We shall critically describe and discuss metal-printed grids to support orthodontic treatment.
2. Materials and Methods
2.1. The Method Used to Produce the Grids Is 3D Additive Printing - Selective Laser Melting (Sintering - SLS)
After the patient and parents have accepted the orthodontic treatment plan, we perform the intraoral digital scan. We design the anchorage orthodontic grid on the obtained STL file with the help of CAD/CAM software. The generated file with the future grids is exported to the 3D metal printing machine for production. For the fabrication of a Co-Cr grids, we used metallic powder Wirobond C+ (BEGO Medical GmbH) with composition Co-64%, Cr-25%, V-5%, Mo-5% and a laser sintering grids Truprint 1000 (Trump Group). In this technology, the powder is heated above the melting temperature using a high-energy CO2 beam, thereby sintering/melting the particles together in a set pattern. Next comes a curing process that proceeds layer by layer until the entire material is printed. It is finished with removing the support elements, avoiding solder joints and other thermal effects.
2.2. We present the treatment of three clinical cases with digitally designed and printed metal grids, used for anchorage in orthodontic treatments. Most often in practice, we use them for extrusion of retained teeth in a mixed dentition or in segmental treatments. We incorporate segments on the same or opposite side with stable permanent teeth. The system of fixed and blocked teeth, placed away from the area of action, is built to absorb the generated counter force.
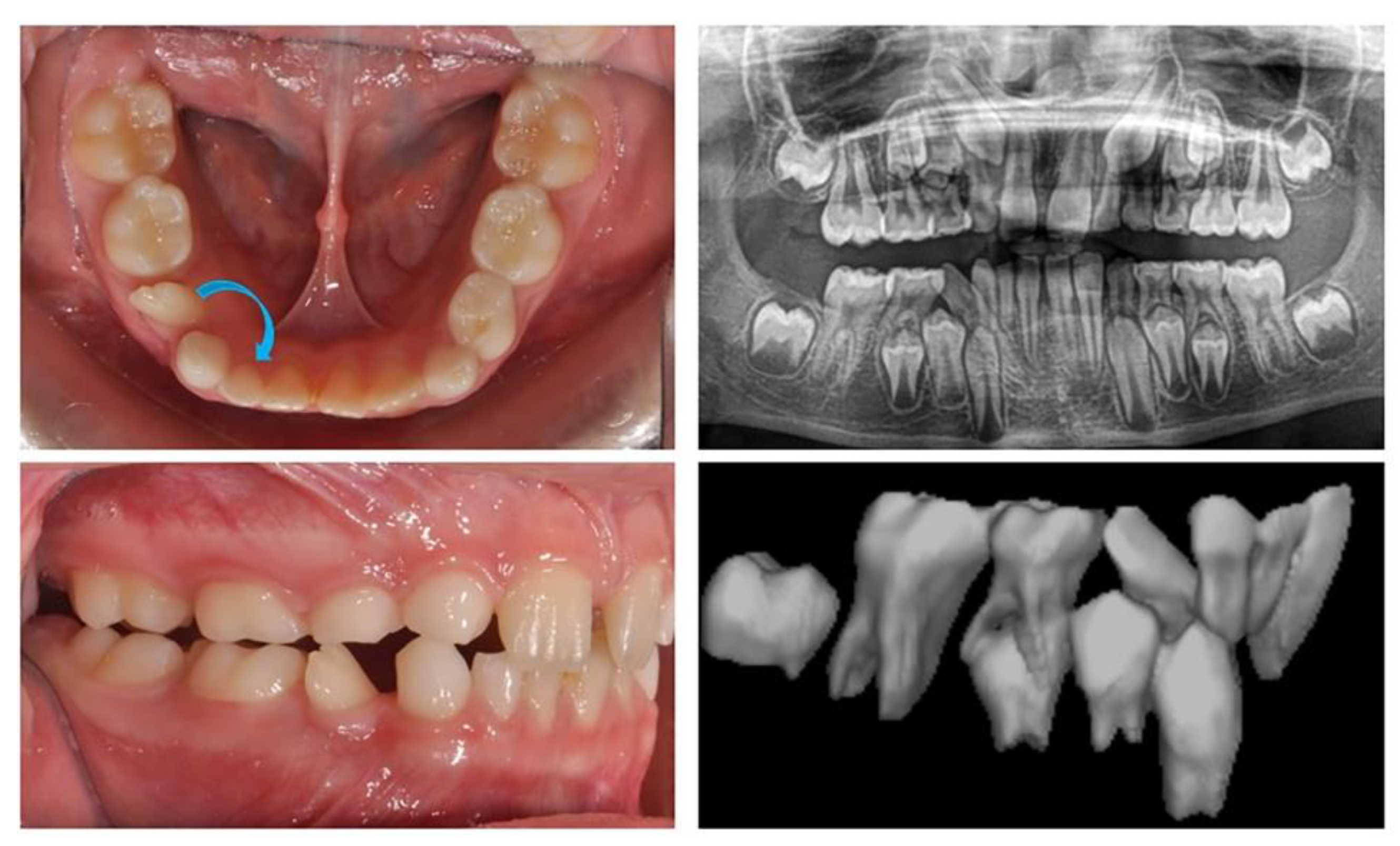
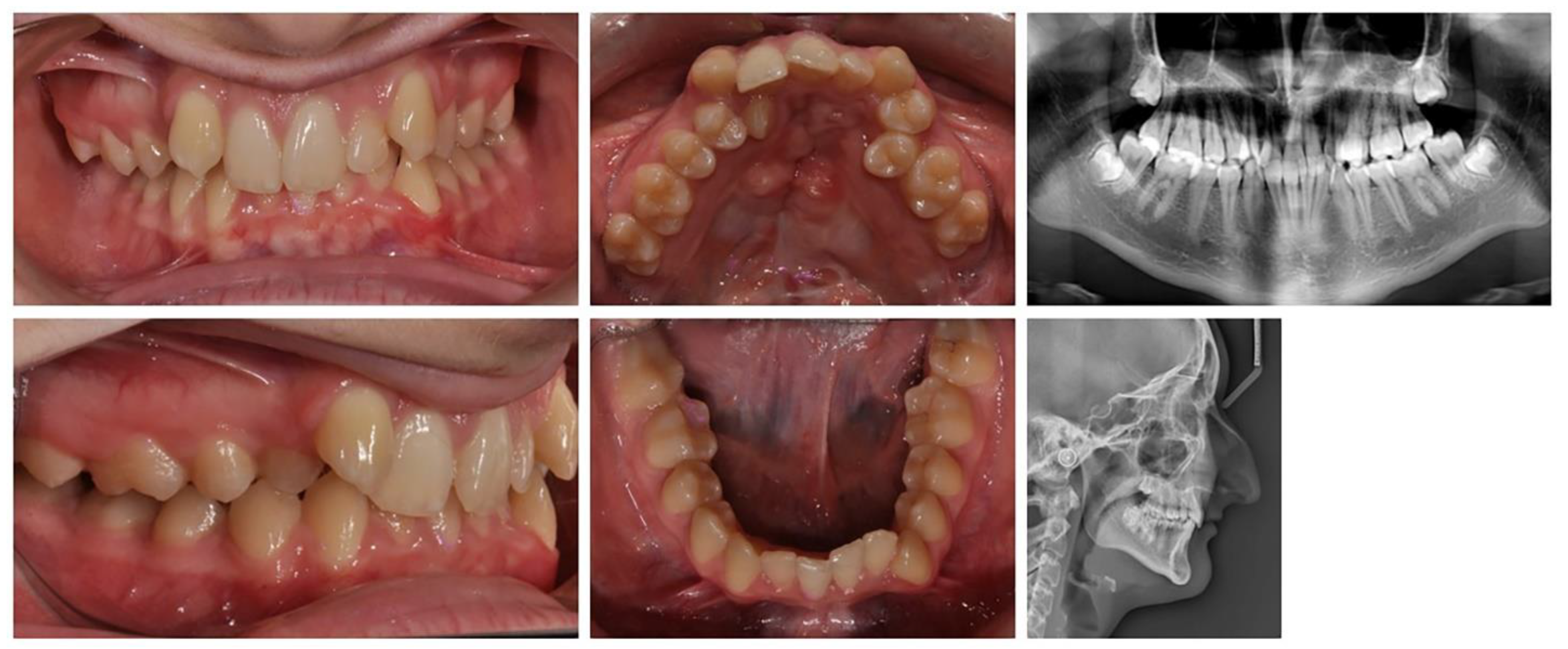
2.2.1 We present an 8-year-old girl with an ectopic eruption of the lower right lateral (42) in the area of the first temporary molar. In the lower dental arch, the temporary right lateral and canine are with preserved positions. After an X-ray examination, hypodontia of the upper laterals was established in the upper dental arch. The well-developed and normally positioned germ of right canines and premolars in the lower were found (
Figure 1). In this early phase of mixed dentition, the ectopically placed lower right lateral should be positioned in its normal location. This will prevent future canine transposition or canine retention due to the mechanical barrier that the lateral presents. At the same time, it is important to preserve the perimeter of the dental arch, in the earlier exfoliation of the temporary canine.
Medial movement of the lateral needs to be as lingual as possible along the highest part of the alveolar ridge to accommodate the canine germ, which is positioned more vestibular. Therefore, an anchorage point is needed to apply a medially directed force from the lingual (side). In this phase of mixed dentition, only the permanent first molars are stable. Therefore, the solution is a rigid lingual arch with a hook in the area of the central incisors, as a fulcrum to apply the force to straighten and move the lower right lateral.
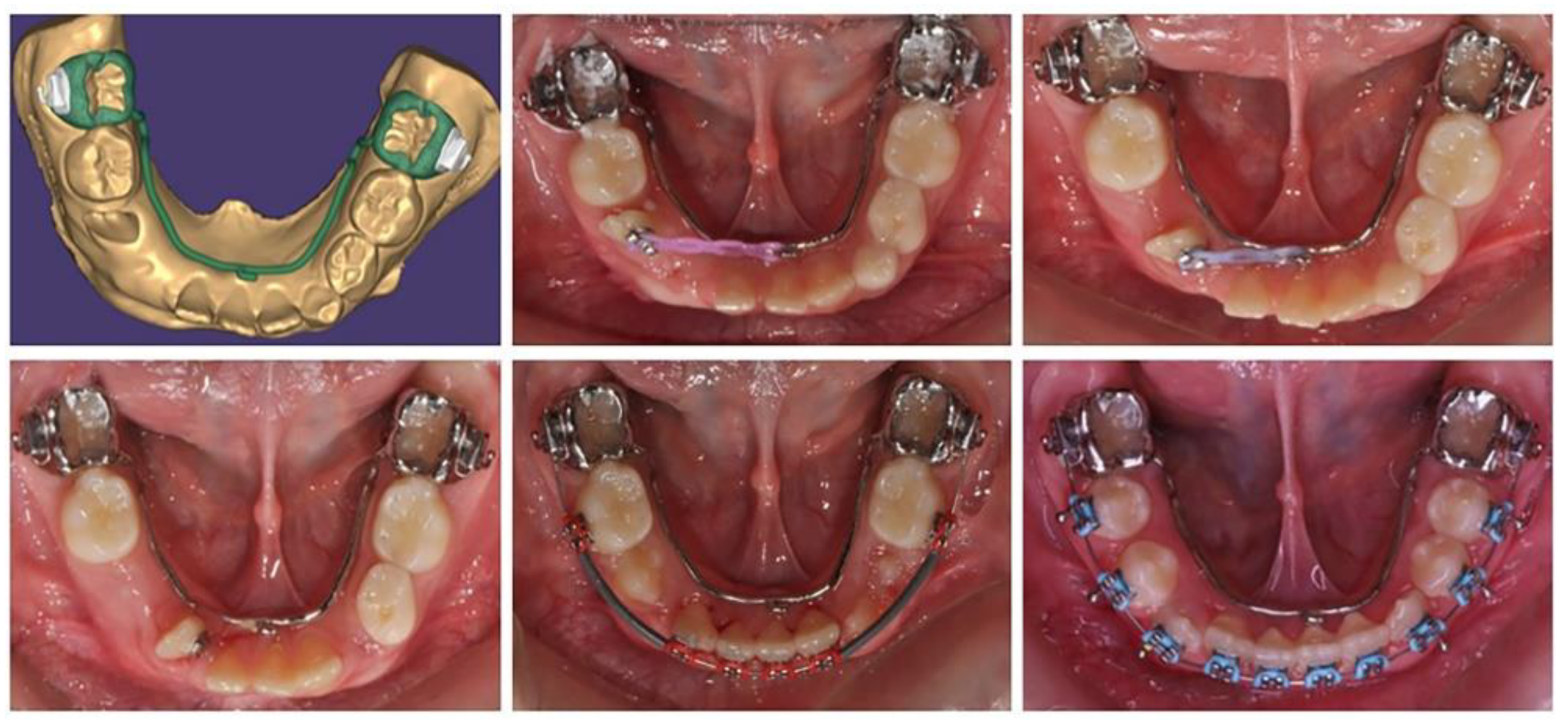
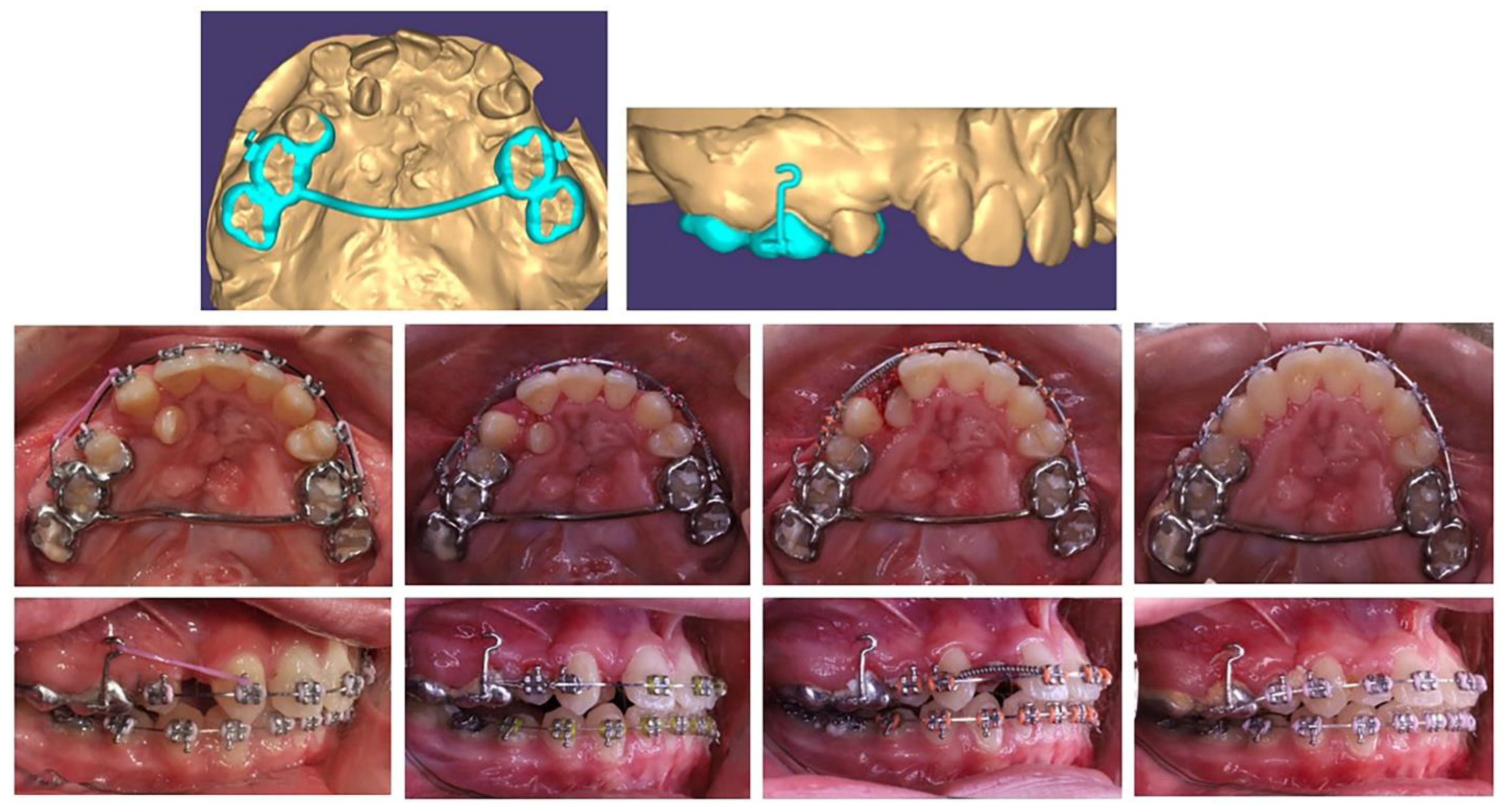
Based on the patient's digital model, a lingual arch design was made with a hook in suitable location and direction for anchorage to tooth movement of the lower right lateral (
Figure 2). The placed printed grids are maximally reduced, but at the same time stable enough to be anchorage. The patient adapted to it in a short time and the biomechanical system used showed a good result.
After moving the lateral incisor to its normal location in the lower dental arch, proceed to its levelling with the Utility arch, follow the eruption of the canine and both premolars. The treatment ended with the complete levelling of the dental arch.
2.2.2. We present a 10-year-old girl aimed for the orthodontic treatment by Maxillofacial surgeon. A cystic lesion involving teeth 44 and 45 was detected, which was operated on and tooth 44 was extracted. A follicle cyst was detected in the upper dental arch at tooth 16, which changed the direction of development of the germ of the upper right first molar (
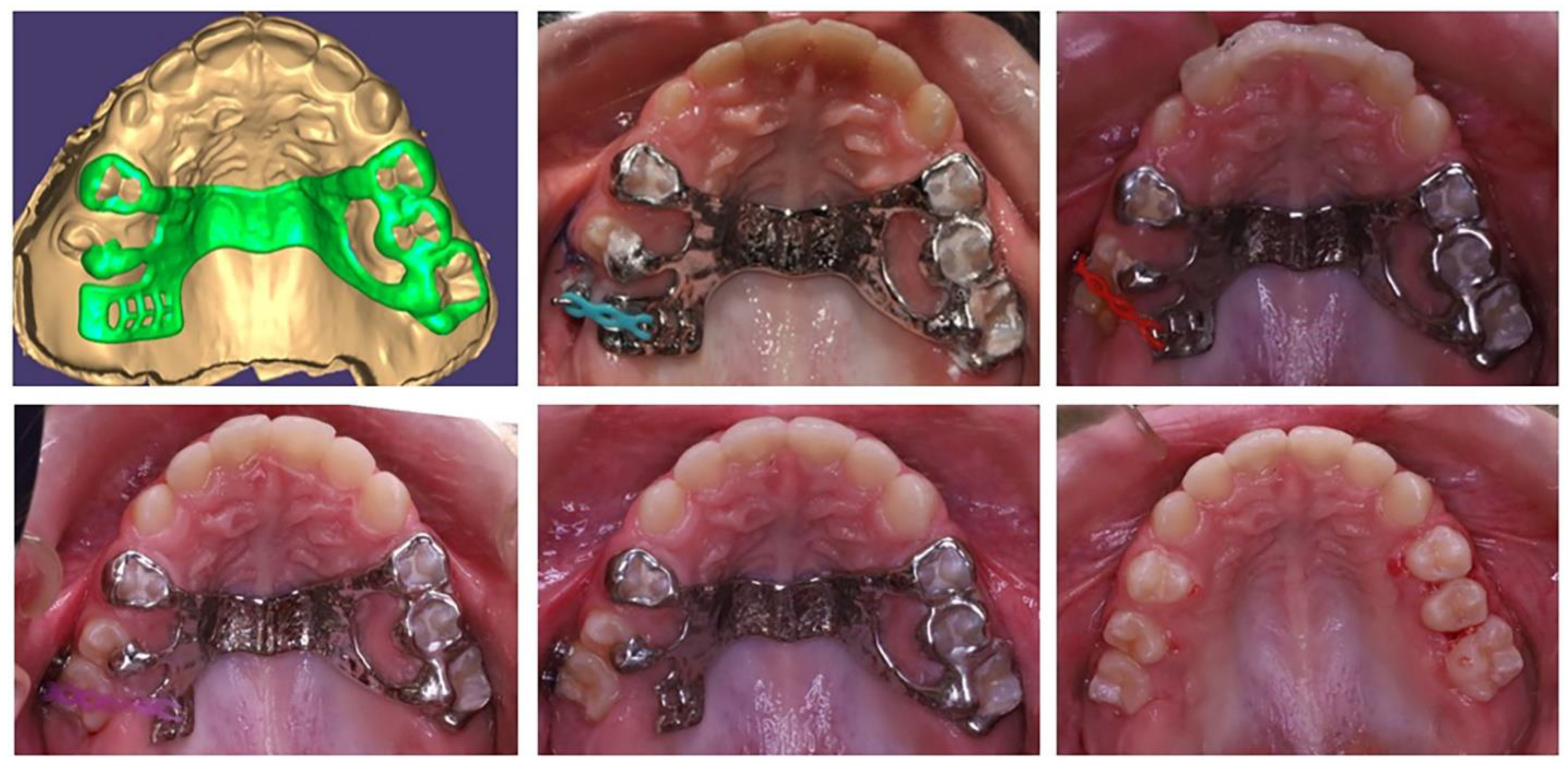
Figure 3). The molar is impacted with the crown in vestibular direction. Its orthodontic traction is recommended. For this, it is necessary to construct an anchorage area in the palate. The characteristics of the bone do not allow the use of mini-implants. Therefore, the plan includes a printed metal grid, including the premolars on both sides and the left first molar, as well as part of the hard palate. In the area of tooth 16, a "ladder" is designed with a series of hooks for attaching the elastic chain. The grid is printed from Co-Cr metal and fits perfectly.
After surgical exposure of the upper right first molar, the grid was glued and molar traction started (
Figure 4). When the position of the molar changed, part of the ladder was removed, so that the bearing area changed along with the movement of the tooth.
The movement of an upper first right molar is firstly- rotation – a change in the direction of the clinical crown from vestibular to occlusal and then vertical movement until reaching the occlusal plane (
Figure 5). The initial position and the change of the fulcrum from the grid allowed these movements. After traction (extrusion) of the upper right first molar to the level of the occlusal plane, the complete corrective orthodontic treatment with a fixed technique is planned.
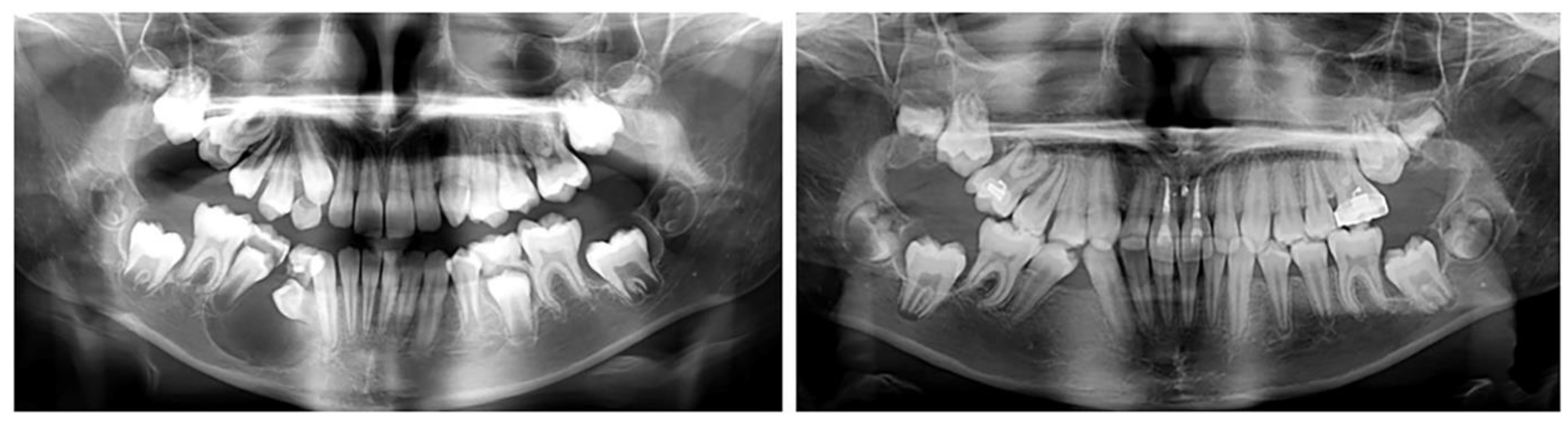
2.2.3. A 17-year-old female patient with a surgically repaired cleft of the hard palate. The patient's complaints are worsened aesthetics. During the first clinical examination, a reduced perimeter of the upper dental arch was found, crowding was observed both in the frontal and in the middle segment (in the area of premolars), the shape of the dental arch was changed - trapezoidal. The upper right lateral is located at the palate and the canine is medially located in contact with the central incisor. The upper frontal teeth are retruded and extruded, the bite is covered (
Figure 6).
For the purposes of orthodontic treatment, extraction of two upper premolars (14 and 25) is required, which will provide a space exactly equal to the crowding size (the sizes of right lateral and left premolar). It is not desirable to design a biomechanical system in which there will be medial displacement of the distal anchorage teeth, as it occurs with the classic distal displacement of canines and anchorage second premolar and first molar (anchorage type A). In this clinical case, a stable distal anchorage zone is required, which can be provided by mini orthodontic implants or a rigid transpalatal arch involving all available anchorage teeth (
Figure 7). When fabricating this type of digitally planned arch, elements can be incorporated into its design to aid in a more body movement of the canines, which will reduce the side-inclination effects of their movement.
The anchorage transpalatal arch construction, designed by us includes first and second molar rings, right second premolar lingual wall, first molar tube, and an extended right first molar hook for a higher level of applied canine distalizing force.
The teeth in the upper and lower dental arch are levelled and the occlusal relationships are normalized. The aesthetics of the frontal segment have been restored. From a smile with five frontal upper teeth (13, 11, 21, 12 and 13) a symmetrical smile was achieved with inclusion of the palatally located upper right lateral in a normal position. A well-designed metal anchorage system did not allow medialization of the abutment teeth. Complete preservation of the perimeter of the upper dental arch was achieved.
3. Results
In the three clinical cases, individually created anchorage systems were used through design software and metal grid were printed. The devices are placed in the oral area which does not disturb the aesthetics of the patient. Due to the extreme accuracy of the devices, their adjustment is not necessary and the clinical time for their placement and management is completely reduced. With the grid constructed in this way, no deviation is foreseen in the biomechanics of their action. Their rigidity is sufficient as a support when using biological orthodontic forces. No movements or other negative changes were detected in the teeth included in the support brackets.
The printed additional grids are applicable both in mixed dentition and in complicated clinical cases in permanent dentition. Their individuality allows for segmental treatments or treatments for dental conditions requiring additional anchorage further from the active force.
4. Discussion
The digital technologies that we use in orthodontic practice expand the possibilities of orthodontic treatments by relying on the creativity of the healer, a good technical and software base. New materials for printing, especially resins and plastics, diversify the type of devices used for leveling (aligners). CAD/CAM designs in orthodontic practice are mostly used in the retention phase to produce metal sintered or milled retainers [
19]. While metal printing or milling helps with complicated orthodontic treatments requiring a sufficient support area or greater forces. It is not unusual to work with printed lingual or transpalatal arches [
7], but the possibilities of their individualization and expansion of the construction with different hooks, buttons and arms have made them a valuable element of orthodontic therapy.
We use conventional TPA most often for support, but its possibilities have impact on the three directions: transverse expansion in the molars, rotational movements, extrusion and intrusion changes of the molars. The disadvantages faced by orthodontists when working with classical TPA are that it requires good manual skills in bending, adapting and activating it [20, 21]. A change in the planned geometry is possible when the arch is activated. The digitally printed arch is rigid and does not allow corrective movements at the molars, but is a stable support. The planned molar rings do not traumatize the papillae. An advantage is that it is possible to plan the inclusion of the second molars in the arch, and even the medially located premolars. The alloy from which it is produced is reliable to take the load.
Many experiments and analyses have been done for their resistance to torsion, which show that their stability and strength can be relied upon [
22]. Zinelis et al. [
14] have tested Co-Cr orthodontic grids and obtained results that show that these grids have clinically acceptable mechanical properties that remain unaffected by intraoral aging.
The biggest advantage in the design of grids designed with appropriate software is that the support points (hooks, extensions, buttons, loops, etc.) can be planned in places approximately close to the level or in the area of the very centre of resistance of the tooth or tooth group that will be moving. This provides a movement that is very close to the hull and at the same time a support area that does not change. The vertical extensions, which can be planned in the printed grids, have a height that is consistent with the centre of resistance of the tooth to be moved. Thus, the power arm is correctly positioned and the body movement of the tooth is achieved [23, 24]. The individually planned vertical extension (shoulder) complies with the relief of the alveolar ridge, the required height and is maximally comfortable for the patient. Such extensions can be made in the design of different orthodontic grids and in different planes.
The role of the lingual arch is also not the same as in the traditional one. With the printed lingual arch, it is not possible to straighten the inclinations of the lower first molars, but only to preserve their existing position. Therefore, with the printed form, we can keep the perimeter, but not increase or change it.
The advantage of the digitally designed lingual arch is that it improves the support zone during orthodontic extraction of impacted teeth even in mixed dentition, in teeth with suspected ankylosis, it can stabilize the adjacent ones and counteract the intruding counter force.
One of the great advantages of digitally printed grids is that their main components can be placed orally, making them more invisible and aesthetic for patients. Their other advantages are cost-effectiveness, improved quality, speed and accuracy; predictability [
28]. Grids produced by the printing method have less material loss than those made by milling, which also affects their price, making them affordable [
25,
26,
27]. The created device is of high complexity and shape that serves individual treatment. At the same time, this is achieved with reduced human involvement, which reduces the level of error, and with reduced costs, because several machines are printing at the same time.
5. Conclusions
Modern orthodontics works with new digital algorithms for diagnosis and treatment planning, as well as for the customized creation and production of orthodontic grids. Orthodontic treatments in the interceptive phase of mixed dentition are possible because it is not necessary to wait for teeth to erupt from the distal anchorage zone. With custom-designed grids, more distant teeth can be incorporated into a common unit to support and normalize the position of individual ectopic or impacted teeth.
Author Contributions
Conceptualization, G.Y.; methodology, G.Y. and M. T.; resources, G.Y.; writing—original draft preparation, G.G. and M.G.; writing—review and editing, G.Y. and M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, G.G., upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jyosthna A, Xavier Dhayananth L, Evan A Clement, Piradhiba R, Navaneetha Nambi, A Review–CAD/CAM in Orthodontics, J Res Med Dent Sci, 2022, 10 (2):253-257. [CrossRef]
- Küffer, M.; Drescher, D.; Becker, K. Application of the Digital Workflow in Orofacial Orthopedics and Orthodontics: Printed Grids with Skeletal Anchorage. Appl. Sci. 2022, 12, 3820. [CrossRef]
- Francisco, I.; Ribeiro, M.P.; Marques, F.; Travassos, R.; Nunes, C.; Pereira, F.; Caramelo, F.; Paula, A.B.; Vale, F. Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art. Biomimetics 2022, 7, 23. [CrossRef]
- Su T, Zhang H, Kang T, Zhou M, Han J, Ning N, Lin H, Chen X, Chen Q. Application progress of three-dimensional printing technology in orthodontics. Digit Med 2022;8:31. [CrossRef]
- Revilla-León M, Meyer MJ, Özcan M. Metal additive manufacturing technologies: literature review of current status and prosthodontic applications. Int J Comput Dent. 2019;22(1):55-67. PMID: 30848255.
- Bartkowiak T, Walkowiak-Śliziuk A. 3D printing technology in orthodontics – review of current applications. Journal of Stomatology. 2018;71(4):356-364. doi:10.5114/jos.2018.83410. [CrossRef]
- Tsolakis, I.A.; Gizani, S.; Tsolakis, A.I.; Panayi, N. ThreeDimensional-Printed Customized Orthodontic and Pedodontic Grids: A Critical Review of a New Era for Treatment. Children 2022, 9, 1107. [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [CrossRef]
- Graf S, Tarraf NE, Kravitz ND. Three-dimensional metalprinted orthodontic laboratory grids. Semin Orthod. 2021; 27:189–93.
- Graf S. Direct printed metal devices - the next level of computer-aided design and computer-aided manufacturing applications in the orthodontic care. APOS Trends Orthod2017; 7:253–259. [CrossRef]
- Graf, S.; Cornelis, M.A.; Hauber Gameiro, G.; Cattaneo, P.M. Computer-aided design and manufacture of hyrax devices: Can we really go digital? Am. J. Orthod. Dentofac. Orthop. 2017, 152, 870–874. [CrossRef]
- Scribante, A.; Gallo, S.; Pascadopoli, M.; Canzi, P.; Marconi, S.; Montasser, M.A.; Bressani, D.; Gandini, P.; Sfondrini, M.F. Properties of CAD/CAM 3D Printing Dental Materials and Their Clinical Applications in Orthodontics: Where Are We Now? Appl. Sci. 2022, 12, 551. [CrossRef]
- Ahmed N, Shetty SK, Urukalan H, Nikhil P M, Younus A, Bhat RKR. Thinking forward: 3-D printing in orthodontics. IP Indian J Orthod Dentofacial Res 2021;7(3):208-215. [CrossRef]
- Zinelis S, Polychronis G, Papadopoulos F, Kokkinos C, Economou A, Panayi N, Papageorgiou SN, Eliades T. Mechanical and electrochemical characterization of 3D printed orthodontic metallic grids after in vivo ageing. Dent Mater. 2022 Nov;38(11):1721-1727. Epub 2022 Sep 16. PMID: 36123188. [CrossRef]
- Eliaz N. Corrosion of metallic biomaterials: a review.Materials 2019:12. [CrossRef]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials 2023, 16, 2166. [CrossRef]
- Cunha TMAD, Barbosa IDS, Palma KK. Orthodontic digital workflow: devices and clinical applications. Dental Press J Orthod. 2021 Dec 15; 26(6):e21spe6. PMID: 34932716; PMCID: PMC8690351. [CrossRef]
- Shannon, T.; Groth, C. Be your own manufacturer: 3D printing intraoral grids. Semin. Orthod. 2021, 27, 184–188. [CrossRef]
- Petrunov V., M. Chalyovski. CAD/CAM retainers – a new era in fixed retention. Digital working protocol for retainer fabrication. Orthod. Review. 2022; 24(2): 8-19.
- Kuang, Y.; Hu, B.; Feng, G.; Huang, L.; Song, J. The Application of a 3-Dimensional Printing Technique in Refining the Orthodontic Trans-Palatal Arch. Appl. Sci. 2022, 12, 7497. [CrossRef]
- Kuang, Y.; Wang, C.; Hu, B.; Feng, G.; Wang, C.; Song, J. Biomechanical analysis of reinstating buccally flared maxillary 2nd molars using 3D printing anchorage supports: A 3D finite element study. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 1085–1096. [CrossRef]
- Barbin, T.; Velôso, D.V.; Del Rio Silva, L.; Borges, G.A.; Presotto, A.G.C.; Barão, V.A.R.; Mesquita, M.F. 3D metal printing in dentistry: An in vitro biomechanical comparative study of two additive manufacturing technologies for full-arch implantsupported prostheses. J. Mech. Behav. Biomed. Mater. 2020, 108, 103821. [CrossRef]
- Grauer, D.; Wiechmann, D.; Heymann, G.C.; Swift, E.J., Jr. Computer-aided design/computer-aided manufacturing technology in customized orthodontic grids. J. Esthet. Restor. Dent. 2012, 24, 3–9. [CrossRef]
- Thurzo, A.; Koˇciš, F.; Novák, B.; Czako, L.; Varga, I. Three-Dimensional Modeling and 3D Printing of Biocompatible Orthodontic Power-Arm Design with Clinical Application. Appl. Sci. 2021, 11, 9693. [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [CrossRef]
- Harikrishnan S, Subramanian AK. 3D printing in orthodontics: A narrative review. J Int Oral Health 2023;15:15-27. [CrossRef]
- Cousley, R.R. Introducing 3D printing in your orthodontic practice. J. Orthod. 2020, 47, 265–. [CrossRef]
- Nathasha MM, Chakravarthi NCS, Srinivasan D, et al.. Orthodontics in the era of digital innovation – a review. J Evolution Med Dent Sci 2021;10(28): 2114-2121. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).