1. Introduction
When ulcerative lesions appear in the oral cavity, there are a wide range of pathologies that could explain their origin.
According to sources cited by the NIH (National Cancer Institute), following data published in the SHEER (Surveillance, Epidemiology, and End Results Program Stat Fact Sheets), there were only 0.6 % of all oral cancer cases diagnosed in children under 20 years of age, with an updated incidence in 2008 of 0.24 cases per 100,0001. The occurrence, therefore, of a non-healing ulcerated lesion, after elimination of possible traumatic factors, may lead the clinician to be at a loss to venture an accurate clinical diagnosis.
However, the existence of a large lesion with a rapid evolution should lead us to consider the existence of a traumatic or injurious agent as the main cause. The natural evolution towards healing, in these cases, must present an evident cause/effect relationship, so that, once the causative agent is over, the injury should resolve or, failing that, improve substantially, in a maximum of two to three weeks. After that time, depending on the characteristics of the lesion, histological examination would be indicated to rule out malignancy.
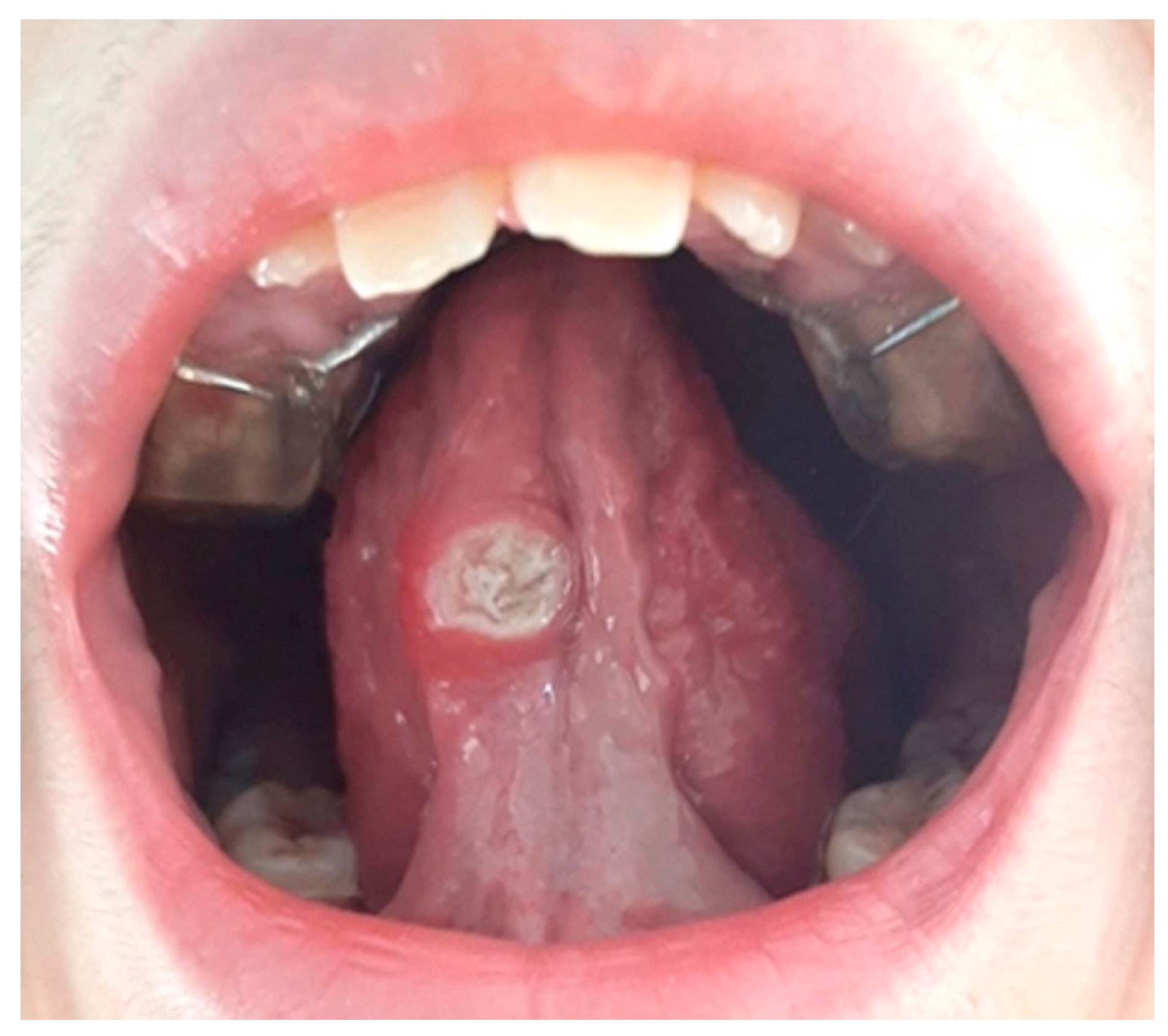
Undoubtedly, the time of evolution of the lesion makes it essential to carry out a biopsy in order to classify the pathology and establish the correct treatment. On the other hand, when we are faced with a large lesion (see Fig. 1), the question arises as to whether we should perform an excisional biopsy or take a representative sample and wait for a histopathological diagnosis.
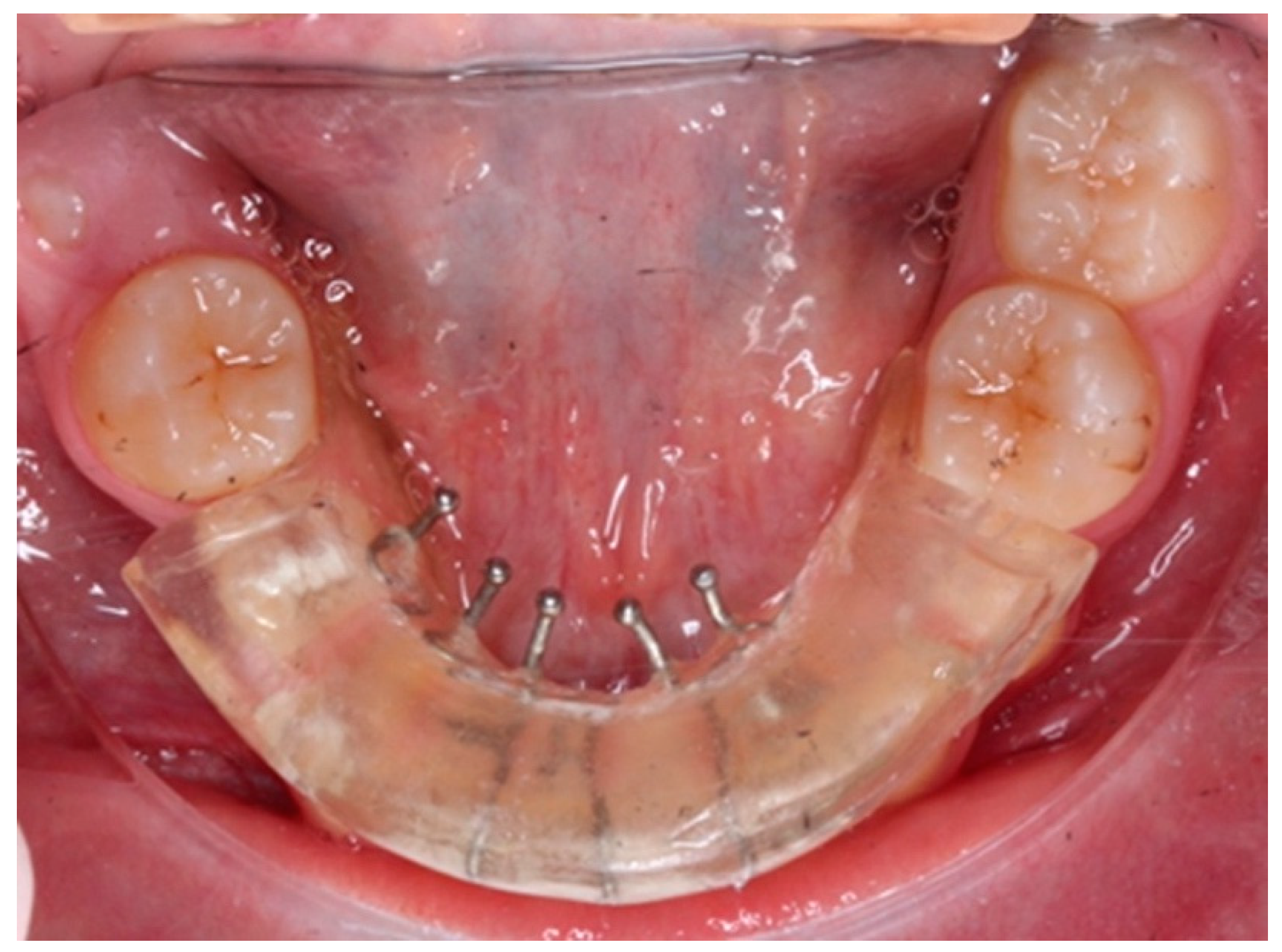
In the case described, our patient, a 13-year-old girl, was referred by her orthodontist after observing the appearance and rapid increase in size of a lesion located on the ventral aspect of the tongue, since after eliminating the most likely causal factor (lower removable acrylic orthodontic appliance with tongue thrusting device (see Fig. 2) and topical treatment with hyaluronic acid and chlorhexidine gel, there was no improvement. After review at the oral medicine clinic, treatment with clobetasol propionate in orobase was prescribed to try to reduce the lesion and, in a short period of time, perform a biopsy, taking into account the low probability of a malignant lesion due to the patient's age and the absence of cofactors. On the other hand, the painful symptoms reported by the patient were scarce, and the lesion appeared 14 months after the start of treatment with orthodontic appliances, and therefore, she was already used to wearing them. During this period, there was no appearance of lesions due to rubbing or ulceration since the fitting, which ruled out the diagnostic suspicion of an ulcer of purely traumatic origin. Due to the concern of the parents and being a family member of a healthcare worker, the mother presented the case to a maxillofacial colleague, who, to reassure her, decided to perform an excisional biopsy and histopathological study of the lesion immediately.
Various differential diagnoses were assessed as a basis for the usual deductive procedure practised in oral medicine consultations. The existence of a worldwide pandemic caused by sars-cov-2 and the continuous and new learning of its sequelae, as well as the side effects caused by the new vaccines, made it essential to investigate a viral cause as a possible origin of the lesion. Thus, different authors have reported the appearance of tongue ulcers as a consequence of the development of Sars-cov-2 2 infection. In a review study of 170 cases, Zarch et al3 found ulcerative lesions on the mucosa and tongue related in many cases to recurrent herpes simplex activation. Furthermore, Coll and Elmahgoub4 in a recent publication raised the interesting question of whether the appearance of oral lesions could be a predictive symptom for the early diagnosis of this disease. In this regard, patient's blood tests were requested, where no alteration of normal parameters was observed (including leukocyte series) and there was no previous history of sars-cov-2 infection.
2. Discussion: differential diagnosis
When faced with an ulcerated lesion in the oral cavity, there are a wide variety of probable causes. We can generally divide them into three groups according to their origin: 1. traumatic, 2. infectious, 3. systemic or autoimmune.
Below, we review the possible differential diagnoses of ulcerative lesions in children.
2.1. Ulcers of traumatic origin
This is a large group in which we find factitious lesions, lesions caused by chemical agents, drugs, mechanical trauma, parafunction, etc. They are characterised by the existence of a clear triggering factor, which is easily discovered during the clinical examination and anamnesis.
Amadori, Bardelini et al5 carried out a study with a sample of more than 6000 cases in an adolescent population and a follow-up of 6 years, where they reported ulcerative processes as the most frequent oral lesions, occupying the first two positions in frequency: firstly aphthous ulcers (19%), followed by ulcers of traumatic origin in 14.3% of cases. The traumatic cause, given the existence of orthodontic treatment and a removable functional orthopaedic appliance, was our first option for diagnostic suspicion, especially given the extreme rarity of other causes in this age group.
2.2. Ulcers of infectious origin
Multisystemic inflammatory syndrome in children (MIS-C) and Kawasaki disease associated with covid-19: Barros Nascimento et al6 conducted a systematic review of oral manifestations in children who developed a multisystemic inflammatory syndrome after sars-cov-2 infection, finding that these were similar to those of Kawasaki disease. These manifestations were described as erythema of the mucous membranes in the oropharynx, oral ulcers, dry lips, swollen and cracked lips and strawberry tongue. They also found that, in more severe cases, oral alterations can be accompanied by thrombotic processes and cardiac lesions (myocarditis, pericarditis...). MIS-C is a disease described after observation of paediatric patients infected with sars-cov-2. The clinical manifestations described and even the laboratory values are similar to Kawasaki disease, so it was initially considered as an incomplete presentation of Kawasaki disease. Findings in the oral cavity may precede systemic complications that could lead to seriousness and even death of patients, hence the importance of the dentist in early diagnosis. In these cases, sars-cov-2 infection must be present and there is usually an accompanying picture of fever, conjunctival injection and burning sensation and pain due to mucosal inflammation, among others. Our patient did not report any of the symptoms described, nor did she have a previous history of the disease.
Atypical presentation of tuberculosis: Deshpande et al7 describe the occurrence of extrapulmonary tuberculosis as a possible atypical manifestation of tuberculosis. Thus, they point to the occurrence of oral ulceration as the main orofacial manifestation of tuberculosis, the most common sites being the tongue and lip. The most typical extrapulmonary presentation, however, is the cervical lymph node lesion, which is almost exclusively found in children. Tuberculosis is not very prevalent in developed countries and oral presentation as a primary form is extremely rare.8
Hunter's chancre (syphilis): Syphilis is a typical infection of sexually promiscuous individuals, which may infrequently cause oral lesions. The chancre appears in the primary form of the disease as a papule that progresses to a large, painless, indurated ulcer on the tongue, lip and palate. Zhou et al9 in a systematic review found that the main manifestation of primary syphilis was a single ulcer in 91.7% of cases. However, these are infections that are not typical of childhood/adolescence.
Epstein-Barr virus (infectious mononucleosis): predominant infection in adolescence, without gender predominance. It mainly manifests in the isthmus of the fauces and is accompanied by petechiae on the palate. It may be accompanied by mouth ulcers, usually multiple.
Other viral causes: other manifestations such as Coxackie virus in younger children can cause hand-foot-and-mouth disease, with a manifestation similar to herpetic primoinfection, varicella zoster virus or herpangina (in this case in the posterior pharyngeal and tonsillar area) where there are vesicular lesions and superficial ulcers. In any case, they do not manifest themselves as a single lesion and are usually accompanied by other symptoms such as fever, general malaise, etc.
2.3. Systemic or autoimmune origin
Relapsing aphthous stomatitis (RAS): relapsing aphthous stomatitis (RAS) is a disease characterised by the appearance of painful recurrent ulcers on mobile and non-keratinised mucosa. It is more prevalent in school-age children and is related to genetic factors, hormonal alterations and nutritional deficiencies.10 Our patient presented with a lesion on the mobile mucosa of the ventral side of the tongue and did not report continuous pain, but rather discomfort due to rubbing against food. It was also a single, large lesion that could correspond to the larger forms of RAS. In these forms, ulcers 1-3 cm in diameter are present with a longer healing period and may leave a scar after healing. The most frequent locations, however, are the labial mucosa, the soft palate and the tonsillar fauces, which does not correspond to our case.
Ulcers as a manifestation of acute myeloid leukaemia in children: from an epidemiological point of view, 80% of myeloid and acute leukaemias occur in adults and rarely in children (where lymphoblastic forms are more frequent). However, leukaemia is the most common paediatric cancer in children under 15 years of age. Oral manifestations are often the way to find a serious occult systemic process. In such cases, petechiae, spontaneous bleeding, ulcerative lesions, gingival enlargement, infections, haemorrhagic blisters on the tongue and cracked lips are frequent findings. Mucosal ulceration appears in 53% of cases and is included in the group of initial lesions of leukaemia.11 The absence of neutropenia in blood tests and other findings of interest, as well as the fact that it is a single lesion and not accompanied by other clinical signs, rules out this diagnosis.
Ulcers associated with Fanconi's anaemia: Kartal et al12 describe the case of a 15-year-old patient who presented with a lesion on the tongue, with a diagnosis of suspected oral carcinoma, showing clinically as a long-standing lesion with an ulcerated appearance. Fanconi's anaemia is a hereditary disorder characterised by progressive aplastic anaemia, multiple congenital anomalies and which may show as its first manifestation the development of cancer, even before the haematological alterations appear. The authors stress the importance of assessing this diagnosis of suspicion in the presence of ulcerated lesions that do not heal within a reasonable period of time and the follow-up of patients diagnosed with this type of anaemia.
Oral manifestations of coeliac disease: although the prevalence of gluten intolerance disease is low (0.5-1%), the most recent studies report a substantial increase in the number of cases, a consequence of a less controlled existence of silent forms. Although the possible intestinal alterations caused by the disease are well known, there are a series of frequent oral manifestations that are less well known, but no less important. At the soft tissue level, children with coeliac disease present more frequently with cases of RAS which, if present, could serve as suspicion for the diagnosis of atypical or silent coeliac disease. A review by Macho et al13 reported up to 3 times higher rates of RAS in coeliac patients compared to control groups. Other soft tissue manifestations were geographic tongue, atrophic glossitis, angular cheilitis and burning mouth.
Behçet's syndrome: a multisystem disorder causing vasculitis that can affect almost all vascularised areas of the body and is characterised by oral ulcers and genital ulcers. It can also be accompanied by arthralgias, ocular, neurological, dermal or digestive disorders. Oral ulcers, which are usually the main manifestation of the disease, are recurrent, of varying size and location and may be related to herpes simplex in their aetiopathogenesis. The typical patient is usually male, aged 25-35 years.14,15
Crohn's disease is an inflammatory disease that presents with periods of activity and remission and can affect any part of the gastrointestinal tract, from the mouth to the anus, which makes the symptoms very varied (abdominal pain, fever, diarrhoea.16 Extraintestinal manifestations are classified as those occurring at the oral level, where the appearance of ulcers stands out (20-50% of patients). As we have seen in previous pathologies, the appearance of ulcerated lesions may precede the onset of an outbreak. They may be due to the inflammation caused by the disease itself, be the result of nutritional deficiencies due to digestive disorders (deficiencies of B-12, Zn, which generally appear on the tongue) or as a result of the medication itself. Patients also suffer from dry mouth and acidosis due to vomiting, favouring the appearance of caries, etc. Ulcerative lesions can be multiform. The onset of the disease is characteristic of the 2nd-3rd decade, although it can occur at paediatric ages. In this case, intestinal disturbances, fatigue and weight loss, accompanying the oral manifestations, may be useful for an early diagnosis of the disease.17
Other skin or dermatological disorders: epidermolysis bullosa is a rare hereditary disorder that causes a fragile cutaneous basement membrane, resulting in blisters, which may ulcerate and whose diagnosis is mainly based on family history. It is rarely located in the mouth. Others such as erythema multiforme, lupus erythematosus (the systemic form may produce oral ulcerations), or pemphigus or pemphigoid lesions are typical of adults and have more specific clinical manifestations.
3. Results
After histopathological study, the lesion was diagnosed as Traumatic Eosinophilic Granuloma of the Oral Mucosa (TUGSE). This is a rare pathology characterised by the appearance of a single ulcerated lesion that may be asymptomatic and predominantly located on the tongue.18 The appearance of the lesion may be confused with a squamous cell carcinoma, which causes concern for the patient and family members. The lesions are self-limiting, but may take months or up to a year to disappear, which complicates diagnosis and decision-making. This type of lesion was described as its own entity by Saphiro and Juhlin19 in 1970, and when it occurs in infants, it is comparable to the pathology catalogued as Riga-Fede disease and characterised by the presence of traumatic ulcers resulting from the appearance of connatal or early erupting teeth. It usually appears from the 5th decade onwards, which leads to a greater suspicion of carcinoma than when it is a lesion in children 20. In the different studies, no consensus has been found on the existence of a gender predilection21,22,23.
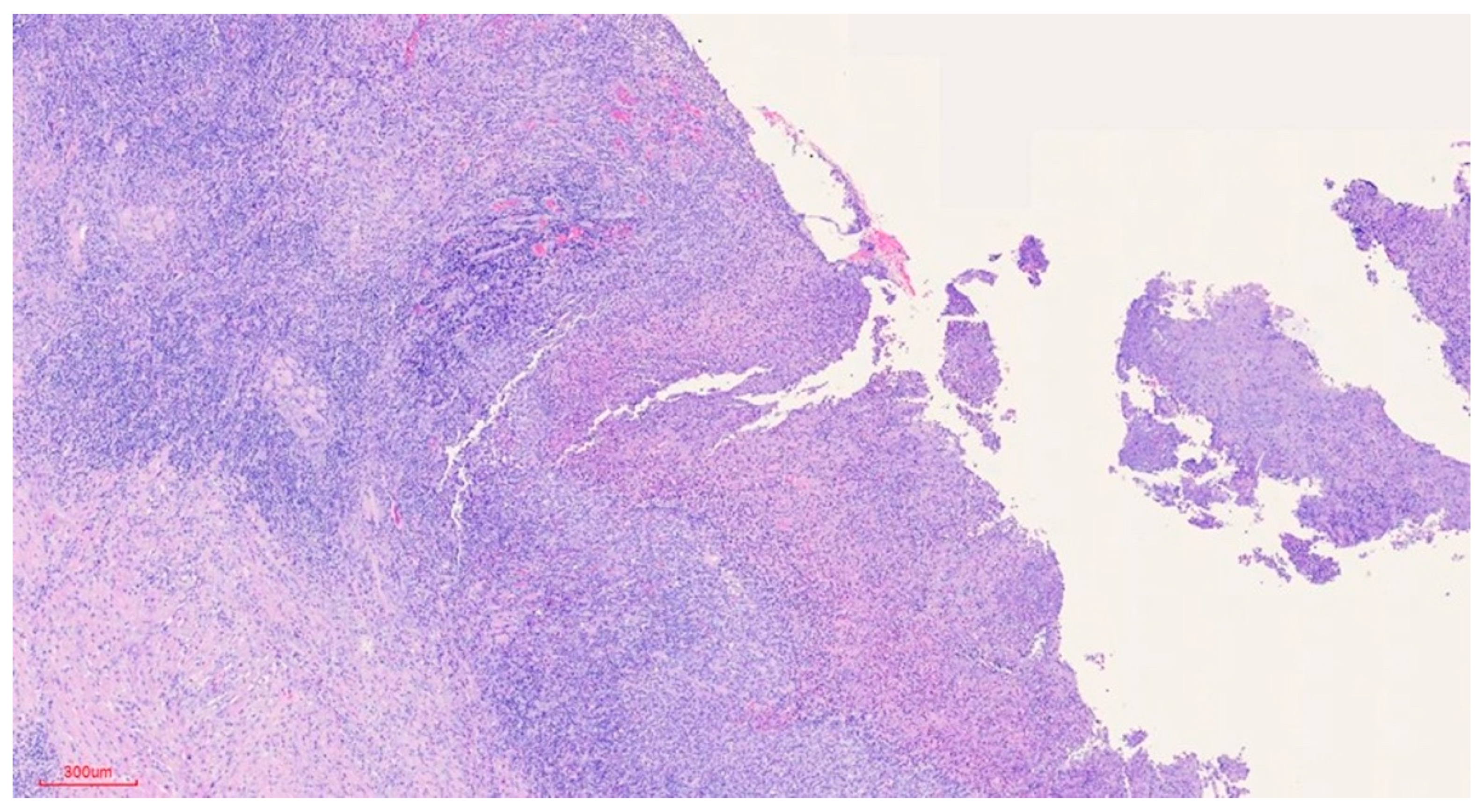
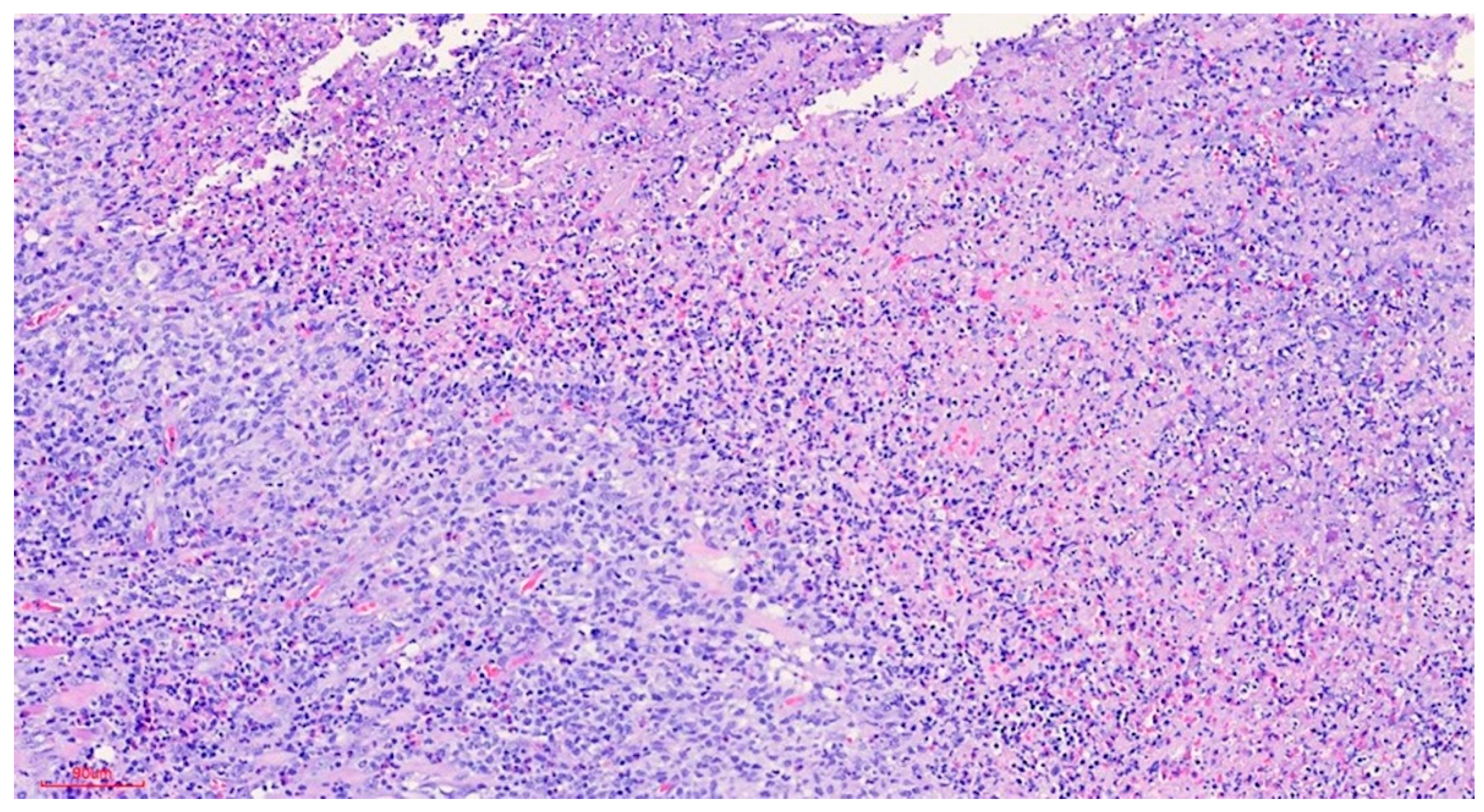
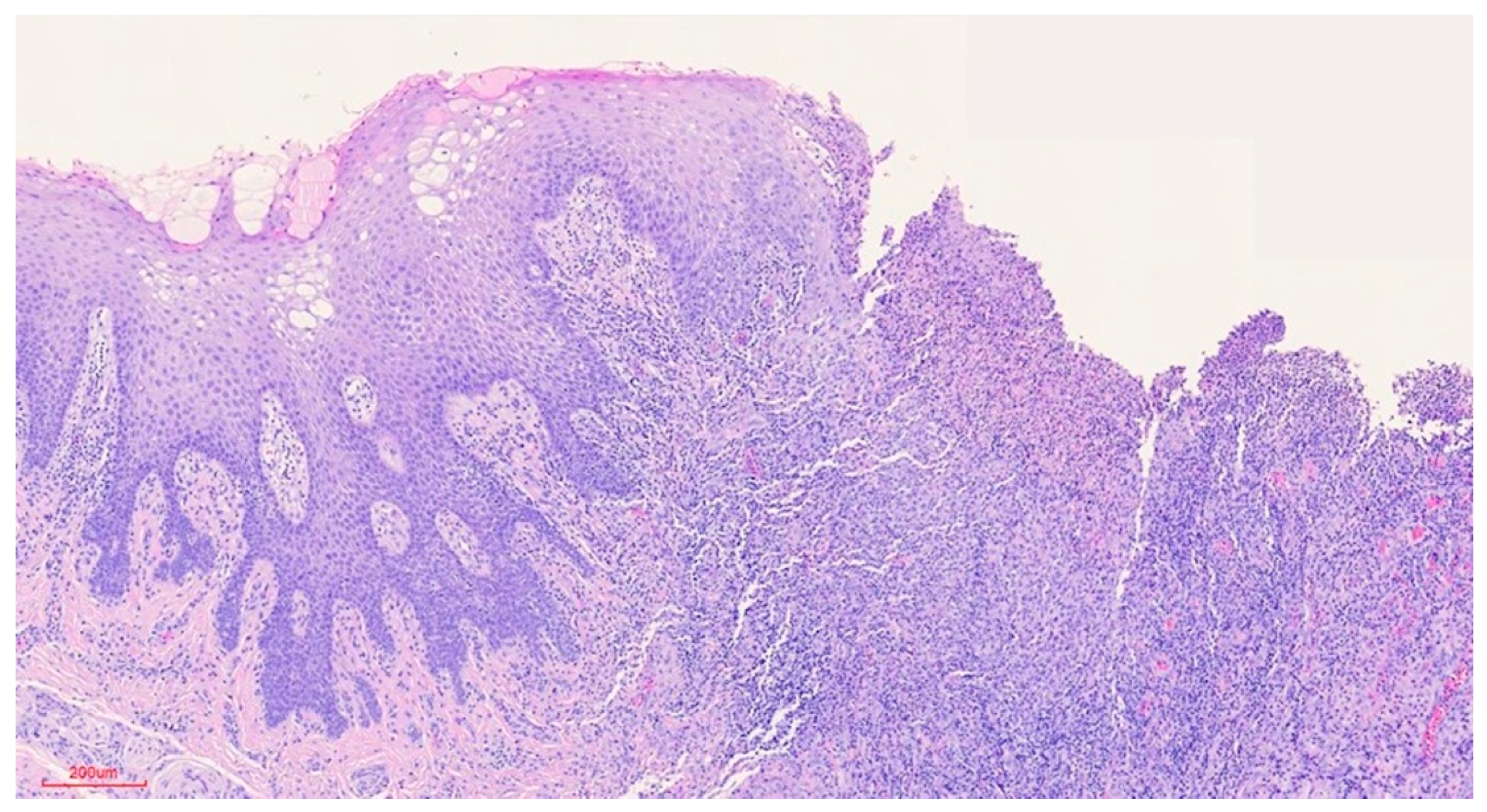
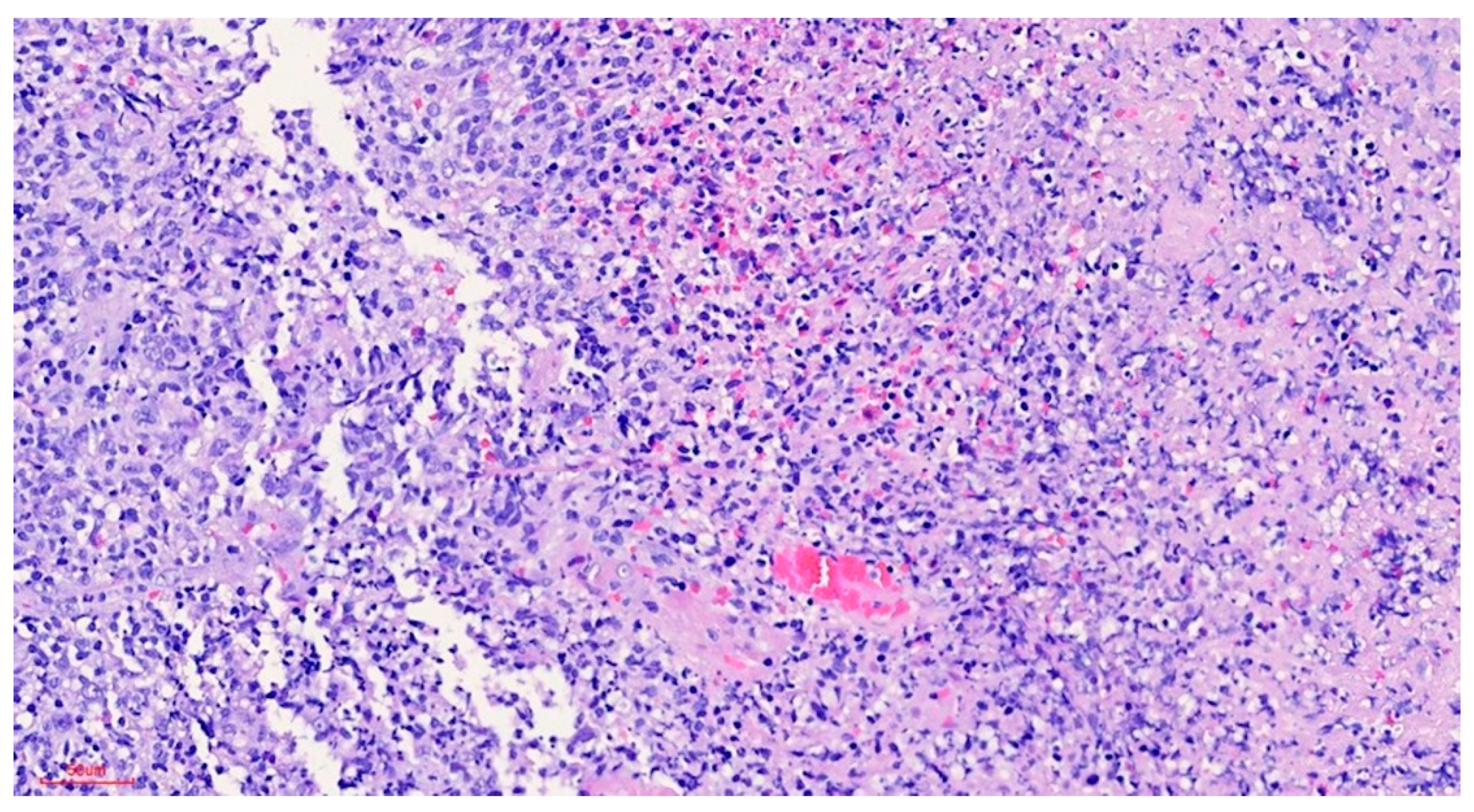
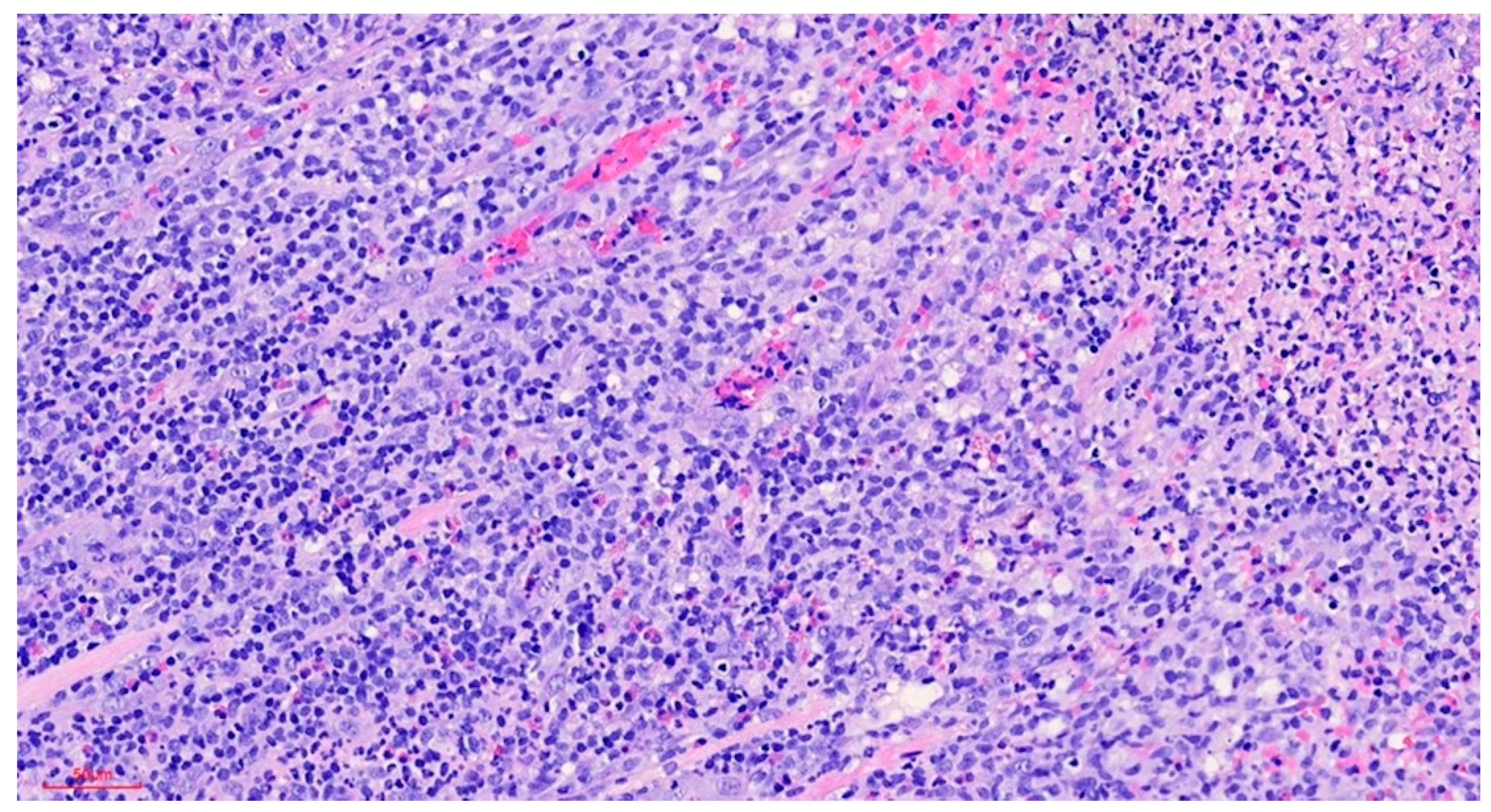
Clinically, the lesion usually has a raised hyperkeratotic border and microscopically it is characterised by a dense infiltrate of T and B lymphocytes, macrophages and mainly eosinophils24 and a tendency to penetrate the underlying muscle.
3.1. Treatment and evolution
Despite the current versatility of diagnostic methods for precancerous or potentially malignant lesions, which include the search for salivary biomarkers, exfoliative cytology studies, liquid cytology25, etc., the classic biopsy of the lesion and its histopathological study are still today the safest and most effective diagnostic protocol.26 Topical treatment with corticosteroids (clobetasol propionate) was considered to try to reduce the lesion, prior to biopsy. However, the decision of his maxillofacial surgeon to perform an excisional biopsy and subsequent histological study, seemed to us to be an appropriate approach. The surgery was performed without complications and the wound was closed with resorbable suture.
The histopathological study was resolved as follows:
a) Macroscopic description: 1.3x2 cm round fragment with 1.2 cm ulcer with raised edges and granular central area. Two samples are submitted, one from the central area and one from the periphery.
b) Microscopic findings: infiltrative ulcerative lesion covered with necrotic-fibrinoid material and consisting of an abundant polymorphous inflammatory infiltrate extending in depth around the seromucinous glands and dissociating the muscle fibres. It consists of cells of histiocytic type, lymphocytes, polynuclear neutrophils and abundant eosinophils. PAS and Grocott stains show no fungal elements. No signs of malignancy are observed (see Figures 4–9).
c) Histopathological diagnosis: histological aspect compatible with traumatic ulcerative granuloma with stromal eosinophilia.
The patient was examined one month after surgery and an area remained inflamed around the resorbable stitches, but showed good healing of the tissues. The patient showed no pain and no decrease in normal tongue function. The images one week later show complete resorption of the suture and an evident improvement of the area that remained swollen (fig.8 and 9).
| Origin |
Pathology |
Age range (typical) |
Location |
Description |
Associated lesions/ clinical or laboratory findings. |
| Traumatic |
Factitious lesions of physical, chemical or mechanical origin. |
Any age |
Areas of friction or trauma. |
Appearance of ulcers, petechiae, hyperkeratosis or soft tumours. |
Search for cause/effect relationship. |
| Yatrogenesis |
frequent in adolescence |
Characteristics of jugal mucous membranes, lip or tongue. |
Parafunctional habits. |
| Infectious |
Extrapulmonary manifestation of tuberculosis. |
Children living with infected adults. |
Tongue and lip |
Ulcer with irregular borders, similar to SCC. |
Cervical nodes. Koch's bacillus. |
| Syphilitic chancre |
Rare in children. Sexually transmitted. |
Any location. Rare isolated lesions in the mouth. |
Syphilitic chancre |
Mucocutaneous lesions/Treponema Pallidum serology positive. |
| Epstein-Bar-associated lesion (EBV). |
Between 10-20 years old. |
Tonsillar pillars and uvula. |
Multiple ulcers |
Presence of EBV. |
| Kawasaki disease, or multi-systemic covid-19 syndrome (MIS-C). |
Children 3-12 years old (average 8). |
Mainly the tongue |
Raspberry tongue. |
Sars-COV-2 infection. |
| |
RAS (major form) |
School-age children. |
Non-keratinised mobile mucous membranes. |
Ulcers 1-3 cm in diameter (larger). |
Possible gluten intolerance. Vitamin deficiencies |
| Systemic/autoimmune |
Beçhet syndrome. |
Average age 25-30 years. Paediatric forms 12 years. |
Any location |
Recurrent oral and genital ulcers. |
Ulcers on other mucous membranes (genital), eye inflammation. |
| |
Acute Myeloblastic Leukaemia. |
Rare infantile form. Average age 68 years. |
Depending on the alterations. |
Ulcers due to leukaemic cell thrombosis, decreased immune response. |
Anaemia, gingivorrhage, petechiae and other vascular alterations. Cervical lymphadenopathy, candidiasis or opportunistic infections. |
| |
Fanconi anaemia. |
4-14 years (average 8 years). |
Any location |
Single or multiple ulvers. |
Congenital malformations (short stature, alterations of the thumb or radius, kidney problems), areas of hyperpigmentation.High concentrations of glucose in urine (normal in blood). Increased phosphate and amino acid concentrations in urine. |
| |
Celiac disease. |
Any age |
Any location |
Single or multiple lesions (similar to RAS) |
Gluten intolerance. Chronic diarrhoea, nausea, vomiting and abdominal swelling. Increased risk of enamel hypoplasia. |
| |
Chron's disease. |
Any age. Young people 3rd-4th decade, or from the 6th decade onwards. |
Any location |
Single or multiple lesions of direct cause or secondary to deficits or medication. |
Diarrhoea, weight loss, bloating and abdominal pain (right side) Dx colonoscopy. Halitosis, reflux caries... |
| |
Nutritional deficits. |
Any age |
Oral mucosa (preferably lips). |
Single or multiple lesions |
Deficiencies of Vitamins C and B group (B12), Zn, Fe++ or folic acid. |
4. Conclusions
The appearance of a single, large ulcerated lesion that does not heal once possible traumatic factors have been controlled can cause concern for the dentist, as well as for the patient and his or her relatives. There are numerous possible causes, which makes the diagnosis more complex. However, once trauma is ruled out as the main cause, possible infectious processes should be investigated, mainly based on their frequency according to the patient's age. Then a systemic cause should be found, where the ulcerated lesion is a primary or premonitory manifestation of another disease. Laboratory studies, however, and a correct anamnesis help us to rule out the presence of a systemic disease, in the absence of alterations such as nutritional deficiencies, alterations in the formal elements of the blood (anaemia, leukopenia, increased lymphocytes, etc.). Finally, an anatomopathological study with excisional biopsy proved to be the most successful therapeutic option with a favourable evolution of the area without functional or aesthetic complications.
References
- Berstein L, Gurney JG: Carcinomas and other malignant epithelial neoplasms. In: Ries LA, Smith MA, Gurney JG, et al., eds.: Cancer incidence and survival among children and adolescents: United States SEER Program 1975-1995. National Cancer Institute, SEER Program, 1999. NIH Pub.No. 99-4649, Chapter 11, pp 139-148. Last accessed June 08, 2020.
- Rusu LC, Ardelean LC, Tigmeanu CV, Matichescu A, Sauciur I, Bratu EA. COVID-19 and Its Repercussions on Oral Health: A Review. Medicina (Kaunas). 2021, 57, 1189.
- Zarch RE, Hosseinzadeh P. COVID-19 from the perspective of dentists: A case report and brief review of more than 170 cases. Dermatol Ther. 2021, 34, 4717.
- Coll Y, Elmahgoub F. Could dentists be the first to diagnose COVID-19 due to oral manifestations?. Evid Based Dent. 2021, 22.
- Amadori F, Bardellini E, Conti G, Majorana A. Oral mucosal lesions in teenagers: a cross-sectional study. Ital J Pediatr. 2017, 43, 50.
- Nascimento RB, Araujo NS, Silva JC, Xavier FCA. Oral manifestations of multisystemic inflammatory syndrome in children (MIS-C) and Kawasaki disease associated to COVID-19: A systematic review. Spec Care Dentist. 2021, 18, 10.
- Deshpande A, Gupta P, A Reddy VS, Reddy R. Atypical presentation of tuberculosis. J Oral Maxillofac Pathol. 2020, 24, 404.
- Mignogna MD, Muzio LL, Favia G, Ruoppo E, Sammartino G, Zarrelli C, et al. Tuberculosis oral: una evaluación clínica de 42 casos. Dis. Oral. 2000, 6, 25–30.
- Zhou X, Wu MZ, Jiang TT, Chen XS. Manifestaciones orales de la sífilis temprana en adultos: una revisión sistemática de los informes de casos y series. Sex Transm Dis. 2021, 48.
- Chiang CP, Yu-Fong Chang J, Wang YP, Wu YH, Wu YC, Sun A.J Recurrent aphthous stomatitis: Etiology, serum autoantibodies, anemia, hematinic deficiencies, and management. Formos Med Assoc. 2019, 118, 1279–1289.
- Cammarata-Scalisi F, Girardi K, Strocchio L, Merli P, Garret-Bernardin A, Galeotti A, Magliarditi F, Inserra A, Callea M. Oral Manifestations and Complications in Childhood Acute Myeloid Leukemia. Cammarata-Scalisi, Cancers, 2020, 12, 1634.
- Kartal I, Dağdemir A, Elli M, Yıldız L, Yılmaz A. A Skeptical Approach to the Management of Persistent Oral Ulceration in a Child. Case Rep Pediatr. 2018, 2018, 2681723.
- Macho VMP, Coelho AS, Veloso E Silva DM, de Andrade DJC. Oral Manifestations in Pediatric Patients with Coeliac Disease: A Review Article. Open Dent J. 2017, 11, 539–545.
- López-García S, Vizán-Caravaca JR, García-Castro JM. Behcet síndrome. Aten Primaria. 2020, 52, 275–276.
- Scherrer MAR, Rocha VB, Garcia LC. Behcet's disease: review with emphasis on dermatological aspects. An Bras Dermatol. 2017, 92, 452–464.
- Townsend CM, Nguyen TM, Cepek J, Abbass M, Parker CE, McDonald JK, Khanna R, Jairath V, Feagan BG. Adalimumab para el mantenimiento de la remisión en la enfermedad de Crohn. Base de Datos Cochrane de Revisiones Sistemáticas 2020, número 5. Arte. Número: CD012877.
- Stavropoulos F, Katz J, Guelmann M, Bimstein E. Oral ulcerations as a sign of Crohn's disease in a pediatric patient: a case report. Pediatr Dent. Jul-Aug 2004, 26, 355–358.
- Benítez B, Mülli J, Tzankov A, Kunz C. Granuloma ulceroso traumático con eosinofilia estromal: informe de caso clínico, revisión de la literatura y diagnóstico diferencial. Mundo J Surg Oncol. 2019, 17, 184.
- Lakkam BD, Astekar M, Alam S, Saleem A. Granuloma ulcerativo traumático con eosinofilia estromal: un rompecabezas. J Oral Patol Maxilofacial. 2021, 8, 2214–2216.
- Hannan TA, Umer M, Syed L, Anis-Alavi. MA A case report of traumatic ulcerative granuloma with stromal eosinophilia (TUGSE) in a 21-year-old. Clin Case Rep. 2020, 8, 2214–2216.
- Segura S., Pujol RM. Úlcera eosinofílica de la mucosa oral: ¿una entidad diferenciada o un patrón reactivo inespecífico? Enfermedades orales 2008, 14, 287–295.
- Mayordomo JN, Kobayashi TT. Granuloma ulcerativo traumático con eosinofilia estromal: una lesión benigna de apariencia maligna. Cutis 2017, 100, 28–31.
- Hirshberg A, Amariglio N, Akrish S, Yahalom R, Rosenbaum H, Okon E, et al. Granuloma ulcerativo traumático con eosinofilia estromal: una lesión reactiva de la mucosa oral. Am J Clin Pathol. 2006, 126, 522–9.
- Sethi A, Banga A, Raja R, Raina R. Granuloma ulcerativo traumático con eosinofilia estromal. Indian J Dent Res. 2020, 31, 636–639.
- Osaka R, Hayashi K, Onda T, Shibahara T, Matsuzaka K. Evaluation of Liquid Based Cytology for Tongue Squamous Cell Carcinoma: Comparison with Conventional Cytology. Bull Tokyo Dent Coll. 2019, 60, 29–37.
- Walsh T, Macey R, Kerr AR, Lingen MW, Ogden GR, Warnakulasuriya S. Diagnostic tests for oral cancer and potentially malignant disorders in patients presenting with clinically evident lesions. Cochrane Database of Systematic Reviews 2021, Issue 7. Art. No.: CD010276.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).