1. Introduction
The coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The infection had spread rapidly from China to other countries across the Asia [
1,
2]. By the end of January 2020, the first COVID-19 cases were reported in United States of America, France, Germany, United Kingdom, Italy and Russia, and the World Health Organization (WHO) announced the outbreak of COVID-19 soon after [
3,
4]. In February 2020 first cases were detected in Spain and Iran, while in the Republic of Srpska (Bosnia and Herzegovina) the first case was identified on March 4, 2020 (4,5). Few days later, on March 11, 2020 the first case of COVID-19 was reported in Turkey and the same day the WHO announced COVID-19 as the pandemic [
3,
4]. The virus spread rapidly during spring 2020 due to several factors such as low level of disease awareness, insufficient prevention and control of the infection, the lack of available laboratory testing, medical supplies and delay of initial treatment. It should be emphasized that the virus was novel and the world population was immune-naive. Furthermore, there were a lot of asymptomatic cases or cases with very mild symptoms causing the identification of the virus more difficult [
5].
The first COVID patient in the Republic of Srpska was identified in the city of Banja Luka, which is the biggest city of the Republic of Srpska [
5]. Afterwards three persons were identified by contact tracing and this first cluster was promptly closed. The following social events and additional imported cases, from Italy and Austria, have caused fast spreading of the SARS-COV-2 in the city [
6]. During the first three months of 2020, the Government, health authorities and health care institutions in the Republic of Srpska undertook numerous measures in order to control the epidemic and to manage patients with COVID-19 infection. The activities were focused to monitoring of the epidemiological situation, providing adequate information to the public, implementing precaution measures, recruiting all available health professionals, developing the set of guidance for health care professionals, and reverse transcriptase polymerase chain reaction (RT-PCR) testing for COVID-19 suspected individuals. Although all epidemiological interventions were implemented, the city of Banja Luka has become the biggest cluster in the country.
From March to May 2020 the lockdown measures were implemented in the Republic of Srpska, in order to slow down the spread of epidemic in the country. During the first few months of epidemic, all COVID-19 patients were isolated in hospitals or in facilities designated for isolation of COVID-19 patients – County quarantines. After the number of cases significantly increased, patients with mild to moderate symptoms of COVID-19, as well as contacts of confirmed and probable COVID-19 cases, had to be isolated at their homes,. On a daily bases those patients were contacted by family medicine (FM) teams. Data on patients` status were recorded in COVID-19 application of Web-Medic data base of the primary health care system. The Web-Medic data electronic platform has been used by FM teams since 2009 for daily routine work. During 2020, the COVID-19 application was installed in order to record epidemiological and clinical data related to COVID-19 patients and their contacts. The FM teams have been assigned to evaluate symptoms and if necessary to organize patient's transportation to laboratory, radiological diagnostic centre, or to hospital. While epidemiologists have carried out contact tracing, the FM teams were obliged to evaluate health status of identified contacts in the time of their quarantine in order to decide if the medical examination was needed. It was important to assess clinical symptoms, to collect data on patients’ demographic characteristics and comorbidities, hence to decide on management of COVID-19.
Occurrence of symptoms in COVID-19 patients and their contacts were mandatory notified in the surveillance form by FM teams on a daily basis. Since the beginning of COVID-19 pandemic, it has been clearly evident that serious form of COVID-19 primarily affects patients with chronic conditions such as: cardiovascular disease, hypertension, chronic obstructive pulmonary disease, diabetes mellitus, obesity and cancer [
7,
8,
9]. Recently published study showed a strong relationship between patient`s socio-demographic characteristics, comorbidities and COVID-19 outcomes [
10].
At the beginning of pandemic, the burden of disease fallen on hospitals, but soon after the epidemiological situation has evolved, the primary health care become the first defence line obliged to respond properly in order to deliver appropriate services for growing number of COVID-19 patients [
11]. There have been many different ways for FM teams to meet the needs of SARS-CoV-2 positive patients and persons at risk of serious COVID-19 infection. Patients with mild symptoms of COVID-19 were followed by FM teams in County quarantines during May and June 2020. After quarantine for contacts and isolation for milder cases were transferred to the home settings, phone consultations were used for assessing the progress of COVID-19 symptoms and planning further diagnostic and treatment procedures. Patients with respiratory symptoms were examined by FM teams in ambulances for acute respiratory infections (ARI) and if needed they were tested on SARS-CoV-2.
The aim of this study was to explore the epidemiological characteristics and clinical risk factors associated with the COVID-19 patients’ outcomes at the primary health care (PHC) centre of Banja Luka County during six waves of epidemic.
2. Materials and Methods
The study was conducted at the PHC center during the period from March 2020 to September 2022. The study included all reported citizens of Banja Luka County who were confirmed and registered as RT-PCR positive on COVID-19. Banja Luka is the capital city of the Republic of Srpska, and the second biggest city in Bosnia and Herzegovina, with total population of 250,000 people, and PHC center was responsible to organize health care through specialized units for COVID-19 patients.
Epidemiological data were obtained from Web-Medic medical records of patients being registered with FM teams in PHC center. The COVID-19 data were obtained from COVID-19 data sheets comprised of patient’s RT-PCR testing forms, surveillance forms for SARS-CoV-2 status, and the map of their positive and isolated contacts. Only the patients’ medical records with completed testing forms were included in the study. Data from the patients who were still on treatment and/or in hospital were not included in the study. Using these criteria 40,692 participants were included in the study.
The patients’ records data were classified as: basic demographics data (age, gender), COVID-19 related data (disease beginning date, laboratory test date, disease end date, hospitalization and disease outcome, death date), symptoms (fever, cough, sore throat, headache, diarrhea, loss of smell and taste), risk factors (smoking, obesity, cancer, hypertension, hyperlipidemia, diabetes). Disease beginning date was calculated from records as a date when the first symptoms started, or as medical examination date.
The results are presented as count (percent) or mean ± standard deviation, depending on data type. Differences regarding the distributions of patients between groups (death/alive and hospitalization/no hospitalization) were analyzed using Pearson chi square test and Mantel-Haenszel chi square test for trends, while differences in mean values were compared using independent samples t test. Relationship between mortality and independent variables were examined using logistic regression, univariable and multivariable analyses.
In this study, all p values less than 0.05 were considered significant. All data were analyzed using SPSS 29.0 (IBM corp.) for Windows.
3. Results
The study included 40692 patients, both genders, minimum age 0 and maximum age 98 years. Distribution of patients with their demographic characteristics in total and by regarding the hospitalization status and lethal outcome is presented in
Table 1.
The average age of hospitalized patients was significantly higher than the age of non-hospitalized patients (64.2±16.1 vs. 45.4±18.7; p<0.001). The average age of patients with lethal outcome was nearly twice higher compared to patients with non-lethal outcome (74.6±11.5 vs. 45.7±18.6; p<0.001).
The youngest patients with lethal outcomes were in 20-29 age group, three females and two males, four died in 2021 while one died in 2022. One person had hypertension while the other one had cancer. Other three persons had no significant risk factors.
Among the 30-39 age group, 9 were females, 4 were males. Two of them had cancer, one had chronic renal insufficiency, and two are smokers. Other patients with lethal outcome had no serious comorbidities. As shown in the
Table 1, the probability of lethal outcome significantly increases with age, being highest in the oldest group. The hospitalization rate had similar trend. Using Mantel-Haenszel chi square test for trend, the significant positive linear trend is observed across age categories regarding the hospitalization and death rate. Male patients had higher hospitalization and mortality rate, compared to females.
The most frequent risk factors were hypertension, obesity, and hypercholesterolemia. The highest hospitalization rate was in CRF, diabetics and heart comorbidity patients while the death rate was the highest among patients with CRF and hearth comorbidities. All risk factors were significant predictors of hospitalization and mortality, except smoking for death outcome (
Table 2). Smokers had less probability for lethal outcome and hospitalization. However, after adjusting for age (older than 18), the smoking becomes favorable significant factor for the lethal outcome (OR=1.260; 95% CI 1.036-1.532). Vaccinated patients had higher rate of hospitalization, but significantly lower rate of lethal outcome. However, the vaccination started during pandemic and the number of doses significantly correlates with the protection from lethal outcome and hospitalization.
Concerning the clinical signs and symptoms, the fever was the most common one, presented in two thirds of patients and followed with cough and fatigue. One quarter of patients had loss of smell and taste. The presence of fever, couth, fatigue, nausea and vomiting, chest pain, shortness of breath and appetite lost favored hospitalization while the patients with diarrhea, throat pain, loss of smell and taste were less probable for hospitalization (
Table 3). Fever, cough, diarrhea, nausea and vomiting and chest pain and shortness of breath were not significant predictors of death outcome. Contrary, fatigue and appetite loss were symptoms significantly dominant in lethal outcome patients, while throat pain, loss of smell and taste, headache, myalgia and arthralgia and rhinitis were symptoms of less probable lethal outcome.
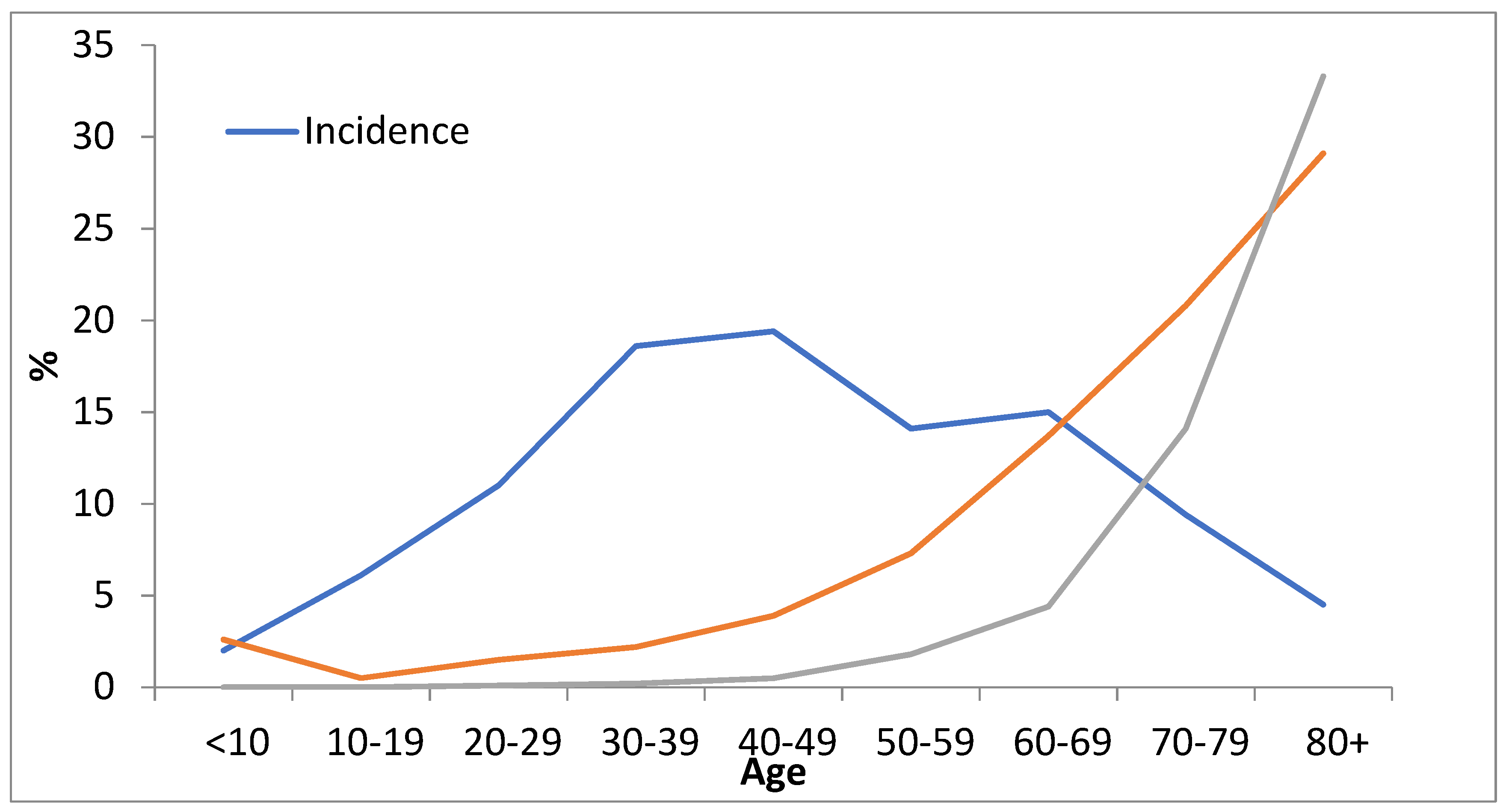
The incidence rate was the highest in 30-39 and 40-49 groups while the hospitalization and death rate had evident positive correlation with age (the higher the age group, the higher the hospitalization and death rates) (
Figure 1). Even though the 30-39 and 40-49 age groups are dominant for incidence, significant increase of hospitalization starts in 50-59 groups, while significant death rate starts in 70-79 age groups. The age above 70 was absolute risk factor for hospitalization and/or lethal outcomes.
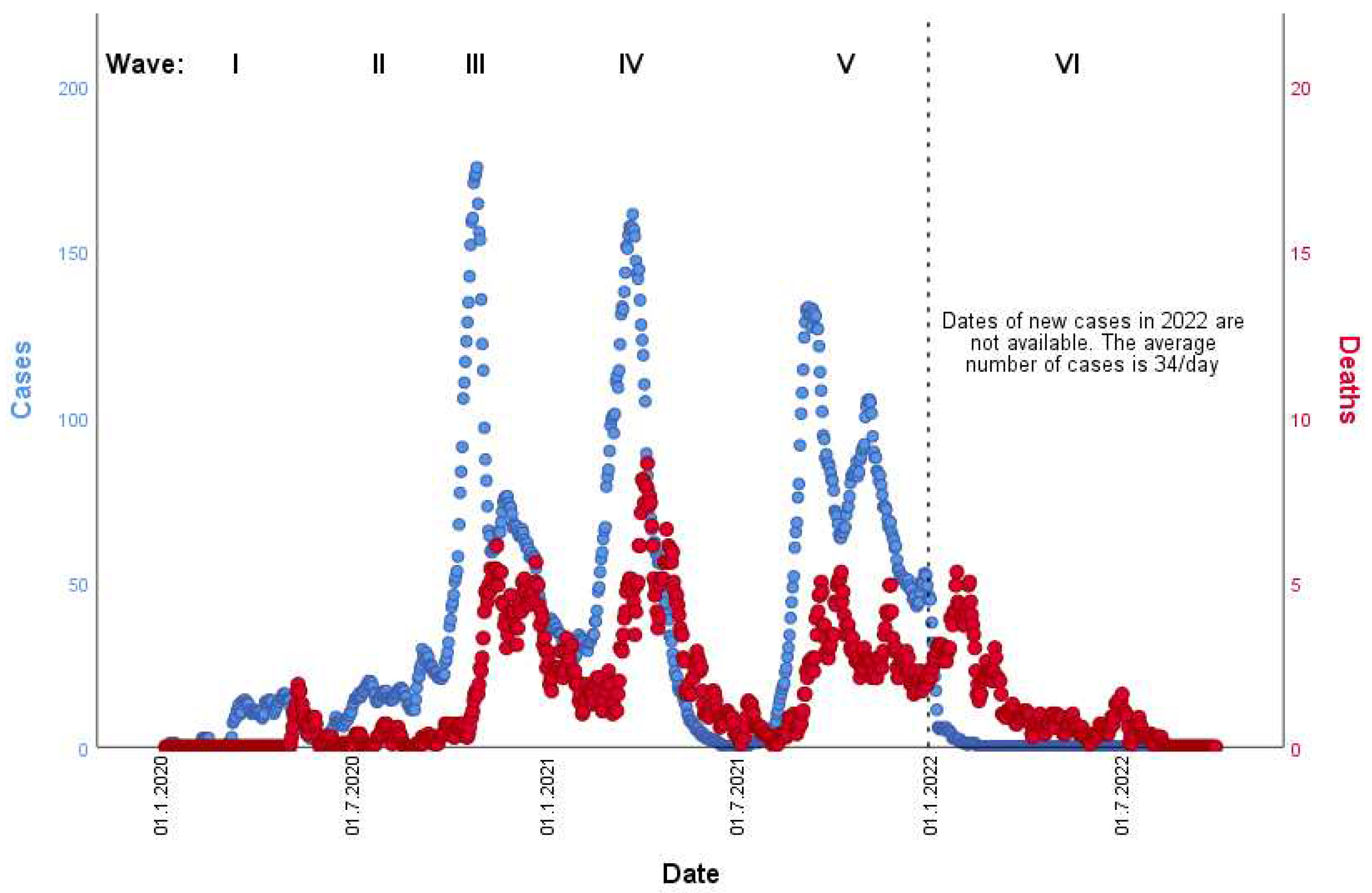
The number of newly diagnosed cases and the number of deaths by date is presented in
Figure 2. There is obvious increase of death rate (with few weeks delay) in the period of six (incidence) waves. While the first/second ones were rather low, the third, fourth, and fifth waves had significantly higher incidence and mortality rates. The third and fifth waves had two peaks, but first significantly higher in third wave, and similar in the fifth wave. The sixth wave was significantly lower to previous three and more like first wave. The number of deaths increased approximately 2-3 weeks after the beginning of each incidence peak.
4. Discussion
In this study, there were 40692 COVID-19 patients, with women slightly overrepresented. The similar proportion was present in Spain, where SARS-CoV-2 positivity was higher in females [
12]. Contrary to those findings, the majority of COVID-19 patients in the United States were males [
13]. Data analysis from 177 countries/territories in 4 continents/regions resulted in higher incidence of COVID-19 in females, while mortality rate was higher in males [
14].
The average age of hospitalized patients or patients with lethal outcome in our study was significantly higher in comparison with non-hospitalized patients. The lethal outcomes significantly increased with age, and was the highest among the elderly (70+ years of age), while majority of young patients recovered successfully, what is similar with study results from the Chongqing Three Gorges Central Hospital in China [
15]. Although majority of patients in our study were younger than 50, the highest percentage of all death cases were from the group of patients over 80. The male patients were overrepresented. Similar to our study, results of the Spanish study which was conducted in primary care setting showed that a mean age of COVID-19 patients with lethal outcome was 83 years, mostly males [
12]. Those data along with other studies [
16,
17] clearly showed that sex and age could be considered as risk factors for COVID-19 related deaths. Results of nationwide study in Tunisia showed faster recovering of younger patients as well as healthcare workers [
18]. Results of the study on seroprevalence of SARS-CoV-2 antibodies in the Republic of Srpska confirmed that younger population had higher seroprevalence values and less hospitalization [
19].
Concerning comorbidities and risk factors analysed by many authors [
20,
21,
22,
23,
24], obesity, hypertension, hyperlipidaemia, diabetes, CRF and CVD were significant predictors for hospitalization and mortality in our study. Smokers had less probability for lethal outcome and hospitalization. However, after adjusting for age, the smoking becomes favourable significant factor for the lethal outcome. Higher proportion of smoking and comorbidities were founded in males in the USA [
13]. Smoking, kidney disease, obesity, pulmonary disease, diabetes and CVD were significant factors for hospitalization in Brazil [
25]. The role of cigarette smoking on COVID-19 has become very controversial issue. Some studies emphasized a positive correlation between cigarette smoking and COVID-19 due to fact that nicotine poses minor anti-inflammatory properties [
26]. Other studies indicates that cigarette smoking urges the severity of COVID-19 by increasing the angiotensin-converting enzyme II (ACE2) gene expression [
27,
28,
29]. All these prompted the WHO to issue a warning letter suggesting that severity of COVID-19 infection was higher among smokers [
30].
The study from the USA found that older males with comorbidities had a higher risk of death [
13] which is in line with the results of our study. However, middle-aged females were dominant COVID-19 patients in Nanchang, China [
31], but hypertension was one of the most frequent comorbidities like in our study. The study in Detroit showed that coronary artery disease and chronic kidney disease were factors for hospitalization [
32], while in Korea additional factors were dementia, neurological diseases and heart failure [
33]. In South Africa, family physicians took care of COVID-19 patients with mild symptoms in small district hospitals, where increasing age, male sex, overweight/obesity, type 2 diabetes mellitus (T2DM), chronic kidney disease, cardiac failure, HIV and cancer were the risk factors for lethal outcome [
34]. There was a strong relationship between lethal outcome and diabetes of patients with COVID-19 in Spain [
12]. The national database of patients with T2DM in the US study showed a higher risk for severe COVID-19 and lethal outcome in older males with comorbidities such as dementia, cancer, congestive heart failure, paraplegia, and metabolic disease [
35]. In Wuhan, the elderly COVID-19 patients with combination of hypertension and heart disease were at greater risk for lethal outcome [
36]. Our results showed that significant number of risk factors influenced hospitalization and death rate, while results from Japan and Colorado (USA) showed that age, obesity, hypertension and diabetes are predictable for oxygen requirement [
37,
38]. Findings from the USA showed that severe COVID-19 clinical course was more frequent in patients with autoimmune diseases, obesity, smoking and female gender. Contrary to our results, aging was not found as a risk factor for severe presentation of COVID-19 in the American study [
39]. However, increased sensitivity to immune response in aged people has been concerned as contributable to severe COVID-19 outcomes [
40].
Vaccinated patients had higher rate of hospitalization, comparing to unvaccinated, but significantly lower rate of lethal outcomes. Number of doses received significantly correlates with the protection from lethal outcome and hospitalization. Results of Swedish study showed that vaccinated patients were in low risk of hospitalization or death. As waning more than 4 months after vaccination was confirmed, administration of a third vaccine dose as a booster was recommended [
41]. A systematic review of 41 worldwide studies showed that most vaccines prevented people from getting infected, as well as reduced the number of people with severe disease [
42]. Results from the study in Korea showed better outcomes of vaccinated patients with mild to severe clinical course [
43].
Concerning the signs and symptoms, fever, cough, fatigue, nausea and vomiting, chest pain, shortness of breath and appetite lost were the most frequent reasons for hospitalization in our study. Findings from Detroit showed that dyspnoea, anorexia, nausea and diarrhoea were the most common symptoms among hospitalized patients [
32]. Some of the symptoms like throat pain, loss of smell and taste, headache, myalgia and arthralgia and rhinitis had significantly higher favourable outcome in our study. Contrary, fatigue and appetite loss were symptoms significantly dominant in lethal outcome patients.
This study has several limitations. First, the analysed data originates from the primary health care information system. We have not dealt with hospital course of the disease. Therefore, we have no proper data to conclude if the patient “died of COVID-19” or “with COVID-19”.
5. Conclusions
Clinical symptoms and outcome of COVID-19 have been associated with basic demographic characteristics and comorbidities of patients in the Republic of Srpska and that is in line with results of many different studies worldwide. Sex and age could be considered as risk factors for COVID-19 related deaths. The most frequent risk factors were hypertension, obesity, and hypercholesterolemia. The highest hospitalization rate was in patients with CRF, diabetes and CVD, while the death rate was the highest among patients with CRF and CVD. Fever, cough, fatigue, nausea and vomiting, chest pain, shortness of breath and appetite loss favoured hospitalization. Patients with fatigue and appetite loss had higher percentage of lethal outcome. Clinical symptoms and signs, as well as clinical outcomes are predictive parameters for management of COVID-19 pandemic. Vaccination against COVID-19 has an important role in clinical outcomes of the disease, clearly reducing risk of death. Number of received doses correlates with the protection from death, with the booster dose as the most effective one.
Author Contributions
All authors made substantial contributions to the conception or design of the manuscript or the acquisition, analysis, or interpretation of data. All authors drafted the work or revised it critically for important intellectual content and approved the version to be published.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was based on anonymous date analyses and did not involve contacts or any intervention with patients. So, it was not necessary to obtain permission from the Ethics Committee.
Data Availability Statement
All data presented in this study are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wu. F.; Zhao, S.; Yu, B.; Chen, Y.; Wang, W.; Song, Z.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579(7798), 265-269. (accessed on 10 January 2022). [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8(5), 475-481. (accessed on 10 January 2022). [CrossRef]
- Sohrabi, C.; Alsafi, Z.; O'Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; et al. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg, 2020, 76, 71–76.
- World Health Organisation (WHO). WHO announces COVID-19 outbreak a pandemic 2020 . Available online: euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic. (accessed on 13 May 2021).
- Aćimović, J.; Jandrić, Lj.; Đaković Dević, J.; Bojanić, J.; Subotić, B.; Radojčić, T.; et al. Epidemiological characteristics of COVID-19 infection in the Republic of Srpska: a hundred days survey. Scr Med. 2020, 51(2), 74–80. [Google Scholar] [CrossRef]
- Durmus, V. Epidemic trends of COVID-19 in 10 countries compared with Turkey. Vacunas 2020, 22(1), 10–9. Available online; (accessed on 13 December 2021). [CrossRef]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; et al. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA 2020, 323(16), 1612-1614. (accessed on 13 December 2021)2020. [Google Scholar] [CrossRef]
- Lam, P.H.; Milam, A.J.; Tou, E.; Dhillon, N.K.; Toscano, S.; Abaalkhail, N. Characteristics of mechanically ventilated patients with COVID-19 and persons under investigation negative for COVID-19 at an academic medical center: A retrospective cross-sectional pilot study. J. Clin. Anesth. (accessed on 10 January 2022)2020; 67, 110029. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, KW. ; the Northwell COVID-19 Research Consor-tium; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323(20), 2052-2059. (accessed on 10 January 2022). [CrossRef]
- Booth, A.; Reed, A.B.; Ponzo, S.; Yassaee, A.; Aral, M.; Plans, D.; et al. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS ONE 2021, 16(3), e0247461. Available from; (accessed on 13 May 2021). [CrossRef]
- Krist, A.H.; DeVoe, J.E.; Cheng, A.; Ehrlich, T.; Jones, S.M. Redesigning primary care to address the COVID-19 pandemic in the midst of the pandemic. Ann Fam Med 2020, 18(4), 349-354. (accessed on 13 May 2021). [CrossRef]
- Mayer, M.A.; Vidal-Alaball, J.; Puigdellívol-Sánchez, A.; Gomez, F.X.M.; Leis, A.; Peña, J.M. Clinical Characterization of Patients With COVID-19 in Primary Care in Catalonia: Retrospective Observational Study. JMIR Public Health Surveill. 2021, 7(2), e25452. [Google Scholar] [CrossRef] [PubMed]
- Vahidy, F.S.; Pan, A.P.; Ahnstedt, H.; Munshi, Y.; Choi, H.A.; Tiruneh, Y.; et al. Sex differences in susceptibility, severity, and outcomes of coronavirus disease 2019: Cross-sectional analysis from a diverse US metropolitan area. PLoS ONE 2021, 16(1), e0245556. Available online; (accessed on 13 May 2021). [CrossRef]
- Hu, D.; Lou, X.; Meng, N.; Li, Z.; Teng, Y.; Zou, Y. Influence of age and gender on the epidemic of COVID-19, Evidence from 177 countries and territories—an exploratory, ecological study. Wien. Klin. Wochenschr. 2021, 133(7-8), 321-330. Available online; (accessed on 10 January 2022). [CrossRef]
- Liao J, Fan S, Chen J, Wu J, Xu S, Guo Y, et al. Epidemiological and Clinical Characteristics of COVID-19 in Adolescents and Young Adults. Intern. Jour. of Infect. Diseases 2021, 105, 113-119. (accessed on 10 January 2022). [CrossRef]
- Adab P, Haroon S, O’Hara M. E, Jordan R.E. Comorbidities and covid-19 Better understanding is essential for health system planning BMJ 2022, 377, o1431 (accessed on 13 May 2021) Available online:. [CrossRef]
- Djaharuddin I, Munawwarah S, Nurulita A, Ilyas M, Tabri N.A, Lihaw N. Comorbidities and mortality in COVID-19 patients. Gac. Sanit. 2021, 35(S2), S530–S532.
- Harizi C, Cherif I, Najar N, Osman M, Mallekh R, Ben Ayed O, et al. Characteristics and prognostic factors of COVID-19 among infected cases: a nationwide Tunisian analysis. BMC Infect. Di. 2021, 21, 140. Available online; (accessed on 13 May 2021). [CrossRef]
- Mijović, B.; Mašić, S.; Petković, M.; Knežević, D.; Aćimović, J.; Djaković-Dević, J.; et al. Seroprevalence of SARS-CoV-2 anti-bodies and knowledge, attitude and practice toward COVID-19 in the Republic of Srpska-Bosnia & Herzegovina: A population-based study. PLoS ONE 2022, 17(1), e0262738. Available online:; (accessed on 23 May 2021). [CrossRef]
- Zidan, N.; Dey, V.; Allen, K.; Price, J.; Zappone, S.R.; et al. Understanding comorbidities and health disparities related to COVID-19: a comprehensive study of 776 936 cases and 1 362 545 controls in the state of Indiana, USA. JAMIA Open 2023, 6(1). Available online:; (accessed on 13 May 2021). [CrossRef]
- Scientific Advisory Group. COVID-19 Scientific Advisory Group Rapid Evidence Report. Risk Factors for Severe COVID-19 Outcomes. Available online: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-sag-rapid-evidence-report-masking-guidance-healthcare-workers. (accessed on 13 May 2021).
- Bigdelou, B.; Sepand, M.R.; Najafikhoshnoo, S.; Negrete, J.A.T.; Sharaf, M.; Ho, J.Q.; et al. COVID-19 and Preexisting Comorbidities: Risks, Synergies, and Clinical Outcomes. Front. Immunol. 2022, 13, 890517. [Google Scholar] [CrossRef] [PubMed]
- Miyashita, K.; Hozumi, H.; Furuhashi, K.; Nakatani, E.; Inoue, Y.; Yasui, H.; et al. Changes in the characteristics and outcomes of COVID-19 patients from the early pandemic to the delta variant epidemic: a nationwide population-based study. Emerg. Microbes Infect. 2022, 12(1), e2155250. Available online:; (accessed on 13 May 2021). [CrossRef]
- Khedr, E.M.; Daef, E.; Mohamed-Hussein, A.; Mostafa, EF.; Zein, M.; Hassany, S.M.; et al. Comorbidities and outcomes among patients hospitalized with COVID-19 in Upper Egypt. Egypt. J. Neurol. Psychiatry Neurosurg. 2022, 58, 92 (accessed on 06 February 2022) Available online:. [Google Scholar] [CrossRef]
- Menezes Soares, R.C.; Rodrigues Mattos, L.; Martins Raposo, L. Risk Factors for Hospitalization and Mortality due to COVID-19 in Esp´ ırito Santo State, Brazil. Am. J. Trop. Med. Hyg. 2020, 103(3), 1184–1190. (accessed on 06 February 2022). [CrossRef]
- Wang, H.; Yu, M.; Ochani, M.; Amella, CA.; Tanovic, M.; Susarla, S.; et al. Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature 2003, 421(6921), 384-388. (accessed on 10 January 2022). [CrossRef]
- Guo, F.R. Active smoking is associated with severity of coronavirus disease 2019 (COVID-19): An update of a meta-analysis. Tob. Induc. Dis. 2020, 18, 37 (accessed on 10 January 2022). [Google Scholar] [CrossRef]
- Cai, G.; Bossé, Y.; Xiao, F.; Kheradmand, F.; Amos, CI. Tobacco smoking increases the lung gene expression of ACE2, the receptor of SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020, 201(12), 1557-1559. (accessed on 10 January 2022). [CrossRef]
- Leung, J.M.; Sin, D.D. Smoking, ACE-2 and COVID-19: ongoing controversies. Eur. Respir. J. 2020, 56(1), 2001759. (accessed on 10 January 2022). [CrossRef]
- World Health Organization. Resources for tobacco use control as part of COVID-19 response. URL: euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technicalguidance/resources-for-tobacco-use-control-as-part-of-covid-19-response.
- Hong, J-M.; Hu, L-H.; Zhong, Q-S.; Zhu, L-C.; Hang, Y-P.; Fang, X-Y.; et al. Epidemiological Characteristics and Clinical Features of Patients Infected With the COVID-19 Virus in Nanchang, Jiangxi, China. Front. Med. 2020; 7:571069. 13 May 2021. [CrossRef]
- Suleyman, G.; Fadel, R.A.; Malette, K.M.; Hammond, C.; Abdulla, H.; Entz, A.; et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Network Open. 2020, 3(6), e2012270. (accessed on 13 May 2021). [CrossRef]
- Kim, S.W.; Kim, S.M.; Kim, Y.K.; Kim, J.Y.; Lee, Y.M.; Kim, B.O.; et al. Characteristics of COVID-19 Cohort Patients in Daegu. J. Korean Med. Sci. 2021, 36(1), e12 Available online; (accessed on 13 May 2021)2021. [Google Scholar] [CrossRef]
- Mash, R.J.; Presence-Vollenhoven, M.; Adeniji, A.; Christoffels, R.; Doubell, K.; Eksteen, L.; et al. Evaluation of patient characteristics, management and outcomes for COVID-19 at district hospitals in the Western Cape, South Africa: descriptive observational study. BMJ Open 2021, 11, e047016. (accessed on 13 May 2021). [CrossRef]
- Boye, K.S.; Erdemir, E.T.; Zimmerman, N.; Reddy, A. Benneyworth B.D. Dabora M.C. Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States. Diabetes Ther. 2021, 12, 2223–2239. Available online; (accessed on 06 February 2022). [CrossRef]
- Lv, Z.; Lv, S. Clinical characteristics and analysis of risk factors for disease progression of COVID-19: A retrospective Cohort Study. Int. J. Biol. Sci. 2021, 17(1), 1-7. (accessed on 13 May 2021). [CrossRef]
- Goto, N.; Wada, Y.; Ikuyama, Y.; Akahane, J.; Kosaka, M.; Ushiki, A.; et al. The usefulness of a combination of age, body mass index, and blood urea nitrogen as prognostic factors in predicting oxygen requirements in patients with coronavirus disease 2019. J. Infect. Chemother. 2021, 27, 1706-1712. Available online; (accessed on 13 May 2021). [CrossRef]
- Vahey, G.M.; McDonald, E.; Marshall, K.; Martin, S. W:; Chun, H.; Herlihy, R.; et al. Risk factors for hospitalization among persons with COVID-19—Colorado. 2021; PLoS ONE 2021, 16(9), e0256917. Available online; (accessed on 06 February 2022). [CrossRef]
- Dreyer, N.; Petruski-Ivleva, N.; Albert, L.; Mohamed, D.; Brinkley, E.; Reynolds, M.; et al. Identification of a Vulnerable Group for Post-Acute Sequelae of SARS-CoV-2 (PASC): People with Autoimmune Diseases Recover More Slowly from COVID-19. Int. J. Gen. Med. 2021, 14, 3941–49. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Vineela Nalla, L.; Sharma, M.; Sharma, N.; Singh, A.A.; Mushtaque Malim, F.; et al. Association of COVID-19 with Comorbidities: An Update. ACS Pharmacol. Transl. Sci. 2023, 6(3), 334–354. [Google Scholar] [CrossRef] [PubMed]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: a retrospective, total population cohort study in Sweden. Lancet. 2022, S0140-6736(22)00089-7. [CrossRef]
- Graña, C.; Ghosn, L.; Evrenoglou, T.; Jarde, A.; Minozzi, S.; Bergman, H.; et al. Efficacy and safety of COVID-19 vaccines. CDSR 2022, 12. Art. No.: CD015477. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858. (accessed on 06 February 2022)0154. [Google Scholar]
- Seo, W.J.; Kanga, J.; Kanga, H.K.; Parka, S.H.; Kooa, H.K.; Park, H.K.; et al. Impact of prior vaccination on clinical outcomes of patients with COVID-19. Emerg. Microbes & Infect. 2022, 11. Available online; (accessed on 06 February 2022). [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).