Introduction
Haemophilus influenzae is one of causative agent of invasive bacterial pathogen that affects both children and adults [
1]. It was once the main cause of meningitis and other diseases of respiratory systems, but because of extremely efficient conjugate vaccine, the frequency of meningitis brought this bacterium has significantly decreased. It continues to be a significant contributor to childhood sepsis, otitis media, sinusitis, conjunctivitis, and other upper respiratory tract infections. Adults World Health Organization (WHO) have chronic obstructive pulmonary disease are particularly at risk for pneumonia because of invasive
H.influenzae diseases [
1,
2].
The pleomorphic, Gram-negative coccobacillus H.influenzae is commonly found in the upper respiratory tract. It's a pathogen that only affects humans and is known to live in healthy people's nasopharynx and oropharynx. It can cause serious invasive sickness [
3,
4]. They are restricted human pathogens that include H. influenzae strains classified encapsulated (a-f) and unencapsulated or non-typeable (NTHi). The genetically varied NTHi strain can invade the nasopharynx and cause local mucosal infections, while encapsulated serotypes can also result in invasive illness [
5,
6].
In contrast, non-type b H. influenzae typically causes opportunistic infections. H.influenzae type b (Hib) caused >80% of invasive infections, mostly in healthy children under the age of five. The NTHi generates a significant amount of H. influenza infections even though Hib strains are thought to be the more harmful since they also cause a significant amount of noninvasive infections including otitis media and sinusitis [
4,
5,
7,
8].
Presently, NTHi is the primary cause of invasive H. influenzae disease in the European Union or European Economic Area (EU/EEA) and other parts of the world. The extra growth factors X factor (hemin) and V factor (nicotinamide adenine dinucleotide) are required for the fastidious Gram-negative coccobacilli Haemophilus species, maybe in combination [
9]. Only humans carry H. influenzae, which colonizes their noses, throats, and, to a lesser extent, their conjunctivae and genital tracts [
10].
The World Health Organization lists H. influenzae as one of its top 12 priority pathogens because of its potential to spread serious invasive, fatal diseases. Vaccination programmes are in place in Ontario as well as other places, consequently, the prevalence of H. influenzae serotype b (Hib) infection is extremely low. But there is still a lack of knowledge regarding the epidemiology of non-Hib serotypes and nontypeable H. influenzae [
11].
H. influenzae pathogenesis is mediated by its antiphagocytic capsule and endotoxin, with most infections occurring in children aged 6 months to 6 years. NTHi subtypes lack these characteristics, allowing bacteria to proliferate more without an anti-capsular antibody. Research on host-pathogen interaction in NTHi patients is ongoing, with NTHi utilizing various host proteins to mediate colonization, maintain adhesion, and enter host cells. Protein D, present in all Haemophilus influenzae, affects ciliary function and increases the ability to generate otitis media, contributing to respiratory tract infections [
12].
A genomic study found that capsulated H. influenza strains cluster into serotype-specific clusters or clonal populations, while non-typeable strains exhibit significant genomic diversity [
13].
NTHi serotype are becoming significant invasive pathogens. Increased prevalence of H. influenzae non typeable as a major cause of invasive disease among Indigenous tribes in North America as a major cause of invasive disease in patient populations where infection is associated with high rates of morbidity and mortality [
14].
Nontypeable H. influenzae (NTHi) invasive infections have increased globally, with bacterial and pneumonia often linked to NTHi infection in adults. NTHi accounted for over 70% of all invasive H. influenzae disease in the US from 2008 to 2019 [
14,37,38,39]. The prevalence and pathogenicity of NTHi in serious lower respiratory diseases like pneumonia, bronchiectasis, cystic fibrosis, and chronic obstructive pulmonary disease are under increasing scrutiny. Typeable strains because systemic illnesses like meningitis, while NTHi lack a capsule and are primarily mucosal infections [
14,40]. On-typeable (NTHi) H. influenzae lack the CPS and cannot be categorized by serotyping. The number of invasive NTHi cases has increased globally. The invasive H. influenzae disease is still evolving, primarily in the elderly, and scientists are concerned about 76% of Hib cases among children who have received two or more doses of the vaccine [41,42,43].
H. influenzae non-b serotypes, such as type a (Hia), f(Hif), and e(Hie), are becoming significant invasive pathogens, particularly in Indigenous tribes in North America and in patient populations with high rates of morbidity and mortality [
8,
14,40]. Other non-Hib capsulated serotypes have also been reported as generating invasive infections over the past two decades. A bivalent Hia-Hib capsular polysaccharide-protein conjugate vaccine might provide defense against these two significant serotypes [
8]. Alaska and Northern Canada have reported high rates of Hia illness, particularly among Indigenous people. The capsule's structure, which includes three areas, is a significant virulence factor. A vaccine is needed to safeguard infants in these areas [
13,27].
Research on the lipooligosaccharide of H. influenzae has focused on its structural and compositional features for bacterial virulence [
1]. However, the function of LOS in activating innate and adaptive immunity is still poorly known. Encapsulated strains have a greater capacity to produce invasive illness due to the capsule inhibiting complement-mediated bacteriolysis [46]. The age distribution is attributed to a decline in maternal IgG in children and the inability to generate sufficient antibody against the polysaccharide capsular antigen until around 2 years. Effective Hib vaccines have been developed by covalently attaching the PRP capsule to a carrier protein, recruiting T-cell assistance for the polysaccharide immune response and stimulating anti-PRP antibody formation even in the first 6 months of life. H. influenzae is a common bacterium found in various respiratory illnesses, and various assays and techniques can be applied to measure the respiratory immune/inflammatory response. Adult patients with chronic renal failure are more likely to develop invasive Hib illness [46,47].
For this review. The most recent studies on the serotype epidemiology, pathobiology, molecular features, and immunology of the invasive H. influenzae disease have been assembled from all around the world. It also covers preventative measures, infection control methods, and risk factors for invasive infections.
2. Methods
2.1. Search STRATEGY
Since there aren't many articles before 2000, we restricted the publication period and examined invasive H.influenzae illness between 01, March 2000 to 01, March 2023. This systematic review was conducted using English databases, such as PubMed and Google Scholar, in order to fully extract all pertinent articles published worldwide.
The search method used exposure keywords like "Invasive Haemophilus", "Invasive Bacteria", "H.influenzae molecular character", "Hi genetic character", "Hi virulence factor", and "Hi Epidemiology" and result keywords like "Invasive Haemophilus Influenza", and "Hi pathogenesis".
Due to the numerous studies on these topics, we also included "Hi Immune response", "Hi Serotype OR", and "Hi Invasive strains" to our list of exposure terms. The references that matched the eligibility requirements were also read together with the full text.
2.2. Selection CRITERIA
We only considered empirical research with full-text available that was published in peer-reviewed journals; we excluded dissertations, conference proceedings, reviews, and commentary papers.
All publications were searched, but case reports, studies evaluating vaccines, non-human studies, and veterinary studies were excluded. The scope of our study was broadened to include the entire world because there hasn't been enough research on the burden of disease in every country. H.influenzae genetic characteristics, immune response, molecular characteristics and epidemiological studies were all reviewed, and laboratory studies on bacteria used in weak clinical evidence, vaccine trials conducted on specific patient’s immunity, population or genes that were only studied in vitro and without strong scientific support were excluded.
In order to provide a thorough summary of the research progress, we reviewed all studies of invasive H. influenzae disease, including global epidemiology, immune responses, and pathobiology, molecular and genetic character, which also discuss risk factors for invasive infection, prevention and control measures, and the need for further research or methodological gaps. A careful and relevant assessment of the epidemiology of invasive H. influenzae infections nowadays worldwide in several parts of the world is also provided in this paper.
2.3. Study SELECTION PROCESS
The Endnote version 21 reference management system was used to import and then eliminate duplicate entries for literature that was exclusively acquired from English-language databases.
The initial title screening was followed by an abstract screening to identify all retrieved studies. The World Health Organization (WHO) text was examined for eligibility if the information in titles or abstracts was insufficient to determine whether to include or exclude a study we also looked through each paper's references to see whether there were any other research that our database searches might have overlooked.
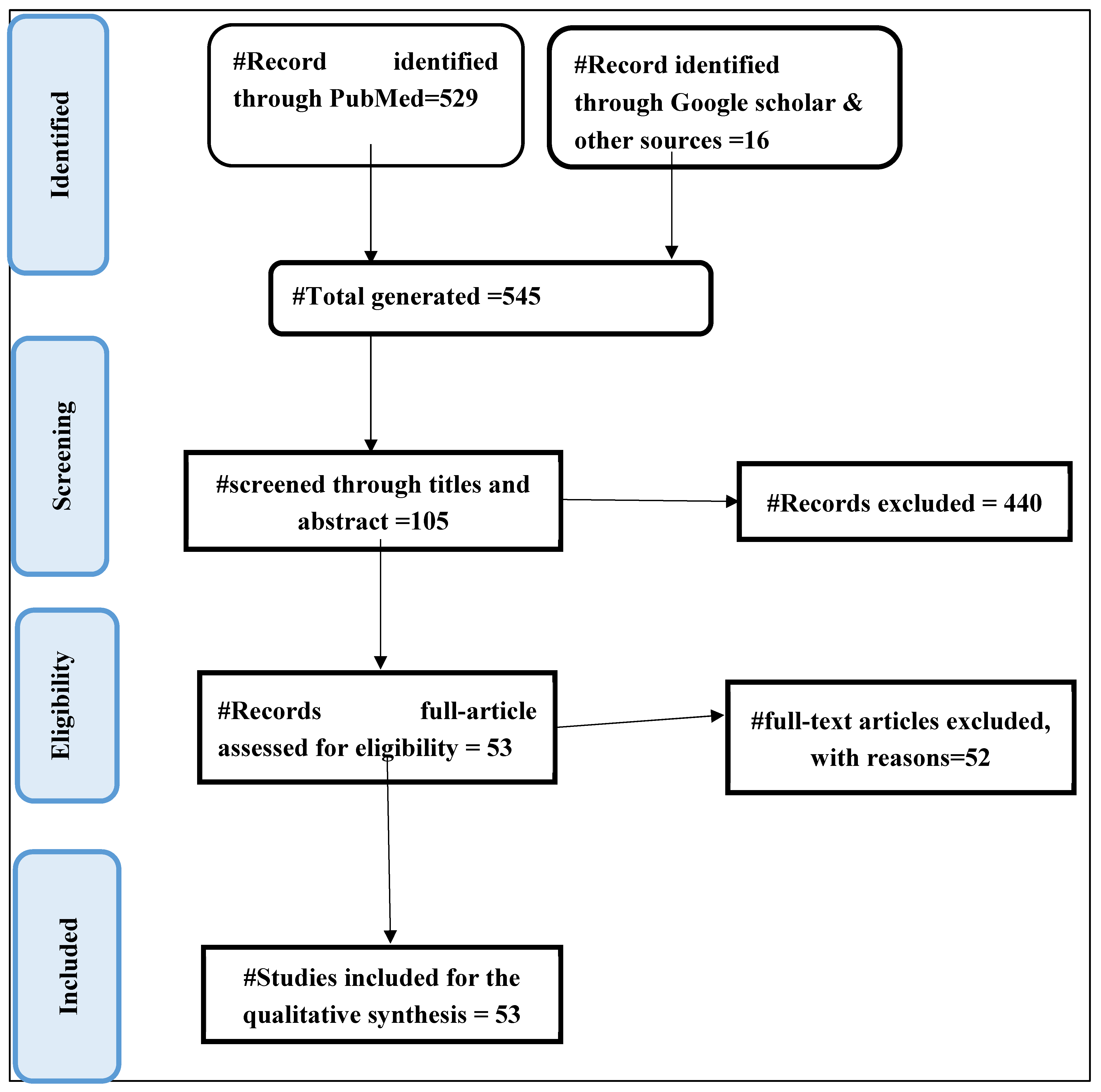
Figure 1 depicts the selection process for the study.
3. Global EPIDEMIOLOGY OF INVASIVE H. INFLUENZAE DISEASE
Before vaccinations were developed, the combined yearly average incidence of invasive Hib disease in children under the age of five was 40% for Asia, 41% for Europe, 60% for Latin America, and 88% for the United States [
14]. Due to the sporadic nature of the disease and the absence of global monitoring programmes that are systematic and thorough, the data on the global epidemiology of invasive
H.influenzae disease are insufficient.
H.influenzae disease infection is present in specific geographic regions and people, according to the examination of published studies on invasive Hia disease and Hia carriage. Currently, locations with a disproportionately high proportion of indigenous peoples, such as the North American Arctic, the Southwest of the United States, and northern and western Canada, have the greatest incidence rates of invasive Hia disease [
8,
15].
A considerable reduction in the prevalence of Hib disease has been observed everywhere the immunization has been used. In children under the age of five, Hib was estimated to have caused around 8.13 million cases of serious illness and 371,000 mortality annually. Between 2000 and 2015, there were 340,000 cases of Hib meningitis, pneumonia, and no pneumonic bacteremia in children under the age of five, with 29,800 deaths globally. Hib deaths decreased by 90% between 2000 and 2015. India was responsible for the majority of Hib-related mortality with 15,600 fatalities.3600 individuals were murdered in Nigeria.3400 people died in China, while 1000 died in South Sudan [
14].
Currently, only a small number of countries where Hib vaccination is either not freely available or is not available at all bear the burden of invasive Hib disease. High immunization rates and efficient surveillance programs for Hib disease are crucial for preventing the spread of invasive Hib disease [
8]. However, concerns were raised that other capsulated serotypes of H. influenzae might take over the ecological niche that Hib once occupied and develop into significant sources of invasive disease after the Hib vaccine was introduced. The highest incidence rates of invasive Haemophilus influenza disease have recently been discovered in various nations, including North America, Canada, and parts of Europe. The epidemiology of invasive
H. influenzae disease due to Hib strain has significantly changed since the Hib conjugate vaccine was launched more than 20 years ago [
16].
Native Americans in North America, Arctic Inuit and Eskimo, and Aboriginal Australians. Studies on population-based surveillance show that there are between 40 and 100 cases of invasive Hib illness per 100,000 children under the age of five in the USA. The annual incidence of H. influenzae meningitis was eight times greater among White Mountain Apache youngsters than in the US population as a World Health Organization (WHO)le. In Alaska, Eskimo children had an invasive Hib illness incidence that was 5.5 times greater than that of non-Native children. Although Hib was the predominant H. influenzae serotype that caused invasive disease globally, Hia was responsible for a number of cases in populations including White Mountain Apache Indians, Australian Aboriginals, and Papua New Guineans. More than 70% of instances of invasive H. influenzae illness are currently caused by NTHi [
17,
18].
Although invasive Hib diseases have significantly decreased as a result of the routine use of H.influenzae type b (Hib) conjugate vaccines, H. influenzae remains a significant cause of invasive disease, primarily sustained by non-vaccine preventable strains [
13].
Figure 2 shows Hib Vaccination coverage by World Health Organization (WHO) by the 2021.
The Hib vaccination has been introduced in all of the nations in the World Health Organization (WHO) Region of the Americas. In 2020, 85% of people have received the recommended three doses of the Hib vaccine. The recurrence of invasive Hi illness from 14 different countries. Of these isolates, 44% were caused by NTHi, 28% by Hib, and 7.9% by other capsulated serotypes [
14,23].
Between 2016 and 2018, Finland experienced 231 cases of invasive H. influenzae infection, with an annual frequency of 1.3 to 1.6/100,000 persons. The majority of the cases (79.2%) were NTHi, followed by Hif (12.6%), Hib (3.5%), and Hie (3.0%). Risky adults were those between the ages of 27 and 79. Invasive H. influenzae disease has an annual incidence of 0.28 per 100,000 people in Italy from 2017 to 2018, with a rate of 0.77 per 100,000 for children under the age of 5 (118). NTHi was responsible for the majority of instances (76.1%), whereas Hib and Hif each contributed 11.5% brought on by non-type b strains that have been observed in other parts of Europe, North America, and Australia [
14,
19].
Table 1 Shows Global Invasive H.influenzae trends since introduction of serotype b vaccine.
3.1. European REGION (EURO)
Nearly every country in the European World Health Organization (WHO) Region included the Hib vaccine in their suggested NIPs.Between 2007 and 2014, 12 European nations reported 10, 624 cases of invasive
H. influenzae infection. Information on the serotyping of 83% of the isolates was available. A population of 78% NTHi, 9% Hif, 3% Hie, and 9% Hib was present .Serotype information was available for 9,117 (80.5%) of the isolates, of which 10,081 instances of invasive
H. influenzae infection were reported based on data gathered and 4.6% [
14,24].
From 2011 to 2018, 260 invasive H. influenzae isolates were characterized in Portugal: The results show that NTHi 206 accounts for 79.2% of the sample, while Hib makes up 13.5%. Hif, Hia, and Hie each make up a smaller percentage, with 8, 7, and 4 occurrences respectively. The NTHi strains were mostly isolated from adults (78.2%), especially those over 65. H. influenzae infections in children were mainly caused by NTHi, accounting for 56.3%. Among the capsulated strains that caused infection in preschool-aged children, Hib, 7 Hia, 2 Hif, and 1 Hie were the majority [
14].
In France, a nation with a high Hib vaccination rate of 98% over the past ten years, the number of invasive Hib cases nearly doubled in 2018 from the previous year's average of 10 (94). At least 10 vaccine failures occurred, and the majority of instances involved children under the age of five. The most prevalent serotype in France was serotype f, while invasive isolates also contained serotypes b and a. A capsule switching event between serotypes B and C was suggested by Whole Genome Sequence analysis. There was significant heterogeneity in non-typeable isolates. According to reports, this area's hib vaccine failed [
14].
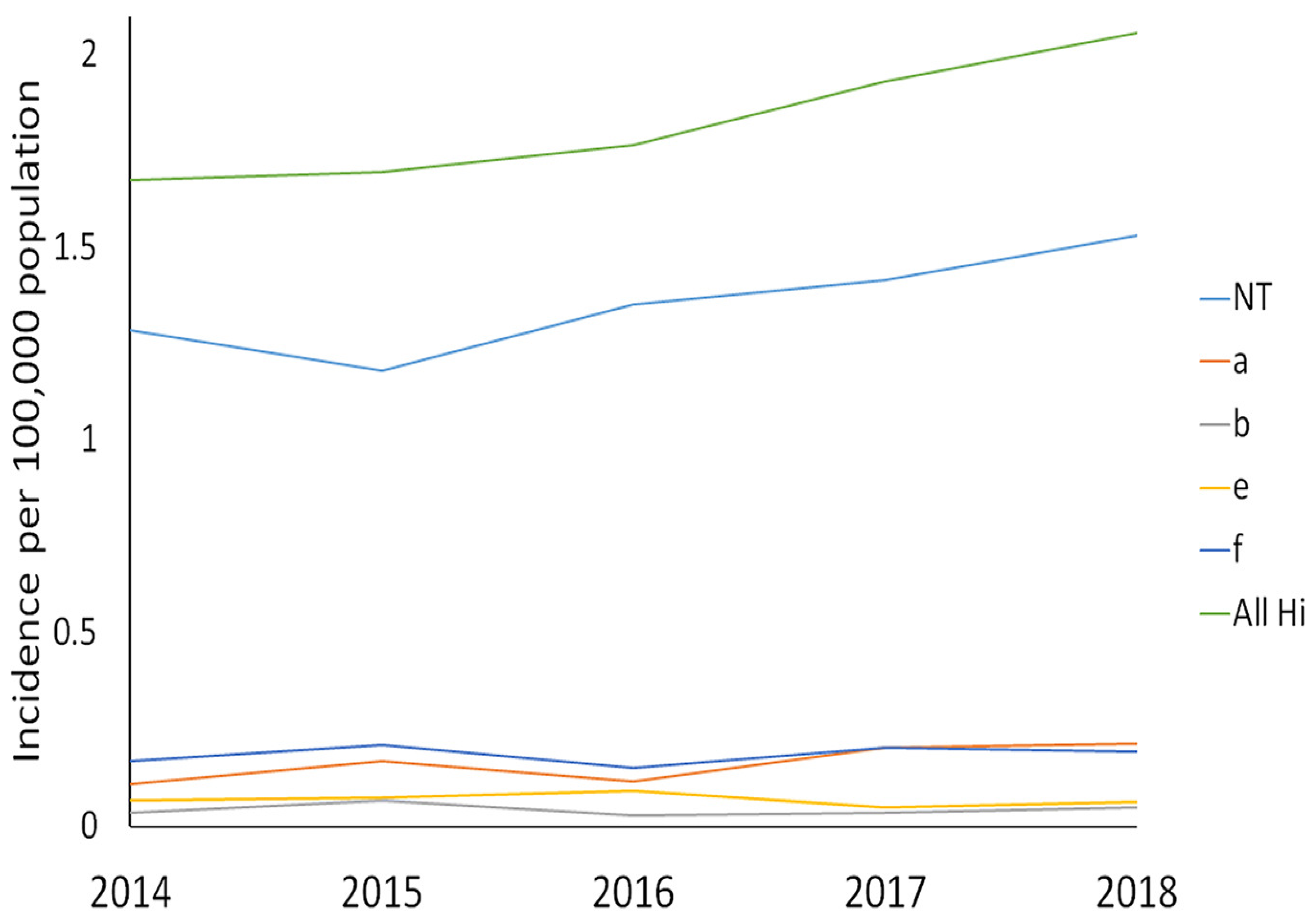
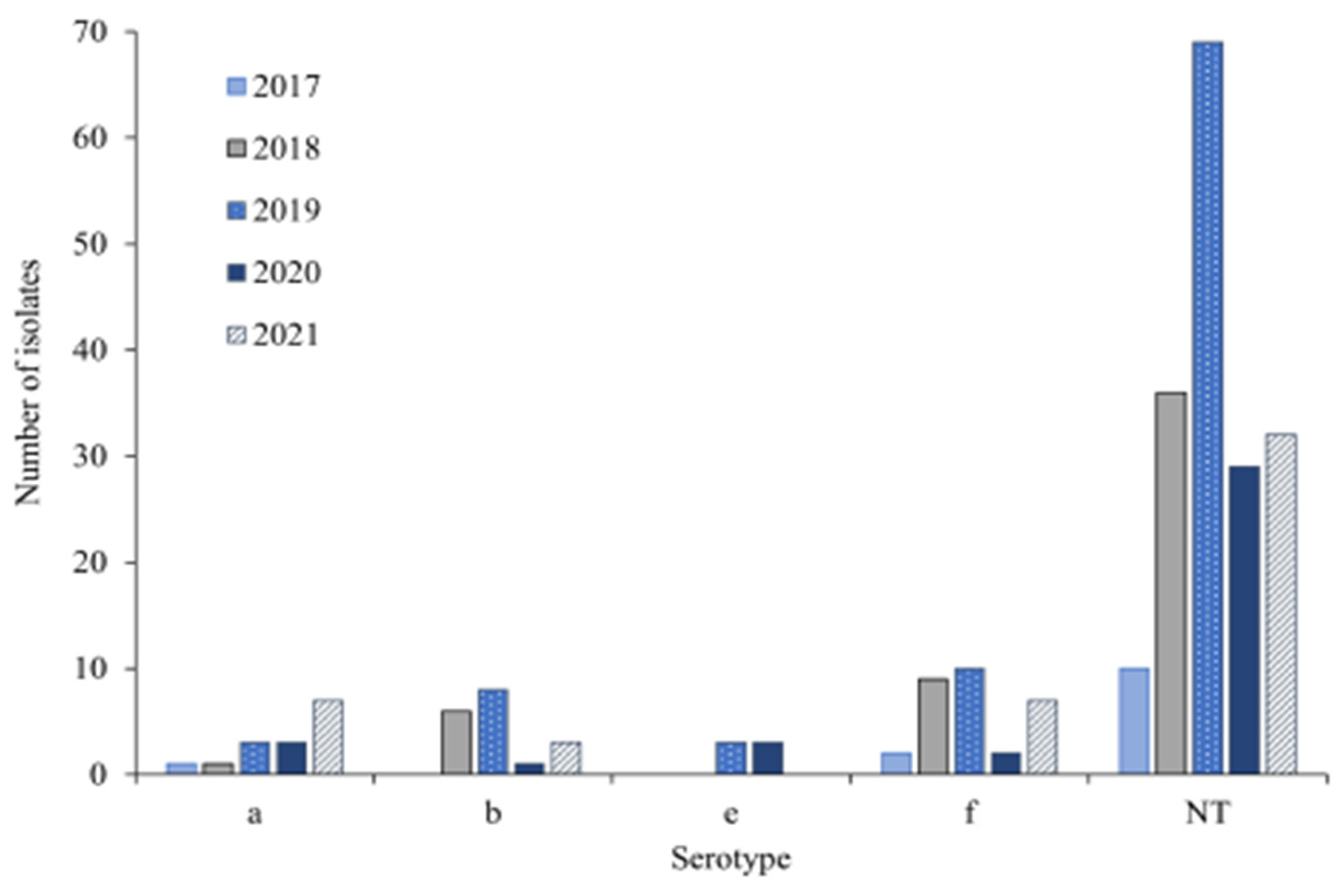
Figure 3 Shows Number of Hi Serotypes per year in 245 invasive H.influenzae isolates from Norway from 2017-2021 [
20,
21].
There were invasive Hib diseases in both Eastern Europe and Central Asia, but the data on their incidence are scarce.
3.2. African REGION (AFR)
In 2018, 327 cases of invasive H. influenzae infection were found by the South African monitoring programme (GERMS), of which 201 produced isolates for typing. 64% were NTHi, while 17% were Hib. Figure 7 Number of cases of invasive H.influenzae infection, by serotype, reported to National Institute of Communicable Diseases (NICD), South Africa, 2006 to 2018 [25] . Other capsulated serotypes made up 12% of the total. Hib isolates were In contrast to NTHi isolates, Hib isolates were more likely to come from meningitis cases. Children under the age of five had the highest prevalence of invasive H. influenzae infections (of all types), with adults between the ages of 25 and 44 seeing a second peak. The incidence of NTHi peaked in people over 65 years old, with babies experiencing the highest rates [
14].
The monitoring in Eastern Gambia found 57 cases of invasive H. influenzae infection, of which 42% were Hib, 30% NTHi, 18% Hia, 2 were Hic, Hid, Hie, or Hif, 2 failed to grow on cultures, and 2 were unrecoverable. While NTHi mainly manifested as bacteremia pneumonia, 14 of the Hib infections (58% of them) were cases of meningitis. NTHi has become a substantial cause of meningitis in Côte d'Ivoire, according to Boni-Cisse et al., which is interesting. The WORLD HEALTH ORGANIZATION (WHO) African Region's 47 member nations have all adopted Hib conjugate vaccines into their national immunization programmes (NIPs), and the average three-dose Hib coverage was 73% on average, with significant regional variation [
22,26].
Ethiopia introduced the NIP against H.influenzae and made the Hib conjugate vaccine accessible in 2007. In 2019, Ethiopia has a 68% hib3 coverage rate. The Hib immunization rate in Ethiopia was 50% in 2008.Children's meningitis and pneumonia are most frequently brought on by Hib in Ethiopia. The Federal Democratic Republic of Ethiopia's Ministry of Health has been working to provide these immunizations to Ethiopian children with cooperation from the WORLD HEALTH ORGANIZATION (WHO) Country Office [
14,27].
H.influenzae strain can cause Meningitis which is a major public health problem
All over the world. The African Meningitis Belt, which is known for its high risk of outbreaks of meningococcal and pneumococcal meningitis, is the region with the highest incidence of meningitis disease in Sub-Saharan Africa [28].
In this region, particularly Ethiopia, there is not enough of research associated with other H. influenzae encapsulated non-serotype b and NTHi strains. It is unknown how prevalent Hi disease is in Asia and Africa. Many African nations that have no comprehensive studies of invasive H influenzae illness or serotype data.
3.3. Region OF THE AMERICAS (AMR)
In this region, the prevalence of invasive H. influenzae is rising. H. influenzae serotypes and nontypeable H. influenzae must be evaluated for incidence and antibiotic susceptibility. Hib vaccination has been introduced in all countries in the WORLD HEALTH ORGANIZATION (WHO) Americas Region. In 2020, three doses of Hib vaccination provided 85% coverage In Navajo, White Mountain Apache, and Alaska Native children, the occurrence of invasive Hib illness was significantly higher. Among American Indian and Alaska Native youngsters, the prevalence of Hia disease has grown [
14,29].
Infections with Hia have also been reported in a number of Caribbean and South American nations, including Columbia, Venezuela, Argentina, and Cuba, with the majority of cases coming from Brazil. Salvador, Brazil, reported a rise in cases of Hia meningitis in children under the age of five during the first year of routine Hib immunization, although this does not seem to have persisted over the course of the following years. Following the implementation of the Hib vaccination in Paraguay, invasive Hib infections in children under the age of five decreased, but there was a corresponding rise in invasive NTHi infections in older children and adults. Other H. influenzae serotypes or NTHi have little information available [
14].
Invasive non-Hib illness has become more common over time; NTHi, Hif, and Hia are developing pathogens in this region. H.influenzae type a (Hia) has emerged as a serious source of severe invasive disease in Indigenous communities in North America. [
8].
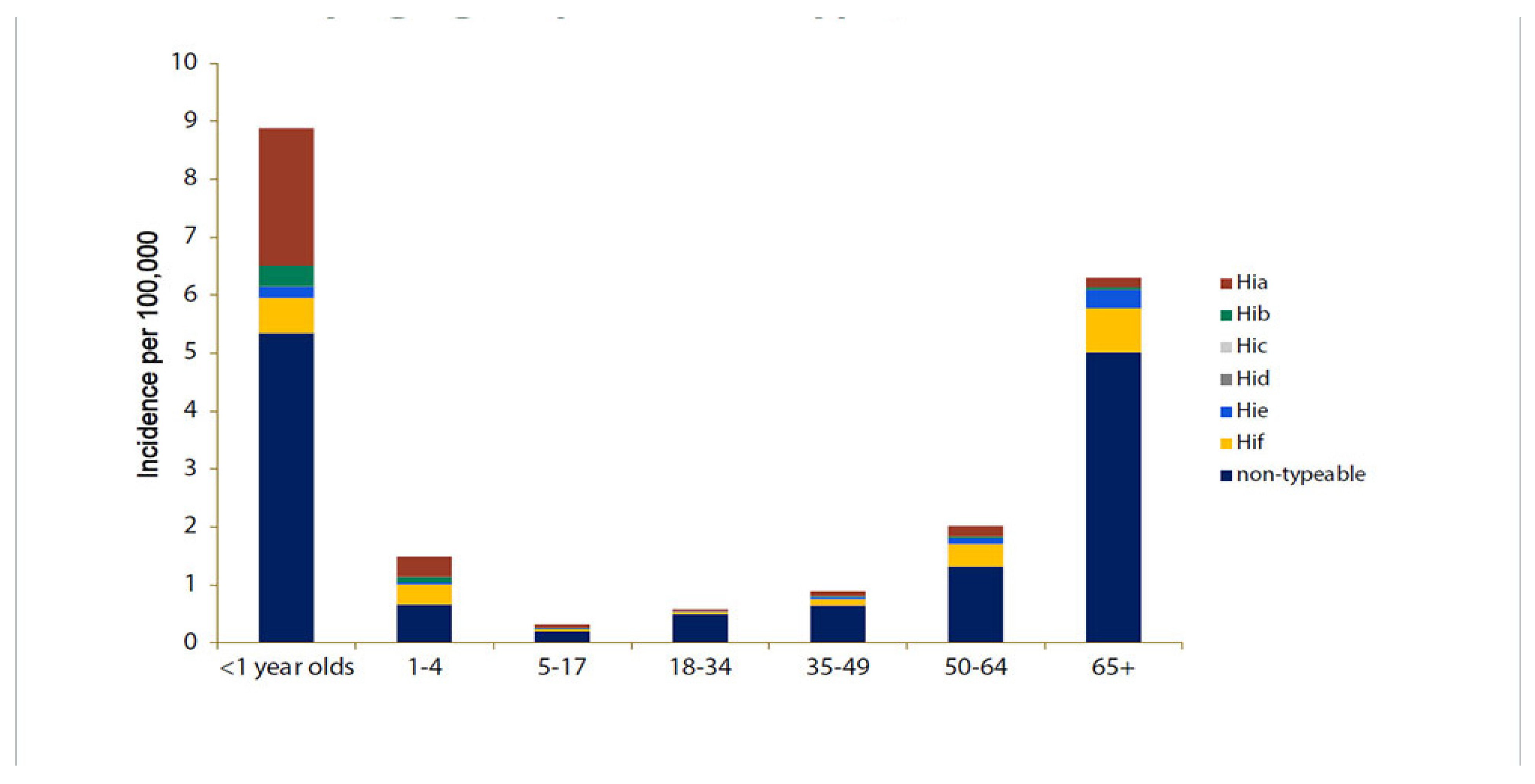
Figure 4 Depicts the estimated incidence rates (per 100,000 people) of invasive H. influenzae illness by serotype and age in the United States from 2016 to 2020 [28].
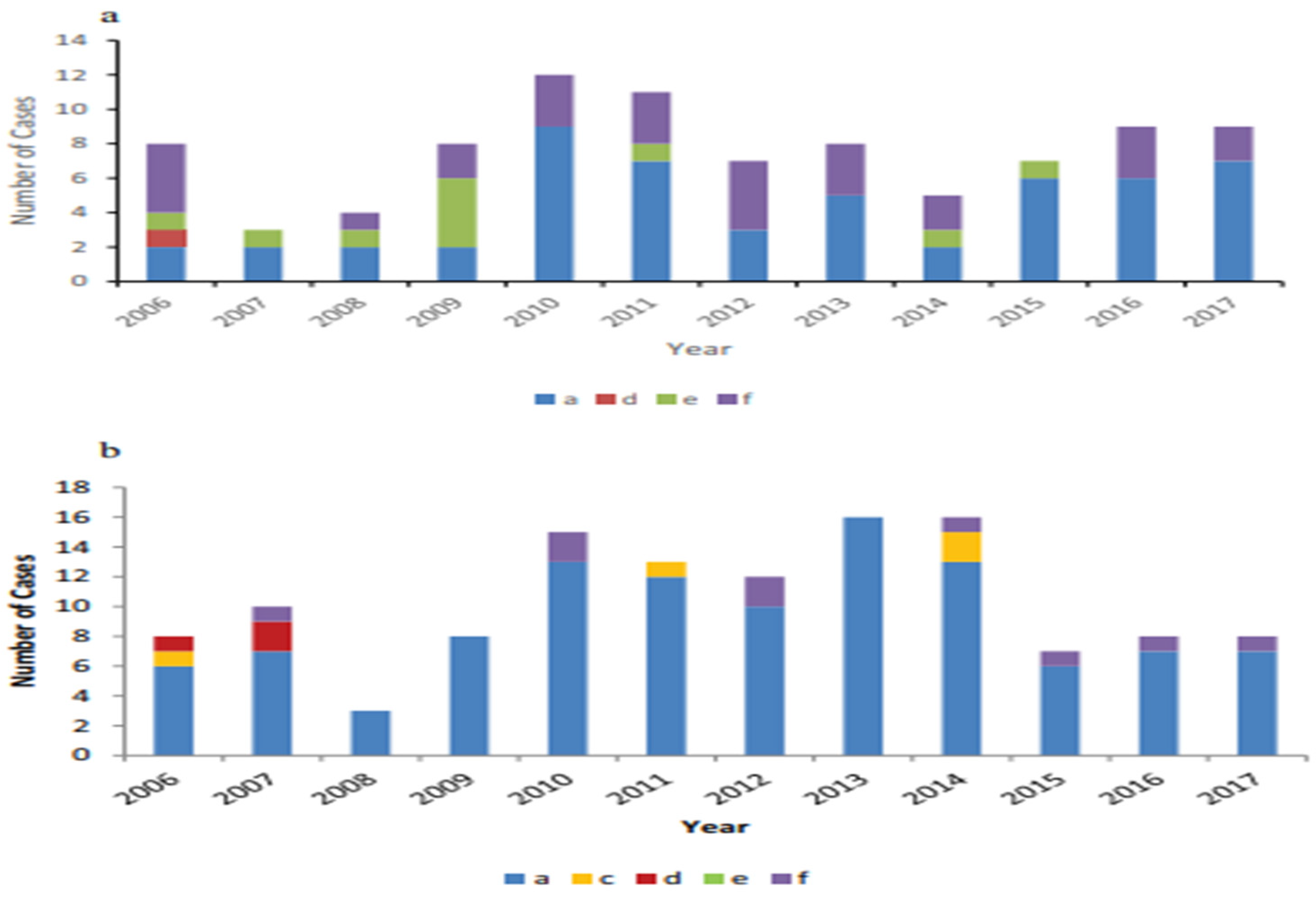
Figure 5 Depicts (a) Invasive non-b encapsulated Hi disease cases reported in Alaska from 2006 to 2017 by serotype. (b) Invasive non-B encapsulated Hi disease cases reported in Northern Canada from 2006 to 2017 by serotype [
3].
Figure 6 Shows Incidence of invasive H. influenzae illness in Ontario, displaying single infection events by serotype from 2014 to 2018 [
20].
3.4. South-EAST ASIAN REGION (SEAR)
After 2009, Hib vaccination was made available throughout The World Health Organization (WHO) South East Asia Region. Thailand was an exception, as the Hib vaccine was accessible on the private market since the late 1990s despite being included to the NIP in 2019 as a 3-dose primary course without a booster dose. Although rates vary greatly between nations, the South East Asian region had an average coverage of 89% for three doses of the Hib vaccine in 2019 .There aren't many reliable data on the invasive cases pneumonia and bacteremia or sepsis in the region, and there are few on the occurrence of invasive illness. In general, little information is available on the effect of Hib vaccine introduction on invasive H. influenzae disease in the World Health Organization (WHO) South East Asian Region. Invasive Hia disease has not been studied in Asia or Africa. In the majority of Asian and African nations, there are no systematic studies of invasive
H.influenzae illness or serotype data [
14,31] .
3.5. Eastern MEDITERRANEAN REGION (EMR)
The Hib vaccine has been made available in every nation in the WORLD HEALTH ORGANIZATION (WHO) Eastern Mediterranean Region. The average coverage of three Hib vaccination doses in 2019 was 82%.According to a recent study, there were Hib complaints from Pakistan (45.7), Saudi Arabia (16.9), Qatar (2.24%), Egypt (39%) and Jordan (27%).Data about non-serotype b strains of Hi is limited in this area. The advent of NTHi or non-b serotypes of H. influenzae producing invasive illness in this region is currently poorly documented [
14].
According to study conducted by Farajzadeh Sheikh A et al. in 2021 in Iran 3 of the 11 H. influenzae isolates were type f, and 2 of the viruses were identified as H. influenzae type b (Hib). 6 isolates could not be typed, though [32].
3.6. WESTERN PACIFIC REGION (WPR)
Invasive Hib disease is thought to have caused 370,000 cases and 3,800 fatalities in the Western Pacific Region in 2015. Between 2004 and 2017, a retrospective investigation was conducted in a tertiary hospital in Budapest, Hungary, and 34 adult invasive H. influenzae infections were discovered. The majority of cases (62%) began with pneumonia and were caused by NTHi (79%), followed by Hif (11%), Hia (5%), and Hib (5%). A third of the patients had underlying comorbid conditions such cancer, diabetes mellitus, and cardiovascular disease and were under 65 years old [
14].
Table 1.
Global Invasive H.influenzae trends since introduction of serotype b vaccine.
Table 1.
Global Invasive H.influenzae trends since introduction of serotype b vaccine.
| Hi serotype |
WORLD HEALTH ORGANIZATION (WHO) Region* |
Country |
Year |
Specimen |
Method used** |
Changes in
incidence
|
Incidence per 100,000*a |
Vaccine |
Ref |
| Hia |
AFRO |
South Africa |
2017 |
Blood |
SA+PCR |
Increased |
2.9 |
No |
[33] |
| Gambia |
2013 |
Blood |
SA+PCR |
Not known |
10 |
No |
[34] |
| AMR |
USA |
2015 |
Blood, CSF |
SA or PCR |
Increased |
8.3 |
No |
[14] |
| Canada |
2021 |
Blood, CSF |
SA+PCR |
Increased |
8.9 |
No |
[35] |
| Brazil |
2000 |
Blood |
Not reported |
Increased |
0.16 |
No |
[14] |
| EURO |
Portugal |
2018 |
Blood, |
PCR |
Increased |
2.7 |
No |
[21] |
| England |
2018 |
Blood, |
SA or PCR |
Increased |
0.8 |
No |
[21] |
| Germany |
2018 |
Blood |
Not reported |
Decreased |
0.5 |
No |
[21] |
| Hungary |
2017 |
Blood |
PCR |
Not known |
5 |
No |
[21] |
| Italy |
|
Blood |
SA or PCR |
Increased |
0.02 |
No |
[14] |
| Ireland |
2009 |
Blood |
SA or PCR |
Increased |
1 |
No |
[14] |
| WPR |
Australia |
2015 |
Blood |
SA+PCR |
Increased |
6.4 |
No |
[20] |
| Hib |
AFR |
South Africa |
2018 |
Blood |
PCR |
Increased |
17 |
Yes |
[33] |
| Gambia |
2013 |
Blood |
PCR |
Increased |
42 |
Yes |
[34] |
| AMR |
USA |
2018 |
Blood |
PCR+SA |
Decreased |
0.02 |
Yes |
[14] |
| Canada |
2018 |
Blood, |
SA+PCR |
Decreased |
2.3 |
Yes |
[21] |
| EURO |
Portugal |
2018 |
Blood, |
PCR |
Increased |
13.5 |
Yes |
[21] |
| England |
2018 |
Blood, |
SA+PCR |
Decreased |
1.2 |
Yes |
[21] |
| Finland |
2018 |
Blood,CSF |
Not reported |
Decreased |
3.5 |
Yes |
[21] |
| Germany |
2018 |
Blood |
Not reported |
Decreased |
2.4 |
Yes |
[14] |
| Italy |
2018 |
Blood |
PCR |
Increased |
11.5 |
Yes |
[14] |
| Taiwan |
2002 |
Blood |
SA |
Increased |
20 |
Yes |
[14] |
| Hungary |
2017 |
Blood |
Not reported |
Not known |
5 |
Yes |
[14] |
| Ireland |
2018 |
Blood |
SA or PCR |
Decreased |
2 |
Yes |
[36] |
| EMR |
Saudi Arabia |
2001 |
Blood |
PCR |
Not reported |
40 |
Yes |
[27] |
| Iran |
|
|
|
|
|
|
|
| UAE |
1999 |
Blood |
PCR |
Not reported |
46 |
Yes |
[27] |
| SEA |
South Korea |
2001 |
Blood |
PCR |
Not reported |
6.8 |
Yes |
[27] |
| Philippine |
2000 |
Blood |
PCR |
Increased |
95 |
Yes |
[27] |
| Japan |
2007 |
Blood |
SA or PCR |
Increased |
4.3 |
Yes |
[27] |
| Singapore |
2007 |
Blood |
PCR |
Decreased |
4.4 |
Yes |
[27] |
| Taiwan |
2000 |
Blood |
PCR |
Decreased |
3.2 |
Yes |
[27] |
| Indonesia |
2005 |
Blood |
PCR |
Increased |
67 |
Yes |
[27] |
| WPR |
Australia |
2013 |
Blood, CSF |
SA+PCR |
Increased |
14.9 |
Yes |
[29] |
| China |
2015 |
Blood |
SA or PCR |
Increased |
74 |
Yes |
[14] |
| Hong Kong |
2015 |
Blood |
SA+PCR |
Increased |
2.7 |
Yes |
[14] |
| Mongolia |
2008 |
Blood |
PCR or SA |
Decreased |
2 |
Yes |
[14] |
| Hic |
AFR |
South Africa |
2017 |
Blood |
PCR or SA |
Not reported |
1.13 |
No |
[33] |
| Gambia |
2013 |
Blood |
PCR or SA |
Not reported |
2 |
No |
[34] |
| Hid |
AFR |
South Africa |
2017 |
Blood |
PCR or SA |
Not reported |
0.31 |
No |
[33] |
| Gambia |
2017 |
Blood |
PCR or SA |
Not reported |
2 |
No |
[34] |
| AMR |
Canada |
2018 |
Blood,CSF |
SA+PCR |
Not reported |
0.1 |
No |
[21] |
| Hif |
AFR |
South Africa |
2017 |
Blood |
SA+PCR |
Not reported |
3.2 |
No |
[33] |
| Gambia |
2013 |
Blood |
SA+PCR |
Not reported |
2 |
No |
[34] |
| AMR |
Canada |
2018 |
Blood, |
SA+PCR |
Increased |
10.2 |
No |
[21] |
| WPR |
Australia |
2013 |
Blood, CSF |
SA+PCR |
Increased |
10.6 |
No |
[21] |
| EURO |
England |
2018 |
Blood |
SA+PCR |
Increased |
8.3 |
No |
[21] |
| Germany |
2018 |
Blood |
Not reported |
decreased |
9.8 |
No |
[14] |
| Finland |
2018 |
Blood |
SA+PCR |
Increased |
12.6 |
No |
[21] |
| Portugal |
2018 |
Blood, |
PCR |
Increased |
3.1 |
No |
[21] |
| Italy |
2018 |
Blood |
SA+PCR |
Increased |
4.6 |
No |
[14] |
| Ireland |
2018 |
Blood |
SA+PCR |
Increased |
7 |
No |
[36] |
| Sweden |
2009 |
Blood,CSF |
PCR |
Increased |
57 |
No |
[74] |
| Hie |
AFR |
South Africa |
2017 |
Blood |
SA+PCR |
Increase |
0.31 |
No |
[33] |
| Gambia |
2013 |
Blood |
Blood,CSF |
Not known |
2 |
No |
[34] |
| WPR |
Australia |
2013 |
Blood |
SA+PCR |
Increased |
14.9 |
No |
[21] |
| EURO |
Germany |
2018 |
Blood |
SA+PCR |
Not reported |
2.4 |
No |
[14] |
| Portugal |
2018 |
Blood,CSF |
PCR |
Increased |
79.2 |
No |
[21] |
| Portugal |
2018 |
Blood,CSF |
PCR |
Increased |
1.5 |
No |
[21] |
| |
Ireland |
2018 |
Blood |
SA+PCR |
Increased |
6 |
No |
[36] |
| NTHi |
AFR |
Gambia |
2013 |
Blood |
SA+PCR |
Not known |
30 |
No |
[34] |
| South Africa |
2017 |
Blood |
Not reported |
Increased |
64 |
No |
[33] |
| AMR |
Canada |
2018 |
Blood, |
SA+PCR |
Increased |
74.2 |
No |
[21] |
| USA |
2023 |
Blood |
SA+PCR |
Increased |
92 |
No |
[37] |
| SEA |
Taiwan |
2002 |
Blood |
SA |
Not Known |
80 |
No |
[30] |
| EURO |
Italy |
2018 |
Blood |
SA+PCR |
Increased |
76.1 |
No |
[21] |
| Germany |
2018 |
Blood |
Not reported |
Increased |
84.5 |
No |
[21] |
| Hungary |
2018 |
Blood |
SA+PCR |
Increased |
79 |
No |
[14] |
| Portugal |
2018 |
Blood |
PCR |
Increased |
79.2 |
No |
[21] |
| Finland |
2018 |
Blood |
SA+PCR |
Increased |
79 |
No |
[21] |
| Ireland |
2018 |
Blood |
SA+PCR |
Increased |
83 |
No |
[36] |
| Sweden |
2009 |
Blood |
PCR |
Increased |
71 |
No |
[14] |
| Spain |
2013 |
Blood |
SA |
Increased |
85 |
No |
[30] |
| Slovenia |
2008 |
Blood |
PCR |
Increased |
85 |
No |
[30] |
Figure 6.
Incidence of invasive H. influenzae illness in Ontario, displaying single infection events by serotype from 2014 to 2018 [
21]. * (N = 1,338).
Figure 6.
Incidence of invasive H. influenzae illness in Ontario, displaying single infection events by serotype from 2014 to 2018 [
21]. * (N = 1,338).
4. Virulence & RISK FACTORS OF INVASIVE H.INFLUENZAE
For some populations, ethnicity is a risk factor. The risk of invasive Hib infections is higher in There is a disparity in health outcomes between different ethnic groups such as American Indians, Inuits, black Africans, Melanesians, and African Americans. The reason for this is uncertain and could be attributed to biological factors or other causes [
14].
Both host variables and exposure factors can increase your risk of getting Hib illness. Family size, child care utilization, low socioeconomic position, parents with low levels of education, and siblings World Health Organization (WHO) are still in school are all exposure factors. Age (young and old ages with elevated risk), race/ethnicity (Native Americans with an elevated risk, possibly complicated by socioeconomic factors associated with both race/ethnicity and Hib disease), and chronic disease (including functional and anatomic asplenia, immunodeficiency virus infection, immunoglobulin deficiency, complement deficiency, and receiving chemotherapy or stem cell transplant) are all host factors. Breastfeeding and passively acquired maternal antibodies (for infants younger than 6 months) are protective factors [37].
Inadequacies in the immune system, including a lack of mannose-binding lectins, infectious flaws in the vaccine or in the way it was administered or stored, maturational delays in immunological responses, and specific, tiny flaws in how the body responded to PRP [53]. Recently, it was shown that receiving a cochlear implant operation could increase your risk of developing invasive H.influenzae disease. Age and, more importantly, a lack of vaccination against Hib for non-Hib strains were in some cases risk factors for the development of invasive Hib disease. Household contacts of an invasive Hib case are more likely to contract the illness [
14].
Due to the severe nature of invasive H.influenzae disease, it is crucial to investigate specific host factors, such as population genetics, patterns of natural immunity against this pathogen, and prevalence in populations with this disease, that may predispose some populations to infection. This type of data will be necessary for the creation of infection preventive and control methods Its capsule, the adhesion proteins, pili, the outer membrane proteins, the IgA1 protease and, last but not least, the lipooligosaccharide, increase the virulence of H. influenzae by participating actively in the host invasion the host by the microrganism. Some of these factors are used in vaccine preparations [
14,54].
5. Prevention AND CONTROL OF INVASIVE HAEMOPHILUS INFLUENZAE
All infants should receive the Hib vaccine before the age of six months, with a booster shot around the age of one. The vaccine is both safe and effective in preventing Hib. Antibiotics can be administered to those World Health Organization (WHO) have been in close contact with someone World Health Organization (WHO) has Hib disease as a preventative measure to assist prevent them from contracting the illness The World Health Organization advises that all routine paediatric immunization programs include the Hib conjugate vaccine. A three-dose primary series should be administered at the same time as the diphtheria, tetanus, and pertussis vaccines. In the second year of life, a booster boosts defense [
14].
The polyribosyl ribitol phosphate (PRP) polysaccharide from the Hib capsule is conjugated to a protein carrier in the Hib conjugate vaccine, which prevents invasive Hib illness and lowers naso-pharyngeal carriage. The only public health measure that can stop the majority of serious Hib diseases is immunization. The polyribosyl ribitol phosphate (PRP) polysaccharide from the Hib capsule is conjugated to a protein carrier in the Hib conjugate vaccine, which prevents invasive Hib illness and lowers naso-pharyngeal carriage. Chemoprophylaxis should be made available to all room contacts, including staff, in the event of an epidemic (two or more cases of Hib illness within 120 days) at a preschool or primary school. All children World Health Organization (WHO) are immunized in part or not at all should receive their full primary immunization. People World Health Organization (WHO) are in close or prolonged contact with someone World Health Organization (WHO) has H. influenzae sickness risk contracting the illness. Close contacts of a person with H. influenzae disease may occasionally need to take antibiotics to prevent getting ill [
14].
6. Conclusion AND FUTURE DIRECTIONS
Invasive Non-typeable (NTHi) and non-b strains of the H.influenzae are currently the main causes of the sickness, with small children and the elderly being the most common populations to contract it. Since the illness burden is still greatest in resource-poor countries, immediate action must be taken to guarantee that children living in locations where this vaccine cannot be used owing to financial and logistical restrictions benefit from its benefits [40,45]. Due to the severe nature of invasive H.influenzae disease, it is crucial to investigate specific host factors, such as patterns of natural immunity against this pathogen, population genetics, and prevalence in populations with this disease that may predispose some populations to infection [
14].
Due to the sporadic nature of the disease and the absence of global monitoring programmes that are systematic and thorough, the data on the global epidemiology of invasive H.influenzae disease are insufficient [
15].
Non-type b strains have been seen causing invasive Hi disease in different regions of Europe, North America, and Australia [38]. Regarding invasive H.influenzae bacterial infections, this review includes the following information’s and knowledge gaps:
Globally, H.influenzae continues to be a common invasive Bacterial pathogen that dramatically raises morbidity and mortality. However, still little is known about the global presence of this pathogen and its emerging pathogenic strains.
For some populations, ethnicity is a risk factor. The risk of invasive Hib infections is higher in American Indians, Inuits, black Africans, Melanesians, and African Americans. Whether this is due to truly biological differences or other factors is not clear and needs further studies on these populations.
NTHi, Hia, Hif, and Hie cause an increasing number of invasive illnesses, especially in children and elderly people. However, the immune response to non-type b Hi infection is poorly studied.
Even though there is still no vaccine available for strains other than type b (Hib).Immunization is necessary to guard against contracting invasive diseases brought on by nontypeable and other encapsulated strains of H. influenzae.
H. influenzae can infect a person several times and a prior Hib infection could not protect you from a later infection. It is recommended to take the Hib vaccine even if one has already had Hib disease.
The reasons for an increased susceptibility to NTHi, Hia, and Hif and Hie infection among some specific populations groups are still unknown and needs further research.
Since Nontypeable Haemophilus influenzae's pathogenicity is significantly rising, international scientific organizations need to raise awareness of the emergence of invasive Hi pathogenicity and characterize the pathobiology of this microorganism.
It is essential to understand the host-pathogen interactions in Hi patients in order to curb the spread of invasive NTHi and other Hi strains. Through a variety of host proteins, including the invasion of certain serum factors and direct adhesion to surface epithelial cells, which disintegrates the extracellular matrix layer.
Finally, this review suggests that an extensive surveillance system that collects information on serotype, genotype, immunological characterization, and vaccination status is required to follow the trends described in this Review and eradicate H.influenzae illnesses and their global impacts.
Supplementary Information
The online version contains supplementary material.
Author Contributions
- All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript. Study design & writing of the manuscript: Abas Mahammed. Revision of the manuscript: Destaw Damtie and Tirusew Sema.
Funding
This review research study did not receive any specific grant from funding agencies in the public, commercial, or not for- profit sectors.
Availability of data and materials
Not applicable.
Acknowledgement
We didn’t used any AI like ChatGPT and others. We would like to acknowledge Bahirdar University, Biomedical Science stream to Review This Review and suggest constructive comments.
Competing of Interest
The authors declare no competing interests or conflict of interests.
Consent for publication
All authors reviewed the results and approved the final version of the manuscript. A preprint has previously been published [55].
Ethics approval and consent to participate
Not applicable.
References
- Levinson W, Chin-Hong P, Joyce E, Nussbaum J, Schwartz B: Host Defenses. Review of Medical Microbiology & Immunology: A Guide to Clinical Infectious Diseases (McGraw-Hill Education 2018.
- Ribeiro GS, Reis JN, Cordeiro SM, Lima JB, Gouveia EL, Petersen M, Salgado K, Silva HR, Zanella RC, Almeida SCG: Prevention of Haemophilus influenzae type b (Hib) meningitis and emergence of serotype replacement with type a strains after introduction of Hib immunization in Brazil. The Journal of infectious diseases 2003, 187(1):109-116. [CrossRef]
- Resman F, Ristovski M, Ahl J, Forsgren A, Gilsdorf JR, Jasir A, Kaijser B, Kronvall G, Riesbeck K: Invasive disease caused by Haemophilus influenzae in Sweden 1997–2009; evidence of increasing incidence and clinical burden of non-type b strains. Clinical Microbiology and Infection 2011, 17(11):1638-1645. [CrossRef]
- Ortiz-Romero M, Espejo-García M, Alfayate-Miguelez S, Ruiz-López F, Zapata-Hernandez D, Gonzalez-Pacanowska A: Collaborators of Study Group of Infectious Diseases in the Child in Cartagena. 2017. Epidemiology of nasopharyngeal carriage by Haemophilus influenzae in healthy children: a study in the Mediterranean coast region. Pediatr Infect Dis J, 36:919-923. [CrossRef]
- O'Neill JM, St. Geme III JW, Cutter D, Adderson EE, Anyanwu J, Jacobs RF, Schutze GE: Invasive disease due to nontypeable Haemophilus influenzae among children in Arkansas. Journal of clinical microbiology 2003, 41(7):3064-3069. [CrossRef]
- Chatziparasidis G, Kantar A, Grimwood K: Pathogenesis of nontypeable Haemophilus influenzae infections in chronic suppurative lung disease. Pediatric Pulmonology 2023. [CrossRef]
- van Wessel K, Rodenburg GD, Veenhoven RH, Spanjaard L, van der Ende A, Sanders EA: Nontypeable Haemophilus influenzae invasive disease in The Netherlands: a retrospective surveillance study 2001–2008. Clinical Infectious Diseases 2011, 53(1):e1-e7. [CrossRef]
- Ulanova M, Tsang RS: Haemophilus influenzae serotype a as a cause of serious invasive infections. The Lancet infectious diseases 2014, 14(1):70-82. [CrossRef]
- Whittaker R, Economopoulou A, Dias JG, Bancroft E, Ramliden M, Celentano LP: Epidemiology of Invasive Haemophilus influenzae Disease, Europe, 2007-2014. Emerg Infect Dis 2017, 23(3):396-404. [CrossRef]
- Tristram S, Jacobs MR, Appelbaum PC: Antimicrobial resistance in Haemophilus influenzae. Clinical microbiology reviews 2007, 20(2):368-389. [CrossRef]
- Slack MP: A review of the role of Haemophilus influenzae in community-acquired pneumonia. Pneumonia 2015, 6:26-43. [CrossRef]
- Soeters HM, Blain A, Pondo T, Doman B, Farley MM, Harrison LH, Lynfield R, Miller L, Petit S, Reingold A et al: Current Epidemiology and Trends in Invasive Haemophilus influenzae Disease-United States, 2009-2015. Clin Infect Dis 2018, 67(6):881-889. [CrossRef]
- Giufrè M, Cardines R, Brigante G, Orecchioni F, Cerquetti M: Emergence of invasive Haemophilus influenzae type a disease in Italy. Clinical Infectious Diseases 2017, 64(11):1626-1628. [CrossRef]
- Slack M, Cripps A, Grimwood K, Mackenzie G, Ulanova M: Invasive Haemophilus influenzae infections after 3 decades of Hib protein conjugate vaccine use. Clinical microbiology reviews 2021, 34(3):e00028-00021. [CrossRef]
- Ulanova M: Global epidemiology of invasive Haemophilus influenzae type a disease: do we need a new vaccine? Journal of Vaccines 2013, 2013. [CrossRef]
- Peltola H: Worldwide Haemophilus influenzae type b disease at the beginning of the 21st century: global analysis of the disease burden 25 years after the use of the polysaccharide vaccine and a decade after the advent of conjugates. Clinical microbiology reviews 2000, 13(2):302-317. [CrossRef]
- Soeters HM, Blain A, Pondo T, Doman B, Farley MM, Harrison LH, Lynfield R, Miller L, Petit S, Reingold A: Current epidemiology and trends in invasive Haemophilus influenzae disease—United States, 2009–2015. Clinical Infectious Diseases 2018, 67(6):881-889. [CrossRef]
- Tsang R, Bruce M, Lem M, Barreto L, Ulanova M: A review of invasive Haemophilus influenzae disease in the Indigenous populations of North America. Epidemiology & Infection 2014, 142(7):1344-1354. [CrossRef]
- WHO W: Definition of regional groupings. 2017.
- Organization WH: www. who. int/healthinfo/global_burden_disease/definition_regions/en.
- Duell BL, Su YC, Riesbeck K: Host–pathogen interactions of nontypeable Haemophilus influenzae: from commensal to pathogen. FEBS letters 2016, 590(21):3840-3853. [CrossRef]
- Potts CC, Topaz N, Rodriguez-Rivera LD, Hu F, Chang H-Y, Whaley MJ, Schmink S, Retchless AC, Chen A, Ramos E: Genomic characterization of Haemophilus influenzae: a focus on the capsule locus. BMC genomics 2019, 20:1-9. [CrossRef]
- Meiring S, Cohen C, de Gouveia L, du Plessis M, Kleynhans J, Quan V, Lengana S, Walaza S, von Gottberg A: GERMS-SA annual surveillance report for laboratory-confirmed invasive meningococcal, Haemophilus influenzae and pneumococcal disease, South Africa, 2017. Public Health Surveillance 2019, 78.
- Organization WH: Health and well-being profile of the Eastern Mediterranean Region: an overview of the health situation in the Region and its countries in 2019. 2020.
- Plotkin S: A short history of vaccination. Vaccines. SA Plotkin and WA Orenstein. In.: Philadelphia, Elsevier; 2004.
- Pinto M, González-Díaz A, Machado M, Duarte S, Vieira L, Carriço J, Marti S, Bajanca-Lavado M, Gomes J: Insights into the population structure and pan-genome of Haemophilus influenzae. Infection, Genetics and Evolution 2019, 67:126-135. [CrossRef]
- Zulz T, Huang G, Rudolph K, DeByle C, Tsang R, Desai S, Massey S, Bruce MG: Epidemiology of invasive Haemophilus influenzae serotype a disease in the North American Arctic, 2006–2017. International Journal of Circumpolar Health 2022, 81(1):2150382. [CrossRef]
- Trotter CL, Lingani C, Fernandez K, Cooper LV, Bita A, Tevi-Benissan C, Ronveaux O, Préziosi M-P, Stuart JM: Impact of MenAfriVac in nine countries of the African meningitis belt, 2010–15: an analysis of surveillance data. The Lancet infectious diseases 2017, 17(8):867-872. [CrossRef]
- Cheong JWS, Smith H, Heney C, Robson J, Schlebusch S, Fu J, Nourse C: Trends in the epidemiology of invasive Haemophilus influenzae disease in Queensland, Australia from 2000 to 2013: what is the impact of an increase in invasive non-typable H. influenzae (NTHi)? Epidemiology & Infection 2015, 143(14):2993-3000. [CrossRef]
- Langereis JD, de Jonge MI: Invasive disease caused by nontypeable Haemophilus influenzae. Emerging infectious diseases 2015, 21(10):1711. [CrossRef]
- Belete H, Kidane T, Bisrat F, Molla M, Mounier-Jack S, Kitaw Y: Routine immunization in Ethiopia. The Ethiopian Journal of Health Development 2015, 29.
- Farajzadeh Sheikh A, Rahimi R, Meghdadi H, Alami A, Saki M: Multiplex polymerase chain reaction detection of Streptococcus pneumoniae and Haemophilus influenzae and their antibiotic resistance in patients with community-acquired pneumonia from southwest Iran. BMC Microbiol 2021, 21(1):343. [CrossRef]
- Diseases NIfC: GERMS South Africa: annual surveillance review 2018. 2018.
- Mackenzie GA, Ikumapayi UN, Scott S, Idoko O, Odutola A, Ndiaye M, Sahito SM, Osuorah CD, Manjang A, Jarju S: Increased disease due to Haemophilus influenzae type b: population-based surveillance in eastern Gambia, 2008–2013. The Pediatric infectious disease journal 2015, 34(5):e107-e112. [CrossRef]
- McTaggart LR, Cronin K, Seo CY, Wilson S, Patel SN, Kus JV: Increased Incidence of Invasive Haemophilus influenzae Disease Driven by Non-Type B Isolates in Ontario, Canada, 2014 to 2018. Microbiology Spectrum 2021, 9(2):e00803-00821. [CrossRef]
- McElligott M, Meyler K, Bennett D, Mulhall R, Drew RJ, Cunney R: Epidemiology of Haemophilus influenzae in the Republic of Ireland, 2010–2018. European Journal of Clinical Microbiology & Infectious Diseases 2020, 39(12):2335-2344. [CrossRef]
- Oliver SE, Rubis AB, Soeters HM, Reingold A, Barnes M, Petit S, Farley MM, Harrison LH, Como-Sabetti K, Khanlian SA: Epidemiology of Invasive Nontypeable Haemophilus influenzae Disease—United States, 2008–2019. Clinical Infectious Diseases 2023:ciad054. [CrossRef]
- Bakaletz LO, Novotny LA: Nontypeable haemophilus influenzae (nthi). Trends in microbiology 2018, 26(8):727-728. [CrossRef]
- Rate A: Invasive Haemophilus influenzae disease.
- Kelly DF, Moxon ER, Pollard AJ: Haemophilus influenzae type b conjugate vaccines. Immunology 2004, 113(2):163-174.
- King PT, Sharma R: The lung immune response to nontypeable Haemophilus influenzae (lung immunity to NTHi). Journal of immunology research 2015, 2015. [CrossRef]
- Gilsdorf JR: What the pediatrician should know about non-typeable Haemophilus influenzae. Journal of Infection 2015, 71:S10-S14. [CrossRef]
- Heliodoro CIM, Bettencourt CR, Bajanca-Lavado MP, Infection PGftSoHiI: Molecular epidemiology of invasive Haemophilus influenzae disease in Portugal: an update of the post-vaccine period, 2011–2018. European Journal of Clinical Microbiology & Infectious Diseases 2020, 39:1471-1480. [CrossRef]
- Gaultier G: Humoral immunity in patients with chronic kidney disease and their response to pneumococcal immunization. 2020.
- Tønnessen R, García I, Debech N, Lindstrøm JC, Wester AL, Skaare D: Molecular epidemiology and antibiotic resistance profiles of invasive Haemophilus influenzae from Norway 2017–2021. Frontiers in Microbiology 2022, 13. [CrossRef]
- Choi J, Cox AD, Li J, McCready W, Ulanova M: Activation of innate immune responses by Haemophilus influenzae lipooligosaccharide. Clinical and Vaccine Immunology 2014, 21(5):769-776. [CrossRef]
- Jin Z, Romero-Steiner S, Carlone GM, Robbins JB, Schneerson R: Haemophilus influenzae type a infection and its prevention. Infection and immunity 2007, 75(6):2650-2654. [CrossRef]
- Dousha L, Sharma R, Lim S, Ngui J, Buckle AM, King PT: Assessing Respiratory Immune Responses to Haemophilus Influenzae. JoVE (Journal of Visualized Experiments) 2021(172):e62572. [CrossRef]
- Ladhani S, Slack MP, Heath PT, Von Gottberg A, Chandra M, Ramsay ME, participants EUIBIS: Invasive Haemophilus influenzae disease, Europe, 1996–2006. Emerging infectious diseases 2010, 16(3):455. [CrossRef]
- High N, Fan F, Schwartzman J: Chapter 97—haemophilus influenzae. Molecular medical microbiology, vol. 3. In.: Amsterdam: Academic Press; 2015.
- Hawdon N, Nix EB, Tsang RS, Ferroni G, McCready WG, Ulanova M: Immune response to Haemophilus influenzae type b vaccination in patients with chronic renal failure. Clinical and Vaccine Immunology 2012, 19(6):967-969. [CrossRef]
- Vikhe PP, Purnell T, Brown SD, Hood DW: Cellular immune response against nontypeable haemophilus influenzae infecting the preinflamed middle ear of the junbo mouse. Infection and Immunity 2019, 87(12):e00689-00619. [CrossRef]
- Heath P, Booy R, Griffiths H, Clutterbuck E, Azzopardi H, Slack M, Fogarty J, Moloney A, Moxon E: Clinical and immunological risk factors associated with Haemophilus influenzae type b conjugate vaccine failure in childhood. Clinical infectious diseases 2000, 31(4):973-980. [CrossRef]
- Soeters HM, Oliver SE, Plumb ID, Blain AE, Zulz T, Simons BC, Barnes M, Farley MM, Harrison LH, Lynfield R: Epidemiology of invasive Haemophilus influenzae serotype a disease—United States, 2008–2017. Clinical Infectious Diseases 2021, 73(2):e371-e379. [CrossRef]
- Mahammed A, Damtie D, Sema T, Abdilahi Z: A Global Review of Invasive Haemophilus influenzae Disease from 2000-2023: Current Status, Challenges and Future Perspectives. 2023. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).