1. Introduction
Weight-bias internalization and eating-disorder psychopathology are two emerging psychological constructs with a relevant association with obesity. Weight bias refers to negative attitudes and manifested beliefs involving stereotypes, rejection and prejudice directed toward people who are perceived as having excess body weight [
1]. In contrast, internalized weight bias refers to people’s self-directed stigmatizing attitudes based on social stereotypes about their perceived weight status [
2]. Research has shown that a greater level of weight-bias internalization predicts lower core self-evaluation, which in turn predicts greater depression and anxiety, lower global health, and greater healthcare utilization [
3]. Internalized weight stigma is also significantly associated with greater eating-disorder psychopathology and depression, and lower perceived mental quality of life in adult patients with loss-of-control eating after sleeve-gastrectomy surgery [
4]. Interestingly, a study examining the frequency of experiencing weight stigma and physiological risk factors in patients with overweight/obesity found that weight stigma was significantly linked to cortisol levels, as well as higher levels of oxidative stress, concluding that weight stigma may contribute to the poor health underlying some forms of obesity [
5].
Only a few studies have evaluated the relationship between weight-bias internalization and eating-disorder psychopathology in patients with obesity [
6]. One study, on a community sample of 228 treatment-seeking adults with overweight or obesity, found that weight-bias internalization was positively associated with eating concerns, weight concerns and shape concerns [
7]. That study also tested the impact of weight-bias internalization on the relationship between perceived weight discrimination and eating pathology (including binge eating, emotional eating, bulimic symptoms and drive for thinness), revealing that weight-bias internalization mediates this relationship even after controlling for body mass index (BMI). Another study collected data on two large samples of college students to assess a theoretical model designed to collectively account for the intermediary role of weight-bias internalization and body dissatisfaction in associations between weight stigma experiences and a variety of eating-disorder behaviours across the weight spectrum [
8]. The data supported the proposed model, and, although patterns of associations differed among individuals with different BMIs, these variations were limited. Finally, two studies specifically investigated the relationship between overvaluation of shape and weight and weight-bias internalization. The first, using mediation analysis, found that overvaluation of shape and weight mediates the relationship between self-esteem and weight-bias internalization [
9]. The second, investigating the relationship between rumination and both overvaluation of shape/weight and eating-disorder psychopathology, found a significant positive association among these constructs [
10].
However, the abovementioned studies used the general constructs (latent variables) of weight-bias internalization and eating-disorder psychopathology to investigate their relationship. To date, no study has evaluated the complex array of reciprocal relationships among specific characteristics of the two constructs, rather than the latent constructs as a whole. Network analysis is a statistical method of enabling graphical and quantitative modelling of associations between constructs to identify specific relationships between clinical features and central symptoms (symptoms that are highly connected with other symptoms in the network) [
11]. With this in mind, network analysis was used to investigate the relationship between the single characteristics of eating-disorder psychopathology and weight-bias internalization in more depth in a sample of treatment-seeking patients with obesity.
2. Materials and Methods
2.1. Participants
The study sample comprised 2,113 patients with obesity admitted to the Villa Garda Hospital Department of Eating and Weight Disorders’ inpatient residential rehabilitative treatment programme between January 2016 and February 2023 upon completion of the baseline assessment. Eligibility criteria for this study were: age ≥18 years, BMI ≥30.0 kg/m
2; and Comprehensive Appropriateness Scale for the Care of Obesity in Rehabilitation (CASCO-R) global score >25. Of note, individuals with a CASCO-R score of >25 experience at least one weight loss-responsive comorbidity and several complications of obesity [
12]. Exclusion criteria were: pregnancy or lactation; any medications that affect body weight; severe psychiatric disorders (i.e., bulimia nervosa, substance-use disorders, bipolar and related disorders, or schizophrenia spectrum/other psychotic disorders), assessed via clinical interview; and any medical comorbidity associated with weight loss.
Approval for the study was granted by the GHC Institutional Review Board (Protocol Code 0005GHCIRB). Each participant provided informed written consent for collection of their clinical data, as well as its anonymous processing in a service-level research setting.
2.2. Measures
All study data was collected on the second day after admission to the unit. Specifically, this involved the admitting physician filling in the following measures on a case report form for each participant:
Weight (baseline), measured on medical weighing scales (Seca Digital Wheelchair Scale Model 664)
Height, measured on a stadiometer (Wall-Mounted Mechanical Height Rod Model 00051A; Wunder)
BMI, calculated using the standard formula (i.e., body weight (kg) divided by height (m) squared).
Eating-disorder features, assessing responses to the Eating Disorder Examination interview (EDE), Italian version [
13]. This semi-structured questionnaire is designed to evaluate eating-disorder psychopathology and behaviours in the 28 days before the interview is conducted. Specifically, scores of 0–6 are assigned to the behavioural symptoms (binge eating, self-induced vomiting, laxative misuse, diuretics misuse, excessive exercising and food restriction) exhibited by individuals with eating disorders. EDE scores can be expressed on a global scale, but also four specific subscales (Restraint, Eating Concern, Weight Concern and Shape Concern) reflecting the respective cognitive features. Excellent criterion validity and high test–retest reliability (r = 0.80) have been reported for the Italian version of the EDE, whose global score has very good inter-rater reliability (rho = 0.97) [
13]. In our sample, Cronbach’s α for the global EDE score was 0.85. For the purposes of this study, the 22 items used to generate the four subscales and the global score were considered. The EDE was administered by assessors trained and supervised by RDG, an expert on the instrument.
Weight-bias internalization, assessed using the Italian version of the Weight Bias Internalization Scale (WBIS) [
14]; this relies on a total of 11 items, rated on a seven-point Likert scale, to measure self-directed weight-related stigma. The Cronbach’s α for the global WBIS score was 0.80 in our sample.
2.3. Statistical analysis
SPSS, version 27, was used for data processing and descriptive analysis, while network analysis was conducted via R software, version 3.5.2 [
15] in the RStudio environment RStudio 2023.03.0+386. Variables are presented either as means and standard deviations or frequencies and percentages, as appropriate. According to the Shapiro–Wilk normality test, study variables were not normally distributed, so nonparametric correlations were calculated using nonparanormal transformation [
16].
2.3.1. Network estimation
The qgraph Rpackage was used to perform the network analysis [
17]. Regularized partial correlation networks [
18] were estimated using EBIC graphical LASSO [
19]; when data points were ordinal, polychoric correlations served as input. As regularization applies an extra penalty for model complexity when estimating statistical model, and the resulting models are conservative and easier to interpret [
20]; indeed, small or unstable correlations are estimated to be zero, thereby removing the connections between nodes (the network “edges”) that are less likely to be meaningful.
Fit optimization of the networks generated in this manner was carried out by minimizing the Extended Bayesian Information Criterion (EBIC) [
21], an approach that is reportedly very effective at revealing the true network structure [
22,
23], and thereby facilitates selection of the best network; the approach functions particularly well when the generating network is sparse, containing a limited number of edges.
In order to identify nodes measuring the same underlying construct, the goldbricker function (Rpackage networktools) was used with the threshold set at 0.25; the net reduce function was applied to combine all node pairs falling below this threshold.
2.3.2. Bridge nodes
The degree to which a node in one cluster relates to nodes in another cluster can be assessed via bridge metrics. The expected influence of a bridge is the sum of the values of all edges that connect a particular node to all nodes that do not belong to the same community [
24]; this approach can be used to quantify the strength and directionality of all the associations a node displays in a specific cluster. In this case, it highlighted the relationship between nodes in the eating disorder cluster (all EDE items and BMI) with nodes in the weight-bias internalization cluster (all WBIS items). The node with the highest bridge centrality (see below) within each cluster were identified as the bridge node.
2.3.3. Centrality indices
The centrality indices of the network structure generated were calculated as a means of evaluating the relative importance of each of its nodes [
18,
25]. The expected influence (EI) of the node centrality index was then calculated and normalized (mean = 0 and standard deviation (SD) = 1). This is a means of quantifying the strength and directionality of the relationships each node has with the other nodes [
18], with a value of <1 indicating that the EI is <1 SD from the mean.
2.3.4. Network robustness, stability and accuracy
The robustness of each resulting network was estimated via calculation of the accuracy of edge weights in each network; the accuracy of the edge weights was calculated by generating nonparametric bootstrapped 95% confidence intervals (CIs) around the original edge values (n boots = 5000) [
19], with narrower CIs indicating greater accuracy [
19]. Pairwise bootstrapped difference testing (n boots = 5000) was then used to identify any significant differences between the two networks’ edge weights and the centrality index [
18].
The EI stability was also calculated for portions of the data, following the procedure suggested by Epskamp et al. [
18]. This involved random sampling of networks of nodes a thousand times, and then calculation of subset bootstraps and correlation stability (CS) coefficients. To allow interpretation of differences in centrality, the CS coefficient must be no lower than 0.25, and preferably above 0.5 [
18]. This can be taken as the greatest proportion of cases that can be dropped while preserving at 95% the probability of the correlation between the original centrality index and the centrality of networks based on subsets being 0.7 or greater.
3. Results
3.1. Patient characteristics
The sample comprised 2,113 treatment-seeking patients with obesity, more than half of whom were female (65.4%); the mean age was 55.0 years (SD=14.0), and the mean BMI was 41.6 kg/m2 (SD=7.9).
3.2. Network structure
The network analysis encompassed all 11 WBIS items, the 22 items of the EDE interview, and the BMI, making a total of 34 items.
Table 1 details each variable included in the network. The goldbricker function indicated no overlap among variables.
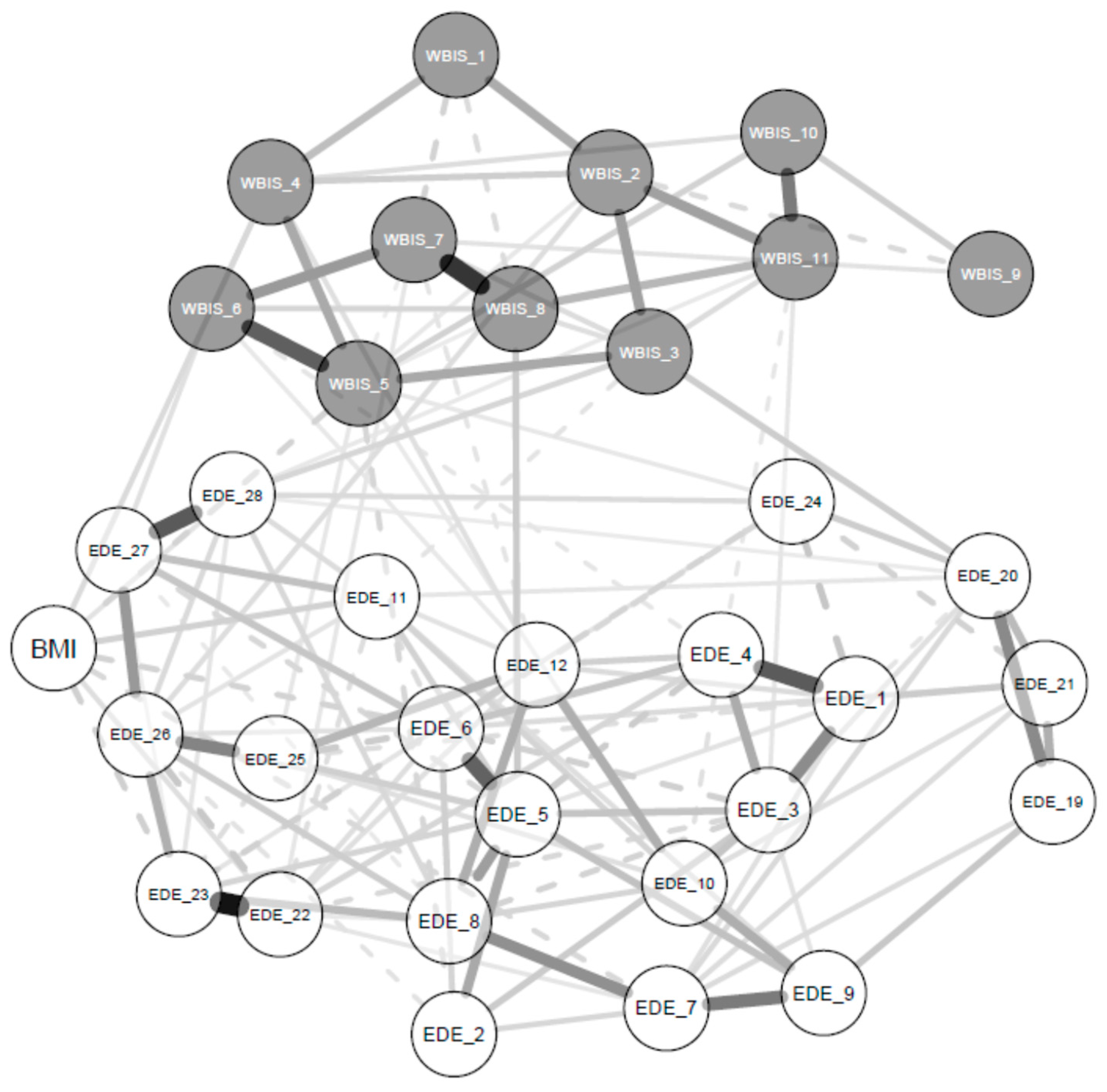
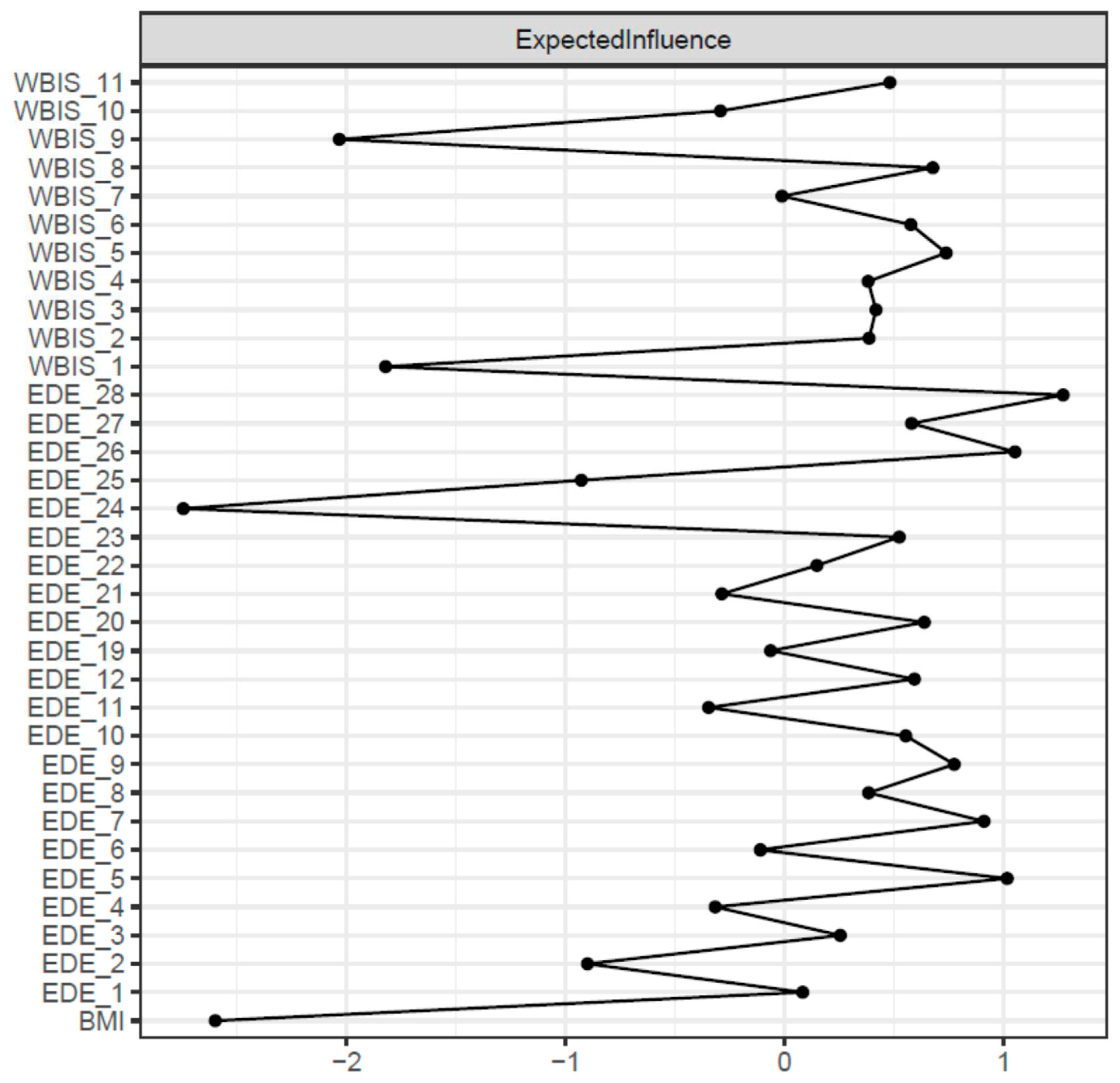
Figure 1 and
Figure 2 show the network structure and expected influence values for the global sample. Nodes presenting higher expected influence were all EDE items, specifically: ‘avoidance of exposure’ (EI = 1.27), ‘dissatisfaction with shape’ (EI = 1.04), and ‘wanting an empty stomach’ (EI = 1.00). Node strengths were stable, and the CS coefficient for EI was 0.67 (a cut-off of 0.5 is required to consider the metric stable) (
Figure 1S).
The bootstrapped difference test for EI values showed that EDE ‘avoidance of exposure’, ‘dissatisfaction with shape’ and ‘wanting an empty stomach’ had significantly greater EI centrality than other symptoms (
Figure 2S). The bootstrapped 95% CIs around the estimated edge weights indicated that many of the edge weights did not significantly differ from one another (
Figure 3S).
Analysis of the bridge nodes indicated that in the specific eating-disorder psychopathology cluster the greatest bridge EI corresponded to EDE ‘avoidance of exposure’. In the weight-bias internalization cluster, on the other hand, the greatest bridge EI corresponded with WBIS ‘I wish I could drastically change my weight’ (
Figure 4S). However, the bootstrap difference test on the bridge EIs indicated non-significant centrality differences, thereby failing to confirm the role of the two nodes as bridge nodes. (
Figure 5S).
4. Discussion
This study used a network approach to assess the relationships between weight-bias internalization and eating-disorder psychopathology in a large sample of treatment-seeking patients with obesity. There were two main findings.
Upon inspection of the network, the first finding was that certain symptoms, namely exposure avoidance, shape dissatisfaction and wanting an empty stomach, all in the eating-disorder psychopathology cluster, were central nodes with strong connections to all the other eating-disorder and weight-stigma variables in the network. Avoidance of exposure and dissatisfaction with shape, two items on the EDE shape concern subscale, represent cognitive and behavioural features of body image dissatisfaction. Several studies have suggested a positive relationship between body image dissatisfaction and obesity [
26,
27,
28], and a meta-analysis of 17 quantitative studies on adult samples found that individuals with obesity reported greater body dissatisfaction than normal-weight individuals [
29]. However, the specific features of body image dissatisfaction in patients with obesity individuated in this study may shed light on the most influential psychological mechanism related to eating-disorder psychopathology and weight-bias internalization; these features could, more so than others, provide the motivation to seek treatment in patients with obesity. In addition, the identification of the desire to have an empty stomach as a central node in the network reflects the relevant role of this feature in patients with obesity. This feature, measured via the EDE restraint subscale, is similarly influential in underweight patients with eating disorder [
30,
31], indicating that it could be an important factor in eating-disorder psychopathology and weight-bias internalization due to its interpretation in terms of control over eating and weight, at least in treatment-seeking patients with obesity.
The second finding from our analysis was that the bridges nodes linking the two separate constructs are not stable, with non-significant centrality differences among nodes. Explaining this finding is complex. Nevertheless, we hypothesize that the two constructs (eating-disorder psychopathology and weight-bias internalization) were made up of very similar variables, with comparable relationship strengths between them, and that the two latent variables measured are only artificially constructed in patients with obesity. However, it could also signify that all nodes are potentially relevant as bridges between eating-disorder psychopathology and weight-bias internalization. This hypothesis is also supported by a visual inspection of the network, which displays strong associations among nodes and an absence of peripheral, unconnected nodes.
The study had three main strengths. First, to our knowledge it is the first to use a network approach to investigate the interconnections between eating-disorder psychopathology and weight-bias internalization in a large sample of patients with obesity. Second, the very large sample permits conclusions about the population of treatment-seeking patients with obesity to be drawn. Third, the use of the EDE interview, conducted by a clinician expert in eating disorders and obesity, to assess the eating-disorder psychopathology provides confidence in the accuracy and reliability of evaluation of these features.
However, the study does present some limitations. The first is that all patients were seeking treatment, and therefore no inference can be drawn regarding the general population of individuals with obesity. Another limitation is the cross-sectional nature of the study, which prevents inferences about the directionality of the relationships we detected to be made. This means that we are not in a position to draw conclusions about clinical treatment, and we can merely point towards avenues for future research.
Future studies should explore the network structure of psychological constructs in obesity in more depth to provide additional knowledge on these mechanisms.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1,
Figure 1S. Average correlations between centrality indices of networks sampled with persons dropped and the original sample. Lines indicate the means, and areas indicate the range from the 2.5
th quantile to the 97.5
th quantile.
Figure 2S. Bootstrapped difference tests (α = 0.05) for centrality within the network. Nodes are presented in descending order of centrality. Values on the diagonal indicate the unstandardized centrality estimates for each node. Black boxes indicate significant centrality differences, meaning that the bootstrapped difference 95% CI does not span 0. Grey boxes indicate non-significant centrality differences, meaning that the bootstrapped difference 95% CI spans 0. See
Table 1 for items corresponding to each node.
Figure 3S. Bootstrapped 95% confidence intervals (CIs) of estimated edge weights for the network. The red line indicates the sample values, and the grey area the bootstrapped 95% CIs. Each horizontal line represents one edge of the network, ordered from the edge with the highest weight to that with the lowest. The y-axis labels have been removed to avoid cluttering.
Figure 4S. Bridge expected influence among the eating-disorder psychopathology and weight-bias internalization symptoms network. See
Table 1 for items corresponding to each node.
Figure 5S. Bootstrapped difference tests (a = 0.05) for expected influence of bridges within the network. Nodes are presented in descending order of centrality. Black boxes indicate significant centrality differences, meaning that the bootstrapped difference 95% CI does not span 0. Grey boxes indicate non-significant centrality differences, meaning that the bootstrapped difference 95% CI spans 0. See
Table 1 for items corresponding to each node.
Author Contributions
Conceptualization, R.D.G. and S.C.; methodology, S.C.; formal analysis, S.C., B.S.; data curation, G.C., M.C., A.D.G, L.D., M.M.; writing—original draft preparation, B.S. and S.C.; writing—review and editing, R.D.G. and S.C.; supervision, R.D.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the GHC Institutional Review Board (Protocol Code 0005GHCIRB).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Informed written consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, SC, upon reasonable request.
Conflicts of Interest
The authors have no conflict of interest to declare.
References
- Puhl, R.; Brownell, K.D. , Bias, discrimination, and obesity. Obes. Res., 2001, 9, 788–805. [Google Scholar] [CrossRef]
- Durso, L.E.; Latner, J.D., Understanding self-directed stigma: development of the weight bias internalization scale. Obesity, 2008, 16 Suppl 2, S80-6. [CrossRef]
- Allegato B alla DGR n. 94, Scheda di appropriatezza della regione veneto per il ricovero riabilitativo intensivo dei disturbi del comportamento alimentare. Regione Veneto: Venezia, 2012.
- Lawson, J.L.; LeCates, A.; Ivezaj, V.; Lydecker, J.; Grilo, C.M. , Internalized weight bias and loss-of-control eating following bariatric surgery. Eat Disord, 2021, 29, 630–643. [Google Scholar] [CrossRef] [PubMed]
- Tomiyama, A.J.; Epel, E.S.; McClatchey, T.M.; Poelke, G.; Kemeny, M.E.; McCoy, S.K.; Daubenmier, J. , Associations of weight stigma with cortisol and oxidative stress independent of adiposity. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 2014, 33, 862–867. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M. , Weight bias internalization and health: A systematic review. Obes. Rev., 2018, 19, 1141–1163. [Google Scholar] [CrossRef] [PubMed]
- Durso, L.E.; Latner, J.D.; Hayashi, K. , Perceived discrimination is associated with binge eating in a community sample of non-overweight, overweight, and obese adults. Obes Facts, 2012, 5, 869–880. [Google Scholar] [CrossRef] [PubMed]
- Romano, K.A.; Heron, K.E.; Henson, J.M. , Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: Does weight status matter? Body Image, 2021, 37, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L.; White, M.A.; Grilo, C.M. , Overvaluation of shape and weight as a mediator between self-esteem and weight bias internalization among patients with binge eating disorder. Eat Behav, 2014, 15, 259–261. [Google Scholar] [CrossRef]
- Wang, S.B.; Lydecker, J.A.; Grilo, C.M. , Rumination in patients with binge-eating disorder and obesity: Associations with eating-disorder psychopathology and weight-bias internalization. Eur Eat Disord Rev., 2017, 25, 98–103. [Google Scholar] [CrossRef]
- Borsboom, D. , A network theory of mental disorders. World Psychiatry, 2017, 16, 5–13. [Google Scholar] [CrossRef]
- Donini, L.M.; Dalle Grave, R.; Di Flaviano, E.; Gentile, M.G.; Mezzani, B.; Pandolfo Mayme, M.; Brunani, A.; Rovera, G.; Santini, F.; Lenzi, A.; Cuzzolaro, M. , Assessing the appropriateness of the level of care for morbidly obese subjects: validation of the CASCO-R scale. Annali di igiene: medicina preventiva e di comunita, 2014, 26, 195–204. [Google Scholar] [CrossRef]
- Calugi, S.; Ricca, V.; Castellini, G.; Lo Sauro, C.; Ruocco, A.; Chignola, E.; El Ghoch, M.; Dalle Grave, R. , The Eating Disorder Examination: Reliability and validity of the Italian version. Eat. Weight. Disord., 2015, 20, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Innamorati, M.; Imperatori, C.; Lamis, D.A.; Contardi, A.; Castelnuovo, G.; Tamburello, S.; Manzoni, G.M.; Fabbricatore, M. , Weight Bias Internalization scale discriminates obese and overweight patients with different severity levels of depression: The Italian version of the WBIS. Current Psychology, 2017, 36, 242–251. [Google Scholar] [CrossRef]
- Team, R.C., R: A language and environment for statistical computing. . R Foundation for Statistical Computing: Vienna, Austria, 2018.
- Zhao, T.; Liu, H.; Roeder, K.; Lafferty, J.; Wasserman, L. , The huge package for high-dimensional undirected graph estimation in R. J Mach Learn Res, 2012, 13, 1059–1062. [Google Scholar]
- Epskamp, S.; Cramer, A.O.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. , qgraph: Network visualizations of relationships in psychometric data. Journal of statistical software, 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. , Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods, 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Epskamp, S.; Fried, E.I. , A tutorial on regularized partial correlation networks. Psychol. Methods, 2018, 23, 617–634. [Google Scholar] [CrossRef]
- Epskamp, S.; Kruis, J.; Marsman, M., Estimating psychopathological networks: Be careful what you wish for. PLoS One, 2017, 12 (6), e0179891. 0179. [CrossRef]
- Chen, J.; Chen, Z. , Extended Bayesian information criteria for model selection with large model spaces. Biometrika, 2008, 95, 759–771. [Google Scholar] [CrossRef]
- Barber, R.F.; Drton, M., High-dimensional Ising model selection with Bayesian information criteria. 2015.
- Foygel, R.; Drton, M., Extended Bayesian information criteria for Gaussian graphical models. Adv. Neural Inf. Process. Syst., 2010, 23.
- Levinson, C.A.; Brosof, L.C.; Vanzhula, I.; Christian, C.; Jones, P.; Rodebaugh, T.L.; Langer, J.K.; White, E.K.; Warren, C.; Weeks, J.W.; Menatti, A.; Lim, M.H.; Fernandez, K.C. , Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. Int. J. Eat. Disord., 2018, 51, 693–709. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O. , State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality, 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Yokoyama, H.; Nozaki, T.; Nishihara, T.; Sawamoto, R.; Komaki, G.; Sudo, N. , Factors associated with the improvement of body image dissatisfaction of female patients with overweight and obesity during cognitive behavioral therapy. Front Psychiatry, 2022, 13, 1025946. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Czepczor-Bernat, K.; Modrzejewska, A. , The relationship between eating patterns, body image and emotional dysregulation: similarities between an excessive and normal body weight sample. Psychiatr. Pol., 2021, 55, 1065–1078. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Cuzzolaro, M.; Calugi, S.; Tomasi, F.; Temperilli, F.; Marchesini, G.; Group, Q.S. , The effect of obesity management on body image in patients seeking treatment at medical centers. Obesity, 2007, 15, 2320–2327. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, N.A.; Kersting, A.; Riedel-Heller, S.G.; Luck-Sikorski, C. , Body dissatisfaction in individuals with obesity compared to normal-weight individuals: A systematic review and meta-analysis. Obes Facts, 2016, 9, 424–441. [Google Scholar] [CrossRef] [PubMed]
- Shafran, R.; Fairburn, C.G.; Nelson, L.; Robinson, P.H. , The interpretation of symptoms of severe dietary restraint. Behav Res Ther, 2003, 41, 887–894. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Di Pauli, D.; Sartirana, M.; Calugi, S.; Shafran, R. , The interpretation of symptoms of starvation/severe dietary restraint in eating disorder patients. Eat. Weight. Disord., 2007, 12, 108–113. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).