Submitted:
08 June 2023
Posted:
09 June 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Subjects of study
Methods
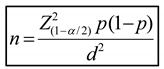
Statistical analysis
Results
Association of Population socio-demographic condition and Health Care Measures With COVID-19 Incidence
| TABLE 1 | Demographic characteristics of the study population(N=600) | |||
| Characteristics | Frequency | (%) | ||
| Gender | ||||
| Male | 188 | 31.3 | ||
| Female | 412 | 68.7 | ||
| Age group | ||||
| 0 - 9 | 40 | 6.7 | ||
| 10 - 19 | 45 | 7.5 | ||
| 20 - 29 | 161 | 26.8 | ||
| 30 - 39 | 143 | 23.8 | ||
| 40 - 49 | 53 | 8.8 | ||
| 50 - 59 | 56 | 9.3 | ||
| 60 - 69 | 58 | 9.7 | ||
| 70 - 79 | 29 | 4.8 | ||
| ≥ 80 | 15 | 2.5 | ||
| Median age (25th - 75th): 32 (24 - 51) year old | ||||
| TABLE2 | Prevalenceof SARS-CoV-2 positivity | ||||
| Gender | Number tests | (+) | (%) |
OR (95% CI) |
P |
| Male | 188 | 9 | 4.8 | 0.8 (0.4 - 1.8) |
0.6 |
| Female | 412 | 24 | 5.8 | ||
| Total | 600 | 33 | 5.5 | ||
| TABLE3 | Prevalenceof SARS-CoV-2 positivityage group | ||
| Age group | Number tests | (+) | (%) |
| 0 - 9 | 40 | 2 | 5.0 |
| 10 - 19 | 45 | 1 | 2.2 |
| 20 - 29 | 161 | 6 | 3.7 |
| 30 - 39 | 143 | 12 | 8.4 |
| 40 - 49 | 53 | 4 | 7.5 |
| 50 - 59 | 56 | 1 | 1.8 |
| 60 - 69 | 58 | 4 | 6.9 |
| 70 - 79 | 29 | 2 | 6.9 |
| ≥ 80 | 15 | 1 | 6.7 |
| Total | 600 | 33 | 5.5 |
| TABLE 4 | Disease severity and treatment outcome (N=33) | |||
| Characteristics | Frequency | (%) | ||
| Disease severity | ||||
| Asymptomatic | 0 | 0.0 | ||
| Mild | 25 | 75.8 | ||
| Moderate | 7 | 21.2 | ||
| Severe | 1 | 3.0 | ||
| Critical | 0 | 0.0 | ||
| Treatment outcome | ||||
| Recover | 33 | 100 | ||
| Death | 0 | 0.0 | ||
Laboratory tests
| TABLE 5 | Concentrations of some laboratory tests | |||||||||||
| Tests | Total(n=33) | Mild(n=25) | Moderate and Severe (n=8) | p | ||||||||
| White Blood Cell(/mm3) | ||||||||||||
| < 4000 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0.05 | |||||
| 4000 - 10.000 | 31 | 93.9 | 25 | 100 | 6 | 75.0 | ||||||
| > 10.000 | 2 | 6.1 | 0 | 0.0 | 2 | 25.0 | ||||||
| Median | 4.600 | 4.500 | 7.500 | <0.01 | ||||||||
| 25th - 75th | 4.400 - 5.000 | 4.300 - 4.600 | 6.000 - 13.500 | |||||||||
| Lymphocytes (/mm3) | ||||||||||||
| < 1.500 | 18 | 54.5 | 11 | 44.0 | 7 | 87.5 | 0.04 | |||||
| Median | 1.100 | 1.600 | 700 | <0.01 | ||||||||
| 25th - 75th | 800 - 2.000 | 1.100 - 2.000 | 625 - 800 | |||||||||
| Platelet Count(/mm3) | ||||||||||||
| < 150.000 | 20 | 60.6 | 14 | 56.0 | 6 | 75.0 | 0.3 | |||||
| Median | 180.000 | 180.000 | 205.000 | >0.05 | ||||||||
| 25th - 75th | 127.500 - 200.000 | 120.000 - 200.000 | 147.500 - 243.750 | |||||||||
| Hemoglobin (g/dl) | ||||||||||||
| Median | 12.2 | 12.2 | 12.6 | >0.05 | ||||||||
| 25th - 75th | 11.0 - 13.1 | 11.1 - 13.2 | 11 - 13 | |||||||||
| CRP (mg%) | ||||||||||||
| CRP > 10 | 3 | 9.1 | 1 | 4.0 | 2 | 25.0 | 0.1 | |||||
| CRP ≤ 10 | 30 | 90.9 | 24 | 96.0 | 6 | 75.0 | ||||||
| Ferritin (ng/mL) | ||||||||||||
| Median | 200 | 170 | 300 | <0.01 | ||||||||
| 25th - 75th | 150 - 275 | 145 - 256 | 273 - 348 | |||||||||
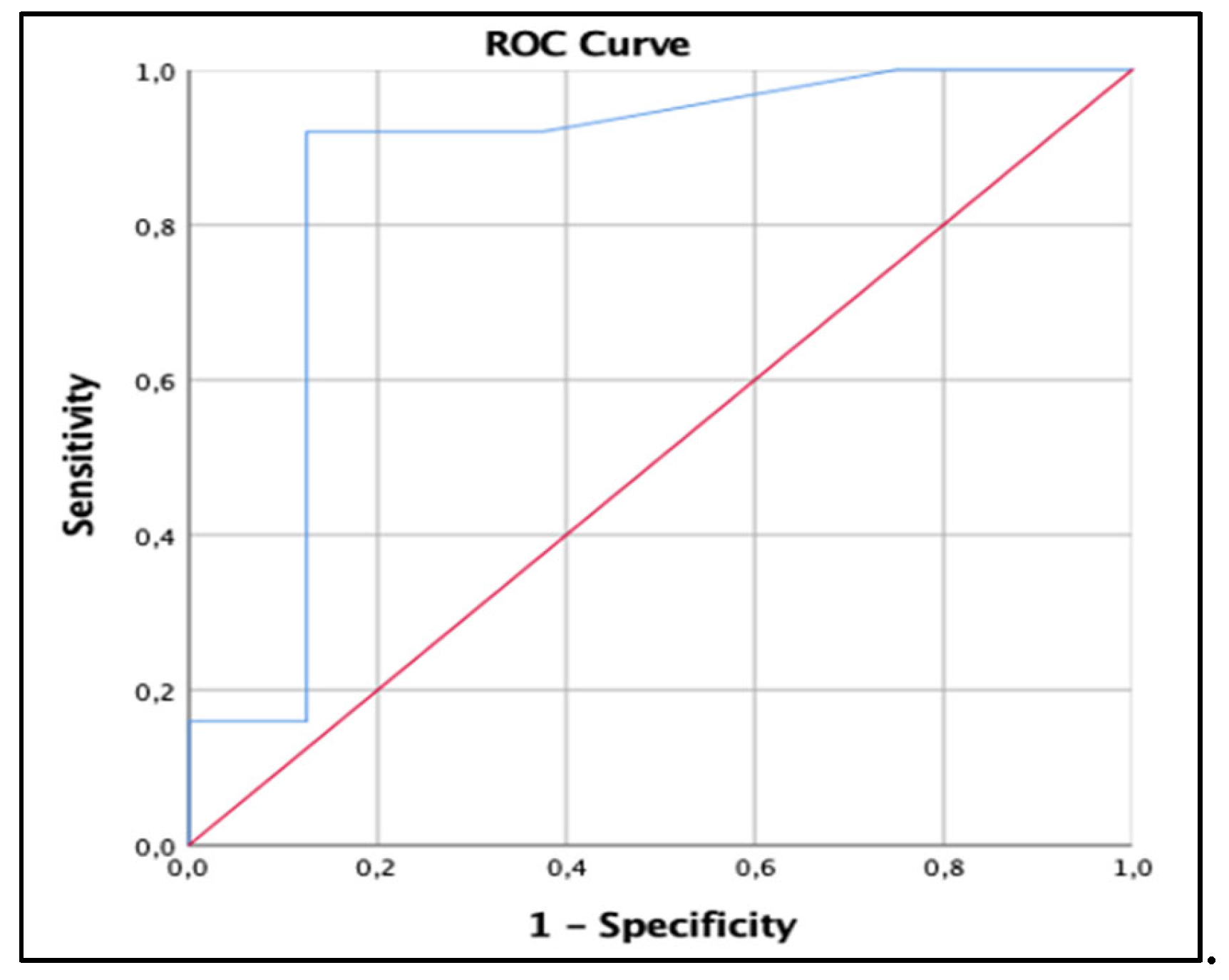
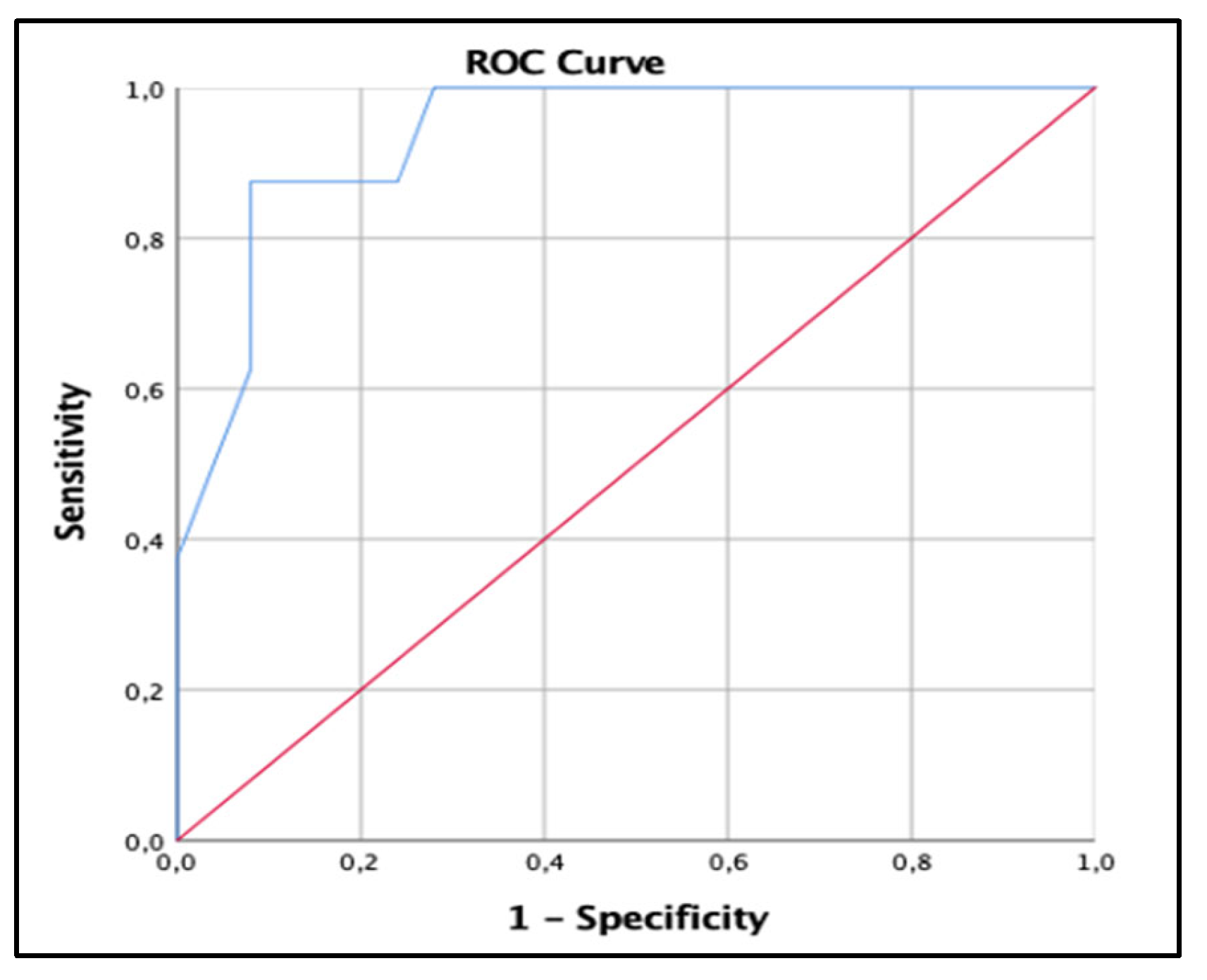
Discussion
Prevalence of positive for SARS-CoV-2, a socio-demographic point of view
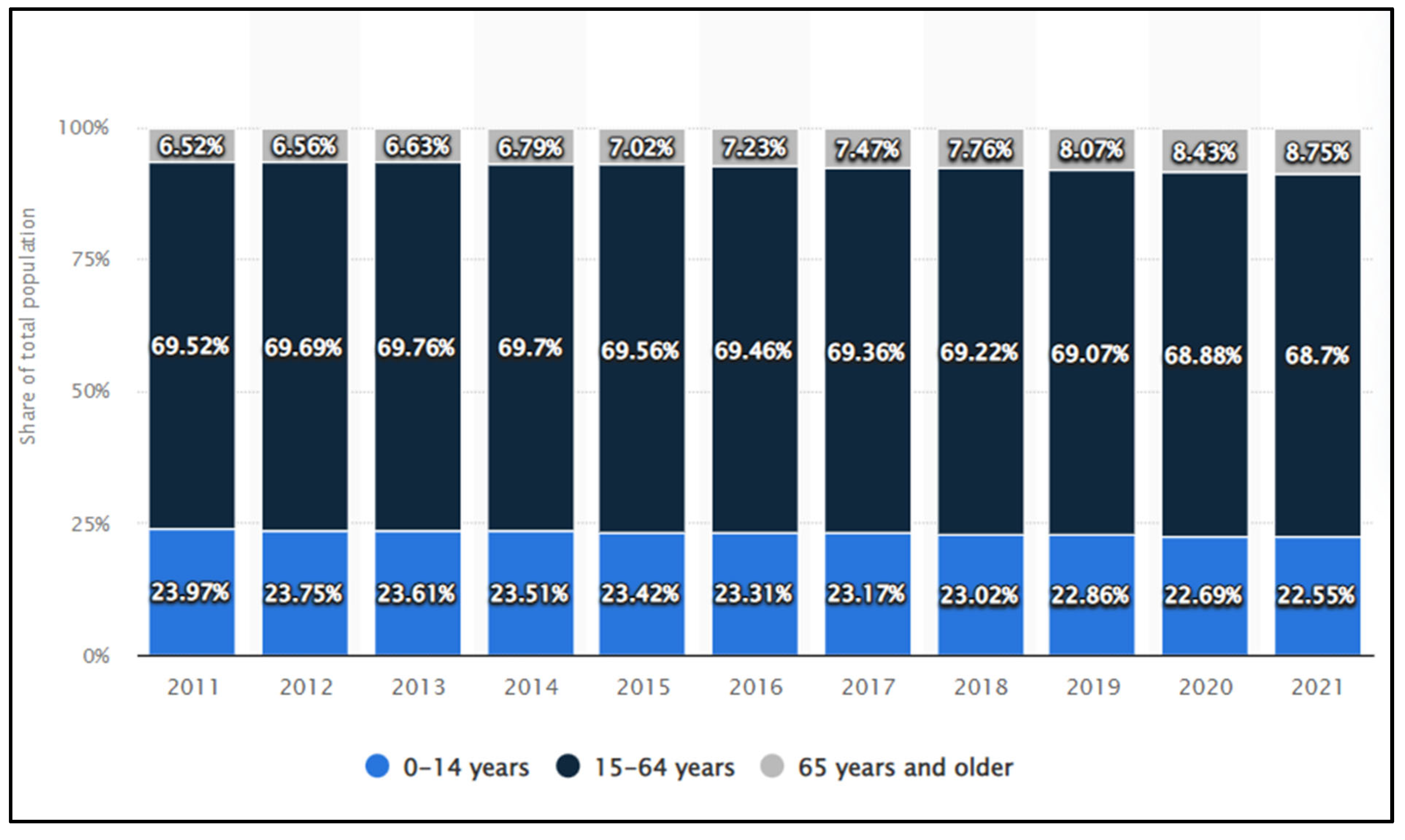
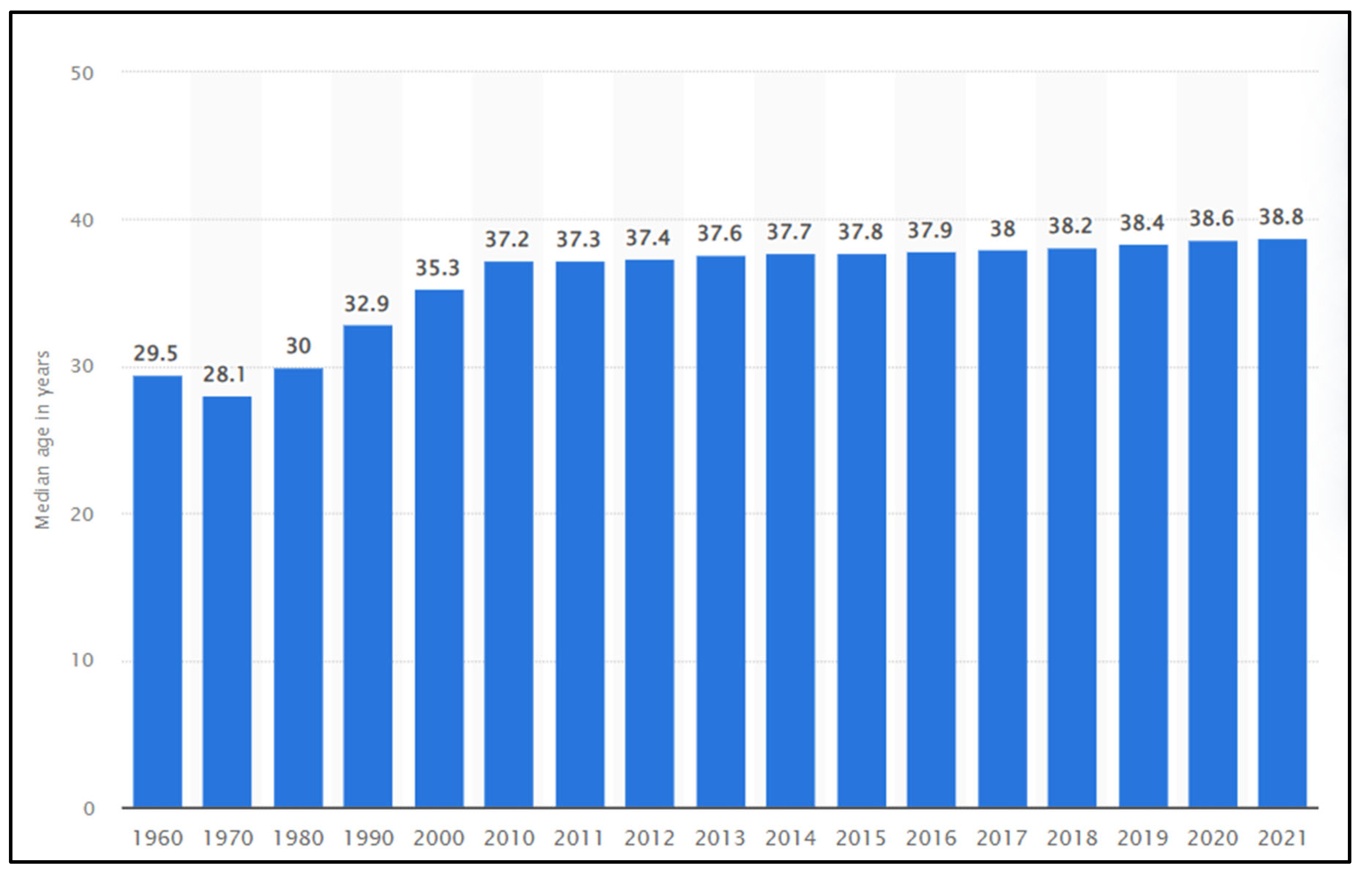
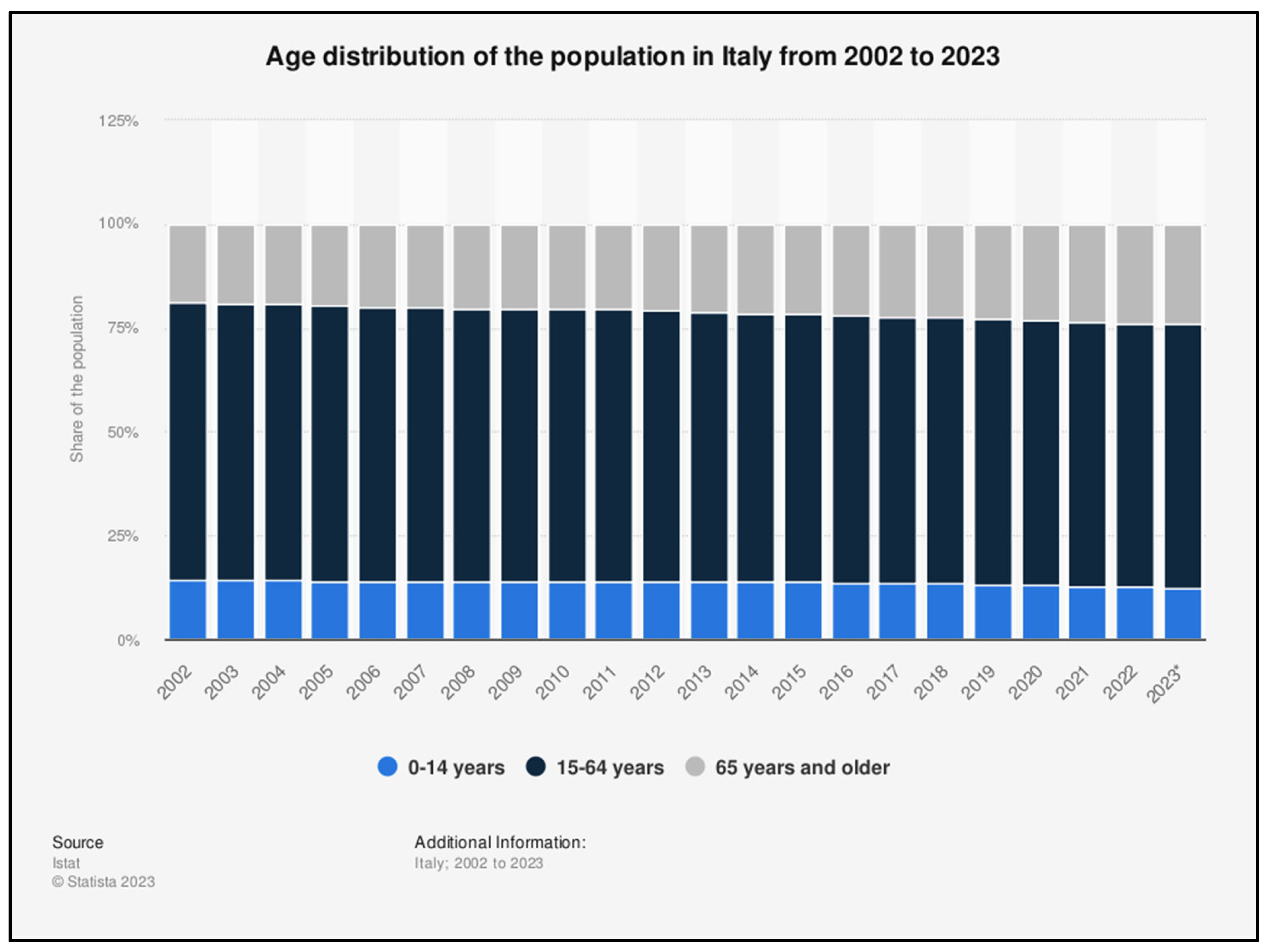
Interpretation of the findings
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
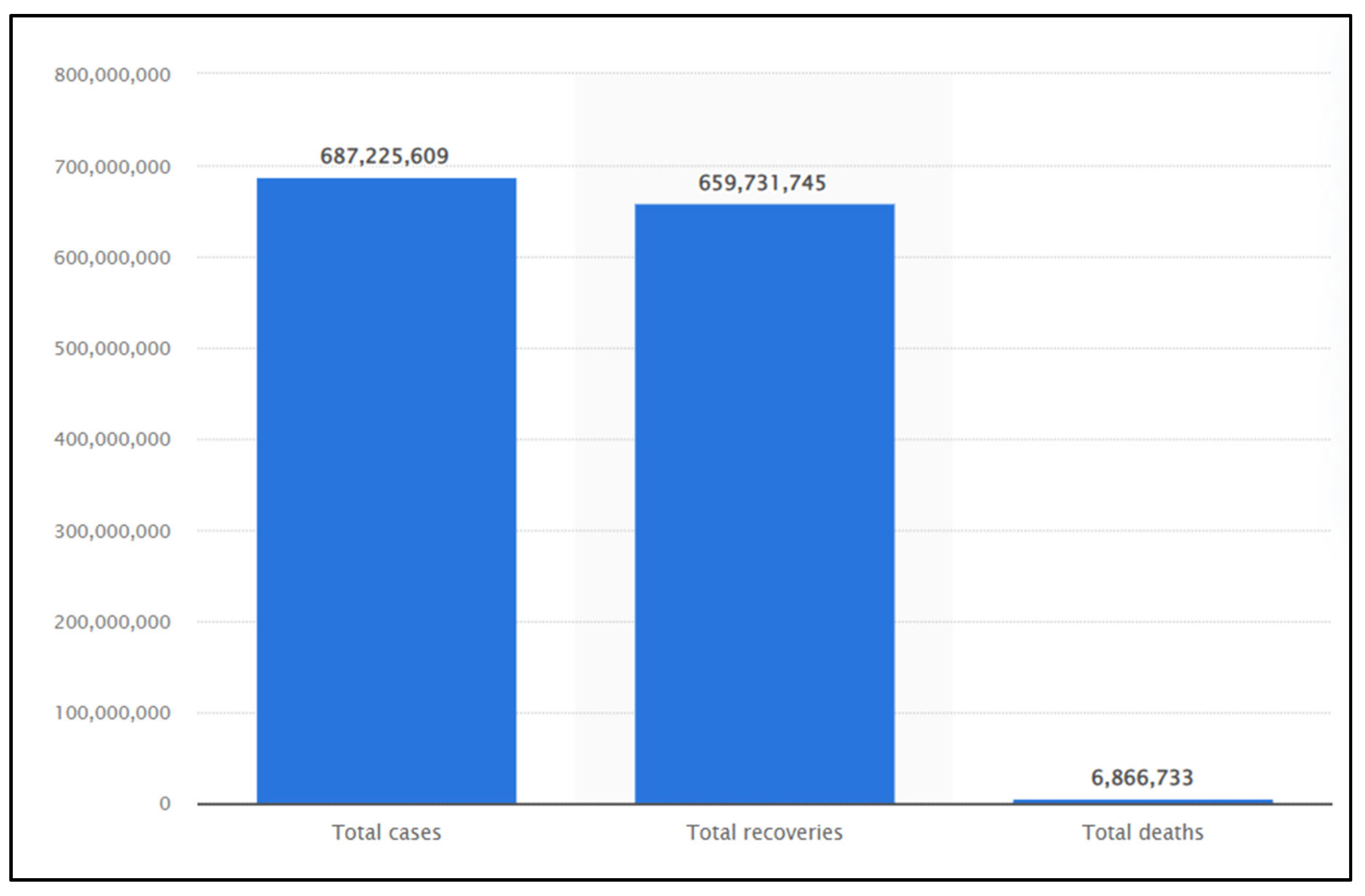
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard 2022. https://covid19.who.int/.
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H. Clinical and immunological features of severe and moderate coronavirus disease 2019. The Journal of clinical investigation 2020, 130, 2620–2629. [Google Scholar] [CrossRef]
- Liu, T.; Zhang, J.; Yang, Y.; Ma, H.; Li, Z.; Zhang, J.; Cheng, J.; Zhang, X.; Zhao, Y.; Xia, Z. The potential role of IL-6 in monitoring severe case of coronavirus disease 2019. MedRxiv. 2020:2020.2003. 2001.20029769..
- Jacob, L.; Koyanagi, A.; Smith, L.; Haro, J.M.; Rohe, A.M.; Kostev, K. Prevalence of and factors associated with COVID-19 diagnosis in symptomatic patients followed in general practices in Germany between March 2020 and March 2021. International journal of infectious diseases 2021, 111, 37–42. [Google Scholar] [CrossRef]
- Balzanelli, G.M.; Distratis, P.; Aityan, K.S.; Amatulli, F.; Catucci, O.; Cefalo, A.; et al. Clinical Features in Predicting COVID-19. Biomed J Sci & Tech Res 29(5)-2020. BJSTR extension. MS.ID.0048743.
- de Lusignan, S.; Dorward, J.; Correa, A.; Jones, N.; Akinyemi, O.; Amirthalingam, G.; Andrews, N.; Byford, R.; Dabrera, G.; Elliot, A. Risk factors for SARS-CoV-2 among patients in the Oxford Royal College of General Practitioners Research and Surveillance Centre primary care network: a cross-sectional study. The Lancet Infectious Diseases 2020, 20, 1034–1042. [Google Scholar] [CrossRef] [PubMed]
- Setiadi, W.; Rozi, I.E.; Safari, D.; Daningrat, W.O.D.; Johar, E.; Yohan, B.; Yudhaputri, F.A.; Lestari, K.D.; Oktavianthi, S.; Myint, K.S.A. Prevalence and epidemiological characteristics of COVID-19 after one year of pandemic in Jakarta and neighbouring areas, Indonesia: A single center study. Plos one 2022, 17, e0268241. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.; Distratis, P.; Catucci, O.; Amatulli, F.; Cefalo, A.; Lazzaro, R.; Aityan, K.S.; Dalagni, G.; Nico, A.; De Michele, A.; Mazza, E.; Tampoia, M.; D'Errico, P.; Pricolo, G.; Prudenzano, A.; D' Ettorre, E.; Di Stasi, C.; Morrone, L.F.P.; Nguyen, K.C.D.; Pham, H.V.; Inchingolo, F.; Tomassone, D.; Gargiulo Isacco, C. Clinical and diagnostic findings in COVID-19 patients: an original research from SG Moscati Hospital in Taranto Italy. J Biol Regul Homeost Agents. 2021, 35, 171–183, https://www.statista.com/statistics/1087466/covid19-cases-recoveries-deaths-worldwide/. [Google Scholar] [CrossRef] [PubMed]
- Statista-2023, https://www.statista. 1087.
- Mani, N.S.; Budak, J.Z.; Lan, K.F.; Bryson-Cahn, C.; Zelikoff, A.; Barker, G.E.; Grant, C.W.; Hart, K.; Barbee, C.J.; Sandoval, M.D. Prevalence of coronavirus disease 2019 infection and outcomes among symptomatic healthcare workers in Seattle, Washington. Clinical Infectious Diseases 2020, 71, 2702–2707. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization: Coronavirus disease 2019 (COVID-19): Situation report, 51. Retrieved , 2020, from https://apps.who.int/iris/handle/10665/331475. In.; 2020a. . 2 May.
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; Marder, E.P.; Raz, K.M.; Felix, S.E.B.; Tie, Y.; Fullerton, K.E. Coronavirus disease 2019 case surveillance-United States, January 22–may 30, 2020. Morbidity and Mortality Weekly Report 2020, 69, 759. [Google Scholar] [CrossRef] [PubMed]
- Boehmer, T.K.; DeVies, J.; Caruso, E.; van Santen, K.L.; Tang, S.; Black, C.L.; Hartnett, K.P.; Kite-Powell, A.; Dietz, S.; Lozier, M. Changing age distribution of the COVID-19 pandemic-United States, May–August 2020. Morbidity and Mortality Weekly Report 2020, 69, 1404. [Google Scholar] [CrossRef]
- Dudel, C.; Riffe, T.; Acosta, E.; van Raalte, A.; Strozza, C.; Myrskylä, M. Monitoring trends and differences in COVID-19 case-fatality rates using decomposition methods: Contributions of age structure and age-specific fatality. PLOS one 2020, 15, e0238904. [Google Scholar] [CrossRef]
- Ferre, J.; Abou Rafeh, A. COVID-19 and Older Persons: A Defining Moment for an Informed, Inclusive and Targeted Response. 2020.
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.; Fu, H. Estimates of the severity of coronavirus disease 2019: a model-based analysis. The Lancet infectious diseases 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Liu, Y.; Gu, Z.; Xia, S.; Shi, B.; Zhou, X.-N.; Shi, Y.; Liu, J. What are the underlying transmission patterns of COVID-19 outbreak? An age-specific social contact characterization. EClinicalMedicine 2020, 22, 100354. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. jama 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Guan W-j Ni Z-y Hu, Y.; Liang W-h Ou C-q He J-x Liu, L.; Shan, H.; Lei C-l Hui, D.S. Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Sannigrahi, S.; Pilla, F.; Basu, B.; Basu, A.S.; Molter, A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sustainable Cities and Society. 2020, 62.102418. ISSN 2210-6707. [CrossRef]
- Government News of the Socialist Republic of Viet Nam. https://en.baochinhphu.vn/viet-nams-population-increases-by-nearly-1-million-in-2022-111230104160334712.htm.
- Tomczyk, S.; Hönning, A.; Hermes, J.; Grossegesse, M.; Hofmann, N.; Michel, J.; et al. Longitudinal SARS-CoV-2 seroepidemiological investigation among healthcare workers at a tertiary care hospital in Germany. BMC Infect Dis. 2022, 22, 80. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Pham, V.H.; Tran, T.C.; Dipalma, G.; Bianco, A.; Serlenga, E.M.; Aityan, S.K.; Pierangeli, V.; Nguyen, K.C.D.; Inchingolo, F.; Tomassone, D.; Gargiulo Isacco, C. Analysis of Gene Single Nucleotide Polymorphisms in COVID-19 Disease Highlighting the Susceptibility and the Severity towards the Infection. Diagnostics (Basel). 2022, 12, 2824. [Google Scholar] [CrossRef]
- Balzanelli, M.G.; Distratis, P.; Lazzaro, R.; Cefalo, A.; Catucci, O.; Aityan, S.K.; Dipalma, G.; Vimercati, L.; Inchingolo, A.D.; Maggiore, M.E.; et al. The Vitamin D, IL-6 and the eGFR Markers a Possible Way to Elucidate the Lung-Heart-Kidney Cross-Talk in COVID-19 Disease: A Foregone Conclusion. Microorganisms. 2021, 9, 1903. [Google Scholar] [CrossRef]
- Martens, P.J.; Gysemans, C.; Verstuyf, A.; Mathieu, A.C. Vitamin D's Effect on Immune Function. Nutrients. 2020, 12, 1248. [Google Scholar] [CrossRef]
- Kaushal, K.; Kaur, H.; Sarma, P.; Bhattacharyya, A.; Sharma, D.J.; et al. Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis. J Crit Care. 2022, 67, 172–181. [Google Scholar] [CrossRef]
- Edeas, M.; Saleh, J.; Peyssonnaux, C. Iron: innocent bystander or vicious culprit in COVID-19 pathogenesis? Int J Infect Dis. 2020. [CrossRef]
- Colafrancesco, S.; Alessandri, C.; Conti, F.; Priori, R. COVID-19 gone bad: a new character in the spectrum of the hyperferritinemic syndrome? Autoimmun Rev. 2020, 19, 102573. [Google Scholar] [CrossRef] [PubMed]
- Drakesmith, H.; Prentice, A. Viral infection and iron metabolism. Nat Rev Microbiol. 2008, 6, 541–552. [Google Scholar] [CrossRef] [PubMed]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China, Clinical Infectious Diseases 2020, 71, 762–768.
- Velavan, T.P.; Meyer, C.G. Mild versus severe COVID-19: laboratory markers. Int J Infect Dis. 2020, 95, 304–7. [Google Scholar] [CrossRef] [PubMed]
- Balzanelli, M.G.; Distratis, P.; Dipalma, G.; Vimercati, L.; Catucci, O.; Amatulli, F.; Cefalo, A.; Lazzaro, R.; Palazzo, D.; Aityan, S.K.; Pricolo, G.; Prudenzano, A.; D'Errico, P.; Laforgia, R.; Pezzolla, A.; Tomassone, D.; Inchingolo, A.D.; Pham, V.H.; Iacobone, D.; Materi, G.M.; Scarano, A.; Lorusso, F.; Inchingolo, F.; Nguyen, K.C.D.; Gargiulo Isacco, C. Immunity Profiling of COVID-19 Infection, Dynamic Variations of Lymphocyte Subsets, a Comparative Analysis on Four Different Groups. Microorganisms. 2021, 9, 2036. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




