1. Introduction
Global sagittal balance is important for patient well-being. Previous studies have reported that spinal imbalance causes more muscle energy expenditure [
1] to maintain body balance and movement, resulting in pain, fatigue, and disability [
2,
3]. For this reason, accurate planning for global sagittal alignment correction is essential for spinal surgeons to achieve the best outcomes and improve patients’ quality of life [
4].
Other than structural spinal deformity, which causes global spinal imbalance, a patient’s functional adaptation can also affect global sagittal alignment [
5]. Lumbar canal stenosis, may compensate for the pain they feel by leaning forward or adopting a flexion posture. This has been proven to alleviate pain due to an increase in the spinal canal diameter [
10,
11]. From previous studies, spinal surgical procedures for treating spinal canal stenosis such as decompression alone[
12], discectomy[
6,
13], or short-segment fusion [
14] result in an improvement of sagittal spinal imbalance. However, to our knowledge, no study is yet to report the effect of Transforaminal Epidural Steroid Injection (TFESI) in sagittal spinal alignment.
TFESI is recognized as a conservative treatment in lumbar spinal stenosis to alleviate symptoms, [
15,
16] and as a diagnostic procedure [
17] to identify pathologic levels in complex cases. TFESI is commonly used as an initial procedure before considering surgical management and this study aims to evaluate the short-term spinal sagittal alignment change after TFESI.
2. Materials and Methods
This study was approved by the Human Ethics Committee of Thammasat University (MTU-EC-OT-6-105/63), and all patients provided written informed consent. We retrospectively reviewed cases from electronic medical records and radiographs of lumbar spinal stenosis patients aged between 18 to 85 years old at Thammasat University Hospital who underwent Transforaminal Epidural Steroids Injections from January 2017 to January 2020. The inclusion criteria were patients who have a history of clinical radiculopathy from spinal stenosis and lumbar disc herniation with complete pre-intervention and post-intervention data records. The exclusion criteria were spinal infection, clinical progressive neurologic deficit, symptoms of cauda equina or conus medullaris syndrome, history of spinal surgery, ankylosing spondylitis, active hip disease, and history of other conditions that can mimic spine pathology (such as urologic, gynecologic, or great vessel disease).
Demographic data were collected from the electronic medical records including age, sex, and the vertebra level injected. Clinical outcomes were recorded pre-intervention and two weeks after intervention. Visual analog scale (VAS) and Oswestry Disability Index (ODI) in Thai version [
18] were collected.
Radiological measurement
Whole spine anteroposterior (AP) and lateral standing radiographs were taken before intervention (Pre-intervention) and two weeks after intervention (Post-intervention) by using 36-inch-full-length films. To standardize the imaging process, all patients were instructed to stand in a comfortable position with full hip and knee extension, and with the elbow flexed at 45
o [
19].
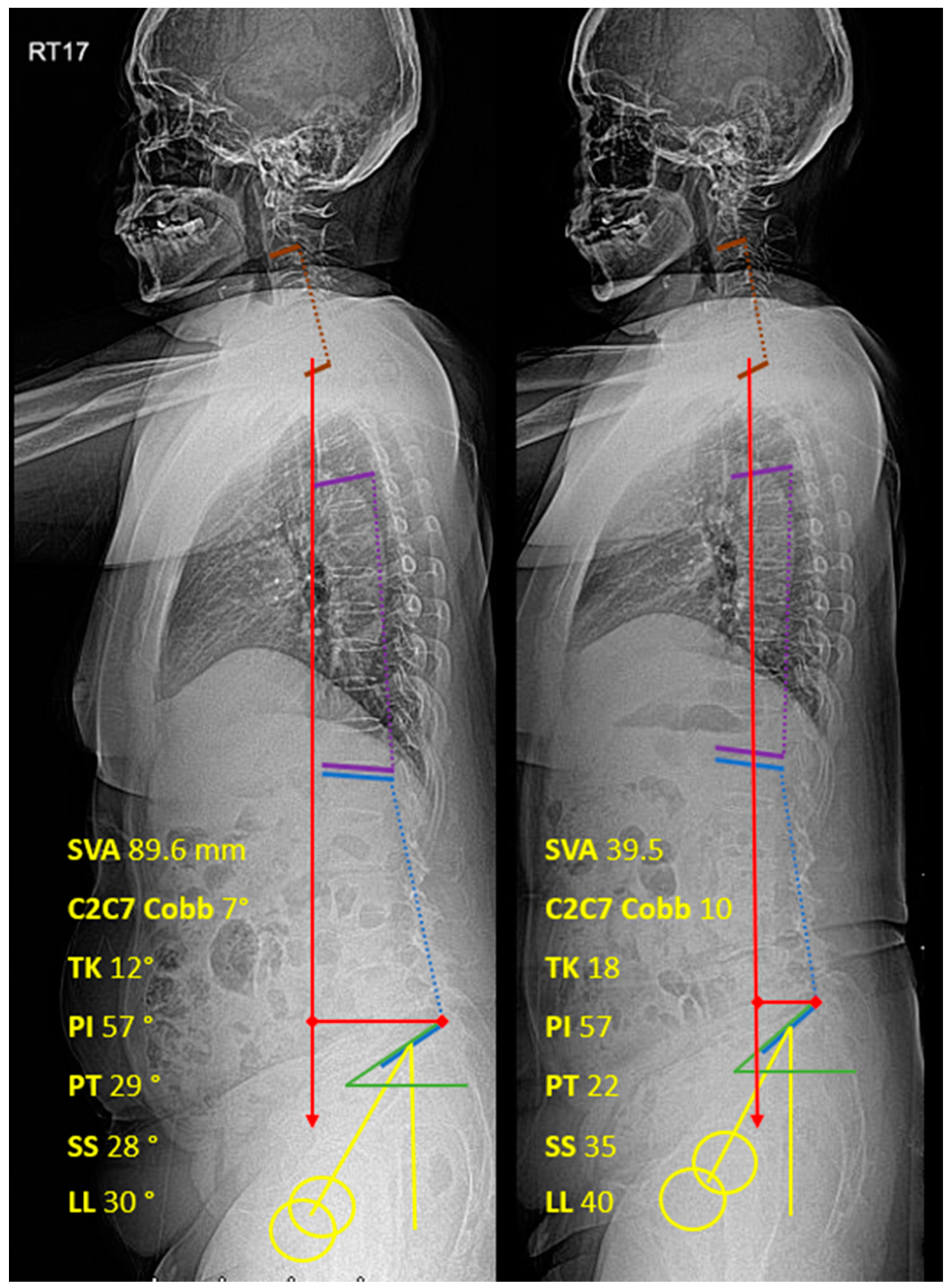
Two spine surgeons independently performed digital radiograph interpretations. The patients’ data and identifications were blinded to the evaluators. The sagittal parameters were measured by PACS (SYNAPSE, Fujifilm’s) measurement tools on the 27-inch monitor. Sagittal Vertical Axis (SVA), Thoracic Kyphosis (TK), Lumbar Lordosis (LL), Pelvic Incidence (PI), Pelvic Tilt (PT), Sacral Slope (SS), and PI-LL (PI minus LL) were measured according to the Scoliosis Research Society-Schwab classification[
1]. C2C7 Cobb was measured from the angle between C2 and C7 lower endplate [
20] (
Figure 1).
Intervention
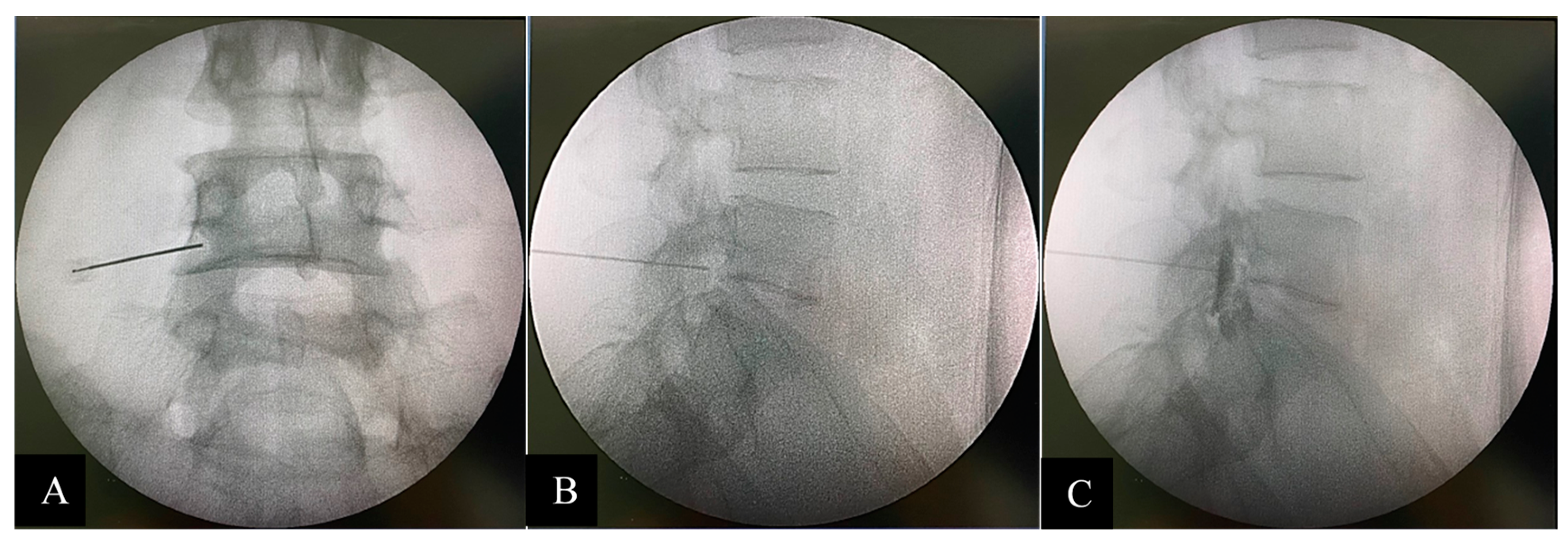
TFESI was performed with triamcinolone acetonide 40mg/1cc (40 mg for one-level injection and 80 mg for 2 to 4 levels injections) and normal saline mixed up to 2 cc for each injection point. In addition, Iohexol (Omipaque 300 Contrast) 0.5-1 cc was administered as a contrast media to confirm the position prior to steroid injection under biplanar (AP and lateral) fluoroscopic guidance (C-arm Fluoroscope, Philips BV Pulsera). Quincke spinal needles size 23 gauge 9 cm were used and they were angled towards the safe triangle [
21,
22] in the AP view and towards the middle of the neural foramen in the lateral view (
Figure 2).
Statistical Analysis
Percentages were used for categorical data. Mean and standard deviation were used for continuous data after the normality assumption was validated, and paired t-test was used in the analysis. Characteristics of the data between groups were analyzed by analysis of variance (ANOVA). The correlation of the data was measured using Pearson correlation coefficients. An r value of more than 0.3 or less than -0.3 confirmed a statistical correlation [
23], and a P value of less than 0.05 indicated a statistical significance. Interobserver reliability testing was done using the Intraclass Correlation Coefficient (ICC). All statistical calculations were performed on IBM SPSS Statistic version 25.0 (IBM Corporation, Armonk, NY).
3. Results
We retrospectively reviewed 120 individual cases with 99 patients. Twenty-one males (21.2%) and 78 females (78.8%) underwent TFESI and were included in the study. The average age was 64.3 ± 9.2 years. The average number of vertebrae level injected was 1.8 ± 0.8 levels.
Pre-intervention and Post-intervention Outcomes
Both VAS and ODI outcomes were statistically improved after the intervention: VAS decreased from 8.31 ± 1.11 to 3.38 ± 1.47 and ODI decreased from 31.06 ± 3.48 to 18.03 ± 4.17. All sagittal parameters were statistically significantly improved. SVA, PT, and lumbopelvic mismatch were significantly decreased, while C2C7 Cobb, TK, SS, and LL were significantly increased after the intervention. Post-intervention SVA showed an improvement of 29.81% (52.76 ± 52.22 mm to 37.03 ± 41.07 mm). Pelvic Incidence (PI) was not statistically affected by TFESI. All data are shown in
Table 1.
Difference between the number of injection levels and sagittal parameters
The collected data were divided according to the total number vertebrae levels injected: 1 level, 2 levels, 3 levels, and 4 levels. The differences in outcomes and sagittal parameters in each group were assessed. The variations of VAS score and ODI among the different numbers of injection levels were not statistically significant both before and after the intervention. The C2C7 Cobb and TK were found to not be statistically significant between each number of injection levels. The sagittal parameters, including SVA, PT, and PI-LL mismatch, were statistically significantly higher in multiple-level injection groups compared to single-level injection groups, both before and after the intervention. In contrast, SS and LL were statistically significantly lower in multiple-level injection groups compared to single-level injection groups both before and after the intervention. All data are shown in
Table 2.
Correlation between sagittal parameters
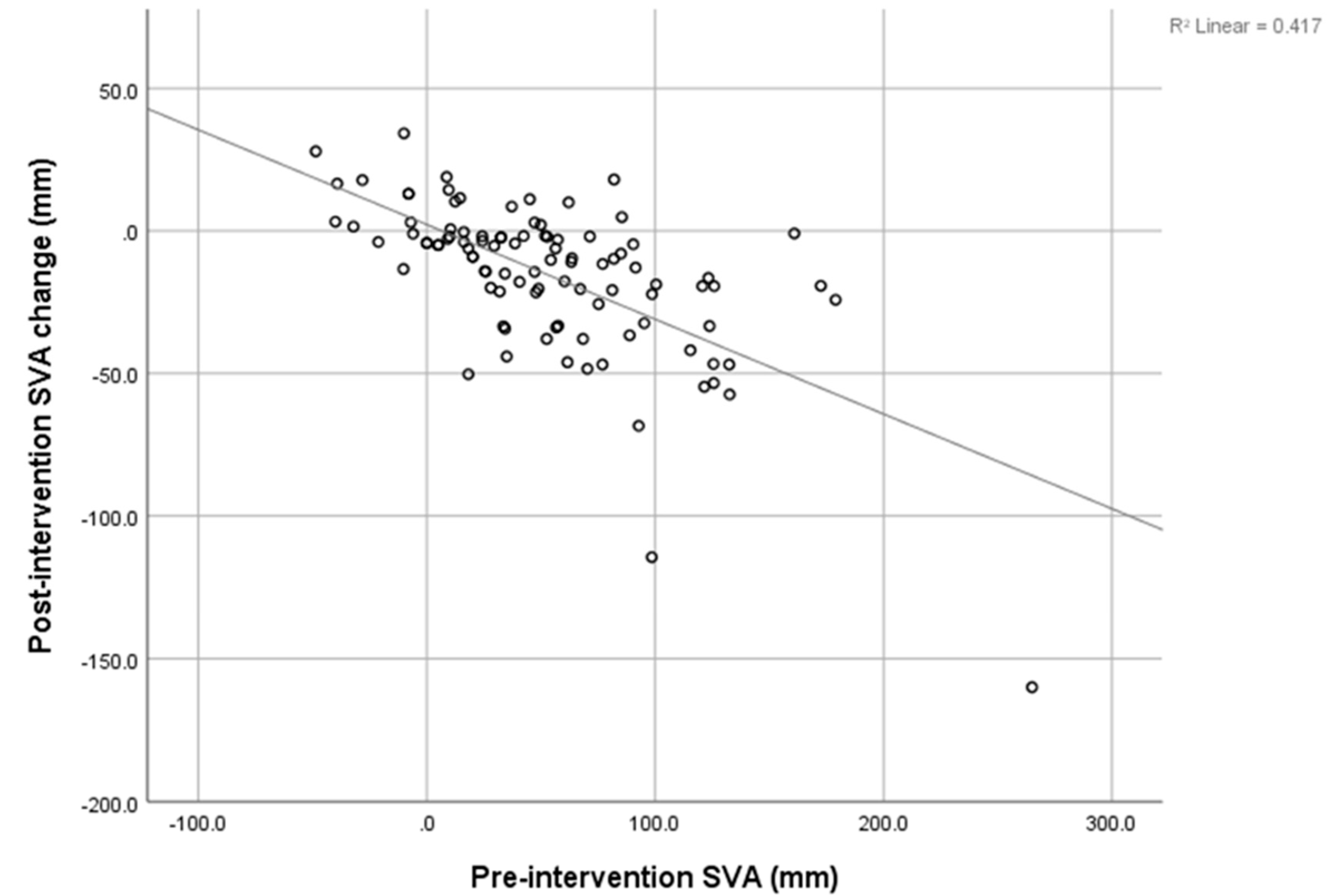
There was a strong negative correlation between the pre-intervention SVA and post-intervention SVA decrement (r = -0.646), shown in
Figure 3. The pre-intervention LL showed a negative correlation with the post-intervention LL increment, shown in
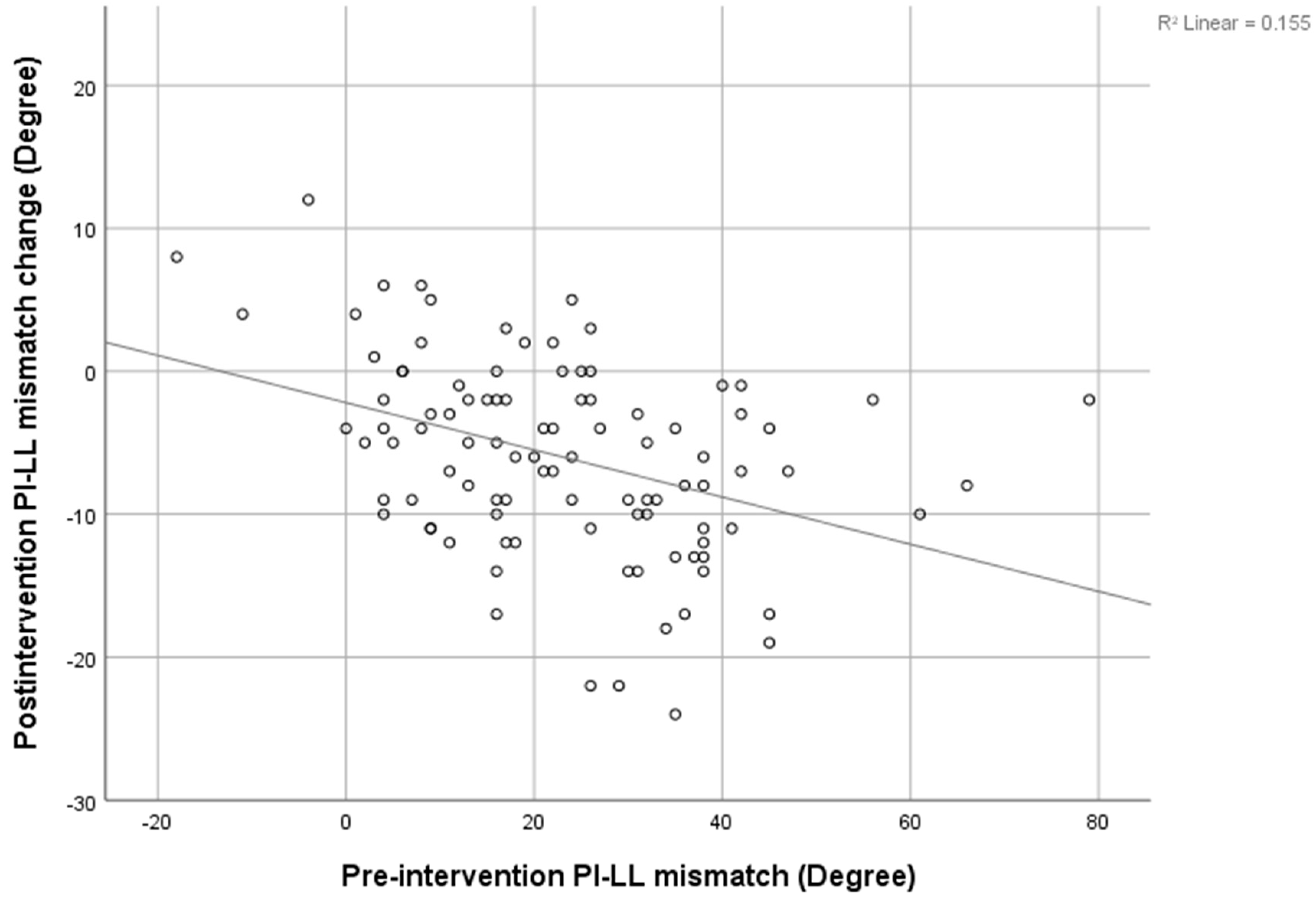
Figure 4 (r = -0.4). The pre-intervention PI-LL mismatch exhibited a negative correlation with the post-intervention PI-LL decrement (r = -0.394), shown in
Figure 5. The significant correlation between pre-intervention parameters and post-intervention changes are shown in
Table 3.
Interobserver Reliability
Interobserver reliability was calculated using the Intraclass Correlation Coefficient. The results were greater than 0.9 in all sagittal parameters. Thus, it was considered that the measurements were valid and achieved excellent reliability.
4. Discussion
In our study, we collected data from patients with lumbar spinal stenosis who received TFESI. The results showed that both the VAS and the ODI improved significantly after the intervention. Ghahreman A. [
24], Kabatas S. [
25], and McCormick Z. [
26] studied the short-term effects of TFESI, which significantly improved VAS and ODI in a similar study. This could support the treatment of pain using TFESI's for short-term efficacy in lumbar spinal stenosis.
Liang C. [
13] conducted a study on lumbar disc herniation and found a significant immediate improvement of all sagittal imbalance parameters on day 1 post-operation, and this improvement continued for three months before the parameters became close to their normal ranges. SVA improved from 11.6 ± 6.6 cm to 2.9 ± 6.1 cm, and three months post-operation LL improved from 25.3° ± 14.0° to 42.4° ± 10.2°. Moreover, Fujii K12 retrospectively reviewed lumbar decompression without fusion in lumbar spinal stenosis and concluded that the SVA, TK, PT, LL, and PI-LL mismatch improved post-operatively. SVA was decreased from 49.1° ± 38.6° to 28.6° ± 30.7°, and LL was changed from 38° ± 13° to 44° ± 11°. A strong correlation was found between pre-op SVA/PI-LL and post-op SVA/PI-LL decrement post-operatively. Likewise, Salimi H et al [
27] also reported that minimal invasive lumbar decompression surgery could convert sagittal malalignment to normal alignment in 2 years and 5 years follow-up. The previous studies mentioned above indicated that spinal decompressive procedures without instrumentation have the ability to improve sagittal spinal parameters. Therefore, we believe that spinal interventions that reduce radicular pain, such as TFESI, can partially improve sagittal spinal parameters because when radicular pain was improved, so compensated forward bending subsided.
This study may be the first study that has collected data on the non-operative management of lumbar spinal stenosis. The present procedure did not interfere with anatomical structure but decreased the inflammation process to neural structure and improve radicular pain. We found a significant change in SVA, C2C7 Cobb, TK, PT, SS, and LL after patients underwent TFESI. The SVA was improved by about 30% (from 52.76 ± 52.22 mm to 37.03 ± 41.07 mm) and PT and LL were improved by about 17% and 18% respectively. This is compared to 42%, 15%, and 16% improvements reported by Fujii K [
12]. Patients with multiple levels of stenosis tend to have significantly more severe positive SVA, higher PT, and lower LL and SS. Furthermore, we found a strong negative correlation between pre-intervention SVA and post-intervention SVA decrement. This indicates that the more positive imbalanced patients were, the greater the resulting improvement in the SVA. This correlation has also been found in recent studies [
12,
13,
28]. Similarly, a strong negative correlation between pre-intervention PI-LL and post-intervention PI-LL was found. The greater the PI-LL mismatch, the larger the PI-LL improvement may be predicted to be. In contrast, the Pre-intervention LL was negatively correlated with the post-intervention LL increment, and this means that in a small degree of Pre-intervention LL patients there may be more improvement in the post-intervention LL.
From a review of previous literature, it can be observed that many spinal pathologies caused a sagittal imbalance, reduced muscle strength [
7,
13,
29], adjacent disc degeneration [
30], disc herniation [
6], and spinal stenosis. Several authors have proposed that spinal stenosis patients have limited lumbar lordosis (LL) [
5] due to the decreased pressure of the epidural venous plexus when bending forward. Furthermore, compensatory lumbar flexion posture lowers epidural pressure, hence, reducing pain and neurogenic claudication [
6,
7,
8,
9]. The anatomical study showed that flexion for the lumbar spine increased spinal canal diameters [
10,
11]. We hypothesized that in global sagittal imbalance patients, there might be two factors that are involved in the imbalance. The first one is a structural imbalance, and the second one is the "functional compensation” of patients to radicular pain. We believe that after undergoing TFESI and the pain becoming less severe, compensation of lumbar flexion may be diminished. In this study, after TSESI, we found that SVA, PT, and LL were significantly improved. Recently, there has been little focus on the functional compensation of sagittal alignment before spinal surgical correction. We believe that it is better to evaluate the spinal surgical balance when the clinical pain of patients is subsiding rather than when the pain remains severe.
Our most recent concern with this main issue was that we were uncertain whether we had to correct the deformity if a global sagittal imbalance existed in the surgical treatment of degenerative lumbar spinal stenosis. This study found that a considerable number of patients' global sagittal alignment significantly improved following TFESI. For this reason, in patients with degenerative lumbar spinal stenosis and global sagittal imbalance, reassessing global sagittal alignment after TFESI might show more accurate structural global sagittal imbalance. We advise obtaining whole-spine AP and lateral standing radiographs again after patients begin improving in terms of pain following on from TFESI.
This study has some limitations. First, this is a retrospective review of the database, so a recall bias and selection bias may be present. Second, this radiographic study focuses on sagittal alignment, but the dynamic compensation of lower limbs, such as hip and knee flexion, is not investigated. It should be noted that we instructed all patients who received the whole spine film to extend their hip and knee before imaging [
31]. Third, due to the short-term effect of TFESI, the outcome and sagittal parameter data were collected only at a short-term follow-up. We suggest a long-term follow-up in future studies.
5. Conclusions
Transforaminal Epidural Steroid Injection (TFESI) can improve SVA, C2C7 Cobb, TK, PT, SS, and LL parameters as well as VAS and ODI in a short-term follow-up study. This could be the choice of treatment to improve quality of life factors in terms of pain and disability in sagittal malalignment patients’ who have contraindications or deny surgery. This could also be effective in correcting functional compensation to evaluate sagittal alignment correction before surgery to avoid postoperative overcorrection alignment.
Funding
This research received no external funding.
Institutional Review Board Statement
Human Ethics Committee of Thammasat University (MTU-EC-OT-6-105/63)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Iyer S, Sheha E, Fu MC, et al. Sagittal Spinal Alignment in Adult Spinal Deformity: An Overview of Current Concepts and a Critical Analysis Review. JBJS Rev. May 2018;6(5):e2. [CrossRef]
- Harroud A, Labelle H, Joncas J, Mac-Thiong JM. Global sagittal alignment and health-related quality of life in lumbosacral spondylolisthesis. Eur Spine J. Apr 2013;22(4):849-56. [CrossRef]
- Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). Aug 1 2009;34(17):1828-33. [CrossRef]
- Yeh KT, Lee RP, Chen IH, et al. Correlation of Functional Outcomes and Sagittal Alignment After Long Instrumented Fusion for Degenerative Thoracolumbar Spinal Disease. Spine (Phila Pa 1976). Oct 1 2018;43(19):1355-1362. [CrossRef]
- Pourtaheri S, Sharma A, Savage J, et al. Pelvic retroversion: a compensatory mechanism for lumbar stenosis. J Neurosurg Spine. Aug 2017;27(2):137-144. [CrossRef]
- Endo K, Suzuki H, Tanaka H, Kang Y, Yamamoto K. Sagittal spinal alignment in patients with lumbar disc herniation. Eur Spine J. Mar 2010;19(3):435-8. [CrossRef]
- Enomoto M, Ukegawa D, Sakaki K, et al. Increase in paravertebral muscle activity in lumbar kyphosis patients by surface electromyography compared with lumbar spinal canal stenosis patients and healthy volunteers. J Spinal Disord Tech. Aug 2012;25(6):E167-73. [CrossRef]
- Lee JH, Kim KT, Suk KS, et al. Analysis of spinopelvic parameters in lumbar degenerative kyphosis: correlation with spinal stenosis and spondylolisthesis. Spine (Phila Pa 1976). Nov 15 2010;35(24):E1386-91. [CrossRef]
- Suzuki H, Endo K, Kobayashi H, Tanaka H, Yamamoto K. Total sagittal spinal alignment in patients with lumbar canal stenosis accompanied by intermittent claudication. Spine (Phila Pa 1976). Apr 20 2010;35(9):E344-6. [CrossRef]
- Schonstrom N, Lindahl S, Willen J, Hansson T. Dynamic changes in the dimensions of the lumbar spinal canal: an experimental study in vitro. J Orthop Res. 1989;7(1):115-21. [CrossRef]
- Miao J, Wang S, Park WM, et al. Segmental spinal canal volume in patients with degenerative spondylolisthesis. Spine J. Jun 2013;13(6):706-12. [CrossRef]
- Fujii K, Kawamura N, Ikegami M, Niitsuma G, Kunogi J. Radiological improvements in global sagittal alignment after lumbar decompression without fusion. Spine (Phila Pa 1976). May 15 2015;40(10):703-9. [CrossRef]
- Liang C, Sun J, Cui X, Jiang Z, Zhang W, Li T. Spinal sagittal imbalance in patients with lumbar disc herniation: its spinopelvic characteristics, strength changes of the spinal musculature and natural history after lumbar discectomy. BMC Musculoskelet Disord. Jul 22 2016;17:305. [CrossRef]
- Kim CH, Chung CK, Park SB, Yang SH, Kim JH. A Change in Lumbar Sagittal Alignment After Single-level Anterior Lumbar Interbody Fusion for Lumbar Degenerative Spondylolisthesis With Normal Sagittal Balance. Clin Spine Surg. Aug 2017;30(7):291-296. [CrossRef]
- Manchikanti L, Kaye AD, Manchikanti K, Boswell M, Pampati V, Hirsch J. Efficacy of epidural injections in the treatment of lumbar central spinal stenosis: a systematic review. Anesth Pain Med. Feb 2015;5(1):e23139. [CrossRef]
- Davis N, Hourigan P, Clarke A. Transforaminal epidural steroid injection in lumbar spinal stenosis: an observational study with two-year follow-up. Br J Neurosurg. Apr 2017;31(2):205-208. [CrossRef]
- Bartleson JD, Maus TP. Diagnostic and therapeutic spinal interventions: Epidural injections. Neurol Clin Pract. Aug 2014;4(4):347-352. [CrossRef]
- Sanjaroensuttikul N. The Oswestry low back pain disability questionnaire (version 1.0) Thai version. J Med Assoc Thai. Jul 2007;90(7):1417-22.
- Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976). Jun 2011;36(13):1037-45. [CrossRef]
- Alijani B, Rasoulian J. The Sagittal Balance of the Cervical Spine: Radiographic Analysis of Interdependence between the Occipitocervical and Spinopelvic Alignment. Asian Spine J. Jan 30 2020;doi:10.31616/asj.2019.0165.
- Lee IS, Kim SH, Lee JW, et al. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. Feb 2007;28(2):204-8.
- Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. Nov 1998;79(11):1362-6.
- Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. Sep 2012;24(3):69-71.
- Ghahreman A, Ferch R, Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. Aug 2010;11(8):1149-68. [CrossRef]
- Kabatas S, Cansever T, Yilmaz C, et al. Transforaminal epidural steroid injection via a preganglionic approach for lumbar spinal stenosis and lumbar discogenic pain with radiculopathy. Neurol India. Mar-Apr 2010;58(2):248-52. [CrossRef]
- McCormick Z, Kennedy DJ, Garvan C, et al. Comparison of Pain Score Reduction Using Triamcinolone vs. Betamethasone in Transforaminal Epidural Steroid Injections for Lumbosacral Radicular Pain. Am J Phys Med Rehabil. Dec 2015;94(12):1058-64. [CrossRef]
- Hamidullah Salimi HT, Kentaro Yamada, Hidetomi Terai, Masatoshi Hoshino. The effect of minimally invasive lumbar decompression surgery on sagittal spinopelvic alignment in patients with lumbar spinal stenosis: a 5-year follow-up study. J Neurosurg Spine. 2021;doi:10.3171/2020.11.SPINE201552.
- Cho JH, Joo YS, Lim C, Hwang CJ, Lee DH, Lee CS. Effect of one- or two-level posterior lumbar interbody fusion on global sagittal balance. Spine J. Dec 2017;17(12):1794-1802. [CrossRef]
- Mitsuhiro Masaki TI, Ko Yanase, Xiang Ji, Jun Umehara, Junichi Aoyama. Association of Pain History and Current Pain With Sagittal Spinal Alignment and Muscle Stiffness and Muscle Mass of the Back Muscles in Middle-aged and Elderly Women. Clin Spine Surg. 2019;32.
- Makhni MC, Shillingford JN, Laratta JL, Hyun SJ, Kim YJ. Restoration of Sagittal Balance in Spinal Deformity Surgery. J Korean Neurosurg Soc. Mar 2018;61(2):167-179. [CrossRef]
- Lafage V, Smith JS, Bess S, et al. Sagittal spino-pelvic alignment failures following three column thoracic osteotomy for adult spinal deformity. Eur Spine J. Apr 2012;21(4):698-704. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).