Introduction
Through the last few years, the prevalence of diabetes has been increasing; specifically, it’s presumed that 643 million will have a diagnosis for diabetes by 2030 and 783 million by 2045 [
1]. Among those, 19-34% can develop a diabetic foot ulcer (DFU) during their life [
2]. DFU is a severe complication of diabetes, leading to a high risk of lower limb amputation [
3,
4] and mortality [
5]. The onset of a DFU increases the risk of mortality by 50–68% at five years, higher than some cancers [
6].
Diabetic foot is a chronic recurrent disease, and after the recovery of an active wound, a close follow-up is mandatory to avoid the recurrence of a new ulceration. Although many improvements have been achieved in this field, currently, one of the major issues of DFU’ patients remain the high risk of middle-long term recurrence after wound healing [
2]. It has been reported a rate of DFU’ recurrence of 40% and 65% at 1 and 3 years respectively [
2].
In several situations, especially in the case of peripheral arterial disease (PAD) or infected DFU, the majority of patients requires hospitalization. The length of the hospital stay has not changed over time [
7,
8] suggesting that multiple admissions and readmissions could be a contributing factor for the increasing burden of DFU care. These kind of patients with tissue loss are a very complex, often requiring multiple wound-related interventions, including lower limb revascularization and/or foot surgical procedures [
9,
10]. Nonetheless, there are few data about the epidemiology of hospital readmission in patients previously admitted for a DFU. Accordingly, the current study aims to evaluate the rate of readmission in patients affected by DFU managed by a multidisciplinary foot team (MDFT), causes and outcomes of patients requiring a new hospitalization.
Materials and Methods
Patient’ selection
The current study is a retrospective observational study. Consecutive patients who referred to tertiary level diabetic foot clinic (DiFo Clinic) from January 2019 to September 2022 due to a new diabetic foot problem requiring hospitalization were included in the study. The included patients were hospitalized in the clinical ward of the Unit of Endocrinology and Diabetology at University Hospital “Fondazione Policlinico “Tor Vergata”, serving Rome, Italy.
Patients who presented at the assessment an extensive foot tissue loss not suitable for limb salvage were excluded such as patients who died during the first hospitalization and those who lost to follow-up.
All patients have been managed by a MDFT through a standardized limb salvage protocol based on the International Working Group on the Diabetic Foot (IWGDF) guidelines including lower limb revascularization in the case of ischaemic/neuro-ischaemic DFU, antibiotic therapy (and surgery if required) in the case of infection, offloading of affected foot, foot surgery according to each specific clinical case including i.e. necrosectomy, minor amputation, bone removal, negative pressure therapy, dermal substitute application, etc [
11]. In addition, metabolic dysfunction, diabetic complications and concomitant co-morbidities were closely managed, and principles of education such as specific recommendations on wound care, foot hygiene, footwear were shared with patients, relatives and caregivers.
Once patients were discharged, they were regularly followed as outpatients in our DiFo Clinic. After 6 months of follow-up, the rate of hospital readmission for a diabetic foot problem was recorded. The following causes of hospital readmission were taken into consideration: infection of surgical site, recurrence of infected wound in the same foot, new infected ulceration in the contralateral foot, clinical recurrence of critical limb ischaemia (CLI) in previous treated limb, and CLI (associated to a new ischaemic/neuro-ischaemic DFU) requiring revascularization in the contralateral limb. Clinical recurrence of CLI was considered in the case of non-healing (absence of granulation tissue, absence of epithelialization signs, and reduction of ulcer size less than 50% after at least 4 weeks of standard of care) and/or recurrence of limb/foot pain in association with transcutaneous oxygen pressure (TcPO2) <30mmHg and positive duplex scanning requiring a new lower limb revascularization.
According to the readmission or not, patients were divided in two-groups, readmitted and not readmitted patients respectively. Hence, all patients were followed for six months more and outcomes for the two groups were analyzed and compared.
All patients provided their verbal consent for data recording and being considered for the study.
Clinical assessment
At the first admission, baseline clinical, wound and vascular characteristics were recorded.
Clinical features
Hypertension was considered in the case current antihypertensive therapy; hypercholesterolemia was considered in the case of statin therapy or in the case of impaired low-density-lipoproteins (LDL) (>70 mg/dl) at the assessment requiring statin therapy [
12]. Presence of ischaemic heart disease (IHD) was defined in the case of previous acute coronary syndrome or coronary revascularization, evidence of angina, significant changes on electrocardiography (above or under-leveling ST, q wave, inversion of T wave, new left bundle branch block). Heart failure (HF) was considered in the case of typical symptoms and echocardiographic signs of HF: reduced left ventricular ejection fraction (LVEF) (<40%) or normal or only mildly reduced LVEF and elevated levels of brain natriuretic peptides (BNP > 35 pg/ml and/or NT-proBNP > 125 pg/ml) with not dilated left ventricle (LV) associated to relevant structural heart disease (LV hypertrophy/left atrial enlargement) and/ or diastolic dysfunction [
13]. Patients were considered smokers only in case of smoke habit at the time of assessment. Cerebrovascular disease was considered in the case of previous cerebral ischaemia, previous carotid artery revascularization, new diagnosis of atherosclerotic plaque occluding carotid artery more than 70% suitable for revascularization. The rate of patients on end-stage-renal-disease (ESRD) requiring dialysis was reported.
Wound assessment
Wounds features were recorded at the first assessment according to IWGDF definitions [
14]. Diagnosis of infection has been done according to clinical signs (redness, warmth, swelling, induration, tenderness, pain, purulent secretion) [
15]. Osteomyelitis was considered in the case of deep ulcer involving the bone, confirmed by radiological evaluation (or magnetic resonance) and positive microbiological analysis [
15].
Vascular assessment
Neuro-ischaemic/ischaemic DFU included in the current study were considered in the case of either no palpable distal pedal pulses, ankle-brachial index (ABI) < 0.5 and/or transcutaneous oxygen pressure (TcPO2) < 30 mmHg requiring lower limb revascularization [
16]. The bed tests used for the vascular assessment were performed only by expert professionals working in this specific clinical setting (interventional radiologists/vascular surgeons) to avoid any risk of inter-observer variability.
Morphological evaluation of vascular tree to detect arterial stenosis/occlusions was performed in all patients by ultra-sound duplex. Computed tomography or MRI were performed only in the case of some doubt concerning vascular plaques and type of vascular intervention. The main aim of revascularization procedures was to open all occluded arteries or, if technically not possible, the revascularization of targeted artery (wound related artery). Patients were treated by dual antiplatelet therapy (acetylsalicylic acid 100 mg and clopidogrel 75 mg once a day) before the procedure and for at least one month after [
17]. In the case of intolerance to aspirin or clopidogrel, ticlopidine was administered.
In the case of clinical recurrence of CLI, patients were considered for another revascularization procedure.
Outcome measures
The outcome measures were to evaluate the rate of healing, healing time, major amputation, and survival for readmitted and not readmitted patients at 1 year of follow-up. Definitive ulcer healing was taken to be complete epithelialization of the target wound and maintenance of the closed healed epithelized surface for minimum of 2 weeks. Healing was defined as complete wound healing without major amputation, including both patients who required a minor amputation for achieving wound healing and those who recovered without a minor amputation. Healing time was reported in weeks. Major amputation was considered any amputation above the ankle.
Statistical analysis
Statistical analysis was performed by SAS (JMP12; SAS Institute, Cary, NC). Continuous variables were expressed as the mean ± SEM. Comparisons between groups’ characteristics were made with a X2 test (frequency data) or ANOVA (continuous data). Univariate logistic regression analysis was performed for all potential predictors of our outcomes of interest (healing, major amputation, survival), and represented as univariate hazard ratios (HRs) along with the respective 95% CI. Following this, all potential predictors were entered simultaneously to form a multivariate logistic regression analysis. Hazard ratios and corresponding 95% confidence intervals were obtained from stratified Cox proportional-hazards models. P<0.05 was considered statistically significant. The variables considered in the univariate analysis (and multivariate analysis) to evaluate the predictors of in-hospital readmission included all the following factors: age, sex, diabetes duration, hypertension, dyslipidemia, smoke, IHD, heart failure, ESRD on dialysis, infection, osteomyelitis, size, CLI, ulcer location (heel vs forefoot and midfoot).
According to local policy and being a retrospective study, no ethical approval was required for the study. The study was performed in the respect of Declaration of Helsinki.
Results
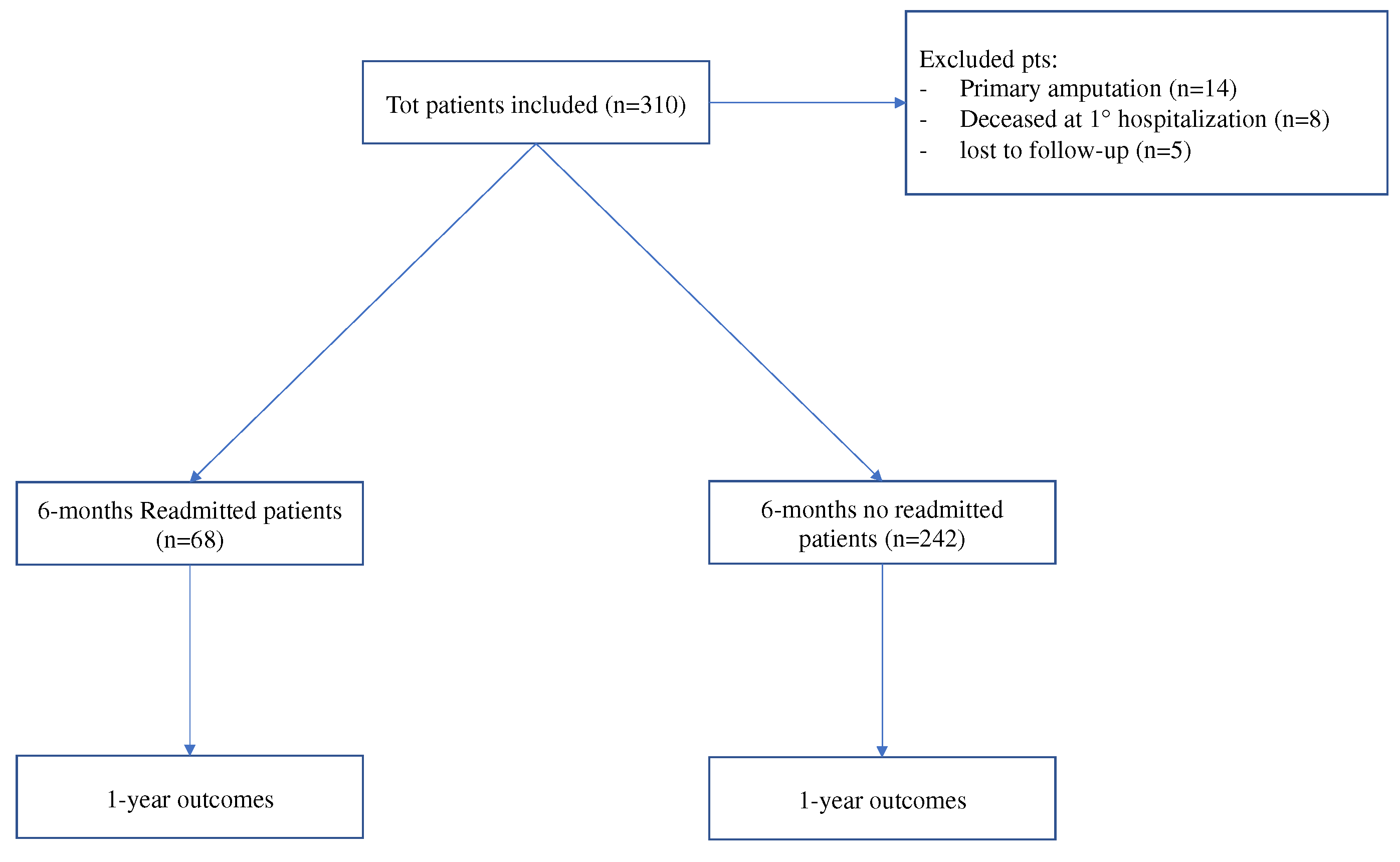
Overall, 310 patients were included, while 27 were excluded due to primary amputation (n=14), death during the 1
st hospitalization (n=8) and lost to follow-up (n=5).
Figure 1
The mean age was 68±12 years, with a prevalence of male (72.6%%); the majority of patients were affected by type 2 diabetes (>90%) with a mean diabetes duration of approximately 20 years.
Table 1.
In the majority of cases, DFUs at the assessment were ischaemic and infected, with a high incidence of osteomyelitis. Readmitted patients reported higher rate of ESRD requiring dialysis, ischemic DFU and osteomyelitis in comparison to not readmitted patients.
Table 1
After 6 months of follow-up, 68 (21.9%) patients had hospital readmission.
Figure 1
The main reason of hospital readmission resulted the presence of CLI in the contralateral limb, followed by the recurrence of CLI in the previous treated limb and the onset of new infected DFU in the contralateral foot.
Table 2.
Readmitted patients showed significantly lower rate of healing and higher rate of major amputation in comparison to not readmitted group, and lower rate of survival and longer healing time even if the differences were not statistically significant.
Table 3
At the multivariate analysis of independent predictors found at univariate analysis, CLI and ESRD resulted independent factors of 6-months hospital readmission.
Table 4
Discussion
The current study showed as hospital readmission at 6 months of follow-up is not rare involving nearly 22% of patients with DFU, and the presence of CLI (in both legs) resulted the main cause of new hospitalization, globally 10.6% of cases. In addition, CLI and ESRD requiring dialysis appeared to be independent predictors of readmission.
A similar study of Remington et al investigated the rate and causes of 30-day return to readmission among a large population including 25911 discharged patients, reporting 30% of readmissions in those who received a toe amputation and 21% among those who had midfoot amputation during the stay. [
18]
Patients with a toe or midfoot amputation procedures were less likely to be readmitted within 30 days, and the presence of concomitant co-morbidities was an independent predictor of readmission.
Holscher et al found 17% of unplanned 30-day readmission rate in a cohort of DFU patients managed by a multidisciplinary setting. [
19] Data are not so far to those reported in our study even if the follow-up was shorter in comparison to our population (30 days vs 6 months) and the authors considered all causes of hospital readmission while we analyzed only factors related to the foot problems. Nonetheless, among readmitted patients, nearly 65% of them required a new hospitalization due to a diabetic foot problem. Only current smoking and hypertension were independent predictors of readmission, while these variables were not significant in our cohort of patients. [
19]
In a larger evaluation of hospital readmission for persons with diabetes regardless the presence or not of diabetic foot disease, Wang et al reported a readmission rate of 32.4% during 5 years of follow-up and 10% of patients were readmitted for the presence of foot disorders such as limb ischaemia and foot infection. [
20]
In our current study, readmitted patients reported worse outcomes at 1 year of follow-up in comparison to not readmitted group, with lower change of healing (51.5 vs 89.2%, p<0.0001) and higher rate of major amputation (10.3 vs 4.5%, p=0.04). They showed also longer healing time (11.1 vs 9.4 weeks, p=0.1) and lower rate of survival (94 vs 97.9%, p=0.3) even if without significant statistically difference.
The data we had from the current study open a focused reflections on some specific points.
The rate of readmission is not so high in comparison to similar study reported in literature [
2] and it may be related to a very close multidisciplinary follow-up after discharge and also after achieving wound healing. Nonetheless, counting that nearly 22% of patients require a new hospitalization within 6 months after the previous hospitalization, the data should be carefully taken into consideration. DFUs should be considered a serious pitfall during the healing reparative pathway and also after wound healing.
Particularly, the impact of PAD in hospital readmission needs a special attention. Overall, CLI recurrence resulted a reason of readmission in 14/310 (4.5%) of cases in the whole population with a prevalence among ischaemic patients in 14/193 (7.2%) of cases. On the one side, data are very encouraging because the rate of clinical CLI recurrence resulted significantly lower than that reported in a previous similar study of our research group in which it was approximately 25% at 1-year of follow-up. [
21] The low rate of clinical CLI recurrence may be related to the new wound healing strategy and reduced healing time due to improvement of surgical strategies [
22], new options for neuro-ischaemic complex wounds [
23,
24] and early referral to specialized DiFo Clinic in our specific region [
25]. In addition, many improvements have been also achieved in revascularizations approach and medical therapy for improving lower limb perfusion also for no-option CLI patients [
26,
27,
28,
29]. At the same time, new drugs have been promoted to maintain a long-term patency in patients endovascular approach [
30,
31] that can help ischaemic DFUs requiring long healing time such as very large post-surgical wounds.
The high rate of new ischaemic/neuro-ischaemic DFU associated to CLI requiring revascularization in the contralateral limb requires also a great attention. In the current study we reported a risk of readmission for a contralateral CLI in 19/310 (6.1%) patients among the whole population and specifically in 19/193 (9.8%) patients considering only ischaemics. This means that primary and secondary prevention should be reinforced in both feet to reduce any risk of new ulceration also in the healthy foot. As reported in previous studies and recommended by guidance, the risk of new ulceration or re-ulceration may be drastically reduced by the integrated foot care involving different healthcare professionals, patient’ education and therapeutic footwear.[
32]
It has been reported a low rate of infection of surgical site in the foot treated during the first hospitalization, showing as an adequate curative surgery in skilled diabetic foot surgeons is useful for achieving wound healing and safe in terms of local complications.
Among concomitant co-morbidities, ESRD resulted an independent predictor of readmission, confirming as renal failure is a heavy risk factor for clinical CLI recurrence [
19], non-healing and major amputation as reported in previous studies. [
33,
34,
35]
These data invite to improve the management strategies in patients on dialysis to promote the healing process before having the recurrence of peripheral ischaemia. In addition, early referral to specialized DiFo Clinic is mandatory to avoid the impairment of ulcer’ characteristics such as depth, size, infection that may lead to worse outcomes.
The study has some limitations. It is a retrospective single centre study. Patients were managed by a MDFT in a tertiary level DiFO Clinic by a local protocol in the respect of standard of care. The rate of readmission has been evaluated after 6 months of follow-up and data can be different in a longer follow-up. The other reasons of hospital readmission not including foot problems were not considered.
Conclusions
To our best knowledge the current study is the first one to analyze the rate and the outcomes of hospital readmission in a long-term follow-up of patients with DFU. These data may help clinicians in the current and future operative strategies to better manage the main causes of readmission and improve outcomes. Particularly, fast wound healing should be achieved in patients with CLI treated by revascularization and a careful attention should be addressed to reduce the risk of new ulceration in the healthy foot in patients with PAD. Among these subjects, those with ESRD should be closely managed having the highest risk of hospital readmission
Author Contributions
Conceptualization, M.M. Methodology, M.M ; Validation, A.A, B.E., R.V., R.M., G.L., B.A., U.L., L.D.; Formal Analysis, M.M.; Investigation, M.M, B.E..; Data Curation, M.M.; Writing – Original Draft Preparation, M.M.; Writing – Review & Editing, D.L.; Visualization, B A.A, B.E., R.V., R.M., G.L., B.A., U.L., L.D.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
-
https://diabetesatlas.org/#:~:text=1%20in%2022%20adults%20(24,for%20416%2C000%20deaths%20in%202021.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017 Jun 15;376(24):2367-2375. [CrossRef] [PubMed]
- Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005; 366(9498):1719–1724. [CrossRef]
- Wu H, Yang A, Lau ESH et al. Secular trends in rates of hospitalization for lower extremity amputation and 1 year mortality in people with diabetes in Hong Kong, 2001-2016: a retrospective cohort study. Diabetologia 2020; 63(12):2689–2698. [CrossRef]
- Morbach S, Furchert H, Gröblinghoff U et al. Long-term prognosis of diabetic foot patients and their limbs: amputation and death over the course of a decade. Diabetes Care 2012;35(10):2021–2027. [CrossRef]
- Armstrong DG, Wrobel J, Robbins JM. Guest editorial: are diabetes related wounds and amputations worse than cancer? Int Wound J 2007; [CrossRef]
- Hicks CW, Selvarajah S, Mathioudakis N, Perler BA, Freischlag JA, Black JH III, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg 2014;60:1247-54.e2. [CrossRef]
- Mantovani A, Grani G, Chioma L, Vancieri G, Giordani I, Rendina R, Rinaldi ME, Andreadi A, Coccaro C, Boccardo C, Fraenza C, Bertazzoni G, Bellia A, Zoppini G, Targher G, Baroni MG, Lauro D, D'Armiento M, Bonora E. Severe hypoglycemia in patients with known diabetes requiring emergency department care: A report from an Italian multicenter study. J Clin Transl Endocrinol. 2016 Aug 20;5:46-52. PMCID: PMC5644438. [CrossRef] [PubMed]
- Wang C, Mai L, Yang C, Liu D, Sun K, Song W, et al. Reducing major lower extremity amputations after the introduction of a multidisciplinary team in patient with diabetes foot ulcer. BMC Endocr Disord 2016;16:38. [CrossRef]
- Williams DT, Majeed MU, Shingler G, Akbar MJ, Adamson DG, Whitaker CJ. A diabetic foot service established by a department of vascular surgery: an observational study. Ann Vasc Surg 2012;26:700-6. [CrossRef]
- Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA; IWGDF Editorial Board. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3266. [CrossRef] [PubMed]
- Bellia A, Andreadi A, Giudice L, De Taddeo S, Maiorino A, D'Ippolito I, Giorgino FM, Ruotolo V, Romano M, Magrini A, Di Daniele N, Rogliani P, Lauro D. Atherogenic Dyslipidemia on Admission Is Associated With Poorer Outcome in People With and Without Diabetes Hospitalized for COVID-19. Diabetes Care. 2021 Sep;44(9):2149-2157. Epub 2021 Jul 12. [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González- Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Rev. Esp. Cardiol. 2016, 69, 1167. [CrossRef]
- Monteiro-Soares M, Russell D, Boyko EJ, Jeffcoate W, Mills JL, Morbach S, Game F; International Working Group on the Diabetic Foot (IWGDF). Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3273. [CrossRef] [PubMed]
- Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, Kono S, Lavery LA, Malone M, van Asten SA, Urbančič-Rovan V, Peters EJG; International Working Group on the Diabetic Foot (IWGDF). Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3280. [CrossRef] [PubMed]
- Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Hong JP, Katsanos K, Mills JL, Nikol S, Reekers J, Venermo M, Zierler RE, Schaper NC; International Working Group on the Diabetic Foot (IWGDF). Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3276. Epub 2020 Jan 20. [CrossRef] [PubMed]
- Aiello A, Anichini R, Brocco E, Caravaggi C, Chiavetta A, Cioni R, Da Ros R, De Feo ME, Ferraresi R, Florio F, Gargiulo M, Galzerano G, Gandini R, Giurato L, Graziani L, Mancini L, Manzi M, Modugno P, Setacci C, Uccioli L; Italian Society of Diabetes; Italian Society of Radiology; Italian Society of Vascular Endovascular Surgery. Treatment of peripheral arterial disease in diabetes: a consensus of the Italian Societies of Diabetes (SID, AMD), Radiology (SIRM) and Vascular Endovascular Surgery (SICVE). Nutr Metab Cardiovasc Dis. 2014 Apr;24(4):355-69. Epub 2013 Dec 25. [CrossRef] [PubMed]
- Remington AC, Hernandez-Boussard T, Warstadt NM, Finnegan MA, Shaffer R, Kwong JZ, Curtin C. Analyzing treatment aggressiveness and identifying high-risk patients in diabetic foot ulcer return to care. Wound Repair Regen. 2016 Jul;24(4):731-6. Epub 2016 Jun 8. [CrossRef] [PubMed]
- Holscher CM, Hicks CW, Canner JK, Sherman RL, Malas MB, Black JH 3rd, Mathioudakis N, Abularrage CJ. Unplanned 30-day readmission in patients with diabetic foot wounds treated in a multidisciplinary setting. J Vasc Surg. 2018 Mar;67(3):876-886. Epub 2017 Oct 7. [CrossRef] [PubMed]
- Junmei Wang, Jiayao Xiong, Chao Yang et al. Analysis of Reasons For Readmission of Diabetic Patients: 2015-2019, 03 January 2022, PREPRINT (Version 1) available at Research Square [https://doi.org/10.21203/rs.3.rs-1199123/v1]. [CrossRef]
- Meloni M, Izzo V, Giurato L, Del Giudice C, Da Ros V, Cervelli V, Gandini R, Uccioli L. Recurrence of Critical Limb Ischemia After Endovascular Intervention in Patients with Diabetic Foot Ulcers. Adv Wound Care (New Rochelle). 2018 Jun 1;7(6):171-176. PMCID: PMC5994148. [CrossRef] [PubMed]
- Uccioli L, Meloni M, Izzo V, Giurato L. Use of Nevelia Dermal-Epidermal Regenerative Template in the Management of Ischemic Diabetic Foot Postsurgical Wounds. Int J Low Extrem Wounds. 2020 Sep;19(3):282-288. Epub 2020 Jan 29. [CrossRef] [PubMed]
- Edmonds M, Lázaro-Martínez JL, Alfayate-García JM, Martini J, Petit JM, Rayman G, Lobmann R, Uccioli L, Sauvadet A, Bohbot S, Kerihuel JC, Piaggesi A. Sucrose octasulfate dressing versus control dressing in patients with neuroischaemic diabetic foot ulcers (Explorer): an international, multicentre, double-blind, randomised, controlled trial. Lancet Diabetes Endocrinol. 2018 Mar;6(3):186-196. Epub 2017 Dec 20. Erratum in: Lancet Diabetes Endocrinol. 2018 Mar 6. [CrossRef] [PubMed]
- Meloni M, Giurato L, Panunzi A, Bellia A, Bohbot S, Lauro D, Uccioli L. Effectiveness of Sucrose Octasulfate Dressing in the Treatment of Neuro-Ischaemic Diabetic Foot Heel Ulcers: A Retrospective Single arm Study. Int J Low Extrem Wounds. 2022 Mar 15:15347346221087499. Epub ahead of print. [CrossRef] [PubMed]
- Meloni M, Lazaro-Martínez JL, Ahluwalia R, Bouillet B, Izzo V, Di Venanzio M, Iacopi E, Manu C, Garcia-Klepzig JL, Sánchez-Ríos JP, Lüedemann C, De Buruaga VR, Vouillarmet J, Guillaumat J, Aleandri AR, Giurato L, Edmonds M, Piaggesi A, Van Acker K, Uccioli L. Effectiveness of fast-track pathway for diabetic foot ulcerations. Acta Diabetol. 2021 Oct;58(10):1351-1358. Epub 2021 May 3. PMCID: PMC8413149. [CrossRef] [PubMed]
- Gandini R, Merolla S, Scaggiante J, Meloni M, Giurato L, Uccioli L, Konda D. Endovascular Distal Plantar Vein Arterialization in Dialysis Patients With No-Option Critical Limb Ischemia and Posterior Tibial Artery Occlusion: A Technique for Limb Salvage in a Challenging Patient Subset. J Endovasc Ther. 2018 Feb;25(1):127-132. Epub 2017 Dec 21. [CrossRef] [PubMed]
- Meloni M, Morosetti D, Giurato L, Stefanini M, Loreni G, Doddi M, Panunzi A, Bellia A, Gandini R, Brocco E, Lazaro-Martinez JL, Lauro D, Uccioli L. Foot Revascularization Avoids Major Amputation in Persons with Diabetes and Ischaemic Foot Ulcers. J Clin Med. 2021 Sep 2;10(17):3977. PMCID: PMC8432560. [CrossRef] [PubMed]
- Panunzi A, Madotto F, Sangalli E, Riccio F, Sganzaroli AB, Galenda P, Bertulessi A, Barmina MF, Ludovico O, Fortunato O, Setacci F, Airoldi F, Tavano D, Giurato L, Meloni M, Uccioli L, Bruno A, Spinetti G, Caravaggi CMF. Results of a prospective observational study of autologous peripheral blood mononuclear cell therapy for no-option critical limb-threatening ischemia and severe diabetic foot ulcers. Cardiovasc Diabetol. 2022 Sep 28;21(1):196. PMCID: PMC9516816. [CrossRef] [PubMed]
- Scatena A, Petruzzi P, Maioli F, Lucaroni F, Ambrosone C, Ventoruzzo G, Liistro F, Tacconi D, Di Filippi M, Attempati N, Palombi L, Ercolini L, Bolognese L. Autologous Peripheral Blood Mononuclear Cells for Limb Salvage in Diabetic Foot Patients with No-Option Critical Limb Ischemia. J Clin Med. 2021 May 20;10(10):2213. PMCID: PMC8161401. [CrossRef] [PubMed]
- Anand SS, Caron F, Eikelboom JW, Bosch J, Dyal L, Aboyans V, Abola MT, Branch KRH, Keltai K, Bhatt DL, Verhamme P, Fox KAA, Cook-Bruns N, Lanius V, Connolly SJ, Yusuf S. Major Adverse Limb Events and Mortality in Patients With Peripheral Artery Disease: The COMPASS Trial. J Am Coll Cardiol. 2018 May 22;71(20):2306-2315. Epub 2018 Mar 11. [CrossRef] [PubMed]
- Bauersachs RM, Szarek M, Brodmann M, Gudz I, Debus ES, Nehler MR, Anand SS, Patel MR, Hess CN, Capell WH, Rogers K, Muehlhofer E, Haskell LP, Berkowitz SD, Hiatt WR, Bonaca MP; VOYAGER PAD Committees and Investigators. Total Ischemic Event Reduction With Rivaroxaban After Peripheral Arterial Revascularization in the VOYAGER PAD Trial. J Am Coll Cardiol. 2021 Jul 27;78(4):317-326. Epub 2021 May 16. [CrossRef] [PubMed]
- Bus SA, Lavery LA, Monteiro-Soares M, Rasmussen A, Raspovic A, Sacco ICN, van Netten JJ; International Working Group on the Diabetic Foot. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3269. [CrossRef] [PubMed]
- Uccioli L, Izzo V, Meloni M, Vainieri E, Ruotolo V, Giurato L. Non-healing foot ulcers in diabetic patients: general and local interfering conditions and management options with advanced wound dressings. J Wound Care. 2015 Apr;24(4 Suppl):35-42. [CrossRef] [PubMed]
- Meloni M, Izzo V, Giurato L, Da Ros V, Morosetti D, Ferrannini M, Brocco E, Gandini R, Uccioli L. Peripheral arterial disease in patients with renal-diabetic foot ulcers. J Wound Care. 2021 Aug 2;30(8):660-664. [CrossRef] [PubMed]
- Meloni M, Giurato L, Izzo V, Stefanini M, Pampana E, Gandini R, Uccioli L. Long term outcomes of diabetic haemodialysis patients with critical limb ischemia and foot ulcer. Diabetes Res Clin Pract. 2016 Jun;116:117-22. Epub 2016 Apr 26. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).