1. Introduction
Among the head and neck cancers, the adenoideocystic carcinoma (AC) recurs as a rare variant that usually affects the parotids and its primary origin from the ceruminous glands of the ear auditory canal (EAC) is considered extremely rare. In fact, the full medical literature reports only very few anecdotal cases or reviews with no controlled studies on clinical management as well as therapeutic responses and survival [
1].The EAC cancers generally occur with protean clinical presentation and symptoms while their morphologies overlap between benign and malignant tumors[
2] and particularly AC, represents 0.0001% of all neoplasms of the cervico-facial district [
3] although it is the most frequent among tumors originating from the ceruminous glands [
1].
Due to the extreme rarity of AC of the ceruminous glands (ACCG), even in the latest AIOM (Italian Association of Oncology) 2019 guidelines there are no survival data and specific indications for treatment. For this reason, the approach to diagnosis, therapy and follow-up must necessarily be related to the general lines of head and neck tumors for which integrated therapeutic protocols are available and primarily include surgical excision followed by chemo-radiotherapy as well as immunotherapy in relation to the clinical stage of the disease.
Several progress in staging has recently grown in relation to the presence of a few viruses including HPV in particular in squamous neoplasms of the oral cavity and to the expression by the cancer cells of the epithelial growth factor receptor (EGFR), namely a cancer proliferation inducer molecule.
The surgical radicalization followed by radiotherapy is the gold standard treatment for these tumors up to their T2-N0 stage, whereas in advanced stages chemotherapy including platinum derivatives combined with anti-EGFR monoclonal antibodies and radiation treatment is functional in inducing the tumor remission. According to international studies, the combined chemo-radio treatment of patients within the III-IV, M0 stage after the surgical resection leads to a 5-year survival in approximately 58% of patients [
4,
5,
6,
7].
ACCG is considered a slow-growing carcinoma and leads to gradually occupy the EAC resulting in hearing loss as first symptom though other common disorders including ear pain, otorrhea, tinnitus and dizziness can also occur. In a review of the ACCG from literature1, it is stated that, if removed at stage I-II N0 M0 and properly treated with chemo-radio, the survival is variable and depends on various factors. According to Craig et all1, the survival over 10 years occurred in more than 50% of patients considered in the study which, however, included a cohort of 17 cases.
However, although slow in its growing, ACCG shows marked infiltrative and metastatic properties whose clinical effects occur even several years after the tumor ablation. The organs frequently affected are beyond the structures adjacent to the excision site and may include the central nervous system, lungs, liver, kidneys and skeleton [
8] for which the positive surgical margins for tumor on the operative report, bone infiltration and invasion perineural are considered to be unfavorable prognostic criteria [
9].
From the medico-legal point of view, this neoplasm presents some criticalities represented by the difficulty of making a diagnosis due to the rarity of the tumor thus rendering quite difficult the histotype classification and for the fact that the patient often underestimates the symptoms affecting the ear thus delaying the visit to the otrorinolaryngologist specialist. This case report aims to clarify what potential cases of malpractice can be related to this type of cancer.
2. Case report
This is the case of Mrs. A.D. who in April 2010 was admitted to a hospital in southern Italy for left hearing loss since about 4 years. A ceruminous plug was extracted and both antibiotics and cortisone were administered. The patient was discharged with a diagnosis of perichondritis of the left auricle. In September 2010, the patient underwent a biopsy of the lesion whose histological examination indicated the presence of fragments of basal cell carcinoma with cutaneous aspects of Morphea whose resection margins were site of neoplasm. MRI performed to stage the neoplasm described the pathological thickening of the skin, subcutaneous and mucous layers of the external auditory canal (EAC) which was impregnated with contrast medium without other signs of involvement of nearby and intracranial structures as well as organs.
In January 2011 a histopathological revision of the biopsy was made and she underwent surgery after the diagnosis of benign eccrine EAC neoplasm for which the patient underwent surgery of the lesion which occupied the anterior pretragal and perianular area with initial erosion of the bone duct on the back. During surgery, the extemporaneous histological examination described an AC. Due to the complexity of the surgery caused by the extension of the tumor, the patient was advised to necessity of the petrosectomy to be performed at a Swiss otolaryngology center where the histological evaluation of the removed lesion confirmed the extemporaneous diagnosis of AC, with trabecular growth characteristics, onset from the ceruminous glands with EAC and surrounding tissue infiltration, involvement of the surgical margins and perineural infiltration.
In February 2011 the patient underwent In the Swiss hospital, to resection of the left auricle, left subtotal petrosectomy, left parotidectomy, and resection of the left mandibular joint capsule. The examination of the surgical specimen confirmed the histological diagnosis of AC in fragments residual from the previous surgery, and revealed tumor infiltration only in the soft tissues without further tumor presence in the other resected structures.
In April 2011 she began radiotherapy treatment for adjuvant purposes.
In July 2012, the total body PET examination highlighted "... Multiple millimeter bilateral pulmonary nodular formations not metabolically characterized due to their small size ...".
In November 2012, following a follow-up CT scan, the patient was diagnosed with volumetric enlargement of some pulmonary nodular lesions in the right lower lobe which were interpreted as metastatic repeats. The patient was then submitted to first line chemotherapy (Cisplatin + 5FU + Erbitux) until May 2013 and then to second line protocol from February to April 2014 to counteract the progression of lung metastases whereas In November 2019 she underwent hypofractionated radiotherapy on lung metastatic lesions refractory to chemotherapies. The procedure involved only the most voluminous lesions at risk of bronchial compression.
By September 2020, the patient underwent further radiotherapy regimens to slow the progression of lung lesions and several lesions were reducing as effect of radiation therapy applications, whereas other nodular lesions showed a tendency to increase in their size. Besides the lung lesions, a metastatic nodule was detected on the VI segment of the liver that was ablated by stereotaxis radio-treatment in March 2021.
2.2. Figures
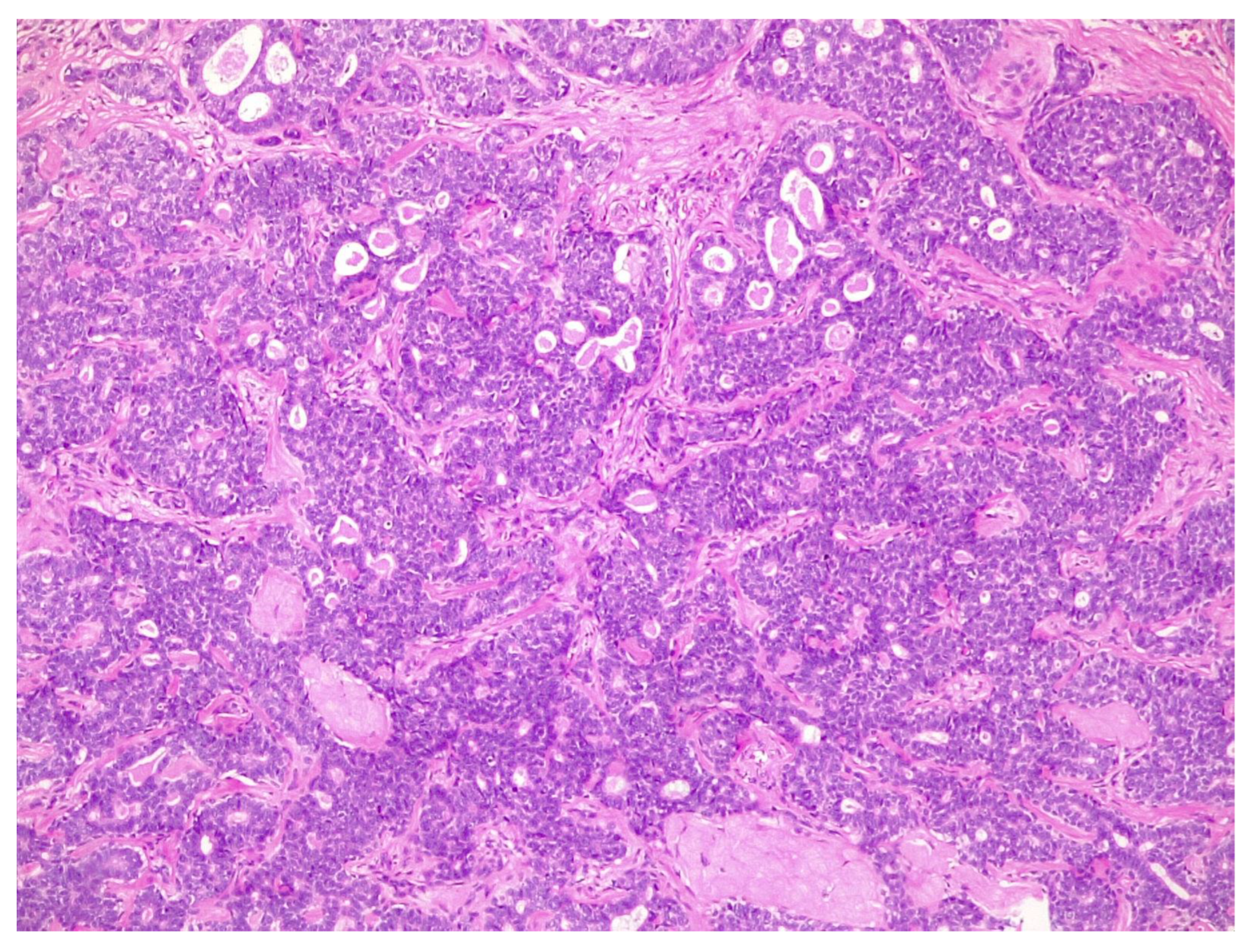
Figure 1.
Solid pattern of adenoid cystic carcinoma: densely cellular, irregular-shaped islands of tumor cells containing only some small pseudocysts.
Figure 1.
Solid pattern of adenoid cystic carcinoma: densely cellular, irregular-shaped islands of tumor cells containing only some small pseudocysts.
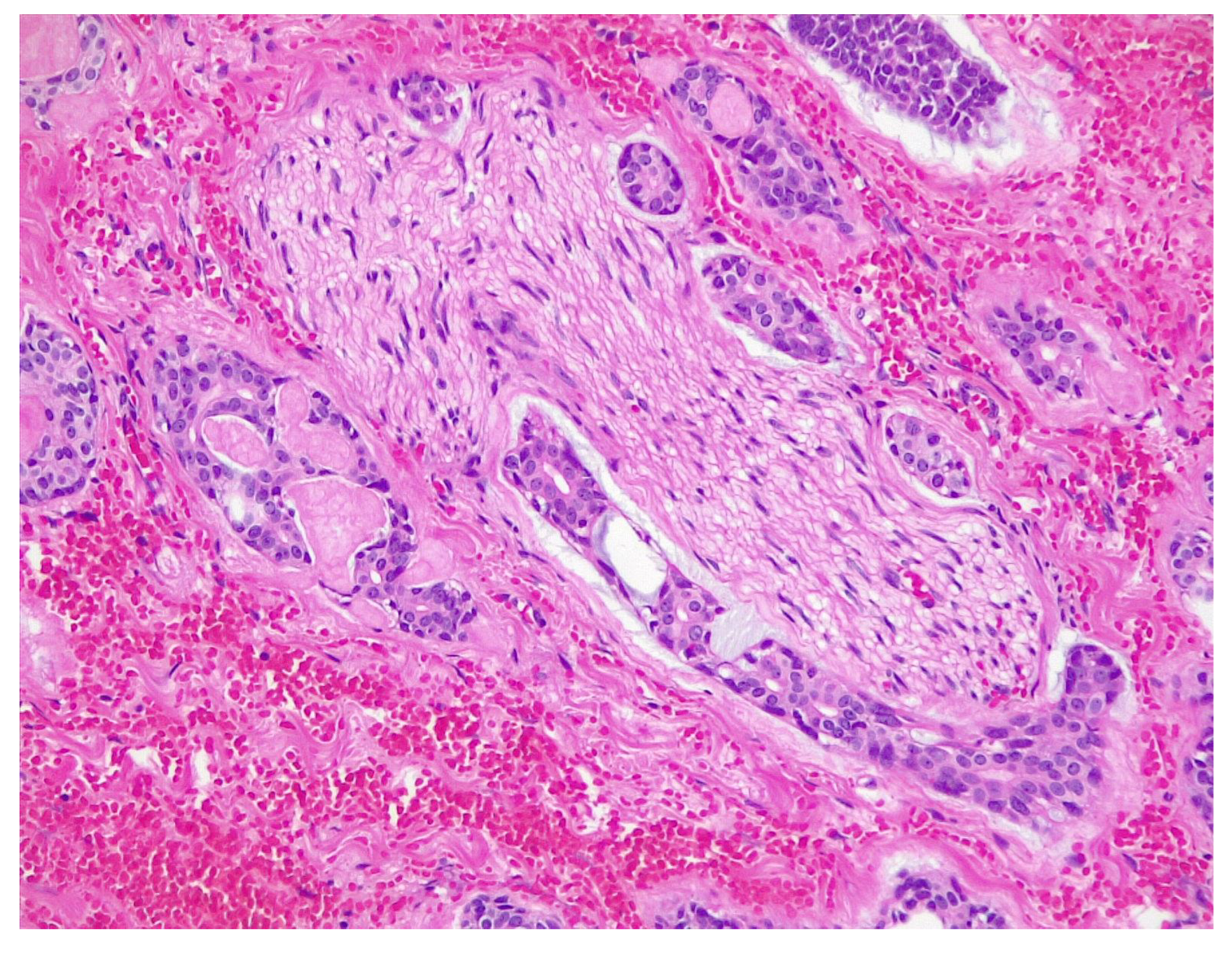
Figure 2.
Peripheral nerve invasion is one of the hallmarks of adenoid cystic carcinoma: it is usually perineural, within the nerve sheath.
Figure 2.
Peripheral nerve invasion is one of the hallmarks of adenoid cystic carcinoma: it is usually perineural, within the nerve sheath.
4. Discussion
The patient presented a definitely aggressive variant of AC as effect of both perineural and bone invasion described in the surgical specimen following the first excisional surgery in January 2011. Furthermore, in the natural evolution of the neoplasm, despite the chemo-radiotherapy treatment, the metastatic disease progressed with high aggressiveness in relation to the discovery of the voluminous pulmonary nodules detected by PET in July 2012 as well as the liver metastasis in the examination TC of March 2021. Therefore, based on the time longer than 10 years since the original symptoms and accordingly to the natural history of the tumor, the unfavorable prognostic factors including perineural, bone and soft tissue invasion, were predictors of the metastatic progression that occurred in the following years.
In our case the diagnostic delay (2008-2011) may have influenced the evolution of the tumor. In fact, due to the slow progression of ACCG neoplasm, if in 2008 an MRI examination of the left EAC would have been performed, the tumor diagnosis would have been easier and more prompt. It should be emphasized that the symptoms presented by the patient, since 2006, characterized by hearing loss and otalgia, should have required in addition to the attending physician also the otolaryngologist for a necessary diagnostic investigation. Furthermore, according with Prasad et all, patients with long standing otalgia, decreased hearing and ear canal mass should be early considered for deep incisional biopsy along with imaging since early prompt surgery combined with adjuvant radiotherapy may help to prevent distant metastasis. It must be considered, according with Markou, that the rarity of the disease and the relative inexperience combined with the nonspecific symptomatology and the often-vague imaging results render the diagnosis especially difficult. It must be reported that the lack of specific clinical and radiological signs makes the diagnosis of ceruminous gland tumors challenging. In his study CT scans were performed in a few cases, but no tumor suspicion was addressed by the radiologist while, moreover, the difficulty of achieving an accurate pathological diagnosis when inadequate specimens are provided has been repeatedly emphasized.
5. Conclusions
From the legal medical point of view, the profile of responsibility is substantiated on the delayed diagnosis when the lately observed tumor progression by the invasion of both surrounding bone and vascular structures. The perineural invasion, indeed, represents an important prognostic factor for detecting the progress of the tumor since, when present, it should be considered as dipendent from advanced aggression and correlates with distant metastases.
Therefore, if the diagnostic delay caused by the erroneous professional approach occurred before the tumor generated the perineural spread, it would probably require a more extensive and demolishing surgery for the higher probability of metastasis spead.
In the event that the patient has died, due to the tumor disease, at the time of the medical-legal evaluation, he will be recognized a loss of chance of survival which will have to consider the worst prognosis of the neoplastic disease caused by the diagnostic delay.
On the contrary, if the diagnostic delay does not lead to tumor invasion of the osteo-vascular structures, from the point of view of responsibility we can then sustain that it is not productive of compensable damage.
Author Contributions
Conceptualization, N.D., C.R. and F.S.; methodology, N.D., G.C., M.E., S.R. and E.S.; validation, N.D., C.R. and F.S.; investigation, N.D. and F.S.; writing—original draft preparation, N.D., G.C., M.E., S.R. and E.S.; writing—review and editing, N.D., C.R. and F.S.; visualization, G.C., M.E., S.R. and E.S.; supervision, N.D., C.R. and F.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
The authors are deeply grateful to Prof. Mauro Melato for his constant support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Beckmann S, Dettmer MS, Caversaccio MD, Giger R, Anschuetz L. Pleomorphic Adenoma of External Auditory Canal: Case Report of First Endoscopic Resection and Literature Review. Medicina. 2020, 56, 248. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, P. Ceruminous neoplasms of the ear. Head and Neck Pathol. 2018, 12, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Crain N, L. Nelson BL, Barnes LE, Thompson LDR, Ceruminous gland carcinomas: a clinicopathologic and immunophenotypic study of 17 cases. Head and Neck Pathol. 2009, 3, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Mohan H, Handa U, Amanjit, Kotwal AS, Dass A. Adenoid Cystic Carcinoma of the External Auditory Canal. A Case Report with Diagnosis by fine Needle Aspiration. Acta Cytol. 2003, 47, 792–794. [Google Scholar] [CrossRef] [PubMed]
- Triantafillidou K, Dimitrakopoulos J, Iordanidis F, Koufogiannis D. Management of Adenoid Cystic Carcinoma of Minor Salivary Glands. J Oral Maxillofac Surg. 2006, 64, 1114–1120. [Google Scholar] [CrossRef] [PubMed]
- Associazione Italiana di Oncologia Medica (AIOM), Linee Guida 2019.
- Santiago GS, Tapia JPR, Pendás JLL, Nieto CS. Factores Prognósticos en el Carcinoma Adenoide Quístico de Glândulas salivares. Acta Otorrinolaringol Esp. 2005, 56, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Koopot R, Reyes C, Pifarré R. Multiple pulmonary metastases from adenoid cystic carcinoma of ceruminous glands of external auditory canal. A case report and review of the literature. J Thorac Cardiovasc Surg. 1973, 65, 909–913. [Google Scholar] [CrossRef]
- Moore MG, et al. : Management outcomes following lateral temporal bone resection for ear and temporal bone malignancies. Otolaryngol Head Neck Surg 2007, 137, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Prasad V, Shenoy VS, Rao RA, Kamath PM, Shihab H. Adenoid Cystic Carcinoma– A rare Differential Diagnosis for a mass in the External Auditory Canal. J Clin Diagn Res. 2015, 9, MD01–MD02. [Google Scholar]
- Markou K, Karasmanis I, Vlachtsis K, Petridis D, Nikolaou A, Vital V. Primary pleomorphic adenoma of the external ear canal. Report of a case and literature review. Am J Otolaryngol. 2008, 29, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Mills RG, Douglas-Jones T, Williams RG. ‘Ceruminoma’ a defunct diagnosis. J Laryngol Otol. 1995, 109, 180–188. [Google Scholar] [CrossRef]
- Lassaletta L, Patron M, Oloriz J, Perez R, Gavilan J. Avoiding misdiagnosis in ceruminous gland tumours. Auris Nasus Larynx. 2003, 30, 287–290. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).