1. Introduction
Odontogenic cysts are a unique disorder characterized by an epithelial lined pathological cavity [
1]. This condition appears as a result of inflammatory occurrence or of the pathogenic causes associated with the epithelium development of tooth-forming apparatus [
2]. Thus, the epithelial lining of these cysts can derive from the odontogenic epithelium, which includes reduced enamel epithelium, the epithelial cell rests of Serres, and the epithelial cell rests of Malassez [
3].
The most common odontogenic cysts are radicular cysts, which develop from an inflammatory process. Cysts evolve at the root apex of a non-vital tooth typically due to dental caries or associated trauma. The inflammatory process spreads into the tissues that envelop the tooth, including the periodontal ligament — containing the epithelial rests of Malassez cells— and the bone [
4]. The release of inflammatory mediators is thought to stimulate the epithelial rests to proliferate [
5].
Radiographically, radicular cysts are shown as a well-demarcated radiolucency directly associated with the apex of the tooth. Although typically small, with less than 1cm, they can enlarge to many times its size with destructive capabilities because of their expansion potential [
6].
The treatment of radicular cysts can be accomplished through non-surgical and root canal surgical root canal therapy or as well as with extraction. After excision, the entire cyst should be histologically examined because other lesions, including tumors, can appear radiographically similar [
4].
After the complete removal of a cyst, patients can be left with insufficient bone volume for implant placement.
Bone augmentation procedures have been studied by many authors and can be broadly divided into horizontal (increase in width) or vertical bone augmentation (increase in height) [
7]. In many cases, a combination of both is needed. Non-resorbable membranes or titanium meshes can be used to predictably augment bone in alveolar bone deficiencies. In Guided Bone Regeneration (GBR), these barrier membranes can be used in combination with graft materials [
8].
In 2013, Merli et al. described the “fence technique” in which a space is created by molding an osteosynthesis plate, based on the volume of the bone graft that is planned ahead. The molded plate, or the “fence”, will not only provide a retaining space for the bone graft but also serve as a support for the collagen membranes covering the grafted material [
8,
9].
The “fence technique” can be applied in osseous defects localized to a portion of the maxillary or mandibular arch when anatomic prosthodontic requirements do not permit the use of short or tilted implants [
8].
This two-stage technique is described to cause limited discomfort to the patient and has been proposed for cases of extreme bone atrophy due to the capacity for the formation of large quantities of regenerated bone in both vertical and horizontal dimensions [
8].
2. Materials and Methods
A Caucasian male patient, 50 years old, without systemic pathologies and no smoker, was attended at the private clinic for rehabilitation with dental implants at the region of teeth 11 and 21.
The tooth 11 was previously submitted to an endodontic treatment being the prognostic impossible.
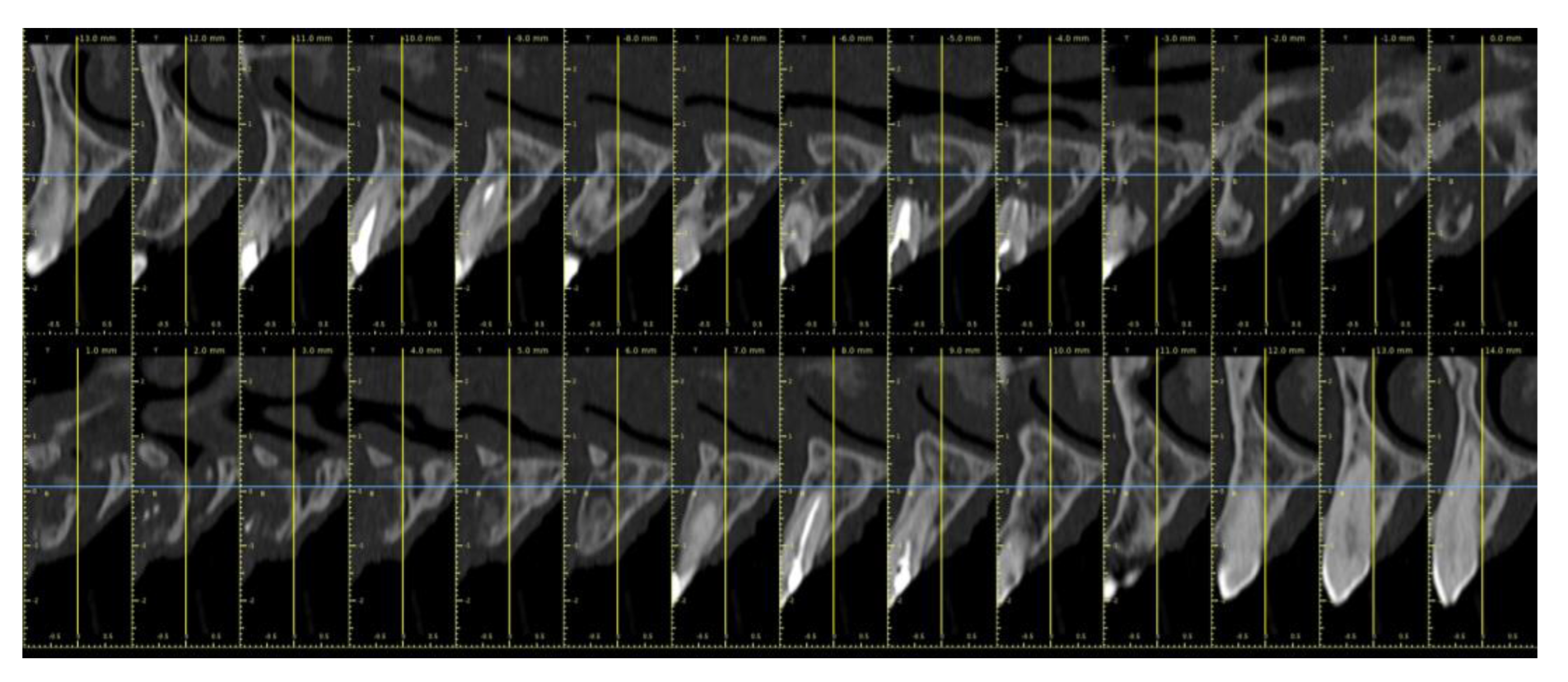
Through the computer tomography (
Figure 1 and
Figure 2) was observed a large cyst that extend from tooth 12 to mesial of tooth 22, at the apical portion of the region of the 21 along with the invasion of the nasal floor and the nasopalatine nerve canal.
A new endodontic treatment was performed at tooth 12 and the tooth 11 was extracted; a partial removal prothesis was placed.
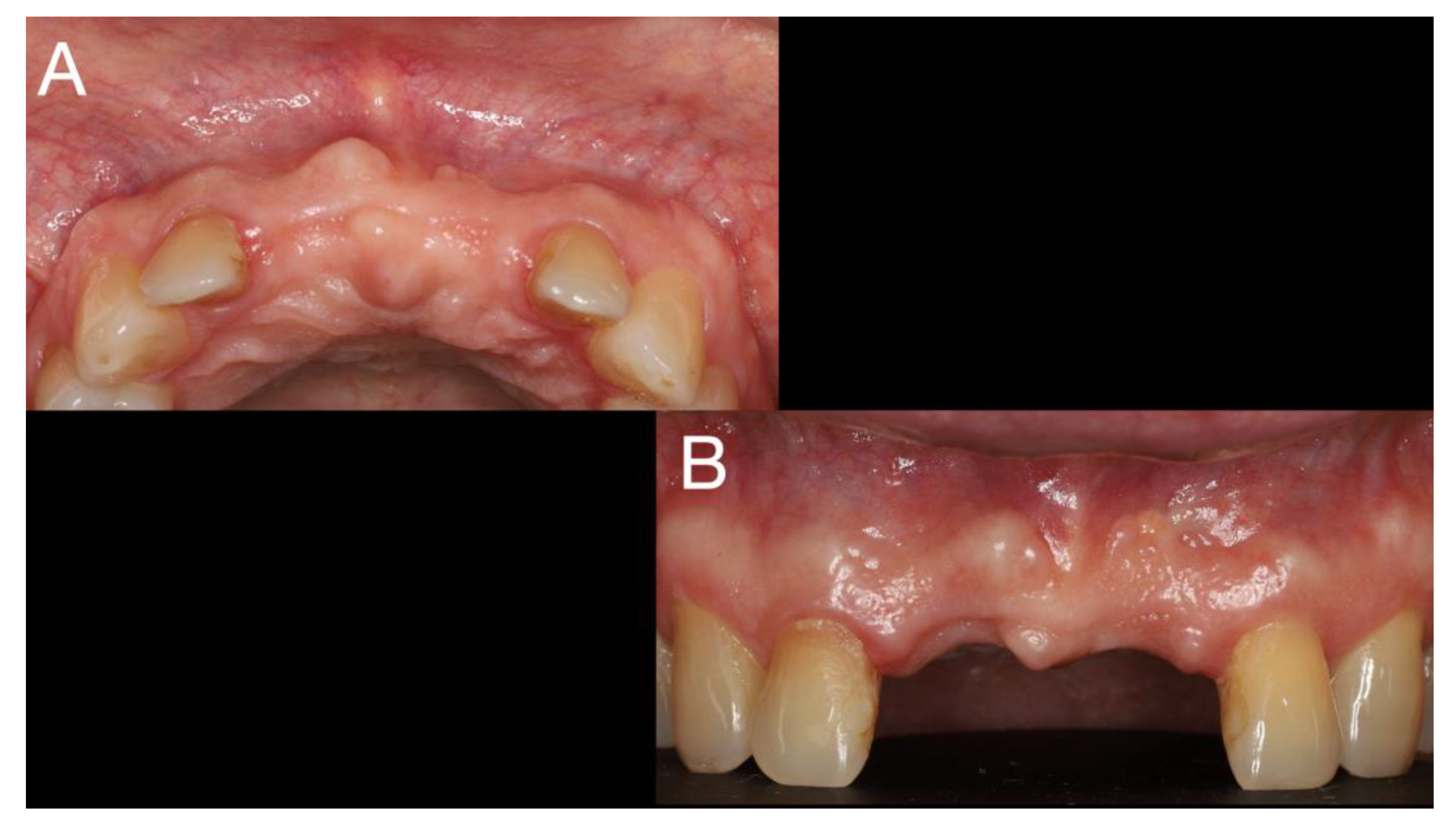
After 6 weeks for healing of soft tissue (
Figure 3), the surgery of cyst enucleation and guide bone regeneration with fence technique [
9] was performed.
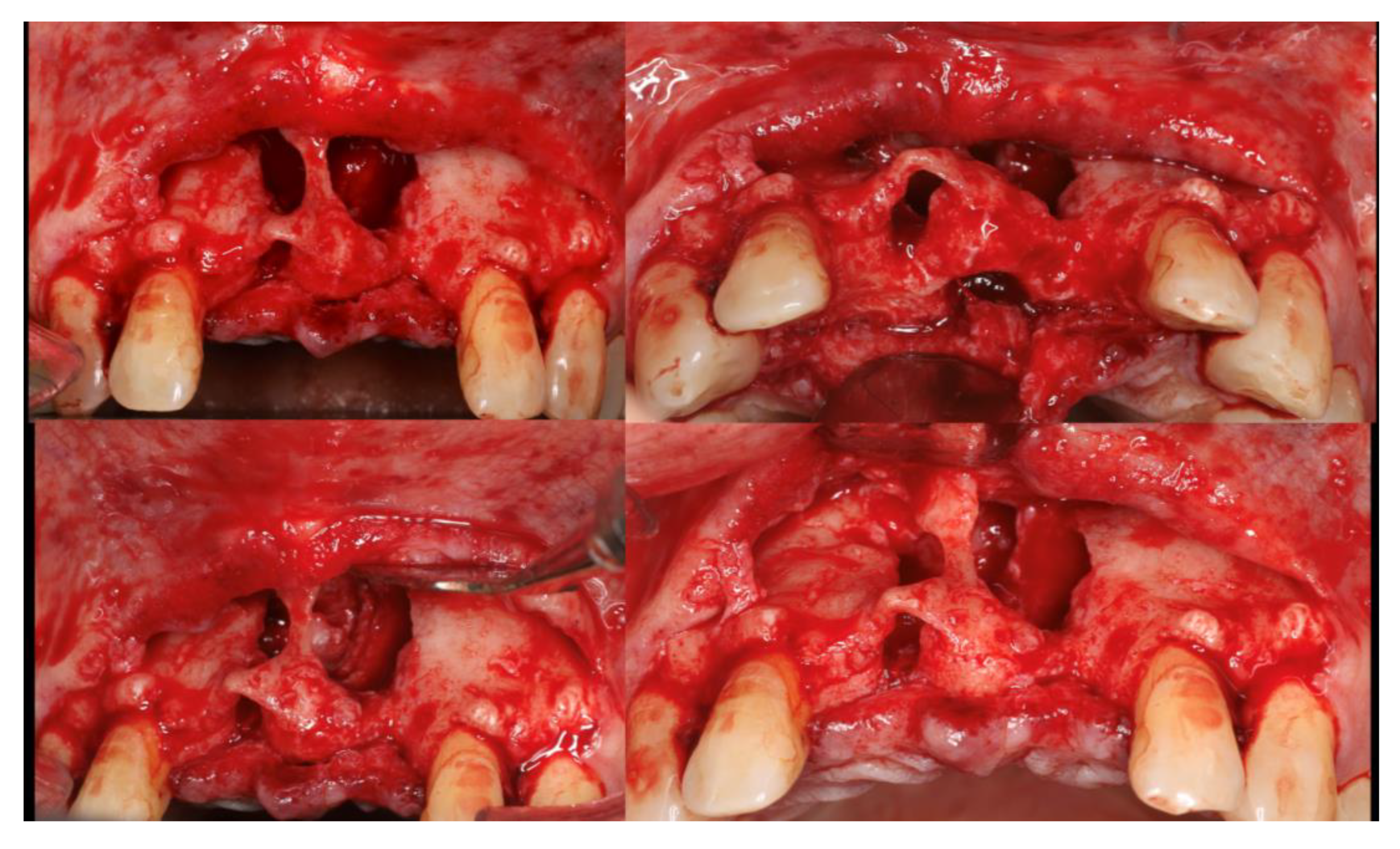
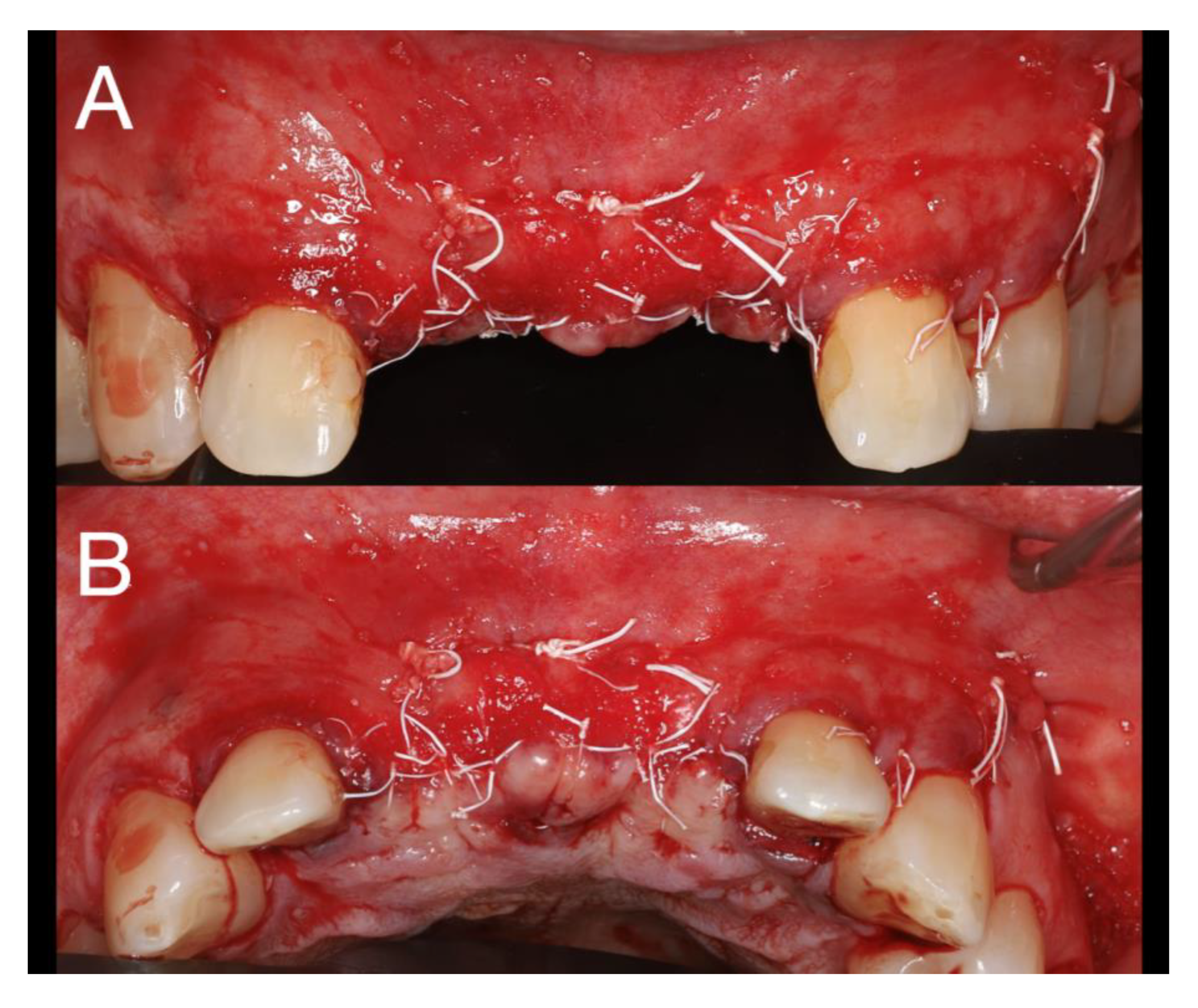
Local anesthesia with articaine (artinibsa® 40mg/ml + 0.01mg/ml, Inibsa®, Spain) was given. A linear incision with a 15 blade was performed form the distal aspect of tooth 13 to mesial of tooth 23 where a releasing incision that cross the mucogingival line was performed. A full thickness flap was elevated, and the cyst was enucleated (
Figure 4). During odontogenic of the cyst enucleation (histological established), special attention was given to maintain the integrity of the anterior nasal spine. Even with the carfule enucleation, a communication with the nasal floor occurred and a loss of the palatine bone plate was observed (
Figure 4).
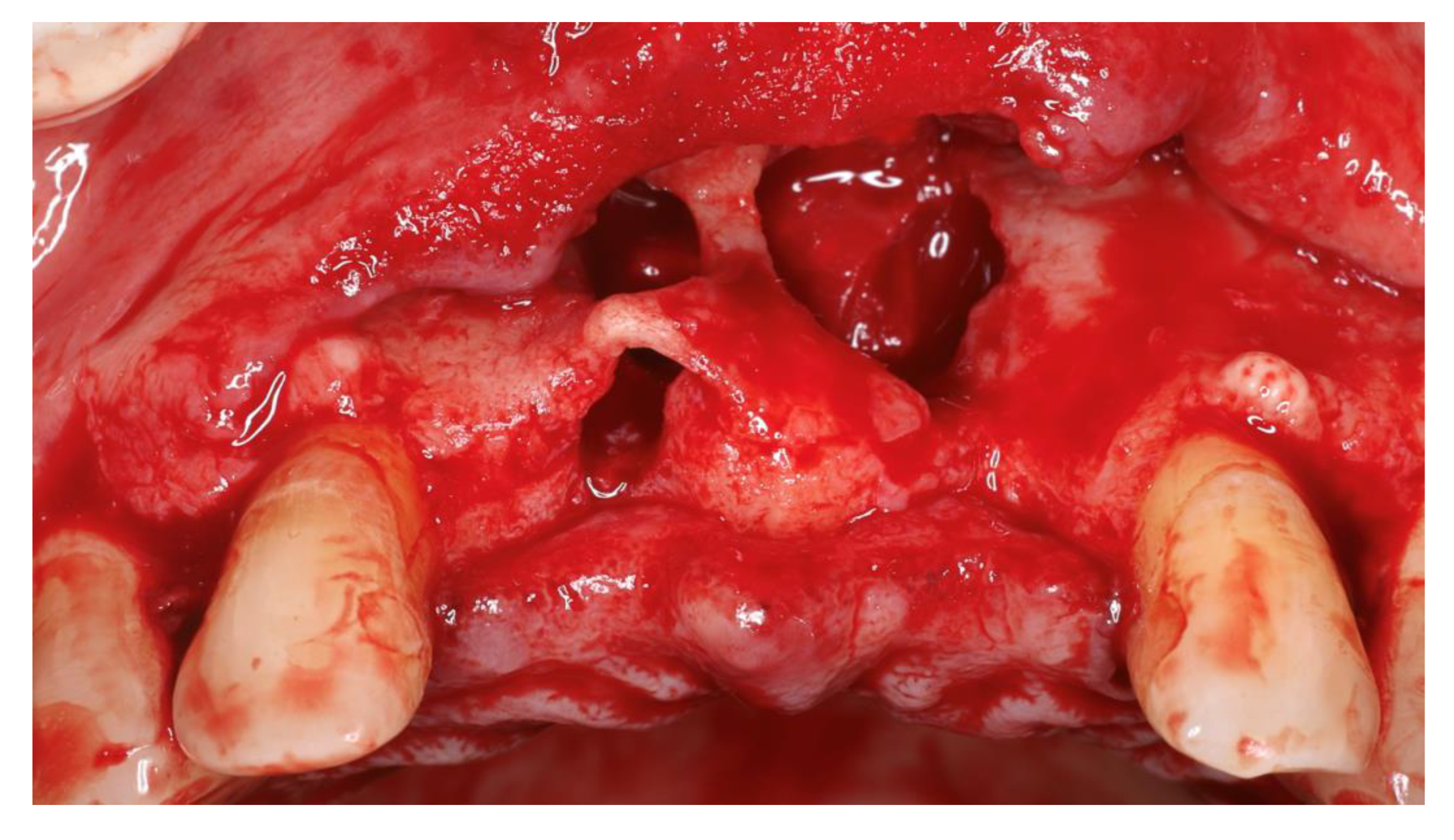
A collagen membrane (Bio-Gide
®, Geistlich
®, Swiss) was placed (
Figure 5) to seal the nasal floor communication and palatine bone plate was collocated prior to the placement of the particulate xenograft (Bio-Oss
® S, Geistlich
®, Swiss).
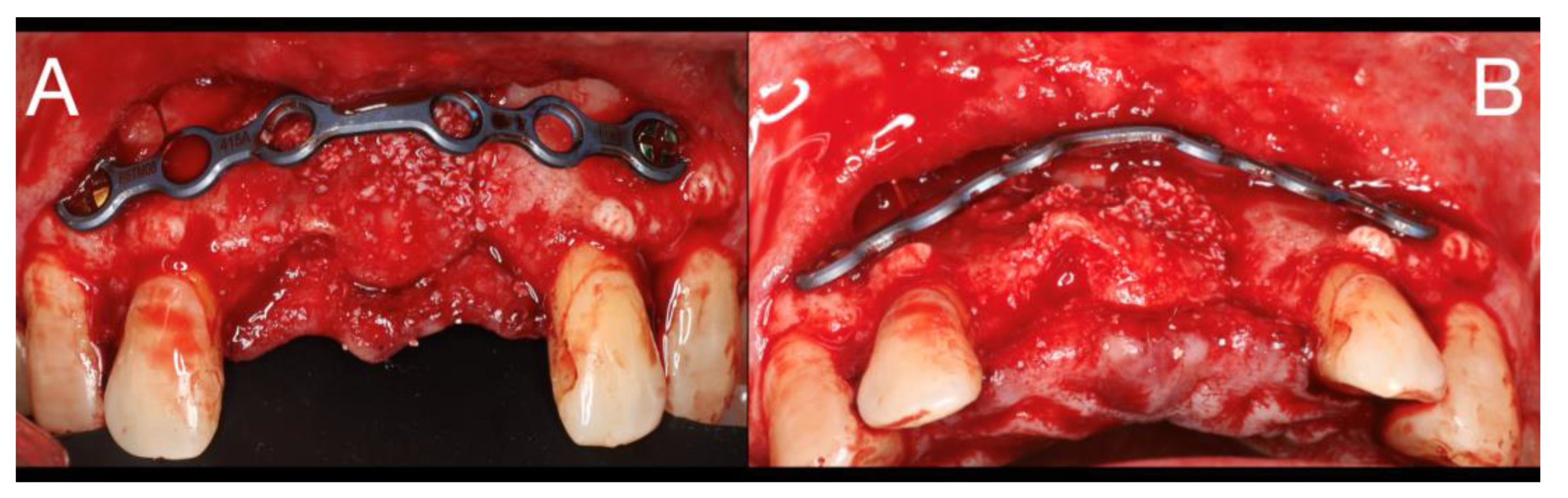
A titanium straight plate with 0.8 mm of thickness (Global D, Brignais
®, France) was molded to give the shape of the alveolar ridge and fixed with two screws (
Figure 6) and the released periosteous incisions was performed with a 15 blade.
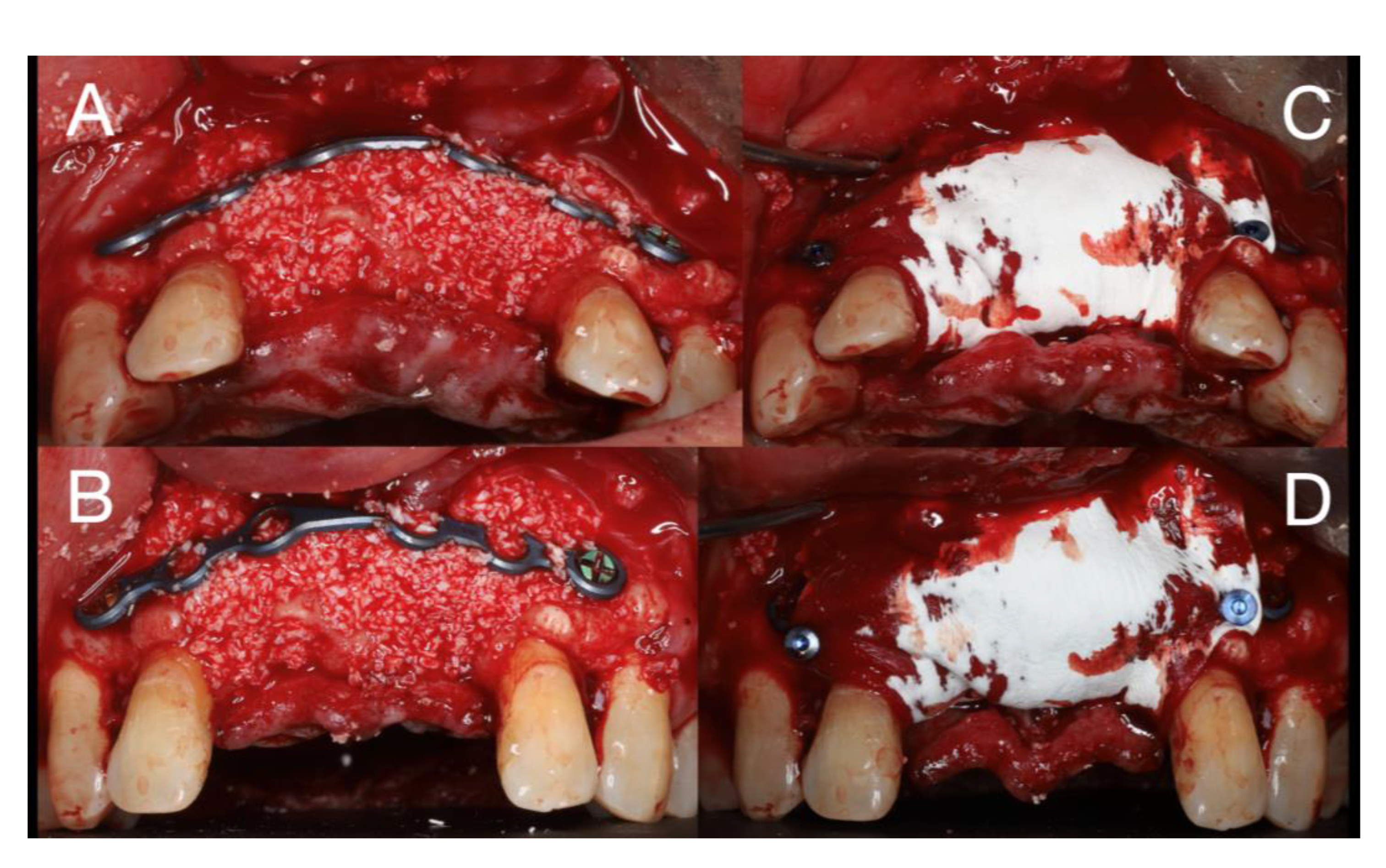
The gap between the bone and the plate was filled with particulate xenograft (Bio-Oss
® S, Geistlich
®, Swiss) and covered with a collagen membrane (Bio-Gide
®, Geistlich
®, Swiss) fixed with pins (
Figure 7). The flap was sutured with PTFE 5.0 (Medipac, Kilkis
®, Greece) with horizontal mattress suture and simple stiches (
Figure 8).
The prescription comprised of an antibiotic (amoxicillin and clavulanic acid 875+125mg) 12/12h for 8 days; corticoid (glucocorticoid) 60mg/day for 3 days; a pain killer (paracetamol 500mg + Codeine hemihydrate phosphate 30mg) 12/12h for 3 days; and chlorhexidine mouthwash 0,12%, 3 times/day for 10 days. The suture was removed after 10 days.
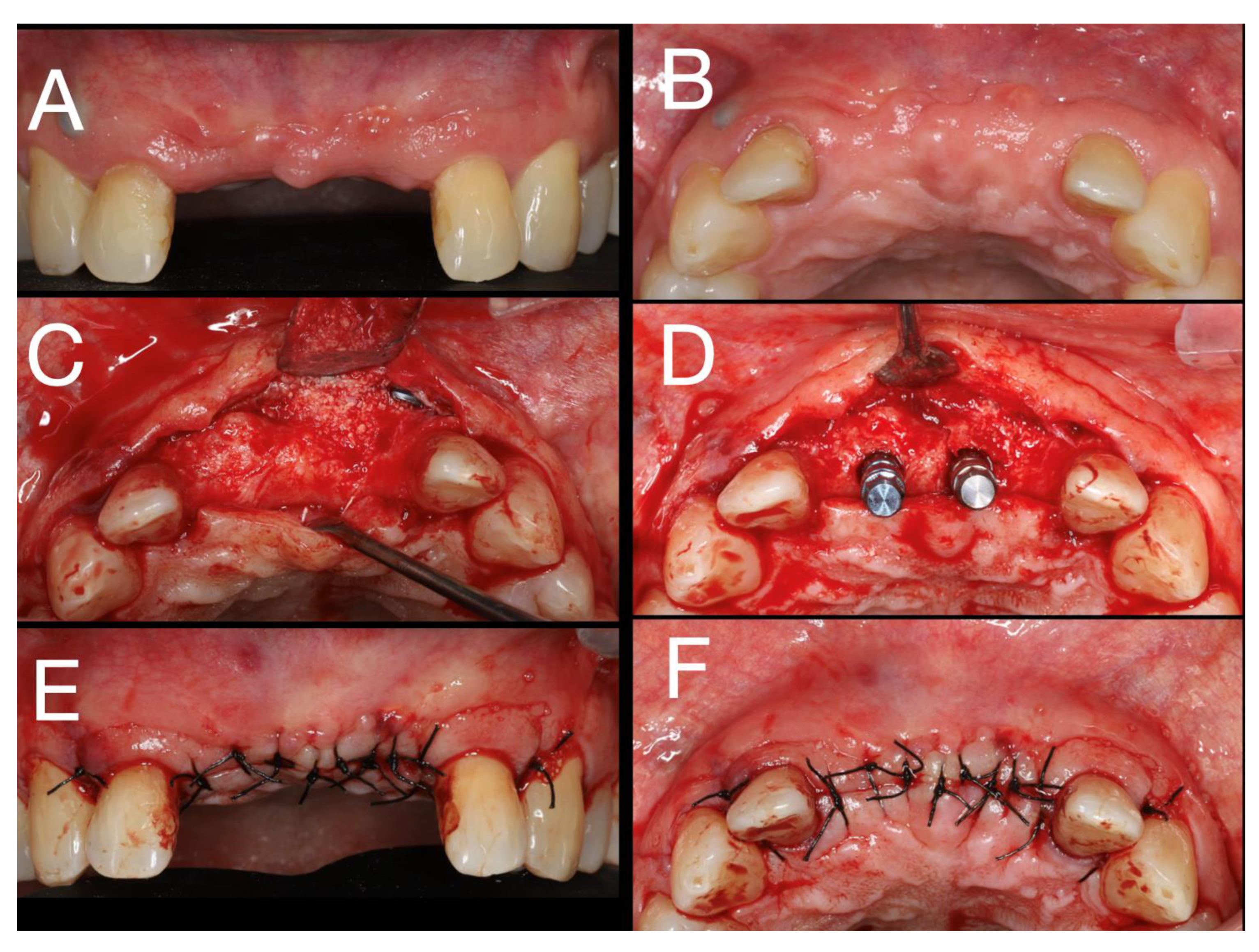
After 6 months, with healing without any adverse event, the placement of the 2 implants was planned (
Figure 9A,B).
An incision with a 15 blade between teeth 13 and 23 under local anesthesia with articaine (artinibsa
® 40mg/ml + 0.01mg/ml, Inibsa
®, Spain) was executed and a full-thickness flap was raised (
Figure 9C).
The Bone level
® (Straumann
®, Swiss) drilling protocol for the two dental implants 4.1x10RC at the region of the teeth 11 and 21 was followed (
Figure 9D). The cover screws were placed, and the flap sutured with polyamide 4.0 (Supramida
®, B Braun
®, Germany)) (
Figure 9E,F). As follow-up it, was indicated azithromycin 500mg 1 pill at day for 3 days, ibuprofen 600mg, 12/12h for 4 days, chlorhexidine mouthwash 0,12%, 3 times/day for 10 days and the suture removed after 8 days.
Nine weeks after, the second phase implant surgery was performed, being both implants osteointegrated. The implant-supported prostheses were placed two months after.
After 18 months is possible to observe a (
Figure 10) aesthetic pleasant soft tissue architecture and a manutention of the bone volume achieve with the bone regeneration. No signs of reoccurrence of cyst were found.
4. Discussion
Radicular cysts are the most common inflammatory odontogenic cysts of tooth bearing-areas of the jaws [
10]. In the maxilla, this type of lesion has a prevalence of 60% [
11]. With a typically slow and asymptomatic evolution, it can lead to extensive bone resorption and tooth mobility or loss, thus, a radiographic diagnosis is of major importance [
10]. During cyst enucleation it is crucial to ensure that the cystic capsule is completely removed, therefore preventing the possibility of recurrence [
12]. Recurrence rates can vary from 33% to 44% [
13,
14].
In the presented case, the cyst expansion resulted in extensive bone loss that led to communication with the nasal floor and an extensive bone loss, leaving no palatine bone plate after the cyst enucleation. Since insufficient bone was left for adequate implant placement, guided bone regeneration (GBR) arises as an adequate tissue engineering-based reconstruction technique to achieve good bone regeneration. The “fence technique” principle uses a modeled plate to prevent the invasion of soft tissue into the defect area, providing a retaining space for the bone graft based on the volume of the bone graft that is planned prior to the surgery. With the use of a membrane, it provides a microenvironment for osteoprogenitor cells to develop and proliferate to become mature osteoblast cells [
15].
The major disadvantage of synthetic membranes is that the body cannot absorb them, so a second surgery is needed to remove the membrane after the bone is well-formed and matured [
16].
A 2020 study by Merli M. et al.[
17] compares vertical bone augmentation grafting with 100% autogenous bone vs 50% deproteinized bovine bone matrix/50% autogenous bone using the fence technique, in a two-stage implant placement, presenting no significant differences in the histomorphometric comparisons 6 months after grafting.
Xenografts have been shown to have valid properties for GBR, like its biocompatibility, formation of a scaffold (osteoconduction), slow resorption rates, and the ability to define and maintain the volume for bone gain [
18]. Thus, xenografts are an attractive alternative for not submitting the patient to further procedures [
19,
20,
21].
In the 2015 meta-analysis by Sanz-Sánches I. et al. [
22], the use of bone replacement grafts with barrier membranes and a staged approach presented a mean high survival and success rates (>95%) for the implants placed on the regenerated sites, with the non-exposure of the membranes being an important aim.
In this case, contrary to the described by Merli M.[
8], a 100% xenograft (Bio-Oss
® S, Geistlich
®, Swiss) was used. This bone graft is derived from bovine bone without the organic substances. No signs of inflammation nor infection were visible, as well as no tendency for a decrease in bone volume was observed over time, as described by Mello I. et al. [
18] The patient was pleased with the result, minor complications were associated with the procedure, only a slight edema that was self-limiting. Thereby, the use of only xenografts appears to be a viable option for GBR, when the patient is not predisposed to further procedures. Nonetheless, at reentry, xenograft particles were still observed. This is expected since the literature reports a “slow-turnover” for the resorption and replacement of bovine bone xenografts [
23]. However, further controls must be done throw time to guarantee the stability and health of the implants.
Since the patient has a lower smile, he hasn´t any complains of the plate translucidities’ and to avoid a more invasive process, it was opted for leave the titanium plate. Since this plate is biocompatible, no major problems are expecting to occur.
As reported by Merli M. et al.[
17], this two-stage technique allows for the formation of large quantities of regenerated bone in both vertical and horizontal dimensions in cases of extreme bone atrophy, enabling a correct implant placement and pleasant results resulting into the patient satisfaction. Thus, this technique appears as a valid GBR technique [
8].
5. Conclusions
In this clinical case with a follow up of 18 months, is possible to observe that bone volume reconstructed is stable and allowed an aesthetics result in terms of soft and hard tissue.
Radiographically, no reoccurrence of the odontogenic cyst was observed, being the enucleation successful.
The fence technique allowed the maintenance of the space that help to obtain a normal contour of the maxillary arch and aloud the dental implant placement.
Author Contributions
F. Correia, contributed to the conception, data acquisition, analysis, draft and critical review of the manuscript; A. Brum Marques, contributed to the conception, analysis, interpretation, draft and critical review of the manuscript; : C. Rodrigues, contributed to the conception, data acquisition and critical review of the manuscript; R. Faria Almeida, contributed to the conception, draft and critical review of the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Not applicable.
Acknowledgments
In this section, you can acknowledge any support given which is not covered by the author contribution or funding sections. This may include administrative and technical support, or donations in kind (e.g., materials used for experiments).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Johnson, N.R.; Gannon, O.M.; Savage, N.W.; Batstone, M.D. , Frequency of odontogenic cysts and tumors: a systematic review. J Investig Clin Dent 2014, 5, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Rajendra Santosh, A.B. , Odontogenic Cysts. Dent Clin North Am 2020, 64, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Rioux-Forker, D.; Deziel, A.C.; Williams, L.S.; Muzaffar, A.R. , Odontogenic Cysts and Tumors. Ann Plast Surg 2019, 82, 469–477. [Google Scholar]
- Robinson, R.A. , Diagnosing the most common odontogenic cystic and osseous lesions of the jaws for the practicing pathologist. Mod Pathol 2017, 30, S96–S103. [Google Scholar] [CrossRef] [PubMed]
- Browne, R.M. , Some observations on the fluids of odontogenic cysts. J Oral Pathol 1976, 5, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Marmary, Y.; Kutiner, G. , A radiographic survey of periapical jawbone lesions. Oral Surg Oral Med Oral Pathol 1986, 61, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Felice, P.; Karatzopoulos, G.; Worthington, H.V.; Coulthard, P. , Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev 2009, 2009, CD003607. [Google Scholar] [CrossRef]
- Merli, M.; Mariotti, G.; Moscatelli, M.; Motroni, A.; Mazzoni, A.; Mazzoni, S.; Nieri, M. , Fence technique for localized three-dimensional bone augmentation: a technical description and case reports. Int J Periodontics Restorative Dent 2015, 35, 57–64. [Google Scholar] [CrossRef]
- Merli, M.; Moscatelli, M.; Mazzoni, A.; Mazzoni, S.; Pagliaro, U.; Breschi, L.; Motroni, A.; Nieri, M. , Fence technique: guided bone regeneration for extensive three-dimensional augmentation. Int J Periodontics Restorative Dent 2013, 33, 129–136. [Google Scholar] [CrossRef]
- Deshmukh, J.; Shrivastava, R.; Bharath, K.P.; Mallikarjuna, R. , Giant radicular cyst of the maxilla. BMJ Case Rep 2014, 2014. [Google Scholar] [CrossRef]
- Shear, M.; Speight, P.M. , Cysts of the oral and maxillofacial regions. John Wiley & Sons:, 2008. [Google Scholar]
- Chhabra, N.; Chhabra, S.; Kumar, A. , Cyst Enucleation Revisited: A New Technical Modification to Ensure Complete Removal of Cystic Lining. J Maxillofac Oral Surg 2020, 19, 173–177. [Google Scholar] [CrossRef]
- Pindborg, J.J.; Hansen, J. , Studies on Odontogenic Cyst Epithelium. 2. Clinical and Roentgenologic Aspects of Odontogenic Keratocysts. Acta Pathol Microbiol Scand 1963, 58, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Toller, P.A. , Newer concepts of odontogenic cysts. Int J Oral Surg 1972, 1, 3–16. [Google Scholar] [CrossRef]
- Ren, Y.; Fan, L.; Alkildani, S.; Liu, L.; Emmert, S.; Najman, S.; Rimashevskiy, D.; Schnettler, R.; Jung, O.; Xiong, X.; Barbeck, M. , Barrier Membranes for Guided Bone Regeneration (GBR): A Focus on Recent Advances in Collagen Membranes. Int J Mol Sci 2022, 23, 14987. [Google Scholar] [CrossRef]
- Retzepi, M.; Donos, N. , Guided Bone Regeneration: biological principle and therapeutic applications. Clin Oral Implants Res 2010, 21, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Merli, M.; Mariotti, G.; Pagliaro, U.; Mazzoni, A.; Moscatelli, M.; Nieri, M. , The Fence Technique: 100% Autogenous Bone Graft vs 50% Deproteinized Bovine Bone Matrix and 50% Autogenous Bone Graft. A Histologic Randomized Controlled Trial. Int J Periodontics Restorative Dent 2020, 40, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Mello, B.F.; de Carvalho Formiga, M.; de Souza da Silva, L.F.; Dos Santos Coura, G.; Shibli, J.A. , Horizontal Ridge Augmentation Using a Xenograft Bone Substitute for Implant-Supported Fixed Rehabilitation: A Case Report with Four Years of Follow-Up. Case Rep Dent 2020, 2020, 6723936. [Google Scholar] [CrossRef]
- Al-Nawas, B.; Schiegnitz, E. , Augmentation procedures using bone substitute materials or autogenous bone - a systematic review and meta-analysis. Eur J Oral Implantol 2014, 7 (Suppl 2), S219–S234. [Google Scholar]
- Urban, I.A.; Nagursky, H.; Lozada, J.L.; Nagy, K. , Horizontal ridge augmentation with a collagen membrane and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: a prospective case series in 25 patients. Int J Periodontics Restorative Dent 2013, 33, 299–307. [Google Scholar] [CrossRef]
- Pellegrini, G.; Pagni, G.; Rasperini, G. , Surgical Approaches Based on Biological Objectives: GTR versus GBR Techniques. Int J Dent 2013, 2013, 521547. [Google Scholar] [CrossRef]
- Sanz-Sanchez, I.; Ortiz-Vigon, A.; Sanz-Martin, I.; Figuero, E.; Sanz, M. , Effectiveness of Lateral Bone Augmentation on the Alveolar Crest Dimension: A Systematic Review and Meta-analysis. J Dent Res 2015, 94 (Suppl. 9), 128S–142S. [Google Scholar] [CrossRef] [PubMed]
- Galindo-Moreno, P.; Hernandez-Cortes, P.; Mesa, F.; Carranza, N.; Juodzbalys, G.; Aguilar, M.; O'Valle, F. , Slow resorption of anorganic bovine bone by osteoclasts in maxillary sinus augmentation. Clin Implant Dent Relat Res 2013, 15, 858–866. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).