Submitted:
23 June 2023
Posted:
25 June 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and methods
Sample preparation
- 0-
- no treatment (control samples),
- 1-
- exposed to brushing (with a professional dental cleaning brush and abrasive paste, Super Polish, Kerr),
- 2-
- exposed to ultrasonic scaling (with a ultrasonic scaler incorporated in a dental unit).
Surface characteristics of zirconia surface
Scanning electron microscopy (SEM)
Biofilm formation assay
Statistical analysis
Results
SEM imaging
Biofilm formation on different zirconia samples
Discussion
Conclusion
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gomes, A.L.; Montero, J. Zirconia implant abutments: A review. Med Oral Patol Oral Cir Bucal 2011, 16, e50–e55. [Google Scholar] [CrossRef] [PubMed]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Hisbergues, M.; Vendeville, S.; Vendeville, P. Zirconia: Established facts and perspectives for a biomaterial in dental implantology. Journal of Biomedical Materials Research. Part B, Applied Biomaterials 2009, 88, 519–529. [Google Scholar] [CrossRef]
- Lee, B.C.; Jung, G.Y.; Kim, D.J.; Han, J.S. Initial bacterial adhesion on resin, titanium and zirconia in vitro. Journal of Advanced Prosthodontics 2011, 3, 81–84. [Google Scholar] [CrossRef]
- Saravi, B.; Vollmer, A.; Hartmann, M.; Lang, G.; Kohal, R.-J.; Boeker, M.; Patzelt, S.B.M. Clinical Performance of CAD/CAM All-Ceramic Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. Materials 2021, 14, 2672. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, I.F.A.; Santos Marques, T.M.S.; Araújo, F.M.; Azevedo, L.F.; Donato, H.; Correia, A. Clinical Performance of CAD/CAM Tooth-Supported Ceramic Restorations: A Systematic Review. Int. J. Periodontics Restor. Dent. 2018, 38, e68–e78. [Google Scholar] [CrossRef]
- Vitti, R.P.; Catelan, A.; Amaral, M.; Pacheco, R.R. Zirconium in dentistry. Advanced Dental Biomaterials 2019, 317–345. [Google Scholar]
- Cantner, F.; Cacaci, C.; Mücke, T.; Randelzhofer, P.; Hajtó, J.; Beuer, F. Clinical performance of tooth- or implant-supported veneered zirconia single crowns: 42-month results. Clin Oral Investig 2019, 23, 4301–4309. [Google Scholar] [CrossRef]
- de Matos, J.D.M.; Lopes, G.R.S.; Queiroz, D.A.; Nakano, L.J.N.; Ribeiro, N.C.R.; Barbosa, A.B.; Anami, L.C.; Bottino, M.A. Dental Ceramics: Fabrication Methods and Aesthetic Characterization. Coatings 2022, 12, 1228. [Google Scholar] [CrossRef]
- Vieira Colombo, A.P.; Magalhães, C.B.; Hartenbach, F.A.; Martins do Souto, R.; Maciel da Silva-Boghossian, C. Periodontal-disease-associated biofilm: A reservoir for pathogens of medical importance. Microb Pathog. 2016, 94, 27–34. [Google Scholar] [CrossRef]
- Offenbacher, S.; Barros, S.P.; Singer, R.E.; Moss, K.; Williams, R.C.; Beck, J.D. Periodontal disease at the biofilm–gingival interface. Journal of periodontology 2007, 78, 1911–1925. [Google Scholar] [CrossRef]
- Heitz-Mayfield, L.J.; Lang, N.P. Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontology 2000 2010, 53, 167–181. [Google Scholar] [CrossRef] [PubMed]
- Pita, P.P.C.; Rodrigues, J.A.; Ota-Tsuzuki, C.; Miato, T.F.; Zenobio, E.G.; Giro, G.; Figueiredo, L.C.; Gonçalves, C.; Gehrke, S.A.; Cassoni, A. Oral streptococci biofilm formation on different implant surface topographies. BioMed Res. Int. 2015, 2015, 159625. [Google Scholar] [CrossRef]
- Li, J.; Helmerhorst, E.J.; Leone, C.W.; Troxler, R.F.; Yaskell, T.; Haffajee, A.D.; Socransky, S.S.; Oppenheim, F.G. Identification of early microbial colonizers in human dental biofilm. Journal of Applied Microbiology 2004. [Google Scholar] [CrossRef]
- Øilo, M.; Bakken, V. Biofilm and dental biomaterials. Materials 2015, 8, 2887–2900. [Google Scholar] [CrossRef]
- Cinquini, C.; Alfonsi, F.; Marchio, V.; Gallo, F.; Zingari, F.; Bolzoni, A.R.; Romeggio, S.; Barone, A. The Use of Zirconia for Implant-Supported Fixed Complete Dental Prostheses: A Narrative Review. Dent. J. 2023, 11, 144. [Google Scholar] [CrossRef] [PubMed]
- Hjerppe, J.; Rodas, S.; Korvala, J.; Pesonen, P.; Kaisanlahti, A.; Özcan, M.; Suojanen, J.; Reunanen, J. Surface Roughness and Streptococcus mutans Adhesion on Metallic and Ceramic Fixed Prosthodontic Materials after Scaling. Materials 2021, 14, 1027. [Google Scholar] [CrossRef] [PubMed]
- Jaeggi, M.; Gyr, S.; Astasov-Frauenhoffer, M.; Zitzmann, N.U.; Fischer, J.; Rohr, N. Influence of different zirconia surface treatments on biofilm formation in vitro and in situ. Clin Oral Implants Res. 2022, 33, 424–432. [Google Scholar] [CrossRef]
- Chen, H.L.; Yang, S.; Yu, P.; Wu, J.; Guan, H.; Wu, Z. Comparison of bacterial adhesion and biofilm formation on zirconia fabricated by two different approaches: An in vitro and in vivo study. Advances in Applied Ceramics 2020, 119, 323–331. [Google Scholar] [CrossRef]
- Alves, L.M.M.; Contreras, L.P.C.; Bueno, M.G.; Campos, T.M.B.; Bresciani, E.; Valera, M.C. The wear performance of glazed and polished full contour zirconia. Braz Dent J 2019, 30, 511–518. [Google Scholar] [CrossRef]
- Tunkel, J.; Heinecke, A.; Flemmig, T.F. A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002, 29 (Suppl. 3), 72–81. [Google Scholar] [CrossRef]
- Ivanovic, V.; Popovic, D.; Petrovic, S.; Rudolf, R.; Majerič, P.; Lazarevic, M.; Djordjevic, I.; Lazic, V.; Radunovic, M. Unraveling the Antibiofilm Activity of a New Nanogold Resin for Dentures and Epithesis. Pharmaceutics 2022, 14, 1513. [Google Scholar] [CrossRef] [PubMed]
- Brugger, S.D.; Baumberger, C.; Jost, M.; Jenni, W.; Brugger, U.; et al. Automated Counting of Bacterial Colony Forming Units on Agar Plates. PLoS ONE 2012, 7, e33695. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, K.; Nakamura, K.; Harada, A.; Shirato, M.; Inagaki, R.; Örtengren, U.; Kanno, T.; Niwano, Y.; Egusa, H. Surface properties of dental zirconia ceramics affected by ultrasonic scaling and low-temperature degradation. PLoS ONE 2018, 13, e0203849. [Google Scholar] [CrossRef]
- Zupancic Cepic, L.; Dvorak, G.; Piehslinger, E.; Georgopoulos, A. In vitro adherence of Candida albicans to zirconia surfaces. Oral Dis. 2020, 26, 1072–1080. [Google Scholar] [CrossRef]
- Lee, W.F.; Iwasaki, N.; Peng, P.W.; Takahashi, H. Effect of toothbrushing on the optical properties and surface roughness of extrinsically stained high-translucency zirconia. Clin Oral Investig. 2022, 26, 3041–3048. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, S.H.; Han, J.S.; Luke Yeo, I.S.; Yoon, H.I.; Lee, J. Effects of ultrasonic scaling on the optical properties and surface characteristics of highly translucent CAD/CAM ceramic restorative materials: An in vitro study. Ceramics International. 2019, 45, 14594–14601. [Google Scholar] [CrossRef]
- Yoon, H.I.; Noh, H.M.; Park, E.J. Surface changes of metal alloys and high-strength ceramics after ultrasonic scaling and intraoral polishing. J. Adv. Prosthodont. 2017, 9, 188–194. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Camino, R.N.; Cook, R.; Delgado, A.J.; Roulet, J.F.; Clark, W.A. Time-lasting ceramic stains and glaze: A toothbrush simulation study. J Esthet Restor Dent. 2020, 32, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Fiorin, L.; Oliveira, P.E.B.S.; Silva, A.O.d.; Faria, A.C.L.; Macedo, A.P.; Ribeiro, R.F.; Rodrigues, R.C.S. Wear Behavior of Monolithic Zirconia after Staining, Glazing, and Polishing Opposing Dental Restorative Materials: An In Vitro Study. Coatings 2023, 13, 466. [Google Scholar] [CrossRef]
- Yuan, J.C.C.; Barão, V.A.R.; Wee, A.G.; Alfaro, M.F.; Afshari, F.S.; Sukotjo, C. Effect of brushing and thermocycling on the shade and surface roughness of CAD-CAM ceramic restorations. The Journal of prosthetic dentistry 2018, 119, 1000–1006. [Google Scholar] [CrossRef]
- Kreve, S.; Dos Reis, A.C. Effect of surface properties of ceramic materials on bacterial adhesion: A systematic review. J Esthet Restor Dent. 2022, 34, 461–472. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, G.; Kaplan, H.B.; Kolter, R. Annual Rewiev of Microbiology. 2000, 54, 49–79. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.S.; Kranz, H.T.; Schneider, M.; Tietze, J.P.; Piwowarcyk, A.; Kuzius, T.; Arnold, W.; Naumova, E.A. Biofilm formation on different dental restorative materials in the oral cavity. BMC Oral Health 2020, 20, 162. [Google Scholar] [CrossRef]
- Song, F.; Koo, H.; Ren, D. Effects of material properties on bacterial adhesion and biofilm formation. J. Dent. Res. 2015, 94, 1027–1034. [Google Scholar] [CrossRef]
- Karygianni, L.; Jähnig, A.; Schienle, S.; Bernsmann, F.; Adolfsson, E.; Kohal, R.J.; Chevalier, J.; Hellwig, E.; Al-Ahmad, A. Initial Bacterial Adhesion on Different Yttria-Stabilized Tetragonal Zirconia Implant Surfaces in Vitro. Materials 2013, 6, 5659–5674. [Google Scholar] [CrossRef]
- Dal Piva, A.M.O.; Contreras, L.P.C.; Ribeiro, F.C.; Anami, L.C.; Camargo, S.E.A.; Jorge, A.O.C.; Bottino, M.A. Monolithic Ceramics: Effect of Finishing Techniques on Surface Properties, Bacterial Adhesion and Cell Viability. Oper Dent 2018, 43, 315–325. [Google Scholar] [CrossRef]
- de Carvalho, I.H.G.; da Silva, N.R.; Vila-Nova, T.E.L.; de Fatima, D.; de Almeida, L.; Veríssimo, A.H.; de Melo, R.M.; Zhang, Y.; de Assunção, E.; Souza, R.O. Effect of finishing/polishing techniques and aging on topography, C. albicans adherence, and flexural strength of ultra-translucent zirconia: An in situ study. Clin Oral Investig. 2022, 26, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Tsoi, J.K.-H.; Matinlinna, J.P.; Chen, Z. Influence of Grit-Blasting and Hydrofluoric Acid Etching Treatment on Surface Characteristics and Biofilm Formation on Zirconia. Coatings 2017, 7, 130. [Google Scholar] [CrossRef]
- Lee, D.H.; Mai, H.N.; Thant, P.P.; Hong, S.H.; Kim, J.; Jeong, S.M.; Lee, K.W. Effects of different surface finishing protocols for zirconia on surface roughness and bacterial biofilm formation. J Adv Prosthodont 2019, 11, 41–47. [Google Scholar] [CrossRef]

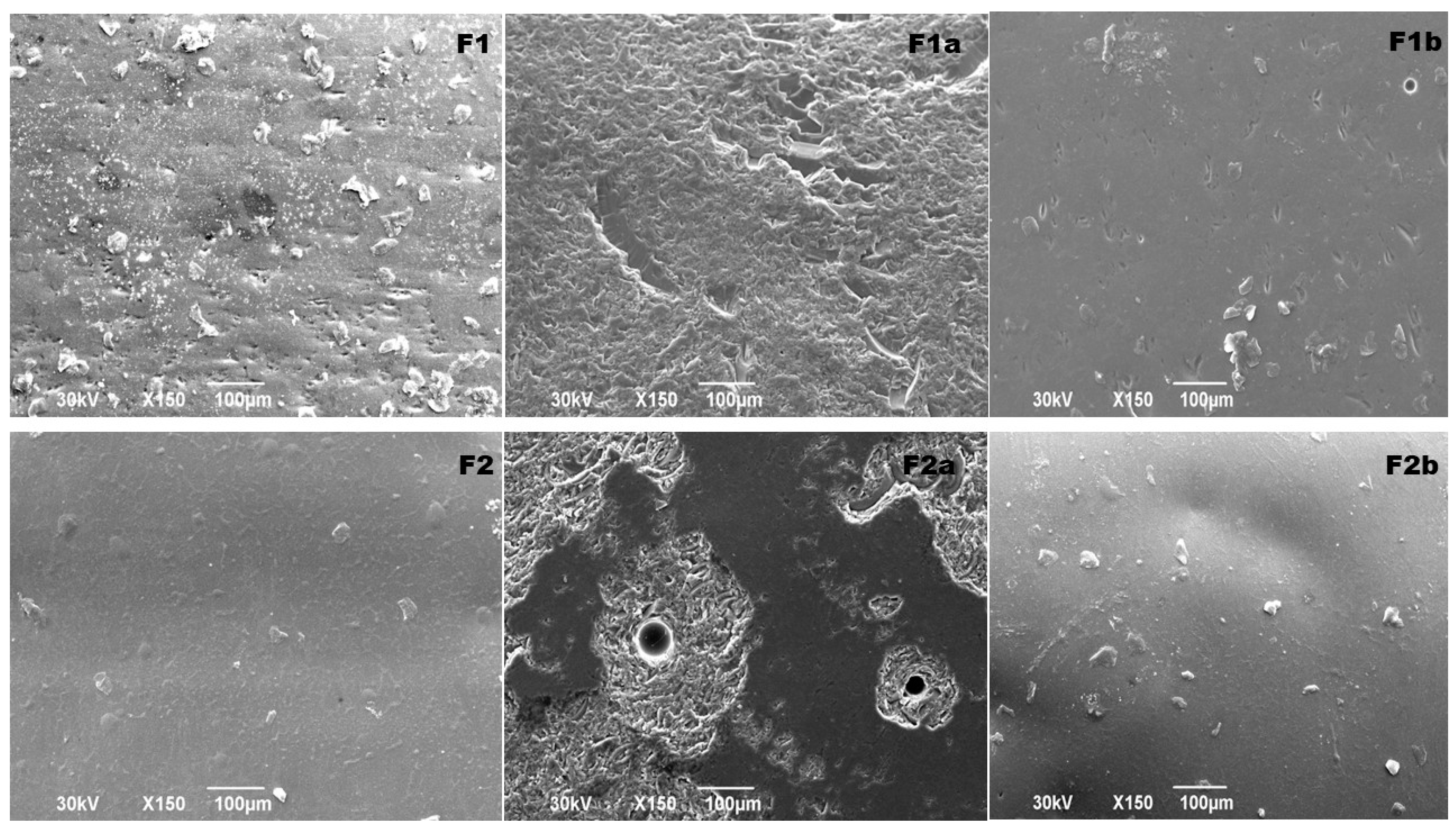
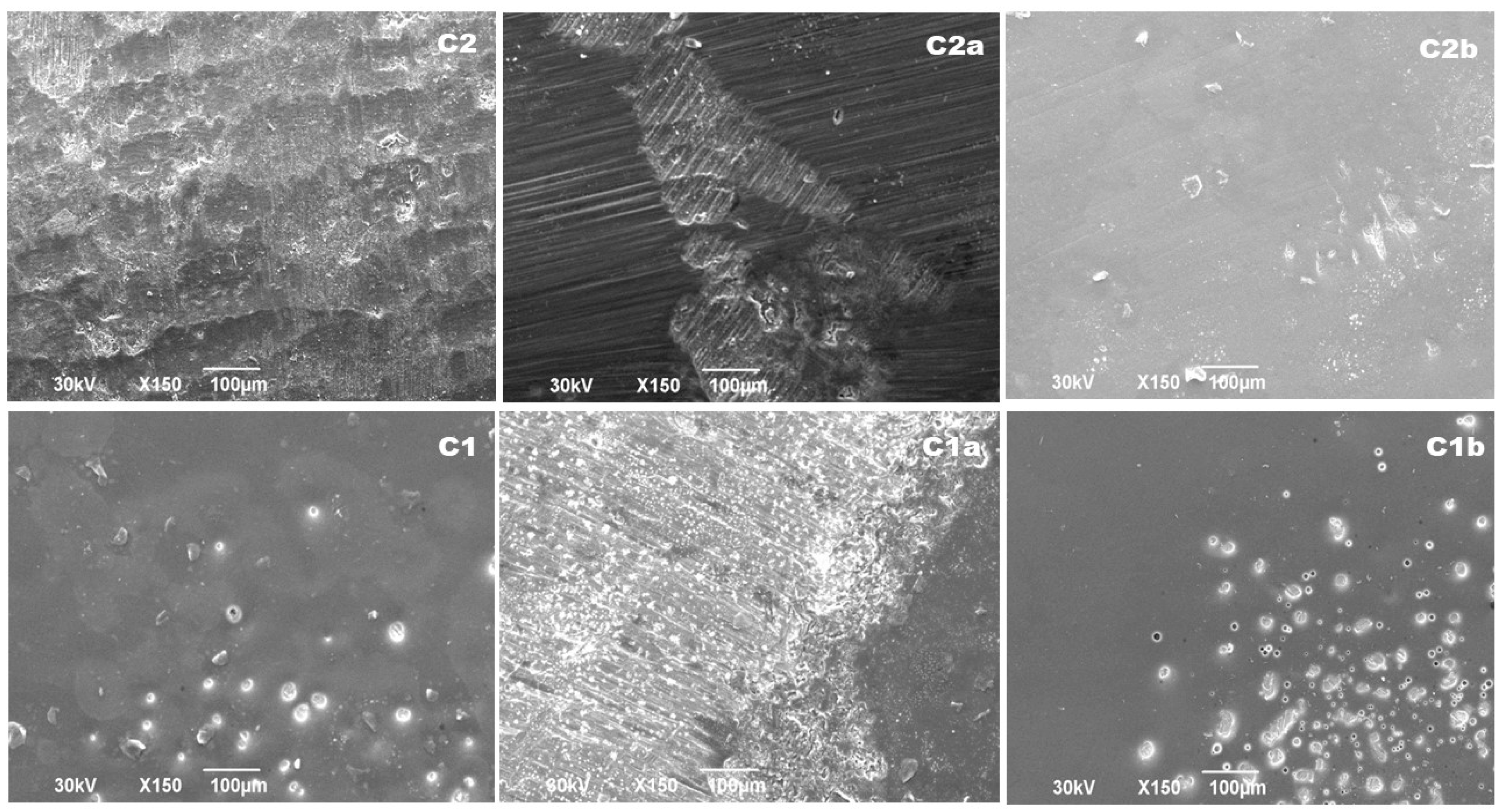
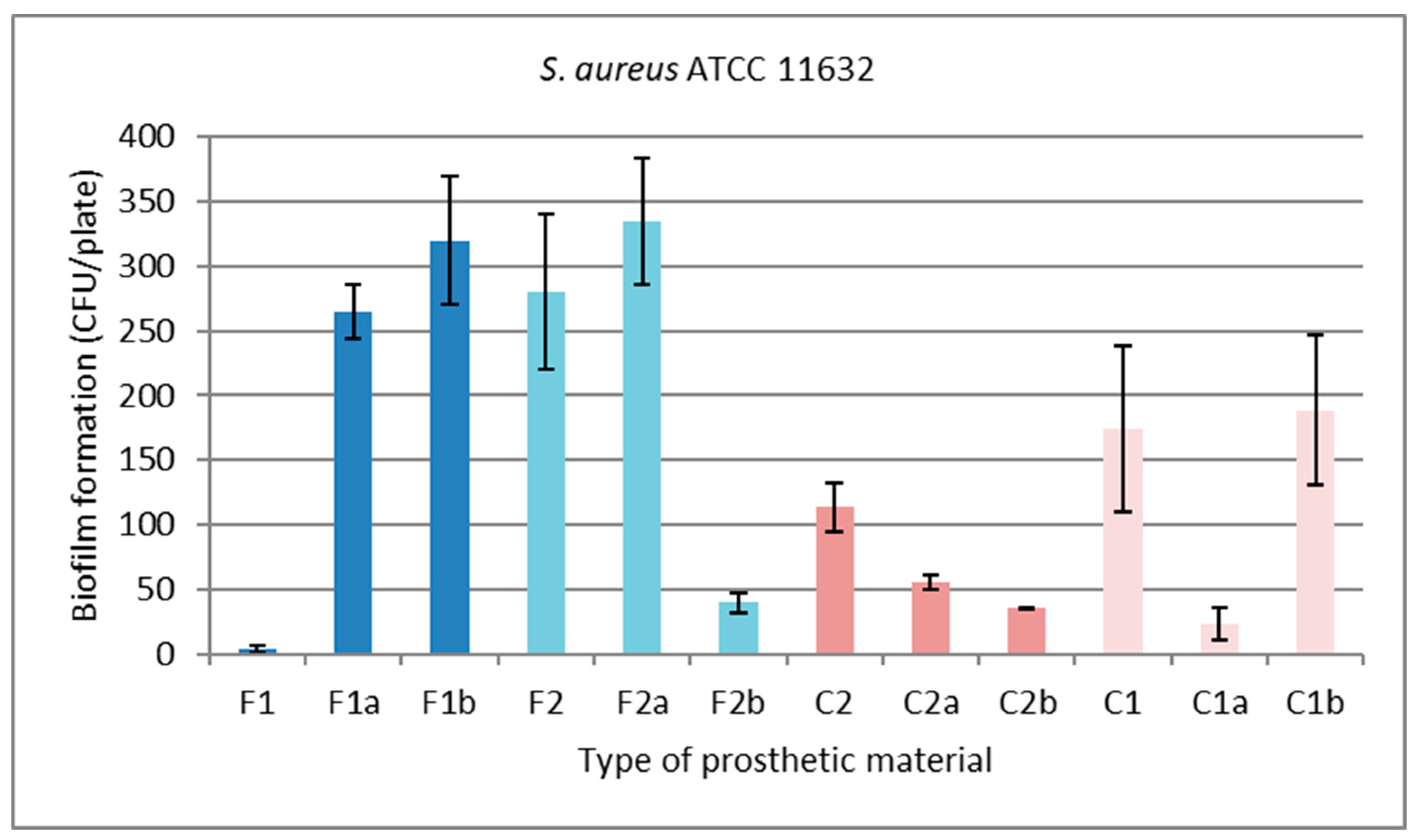
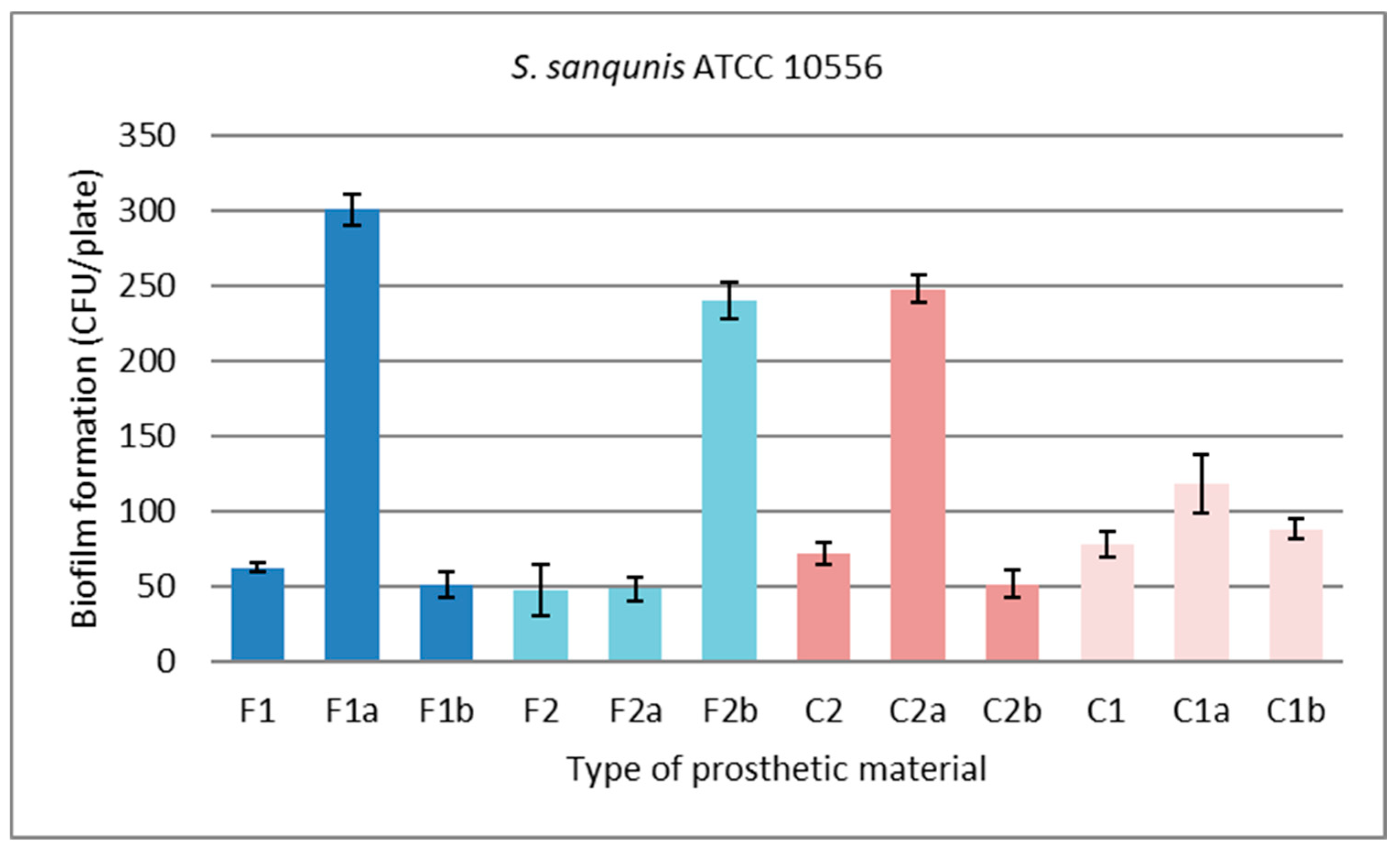
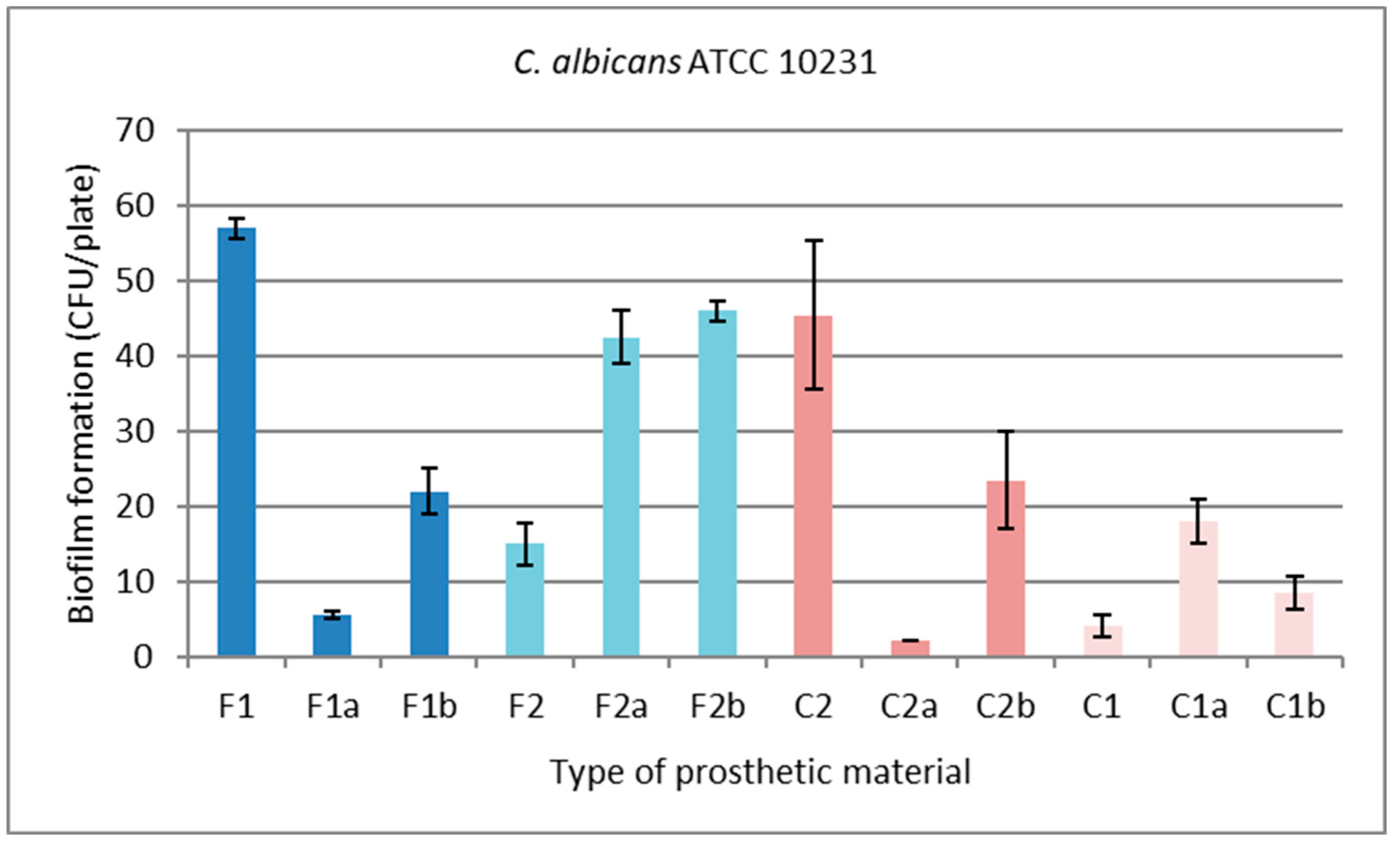
| Material Name | Material Code | |
|---|---|---|
| veneered zirconia | Polished | F1 |
| polished treated with ultrasonic scaling | F1a | |
| polished treated with a brushing | F1b | |
| Glazed | F2 | |
| glazed treated with ultrasonic scaling | F2a | |
| glazed treated with brushing | F2b | |
| CAD/CAM milled zirconia | Polished | C2 |
| polished treated with ultrasonic scaling | C2a | |
| polished treated with brushing | C2b | |
| Glazed | C1 | |
| glazed treated with ultrasonic scaling | C1a | |
| glazed treated with brushing | C1b | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





