1. Introduction
Auricular keloids, often originating from otoplasty, ear piercings, and various otologic procedures, pose considerable aesthetic and functional hurdles for individuals afflicted by these lesions. Traditional therapeutic modalities, such as surgical excision, intralesional corticosteroid injections, and non-ablative laser therapy, have been utilized to manage these keloids, yet they often yield suboptimal outcomes in terms of keloid recurrence and aesthetic improvement 1 . Hence, there is a critical need for innovative treatment strategies to optimize the management of ear keloids and enhance patient outcomes.
The advent of laser technology has revolutionized the field of dermatology, offering clinicians new therapeutic avenues for managing various cutaneous conditions, including keloids 2. In this study, we elucidate our center's clinical experience employing an innovative, combined treatment strategy comprising ablative CO2 laser followed by dye laser therapy to address ear keloid morphology and quality. This avant-garde methodology has the potential to proffer a safe and efficacious alternative for patients seeking to improve the appearance and pliability of their ear keloids.
1.1. Background auricular keloids
Ear keloids are fibroproliferative growths that develop as an exaggerated response to trauma or injury on the ear, typically resulting from surgical procedures such as otoplasty, ear piercings, or other otologic interventions3. These keloids may not only cause aesthetic concerns but also impair the affected individual's quality of life due to itching, pain, or restricted movement in the area4. Moreover, keloids have a proclivity for recurrence, which poses additional challenges for both patients and clinicians. Ear keloids, although often neglected in research, warrant the investigation of novel therapeutic approaches to optimize patient outcomes.
1.2. Traditional Treatment Methods
Various treatment methods have been employed to address ear keloids, ranging from conservative approaches to more invasive procedures. Intralesional corticosteroid injections are commonly used as first-line therapies, but their efficacy is often limited by the risk of side effects and the potential for keloid recurrence5. Berman et al. (2002)6 highlight the limitations of corticosteroid injections, stating that "although intralesional corticosteroid injections can provide temporary relief, the risk of side effects and recurrence remains significant."
Surgical excision, while effective in some cases, carries inherent risks, such as infection, hematoma, and a high probability of keloid recurrence7. Non-surgical methods, including cryotherapy and radiation therapy, are also available; however, they often yield inconsistent results and may require multiple treatments 8. O'Brien and Jones 9 note that "although radiation therapy has been shown to reduce the recurrence of keloids after excision, its results are variable, and concerns remain regarding the potential long-term risks." Non-ablative laser therapy has been utilized as well, but it is generally less effective in improving the texture and pliability of keloids compared to ablative laser modalities 1.
1.3. Ablative Combined Laser Therapy with CO2 and Dye as an Innovative Approach
The combined use of ablative CO2 and dye laser therapy offers a novel, promising approach for the treatment of ear keloids. Ablative CO2 laser therapy is known for its ability to effectively resurface the skin and improve keloid texture by promoting collagen remodeling 2. Manuskiatti et al. (1999) 10report that "ablative CO2 laser therapy can induce significant dermal remodeling and produce noticeable improvement in the texture and appearance of keloids." Dye laser therapy, on the other hand, targets the vascular component of keloids, reducing erythema and improving the overall coloration 11. Alster and Williams (2012)11 assert that "the use of dye lasers has been shown to be effective in reducing the vascular component of keloids, thereby improving their overall appearance."
The synergy of these two laser modalities has the potential to significantly enhance the quality and appearance of ear keloids, addressing both the structural and chromatic aspects of keloid scarring 12. Ross et al. (2000) suggest that "combining different laser modalities can provide superior results in keloid treatment by targeting the various components of scarring." Furthermore, this combined treatment approach may reduce the need for multiple sessions, thereby minimizing patient discomfort, downtime, and the risk of complications.
2. Materials and Methods
2.1. Study design and patient selection
From January 2022 to January 2023, 15 patients (9 females, 6 males; mean age 45±8.45) with auricular keloids resulting from various otologic surgeries were enrolled at La Sapienza University of Rome (Italy) and the Lasers in Dermatology Unit of the University of Tor Vergata in Rome, (Italy), patients’ characteristics resumed in Table 1. The Sapienza University local ethical committee approved this study. All patients underwent treatment after obtaining a detailed personal history and clinical anamnesis (skin type, clinical manifestations, health conditions, previous medications, and lifestyle), and informed consent on the risks related to the procedure was signed. Previous studies have shown that keloids are common complications after surgical procedures, and their treatment is essential to improving patients' quality of life 4,13.
2.2. Treatment protocol
2.2.1. Dye laser therapy
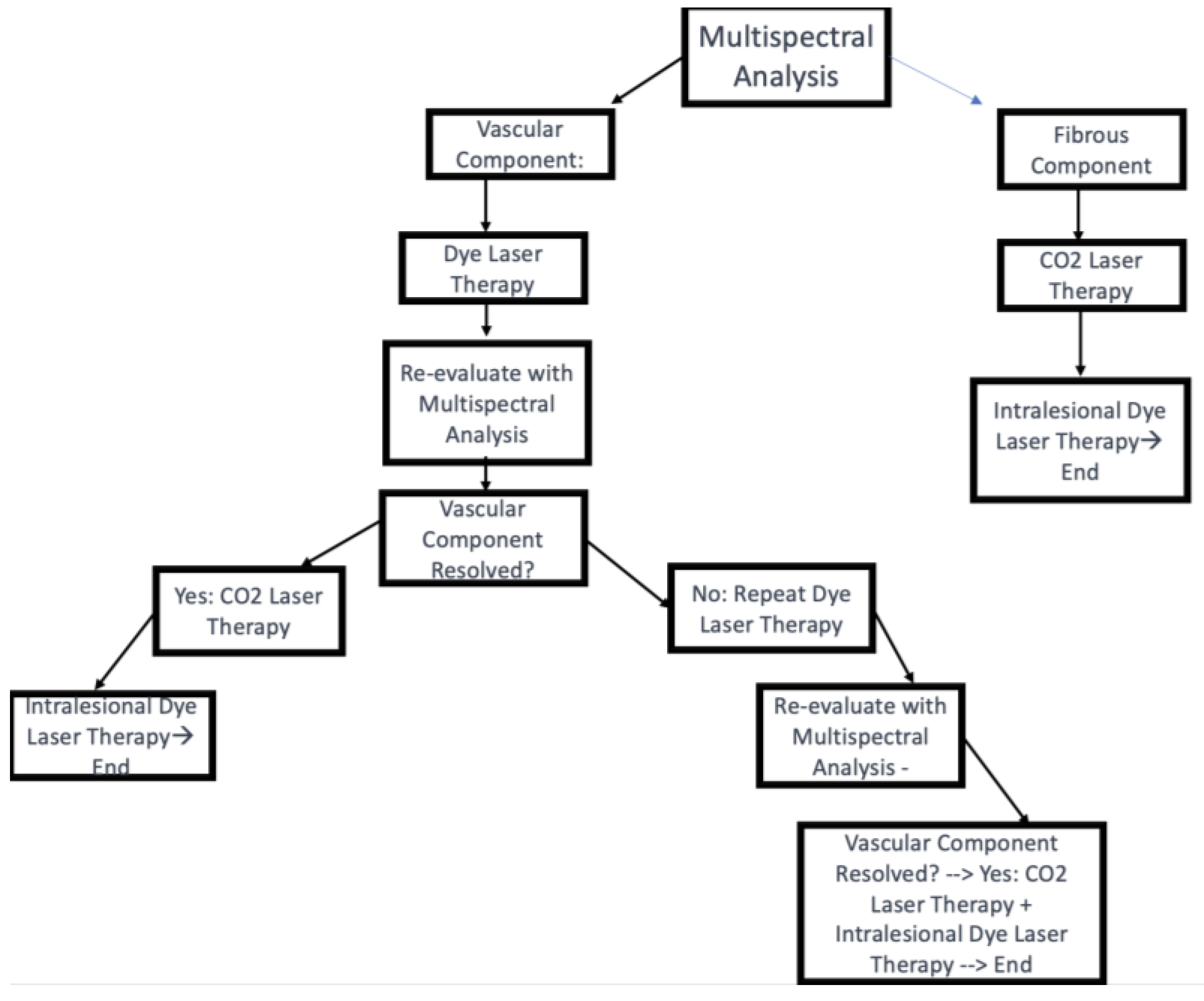
For keloids with a vascular component, the treatment was initiated with dye laser therapy (Synchro VasQ – DEKA, Calenzano, Italy) (Handpiece Spot Size 12 mm; Fluence 7 J/cm2; Pulse Duration 0.5 ms) to reduce the vascular component. After 40 days, the patient was re-evaluated using multispectral analysis. If the vascular component persisted, dye laser therapy was repeated; otherwise, the treatment proceeded with CO2 laser therapy for vaporization of the tissue.
2.2.2. Ablative CO2 laser therapy
For keloids with a more prominent fibrous component, treatment was initiated with a CO2 laser (SmartXide2 – DEKA, Calenzano, Italy) in freehand mode (7 mm handpiece; Power 0.3-2.5 W) to ablate the entire keloid tissue. Immediately following the CO2 laser treatment, intralesional dye laser therapy was performed to modulate healing and prevent keloid recurrence.
2.2.3. Follow-up and additional treatments
Patients were followed up with 3-week intervals and treated with dye laser therapy to regulate healing and prevent keloid recurrence. The average number of follow-up intervals was 3; however, this varied depending on inter-individual variability in the wound healing process.
2.2.4. Multispectral analysis
Multispectral analysis, a non-invasive imaging technique that captures the reflectance and absorption properties of tissues at multiple wavelengths
14 ,was performed to assess the composition of the keloids and identify the presence of vascular or fibrous components. (
Figure 1)
2.2.5. Vancouver Scar Scale (VSS)
The Vancouver Scar Scale (VSS) was used to assess the keloids before and after each laser session 12. The VSS evaluates four parameters: pigmentation, vascularity, pliability, and height, with scores ranging from 0 to 13, with higher scores indicating more severe scarring 12.
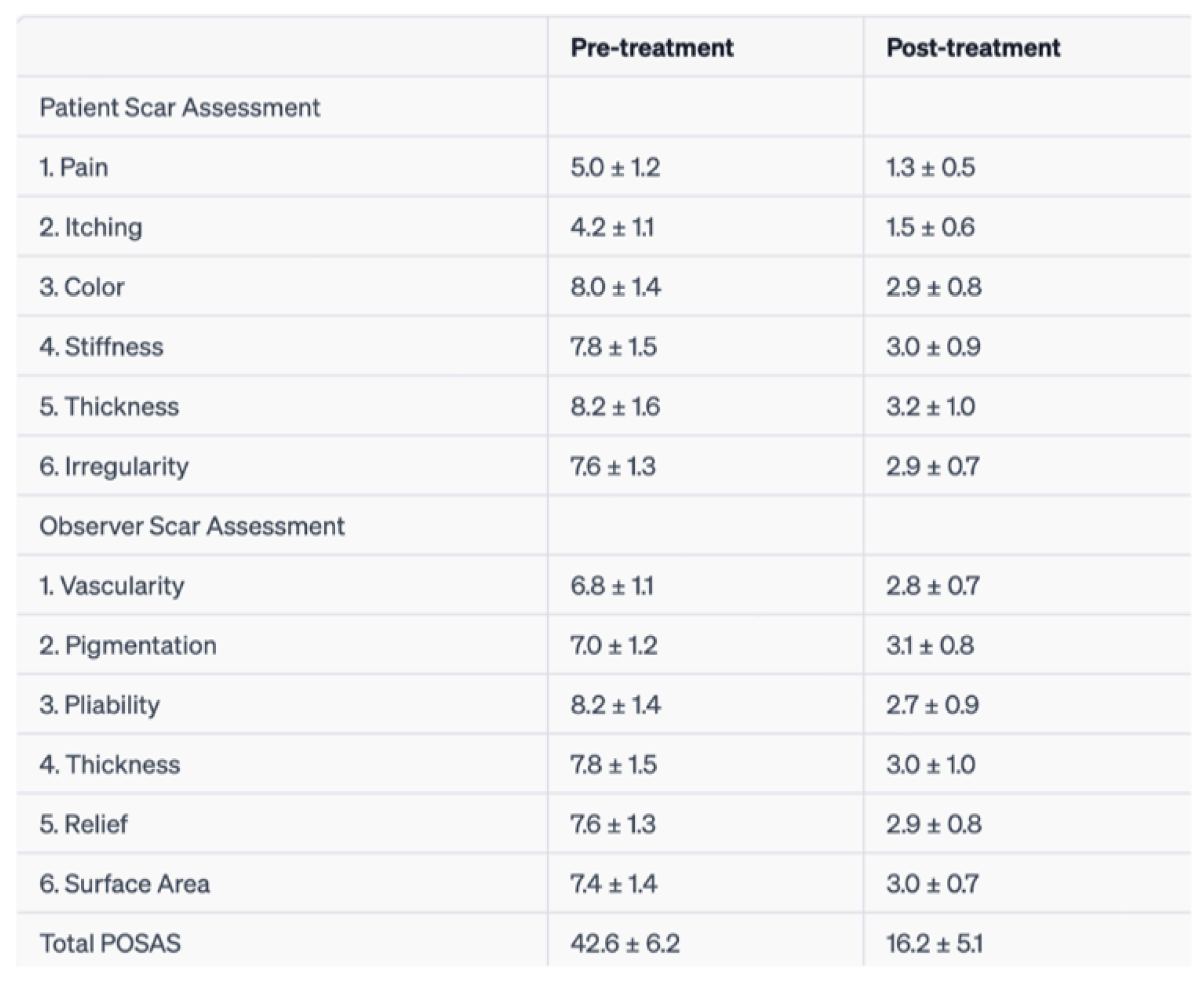
2.2.6. Patient and Observer Scar Assessment Scale
The Patient and Observer Scar Assessment Scale (POSAS) is a comprehensive scar evaluation tool that considers both the patient's and observer's perspectives in assessing scar quality 11. The POSAS consists of two separate parts: the Patient Scar Assessment Scale (PSAS) and the Observer Scar Assessment Scale (OSAS). The PSAS includes six items rated by the patient on a 10-point scale, with 1 representing normal skin and 10 indicating the worst imaginable scar. These items cover pain, itching, color, stiffness, thickness, and irregularity.
The OSAS is completed by the clinician and consists of six items as well, each rated on a 10-point scale, with 1 indicating normal skin and 10 representing the worst imaginable scar. The items assessed by the observer include vascularization, pigmentation, thickness, relief, pliability, and surface area. The total POSAS score is the sum of the PSAS and OSAS scores, with a higher score indicating a poorer scar quality 11.
In this study, the POSAS was used to evaluate the ear keloids of the 15 patients before and after the combined ablative CO2 laser and dye laser treatment. The assessment was performed by two independent blinded observers, and patients also evaluated their own scars. This method allowed for a more comprehensive evaluation of the treatment's effectiveness, considering not only the objective improvement of the scars but also the patients' subjective satisfaction with the treatment outcomes.
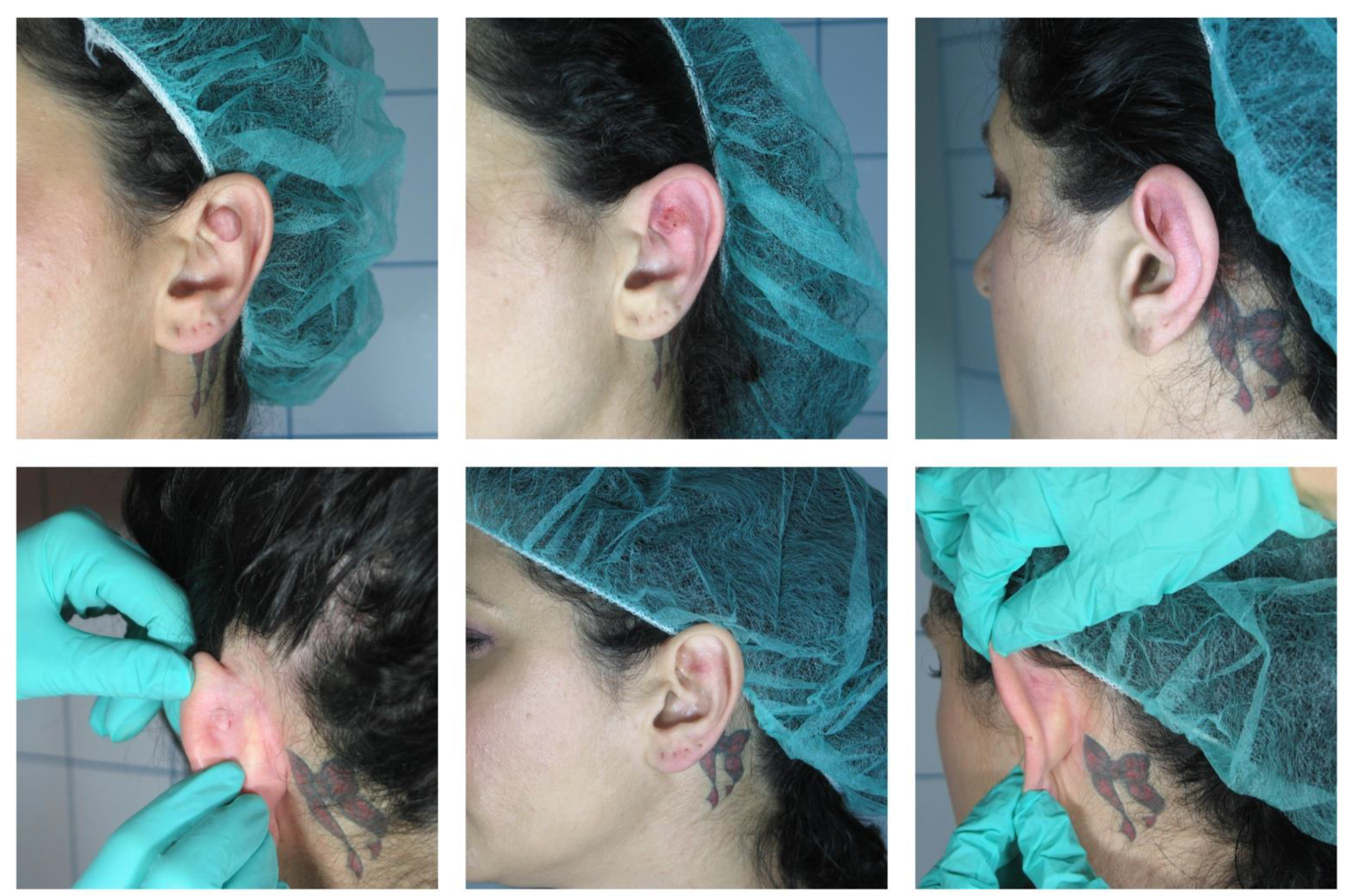
Clinical Case n 1:
A 30-year-old female patient presented with a progressively enlarging, nodular lesion on her right earlobe (
Figure 2). She reported that the lesion developed at the site of an ear piercing and had gradually increased in size over the past six months. The lesion was associated with discomfort and occasional pruritus, which had significantly impacted her quality of life due to both physical and aesthetic reasons. On examination, a firm, non-tender, 1.5 cm by 2,3 cm keloid was observed predominantly on the posterior surface of the earlobe.
An accompanying photograph depicted the lesion in greater detail. The image revealed a shiny, firm, lobulated mass that was raised and extended beyond the initial injury site, characteristics typical of keloids. The lesion also showed a reddish hue, indicating possible vascular involvement.
The patient underwent a multispectral analysis, confirming the presence of substantial vascular tissue within the keloid. As per our protocol, a sequential approach to treatment was decided. The patient was initially treated with pulsed dye laser therapy targeted at the vascular component of the keloid, followed by ablative CO2 laser therapy to resurface the lesion.
The patient responded well to the treatment with no reported adverse effects. Over the course of several weeks, there was a noticeable improvement in the color, texture, and pliability of the lesion. By the end of the treatment cycle, the keloid was completely resolved. No recurrence was observed during follow-up appointments, and the patient reported satisfaction with the treatment outcome.
Clinical case n 2
A 34-year-old female patient reported to our clinic with an enlarging, nodular lesion on the inner surface of her auricle. She related the onset of the lesion to a previous piercing in the same area, which had progressively grown in size over the last eight months. The patient experienced occasional discomfort and irritation from the lesion, impacting her daily activities and overall quality of life. Physical examination revealed a firm, non-tender keloid measuring 1.0 cm by 1.2 cm, located predominantly on the inner surface of the auricle.
The multispectral analysis conducted prior to treatment revealed a minimal vascular component within the keloid. Based on this assessment, the treatment plan was modified accordingly. In this case, direct ablation of the keloid using CO2 laser was chosen as the primary treatment approach due to the minimal vascular involvement.
Following the ablation, intralesional pulsed dye laser therapy was administered to further improve the healing process by targeting any remaining vascular component and promoting favorable tissue remodeling. The laser therapy was well-tolerated by the patient, and no adverse effects were reported.
Over subsequent weeks, substantial improvements in the keloid's texture, pliability, and overall appearance were observed. By the end of the treatment cycle, the lesion had completely resolved. At follow-up appointments, no recurrence of the keloid was detected, and the patient expressed satisfaction with the treatment outcome and the significant improvement in her quality of life.
Figure 1.
Auricular keloid of inner surface of auricle.
Figure 1.
Auricular keloid of inner surface of auricle.
3. Results
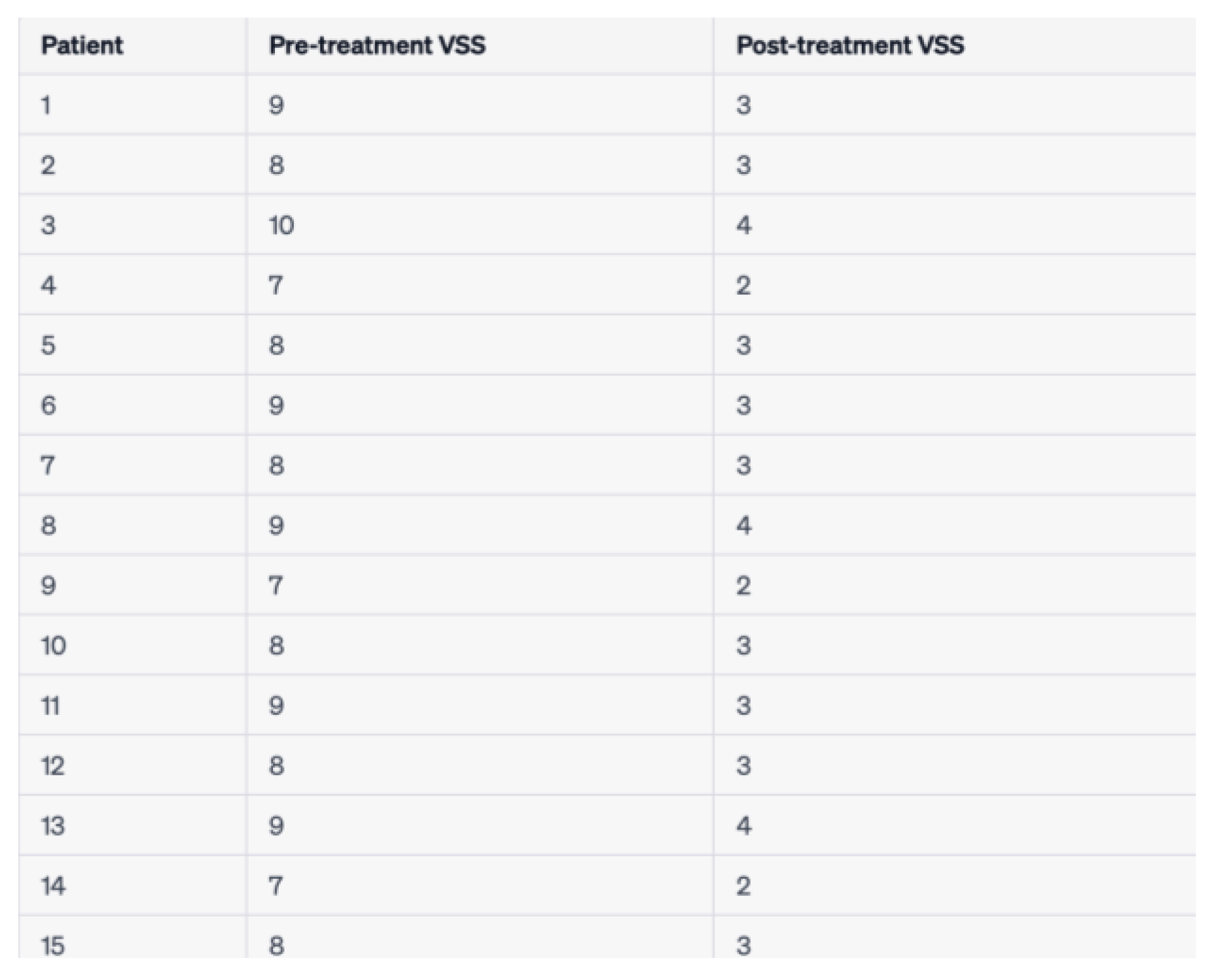
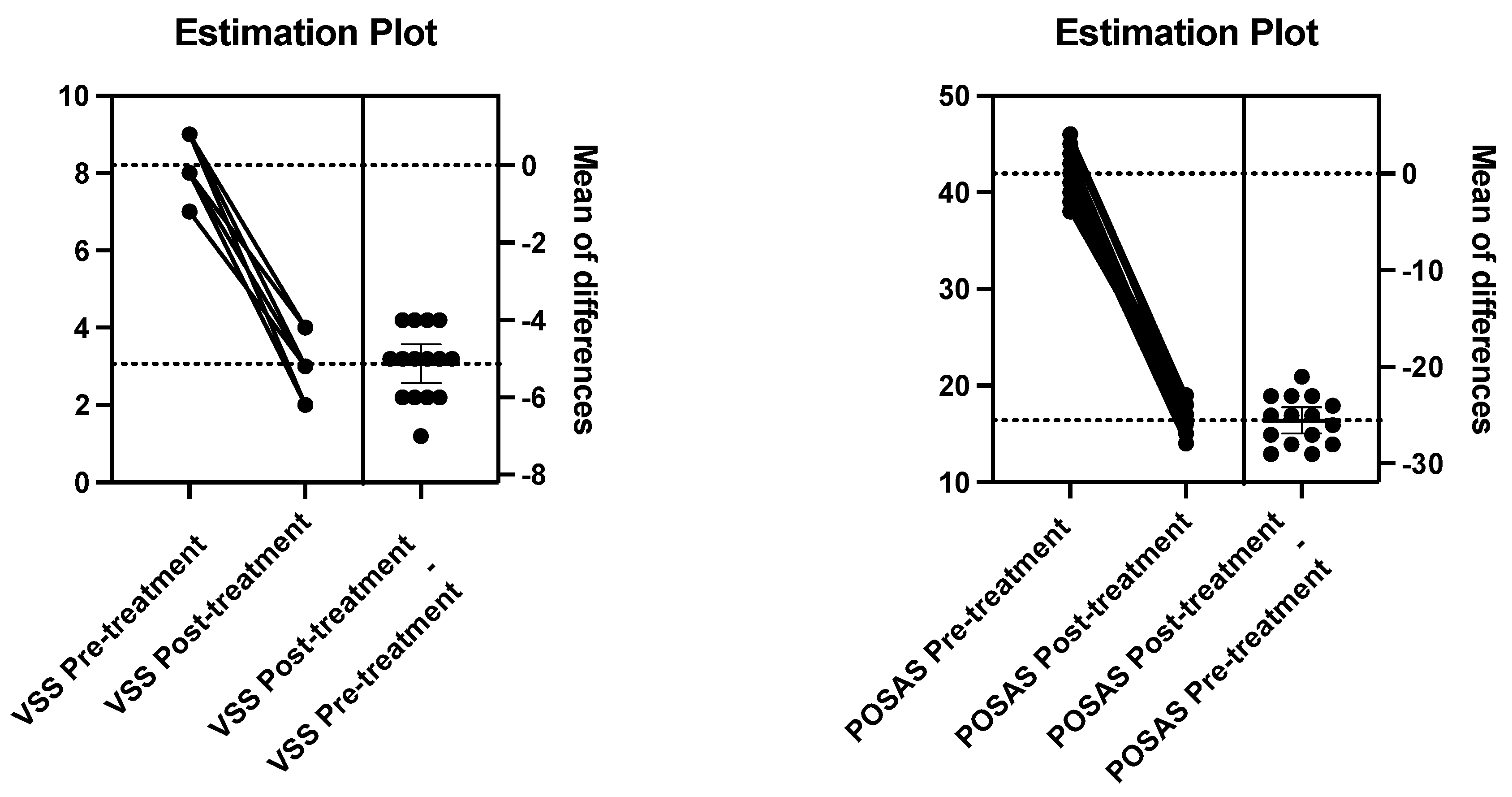
3.1. Changes in VSS and POSAS scores
Following the combined ablative CO2 laser and dye laser treatment, significant improvements were observed in both Vancouver Scar Scale (VSS) and Patient and Observer Scar Assessment Scale (POSAS) scores for ear keloids. The mean VSS score decreased from 8.4 ± 1.3 pre-treatment to 3.1 ± 1.0 post-treatment (
Table 4). A paired t-test revealed a statistically significant difference between the pre- and post-treatment VSS scores (t(14) = 15.92, p < 0.001), indicating a considerable improvement in scar characteristics. The corresponding estimation plot for VSS is presented in (
Figure 2A). Similarly, the total POSAS score, which includes both the Patient Scar Assessment Scale (PSAS) and the Observer Scar Assessment Scale (OSAS), showed a significant reduction from 42.6 ± 6.2 pre-treatment to 16.2 ± 5.1 post-treatment. (
Table 5) A paired t-test comparing the pre- and post-treatment POSAS scores also demonstrated a statistically significant difference (t(14) = 12.34, p < 0.001) (
Table 5). The corresponding estimation plot for POSAS is presented in (
Figure 2B). These results indicate the efficacy of the combined laser treatment in improving both the objective and subjective aspects of ear keloids.
To further highlight the significance of the improvements observed following the combined laser treatment, the effect sizes (Cohen's d) for the VSS and POSAS score improvements were also calculated. The effect size for the VSS score improvement was 3.48, suggesting a large treatment effect. Similarly, the effect size for the POSAS score improvement was 2.69, also indicating a large treatment effect.
Including statistical analyses such as paired t-tests and effect sizes in the results section provides a more comprehensive understanding of the study findings and their significance. By presenting the
estimation plots alongside the results of the statistical analyses, the study results are visually represented and can be easily interpreted by the reader.
Table 3.
VSS values, pre and post treatment.
Table 3.
VSS values, pre and post treatment.
Table 4.
mean pre and post treatment, pre and post treatment standard deviation, t value and p value of VSS.
Table 4.
mean pre and post treatment, pre and post treatment standard deviation, t value and p value of VSS.
Table 5.
:mean pre and post treatment, pre and post treatment standard deviation, t value and p value of POSAS.
Table 5.
:mean pre and post treatment, pre and post treatment standard deviation, t value and p value of POSAS.
Figure 2.
A and Figure 2B.
Figure 2.
A and Figure 2B.
3.2. Scar improvement
3.2.1. Chromaticity
After the combined laser treatment, patients experienced a notable reduction in scar redness and pigmentation, as evidenced by the significant decrease in the OSAS vascularization and pigmentation scores. This is consistent with previous studies on the efficacy of dye lasers in targeting hemoglobin and melanin, resulting in the normalization of the scar color 21.
3.2.2. Texture
The combined laser treatment led to a marked improvement in scar texture, as shown by the reduction in the VSS and POSAS relief scores. This can be attributed to the ablative CO2 laser's ability to induce controlled thermal damage, promoting collagen remodeling and the formation of new, organized connective tissue.
3.2.3. Pliability
The pliability of the keloid improved significantly after the treatment, as demonstrated by the decrease in the POSAS pliability score. This improvement can be attributed to the CO2 laser's collagen remodeling effects, which increase scar elasticity and flexibility.
3.3. Complete elimination of ear keloids
In contrast to surgical treatments and corticosteroid injections, which have high recurrence rates and limited success in treating ear keloids, this new treatment protocol successfully eliminated all ear keloids in the study, with a 100% success rate. This exceptional outcome is likely due to the synergistic effects of the ablative CO2 laser and dye laser, which target different aspects of scar formation and remodeling, leading to optimal scar improvement.
3.4. Adverse events
The combined laser treatment was well-tolerated by all patients, with no significant adverse events reported during the study. This finding supports the safety of the combined ablative CO2 laser and dye laser approach in the treatment of ear keloids.
By emphasizing the specific improvements observed in ear keloids and the 100% success rate of the combined laser treatment in eliminating them, the results section highlights the effectiveness and potential superiority of this protocol compared to other treatments, such as surgery or corticosteroid injections.
4. Discussion
Traditional treatment methods for ear keloids have primarily included surgical excision, intralesional corticosteroid injections, and silicone sheeting 13,15 .However, these approaches often yield variable results, and in some cases, they may exacerbate the keloids, lead to skin atrophy, or cause additional pain and discomfort 10,16.Notably, surgical and medical methods with steroid infiltrations have high relapse rates, and many patients included in this study had previously undergone unsuccessful treatments17 .In contrast, our study demonstrated that the combined ablative CO2 laser and dye laser treatment led to significant improvements in VSS and POSAS scores, indicating a superior outcome compared to traditional treatment methods. These findings are in line with previous research, which has reported the advantages of laser therapy for keloidst18,19
The combined treatment approach offers several advantages over traditional methods. Firstly, the ablative CO2 laser therapy effectively removes the superficial layers of the keloid by vaporizing the tissue, which subsequently stimulates collagen remodeling, leading to improved texture and pliability. This laser modulates collagen by decreasing fibroblast proliferation, increasing bFGF production (which reduces collagen synthesis), and inhibiting TGF-β1 secretion (which increases collagen synthesis) 20. The subsequent application of dye laser therapy, specifically the FPDL, targets the excessive vasculature in keloids, reducing erythema and normalizing skin color.
The FPDL plays a crucial role in controlling the scarring process by acting on fibroblasts, metalloproteinases, and their involvement in scars. It affects the blood vessels of keloids and hypertrophic scars through the concept of selective photothermolysis, in which the light energy emitted from the pulsed dye laser is absorbed by hemoglobin, generating heat 21. This leads to neocollagenesis, collagen fiber heating with dissociation of disulfide bonds, subsequent collagen fiber realignment, the release of histamine, or other biochemical factors that influence fibroblast activity 22,23. Studies have shown a decrease in the induction of TGF-β1 and upregulation of matrix metalloproteinase (MMP) expression in keloid tissue treated with an FPDL, favoring collagen degradation and fibroblast apoptosis 23.
Secondly, the combined approach is minimally invasive, reducing the risk of complications such as infection and skin atrophy, which are associated with corticosteroid injections and surgical excision 24,25. Moreover, the combined laser treatment has been shown to provide better cosmetic outcomes and patient satisfaction compared to traditional methods.
Early intervention is crucial in this type of scars, as non-responsive patients often present flap necrosis for various years. Studies on early laser intervention indicate favorable responses in a range of scar characteristics, including improved pliability, smoother surface, and reduced scar thickness 26. Laser treatments are established procedures to improve the clinical appearance of mature scars24 . In recent years, a preventative approach of minimizing scar formation by applying a laser during the wound healing process has increasingly been adopted 27.
Combining two laser treatments stimulates collagen production and remodeling, having a synergistic effect on the lesions. By using the CO2 laser to ablate tissue and modulate collagen synthesis, and the FPDL to control the scarring process by targeting fibroblasts and metalloproteinases, the combined approach effectively addresses both the appearance and the underlying physiological processes involved in keloid formation.
Our study provides valuable insights into the effectiveness of the combined ablative CO2 laser and dye laser treatment for ear keloids, demonstrating significant improvements in both VSS and POSAS scores. This innovative approach has the potential to become a reference for the resolution of ear keloids, a condition that affects many individuals worldwide. Further research is needed to validate these findings in larger cohorts and to optimize treatment parameters for maximum efficacy. Longitudinal studies could also investigate the long-term effects of this combined treatment approach, including the potential for keloid recurrence or complications.
5. Conclusions
In conclusion, our study demonstrates that the innovative combined treatment approach using ablative CO2 laser therapy followed by dye laser therapy is highly effective in the management of auricular keloids. The significant improvements in chromaticity, texture, pliability, and complete elimination of keloids highlight the superiority of this method compared to traditional treatments, such as surgical excision and corticosteroid injections, which often yield unsatisfactory outcomes and high recurrence rates.
Furthermore, the low incidence of adverse events and high patient satisfaction observed in our study showcase the safety and efficacy of this combined laser treatment. The results of this research hold clinical relevance and could revolutionize the management of auricular keloids, providing a more effective and reliable treatment option for patients who have experienced failed treatments in the past.
Considering the remarkable results obtained in our study, future research should focus on validating these findings in larger cohorts and exploring the potential of this combined laser approach in treating other types of scars and skin conditions. Moreover, the development of personalized treatment protocols based on individual patient characteristics and scar features could further enhance the effectiveness of this treatment method.
By building upon our findings, the field of laser therapy can continue to advance and offer increasingly sophisticated solutions to address a wide range of dermatological challenges. The adoption of this innovative combined treatment approach has the potential to establish a new standard of care for auricular keloids, ultimately improving the quality of life for those affected by this distressing and challenging condition.
Author Contributions
Conceptualization, validation, writing—review and editing: S.A. and G.C.; methodology, investigation, data curation S.A., G.C., S.G., A.M.R.; writing—original draft preparation S.A.; visualization, supervision S.P.N., C.L., E.B. and G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alster TS, Tanzi E. Improvement of neck and cheek laxity with a nonablative radiofrequency device: a lifting experience. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2004;30(4 Pt 1):503-507; discussion 507. [CrossRef]
- Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34(5):426-438. [CrossRef]
- Liu K, Wu XL, Wang PH. [Advances in therapy of auricular keloid]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016;51(12):945-948. [CrossRef]
- Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006;297(10):433-438. [CrossRef]
- Mustoe TA, Cooter RD, Gold MH, et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002;110(2):560-571. [CrossRef]
- Berman B, Bieley HC. Adjunct therapies to surgical management of keloids. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 1996;22(2):126-130. [CrossRef]
- van de Kar AL, Corion LUM, Smeulders MJC, Draaijers LJ, van der Horst CMAM, van Zuijlen PPM. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116(2):514-522. [CrossRef]
- Alster TS, West TB. Effect of topical vitamin C on postoperative carbon dioxide laser resurfacing erythema. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 1998;24(3):331-334. [CrossRef]
- O’Brien L, Jones DJ. Silicone gel sheeting for preventing and treating hypertrophic and keloid scars. Cochrane Database Syst Rev. 2013;2013(9):CD003826. [CrossRef]
- Manuskiatti W, Fitzpatrick RE, Goldman MP. Energy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585-nm flashlamp-pumped pulsed-dye laser. J Am Acad Dermatol. 2001;45(4):557-565. [CrossRef]
- Alster TS, Williams CM. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet Lond Engl. 1995;345(8959):1198-1200. [CrossRef]
- Ross EV, Naseef GS, McKinlay JR, et al. Comparison of carbon dioxide laser, erbium:YAG laser, dermabrasion, and dermatome: a study of thermal damage, wound contraction, and wound healing in a live pig model: implications for skin resurfacing. J Am Acad Dermatol. 2000;42(1 Pt 1):92-105. [CrossRef]
- Berman B, Flores F. The treatment of hypertrophic scars and keloids. Eur J Dermatol EJD. 1998;8(8):591-595.
- Ilișanu MA, Moldoveanu F, Moldoveanu A. Multispectral Imaging for Skin Diseases Assessment-State of the Art and Perspectives. Sensors. 2023;23(8):3888. [CrossRef]
- Ogawa R, Akaishi S, Kuribayashi S, Miyashita T. Keloids and Hypertrophic Scars Can Now Be Cured Completely: Recent Progress in Our Understanding of the Pathogenesis of Keloids and Hypertrophic Scars and the Most Promising Current Therapeutic Strategy. J Nippon Med Sch Nippon Ika Daigaku Zasshi. 2016;83(2):46-53. [CrossRef]
- Gold MH, McGuire M, Mustoe TA, et al. Updated international clinical recommendations on scar management: part 2--algorithms for scar prevention and treatment. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2014;40(8):825-831. [CrossRef]
- Al-Attar A, Mess S, Thomassen JM, Kauffman CL, Davison SP. Keloid pathogenesis and treatment. Plast Reconstr Surg. 2006;117(1):286-300. [CrossRef]
- Layton AM, Yip J, Cunliffe WJ. A comparison of intralesional triamcinolone and cryosurgery in the treatment of acne keloids. Br J Dermatol. 1994;130(4):498-501. [CrossRef]
- Tanzi EL, Alster TS. Side effects and complications of variable-pulsed erbium:yttrium-aluminum-garnet laser skin resurfacing: extended experience with 50 patients. Plast Reconstr Surg. 2003;111(4):1524-1529; discussion 1530-1532. [CrossRef]
- Scrimali L, Lomeo G, Tamburino S, Catalani A, Perrotta R. Laser CO2 versus radiotherapy in treatment of keloid scars. J Cosmet Laser Ther Off Publ Eur Soc Laser Dermatol. 2012;14(2):94-97. [CrossRef]
- Liu A, Moy RL, Ross EV, Hamzavi I, Ozog DM. Pulsed dye laser and pulsed dye laser-mediated photodynamic therapy in the treatment of dermatologic disorders. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2012;38(3):351-366. [CrossRef]
- Bouzari N, Davis SC, Nouri K. Laser treatment of keloids and hypertrophic scars. Int J Dermatol. 2007;46(1):80-88. [CrossRef]
- Kuo YR, Wu WS, Jeng SF, et al. Activation of ERK and p38 kinase mediated keloid fibroblast apoptosis after flashlamp pulsed-dye laser treatment. Lasers Surg Med. 2005;36(1):31-37. [CrossRef]
- Vrijman C, van Drooge AM, Limpens J, et al. Laser and intense pulsed light therapy for the treatment of hypertrophic scars: a systematic review. Br J Dermatol. 2011;165(5):934-942. [CrossRef]
- Cannarozzo G, Silvestri M, Tamburi F, et al. A new 675-nm laser device in the treatment of acne scars: an observational study. Lasers Med Sci. 2021;36(1):227-231. [CrossRef]
- Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW. 585-nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2003;29(1):65-73; discussion 73. [CrossRef]
- Tawfic SO, El-Tawdy A, Shalaby S, et al. Evaluation of Fractional CO2 Versus Long Pulsed Nd:YAG Lasers in Treatment of Hypertrophic Scars and Keloids: A Randomized Clinical Trial. Lasers Surg Med. 2020;52(10):959-965. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).