1. Introduction
The rising prevalence of obesity in older adults is a global concern, as it is accompanied by a natural increase in fat mass and decrease in muscle mass and strength, resulting in sarcopenic obesity (SO) [
1,
2,
3]. The synergistic impact of obesity and muscle impairment heightens the risk of developing multiple health outcomes, including functional limitations and injury risk [
4,
5]. The associated muscle impairment may cause functional limitations in activities of daily living, particularly walking [
6,
7]. Furthermore, individuals with large body sizes but disproportionately low muscle strength are at a higher risk of both disability and future disability development [
3,
8]. Therefore, implementing tailored physical activity programs that suit older adults with SO is critical in preventing falls [
9], enhancing mobility, and promoting healthy aging among obese older adults [
10].
Aging is associated with a decline in a variety of neural, hormonal, and environmental trophic signals to muscle [
11,
12,
13,
14]. The loss of muscle mass and mass-specific strength is accelerated by a variety of factors, including physical inactivity [
15], hormonal changes [
16], pro-inflammatory state [
17], malnutrition [
18], loss of alpha-motor units in the central nervous system [
19,
20]. These factors negatively alter functional capacities, postural control, and walking [
21,
22,
23,
24], limit autonomy, and increase the risk of falls [
21,
24].
Research has demonstrated that obese individuals may experience difficulties in performing simple motor tasks with sufficient velocity, and they often exhibit greater instability during walking [
25,
26]. In addition, spatiotemporal gait parameters, such as speed, cadence, and stride, are significantly lower in obese individuals [
27,
28,
29]. These alterations are associated with multiple adverse consequences for skeletal muscle, including inflammation [
30], oxidative stress [
31], and insulin resistance [
32]. Fatty infiltration of skeletal muscle is also associated with reduced strength, functional status, and muscle dysfunction, decreased contractility and motor unit recruitment, and interference in normal cellular signaling [
33].
In addition to the above studies, there is growing evidence for the synergistic impact of sarcopenia and obesity on gait and mobility in older adults [
6,
34,
35,
36,
37]. In fact, obesity presents additional constraints to age-related postural control deteriorations [
38,
39] and increases risk of falls [
40]. Recently, Maktouf et al. [
34] showed that obese older adults had lower vertical ground reaction force (GRFv), higher center of pressure (CoP) velocity, shorter and wider stride, and spent more time in support phase. These gait alterations were associated with higher ankle muscle activity. These findings underscore the significance of addressing sarcopenia and obesity as interdependent yet distinct factors while devising interventions to enhance gait and mobility in older adults. Moreover, the impact of obesity on gait parameters may differ between adults and older individuals, emphasizing the need to differentiate between these age groups when designing interventions to enhance functional capacities.
Many studies have indicated that physical activity is one of the most effective non-pharmacological interventions for the management of older adults with SO [
41,
42,
43]. Various studies have shown that PA can lead to improvements in body composition [
42,
43], muscle mass, strength [
41,
42,
43,
44], and physical performance [
45,
46,
47,
48]. However, no prior investigations have explored the effects of a physical activity regimen emphasizing posture, strengthening, and motricity exercises (PSM) on neuromuscular strategies, CoP displacements, and kinematic and kinetic gait parameters in older adults with SO. Furthermore, it is important to address some limitations observed in previous studies. These include the lack of information on the methodology for setting up the physical activity protocol, the program’s progressiveness, the quality, and intensity of exercises to be performed, and the quantification of each session based on individual feedback. These limitations underscore the need for more comprehensive studies that develop effective physical activity interventions tailored to the specific needs and capacities of older adults with SO.
The objective of the study was to assess the effectiveness of the PSM program on body composition, physical performance, neuromuscular strategies at the ankle joint during walking, and kinematic and kinetic gait parameters in older adults with SO.
2. Materials and Methods
2.1. Study design
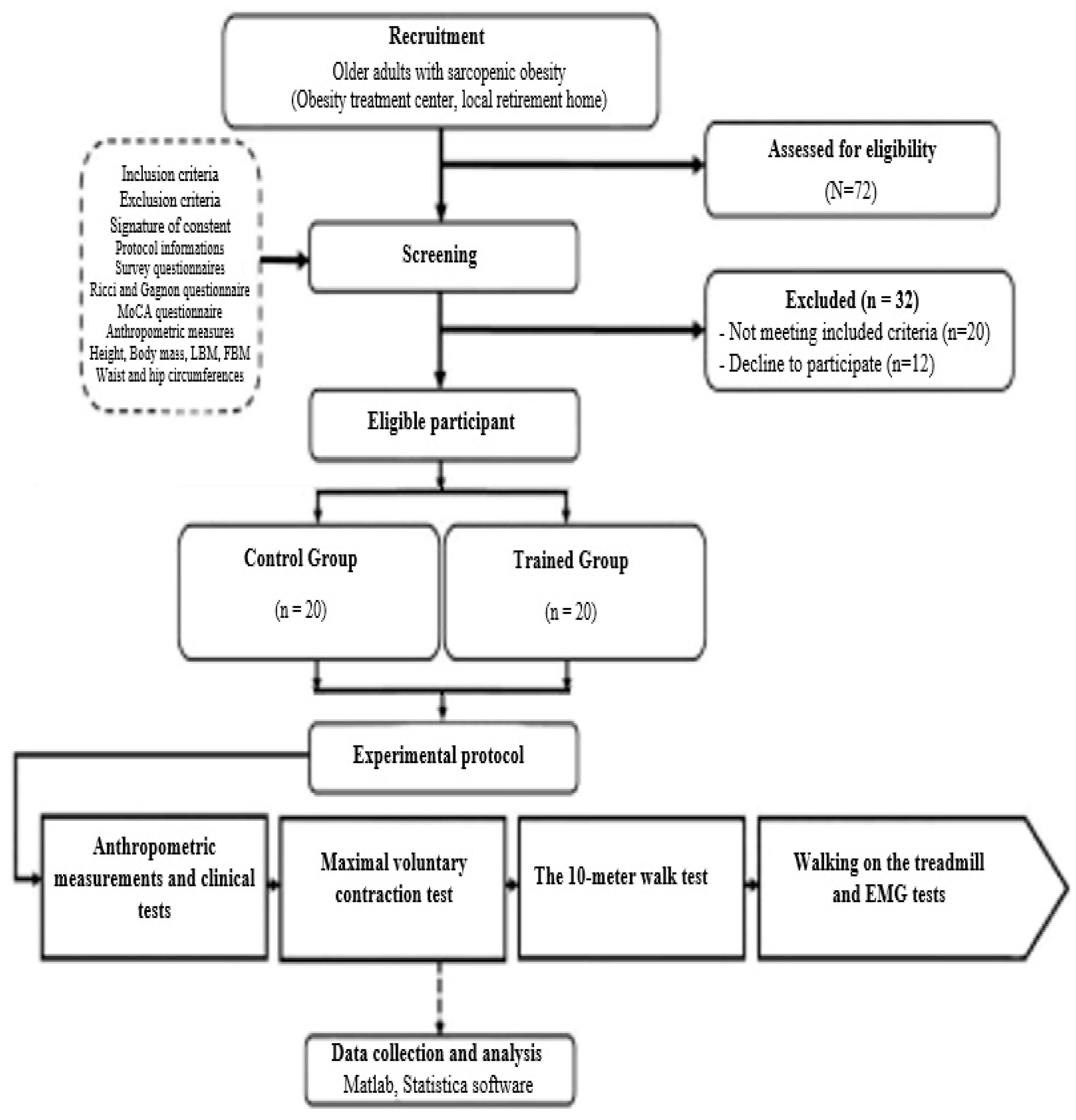
This study was a multicenter randomized controlled trial in which participants were allocated to either the trained group (TG) or the control group (CG) (
Figure 1). CG did not receive any intervention but underwent before- and after-evaluation tests. TG received a 6-month program consisting of two sessions per week. The study followed a standardized recruitment process, with a 3-week recruitment period, a 1-week screening period, and a 3-week experimental testing period before and after the intervention. During before and after evaluations, participants underwent a standardized assessment protocol consisting of 5 assessments, including anthropometric measurements, the walking test, the treadmill test, the maximal voluntary contraction test, and clinical evaluations.
2.2. Participants
2.2.1. Estimation of sample size
The sample size was calculated using the freeware G*Power (version 3.1.9.4)49. The ANOVA test was predefined for power analysis. The estimation was based on predefined control of type I error (alpha = 0.05) and Type II error (beta = 0.60), with a moderate level of estimated effect size (r = 0.35). Under these settings, 40 participants were required as the minimum sample size.
2.2.2. Recruitment
In the present study, we initially recruited a total of 72 volunteers from various obesity care centers located across the region. Based on the predetermined inclusion and exclusion criteria, only 52 participants met the eligibility requirements. Regrettably, due to non-adherence to the study protocol, 12 individuals were unable to complete the entire study as intended. A cohort of 40 participants who successfully completed the study in its entirety were randomly divided into two groups (
Table 1). The control group (CG; n = 20; age = 76.6 ± 5.6 years; BMI = 35.8 ± 2.7 kg/m²) and the trained group (TG; n = 20; age = 74.1 ± 3.7 years; BMI = 35.8 ± 2.7 kg/m²).To ensure that participants met the study’s inclusion criteria, they were required to have a BMI > 30 Kg/m², a Handgrip force (HF) <17 N, gait speed <1.0 m/s [
50], be over 65 years of age, able to verbally communicate with the experimenters, and physically independent. Exclusion criteria included the presence of neurological or cognitive impairments, severe cardiovascular problems, severe musculoskeletal deformities or injuries of the lower limb, comorbidities or chronic diseases, medication use that could interfere with testing, and a Montreal Cognitive Assessment (MoCA) test score of <26. To verify that participants met the criteria, they completed a survey questionnaire that assessed comorbidities, chronic diseases, falls history, medication use, physical independence, and levels of frailty. This information was also reviewed by medical staff at the facilities. Physical activity level and cognitive score were assessed using the Ricci and Gagnon [
51] and the MoCA tests [
52]. Before the study began, each participant provided written informed consent. The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee (C.P.P. SOUTH /No. 0477/2022). Participant confidentiality and data privacy was strictly maintained throughout the study, and all data was analyzed in an aggregated and anonymous manner to ensure the anonymity of participants.
2.3. Intervention: PSM program
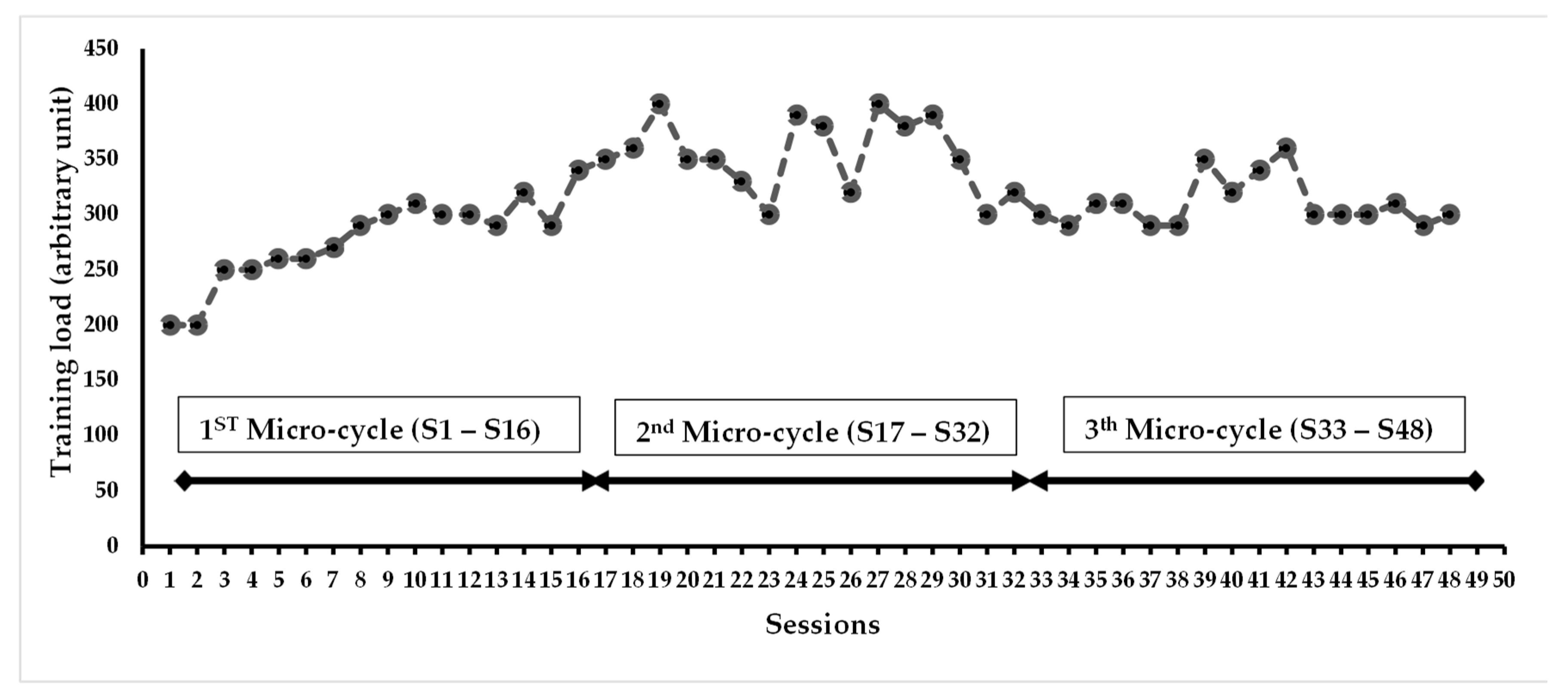
The PSM program spanned over 24 weeks and consisted of 2 sessions of 60 minutes each week, for a total of 48 sessions. The program’s progressiveness was based on two aspects: a quantitative aspect related to the training load (volume/intensity) and a qualitative aspect related to the type of exercises (muscle strengthening, balance, and motor skills exercises). According to the quantitative aspect, the PSM program was structured into 3 micro-cycles of 16 sessions each: the first micro-cycle focused on volume, the second on intensity, and the third micro-cycle aimed to balance both volume and intensity (
Figure 1). The variation in training load was determined after each session, based on the perceived exercise level 53 using the rating of perceived exertion scale (RPE), The RPE scale ranges from 0 (no difficulty) to 10 (extremely difficult), and the training load of the group was calculated by multiplying the session’s RPE score by its duration (e.g., for a group with an average RPE score of 6 in a 60-minute session, the training load would be equal to 360 arbitrary units (µA). This method ensures the training’s efficiency, especially regarding the progression of solicitation, and allows for the monitoring of a possible overtraining syndrome. When the training load exceeded 300 µA (equivalent to 5 × 60 min), it was maintained for the next session. When the training load was below 300, the number of series and repetitions was increased by 25% in the next session. The training load evolution during the PSM program was measured in all participants (
Figure 1).
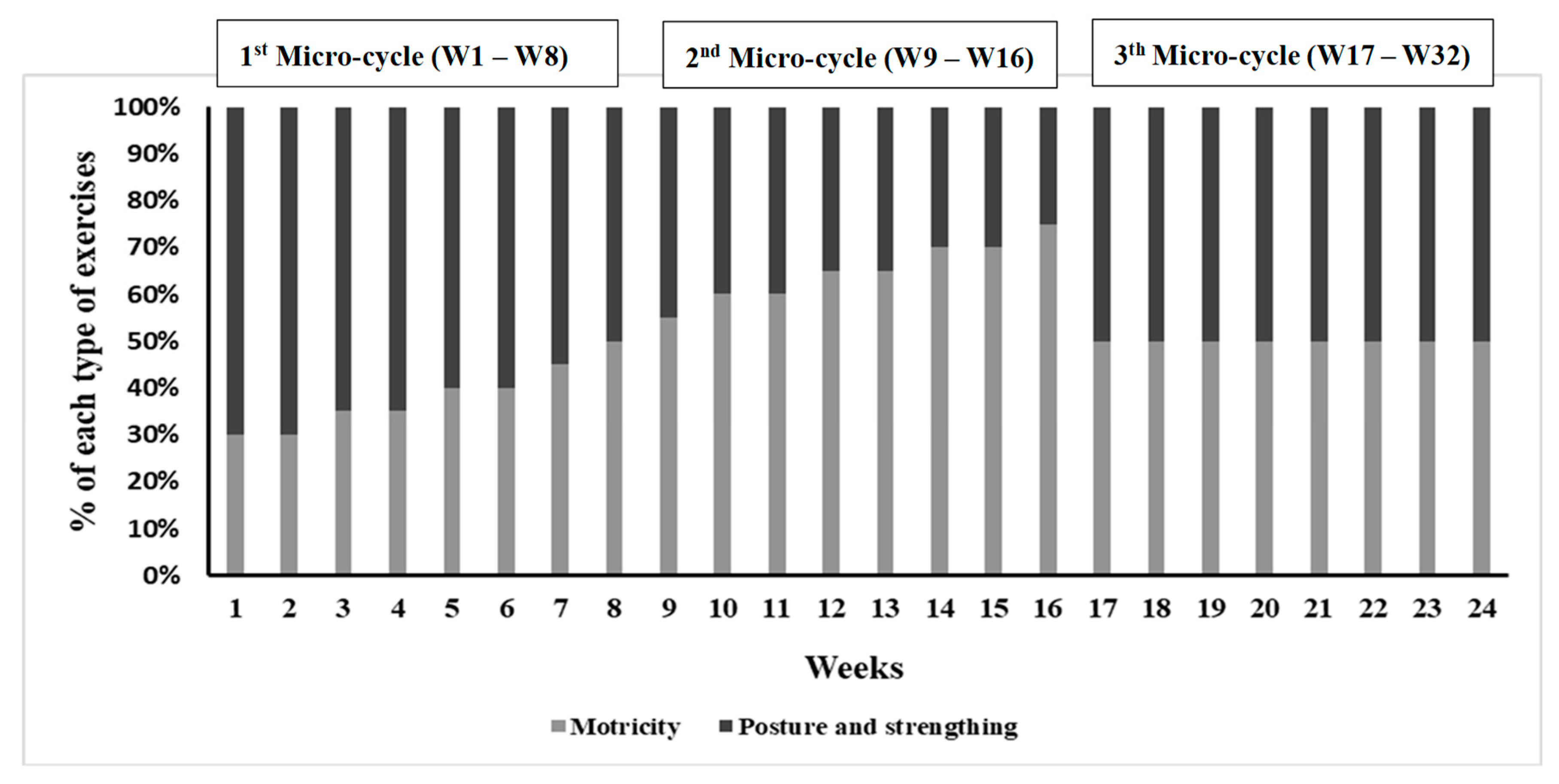
According to the qualitative aspect, the PSM program was divided into 3 micro-cycles based on the type of exercises. The first cycle mainly focused on motor skills exercises (50% to 70% of the session), the second on balance and muscle strengthening exercises, and the third cycle offered all types of exercises in a balanced way. The quantity of the different types of exercise was regulated every week (
Figure 2).
2.4. Evaluation Protocol
The evaluations described below were conducted in an identical manner and at the same time of day by the same experimenters before and after PSM program.
2.4.1. Anthropometric measurements and clinical tests
Anthropometric measurements were taken, including height (measured at the midpoint between the 12th rib and the iliac crest), waist circumference, and hip circumference (measured at the widest part of the hip) using a tape measure. Body weight (BW) and fat body mass (FBM, %) were measured using an impedance-meter (Tanita; SC 240-Class III; Tanita Europe B.V., Amsterdam, The Netherlands). FBM and lean body mass (LBM) were calculated using the equations from [
54]:
Then, participants were instructed to complete two walking trials in a 20-meter corridor to determine their preferred and maximal gait speed (m/s). To eliminate the acceleration and deceleration phases from the analysis, only the speed between the 5th and 15th meters was measured. Finally, the senior fitness test was performed as assessment tools to measure the physical performance of participants and detect any functional limitations.
2.4.2. Maximal voluntary contraction test
Isometric contractions of the ankle plantar flexors (PF) and dorsal flexors (DF) muscles of the dominant leg, maximal voluntary contractions (MVC) were recorded using a dynamometer (Sauter FL1K; Type: Force Gauge; Sauter GmbH, Balingen, Germany). Participants were instructed to keep their back, buttock, and thigh in contact with the chair and their leg stretched horizontally while pushing with the tips of the foot on the dynamometer for PF. For DF, participants were asked to stand up, keep their ankle at 90° and push with the foot on the dynamometer [
55]. To ensure stability, a strap was placed around the dominant leg and firmly secured to the foot plane during PF contractions. During each contraction, participants were strongly encouraged to provide maximal effort. Two trials were performed with a 1-minute rest in-between, and the mean of the single maximal value of the two trials was taken for both MVC of PF and DF. Relative force (MVC/LBM, N/Kg) was calculated according to Paolillo et al. [
56].
2.4.3. Walking test
Participants were familiarized with walking on an instrumented gait analysis treadmill (Zebris; FDM-T) for 5 minutes at their pre-calculated preferred walking speed previously measured, followed by a 2-minute seated rest period. If participants experienced any difficulty in walking on the treadmill, they were given an additional 2 minutes of training. Subsequently, participants performed three 1-minute trials, with each trial separated by a 5-minute seated rest period. Data were collected for a period of 10 seconds, starting at the 10th second of each trial. The treadmill software (Zebris, Suite FDM-T) sampled the gait parameters at 100 Hz from the treadmill force plates. These parameters included spatiotemporal parameters, walking cycle phases, GRFv, CoP displacements. Spatiotemporal parameters such as step length, step width, and stride length were recorded. The software divided the walking cycle into support phase (SU) and swing phase (SW), consisting of the 1st double support (1st DS), a single support (SS), and the 2nd double support (2nd DS). The absolute GRFv peaks were used to calculate the relative GRFv peaks (P1, P2, N/kg, respectively) by dividing the absolute value of the GRFv peak by the body mass. The CoP data were used to extract the CoP length during the SU and SS, the CoP anteroposterior position, and the CoP velocity during walking (cm/s).
2.4.4. Electromyography test
Electromyographic (EMG) data from ankle joint muscles were collected during MVC of PF and DF, and during a treadmill walking test using Trigno® Wireless Biofeedback System (Delsys Inc., Natick, MA). The EMG recording was synchronized with the treadmill data using a control device operating on the principle of a synchronization switch system (ON/OFF). The sensors composed of two pairs of silver bar contacts with 10 mm interelectrode spacing electrodes were placed on the gastrocnemius medialis (GM), soleus (SOL), and tibialis anterior (TA) of the dominant leg, conforming to the recommendations of SENIAM. The raw EMG signals were post-processed using Matlab software (Matlab R2013a, MathWorks, Natick, USA). The data from 10 strides were collected for a period of 10 seconds, in the 10th second of each trial (i.e., the same period of the treadmill recording), and were band-pass filtered at 15–500 Hz through a second-order Butterworth digital filter to remove noise or movement interference (Luca et al., 2010). The data were rectified and smoothed using root mean square analysis (RMS) with a 20-ms window38 and calculated using the following equation [
57]:
where T is the time of integration.
For the MVC tests, a moving window with a width of 20 ms was used to find the maximum RMS EMG activity resulting from the three efforts of MVC for each kind of contraction. Then, all RMS EMG data of walking on the treadmill test were normalized using the following equation for each muscle:
The normalized RMS of the GM (RMS GM), SOL (RMS SOL), and TA (EMG TA) of each walking cycle’s phase were used in the study.
2.5. Statistical analysis
The statistical analyses were conducted using Statistica Software 13.0 (Software, Inc., Tulsa, OK). The normality of the data distribution was checked using Kolmogorov-Smirnov tests. When the data distribution followed a normal distribution, paired t-tests were applied to compare the results of the same group before and after the PSM program. The independent samples t-test was also used to compare between the TG and CG before and after the PSM program. The relationships between the changes in gait parameters and the relative maximal force of the DF and PF, anthropometric parameters and muscle activity of GM, SOL and TA were evaluated using the Pearson’s correlation analysis. The data were expressed as means and standard deviations. The significance threshold was set at p < 0.05 for all results.
3. Results
The analysis of the Ricci and Gagnon questionnaire revealed that CG (10.9 ± 2.5) and TG (9.7 ± 3.4) were inactive before the PSM program. After the PSM program, TG showed a significant increase in LBM (+10%, p<0.05) and a decrease in FBM (-12.4%, p<0.05) (
Table 1). GT demonstrated improved physical performance in various exercises including arm flexion (+29.1%, p<0.01), sit-to-stand test (+45.5%, p<0.001), walking back and forth (-32.7%, p<0.01), 2-minute walk (+81%, p<0.001), and 2-minute knee lifts (+47.3%, p<0.001) (
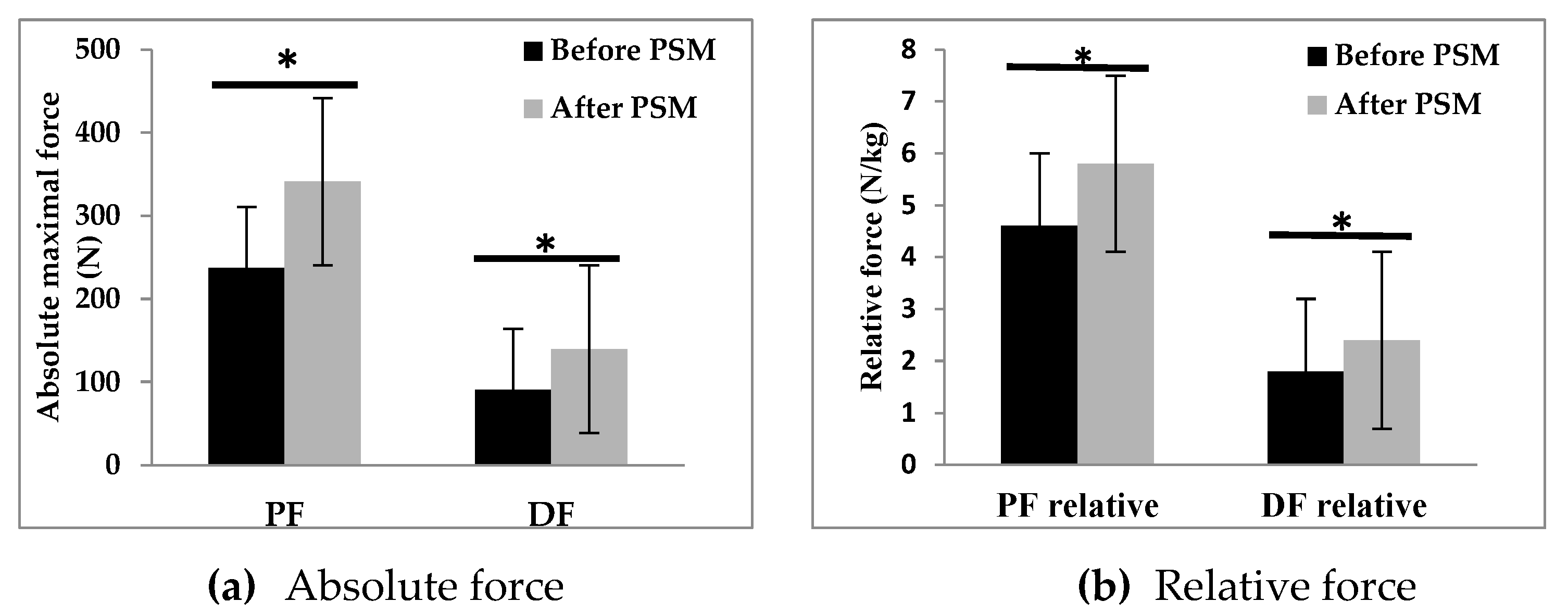
Table 2). The PSM program also resulted in an increase in absolute and relative maximal strength of plantar (+43%, +26%, p<0.05, respectively) and dorsiflexor (+54%, +33%, p<0.05, respectively) muscles (
Figure 4).
3.1. Gait parameters
The findings related to spatiotemporal parameters, gait cycle parameters, center of pressure displacement parameters, and vertical ground reaction forces are presented in
Table 3. Following the PSM program, TG exhibited significant improvements, including a remarkable increase in comfortable walking speed (+80%, p<0.001) and step length (+38%, p<0.05). The duration of the left and right stance phases decreased (-5%, -5%, respectively; p<0.05), while the durations of the left and right swing phases increased (+4.9%, +5%, respectively; p<0.05). Additionally, the durations of the initial left and right double stance phases (-4.1%, -4%, respectively) and the left and right pre-swing phases (-3%, -3%, respectively; p<0.05) decreased. Moreover, TG demonstrated a reduction in CoP velocity (-26%, p<0.01). Notably, TG also displayed increased GRFv in the left (+16%, p<0.05) and right (+14%, p<0.05) P1 forces, as well as the left (+24%, p<0.05) and right (+31%, p<0.05) P2 forces.
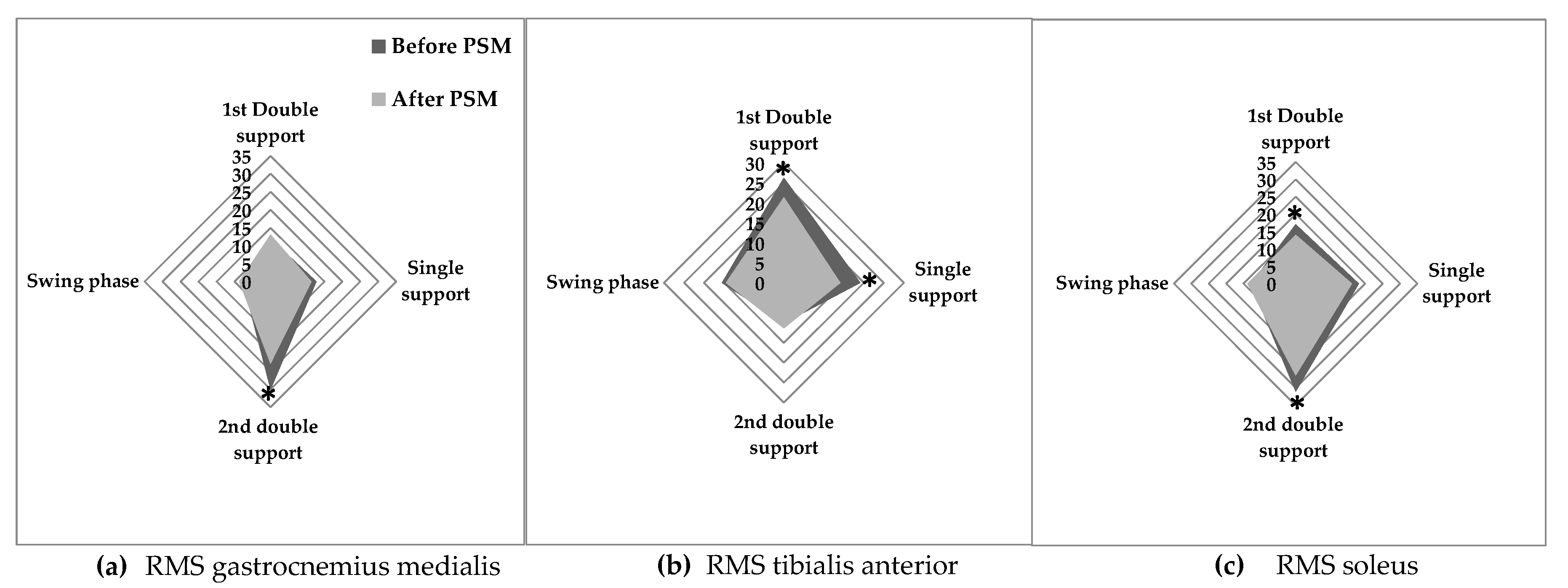
3.2. EMG muscle activity
after the PSM program, GT exhibited decreased GM activity during the 2
nd double support phase (-23.9%; p<0.01). Additionally, TA activity decreased during the 1
st double support phase (-18.6%; p<0.05) and single support phase (-26.6%; p<0.01), while muscle activity in SOL decreased during the 1
st stance phase (-17.5%; p<0.05) and 2
nd double support phase (-15.1%; p<0.05) (
Figure 5).
3.3. Pearson’s correlation analysis
The person correlation analysis revealed significant correlations between the changes in gait parameters and the evolution of neuromuscular parameters following the PSM program (
Table 4). Notably, positive correlations were found between the decrease in CoP velocity and the increase in relative force of PF (r = 0.61, p < 0.05) as well as DF (r = 0.63, p < 0.05). Furthermore, a positive correlation was observed between the decrease in CoP velocity and the reduction in RMS SOL (r = 0.57, p < 0.05) and RMS TA (r = 0.54, p < 0.05). Additionally, a positive correlation was identified between the increase in relative P1 and the relative DF force (r = 0.57, p < 0.05). A positive correlation was also found between relative P2 and the increase in DF force.
4. Discussion
The objective of this study was to evaluate the impact of a physical activity program based on muscle strengthening, balance, and motor exercises on body composition, physical performance, neuromuscular capacities, and biomechanical gait parameters in older adults with SO. The results indicate that the PSM program improved walking Ability and functional capacities in this population. These improvements were associated with an improvement in neuromuscular capacities.
4.1. Body composition
Our study contributes to the existing body of literature [
43,
46,
47] by demonstrating significant improvements in lean body mass (LBM) (+10%) and a decrease in fat body mass (FBM) (-12.4%) among participants in the intervention group after completing the PSM program. However, we did not observe significant impacts on BMI or body weight, which is consistent with previous studies that have explored the effects of different exercise modalities on body composition [
43,
46,
47,
50,
58]. The lack of significant changes in BMI and BW can be attributed to the substantial increase in LBM, which replaced FBM. This underscores the importance of considering body composition as a crucial indicator of the effectiveness of exercise programs, particularly in individuals with SO. Focusing solely on changes in BW or BMI may overlook the positive transformations occurring within the body, such as the development of LBM and the reduction of FBM. While some previous studies have also reported similar findings of non-significant changes in BMI and body weight [
43,
58] it is essential to recognize that the effects of exercise interventions can vary based on factors such as duration, intensity, and individual characteristics. Therefore, the absence of significant changes in these measures should not be interpreted as an indication of ineffectiveness but rather as a reflection of the specific adaptations occurring within the body, primarily the beneficial increase in lean muscle mass. Changing the body composition of individuals with SO presents significant challenges and complexities. It has been observed that individuals with OS may exhibit a blunted response to exercise, which can be attributed to poor insulin sensitivity [
59]. Poor insulin sensitivity is known to impair muscle protein breakdown and hinder muscle protein synthesis [
60]. The presence of obesity often accompanies a chronic inflammatory state and negatively influences the progression [
61]. Considering our findings, the effectiveness of our proposed program, including the specific modalities of intensity and frequency, can be considered as a promising approach in addressing these challenges.
4.2. Physical performance
Our study demonstrated significant improvements in various measures of physical performance following the implementation of the PSM program (
Table 2). Notably, the program led to a substantial increase in the relative maximal force of the plantar (+26%) and dorsal (+33%) flexors muscle. These findings are consistent with a previous study that reported enhanced mobility and functional performance in older adults with SO. Overall, our results suggest that the PSM program has the potential to enhance physical performance in individuals with SO through multiple mechanisms. Firstly, exercise has been shown to stimulate the secretion of insulin-like growth factor 1 (IGF-1), a potent anabolic hormone that promotes muscle maintenance and growth [
43,
47]. It is plausible that the proposed exercise interventions in our program significantly improve IGF-1 levels, thereby contributing to the observed improvements in muscle mass and function. Secondly, the improvements in physical performance observed in our study are likely associated with the increase in strength and lean body mass [
44,
62,
63].
4.3. Gait and neuromuscular capacities
To our knowledge, this study is the first to evaluate the effects of a physical activity program on neuromuscular capacities and their contribution to the improvement of walking abilities in older adults with SO. The results of this study showed that walking parameters, including preferred gait speed (+66%), maximal gait speed (+71%) and step length (+38%) in SO older adults were significantly improved after the PSM program and were associated with a reduction in the duration of the stance phase (-5%) and an increase in the duration of the swing phase (+4.9%). These improvements can be attributed to two possible mechanisms. First, the improvements in gait parameters could be attributed to a reduction in postural instability during walking. Maktouf et al. [
34], demonstrated that obese older adults exhibited higher CoP velocity and increased activity of TA during walking. The TA muscle plays a significant role in amortizing body mass during the first double support phase of walking. Interestingly, age appears to be a stronger predictor of increased TA activity in obese older adults [
34]. This adaptive neuromuscular response, which may serve as a compensatory mechanism, can be explained by age-related muscle postural control and somatosensory system alterations [
64]. The inclusion of specific balance exercises in our PES program likely played a crucial role in enhancing the participants’ balance capacities and stability during walking. This can be supported by the positive correlation observed between the decrease of CoP velocity and the SOL (r = 0.57) and TA (r = 0.54) activities among individuals with SO following the program. The decrease in CoP velocity indicates improved postural control, while the reduction in TA activity suggests a more efficient utilization of the muscle during walking. These outcomes further underscore the positive effects of the PES program on enhancing balance and stability, ultimately contributing to the improvements in gait among individuals with SO.
Secondly, the improvements in gait parameters observed in our study may be attributed to the enhanced neuromuscular capacities of the ankle muscles. Results showed a positive correlation between the increase of the relative PF and DF forces and the relative P2 (r = 0.73) and P1 (r = 0.71) in the TG. The increase of the GRFv during walking indicates improved force generation during the amortization (P1) and propulsion (P2) phases of walking. Notably, this increase in force generation was accompanied by a decrease in muscle activity of the GM (-23.9%) and SOL (-17.5%) during the first stance phase and propulsive phase, respectively. These findings suggest that the augmented maximal force production capacity of the plantar flexor muscles, achieved through muscle strengthening exercises, partially contributed to the enhancement of gait quality in older adults with SO. Specifically, obese older adults face difficulties in generating adequate force relative to their body mass during forward propulsion [
34]. Consequently, they tend to increase GM and SOL muscle activity during the propulsive phase of gait to manage the propulsive movement of their greater body mass and stabilize the excessive body mass during forward propulsion [
34]. The decrease in muscle activity was also observed in SOL during the first stance phase, where it acts as an antagonist muscle. This finding suggests a reduction in muscle coactivation among obese elderly individuals, which may contribute to a decrease in energy expenditure during walking [
65,
66]. By minimizing the coactivation of muscles during the first stance phase, individuals can optimize their movement efficiency and potentially reduce the metabolic demands associated with walking [
67]. Considering these observations, it can be inferred that the PSM program improved force production capacities through targeted strengthening exercises designed to counter the mechanical constraints imposed by obesity, such as mobilizing a significant body mass and addressing the sarcopenia-associated decline in force production.
Furthermore, it is crucial to recognize that the observed improvement in force production capacity, specifically the increased muscle strength of the ankle muscles, did not demonstrate a direct correlation with the enhancement of gait parameters, such as maximal speed and step length. This finding highlights the multifaceted nature of walking and suggests that solely focusing on developing greater muscle strength or improving postural control stability may not be sufficient to enhance the overall quality of walking [
68]. Walking involves a coordinated integration of various factors, including muscle strength, joint mobility, and postural control [
69]. While muscle strength is undoubtedly important for generating force during walking, other factors, such as joint range of motion, also play a critical role in determining walking capacity [
69,
70]. Joint mobility, particularly at the ankle joint, allows for a fluid and efficient stride, contributing to stride length and overall walking mechanics [
68,
71]. Therefore, it is plausible to consider that the motor exercises incorporated into the PES program, which specifically targeted joint range of motion and lower limb mobility, made significant contributions to the observed improvements in walking parameters. By addressing joint mobility and lower limb flexibility, these exercises likely facilitated a more optimal range of motion at the ankle joint, enabling smoother and more efficient gait patterns. This, in turn, could have positively influenced walking parameters such as stride length and step cadence.
4.4. Practical recommendations
Based on the findings of our study, the implementation of a physical activity program for frail populations, such as older adults with OS, should prioritize two key aspects. Firstly, it is crucial to tailor the quality of exercise to address the specific characteristics and impairments of each individual. This personalized approach is essential to directly target the identified alterations and promote effective interventions. Secondly, the quantitative aspect of the program should be based on patients’ perceived exertion, allowing for the prescription of an optimal exercise intensity for each individual. This approach ensures that patients do not work under fatigued conditions, which may yield negative outcomes. Moreover, it enables the provision of an appropriate intensity that adequately challenges the targeted systems, preventing the use of inefficient dosages that fail to elicit the necessary stimulation for adaptation. Moreover, Regular assessments throughout the program are essential to monitor progress and make necessary adjustments to the training load or exercise type, facilitating ongoing adaptation and optimal outcomes. Finally, it is vital to consider psychological and social factors, such as motivation, to ensure the continuity of physical activity practice among older adults. By creating a supportive and engaging environment, the program can foster sustained motivation, thereby promoting adherence and the continued benefits of physical activity for older adults with OS.
5. Conclusions
This study demonstrated that a physical activity program incorporating muscle strengthening, balance, and motor exercises had a positive impact on older adults with SO. The program effectively improved body composition, physical performance, gait, and neuromuscular capacities in this population. The improvement in walking ability can be attributed to the reduction of age- and obesity-related impairments. Despite the acute effects of aging and obesity, the study confirmed the trainability of neuromuscular capacities in older adults with SO, highlighting the potential for reversibility and improvement. Considering the reversibility of neuromuscular impairments, it is crucial to promote early intervention and sustained engagement in physical activity to maximize the potential for long-term improvements in mobility and independence. By integrating these findings into clinical practice and public health strategies, we can work towards optimizing the health and well-being of older adults with SO.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, H.F. and W.M.; methodology, H.F. and W.M.; software, H.F. and S.G.; validation, S.D, S.B. and S.D.; formal analysis, H.F. and S.G.; investigation, H.F.; data curation, W.M.; writing—original draft preparation, H.F.; writing—review and editing, H.F.; visualization, W.M.; supervision, S.G.; project administration, S.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of South Ethics Committee for the Protection Persons (C.P.P. SOUTH /No. 0477/2022, 2022/02/22).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data supporting the reported results of this study will be published on the Pan African Clinical Trials Registry after the publication of the article. Interested parties can access the data by referring to the registry once it becomes available.
Acknowledgments
We would like to extend our sincere appreciation to the medical staff and directors of the institutions where we recruited the participants for their valuable support and facilitation throughout this study. We would also like to express our gratitude to the patients who participated in this study. Their willingness to be involved and their cooperation during the data collection process have been crucial to the success of our research.
Conflicts of Interest
Authors must identify and declare any personal circumstances or interest that may be perceived as inappropriately influencing the representation or interpretation of reported research results. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Colleluori, G.; Villareal, D.T. Aging, obesity, sarcopenia and the effect of diet and exercise intervention. Exp. Gerontol. 2021, 155, 111561–111561. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Yu, K.; Shyh-Chang, N.; Jiang, Z.; Liu, T.; Ma, S.; Luo, L.; Guang, L.; Liang, K.; Ma, W.; et al. Pathogenesis of sarcopenia and the relationship with fat mass: descriptive review. J. Cachex- Sarcopenia Muscle 2022, 13, 781–794. [Google Scholar] [CrossRef]
- Zamboni, M.; Rubele, S.; Rossi, A.P. Sarcopenia and obesity. Curr. Opin. Clin. Nutr. Metab. Care 2019, 22, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Kopelman, P.G. Obesity as a medical problem. Nature 2000, 404, 635–643. [Google Scholar] [CrossRef]
- Bray, G.A. Medical Consequences of Obesity. J. Clin. Endocrinol. Metab. 2004, 89, 2583–2589. [Google Scholar] [CrossRef]
- Liao, C.-D.; Chen, H.-C.; Liou, T.-H.; Lin, C.-L.; Huang, S.-W. Impact of Sarcopenia and Obesity on Gait Speed After Total Knee Replacement. J. Am. Med Dir. Assoc. 2022, 23, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.-D.; Huang, S.-W.; Huang, Y.-Y.; Lin, C.-L. Effects of Sarcopenic Obesity and Its Confounders on Knee Range of Motion Outcome after Total Knee Replacement in Older Adults with Knee Osteoarthritis: A Retrospective Study. Nutrients 2021, 13, 3817. [Google Scholar] [CrossRef] [PubMed]
- Kalinkovich, A.; Livshits, G. Sarcopenic obesity or obese sarcopenia: A cross talk between age-associated adipose tissue and skeletal muscle inflammation as a main mechanism of the pathogenesis. Ageing Res. Rev. 2017, 35, 200–221. [Google Scholar] [CrossRef]
- Bilski, J.; Pierzchalski, P.; Szczepanik, M.; Bonior, J.; Zoladz, J.A. Multifactorial Mechanism of Sarcopenia and Sarcopenic Obesity. Role of Physical Exercise, Microbiota and Myokines. Cells 2022, 11, 160. [Google Scholar] [CrossRef]
- Wearing, S.C.; Hennig, E.M.; Byrne, N.M.; Steele, J.R.; Hills, A.P. The biomechanics of restricted movement in adult obesity. Obes. Rev. 2006, 7, 13–24. [Google Scholar] [CrossRef]
- Frontera, W.R. Physiologic Changes of the Musculoskeletal System with Aging. Phys. Med. Rehabilitation Clin. North Am. 2017, 28, 705–711. [Google Scholar] [CrossRef]
- Ortega, J.D.; Farley, C.T. Effects of aging on mechanical efficiency and muscle activation during level and uphill walking. J. Electromyogr. Kinesiol. 2014, 25, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Frimenko, R.; Goodyear, C.; Bruening, D. Interactions of sex and aging on spatiotemporal metrics in non-pathological gait: a descriptive meta-analysis. Physiotherapy 2015, 101, 266–272. [Google Scholar] [CrossRef]
- Doherty, T.J. Invited Review: Aging and sarcopenia. J. Appl. Physiol. 2003, 95, 1717–1727. [Google Scholar] [CrossRef]
- Cunningham, C.; O’ Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef]
- van den Beld, A.W.; Kaufman, J.-M.; Zillikens, M.C.; Lamberts, S.W.J.; Egan, J.M.; Van Der Lely, A.J. The physiology of endocrine systems with ageing. Lancet Diabetes Endocrinol. 2018, 6, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Judith Campisi, Pankaj Kapahi, Gordon J Lithgow, Simon Melov, John C. Newman EV. Nature 2020, 571, 183–192. [CrossRef]
- Norman, K.; Haß, U.; Pirlich, M. Malnutrition in Older Adults—Recent Advances and Remaining Challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef] [PubMed]
- Tezuka, T.; Inoue, A.; Hoshi, T.; Weatherbee, S.D.; Burgess, R.W.; Ueta, R.; Yamanashi, Y. The MuSK activator agrin has a separate role essential for postnatal maintenance of neuromuscular synapses. Proc. Natl. Acad. Sci. 2014, 111, 16556–16561. [Google Scholar] [CrossRef]
- Li, L.; Xiong, W.-C.; Mei, L. Neuromuscular Junction Formation, Aging, and Disorders. Annu. Rev. Physiol. 2018, 80, 159–188. [Google Scholar] [CrossRef]
- Jepsen, D.B.; Robinson, K.; Ogliari, G.; Montero-Odasso, M.; Kamkar, N.; Ryg, J.; Freiberger, E.; Masud, T. Predicting falls in older adults: an umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr. 2022, 22, 1–27. [Google Scholar] [CrossRef]
- Chen, S.-H.; Chou, L.-S. Gait balance control after fatigue: Effects of age and cognitive demand. Gait Posture 2022, 95, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Macie, A.; Matson, T.; Schinkel-Ivy, A. Age affects the relationships between kinematics and postural stability during gait. Gait Posture 2023, 102, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, M.d.M.; Gouveia. R.; Gouveia, B.R.; Marques, A.; Martins, F.; Przednowek, K.; França, C.; Peralta, M.; Ihle, A. Associations of Gait Speed, Cadence, Gait Stability Ratio, and Body Balance with Falls in Older Adults. Int. J. Environ. Res. Public Heal. 2022, 19, 13926. [Google Scholar] [CrossRef]
- Kim, D.; Lewis, C.L.; Gill, S.V. The effect of obesity on whole-body angular momentum during steady-state walking. Gait Posture 2022, 94, 93–101. [Google Scholar] [CrossRef]
- Capodaglio, P.; Gobbi, M.; Donno, L.; Fumagalli, A.; Buratto, C.; Galli, M.; Cimolin, V. Effect of Obesity on Knee and Ankle Biomechanics during Walking. Sensors 2021, 21, 7114. [Google Scholar] [CrossRef]
- Deforche, B.I.; Hills, A.P.; Worringham, C.J.; Davies, P.S.W.; Murphy, A.J.; Bouckaert, J.J.; De Bourdeaudhuij, I.M. Balance and postural skills in normal-weight and overweight prepubertal boys. Pediatr. Obes. 2009, 4, 175–182. [Google Scholar] [CrossRef]
- Hue, O.; Simoneau, M.; Marcotte, J.; Berrigan, F.; Doré, J.; Marceau, P.; Marceau, S.; Tremblay, A.; Teasdale, N. Body weight is a strong predictor of postural stability. Gait Posture 2007, 26, 32–38. [Google Scholar] [CrossRef]
- Berrigan, F.; Simoneau, M.; Tremblay, A.; Hue, O.; Teasdale, N. Influence of obesity on accurate and rapid arm movement performed from a standing posture. Int. J. Obes. 2006, 30, 1750–1757. [Google Scholar] [CrossRef]
- Vankrunkelsven, W.; Derde, S.; Gunst, J.; Perre, S.V.; Declerck, E.; Pauwels, L.; Derese, I.; Berghe, G.V.D.; Langouche, L. Obesity attenuates inflammation, protein catabolism, dyslipidaemia, and muscle weakness during sepsis, independent of leptin. J. Cachex- Sarcopenia Muscle 2022, 13, 418–433. [Google Scholar] [CrossRef]
- Pérez-Torres, I.; Castrejón-Téllez, V.; Soto, M.E.; Rubio-Ruiz, M.E.; Manzano-Pech, L.; Guarner-Lans, V. Oxidative Stress, Plant Natural Antioxidants, and Obesity. Int. J. Mol. Sci. 2021, 22, 1786. [Google Scholar] [CrossRef]
- Al-Sulaiti, H.; Diboun, I.; Agha, M.V.; Mohamed, F.F.S.; Atkin, S.; Dömling, A.S.; Elrayess, M.A.; Mazloum, N.A. Metabolic signature of obesity-associated insulin resistance and type 2 diabetes. J. Transl. Med. 2019, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.M.; Perrard, X.-Y.; Brunner, G.; Lui, H.; Sparks, L.M.; Smith, S.R.; Wang, X.; Shi, Z.-Z.; E Lewis, D.; Wu, H.; et al. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int. J. Obes. 2015, 39, 1607–1618. [Google Scholar] [CrossRef] [PubMed]
- Maktouf, W.; Durand, S.; Boyas, S.; Pouliquen, C.; Beaune, B. Interactions among obesity and age-related effects on the gait pattern and muscle activity across the ankle joint. Exp. Gerontol. 2020, 140, 111054. [Google Scholar] [CrossRef]
- Máximo, R.d.O.; de Oliveira, D.C.; Ramírez, P.C.; Luiz, M.M.; de Souza, A.F.; Delinocente, M.L.B.; Steptoe, A.; de Oliveira, C.; Alexandre, T.d.S. Dynapenia, abdominal obesity or both: which accelerates the gait speed decline most? Age Ageing 2021, 50, 1616–1625. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Jiang, J.; Hao, Q.; Luo, L.; Dong, B. Dynapenic Obesity and Lower Extremity Function in Elderly Adults. J. Am. Med Dir. Assoc. 2014, 16, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Gorniak, S.L. Obesity Is Associated With Gait Alterations and Gait Asymmetry in Older Adults. Mot. Control. 2023, 27, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Maktouf, W.; Durand, S.; Boyas, S.; Pouliquen, C.; Beaune, B. Combined effects of aging and obesity on postural control, muscle activity and maximal voluntary force of muscles mobilizing ankle joint. J. Biomech. 2018, 79, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Melzer, I.; Oddsson, L.I. Altered characteristics of balance control in obese older adults. Obes. Res. Clin. Pr. 2015, 10, 151–158. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Agosti, F.; Proietti, M.; Riva, D.; Resnik, M.; Lafortuna, C.L.; Sartorio, A. Postural instability of extremely obese individuals improves after a body weight reduction program entailing specific balance training. J. Endocrinol. Investig. 2005, 28, 2–7. [Google Scholar] [CrossRef]
- Theodorakopoulos, C.; Jones, J.; Bannerman, E.; Greig, C.A. Effectiveness of nutritional and exercise interventions to improve body composition and muscle strength or function in sarcopenic obese older adults: A systematic review. Nutr. Res. 2017, 43, 3–15. [Google Scholar] [CrossRef]
- Hita-Contreras, F.; Bueno-Notivol, J.; Martínez-Amat, A.; Cruz-Díaz, D.; Hernandez, A.V.; Pérez-López, F.R. Effect of exercise alone or combined with dietary supplements on anthropometric and physical performance measures in community-dwelling elderly people with sarcopenic obesity: A meta-analysis of randomized controlled trials. Maturitas 2018, 116, 24–35. [Google Scholar] [CrossRef]
- Hsu, K.-J.; Liao, C.-D.; Tsai, M.-W.; Chen, C.-N. Effects of Exercise and Nutritional Intervention on Body Composition, Metabolic Health, and Physical Performance in Adults with Sarcopenic Obesity: A Meta-Analysis. Nutrients 2019, 11, 2163. [Google Scholar] [CrossRef]
- Maktouf, W.; Durand, S.; Beaune, B.; Boyas, S. Influence of Obesity and Impact of a Physical Activity Program on Postural Control and Functional and Physical Capacities in Institutionalized Older Adults: A Pilot Study. J. Phys. Act. Heal. 2020, 17, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Chiu, S.-C.; Yang, R.-S.; Yang, R.-J.; Chang, S.-F. Effects of resistance training on body composition and functional capacity among sarcopenic obese residents in long-term care facilities: a preliminary study. BMC Geriatr. 2018, 18, 21. [Google Scholar] [CrossRef]
- Park, J.; Kwon, Y.; Park, H. Effects of 24-Week Aerobic and Resistance Training on Carotid Artery Intima-Media Thickness and Flow Velocity in Elderly Women with Sarcopenic Obesity. J. Atheroscler. Thromb. 2017, 24, 1117–1124. [Google Scholar] [CrossRef]
- WANG LZ, GUO YB, LOU JH. Effects of Home Exercise on Sarcopenia Obesity for Aging People. Chinese J Rehabil Theory Pract. 2019, 90–96. [CrossRef]
- Liao, C.-D.; Tsauo, J.-Y.; Lin, L.-F.; Huang, S.-W.; Ku, J.-W.; Chou, L.-C.; Liou, T.-H. Effects of elastic resistance exercise on body composition and physical capacity in older women with sarcopenic obesity. Medicine 2017, 96, e7115. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Kim, H.; Kim, M.; Kojima, N.; Fujino, K.; Hosoi, E.; Kobayashi, H.; Somekawa, S.; Niki, Y.; Yamashiro, Y.; Yoshida, H. Exercise and Nutritional Supplementation on Community-Dwelling Elderly Japanese Women With Sarcopenic Obesity: A Randomized Controlled Trial. J. Am. Med Dir. Assoc. 2016, 17, 1011–1019. [Google Scholar] [CrossRef]
- Reichhart, K.; Evesque, M.; Cavana, M.M.; Muszynski, P.; Leclercq, M.-M.; Winisdoerffer, N.; Sonntag, M. How to promote physical activity maintenance after an exercise-training program in cancer patients? Ann. Phys. Rehabilitation Med. 2016, 59, e55. [Google Scholar] [CrossRef]
- Ciesielska, N.; Sokołowski, R.; Mazur, E.; Podhorecka, M.; Polak-Szabela, A.; Kędziora-Kornatowska, K. Is the Montreal Cognitive Assessment (MoCA) test better suited than the Mini-Mental State Examination (MMSE) in mild cognitive impairment (MCI) detection among people aged over 60? Meta-analysis. Psychiatr. Polska 2016, 50, 1039–1052. [Google Scholar] [CrossRef]
- Foster, C. Monitoring training in athletes with reference to overtraining syndrome. Med. Sci. Sports Exerc. 1998, 30, 1164–1168. [Google Scholar] [CrossRef]
- Gartner, A.; Dioum, A.; Delpeuch, F.; Maire, B.; Schutz, Y. Use of hand-to-hand impedancemetry to predict body composition of African women as measured by air displacement plethysmography. Eur. J. Clin. Nutr. 2004, 58, 523–531. [Google Scholar] [CrossRef]
- Nagai, K.; Yamada, M.; Mori, S.; Tanaka, B.; Uemura, K.; Aoyama, T.; Ichihashi, N.; Tsuboyama, T. Effect of the muscle coactivation during quiet standing on dynamic postural control in older adults. Arch. Gerontol. Geriatr. 2013, 56, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Paolillo, F.R.; Milan, J.C.; Bueno, P.d.G.M.; Paolillo, A.R.M.; Borghi-Silva, A.; Parizotto, N.A.; Arena, R.; Kurachi, C.; Bagnato, V.S. Effects of excess body mass on strength and fatigability of quadriceps in postmenopausal women. Menopause 2012, 19, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-H.; Lee, P.-H.; Lin, L.-F.; Liao, C.-D.; Liou, T.-H.; Huang, S.-W. Effects of progressive elastic band resistance exercise for aged osteosarcopenic adiposity women. Exp. Gerontol. 2021, 147, 111272. [Google Scholar] [CrossRef] [PubMed]
- Nygren, J.; Nair, K.S. Differential Regulation of Protein Dynamics in Splanchnic and Skeletal Muscle Beds by Insulin and Amino Acids in Healthy Human Subjects. Diabetes 2003, 52, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Moller-Loswick, A.C.; Zachrisson, H.; Hyltander, A.; Korner, U.; Matthews, D.E.; Lundholm, K. Insulin selectively attenuates breakdown of nonmyofibrillar proteins in peripheral tissues of normal men. Am. J. Physiol. Metab. 1994, 266, E645–E652. [Google Scholar] [CrossRef] [PubMed]
- Wijesinghe, S.N.; Nicholson, T.; Tsintzas, K.; Jones, S.W. Involvements of long noncoding RNAs in obesity-associated inflammatory diseases. Obes. Rev. 2020, 22. [Google Scholar] [CrossRef] [PubMed]
- Cadore, E.L.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Idoate, F.; Millor, N.; Gómez, M.; Rodríguez-Mañas, L.; Izquierdo, M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. AGE 2014, 36, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Rossi-Izquierdo, M.; Santos-Pérez, S.; Faraldo-García, A.; Vaamonde-Sánchez-Andrade, I.; Gayoso-Diz, P.; Del-Río-Valeiras, M.; Lirola-Delgado, A.; Soto-Varela, A. Impact of obesity in elderly patients with postural instability. Aging Clin. Exp. Res. 2015, 28, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Blaszczyk, J.; Lowe, D.; Hansen, P. Ranges of postural stability and their changes in the elderly. Gait Posture 1994, 2, 11–17. [Google Scholar] [CrossRef]
- Cattagni, T.; Scaglioni, G.; Laroche, D.; Van Hoecke, J.; Gremeaux, V.; Martin, A. Ankle muscle strength discriminates fallers from non-fallers. Front. Aging Neurosci. 2014, 6, 336. [Google Scholar] [CrossRef] [PubMed]
- Laroche, D.P.; Marques, N.R.; Shumila, H.N.; Logan, C.R.; Laurent, R.S.; Gonçalves, M. Excess Body Weight and Gait Influence Energy Cost of Walking in Older Adults. Med. Sci. Sports Exerc. 2015, 47, 1017–1025. [Google Scholar] [CrossRef]
- Peyrot, N.; Morin, J.-B.; Thivel, D.; Isacco, L.; Taillardat, M.; Belli, A.; Duche, P. Mechanical Work and Metabolic Cost of Walking after Weight Loss in Obese Adolescents. Med. Sci. Sports Exerc. 2010, 42, 1914–1922. [Google Scholar] [CrossRef]
- Hortobágyi, T.; DeVita, P. Muscle pre- and coactivity during downward stepping are associated with leg stiffness in aging. J. Electromyogr. Kinesiol. 2000, 10, 117–126. [Google Scholar] [CrossRef]
- Nene, A.; Mayagoitia, R.; Veltink, P. Assessment of rectus femoris function during initial swing phase. Gait Posture 1999, 9, 1–9. [Google Scholar] [CrossRef]
- Paróczai R, Bejek Z, Illyés Á. Gait parameters of healthy, elderly people. Phys Educ Sport. 2006, 4, 49–58.
- Winter, D.A.; Patla, A.E.; Frank, J.S.; Walt, S.E. Biomechanical Walking Pattern Changes in the Fit and Healthy Elderly. Phys. Ther. 1990, 70, 340–347. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).