1. Introduction
Unilateral cerebral palsy (UCP) is a leading cause of childhood disability [
1]. Children with UCP have difficulty in bimanual coordination, which further restricts the child’s independence in daily activities and impairs quality of life [
2]. Hand arm bimanual intensive therapy (HABIT) is a well-established intervention to improve hand function and bimanual coordination in children with UCP [
3]. Traditionally, the intensity of HABIT has been quantified as number of hours of therapy [
4,
5]. Despite the reported improvements in upper extremity (UE) function, discrepancy exists in the intensity of training protocols [
6,
7]. Evidence indicates that greater intensities in terms of hours result in larger gains in UE motor outcomes [
4,
8]. However, time is recognized as a proxy measure of training intensity since it does not reveal specific information about the goal-directed UE or bimanual movements occurring during training [
9]. Hence, it is crucial to develop objective methods to quantify the intensity of HABIT in terms of bimanual movement characteristics that would provide insights into bimanual training intensity.
Accelerometers have been accepted as a valid tool to objectively capture UE movement characteristics in the real-world environment [
10,
11,
12]. They measure accelerations of UE movements along the predefined axes in gravitational units called activity counts. The gold standard methods to monitor quality and quantity of UE use such as 3D kinematic [
13] and human-observed coding [
14] of video recordings can be time consuming and expensive to quantify intensity of HABIT. Accelerometer metrics overcome these problems and provide a convenient option to measure movement characteristics during intensive therapy as well as in the real-world environment, thus capturing the activities and participation domains per the International Classification of Functioning, Disability, and Health - Children and Youth Version (ICF-CY) [
15]. Acceleration metrics that reflect UE movement characteristics are broadly classified into three categories [
16]. The first category indicates the relative contributions of the affected and less affected UE movements using use ratio, magnitude ratio, and bilateral magnitude [
16]. The second category comprises of characteristics specific to the accelerations of the affected extremity through median acceleration and acceleration variability. The third category provides the number of accelerations using activity counts of both the extremities [
16]. Our novel approach capitalized on these three categories to quantify the characteristics of 30-hour (intensity) HABIT. An understanding about bimanual movement characteristics can provide clinically meaningful information regarding the contribution of the affected vs. less affected extremity to bimanual activities during HABIT and thereby guide clinical dosing criteria, and to capture gains in bimanual performance in real-world activities.
Performance refers to what a person actually does in real-world environment whereas capacity refers to what a person can do in a controlled environment such as in a clinic [
17]. The International Classification of Functioning, Disability, and Health- Children and Youth Version (ICF-CY) by the World Health Organization, provides a clear differentiation between performance and capacity within the domains of activities and participation [
15]. Activity refers to execution of a task or action by an individual, whereas participation is involvement in a life situation. Performance qualifier, according to ICF-CY, refers to what a person does in current (real-world or the lived experience) environment, signifying participation, whereas capacity refers to what a person can do in a controlled (standard) environment such as in a clinic, signifying activity [
17]. Traditionally, studies examining the efficacy of HABIT have assessed changes in UE capacity using standardized clinical tests such as the Assisting Hand Assessment (AHA), Box and Block Test (BBT), Nine-Hole Peg Test (NHPT), Jebsen Hand Function Test (JHFT) etc., that primarily captures body function and activity per ICF-CY [
18]. Whereas UE performance (activity and participation) has been assessed using self-reported measures such as Canadian Occupational Performance Measure, Pediatric Evaluation and Disability Inventory, and ABILHAND [
18]. Collectively, these studies indicate that HABIT improves UE capacity as well as performance of children with UCP. However, self-report measures are prone to subjective and social desirability biases which questions whether in-clinic improvements are indicative of change in real-world bimanual activities and participation [
19]. Recent evidence supports this conjecture since discrepancies between parent’s perception of their child’s performance using self-reported measures and therapists’ assessment of capacity have been reported [
20]. Furthermore, changes in standardized assessments may not translate to improvements in the affected UE use in daily life when assessed with accelerometers in children with UCP [
21,
22] as well as adult stroke population [
23]. Therefore, capturing the performance of the affected UE during daily bimanual activities using accelerometers is crucial to elucidate whether improvements in capacity with HABIT translate to gains in performance of real-world bimanual activities and participation in children with UCP.
In the last decade, accelerometers have been primarily used to assess UE performance after intervention in adult stroke survivors [
24,
25] and to detect motor asymmetries in children with UCP [
26]. Only a few studies have used accelerometers to monitor UE gains in children with UCP following intensive therapy such as constraint induced movement therapy (CIMT) [
21,
27]. Collectively, results of the studies in adult stroke [
16] as well as in children with UCP [
21,
27] indicate that despite improvements in UE capacity, UE performance in daily life showed little to no improvement. Despite an excellent capacity of accelerometers to capture activity counts and movement characteristics in real-world environment, none of the studies have utilized accelerometers to measure real-world bimanual performance post-HABIT.
Therefore, the primary purpose of this novel study was to objectively quantify the characteristics of bimanual movements during 30-hour (intensity) HABIT using bilateral wrist-worn accelerometers. The second purpose was to examine the gains in real-world bimanual performance following HABIT using accelerometer-derived variables reflecting the activities and participation. We hypothesize that accelerometers will accurately capture the UE movement characteristics reflecting bimanual use during HABIT. Furthermore, 30-hour HABIT will enhance children’s affected UE contributions to the performance of real-world bimanual activities.
2. Materials and Methods
2.1. Study design and setting
This study is an ancillary analysis [
28] of a double-blind, randomized controlled trial (NCT05355883). It was a prospective, pre- and post-training study, conducted at the Pediatric Assessment and Rehabilitation Laboratory (PeARL) at East Carolina University (ECU), NC. The University and Medical Center Institutional Review Board, ECU approved the study. We obtained parental consent and child assent. The assessors were blinded to pre- and post-testing assessments. The study was conducted between November 2021- January 2023.
2.2. Participants
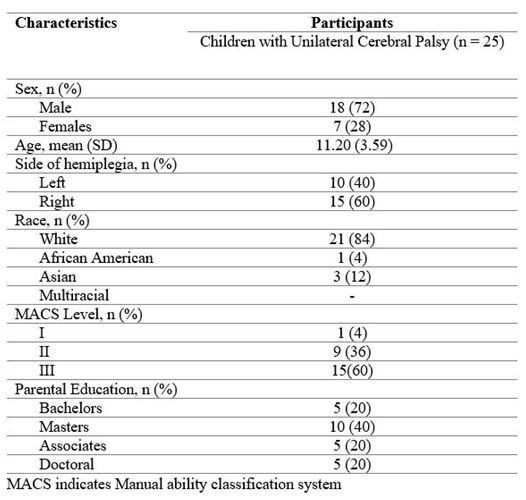
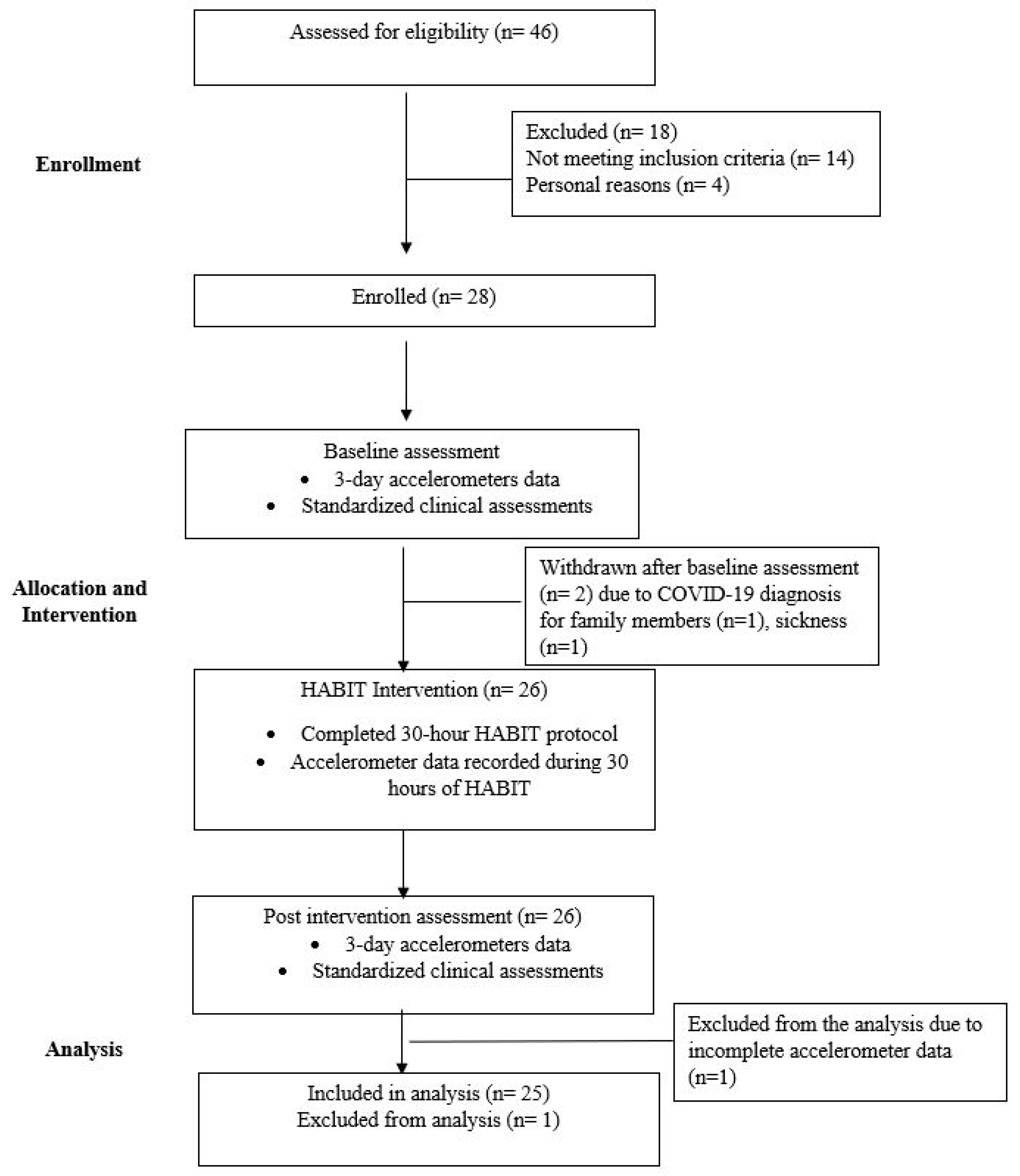
Twenty-five children with UCP, age 6–16 years (mean age = 11.20 ± 3.59 years) and Manual Ability Classification system levels I–III participated in this study.
Figure 1 shows the CONSORT diagram, describing the flow of participants through the study, withdrawals, and inclusion in analyses.
Children with other neuromotor disabilities, cognitive and communication deficits, cardiorespiratory dysfunctions, metabolic disorders, neoplasms, and a history of botulinum neurotoxin injections on the affected UE in the past 6 months were excluded.
Table 1 describes further details of participant characteristics.
Table 1.
Demographic details of the participants.
Table 1.
Demographic details of the participants.
2.3. Procedures
2.3.1. Hand Arm Bimanual Intensive Therapy (HABIT) Protocol
HABIT is a well-established intervention shown to improve bimanual coordination in children with UCP [
3]. We administered HABIT in a camp-based setting with a pre-determined duration of total of 30 hours of structured, task-specific, bimanual activities, six hours per day for five consecutive days. The therapy included age-appropriate bimanual gross and fine motor tasks in a playful context (please see
supplementary material 1). The child to interventionists (trained physical and occupational therapy students) ratio was 1:4. Individualized therapy goals were formulated based on the pre-training behavioral hand function tests as well as parent and children identified bimanual goals. Interventionists progressively increased the complexity of bimanual activities. The task demands were graded based on the task performance to allow the child to complete the task successfully. Children were encouraged to use the affected and the less affected UE in a coordinated manner. Positive reinforcement and knowledge of performance were provided to motivate and reinforce desired goal-directed activities. Emphasis was placed on different roles of the affected UE, such as stabilizer, manipulator, and assistor depending on the child’s ability and task goal. Sessions comprised of whole-task and part-task practice. Throughout the HABIT, three licensed physical therapists supervised the interventionists to ensure fidelity of therapy. Activities performed by the children were documented by the interventionists [
7].
2.3.2. Accelerometry Methodology
Bilateral wrist-worn accelerometers (Actigraphy GT9X Link, Pensacola, FL, USA) were used to quantify the movement characteristics during the five days of HABIT and the performance (real-world UE activity) gains post-HABIT. Actigraph GT9X Link measures accelerations in activity counts along three axes, with one count equaling 0.001664g [
29]. Accelerometer data were sampled at 30 Hz, and activity counts were binned into 1-second epochs for each axis using ActiLifeTM 6 software. Data was then processed in MATLAB (Mathworks Inc, Natick, MA, USA) using custom-written software developed by Lang et al. [
29]. To determine movement characteristics during HABIT days, children wore accelerometers during 5-days of HABIT (30 hours total wear time). To measure UE performance gains, children wore accelerometers for three consecutive days pre- and post-HABIT during their daily activities which included home, school, and play. This approach was designed to capture bimanual activities throughout the day in a natural, real-world environment. Moreover, the three days accelerometer wearing time pre- and post-HABIT was chosen since it produces a reliable estimate of performance in children with CP [
30]. Detailed instructions were provided to both parents and children on the proper wearing and usage of accelerometers. Specifically, they were instructed to keep the Actigraphs on during waking hours, but to remove them while bathing or engaging in water-related activities.
2.4. Outcome measures
2.4.1. Bimanual Movement Intensity Characteristics and Performance measures
Accelerometer-derived metrics [
16,
29]
: Activity and Participation Domains of ICF-CY
We quantified the bimanual movement characteristics using six standard accelerometry derived variables– 1) use ratio (UR), 2) magnitude ratio (MR), 3) bilateral magnitude (BM), 4) median acceleration (MA), 5) acceleration variability (AV), and 6) affected UE activity counts (AAC). Changes in UE performance pre- and post-HABIT reflecting real-world performance (activity and participation) were assessed using – 1) UR, 2) MR, 3) BM, 4) MA, and 5) AV [
15].
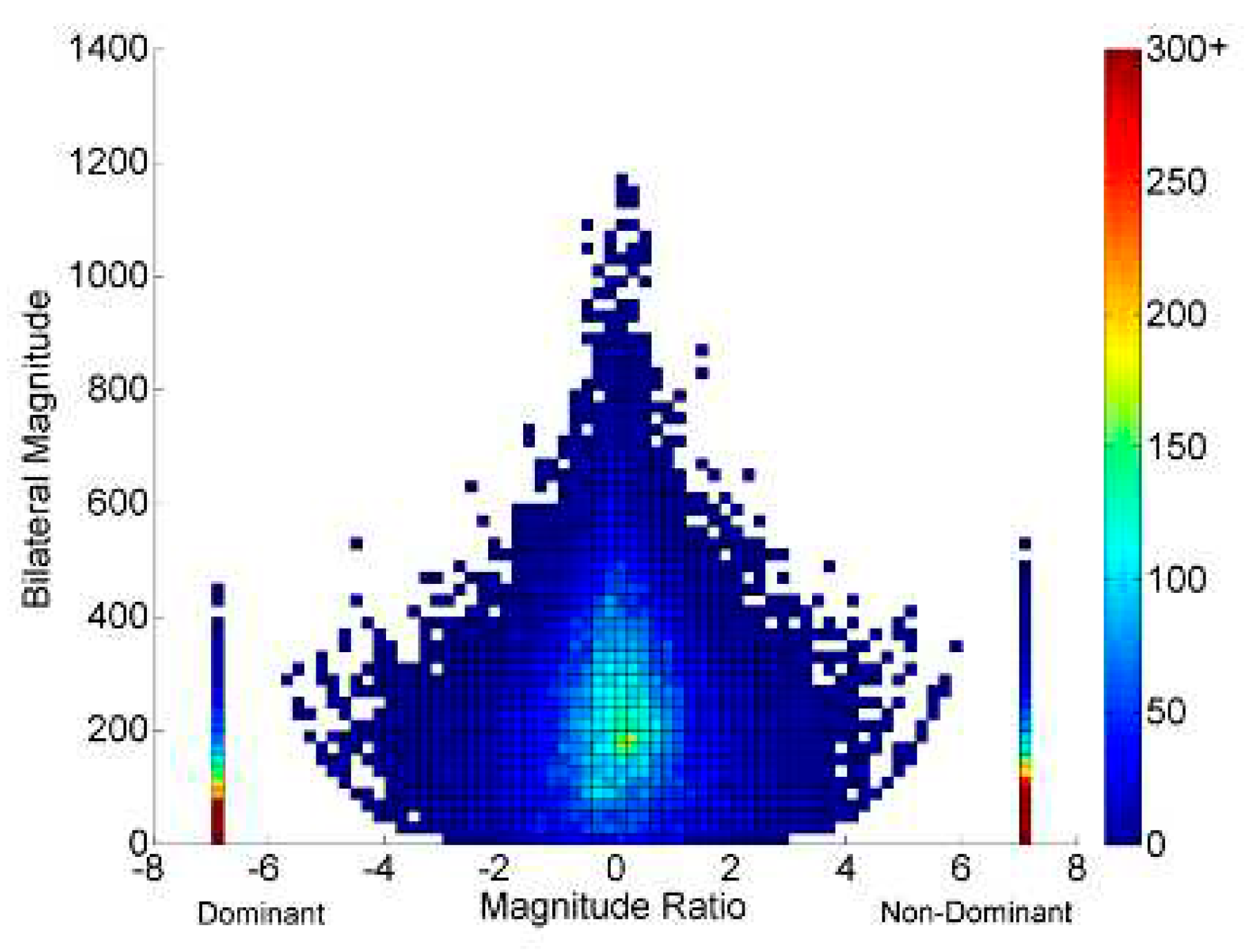
Figure 2 explains the accelerometry derived variables.
1) Use ratio reflects the contribution of the affected relative to the less affected UE and calculated as the ratio of the active duration of the affected to that of the less affected arm. UR value ranges between 0 and 1. A value close to or equal to 1 indicates symmetrical use of extremities whereas a value closer to zero indicates the less affected UE use.
2) Magnitude ratio is the ratio of acceleration magnitude (range of movement) of both UEs and is calculated by dividing the acceleration magnitude of the affected and the less affected UE. The value of MR ranges from -7 to +7. A value closer to 0 indicates equal contributions from both UEs; positive values indicate greater movement magnitude of the affected UE and negative values indicate greater magnitude of the less affected UE.
3) Bilateral magnitude reflects the magnitude of accelerations across both UEs and is calculated by summating the smoothed vector magnitudes of both UEs for each second of activity. Zero indicates no activity and increasing value indicates greater magnitudes of bilateral UE activity.
4) Median acceleration and acceleration variability are variables that reflect movement characteristics considering only the affected UE. Median acceleration represents the acceleration of the affected UE magnitude over the entire wear time.
5) Acceleration variability is the variance of the mean acceleration and represents the average distance of the affected UE accelerations from the mean acceleration. A higher score for both these variables indicates better overall UE movement and variability, respectively [
16,
21].
6) Affected extremity activity counts quantifies the number of the affected extremity accelerations (activity counts) during therapy.
2.4.2. Capacity measures
Standardized Clinical Assessments - Body Function and Activity Domains of ICF-CY
Standardized clinical assessments were used to measure changes in UE capacity pre- and post-HABIT in a controlled laboratory setting [
15]. The AHA assesses the affected hand function and bimanual coordination in children with UCP [
31]. An improvement of 5 units is considered clinically meaningful [
32]. JHFT (reliability; interrater= 0.94, test-retest= 0.91 [
33]) and NHPT (reliability; interrater= 0.99, test-retest= 0.81 [
34]) measures unimanual dexterity and speed. BBT (reliability; interrater= 0.99, test-retest= 0.85 [
35]) assesses the unimanual speed.
2.5. Statistical Analysis
Data were analyzed using IBM Statistical Package for Social Sciences Version 28.0.0. Data are presented as mean ± SD for continuous variables and n (%) for categorical variables. The intensity of UE movement characteristics during 5 days of HABIT were quantified using descriptive statistics for UR, MR, BM, MA, AV, and AAC. Repeated measures analysis of variance (ANOVA) was used with time (five days) as within group variable to determine variability in training using UR, MR, BM, MA, AV, and AAC. Considering the repetitive measurements, the significance level for the ANOVA was set at p value ≤ 0.01 using Bonferroni method. Capacity and performance outcomes were assessed for normality using the Shapiro-Wilk test. Pre- and post-HABIT changes in the capacity and performance measures were assessed using a paired t-test for all the variables, except for MR and BBT score. Wilcoxon signed rank test was used to analyze changes in MR and BBT score pre- and post-HABIT as the data violated assumption of normality. The significance level was set at p value = 0.05 for paired t-test.
3. Results
Twenty-eight participants were enrolled, and twenty-six completed the study intervention. However, data were analyzed for only 25 participants due to incomplete accelerometer data from one participant. There were no adverse events reported during HABIT. Power was derived based on Goodwin et al.’s [
21] study and computed using G*Power [
36]. To detect the mean difference of 0.25 (μ1=1.36, μ2=1.61; SD1=0.12, SD2=0.21) in the primary outcome use ratio (UR), a total of 26 participants provides 94% power to detect an effect size of 1.46 at a significance level of 0.05. The sample size was calculated based on a two-sided t-test.
3.1. Characteristics of Bimanual Movement Intensity during HABIT
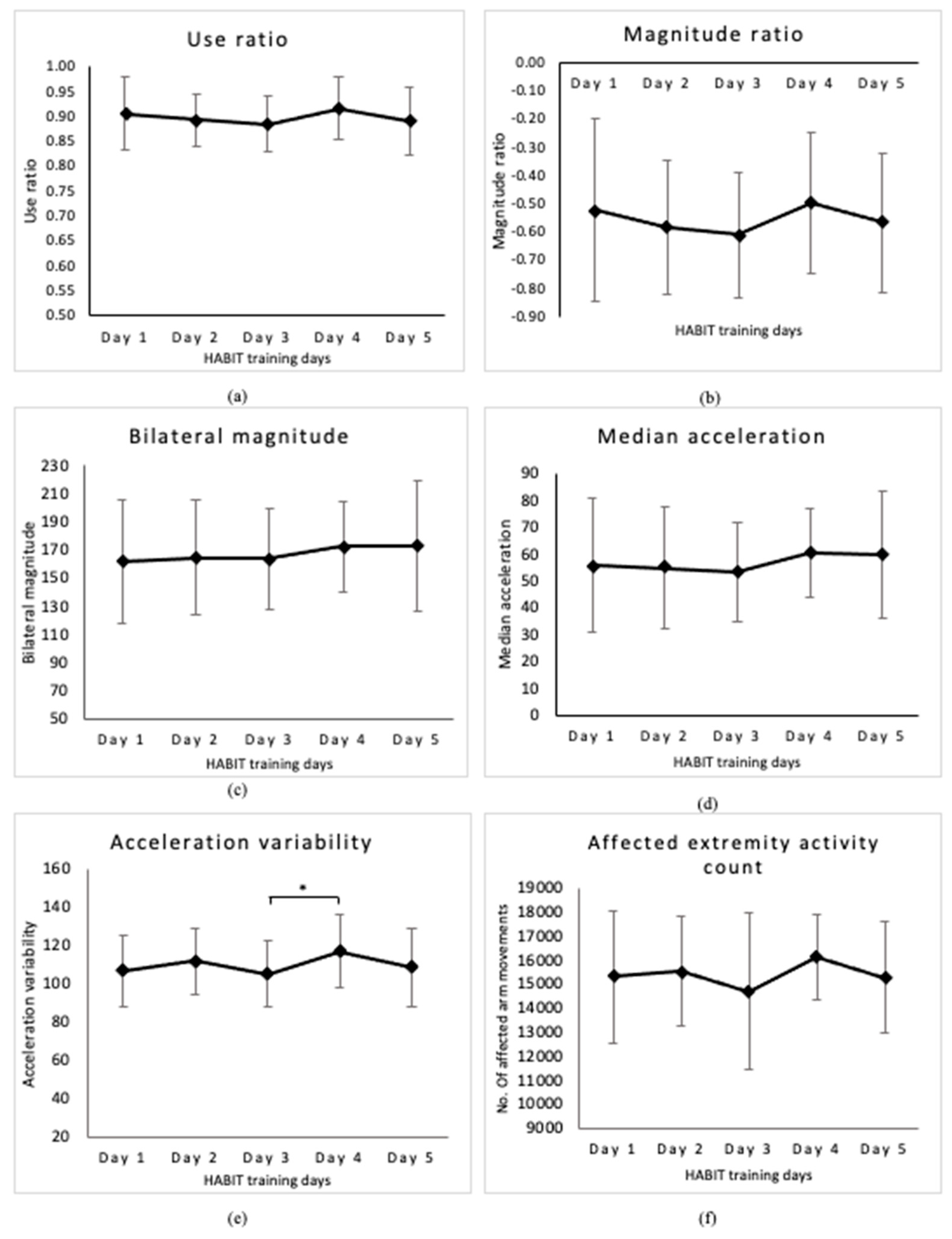
Accelerometer metrics, UR, MR, BM, MA, AV and AAC, representing the bimanual movement characteristics during HABIT days are summarized as descriptive statistics in
Table 2. All the children participated in 30-hour HABIT training across five days. Overall, during HABIT, the affected UE use was 47.26% as compared to 53.73% of the less affected UE use.
Table 2.
Descriptive statistics of accelerometer derived variables across five days of HABIT.
Table 2.
Descriptive statistics of accelerometer derived variables across five days of HABIT.
1) Use ratio (UR): The average use ratio across five days of HABIT was 0.90 ± 0.06 (range: 0.79 – 1.00,
Figure 3a). There was no significant main effect of time (F (4,96) = 1.873, p = 0.121)) for UR.
2) Magnitude ratio (MR): The average MR across five days of HABIT was –0.56 ± 0.26 (range: -0.97 to 0.05,
Figure 3b). There was no significant main effect of time (F (4,96) = 1.688, p = 0.159)) for MR.
3) Bilateral Magnitude (BM): The average BM across five days of HABIT was 167.25 ± 39.83 (range: 101.98 – 267.51,
Figure 3c). There was no significant main effect of time (F (4,96) = 1.923, p = 0.113)) for BM.
4) Median acceleration (MA): The average MA across five days of HABIT was 56.99 ± 21.21 (range: 28.49 – 115.07,
Figure 3d). There was no significant main effect of time (F (4,96) = 2.004, p = 0.1)) for MA.
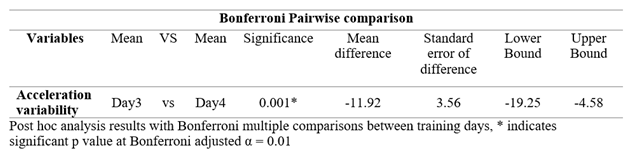
5) Acceleration variability (AV): The average AV across five days of HABIT was 110.27 ± 18.63 (range: 69.07 – 143.05,
Figure 3e). There was a significant main effect of time (F (4,96) = 3.666, p = 0.008).
Table 3 shows significant post hoc analysis results using Bonferroni multiple comparisons for acceleration variability across five days of HABIT.
6) Affected extremity activity counts (AAC): The average daily number of affected UE accelerations during 6 hours across five days of HABIT were (mean ± SD) 15399 ± 2477 (range; 9863 – 20057 counts) (
Figure 3f). The total affected UE accelerations reflecting UE use (sum of the means of daily affected UE accelerations) during 30 hours of HABIT was 76,997 movements. There was a significant main effect of time (F (4,96) = 2.633, p = 0.03)) for the AAC.
Table 3 shows significant post-hoc analysis results using Bonferroni multiple comparisons for AAC across five days of HABIT.
Figure 3.
HABIT intensity across 5 days of training using accelerometer derived variables. Values are means ± SD for each day of HABIT (a) Use ratio, (b) Magnitude ratio, (c) Bilateral magnitude, (d) Median acceleration, (e) Acceleration variability, and (f) Affected extremity use count. Variability is observed in all the accelerometer variables during the five training days.
Figure 3.
HABIT intensity across 5 days of training using accelerometer derived variables. Values are means ± SD for each day of HABIT (a) Use ratio, (b) Magnitude ratio, (c) Bilateral magnitude, (d) Median acceleration, (e) Acceleration variability, and (f) Affected extremity use count. Variability is observed in all the accelerometer variables during the five training days.
Table 3.
Pairwise comparison of the accelerometer metrics between different HABIT training days.
Table 3.
Pairwise comparison of the accelerometer metrics between different HABIT training days.
3.2. Pre- and Post-HABIT Change in Upper Extremity Performance Measures: Activity and Participation
There was a significant improvement in UR (p= 0.002,
Figure 4a), MR (p= 0.018,
Figure 4b), bilateral magnitude (p= 0.006,
Figure 4c), median acceleration (p= 0.002,
Figure 4d) and acceleration variability (p= 0.024,
Figure 4e) post-HABIT. These findings indicate that 30 hours of HABIT enhanced children’s use of the affected arm in terms of movement symmetry, magnitudes, and variability.
Supplementary material 2 shows an exemplary data of a study participant with pre- and post-HABIT changes in these performance measures.
Supplementary material 3 shows the inter- and intra-individual differences in accelerometer-derived variables for all the participants across time points.
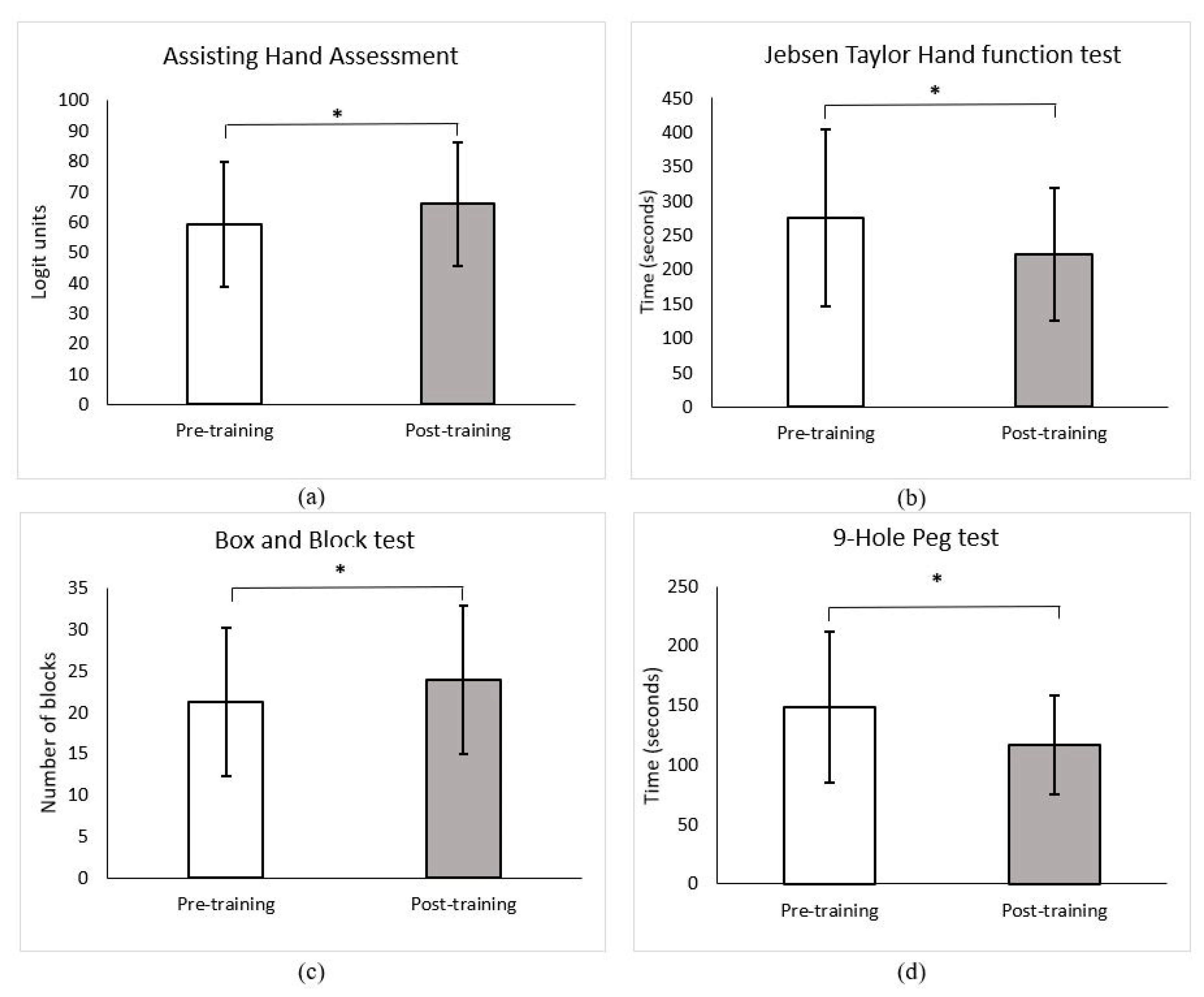
3.3. Pre- and Post-HABIT Change in Capacity measures of the Affected Upper Extremity: Body Function and Activity
There was significant improvement in the mean scores of the AHA (p=0.001,
Figure 5a), the JHFT (p= 0.001,
Figure 5b), the BBT (p= 0.002,
Figure 5c), and the NHPT (p= 0.011,
Figure 5d) from pre- to post-HABIT. The mean scores of AHA and BBT exceeded the minimal clinical important difference (MCID) of 5 logit scores [
32] and 2 blocks [
37]. Mean score of JHFT was very close (53.4 seconds) to the MCID of 55 seconds [
37]. These findings indicate that post-HABIT, children showed increase in bimanual coordination, dexterity, and speed of the affected hand use.
4. Discussion
Our primary aim was to quantify the characteristics of bimanual movement intensity during 30 hours of HABIT utilizing bilateral wrist worn accelerometers. Our findings illustrate that the standard accelerometer derived variables can quantify the contribution of the affected UE to bimanual activities and hence can provide an objective metric for the intensity of bimanual movements practiced during HABIT. Moreover, our results indicate that children performed a total of 76,997 accelerations with their affected UE during HABIT. Our secondary aim was to examine gains in bimanual performance (activity and participation in real-world environment) and capacity (body function and activity in a clinical set-up) post-HABIT using accelerometer-derived metrics and standardized outcomes respectively. We found significant gains in real-world performance of bimanual activities post-HABIT suggesting improved activities and participation in the child’s natural, real-world environment. Furthermore, consistent with prior studies, our results indicate improvements in UE capacity following HABIT. Overall, this is the first study that utilized wearable technology to quantify the intensity of HABIT and demonstrated that accelerometers can objectively quantify bimanual movement characteristics reflecting the intensity of UE use during HABIT. Moreover, 30 hours of HABIT has the potential to improve the UE capacity as well as real-world bimanual performance in children with UCP.
Time is a dominant measure used to define intensity of arm use during intensive therapies [
4,
5]. However, time does not indicate the actual number of movements or movement characteristics performed during a particular session [
9,
38]. In this study, we overcame this limitation using accelerometers and demonstrated a more accurate method to objectively quantify UE movement characteristics during HABIT. UR and MR signify contributions of affected relative to less affected UE considering the duration and magnitude (range of movement) during bimanual activities. Children in our study attained an average UR of 0.90 during HABIT which was 22% higher than pre-training. The UR being close to 1 suggests that there was nearly equal use of both UE during HABIT. Average MR during HABIT was -0.56, which was 64.6% higher than pre-training. The value of MR moved substantially closer to 0 indicating greater magnitude of the affected UE during training. Likewise, the average BM reflecting the combined magnitudes of accelerations from both UEs during HABIT was 167.25, which was 58.8% higher than pre-training. The average MA and AV reflecting mean accelerations of the affected UE and variability of accelerations also increased (MA =56.9, AV = 110.3) noticeably during HABIT by 154.36% and 54.4% compared to pre-training. Collectively, these results indicate greater symmetry in UE use and higher affected arm use during HABIT. These improvements can be attributed to the intensive nature of bimanual, task-specific activities incorporated in HABIT. Notably, the UR and MR attained during training were comparable to those reported in accelerometer studies in typically developing children of 0.96 and -0.28, respectively, which suggests that the bimanual activities incorporated in HABIT were comparable with the amount of typical bimanual activities [
21,
26]. Overall, our findings provide preliminary evidence for using accelerometers to quantify movement characteristics during HABIT. These findings could serve as foundation for future studies to understand the relationship between accelerometer metrics and motor outcomes in children with UCP.
Affected UE activity counts (AAC) during 6 hours of HABIT ranged from 14,714 to 16,160 and a total of nearly 76,997 accelerations occurred during 30 hours of HABIT. Use of repetitions to quantify intensity is limited in rehabilitation research and clinical practice. Some studies on stroke survivors have investigated repetitions of UE training by observing video recordings of therapy sessions [
14,
39]. Lang and colleagues used repetitions to quantify the intensity of upper limb exercise during stroke rehabilitation and inpatient hospital stays [
40]. These observational studies, however, focused on routine therapy sessions, which are invariably of shorter duration. Although this is a gold standard method for monitoring repetitions, manual coding by human observers could be exceedingly strenuous, especially for extended hours of therapy such as HABIT. Despite the differences regarding the inability of accelerometers to isolate purposeful movements; UE movement characteristics derived from accelerometer metrics could still provide clinically relevant data about UE use during prolonged hours of training. Moreover, previous studies have found an agreement between the affected UE activity counts and human-observed purposeful repetitions during group [
41] and individual therapy [
39] sessions suggesting that accelerometers measures have concurrent validity. As a result, this study is unique in two ways: 1) for the first time, we provide objective data on bimanual movement characteristics reflecting the intensity of arm use during HABIT; and 2) were able to quantify the number of affected UE activity counts during 30 hours of HABIT, which, while an overestimation, could still be considered a key component to influence motor learning.
Our results demonstrated significant improvements on all standardized clinical tests, reflecting enhanced UE capacity suggesting improvements in body function and activity measured in a constrained, clinical environment, post-HABIT. Notably, the AHA scores exceeded the minimal clinically important (MCID) difference of 5 units [
32]. Children were able to transfer a greater number of blocks (> 2 blocks compared to pre-training, MCID = 2 [
37]) with their affected UE (12% increase in BBT) and complete the NHPT (21.04% faster) and JHFT (19.35% faster, pre- to post-HABIT difference = 53.4 seconds, very close to MCID of 55 seconds [
37] in less time, indicating greater speed and dexterity post-HABIT. These findings are consistent with previous studies that demonstrated an increase in hand capacity following intensive therapies [
18].
Our study results also indicate gains in UE performance following HABIT, which indicates enhanced activities and participation in natural, real-world environment in these participants [
15]. Children demonstrated increase in UR, MR, and BM by 6.85%, 34.81%, and 15.84% respectively, indicating greater symmetry and contribution of the affected UE in terms of hours of use and magnitude of real-world bimanual activities. Additionally, post-HABIT, MA and AV increased by 39.56% and 9.48%, respectively, which indicates an increase in the affected UE speed and variations in movement speed following HABIT. However, our accelerometer measures also revealed a significant degree of variability at pre- and post-HABIT time points, aligning with previous studies that employed similar methods [
21,
27]. This variability can be attributed to the heterogeneity of our study population, including differences in age, gender, and functional level as measured by the MACS levels. Further analysis of the individual profile plots depicting inter-individual differences (
supplementary material 2a) revealed that a few participants with MACS level III exhibited higher UR (> 0.8) at baseline. This could be due to involuntary and mirror movements in their more affected UE, resulting in higher accelerometer readings indicating increased affected UE use. Additionally, the profile plot of MR (
supplementary material 2b) indicated that the changes in the magnitude of movement of the more affected UE following HABIT were significantly driven by three participants. These three participants were relatively older (≥ 15 years) compared to younger children and likely had higher motivation for high amplitude activities, such as overhead catch and throw with a soccer ball or hitting a baseball etc., which plausibly lead to greater improvements in MR post-HABIT. The profile plots for BM, MA, and AV (
supplementary material 2c, 2d, and 2e) revealed similar trends––participants with MACS level III, who initially had lower baseline scores, exhibited more pronounced improvements after undergoing HABIT compared to those with MACS levels I and II. Similar to MR, the profile plots for BM and MA indicated that a small subset of participants with MACS level III, who were comparatively older demonstrated re pronounced changes post-HABIT. Despite the observed variability, which is typical in clinical population, collectively, our study findings demonstrated improvements in real-world bimanual performance, which contradict the findings of previous studies that utilized accelerometers to assess UE performance gains post-CIMT [
21,
27]. The limited gains reported in those studies could be due to the lack of a bimanual training component in the CIMT approach. We believe the intensity of HABIT administered in our study, as seen by improved UE movement characteristics, was potentially adequate to drive changes in UE capacity beyond a specific threshold required to produce a change in UE performance.
Study Limitations: We recognize a few study limitations and propose future study directions. First, wrist worn accelerometers capture only arm and forearm accelerations (gross motor function), but they are limited in capturing the finger accelerations (fine motor function). Thus, future studies could use finger worn inertial sensors to quantify fine movements in this population. Second, although we attempted to perform bimanual activities during HABIT training to achieve purposeful movements, a part of our data may contain non-purposeful movements occurring during non-therapy time such as normal walking, washroom breaks, etc. Therefore, caution should be used when interpreting the results of this study. Third, we did not measure long-term retention of the UE performance gains in this study. We suggest that future studies address this limitation by conducting follow-up assessments to determine the persistence of immediate gains in performance, which could provide insight into the retention and transfer components of motor skill learning. Finally, the generalizability of our study findings could be limited due to heterogeneous study participants and a lack of a control group.
5. Conclusions
Accelerometers can be used to quantify movement characteristics of UE during HABIT, which could provide objective measure regarding the intensity of UE use. Thirty hours of HABIT has the potential to improve UE function in real-world bimanual activities indicating improvements in activities and participation in natural environment and to enhance the speed and dexterity of the affected UE indicating improvements in body function and activity in a clinical environment. Overall, accelerometer is a valuable tool for clinicians to quantify the different aspects of UE movements conveniently and monitor in-clinic as well as real-world improvements in UE use in children with UCP.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org., Supplementary material 1. Activities included in the HABIT protocol. Supplementary material 2. Figure 1A & 1B: Representative example of pre- and post-HABIT density plots of a child with unilateral cerebral palsy. Supplementary material 3. Figure 2 (a) – 2 (e): Profile plots illustrating individual differences in accelerometer-derived variables.
Author Contributions
Conceptualization, S.S.; methodology, S.G., S.S., and S.K.; software, S.G., and S.S.; validation, S.S.; formal analysis, S.G., and S.S.; investigation, S.G., C.L., A.G.M., and J.W., S.S.; resources, C.L., A.G.M., J.W., and S.S.; data curation, S.G., and S.S.; writing—original draft preparation, S.G; writing—review and editing, S.G., C.L., A.G.M., S.K., J.W., and S.S.; visualization, S.G., and S.S.; supervision, S.S.; project administration, S.S.; funding acquisition, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
Research reported in this publication was supported in part by the Eunice Kennedy Shriner National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R03HD107644 and APTA’s Pediatric Physical Therapy (grant no. 21-0810).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the University and Medical Center Institutional Review Board of East Carolina University, NC (protocol code 21-001913, and approval date 09/29/2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank the children and their families who participated in the study, and all the volunteer (physical and occupational therapy students) interventionists for their contributions in the HABIT camp. We sincerely thank the graduate research assistants Casey Burroughs, David Turnure, Mary Scott Faircloth, Caroline Pusey-Brown, Katie Woosley, Natalie McBryde, Grant Kirkman, Jovanna Zapata, and Brody Morton for their contributions to this project.
Conflicts of Interest
The authors have no conflicts of interest to declare. All co-authors have seen and agree with the contents of the manuscript and there is no financial interest to report. We certify that the submission is original work and is not under review at any other publication. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Stavsky, M.; Mor, O.; Mastrolia, S.A.; Greenbaum, S.; Than, N.G.; Erez, O. Cerebral Palsy-Trends in Epidemiology and Recent Development in Prenatal Mechanisms of Disease, Treatment, and Prevention. Front Pediatr. 2017, 5, 21. [Google Scholar] [CrossRef]
- Hung, Y.-C.; Charles, J.; Gordon, A.M. Bimanual Coordination during a Goal-Directed Task in Children with Hemiplegic Cerebral Palsy. Dev Med Child Neurol 2004, 46, 46–53. [Google Scholar] [CrossRef]
- Novak, I.; Mcintyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.-A.; Goldsmith, S. A Systematic Review of Interventions for Children with Cerebral Palsy: State of the Evidence. Dev Med Child Neurol 2013, 55, 885–910. [Google Scholar] [CrossRef] [PubMed]
- Sakzewski, L.; Provan, K.; Ziviani, J.; Boyd, R.N. Comparison of Dosage of Intensive Upper Limb Therapy for Children with Unilateral Cerebral Palsy: How Big Should the Therapy Pill Be? Res Dev Disabil 2015, 37, 9–16. [Google Scholar] [CrossRef]
- Brandão, M.B.; Mancini, M.C.; Ferre, C.L.; Figueiredo, P.R.P.; Oliveira, R.H.S.; Gonçalves, S.C.; Dias, M.C.S.; Gordon, A.M. Does Dosage Matter? A Pilot Study of Hand-Arm Bimanual Intensive Training (HABIT) Dose and Dosing Schedule in Children with Unilateral Cerebral Palsy. Phys Occup Ther Pediatr 2018, 38, 227–242. [Google Scholar] [CrossRef]
- Gordon, A.M.; Hung, Y.C.; Brandao, M.; Ferre, C.L.; Kuo, H.C.; Friel, K.; Petra, E.; Chinnan, A.; Charles, J.R. Bimanual Training and Constraint-Induced Movement Therapy in Children with Hemiplegic Cerebral Palsy: A Randomized Trial. Neurorehabil Neural Repair 2011, 25, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Surkar, S.M.; Hoffman, R.M.; Willett, S.; Flegle, J.; Harbourne, R.; Kurz, M.J. Hand-Arm Bimanual Intensive Therapy Improves Prefrontal Cortex Activation in Children with Hemiplegic Cerebral Palsy. Pediatr Phys Ther. 2018, 30, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.M. To Constrain or Not to Constrain, and Other Stories of Intensive Upper Extremity Training for Children with Unilateral Cerebral Palsy. Dev Med Child Neurol. 2011, 53, 56–61. [Google Scholar] [CrossRef]
- Lang, C.E.; Macdonald, J.R.; Reisman, D.S.; Boyd, L.; Jacobson Kimberley, T.; Schindler-Ivens, S.M.; Hornby, T.G.; Ross, S.A.; Scheets, P.L. Observation of Amounts of Movement Practice Provided during Stroke Rehabilitation. Arch Phys Med Rehabil. 2009, 90, 1692–1698. [Google Scholar] [CrossRef]
- Urbin, M.A.; Bailey, R.R.; Lang, C.E. Validity of Body-Worn Sensor Acceleration Metrics to Index Upper Extremity Function in Hemiparetic Stroke. J Neurol Phys Ther. 2015, 39, 111–118. [Google Scholar] [CrossRef]
- Uswatte, G.; Giuliani, C.; Winstein, C.; Zeringue, A.; Hobbs, L.; Wolf, S.L. Validity of Accelerometry for Monitoring Real-World Arm Activity in Patients With Subacute Stroke: Evidence From the Extremity Constraint-Induced Therapy Evaluation Trial. Arch Phys Med Rehabil 2006, 87, 1340–1345. [Google Scholar] [CrossRef]
- Uswatte, G.; Foo, W.L.; Olmstead, H.; Lopez, K.; Holand, A.; Simms, L.B. Ambulatory Monitoring of Arm Movement Using Accelerometry: An Objective Measure of Upper-Extremity Rehabilitation in Persons With Chronic Stroke. Arch Phys Med Rehabil 2005, 86, 1498–1501. [Google Scholar] [CrossRef]
- Kwakkel, G.; Van Wegen, E.; Burridge, J.H.; Winstein, C.J.; van Dokkum, L.; Alt Murphy, M.; Levin, M.F.; Krakauer, J.W. Standardized Measurement of Quality of Upper Limb Movement after Stroke: Consensus-Based Core Recommendations from the Second Stroke Recovery and Rehabilitation Roundtable. Int J Stroke 2019, 14, 783–791. [Google Scholar] [CrossRef]
- Lang, C.E.; MacDonald, J.R.; Gnip, C. Counting Repetitions: An Observational Study of Outpatient Therapy for People with Hemiparesis Post-Stroke. J Neurol Phys Ther. 2007, 31, 3–10. [Google Scholar] [CrossRef]
- International classification of functioning, disability and health: children and youth version: ICF-CY. World Health Organization, 2007. Available online: https://apps.who.int/iris/handle/10665/43737 (accessed on 10 May 2023).
- Waddell, K.J.; Strube, M.J.; Bailey, R.R.; Klaesner, J.W.; Birkenmeier, R.L.; Dromerick, A.W.; Lang, C.E. Does Task-Specific Training Improve Upper Limb Performance in Daily Life Poststroke? Neurorehabil Neural Repair 2017, 31, 290–300. [Google Scholar] [CrossRef]
- Holsbeeke, L.; Ketelaar, M.; Schoemaker, M.M.; Gorter, J.W. Capacity, Capability, and Performance: Different Constructs or Three of a Kind? Arch Phys Med Rehabil 2009, 90, 849–855. [Google Scholar] [CrossRef]
- Ouyang, R.G.; Yang, C.N.; Qu, Y.L.; Koduri, M.P.; Chien, C.W. Effectiveness of Hand-Arm Bimanual Intensive Training on Upper Extremity Function in Children with Cerebral Palsy: A Systematic Review. Eur. J. Paediatr. 2020, 17–28. [Google Scholar] [CrossRef]
- Adams, S.A. The Effect of Social Desirability and Social Approval on Self-Reports of Physical Activity. Am J Epidemiol 2005, 161, 389–398. [Google Scholar] [CrossRef]
- Elad, D.; Barak, S.; Eisenstein, E.; Bar, O.; Givon, U.; Brezner, A. Discrepancies between Mothers and Clinicians in Assessing Functional Capabilities and Performance of Children with Cerebral Palsy. Res Dev Disabil 2013, 34, 3746–3753. [Google Scholar] [CrossRef]
- Goodwin, B.M.; Sabelhaus, E.K.; Pan, Y.C.; Bjornson, K.F.; Pham, K.L.D.; Walker, W.O.; Steele, K.M. Accelerometer Measurements Indicate That Arm Movements of Children with Cerebral Palsy Do Not Increase after Constraint-Induced Movement Therapy (CIMT). Am J Occup Ther. 2020, 74, 7405205100p1–7405205100p9. [Google Scholar] [CrossRef]
- Mitchell, L.E.; Ziviani, J.; Boyd, R.N. A Randomized Controlled Trial of Web-Based Training to Increase Activity in Children with Cerebral Palsy. Dev Med Child Neurol 2016, 58, 767–773. [Google Scholar] [CrossRef]
- Doman, C.A.; Waddell, K.J.; Bailey, R.R.; Moore, J.L.; Lang, C.E. Changes in Upper-Extremity Functional Capacity and Daily Performance During Outpatient Occupational Therapy for People With Stroke. Am J Occup Ther. 2016, 70, 7003290040p1–7003290040p11. [Google Scholar] [CrossRef] [PubMed]
- Waddell, K. Exploring the Complexities of Real-World Upper Limb Exploring the Complexities of Real World Upper Limb Performance after Stroke Performance after Stroke . 2019. Available online: https://openscholarship.wustl.edu/art_sci_etds/1800.
- Bailey, R.R.; Klaesner, J.W.; Lang, C.E. Quantifying Real-World Upper-Limb Activity in Nondisabled Adults and Adults with Chronic Stroke. Neurorehabil Neural Repair 2015, 29, 969–978. [Google Scholar] [CrossRef]
- Hoyt, C.R.; Brown, S.K.; Sherman, S.K.; Wood-Smith, M.; Van, A.N.; Ortega, M.; Nguyen, A.L.; Lang, C.E.; Schlaggar, B.L.; Dosenbach, N.U.F. Using Accelerometry for Measurement of Motor Behavior in Children: Relationship of Real-World Movement to Standardized Evaluation. Res Dev Disabil 2020, 96, 103546. [Google Scholar] [CrossRef]
- Coker-Bolt, P.; Downey, R.J.; Connolly, J.; Hoover, R.; Shelton, D.; Seo, N.J. Exploring the Feasibility and Use of Accelerometers before, during, and after a Camp-Based CIMT Program for Children with Cerebral Palsy. J Pediatr Rehabil Med 2017, 10, 27–36. [Google Scholar] [CrossRef]
- National Institute of Allergy and Infectious Diseases (NIAID). For ancillary studies, consider NIH definitions carefully. Available online: https://www.niaid.nih.gov/grants-contracts/ancillary-studies-definitions (accessed on 23 May 2023).
- Lang, C.E.; Waddell, K.J.; Klaesner, J.W.; Bland, M.D. A Method for Quantifying Upper Limb Performance in Daily Life Using Accelerometers. J Vis Exp. 2017, (122), 55673. [Google Scholar]
- Mitchell, L.E.; Ziviani, J.; Boyd, R.N. Variability in Measuring Physical Activity in Children with Cerebral Palsy. Med Sci Sports Exerc 2015, 47, 194–200. [Google Scholar] [CrossRef]
- Krumlinde-Sundholm, L.; Holmefur, M.; Kottorp, A.; Eliasson, A.-C. The Assisting Hand Assessment: Current Evidence of Validity, Reliability, and Responsiveness to Change. Dev Med Child Neurol 2007, 49, 259–264. [Google Scholar] [CrossRef]
- Krumlinde-Sundholm, L. Reporting Outcomes of the Assisting Hand Assessment: What Scale Should Be Used? Dev Med Child Neurol 2012, 54, 807–808. [Google Scholar] [CrossRef]
- Tofani, M.; Castelli, E.; Sabbadini, M.; Berardi, A.; Murgia, M.; Servadio, A.; Galeoto, G. Examining Reliability and Validity of the Jebsen-Taylor Hand Function Test Among Children with Cerebral Palsy. Percept Mot Skills 2020, 127, 684–697. [Google Scholar] [CrossRef]
- Poole, J.L.; Burtner, P.A.; Torres, T.A.; McMullen, C.K.; Markham, A.; Marcum, M.L.; Anderson, J.B.; Qualls, C. Measuring Dexterity in Children Using the Nine-Hole Peg Test. J Hand Ther. 2005, 18, 348–351. [Google Scholar] [CrossRef] [PubMed]
- Jongbloed-Pereboom, M.; Nijhuis-van der Sanden, M.W.G.; Steenbergen, B. Norm Scores of the Box and Block Test for Children Ages 3–10 Years. Am J Occup Ther. 2013, 67, 312–318. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav Res Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Araneda, R.; Ebner-Karestinos, D.; Paradis, J.; Saussez, G.; Friel, K.M.; Gordon, A.M.; Bleyenheuft, Y. Reliability and Responsiveness of the Jebsen-Taylor Test of Hand Function and the Box and Block Test for Children with Cerebral Palsy. Dev Med Child Neurol 2019, 61, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Lohse, K.R.; Birkenmeier, R.L. Dose and Timing in Neurorehabilitation: Prescribing Motor Therapy after Stroke. Curr. Opin. Neurol. 2015, 28, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Connell, L.A.; McMahon, N.E.; Simpson, L.A.; Watkins, C.L.; Eng, J.J. Investigating Measures of Intensity During a Structured Upper Limb Exercise Program in Stroke Rehabilitation: An Exploratory Study. Arch Phys Med Rehabil 2014, 95, 2410–2419. [Google Scholar] [CrossRef]
- Lang, C.E.; Wagner, J.M.; Edwards, D.F.; Dromerick, A.W. Upper Extremity Use in People with Hemiparesis in the First Few Weeks after Stroke. J Neurol Phys Ther 2007, 31, 56–63. [Google Scholar] [CrossRef]
- Rand, D.; Givon, N.; Weingarden, H.; Nota, A.; Zeilig, G. Eliciting Upper Extremity Purposeful Movements Using Video Games. Neurorehabil Neural Repair 2014, 28, 733–739. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).