Submitted:
27 June 2023
Posted:
27 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
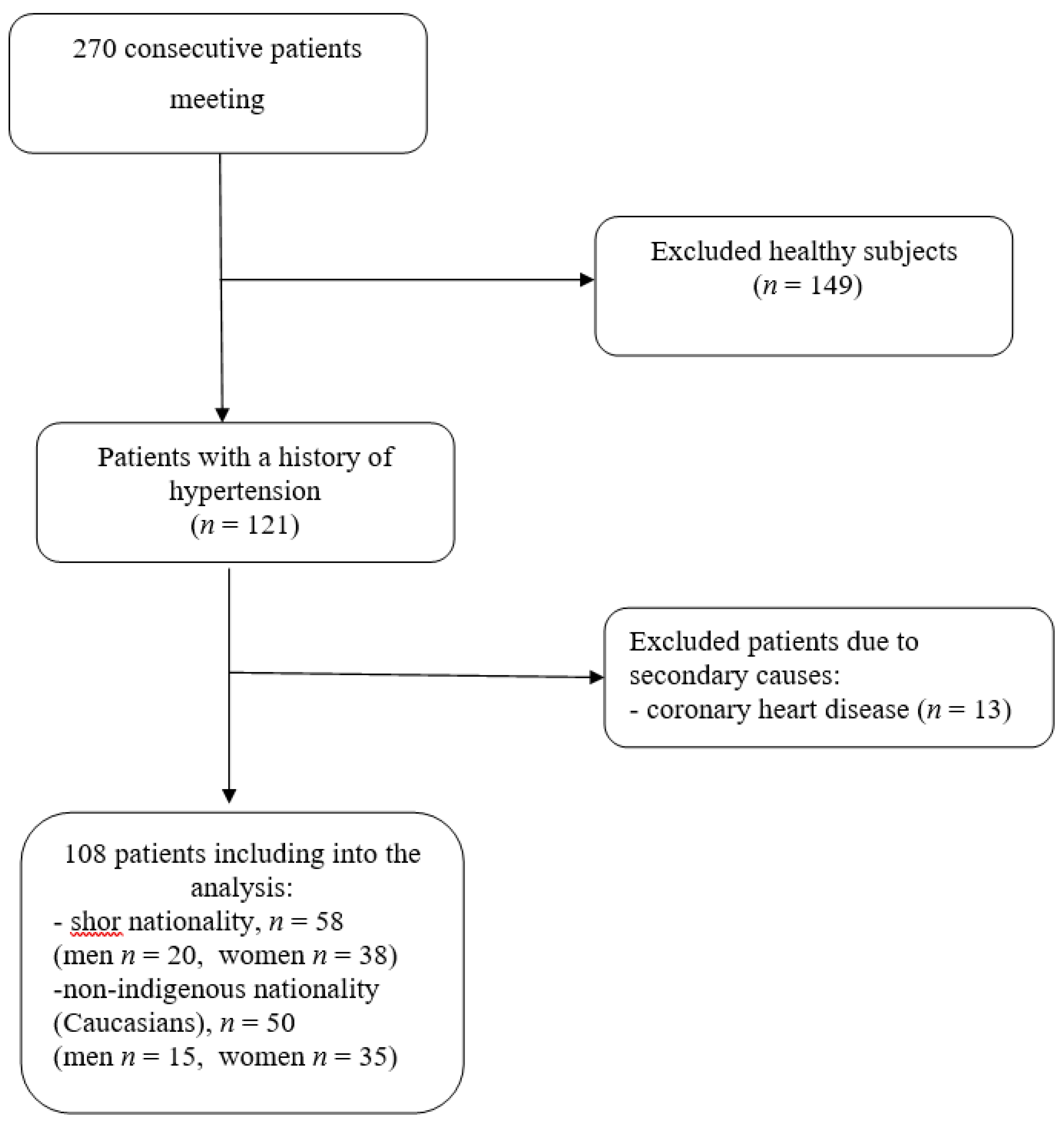
2.1. Patients
2.2. Echocardiography
2.3. Statistical analysis
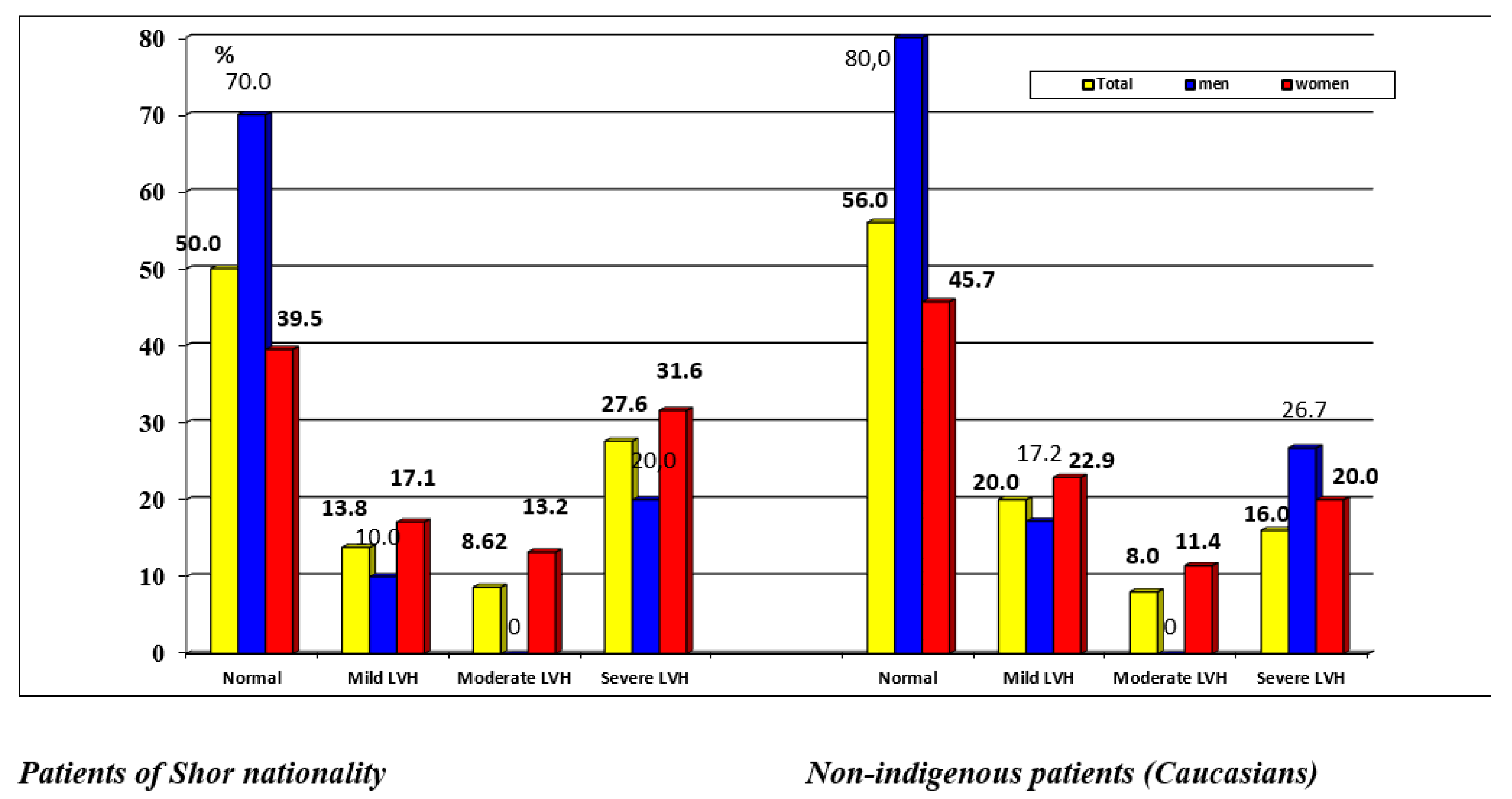
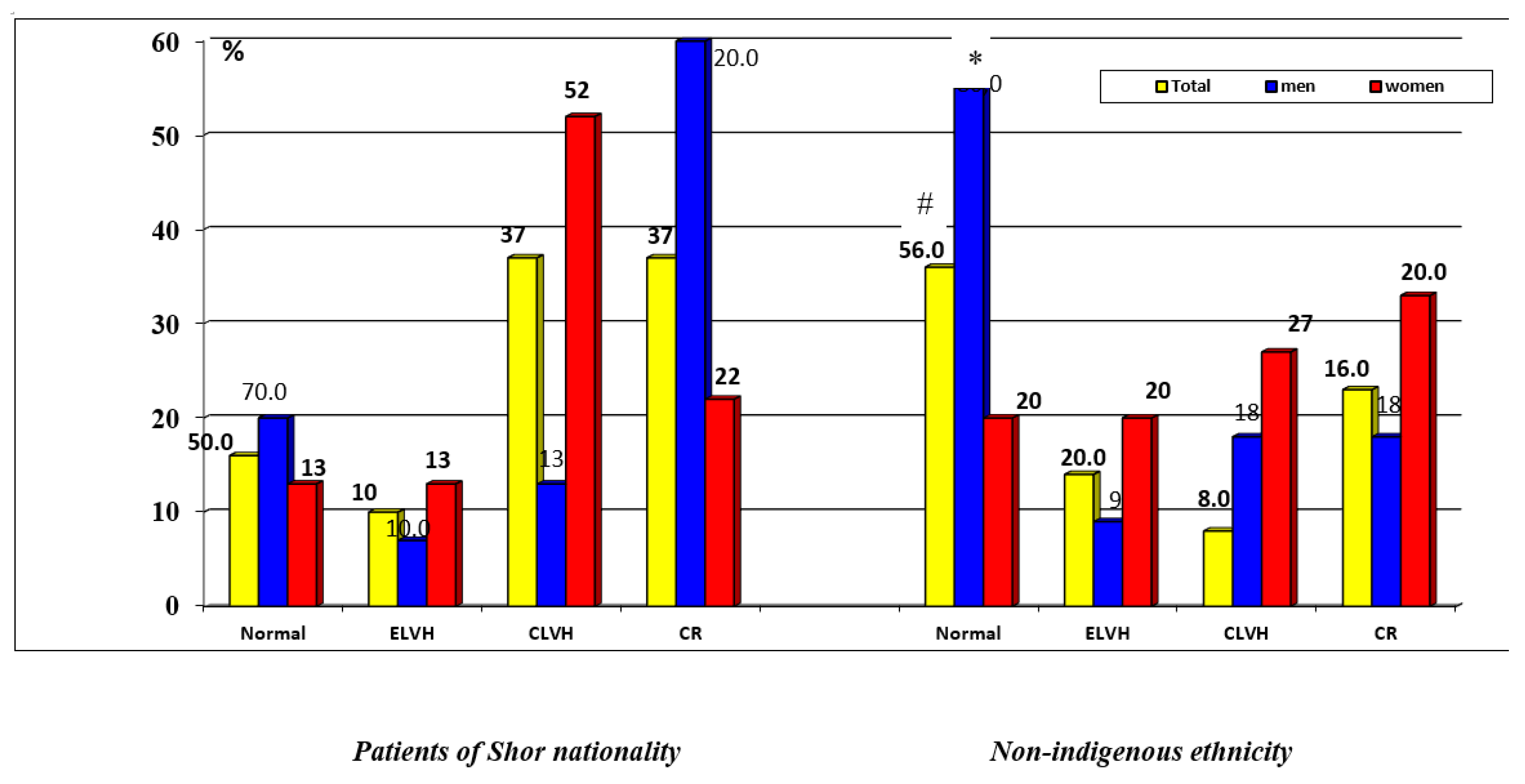
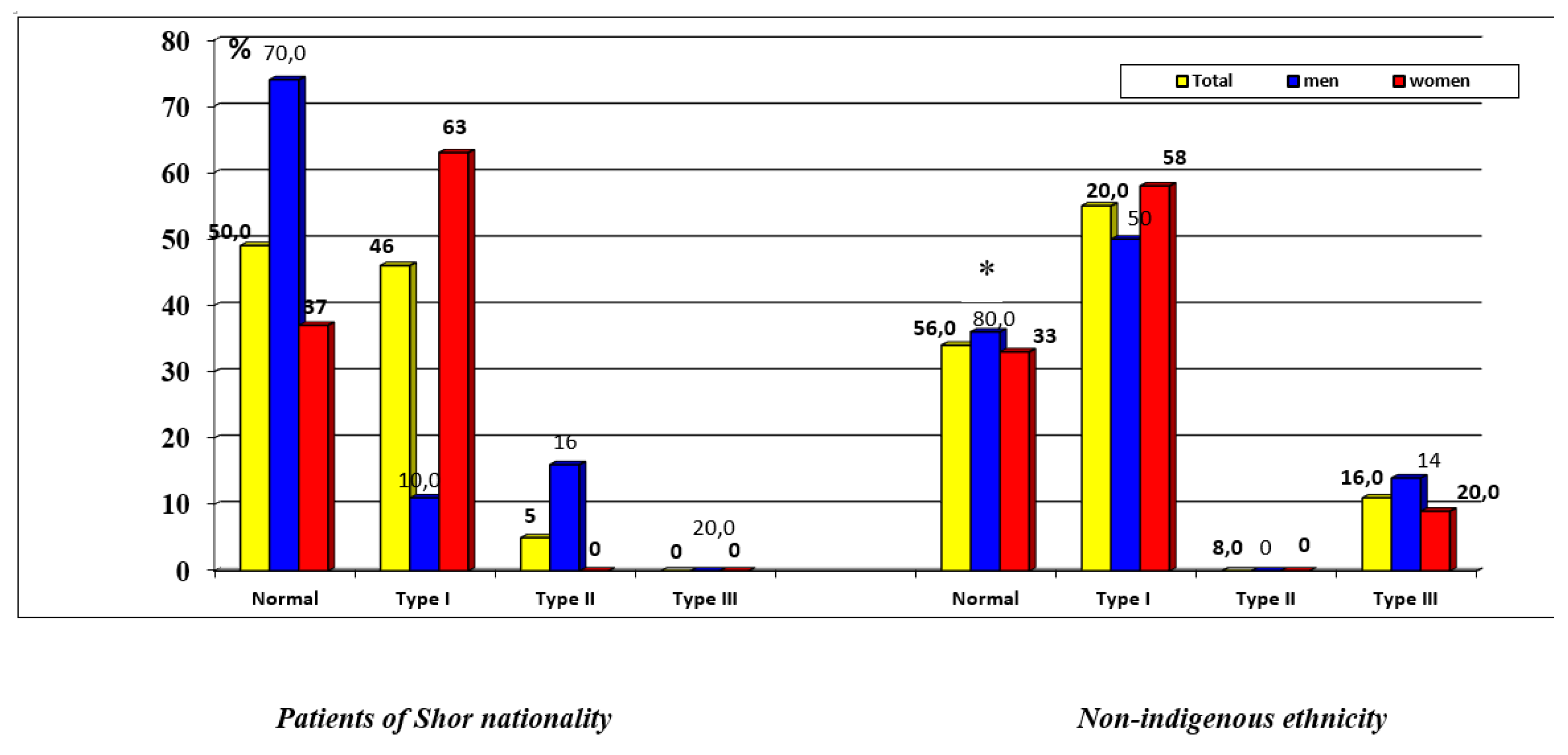
3. Results
4. Discussion
Study limitation
5. Conclusion
Supplementary Materials
Conflicts of Interest
References
- Kawel-Boehm N, Kronmal R, Eng J, Folsom A, Burke G, Carr JJ, Shea S, Lima JAC, Bluemke DA. Left Ventricular Mass at MRI and Long-term Risk of Cardiovascular Events: The Multi-Ethnic Study of Atherosclerosis (MESA). Radiology. 2019;293(1):107-114. [CrossRef]
- Lertlaksameewilai P, Songsangjinda T, Kaolawanich Y, Yindeengam A, Krittayaphong R. Extracellular volume and left ventricular hypertrophy by cardiac magnetic resonance are independent predictors of cardiovascular outcome in obesity. Sci Rep. 2022;12(1):18758. [CrossRef]
- Lang RM, Mor-Avi V. One Size Does Not Fit All: A Cliché or a Hard Fact in Cardiac Chamber Quantification? JACC Cardiovasc Imaging. 2015 Jun;8(6):666-8. [CrossRef]
- Asch FM, Banchs J, Price R, Rigolin V, Thomas JD, Weissman NJ, Lang RM. Need for a Global Definition of Normative Echo Values-Rationale and Design of the World Alliance of Societies of Echocardiography Normal Values Study (WASE). J Am Soc Echocardiogr. 2019;32(1):157-162.e2. [CrossRef]
- Piskorz, D. Ethnicity and Left Ventricular Hypertrophy: Tools and Uncertainties. High Blood Press Cardiovasc Prev. 2018 Sep;25(3):291-294. [CrossRef]
- Wegener A, Kaagaard MD, Gomes LC, Holm AE, Matos LO, Lima KO, Vieira IVM, de Souza RM, Olsen FJ, Marinho CRF, Biering-Sørensen T, Silvestre OM, Brainin P. Reference values for left ventricular dimensions, systolic and diastolic function: a study from the Amazon Basin of Brazil. Int J Cardiovasc Imaging. 2021 Nov 22. [CrossRef]
- Sheng Y, Li M, Xu M, Zhang Y, Xu J, Huang Y, Li X, Yao G, Sui W, Zhang M, Zhang Y, Zhang C, Zhang Y, Zhang M. Left ventricular and atrial remodelling in hypertensive patients using thresholds from international guidelines and EMINCA data. Eur Heart J Cardiovasc Imaging. 2022 Jan 24;23(2):166-174. [CrossRef]
- Vidula MK, Chirinos JA. Adverse cardiac remodelling: discerning the normal from the pathologic using ethnic-specific echocardiographic thresholds. Eur Heart J Cardiovasc Imaging. 2022;23(2):175-176. [CrossRef]
- Cuspidi C, Tadic M. Left ventricular hypertrophy in hypertension: Need of ethnic-specific criteria. J Clin Hypertens (Greenwich). 2022 Nov;24(11):1530-1531. [CrossRef]
- Asch FM, Miyoshi T, Addetia K, Citro R, Daimon M, Desale S, Fajardo PG, Kasliwal RR, Kirkpatrick JN, Monaghan MJ, Muraru D, Ogunyankin KO, Park SW, Ronderos RE, Sadeghpour A, Scalia GM, Takeuchi M, Tsang W, Tucay ES, Tude Rodrigues AC, Vivekanandan A, Zhang Y, Blitz A, Lang RM; WASE Investigators. Similarities and Differences in Left Ventricular Size and Function among Races and Nationalities: Results of the World Alliance Societies of Echocardiography Normal Values Study. J Am Soc Echocardiogr. 2019 Nov;32(11):1396-1406.e2. [CrossRef]
- Arkhipov, O.G. , Suslova N.S., Sumin A.N. Structural and Functional Indicators of Echocardiography in Healthy Representatives of Indigenous and Non-organized Urbanized Population of Gornaya Shoria. The Siberian Medical Journal. 2019;34(1):152–161. (in Russian). [CrossRef]
- Sumin AN, Gomozova NS, Shcheglova AV, Arkhipov OG. Ethnic differences in right ventricular structure and function in urbanized hypertensive patients in the Gornaya Shoriya region. Sci Rep. 2023 Mar 21;13(1):4628. [CrossRef]
- Mulerova T, Ogarkov M, Uchasova E, Voevoda M, Barbarash O. A comparison of the genetic and clinical risk factors for arterial hypertension between indigenous and non-indigenous people of the Shoria Mountain Region. Clin Exp Hypertens. 2018;40(4):324-331. [CrossRef]
- Mihalina EV, Mulerova TA, Polikutina OM, Ogarkov MYu. Prevalence of coronary artery disease in the indigenous population of Gornaya Shoria (the results of epidemiological studies in 1998-2001 and 2013-2017). Complex Issues of Cardiovascular Diseases. 2019; 8 (4S): 15-21. (in Russ.). [CrossRef]
- Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015; 16:233-270.
- Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, Gottdiener J, Haluska B, Ofili E, Segers P, Senior R, Tapp RJ, Zamorano JL. Recommendations on the Use of Echocardiography in Adult Hypertension: A Report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015 Jul;28(7):727-54. [CrossRef]
- Barbarash OL, Mulerova TA, Maksimov VN, Chigisova AN, Voevoda MI, Ogarkov MY. Left Ventricular Myocardial Hypertrophy as a Result of Arterial Hypertension Among Mountain Shoria Population. The Role of Genetic Polymorphism. Kardiologiia. 2018 Sep;58(9):37-46. (in Russian).
- Park CM, March K, Ghosh AK, Jones S, Coady E, Tuson C, Francis D, Mayet J, Tillin T, Chaturvedi N, Hughes AD. Left-ventricular structure in the Southall And Brent REvisited (SABRE) study: explaining ethnic differences. Hypertension. 2013 May;61(5):1014-20. [CrossRef]
- Poppe KK, Bachmann ME, Triggs CM, Doughty RN, Whalley GA. Geographic variation in left ventricular mass and mass index: a systematic review. J Hum Hypertens. 2012 Jul;26(7):420-9. [CrossRef]
- Echocardiographic Normal Ranges Meta-Analysis of the Left Heart Collaboration. Ethnic-Specific Normative Reference Values for Echocardiographic LA and LV Size, LV Mass, and Systolic Function: The EchoNoRMAL Study. JACC Cardiovasc Imaging. 2015 Jun;8(6):656-65. [CrossRef]
- Miyoshi T, Addetia K, Citro R, Daimon M, Desale S, Fajardo PG, Kasliwal RR, Kirkpatrick JN, Monaghan MJ, Muraru D, Ogunyankin KO, Park SW, Ronderos RE, Sadeghpour A, Scalia GM, Takeuchi M, Tsang W, Tucay ES, Tude Rodrigues AC, Vivekanandan A, Zhang Y, Blitz A, Lang RM, Asch FM; WASE Investigators. Left Ventricular Diastolic Function in Healthy Adult Individuals: Results of the World Alliance Societies of Echocardiography Normal Values Study. J Am Soc Echocardiogr. 2020 Oct;33(10):1223-1233. [CrossRef]
- Chahal NS, Lim TK, Jain P, Chambers JC, Kooner JS, Senior R. Ethnicity-related differences in left ventricular function, structure and geometry: a population study of UK Indian Asian and European white subjects. Heart. 2010 Mar;96(6):466-71. [CrossRef]
- Chang SN, Sung KT, Huang WH, Lin JW, Chien SC, Hung TC, Su CH, Hung CL, Tsai CT, Wu YW, Chiang FT, Yeh HI, Hwang JJ. Sex, racial differences and healthy aging in normative reference ranges on diastolic function in Ethnic Asians: 2016 ASE guideline revisited. J Formos Med Assoc. 2021;120(12):2160-2175. [CrossRef]
- de Simone, G. Left ventricular hypertrophy in blacks and whites: different genes or different exposure? Hypertension. 2005;46(1):23-4. [CrossRef]
| Patients of Shor nationality (n=58) | Patients with non-indigenous ethnicity (n=50) | Н | p | |||
|---|---|---|---|---|---|---|
| men (n=20) | women (n=38) | men (n=15) | women (n=35) | |||
| Age (years) | 51.5 [45-55] | 48 [43-53] | 52 [41-55] | 51 [44-55] | 2.11 | 0.27 |
| Weight (kg) | 65 [60-69] | 71 [64-80] ^ | 75 [65-90] * | 79 [67-88] | 10.77 | 0.005 |
| Height (cm) | 161 [157.5-166.5] | 156.5 [154-162] ^ | 169 [166-171] * | 160 [157-164] + | 28.93 | 0.036 |
| BSA (m2) | 1.7 [1.64-1.8] | 1.75 [1.7-1.8] ^ | 1.8 [1.7-1.9] * | 1.8 [1.7-1.9] | 9.63 | 0.004 |
| BMI (kg / m2) | 24.61[22.29-27.36] | 29.14 [26.48-32.79] ^ | 26.89[23.22-31.24] | 31.16 [26.98-33.79] | 15.48 | 0.0014 |
| Obesity | 0 (0%) | 2 (5.3%) | 2 (13.3%) | 3 (8.57%) | 2.87 | 0.41 |
| Elementary education | 2 (10%) | 2 (5.3%) | 0 (0%) | 1 (2.86%) | 0.43 | 0.5 |
| Secondary education | 9 (45%) | 14 (36.84%) | 1 (6.66%) * | 11 (31.43%) | 6.3 | 0.09 |
| Vocational education | 8 (40%) | 20 (52.6%) | 14 (93.3%) * | 20 (57.14%) + | 10.65 | 0.013 |
| Higher education | 1 (5%) | 2 (5.3%) | 0 (0%) | 3 (8.57%) | 1.49 | 0.68 |
| Hard physical labor | 16 (80%) | 20 (52.6%) ^ | 8 (53.3%) | 16 (45.7%) | 0.45 | 0.5 |
| Smoking | 14 (24.1%) | 9 (23.7%) ^ | 4 (26.6%) * | 5 (14.3%) | 11.54 | 0.003 |
| Cholesterol (mmol / L) | 6.65 [5.2-7.3] | 6.4 [5.9-6.9] | 6.4 [5.4-6.9] | 6.4 [5.9-7.4] | 1.47 | 0.73 |
| LDL (mmol / l) | 2.5 [2.0-3.9] | 2.9 [2.3-3.7] | 2.9 [2.5-4.1] | 3.8 [3.1-4.1] | 14.93 | 0.83 |
| HDL (mmol / L) | 1.2 [1.1-1.5] | 1.12 [0.96-1.59] | 1.05 [0.92-1.2] | 1.06 [0.94-1.2] | 6.28 | 0.21 |
| Glucose (mmol / L) | 5.14 [4.37-5.9] | 4.7 [4.2-5.5] | 5.8 [5.1-6.2] | 5.9 [5.1-6.1] | 12.85 | 0.33 |
| SBP (mm Hg) | 140 [125-150] | 140 [130-150] | 150 [130-160] | 140 [130-150] | 4,2 | 0.97 |
| DBP (mm Hg) | 80 [80-80] | 80 [80-80] | 80 [80-100] | 80 [80-90] | 6,9 | 0,44 |
| Patients of Shor nationality (n=58) |
Patients with non-indigenous ethnicity (n=50) |
Н | р | |||
|---|---|---|---|---|---|---|
| men (n=20) | women (n=38) | men (n=15) | women (n=35) | |||
| Aorta (mm) | 35.5 [33-37] | 37 [36-38] | 38 [37-38] | 37 [35-38] | 8.14 | 0.06 |
| Aorta index (mm/m2) | 29.5 [25.4-31] | 26 [24-30] | 28.3 [22.9-31.2] | 25.6 [22.2-30] | 4.14 | 0.1 |
| TPW (mm) | 11 [11.0-12.0] | 12 [11.0-13.0] | 11 [11.0-12.0] | 11 [11.0-13.0] | 1.25 | 0.38 |
| TPWi (mm/m2) | 9.06 [8.5-10.3] | 8.6 [7.2-10.3] | 8.8 [6.6-9.7] | 8.5 [7.5-9.6] | 3.7 | 0.15 |
| TIVS (mm) | 12 [11.0-13.0] | 12.5 [11.0-13.0] | 11 [11.0-12.0] | 12.0 [10.0-13.0] | 3.99 | 0.18 |
| TIVSi (mm/m2) | 9.8 [7.9-10.7] | 9.08 [8.09-10.4] | 8.8 [6.6-9.7] | 8.3 [7.2-9.5] | 8.7 | 0.39 |
| LVM (g) | 173.5 [155.5-193] | 176 [159-214] | 182 [167-196] | 185 [161-205] | 0.98 | 0.53 |
| LVMi (g/m2) | 141.9[119.7-164.2] | 132 [114-162] | 127.4 [105-147] | 134 [108.4-154] | 1.74 | 0.37 |
| EDD (mm) | 50 [48-53] | 53 [48-54] | 55.5 [53-56] | 51 [49-55] | 4.65 | 0.30 |
| EDV (ml) | 109.5 [103-122] | 132 [100-142] | 135 [127-150] | 124 [104-150] | 6.05 | 0.15 |
| LVEDVi (ml/m2) | 89.4 [84-98] | 86.7 [73.5-110] | 102 [77.9-120] | 89.8 [79.5-104.6] | 1.46 | 0.46 |
| LVEF % | 66 [62-69] | 65 [63-68] | 67 [64-70] | 67 [64-70] | 3.18 | 0.52 |
| LA (mm) | 38 [35-39] | 38 [37-40] | 39 [37-40] | 39 [37-40] | 4.43 | 0.26 |
| LAV (ml) | 81 [50-89] | 79 [57-88] | 89 [68-91] | 81 [66-89] | 4.12 | 0.68 |
| LAVi (ml/m2) | 63.2 [41.9-72.5] | 54.5 [44.5-62.5] | 64.3 [47.8-69.7] | 53.1 [40.4-66.4] | 3.46 | 0.14 |
| PA (mm) | 21 [20-21] | 21 [20-22] | 22 [20-22] | 21 [20-22] | 3.88 | 0.16 |
| PAi (mm/m2) | 17.2 [15-18] | 15.7 [13.9-17.9] ^ | 15.3 [12.6-17.6] | 15.4 [13-17.4] | 5.47 | 0.05 |
| RA (mm) | 32 [31.5-35] | 35 [32-36] ^ | 35 [33-38] * | 35 [32-38] | 7.59 | 0.04 |
| RAS (cm2) | 11.5 [11.5-14.4] | 14.4 [11.5-16.3] | 15.4 [12-17.5] | 14.2 [11.5-17] | 5.35 | 0.067 |
| RASi (cm2/m2) | 10 [8.4-11.7] | 10.3 [8.7-11.7] | 10.7 [9.3-12] | 9.3 [7.6-11.5] | 2.56 | 0.78 |
| Patients of Shor nationality (n=58) |
Patients with non-indigenous ethnicity (n=50) |
H | р | |||
|---|---|---|---|---|---|---|
| men (n=20) | women (n=38) | men (n=15) | women (n=35) | |||
| IVRT (msec) | 68 [60-81] | 81 [74-90] | 80 [67-104] | 89 [70-100] | 7.23 | 0.065 |
| E (cm/sec) | 76 [64-89.5] | 62.5 [56-76] | 69 [57-94] | 61.5 [53-76] | 4.74 | 0.112 |
| A (cm/sec) | 59.1 [47.1-73.1] | 71.3 [57.5-82.0] | 68.5 [48.2-83.0] | 72.7 [58.7-82.0] | 4.50 | 0.213 |
| Е/А | 1.3 [1.1-1.54] | 0.87 [0.75-1.15] | 0.99 [0.63-1.28] | 0.81 [0.71-1.27] | 4.70 | 0.016 |
| DT (msec) | 171.5 [148-200] | 203.5 [163-222] | 163 [115-222] | 177 [137-214] | 3.71 | 0.295 |
| Vf (cm/sec) | 47 [42-50.5] | 47 [35-53] | 42 [39-54] | 48 [39-60] | 1.94 | 0.585 |
| е' (cm/sec) | 12.0 [10-13] | 11.5 [9.0-13.0] | 11.0 [10.0-14.0] | 11.0 [9.0-14.0] | 0.581 | 0.901 |
| а' (cm/sec) | 9.4 [6.5-12.0] | 10.8 [8.2-12.8] | 9.4 [6.7-12.03] | 10.0 [9.2-12.6] | 2.380 | 0.497 |
| е'/ а' | 1.36 [0.77-1.7] | 1.0 [0.87-1.33] | 1.04 [0.79-1.73] | 1.2 [0.9-1.6] | 1.715 | 0.634 |
| s' (cm/sec) | 9.5 [9.0-12.0] | 9.0 [7.0-10.7] | 9.0 [7.8-13.0] | 10.0 [8.0-12.0] | 2.064 | 0.559 |
| е'sept (cm/sec) | 9.5 [9.0-12.0] | 9.8 [7.0-12.0] | 9.0 [8.0-11.0] | 10.0 [7.8-11.0] | 1.371 | 0.712 |
| е' sept/ а' sept | 1.0 [0.73-1.2] | 0.97 [0.7-1.1] | 1.06 [0.6-1.3] | 0.95 [0.73-1.3] | 0.914 | 0.822 |
| s' sept (cm/sec) | 10.3 [10.0-11.3] | 9.0 [8.0-10.0] ^ | 9.0 [8.0-11.0] | 9.0 [8.0-11.0] | 7.11 | 0.069 |
| Е/е' | 0.37 [0.30-0.44] | 0.30 [0.26-0.41] ^ | 0.37 [0.29-0.47] | 0.32 [0.28-0.47] | 2.68 | 0.44 |
| Tei index | 0.37 [0.29-0.44] | 0.49 [0.40-0.58] ^ | 0.49 [0.42-0.73] * | 0.50 [0.39-0.64] | 8.646 | 0.034 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




