1. Introduction
Right-sided ligamentum teres (RSLT) is a rare anatomical variant in which the fetal umbilical vein is connected to the right paramedian trunk of the portal vein instead of the left portal vein [
1]. Reported incidence rates of RSLT range between 0.2% and 1.2% [
1,
2]. The ligamentum teres is the remnant of the functioning fetal umbilical vein. RSLT is thought to result from obstruction of the left umbilical vein during development, which causes persistence of the right umbilical vein; normally, the right umbilical vein obliterates and the left one persists [
3]. In the past, many cases of RSLT were reported as a left-sided gallbladder because the ligamentum teres and gallbladder often assumed the opposite position of normal [
1,
2]. However, a left-sided gallbladder associated with RSLT is actually an abnormality of the position of the ligamentum teres and should be distinguished from a "true” left-sided gallbladder, which is an abnormality of the position of the gallbladder itself [
2,
4]. Liver resection in patients with RSLT should be performed cautiously because RSLT is associated with a high frequency of portal vein, hepatic vein, and bile duct abnormalities[
5]. For this reason, most liver tumor patients with RSLT undergo open hepatectomy[
6]. We report a patient with RSLT who successfully underwent laparoscopic extended lateral sectionectomy for resection of a hepatocellular carcinoma.
2. Case report
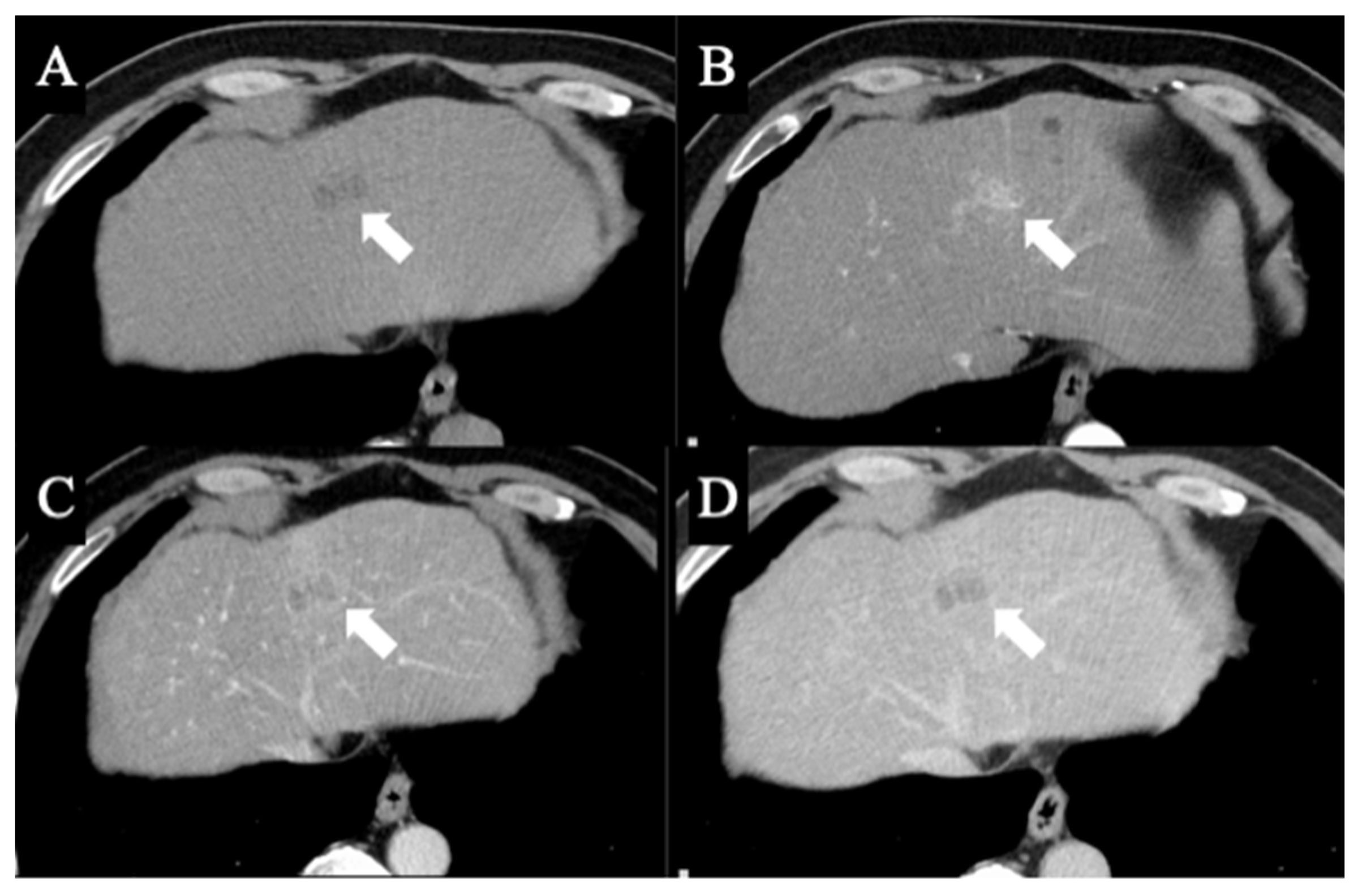
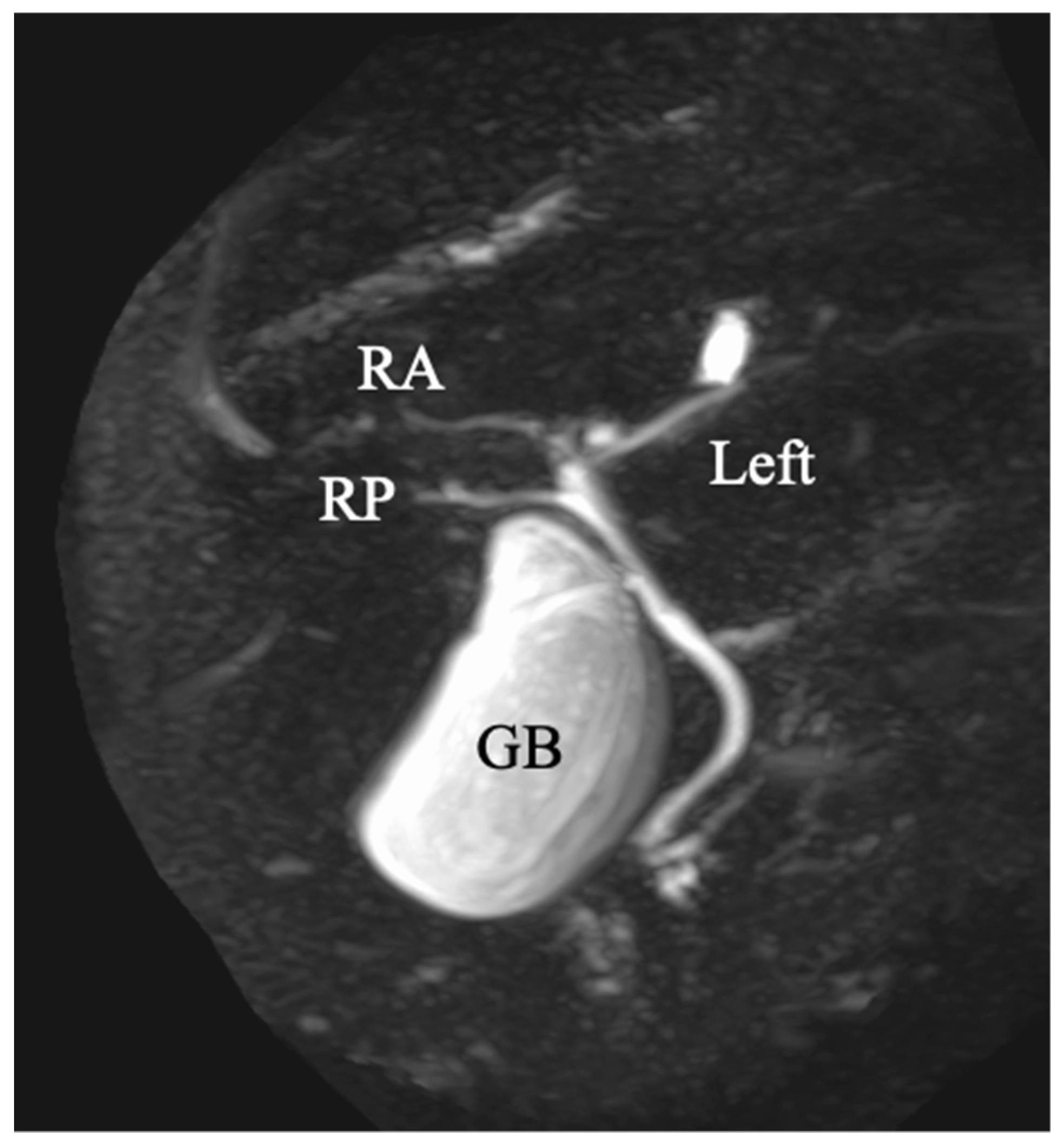
A 69-year-old man was referred for evaluation of a liver tumor detected on abdominal ultrasonography performed for nonalcoholic steatohepatitis follow-up. Blood testing showed elevations in concentrations of aspartate transaminase (56 U/L), alanine transaminase (51 U/L), and protein induced by vitamin K absence-II (224 mAU/mL). Other tumor markers and hepatitis virus markers were negative. The indocyanine green retention rate at 15 minutes was 15.2% and Child–Pugh score was 5 points (class A), suggesting good hepatic function. Computed tomography (CT) showed a 2.4 × 2.0 cm hypodense mass in the left lobe of the liver (S2/3/4b) which exhibited early arterial enhancement and washout (
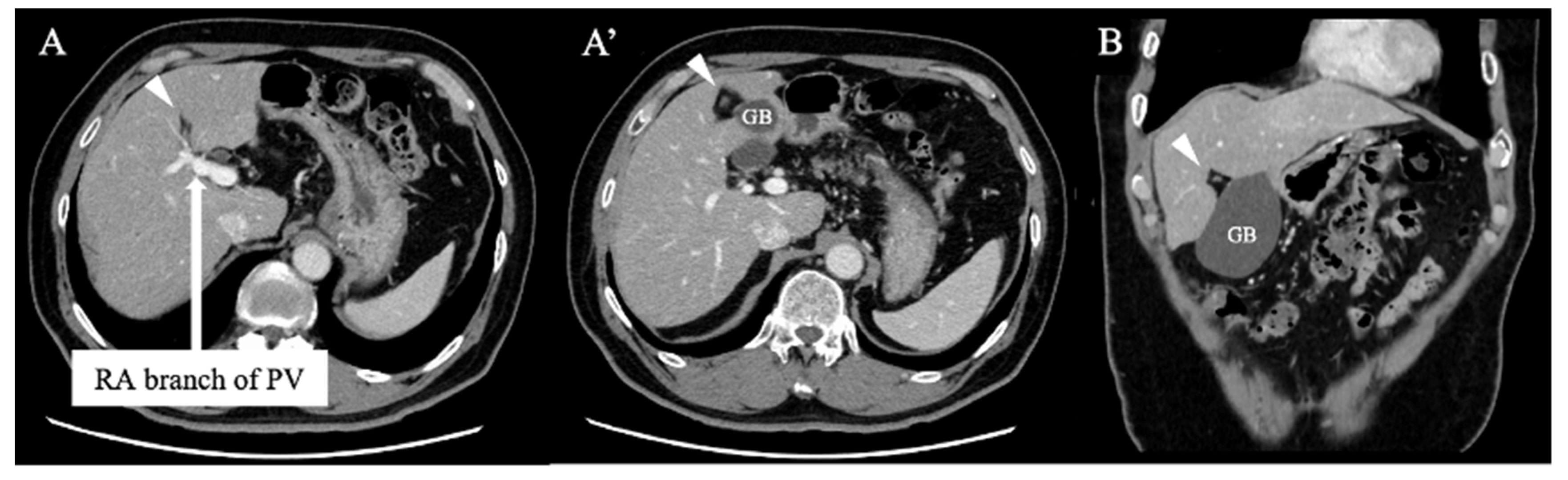
Figure 1). Hepatocellular carcinoma was highly suspected. In addition, the ligamentum teres was connected to the right anterior branch of the portal vein, and the gallbladder was located to its left, indicating RSLT (
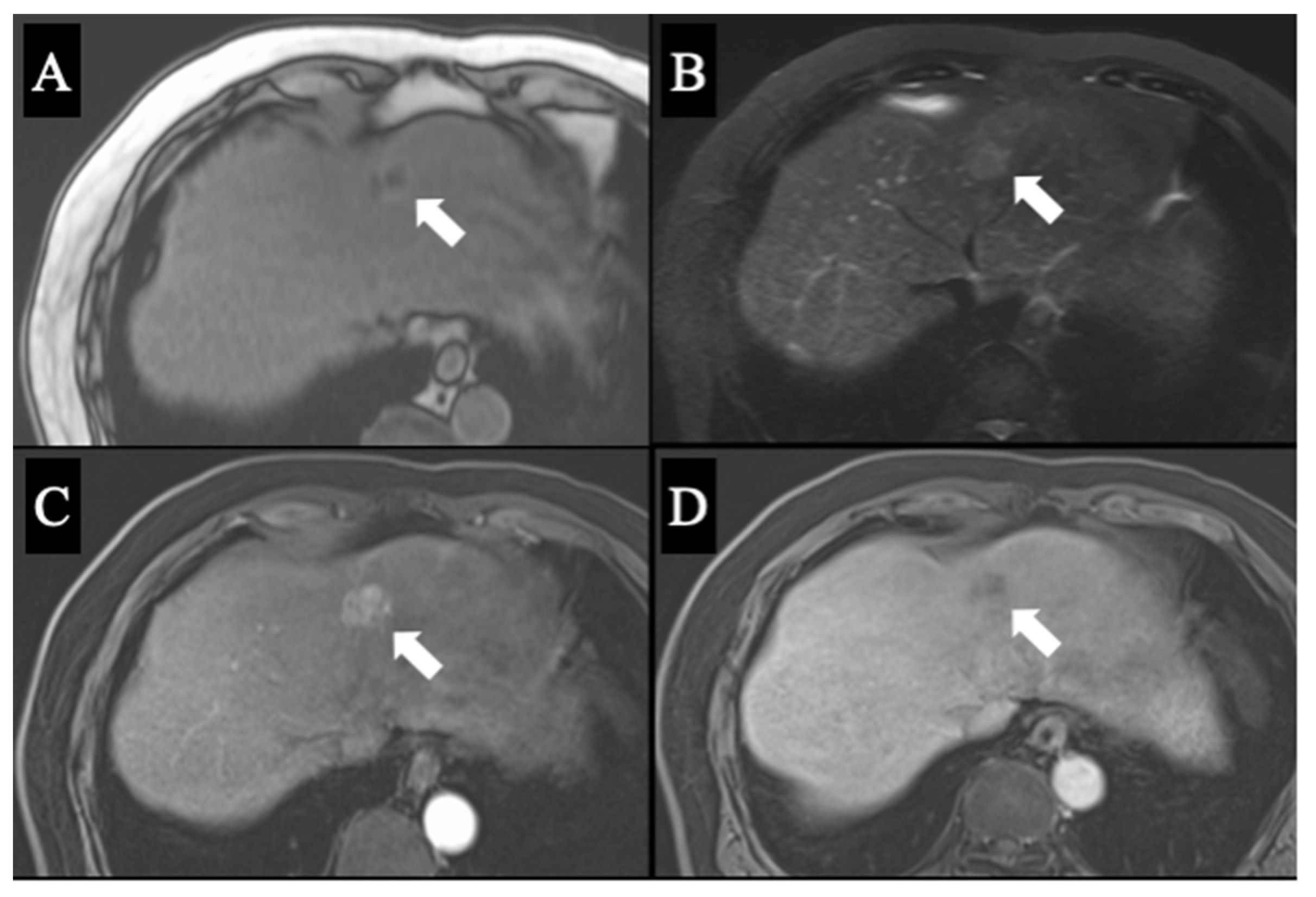
Figure 2). On magnetic resonance imaging, the mass was low signal intensity on T1-weighted images and high signal intensity on T2-weighted and diffusion-weighted images; contrasted imaging using gadolinium ethoxybenzyl diethylenetriamine penta-acetic acid revealed a perfusion defect in the mass in the liver phase (
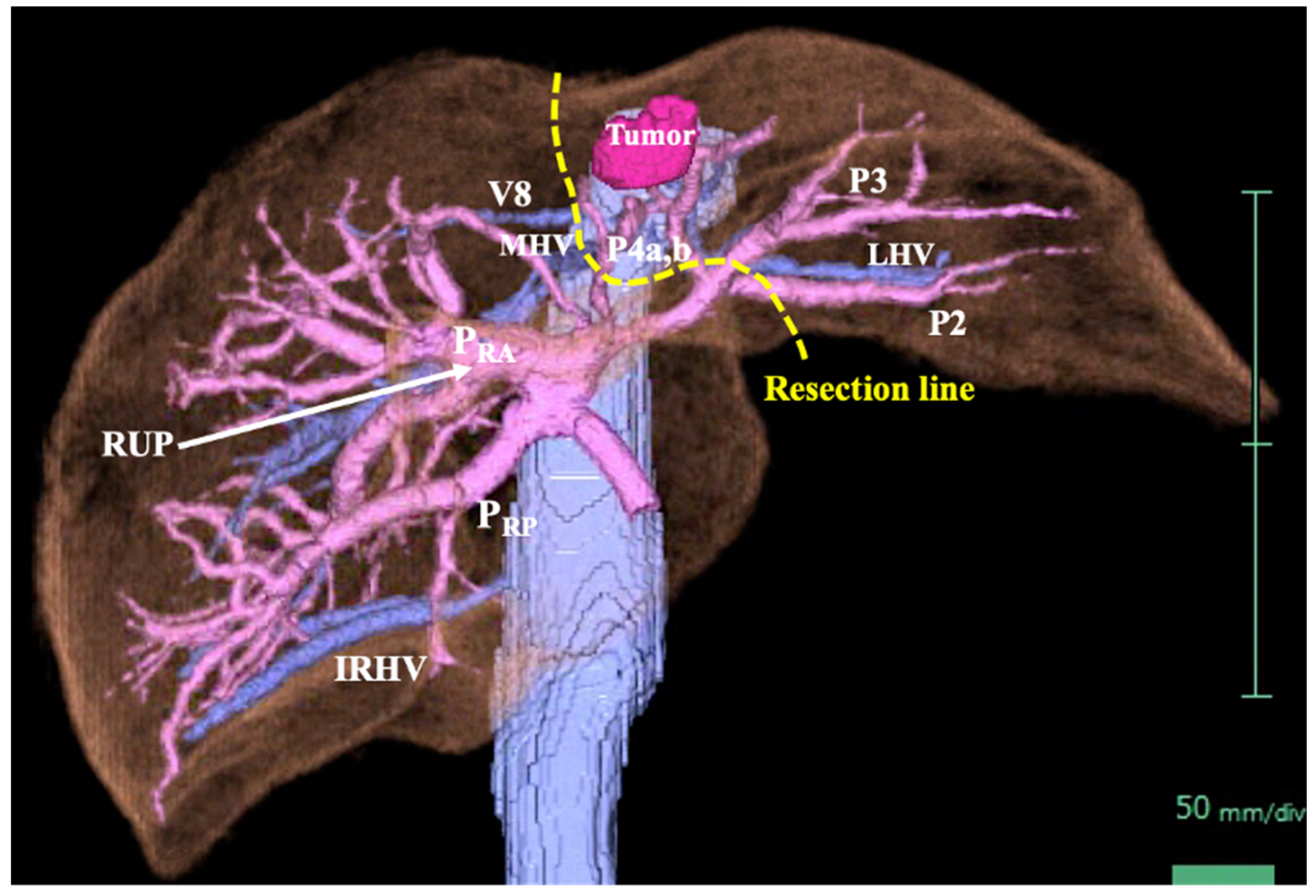
Figure 3). Three-dimensional CT (Synapse Vincent®︎; Fujifilm Medical, Tokyo, Japan) demonstrated right posterior, right anterior, and left branches of the portal vein. The left branch branched into P2 and P3 after two P4 branches separated. A right inferior hepatic vein and V8 were present (
Figure 4). Magnetic resonance cholangiopancreatography revealed that the bile duct system was trifurcated into right posterior, right anterior branch, and left branches (
Figure 5). After the pertinent anatomy was clarified and the preoperative evaluation was completed, we elected to perform laparoscopic extended lateral sectionectomy.
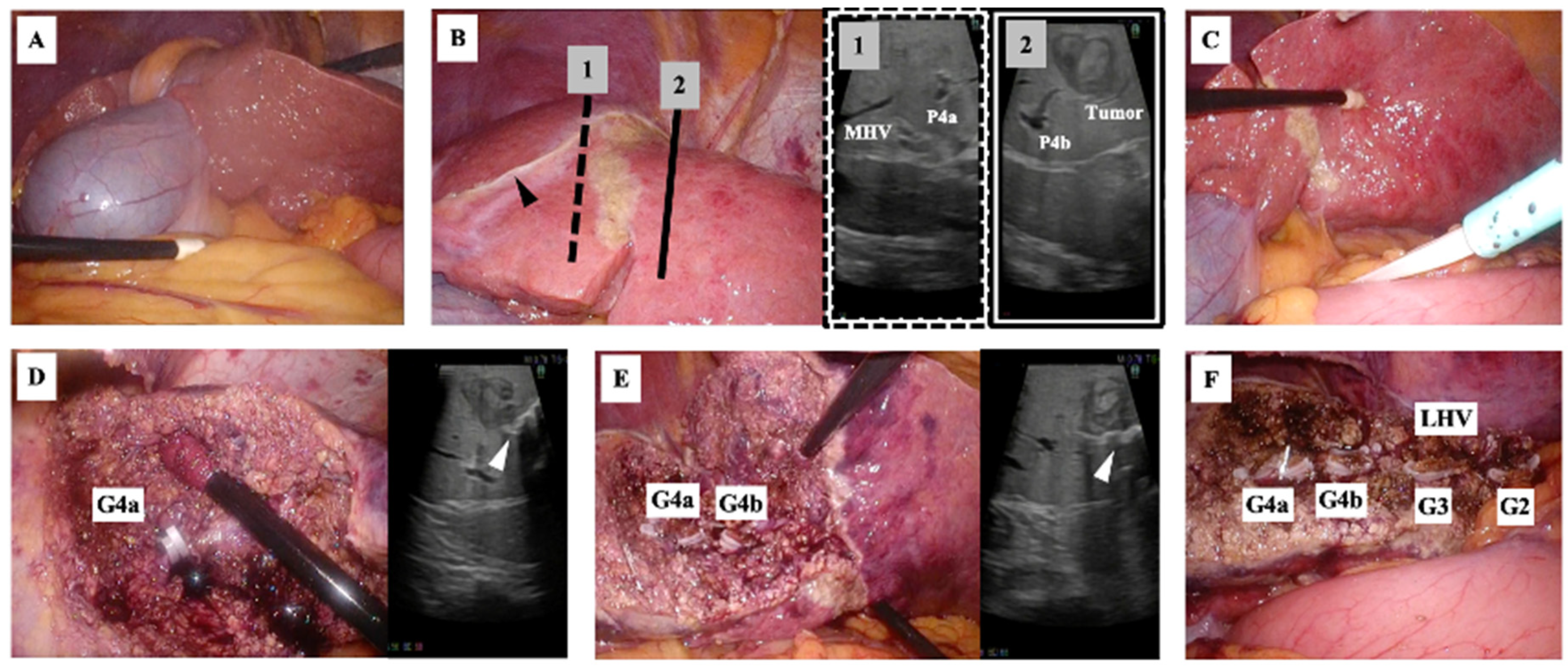
Surgery was performed with the patient in the supine position using a 2K high-definition/three-dimensional monitor. Five laparoscopy ports were placed: a 12 mm camera port at the umbilicus, 12 mm ports below the xiphoid process and below the right rib arch, and 5 mm ports outside the right and left rib arches. After confirmation of the RSLT and the location of the gallbladder (
Figure 6A), the falciform ligament and left triangular ligament were dissected. The tumor was then located using ultrasonography. To determine the extent of resection while avoiding damage to the right-sided vasculature, the head side was marked at the boundary between S4b and the right anterior section (
Figure 6B) and the caudal side was marked at the line where the S4a remained (
Figure 6C). The liver resection was performed using a cavitational ultrasonic surgical aspirator (CUSA®︎ Excel; Integra, Princeton, NJ, USA) and ultrasonic scalpel (Harmonic®︎ HD 1000i shears; Ethicon, Raritan, NJ, USA). The medial inferior, medial superior, lateral inferior, and lateral superior branches of Glisson and left hepatic vein were individually double-clipped using a polymer locking ligation system (Hem-o-lok®; Teleflex, Wayne, PA, USA) and resected. Thin vein branches were clipped using a metallic clip applier (Endo Clip®; Medtronic, Dublin, Ireland) and cut. Finally, the left lateral section, including the partial left median section, was resected (
Figure 6D, E, F). Operation time was 7 hours 35 minutes. Blood loss volume was 109 mL. The patient’s postoperative recovery was uneventful and he was discharged on postoperative day 7. The final pathological diagnosis was well-differentiated hepatocellular carcinoma.
3. Discussion
To the best of our knowledge, laparoscopic sectionectomy for a malignant liver tumor in a patient with RSLT has been reported only once previously [
6]. Most patients with RSLT are treated using open surgery because of the high frequency of vascular and bile duct abnormalities [
5]. However, the laparoscopic approach can be safe and effective with adequate preoperative and intraoperative imaging evaluations.
Our patient exhibited an independent posterior branch of the portal venous system, which is present in more than half of patients with RSLT [
1,
2,
5]. Shindoh et al. classified RSLT into three types based on portal branching pattern: bifurcation, trifurcation, and independent right lateral (posterior) type [
1]. In contrast, Terasaki et al. classified patients into four types: one bilateral ligamentum teres group and three RSLT groups (bifurcation, trifurcation, and independent posterior branch types) [
5,
7]. The newer Terasaki system may become the standard in the future. Regarding hepatic veins in patients with RSLT, a thick vein running along the ventral-dorsal segment border of the anterior sector and a developed V8 are likely to be present [
1,
5]. Our patient exhibited a developed V8. Because the middle hepatic vein (MHV) in patients with RSLT tends to be atrophic and displaced medially, the V8 may be misidentified as the MHV and should be treated with caution [
5]. As for the hepatic artery, most bifurcate and branch normally in patients with an RSLT, as in our patient [
1,
8].
The bile duct system frequently does not bifurcate normally in patients with RSLT. Nishitai et al. classified biliary architecture in such patients into four types: the symmetrical type, in which the right umbilical portion (RUP) is the watershed between the right and left branches of the bile duct; the independent right lateral type, in which the right posterior branch is independent and the right anterior sector branch comes around from the left side of the RUP; and the total left and total right types, in which the entire liver is drained only by the bile duct coming around the RUP from one direction [
8]. In their study, half were symmetrical and 28% were independent right lateral type, as in our patient.
The presence of these vascular and bile duct system abnormalities can lead to unexpected complications [
6,
8]. In our patient, both the portal vein and the bile duct had a bifurcation type in which the right posterior branch independently diverged; this branch then diverged into right anterior and left branches. In such cases, caution is required when performing a left lobectomy, including left lateral sectionectomy, because an incision which is too deep or more right-sided than planned may result in injury to the right anterior branch. In addition, the ligamentum teres and the falciform ligament do not represent landmarks for the P2 and P3 origins in patients with LSRT [
6]. Furthermore, misidentification of a developed V8 as MHV may lead to a situation in which a planned left lobectomy must be converted to a left trisectionectomy. These possibilities were all considered in our case. However, the points to keep in mind will vary depending on the particular combination of anatomical anomalies and the type of surgery planned.
Fifteen cases of hepatectomy for malignant tumors in patients with RSLT have been reported in the English literature, 13 open and two laparoscopic (
Table 1) [
2,
6,
7,
9,
10,
11,
12,
13,
14,
15,
16,
17]. Three-dimensional liver anatomy simulation systems using CT images allow detailed and easy evaluation of tumor location and vasculature. Several reports have shown that such evaluation is quite useful in RSLT cases characterized by many anatomical abnormalities [
6,
15,
16]. Compared with open surgery, many operations are more difficult when performed laparoscopically because of instrument angle limitations and the inability to directly observe the intraperitoneal cavity. Therefore, careful preoperative evaluation of tumor location, progression, and anatomy is necessary. With a thorough evaluation and frequent use of ultrasonography during surgery, laparoscopic hepatectomy can be performed safely in many patients.
4. Conclusions
RSLT is frequently associated with abnormalities of the liver vasculature and bile duct system. These abnormalities can lead to complications when performing hepatectomy. With left lobectomy, including left lateral sectionectomy, it is important to avoid injury to the right liver vasculature. Laparoscopic hepatectomy can be performed safely in patients with RSLT provided that careful surgical planning is conducted using preoperative three-dimensional CT analysis and intraoperative ultrasonography is used.
Author Contributions
Conceptualization, Y.A. and H.Y.; Image analysis, Y.A., H.T., M.H., T.Y. and K.I.; data curation, Y.A., H.T., M.H., T.Y. and K.I.; writing—original draft preparation, Y.A. and H.T.; writing—review and editing, Y.A. and H.Y.; visualization, Y.A.; supervision, H.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Asahikawa Medical University.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original data presented in the study are included in the article. Further inquiries can be directed to hidekiyokoo@asahikawa-med.ac.jp.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shindoh, J.; Akahane, M.; Satou, S.; Aoki, T.; Beck, Y.; Hasegawa, K.; Sugawara, Y.; Ohtomo, K.; Kokudo, N. Vascular architecture in anomalous right-sided ligamentum teres: three-dimensional analyses in 35 patients. HPB (Oxford) 2012, 14, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Kubota, K.; Kawasaki, S.; Takayama, T.; Bandai, Y.; Makuuchi, M. Are left-sided gallbladders really located on the left side? Ann Surg 1997, 225, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Maetani, Y.; Itoh, K.; Kojima, N.; Tabuchi, T.; Shibata, T.; Asonuma, K.; Tanaka, K.; Konishi, J. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology 1998, 207, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Saafan, T.; Hu, J.Y.; Mahfouz, A.E.; Abdelaal, A. True left-sided gallbladder: A case report and comparison with the literature for the different techniques of laparoscopic cholecystectomy for such anomalies. Int J Surg Case Rep 2018, 42, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Ohgi, K.; Aramaki, T.; Uesaka, K. Analysis of right-sided ligamentum teres: The novel anatomical findings and classification. J Hepatobiliary Pancreat Sci 2021, 28, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Ohgi, K.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Uesaka, K. Laparoscopic left lateral sectionectomy for a patient with right-sided ligamentum teres. Surg Case Rep 2019, 5, 43. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, F.; Yamamoto, Y.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Ohgi, K.; Akamoto, S.; Uesaka, K. A case of perihilar cholangiocarcinoma with bilateral ligamentum teres hepatis treated with hepatopancreatoduodenectomy. Surg Case Rep 2020, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Nishitai, R.; Shindoh, J.; Yamaoka, T.; Akahane, M.; Kokudo, N.; Manaka, D. Biliary architecture of livers exhibiting right-sided ligamentum teres: an indication for preoperative cholangiography prior to major hepatectomy. HPB (Oxford) 2016, 18, 929–935. [Google Scholar] [CrossRef] [PubMed]
- Uesaka, K.; Yasui, K.; Morimoto, T.; Torii, A.; Kodera, Y.; Hirai, T.; Yamamura, Y.; Kato, T.; Kito, T. Left-Sided gallbladder with intrahepatic portal venous anomalies. Journal of Hepato-Biliary-Pancreatic Surgery 1995, 2, 425–430. [Google Scholar] [CrossRef]
- Kaneoka, Y.; Yamaguchi, A.; Isogai, M.; Harada, T. Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: anomalous configuration of the intrahepatic biliary tree. J Hepatobiliary Pancreat Surg 2000, 7, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Tashiro, H.; Itamoto, T.; Nakahara, H.; Ohdan, H.; Kobayashi, T.; Asahara, T. Resection of hepatocellular carcinoma in a patient with congenital anomaly of the portal system. Dig Surg 2003, 20, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, T.; Suzuki, S.; Morita, Y.; Oishi, K.; Suzuki, A.; Fukumoto, K.; Inaba, K.; Takehara, Y.; Baba, S.; Nakamura, S.; et al. Hepatectomy for metastatic liver tumors complicated with right umbilical portion. Hepatogastroenterology 2011, 58, 984–987. [Google Scholar] [PubMed]
- Abe, T.; Kajiyama, K.; Harimoto, N.; Gion, T.; Shirabe, K.; Nagaie, T. Resection of metastatic liver cancer in a patient with a left-sided gallbladder and intrahepatic portal vein and bile duct anomalies: A case report. Int J Surg Case Rep 2012, 3, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Almodhaiberi, H.; Hwang, S.; Cho, Y.J.; Kwon, Y.; Jung, B.H.; Kim, M.H. Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies. Korean J Hepatobiliary Pancreat Surg 2015, 19, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Ome, Y.; Kawamoto, K.; Park, T.B.; Ito, T. Major hepatectomy using the glissonean approach in cases of right umbilical portion. World J Hepatol 2016, 8, 1535–1540. [Google Scholar] [CrossRef] [PubMed]
- Hai, S.; Hatano, E.; Hirano, T.; Asano, Y.; Suzumura, K.; Sueoka, H.; Fujimoto, J. Hepatectomy for Hilar Cholangiocarcinoma with Right-Sided Ligamentum Teres Using a Hepatectomy Simulation System. Case Rep Gastroenterol 2017, 11, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Terajima, H.; Yamamoto, T.; Uchida, Y. Hepatectomy for gallbladder-cancer with unclassified anomaly of right-sided ligamentum teres: A case report and review of the literature. World J Hepatol 2018, 10, 523–529. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).