1. Introduction
Global warming is the most serious challenge humanity has ever faced. The global temperature trend points to reach two degrees above that during the pre-Industrial Revolution, changing the conditions of the planet, which has not been seen over the last 3 million years (Folke et al., 2021), and cancelling the habitability range in which Homo sapiens became sedentary and thrived. Crucially, a number of tipping points that mark the path of no return might reinforce humanity’s trajectory farther away from critical resources (Lenton et al., 2023), including buffering negative interspecies interactions.
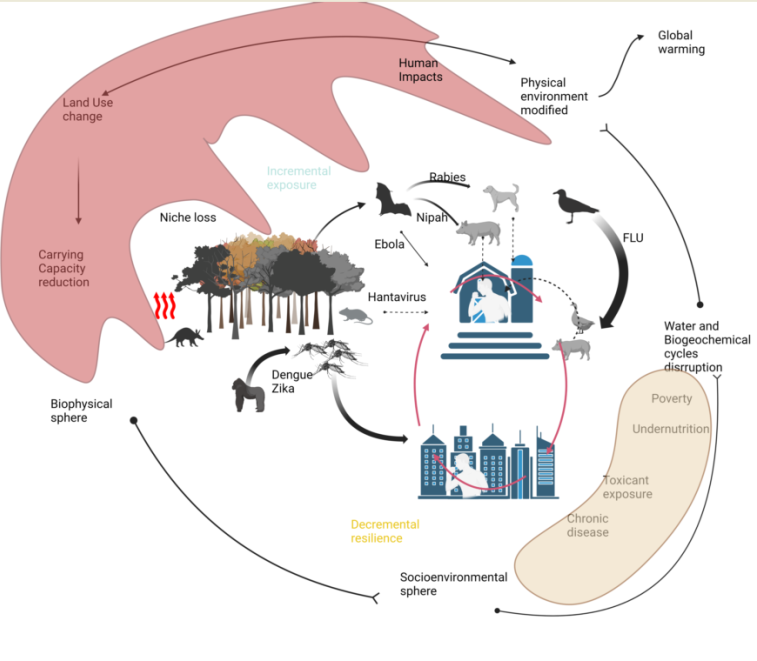
Changes in the systems that sustain the planet, of the magnitude we see today, can clearly modify the epidemiology of chronic but also acute, degenerative and infectious diseases. Currently, we estimate in absolute terms that approximately 60% of infectious diseases cause increased damage to the population, known as the disease burden. This is due to increased and more effective contact due to host susceptibility and fueled by socioenvironmental conditions (Mora et al., 2022).
2. Brink of the emergency in the socioenvironmental interphase
Among the environmental changes that most contribute to the transmission of infectious diseases is the proliferation of reservoirs through changes in land use, which occurs due to the fragmentation and degradation of habitats which causes a greater density of vectors and/or intermediate hosts and ultimately favors contact with humans or domesticated animals. Evolution in a different immunity context, upon contact with humans, may result in the emergence of zoonotic pathogens (Vora, 2008).
At the risk of oversimplifying, in the construction of the margin, there is a framework of sociodemographic and economic variables that affect both the human host and pathogen. If large segments of the population are confronted with a lack of even minimal resources for a healthy and productive life, they may face the alternative of deciding to migrate and frequently occupy poorly adapted areas where microorganism transmission is more likely. In parallel, there is a downward trend in species, mostly in tropical regions (Finn et al., 2023), and mammals that are expelled by human impacts may be displaced from their fundamental climatic niche (Pineda-Munoz et al., 2021); hence, small and increasing numbers of these may intersect with humans in altered habitats. In addition to overcrowding, an economic consequence of overpopulation and degraded lifestyle conditions, a time bomb is set when the economic power of humans converges with cultural factors, such as consumption of food in wet markets, which facilitates the jump of the species barrier by mutated viruses within society strata with poor health.
Moreover, the aging of the population—a demographic event typical of the epidemiological transition—is often accompanied by frailty. Similar to any other high-risk inflammatory condition, such as diabetes mellitus, cardiovascular disease, and dementia, an adequate response in many communities is lacking. The deterioration that accompanies malnutrition and noncommunicable diseases originating from exposure to environmental contaminants, such as atmospheric ultrafine particles, increases the mass of individuals who are susceptible to, and on occasion spread, infectious and contagious diseases, even more so if pollution particles cause inflammation, as much as these particles carry virulent microorganisms (Nor et al., 2021).
Thus, many emerging and reemerging diseases, including neglected tropical diseases, are actually ecosyndemic. That is, their genesis involves the environment physically accelerating dispersion or enhancing virulence adaptation strategies across vulnerable populations. Vibrio and increasing ocean temperature anomalies (Von Schuckmann et al., 2020) are an example. Climate-stressed bacteria acquire a virulent phenotype in high-temperature and hypoxemic conditions in coastal fishing zones; however, after exposure, a disease outbreak occurs only when contact with vulnerable individuals (people of advanced age or with hepatic diseases) is made, as in the case of vibriosis (Vezzulli et al., 2020).
If exceeding a median global temperature of 1.5 °C is unavoidable, then before a greater frequency of extreme meteorological events associated with global warming and epidemics occur in the near future, it is key to shore up the adaptation ability and resilience of individuals and communities and even mitigate inequities and vulnerability. A crude lesson from the last three years of the COVID-19 pandemic was that political will did not translate immediately into straightforward, clear information, access to preventative measures, or opportune vaccines or treatment for deprived communities worldwide, which explains in part the excessive death toll in low- and middle-income countries (Walker et al., 2020). This trend represents the lowest point with regard to the ideal of justice (Thomas et al., 2019). From this, we suggest putting into focus the vulnerability and inequity that fracture societies to understand how the environmental effects of climate change reinforce and contribute to disease.
3. Scale out to understand the complexity of the challenge
Worldwide health insecurity prevails, despite decades of efforts to improve health indicators. In 2017, the UNEP estimated that 821 million people were undernourished due to environmental degradation, drought and biodiversity loss (UNDP, 2023). The food system remains unfair, and the proportion of the population that cannot afford a healthy diet with 52% of their income represents a quarter to 75% of inhabitants in some middle-income countries (Fanzo & Miachon, 2023). Whereas urbanization enhances economic output, it also acts as a sink for resources and might increase air pollution exposure for urbanites and other risks, such as low-nutrient, energy-dense, and protein- and fat-rich diets that promote diabetes and cardiovascular disease.
In the network of events that lead to the reemergence of diseases and/or the emergence of a new pathogen in formerly biodiverse enclaves, social and economic factors in distant areas take preeminence when any of these two phenomena is usually preceded by environmental changes in land use, followed by r-strategist selection (Pianka, 1970) and animal/human spheres getting closer and overlapping with each other. For example, exploitative deforestation leads to the introduction of agriculture and later cattle, which increase the external or environmental costs borne by local communities. By favoring a few wild species that proliferate in altered environments, the probability of zoonotic transmission is increased. In the case of the Ebola epidemic in 2014, the introduction of the virus may have occurred from the consumption of hunted meat, in particular of fruit bats that are attracted by crops and whose meat is eaten semi-raw (Rewar & Mirdha, 2014).
In a short time, the Ebola virus spread, transmitted first among women in families, who were in charge of preparing the bodies of the deceased, which was a risk factor. Additionally, an important aspect of vulnerability came from environmental changes in the local context, which explains why preparing bodies was not viewed as dangerous at first, despite the virus being transmitted by contact with body fluids.
In the climate change context, heat, drought, and conflict erode the resilience of food production systems worldwide, and the most vulnerable are pastoralists in low- and middle-income countries, where little or no support is given (Ahmad & Afzal, 2021). This trend, in addition to aggravating access to animal protein, enhances the consumption of bush meat and subsequent exposure to emerging/reemerging zoonoses.
A number of transmissible diseases and viruses have emerged in recent decades, including HIV, Ebola, Nipah virus, influenza H1N1, Chikungunya, Zika, SARS, MERS, SARS-CoV-2, and mpox, via clear interaction between microbial traits and human epidemiology (Guth et al., 2022), which through the last 25 years has been tied to intensive production systems and international product mobility with the aim of reducing monetary costs. Recognizably, whereas the HACCP ensures some level of protection, the system is far from perfect and not designed to substitute prime ecological services. In this respect, hepatitis E virus endemicity in countries such as India and Mexico occurs probably due to the concurrence of sanitation deficiencies and insufficient pork or boar safety assessments (Cooper et al., 2005).
Following the same line of thought, once viruses with an RNA genome, which are more adept at mutating, jump to farm animals, there are various possible paths depending on how the exposure is managed, if it is, and/or diagnosed and treated. This and further layers of inequity may come from preexisting health conditions, which are also disparately mediated by race, sex, age, geography, etc. (Williams, 2021).
If we consider prototypical examples in which the pathogen clearly benefits from the uniform base that industrial production provides, such as Escherichia coli, which is resistant to antimicrobials and transmitted through chicken consumption, in low-income countries, we find that it is probably associated with other means of transmission and causes a greater disease burden in a context other than acute infection, that is, it plays a role in undernutrition and environmental enteric dysfunction (Arredondo-Hernandez et al., 2022) and the dissemination of antimicrobial resistance. Globally and within Europe, there are statistically significant differences in antimicrobial resistance and GDP, and some other World Bank indicators supporting environmental and human issues require further consideration along one health paradigm (Alvarez-Uria et al., 2016; Collignon et al., 2018).
In a climate characterized by an average temperature of 1.5 °C and with a greater number of hot days and droughts, it is generally anticipated that bacteria of the genus Salmonella could multiply in the environment and increase the cases of dysentery transmitted through foods and contaminated water. An increase in the number of infections that do not respond to antimicrobial treatment is also foreseen and can frequently occur outside the peak of incidence and with association with other climatic variables, which has been seen with the introduction of a Salmonella different from the usual type from the environment (Wang et al., 2022).
5. A warming world in displacement
Temperature is probably the most critical environmental variable; in the end, the state of water accumulation depends on it. It is the motor that moves the hydrological cycle and, in this sense, determines humidity and therefore the distribution of biomes on the earth. To different degrees and depending on the context, temperature influences the chemical medium of aquatic environments, not only concentrating or diluting salts but also because at greater temperatures, the dissolution of oxygen falls and the metabolic expense increases.
From an evolutionary view of life on the planet, we associate temperature with activity and find its footprint in the functioning of mitochondria and metabolic ability (Koch et al., 2021). With exceptions, this translates into the spatial distribution of living beings around the globe within thermal layers.
There are multiple consequences of this segregation due to temperature, but interestingly, the area of distribution of hosts and vectors can be displaced to higher latitudes in the Northern Hemisphere and to higher altitudes in mountain ranges and places that are inhabited but immunologically virgin due to the climate conditions that have been maintained, such as, for example, the reproduction of the Aedes mosquito, an efficient vector for the dengue and Zika viruses. As expected, they have increased activity, despite other environmental factors such as predators, competitors or a too-dry environment, which do not disturb the life cycle of the vector (Semenza et al., 2022).
Based on environmental variables, it is projected that in a world that is 2.0 °C hotter, by 2100 or sooner, bat hosts of sarbecoviruses may shift to Myanmar, Laos, Vietnam, Cambodia and India, countries that account for the highest number of suitable hosts (Muylaert et al., 2022). In some of these countries, population growth and economic development have resulted in greater deforestation (Michinaka et al., 2020) and land use changes, whereas among the remaining wild life, the prevalence of coronavirus increases directly because of human impact (Warmuth et al., 2023).
6. A warming world and asymmetric settlement: When migration causes diseases
Those that pay the price of externalities are those most dependent on environmental conditions and, therefore, sensitive to changes in the state of nature. In the case of the loss of biodiversity associated with the fragmentation of habitats, it is those who live in degraded regions—urban and semiurban—that are exposed to rodents that become carriers or efficient vehicles for the transmission of pathogens (Tian et al., 2018).
This is a reality that intersects with the global tendency toward unplanned, irregular urban growth of marginal areas, which occurs together with the assimilation of rural migrants. The high population density in flood plains causes the occupation of these regions to be unsafe, above all in view of the expectation of a greater number of extreme precipitation events (Tabari, 2020) and the loss of water infiltration.
Poor hygienic conditions derived from overcrowding and poor access to potable water and drainage services play a relevant role in the transmission of “poverty diseases” or neglected tropical diseases, which, in fact, are diseases caused by pathogens whose transmission is sensitive to environmental changes; that is, they affect populations to a greater or lesser extent depending on the occurrence of environmental changes or inversion in adaptation and migratory compensation. In addition to the above, in marginalized urban areas subject to floods that also have open drains and/or a lack of adequate handling of solid waste, noxious fauna, such as rodents carrying Leptospira, seasonally spread the disease when the inhabitants of the margins are exposed by contact with overflowing water contaminated with the urine of rodents. This contributes to a higher burden of zoonotic diseases, whereas the increased frequency of floods associated with climate change threatens to exacerbate this situation (Costa et al., 2015).
In addition to this explosive urban growth, it is worrisome when irregularity is used as an argument to justify exposure when it is a problem of inequality. Prejudice not only obstructs the collection of data on the focus of risk—which alone is insufficient to mitigate the effects of droughts and floods—but also forms part of the problem when there is no intervention in social factors that give rise to risk (Tellman & Eakin, 2022). Thus, the lack of health and hygiene services makes detection and treatment difficult, even for known diseases such as tuberculosis. In addition to the identification of new phenomena such as the expansion of mobile genetic elements for antimicrobial resistance, improvements in the economic connectivity among members of a broader community and discussion from different perspectives and people with varied histories, plus the implementation of specific programs for urban improvement and relocation as necessary would result in avoiding the greater part of the dangers (Streule et al., 2020).
7. A warming world: Vulnerability and broken barriers
A second consideration, upon estimating the vulnerability associated with global warming, is the fact that higher temperatures and other factors associated with environmental degradation, such as malnutrition and exposure to contaminants, can affect the susceptibility of the host and the ability of the pathogens to cause disease (Frumkin & Haines, 2019).
In ectothermic animals such as fish, it has been demonstrated that an increase in temperature corresponding to the least adverse scenarios of climate change increases oxidative stress and produces osmoregulatory failures in the function of parasitism, reducing the viability of the populations (Dittmar et al., 2014).
In more complex beings capable of regulating their body temperature, such as humans and other endothermic animals, the effect of the increase in temperature may depend in part on acclimatization, without it being entirely clear what the degree of physiological tolerance is to exposure to high temperatures that are still under the critical threshold and concerning the possible accumulation of damage (CCH, 2022).
To date, it is suspected without being proven that there is limited renal damage due to temperature, even in asymptomatic people, that progresses to kidney failure (Johnson, 2017). If this is the case, the effects of temperature in some people can be ascribed to another series of environmental exposures—undernutrition, obesity, atmospheric contamination, tobacco smoke, alcohol, etc.—associated with a new form of marginalization, the lack of a functional microbiome and diseases with an inflammatory component (Ishaq et al., 2019).
It has been demonstrated that on the grounds of increasing levels of atmospheric carbon dioxide, the nutritious value of cultivars is lost in a varied proportion; however, for some varieties of rice, the main source of amino acids in low-income countries in Asia, there is a 20% decrease in protein and iron, almost 40% in vitamin B1, and up to 45% in B9 over the proportion of nitrogen vanished (Zhu et al., 2018). Although the Zn concentration in rice is reduced by only 15%, it is still and even more substantial in other grains, such as maize and wheat. Although relying on subestimated data, at least 138 million and 148 million people will face Zn and/or protein deficiency by 2050 (Myers et al., 2015), and by the end of this century, if the global temperature increases by 2.7 °C , one-third of the global population will be out of the human niche (Lenton et al., 2023). In addition, the current negative relationship between per capita CO2 and nutrient deficiency shows that the problem will grow at least three times faster in low- and middle-income countries than in high-income countries (Moore et al., 2020).
Regardless of their cause, nutrition disparities lie beneath an astonishing number of infections in nutrient-deficient children by preventing the development of balanced immunity, and they also account for a large share of chronic degenerative diseases associated with a Western diet (Arredondo-Hernandez et al., 2022), as well as with SARS-CoV-2 infection and COVID-19 severity. Zinc deficiency, which occurs on both sides of the alimentary spectrum, is clinically relevant, even if mild, because Zn is vital to regulatory T lymphocyte induction and tolerogenic function (Maywald et al., 2018). Moreover, zinc deficiency is also responsible for epigenetically shifting energetic metabolism, therefore preventing Th1 activation in the case of an acute infection. Interestingly, momentaneous Zn deprivation acts as a signal that induces a stronger activation; this overresponse is very likely imbalanced (Maywald et al., 2018); in chronically Zn-deficient individuals, this kind of response leads to an inefficient antiviral response, inflammatory damage, cytokine storm, and acute kidney injury, all of which characterize severe and critical COVID-19 cases (Wessels et al., 2022).
8. Conclusions
Whereas global warming has already threatened advances in global health (Organization, 2023), we discussed the margins, exterior limit of the circuit of access to the components necessary for a healthy life, and how under the deterioration of socioenvironmental conditions—foreseeable under the scenarios of climate change—a growing number of people are outside the confines of safety, in a multidimensional space that favors the evolution and selection of variants to the margin; for example, in the case of SARS-CoV-2, people in low income countries may not have a protective immune response obtained by vaccination (Bialek S., Boundy E., Bowen V., Chow N., Cohn A., Dowling N., Ellington S., Gierke R., Hall A., MacNeil J., Patel P., Peacock G., Pilishvili T., Razzaghi H., Reed N., Ritchey M., and Sauber-Schatz et al., 2020), and the inability to mount a protective response has consequences, not just for the individual-if living with HIV, for example-, but also for the collective. If the temperature exceeds the IPCC expectation and increases by 2.0 °C, the planet would be warmer than at any other moment in the last 3 million years. Once tipping points are reached, biophysical conditions will put Earth on a different track (Armstrong McKay et al., 2022). If the conditions preventing pathogen emergence change, we would see in the worst scenario that an acceleration in the rate of emergence of viral pathogens and/or a new constellation of fungal diseases that have opened the gates to thermic adaptation could enlarge the disparity gap (Casadevall & others, 2020).
Time will tell if in the adaptation to climate change we will be able to close the gaps in equality and build free, equal and more inclusive societies through empowered communities and, with that, arrest the spread of disease. Overcoming fear and stigma is the responsibility of everyone and the only way to maintain what makes us feel human.
Acknowledgments
Dirección General de Asuntos para el Personal Académico- Programa de Apoyo a Proyectos de investigación e innovación tecnológica DGAPA-PAPIIT- IV200321.
References
- Ahmad, D., & Afzal, M. (2021). Impact of climate change on pastoralists’ resilience and sustainable mitigation in Punjab, Pakistan. Environment, Development and Sustainability, 23, 11406–11426.
- Alvarez-Uria, G., Gandra, S., & Laxminarayan, R. (2016). Poverty and prevalence of antimicrobial resistance in invasive isolates. International Journal of Infectious Diseases, 52, 59–61. [CrossRef]
- Armstrong McKay, D. I., Staal, A., Abrams, J. F., Winkelmann, R., Sakschewski, B., Loriani, S., Fetzer, I., Cornell, S. E., Rockström, J., & Lenton, T. M. (2022). Exceeding 1.5 C global warming could trigger multiple climate tipping points. Science, 377(6611), eabn7950.
- Arredondo-Hernandez, R., Siebe, C., Castillo-Rojas, G., de León, S., & López-Vidal, Y. (2022). The synergistic interaction of systemic inflammation, dysbiosis and antimicrobial resistance promotes growth restriction in children with acute severe malnutrition: An emphasis on Escherichia coli. Frontiers in Antibiotics, 12. [CrossRef]
- Bialek.S, Boundy. E, Bowen. V, Chow. N, Cohn. A, Dowling. N, Ellington. S, Gierke. R, Hall. A, MacNeil. J, Patel. P, Peacock. G, Pilishvili. T, Razzaghi. H , Reed. N, Ritchey. M, and Sauber-Schatz, C. D. C., Team, R., COVID, C. D. C., Team, R., Bialek, S., Boundy, E., Bowen, V., Chow, N., Cohn, A., Dowling, N., & others. (2020). Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12--March 16, 2020. Morbidity and Mortality Weekly Report, 69(12), 343. 12 February.
- Casadevall, A., & others. (2020). Climate change brings the specter of new infectious diseases. The Journal of Clinical Investigation, 130(2), 553–555. [CrossRef]
- CCH, I. A. P. (2022). Health in the climate emergency: a global perspective.
- Collignon, P., Beggs, J. J., Walsh, T. R., Gandra, S., & Laxminarayan, R. (2018). Anthropological and socioeconomic factors contributing to global antimicrobial resistance: a univariate and multivariable analysis. The Lancet Planetary Health, 2(9), e398--e405. [CrossRef]
- Cooper, K., Huang, F.-F., Batista, L., Rayo, C. D., Bezanilla, J. C., Toth, T. E., & Meng, X.-J. (2005). Identification of genotype 3 hepatitis E virus (HEV) in serum and fecal samples from pigs in Thailand and Mexico, where genotype 1 and 2 HEV strains are prevalent in the respective human populations. Journal of Clinical Microbiology, 43(4), 1684–1688. [CrossRef]
- Costa, F., Hagan, J. E., Calcagno, J., Kane, M., Torgerson, P., Martinez-Silveira, M. S., Stein, C., Abela-Ridder, B., & Ko, A. I. (2015). Global morbidity and mortality of leptospirosis: a systematic review. PLoS Neglected Tropical Diseases, 9(9), e0003898. [CrossRef]
- Dittmar, J., Janssen, H., Kuske, A., Kurtz, J., & Scharsack, J. P. (2014). Heat and immunity: an experimental heat wave alters immune functions in three-spined sticklebacks (G asterosteus aculeatus). Journal of Animal Ecology, 83(4), 744–757.
- Fanzo, J., & Miachon, L. (2023). Harnessing the connectivity of climate change, food systems and diets: Taking action to improve human and planetary health. Anthropocene, 42, 100381. [CrossRef]
- Finn, C., Grattarola, F., & Pincheira-Donoso, D. (2023). More losers than winners: investigating Anthropocene defaunation through the diversity of population trends. Biological Reviews.
- Folke, C., Polasky, S., Rockström, J., Galaz, V., Westley, F., Lamont, M., Scheffer, M., Österblom, H., Carpenter, S. R., Chapin, F. S., & others. (2021). Our future in the Anthropocene biosphere. Ambio, 50(4), 834–869.
- Frumkin, H., & Haines, A. (2019). Global environmental change and noncommunicable disease risks. Annual Review of Public Health, 40, 261–282. [CrossRef]
- Guth, S., Mollentze, N., Renault, K., Streicker, D. G., Visher, E., Boots, M., & Brook, C. E. (2022). Bats host the most virulent—but not the most dangerous—zoonotic viruses. Proceedings of the National Academy of Sciences, 119(14), e2113628119.
- Ishaq, S. L., Rapp, M., Byerly, R., McClellan, L. S., O’Boyle, M. R., Nykanen, A., Fuller, P. J., Aas, C., Stone, J. M., Killpatrick, S., & others. (2019). Framing the discussion of microorganisms as a facet of social equity in human health. PLoS Biology, 17(11), e3000536. [CrossRef]
- Johnson, R. J. (2017). Pro: Heat stress as a potential etiology of Mesoamerican and Sri Lankan nephropathy: a late night consult with Sherlock Holmes. Nephrology Dialysis Transplantation, 32(4), 598–602. [CrossRef]
- Koch, R. E., Buchanan, K. L., Casagrande, S., Crino, O., Dowling, D. K., Hill, G. E., Hood, W. R., McKenzie, M., Mariette, M. M., Noble, D. W. A., & others. (2021). Integrating mitochondrial aerobic metabolism into ecology and evolution. Trends in Ecology & Evolution, 36(4), 321–332. [CrossRef]
- Lenton, T. M., Xu, C., Abrams, J. F., Ghadiali, A., Loriani, S., Sakschewski, B., Zimm, C., Ebi, K. L., Dunn, R. R., Svenning, J.-C., & others. (2023). Quantifying the human cost of global warming. Nature Sustainability, 1–11.
- Maywald, M., Wang, F., & Rink, L. (2018). The intracellular free zinc level is vital for treg function and a feasible tool to discriminate between treg and activated Th cells. International Journal of Molecular Sciences, 19(11), 3575. [CrossRef]
- Michinaka, T., Hlaing, E. E. S., Oo, T. N., Mon, M. S., & Sato, T. (2020). Forecasting forest areas in Myanmar based on socioeconomic factors. Forests, 11(1), 100. [CrossRef]
- Moore, E. R. H., Smith, M. R., Humphries, D., Dubrow, R., & Myers, S. S. (2020). The mismatch between anthropogenic CO2 emissions and their consequences for human zinc and protein sufficiency highlights important environmental justice issues. Challenges, 11(1), 4. [CrossRef]
- Mora, C., McKenzie, T., Gaw, I. M., Dean, J. M., von Hammerstein, H., Knudson, T. A., Setter, R. O., Smith, C. Z., Webster, K. M., Patz, J. A., & others. (2022). Over half of known human pathogenic diseases can be aggravated by climate change. Nature Climate Change, 1–7. [CrossRef]
- Muylaert, R. L., Kingston, T., Luo, J., Vancine, M. H., Galli, N., Carlson, C. J., John, R. S., Rulli, M. C., & Hayman, D. T. S. (2022). Present and future distribution of bat hosts of sarbecoviruses: implications for conservation and public health. Proceedings of the Royal Society B, 289(1975), 20220397. [CrossRef]
- Myers, S. S., Wessells, K. R., Kloog, I., Zanobetti, A., & Schwartz, J. (2015). Effect of increased concentrations of atmospheric carbon dioxide on the global threat of zinc deficiency: a modelling study. The Lancet Global Health, 3(10), e639--e645. [CrossRef]
- Nor, N. S. M., Yip, C. W., Ibrahim, N., Jaafar, M. H., Rashid, Z. Z., Mustafa, N., Hamid, H. H. A., Chandru, K., Latif, M. T., Saw, P. E., & others. (2021). Particulate matter (PM2. 5) as a potential SARS-CoV-2 carrier. Scientific Reports, 11(1), 2508.
- Organization, W. H. (2018). World health statistics 2023: monitoring health for the SDGs, sustainable development goals. World Health Organization.
- Pianka, E. R. (1970). On r-and K-selection. The American Naturalist, 104(940), 592–597.
- Pineda-Munoz, S., Wang, Y., Lyons, S. K., Tóth, A. B., & McGuire, J. L. (2021). Mammal species occupy different climates following the expansion of human impacts. Proceedings of the National Academy of Sciences, 118(2), e1922859118. [CrossRef]
- Rewar, S., & Mirdha, D. (2014). Transmission of Ebola virus disease: an overview. Annals of Global Health, 80(6), 444–451. [CrossRef]
- Semenza, J. C., Rocklöv, J., & Ebi, K. L. (2022). Climate Change and Cascading Risks from Infectious Disease. Infectious Diseases and Therapy, 1–20. [CrossRef]
- Streule, M., Karaman, O., Sawyer, L., & Schmid, C. (2020). Popular urbanization: Conceptualizing urbanization processes beyond informality. International Journal of Urban and Regional Research, 44(4), 652–672. [CrossRef]
- Tabari, H. (2020). Climate change impact on flood and extreme precipitation increases with water availability. Scientific Reports, 10(1), 1–10. [CrossRef]
- Tellman, B., & Eakin, H. (2022). Risk management alone fails to limit the impact of extreme climate events. Nature Publishing Group. [CrossRef]
- Thomas, K., Hardy, R. D., Lazrus, H., Mendez, M., Orlove, B., Rivera-Collazo, I., Roberts, J. T., Rockman, M., Warner, B. P., & Winthrop, R. (2019). Explaining differential vulnerability to climate change: A social science review. Wiley Interdisciplinary Reviews: Climate Change, 10(2), e565. [CrossRef]
- Tian, H., Hu, S., Cazelles, B., Chowell, G., Gao, L., Laine, M., Li, Y., Yang, H., Li, Y., Yang, Q., & others. (2018). Urbanization prolongs hantavirus epidemics in cities. Proceedings of the National Academy of Sciences, 115(18), 4707–4712. [CrossRef]
- UNDP. (2023). The SDGS in action.
- Vezzulli, L., Baker-Austin, C., Kirschner, A., Pruzzo, C., & Martinez-Urtaza, J. (2020). Global emergence of environmental non-O1/O139 Vibrio cholerae infections linked with climate change: a neglected research field? Environmental Microbiology, 22(10), 4342–4355.
- Von Schuckmann, K., Cheng, L., Palmer, M. D., Hansen, J., Tassone, C., Aich, V., Adusumilli, S., Beltrami, H., Boyer, T., Cuesta-Valero, F. J., & others. (2020). Heat stored in the Earth system: where does the energy go? Earth System Science Data, 12(3), 2013–2041.
- Vora, N. (2008). Impact of anthropogenic environmental alterations on vector-borne diseases. The Medscape Journal of Medicine, 10(10), 238.
- Walker, P. G. T., Whittaker, C., Watson, O. J., Baguelin, M., Winskill, P., Hamlet, A., Djafaara, B. A., Cucunubá, Z., Olivera Mesa, D., Green, W., & others. (2020). The impact of COVID-19 and strategies for mitigation and suppression in low-and middle-income countries. Science, 369(6502), 413–422.
- Wang, P., Asare, E., Pitzer, V. E., Dubrow, R., & Chen, K. (2022). Associations between long-term drought and diarrhea among children under five in low-and middle-income countries. Nature Communications, 13(1), 3661. [CrossRef]
- Warmuth, V. M., Metzler, D., & Zamora-Gutierrez, V. (2023). Human disturbance increases coronavirus prevalence in bats. Science Advances, 9(13), eadd0688. [CrossRef]
- Wessels, I., Rolles, B., Slusarenko, A. J., & Rink, L. (2022). Zinc deficiency as a possible risk factor for increased susceptibility and severe progression of Corona Virus Disease 19. British Journal of Nutrition, 127(2), 214–232. [CrossRef]
- Williams, J. (2021). Climate Change is Racist: Race, privilege and the struggle for climate Justice. Icon Books.
- Zhu, C., Kobayashi, K., Loladze, I., Zhu, J., Jiang, Q., Xu, X., Liu, G., Seneweera, S., Ebi, K. L., Drewnowski, A., & others. (2018). Carbon dioxide (CO2) levels this century will alter the protein, micronutrients, and vitamin content of rice grains with potential health consequences for the poorest rice-dependent countries. Science Advances, 4(5), eaaq1012. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).