Submitted:
22 June 2023
Posted:
27 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Data Source and Ethics Statement
2.2. Inclusion and Exclusion Criteria
2.3. Extraction of Demographic and Clinical Characteristics
- 1)
- First visit date
- 2)
- Sex: male, female
- 3)
- Age groups: under 20 years, 20s-30s (20-39 years), 40s-50s (40-59 years), over 60 years
- 4)
- Lesion site: left, right
- 5)
- Predisposing factors: fatigue and overwork, insomnia, stress, on a diet, exposure to severe temperature difference, virus disease (i.e., cold, enteritis), Covid-19 vaccination, others
- 6)
- Disease phase: acute phase (within 7 days from onset), subacute phase (over 7 days and within 3 months from onset), chronic phase (over 3 months)
- 7)
- Residence: Seoul, Gyeonggi-do, Incheon, Hoseo region (Chungchoeng-do, Daejeon, Sejong), Gangwon-do, Yeongnam region (Gyeongsang-do, Busan, Ulsan, Daegu), Honam region (Jeolla-do, Gwangju), Jeju-do, Foreign region (Figure A)
- 8)
- Residence in Seoul: northeastern region, northwestern region, inner city region, southeastern region, southwestern region
- 9)
- Hospital visit routes: ‘no treatment prior to visit’, ‘only Western Medicine treatment prior to visit’, ‘only Korean Medicine treatment prior to visit’, ‘both Western and Korean Medicine treatment prior to visit’
- 10)
- Patient care type: only outpatient care, both outpatient and inpatient care
2.4. Statistical Analysis
3. Results
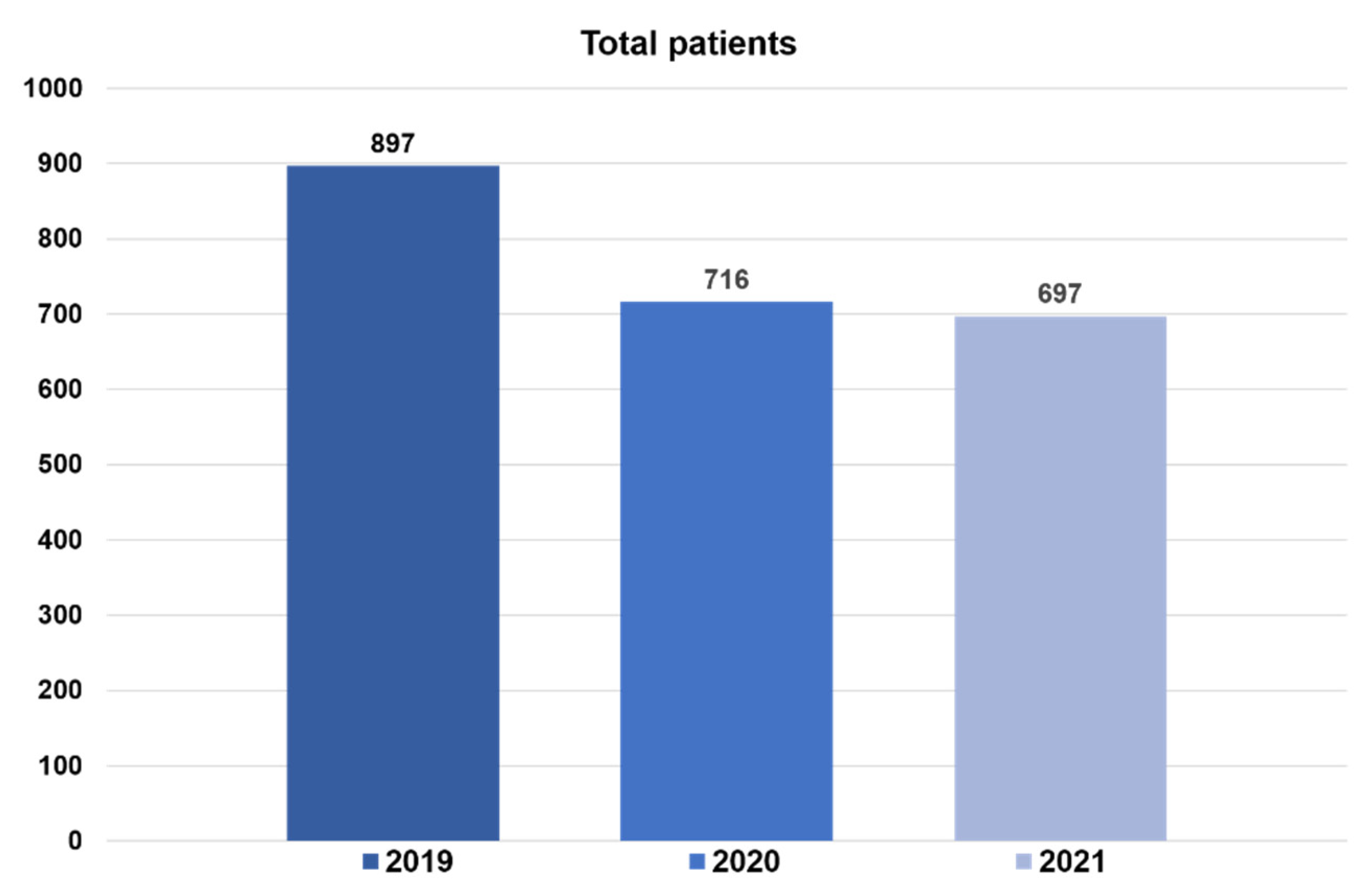
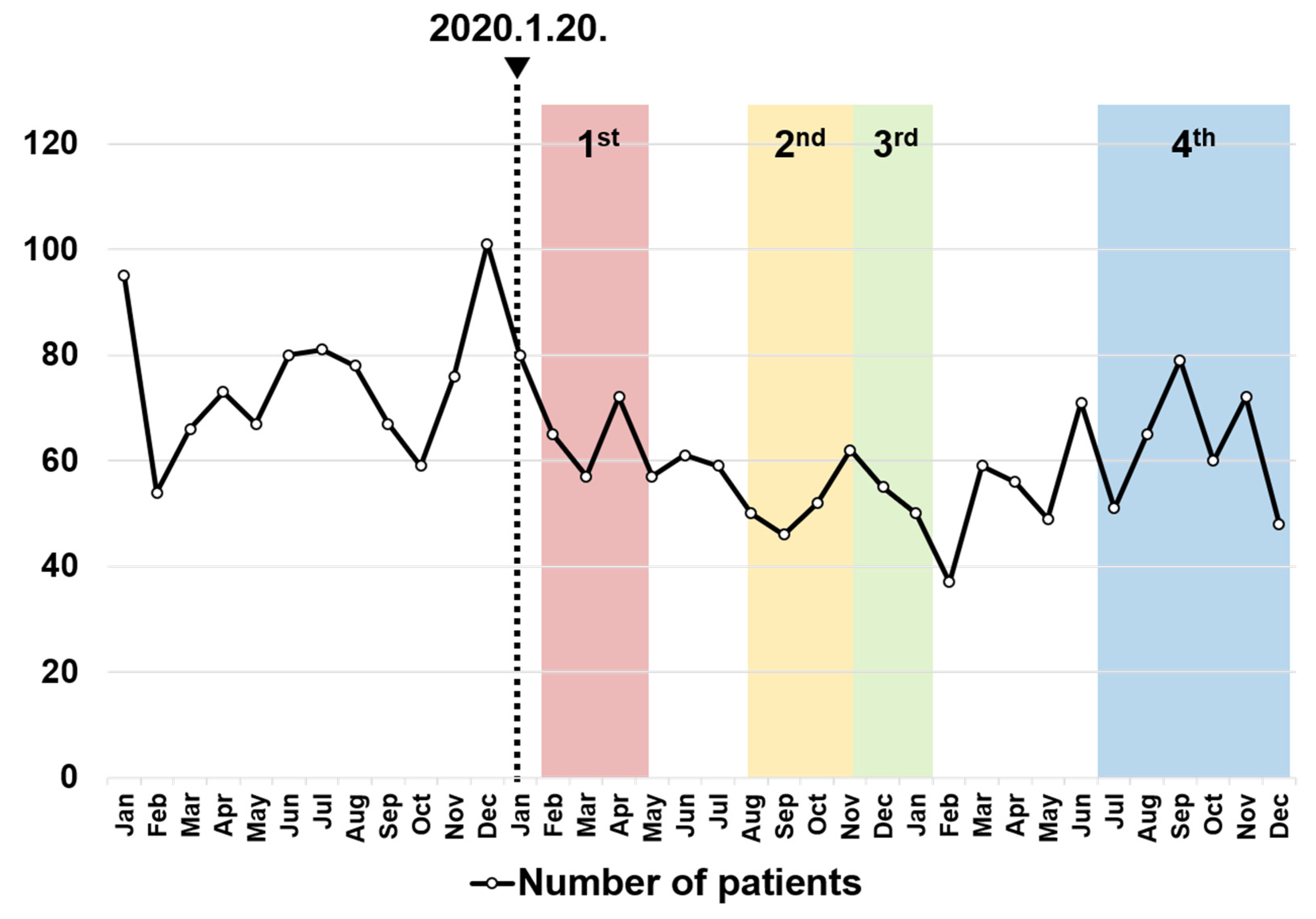
3.1. Total Numbers of Patients by Year
3.2. Demographic Characteristics
3.3. Disease Phase Distribution
3.4. Distribution of Residence Locations
3.5. Distribution of Residence Locations in Seoul
3.6. Distribution of the Hospital Visit Routes
3.7. Distribution of Patient Care Type
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Classification of Administrative Districts of South Korea Used in the Study

Appendix B. The Proportion of Residence by Disease Stage before and during COVID-19
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Seoul | 264 (60.4%) | 253 (66.9%) | 239 (62.1%) | 492 (64.5%) | 0.6564 | |
| Geonggi | 123 (28.1%) | 97 (25.7%) | 116 (30.1%) | 213 (27.9%) | ||
| Incheon | 15 (3.4%) | 7 (1.9%) | 11 (2.9%) | 18 (2.4%) | ||
| Ho-seo | 8 (1.8%) | 5 (1.3%) | 4 (1.0%) | 9 (1.2%) | ||
| Gwang Won | 6 (1.4%) | 7 (1.9%) | 6 (1.6%) | 13 (1.7%) | ||
| Yeongnam | 14 (3.2%) | 6 (1.6%) | 6 (1.6%) | 12 (1.6%) | ||
| Honam | 4 (0.9%) | 3 (0.8%) | 2 (0.5%) | 5 (0.7%) | ||
| Jeju | 1 (0.2%) | 0 (0.0%) | 1 (0.3%) | 1 (0.1%) | ||
| Foreign region | 2 (0.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Seoul | 157 (48.0%) | 113 (46.5%) | 111 (52.4%) | 224 (49.2%) | 0.110 | |
| Geonggi | 109 (33.3%) | 85 (35.0%) | 61 (28.8%) | 146 (32.1%) | ||
| Incheon | 14 (4.3%) | 15 (6.2%) | 9 (4.2%) | 24 (5.3%) | ||
| Ho-seo | 8 (2.4%) | 7 (2.9%) | 9 (4.2%) | 16 (3.5%) | ||
| Gwang Won | 12 (3.7%) | 6 (2.5%) | 10 (4.7%) | 16 (3.5%) | ||
| Yeongnam | 10 (3.1%) | 6 (2.5%) | 4 (1.9%) | 10 (2.2%) | ||
| Honam | 8 (2.4%) | 10 (4.1%) | 8 (3.8%) | 18 (4.0%) | ||
| Jeju | 4 (1.2%) | 1 (0.4%) | 0 (0.0%) | 1 (0.2%) | ||
| Foreign region | 5 (1.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Seoul | 60 (45.1%) | 45 (47.4%) | 50 (50.0%) | 95 (48.7%) | 0.766 | |
| Geonggi | 41 (30.8%) | 32 (33.7%) | 27 (27.0%) | 59 (30.3%) | ||
| Incheon | 3 (2.3%) | 0 (0.0%) | 3 (3.0%) | 3 (1.5%) | ||
| Ho-seo | 5 (3.8%) | 6 (6.3%) | 4 (4.0%) | 10 (5.1%) | ||
| Gwang Won | 9 (6.8%) | 4 (4.2%) | 6 (6.0%) | 10 (5.1%) | ||
| Yeongnam | 9 (6.8%) | 3 (3.2%) | 6 (6.0%) | 9 (4.6%) | ||
| Honam | 3 (2.3%) | 5 (5.3%) | 3 (3.0%) | 8 (4.1%) | ||
| Jeju | 2 (1.5%) | 0 (0.0%) | 1 (1.0%) | 1 (1.5%) | ||
| Foreign region | 1 (0.8%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
Appendix C. The Proportion of Hospital Visit Routes by Disease Stage before and during COVID-19
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| After no treatment | 66 (15.1%) | 55 (14.6%) | 42 (10.9%) | 97 (12.7%) | X2=4.768 0.190 |
|
| After only Western Medicine treatment | 216 (49.4%) | 212 (56.1%) | 213 (55. 3%) | 425 (55.7%) | ||
| After only Korean Medicine treatment | 60 (13.7%) | 45 (11.9%) | 42 (10.9%) | 87 (11.4%) | ||
| After both Western and Korean Medicine treatment | 95 (21.7%) | 66 (17.5%) | 88 (22.9%) | 154 (20.2%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| After no treatment | 6 (1.8%) | 4 (1.6%) | 2 (0.9%) | 6 (1.3%) | X2=5.544 0.136 |
|
| After only Western Medicine treatment | 130 (39.8%) | 93 (38.3%) | 72 (34.0%) | 165 (36.3%) | ||
| After only Korean Medicine treatment | 24 (7.3%) | 10 (4.1%) | 10 (4.7%) | 20 (4.4%) | ||
| After both Western and Korean Medicine treatment | 167 (51.1%) | 136 (56.0%) | 128 (60.4%) | 264 (58.0%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| After no treatment | 7 (5.3%) | 3 (3.2%) | 0 (0.0%) | 3 (1.5%) | X2=6.466 0.091 |
|
| After only Western Medicine treatment | 24 (18.0%) | 13 (13.7%) | 13 (13.0%) | 26 (13.3%) | ||
| After only Korean Medicine treatment | 18 (13.5%) | 22 (23.2%) | 16 (16.0%) | 38 (19.5%) | ||
| After both Western and Korean Medicine treatment | 84 (63.2%) | 57 (60.0%) | 71 (71.0%) | 128 (65.6%) | ||
References
- Sweeny K; Rankin K; Cheng X; Hou L; Long F; Meng Y; et al. Flow in the time of COVID-19: Findings from China. PloS one 2020, 15, e0242043.
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 6 september 2022).
- Coronavirus (COVID-19), Republic of Korea. Available online: http://ncov.kdca.go.kr/?brdId=1&brdGubun=11&ncvContSeq=&contSeq=&board_id=&gubun= (accessed on 6 september 2022).
- Changes in people’s medical usage behavior due to COVID-19. Available online: http://www.alioplus.go.kr/news/newsDetail.do;jsessionid=623l2hH4RmlgHPOwKwIq1SZQ.node21?brdSeq=10340 (accessed on 6 september 2022).
- Health Insurance Review and Assessment Service. Healthcare Bigdata Hub. Available online: http://opendata.hira.or.kr/op/opc/olapHthInsRvStatInfo.do (accessed on 6 september 2022).
- Codeluppi L; Venturelli F; Rossi J; Fasano A; Toschi G; Pacillo F; et al. Facial palsy during the COVID-19 pandemic. Brain Behav 2021, 11, e01939.
- Kerstens J; Deschuytere L; Schotsmans K; Maréchal E. Bilateral peripheral facial palsy following asymptomatic COVID-19 infection: a case report. Acta Neurologica Belgica 2021, 121, 815-6.
- Al-Kaisy M; Eid MM. Bell’s Palsy Caused by SARS-CoV-2. Case Rep. Acute Med 2021, 4, 91-4.
- Lima MA; Silva MTT; Soares CN; Coutinho R; Oliveira HS; Afonso L; et al. Peripheral facial nerve palsy associated with COVID-19. JNV 2020, 26, 941-4.
- Finsterer J; Scorza FA; Scorza CA; Fiorini AC. Attributing increased prevalence of facial palsy to SARS-CoV-2 requires evidence. Brain Behav 2020, 11, e01996. doi: 10.1002/brb3.1996.
- Mutlu A; Kalcioglu MT; Gunduz AY; Bakici B; Yilmaz U; Cag Y. Does the SARS-CoV-2 pandemic really increase the frequency of peripheral facial palsy? Am. J. Otolaryngol 2021, 42, 103032.
- Martin-Villares C; Alba JR; Gonzalez-Gimeno MJ. Data from 235 Cases of Bell's Palsy during COVID-19 Pandemic: Were There Clusters of Facial Palsy? Neuroepidemiology 2021, 55, 495.
- Colella G; Orlandi M; Cirillo N. Bell’s palsy following COVID-19 vaccination. J. Neurol 2021, 268, 3589-91.
- Martin-Villares C; Vazquez-Feito A; Gonzalez-Gimeno MJ; de la Nogal-Fernandez B. Bell’s palsy following a single dose of mRNA SARS-CoV-2 vaccine: a case report. J. Neurol 2022, 269, 47-8.
- Obermann M; Krasniqi M; Ewers N; Fayad J; Haeberle U. Bell’s palsy following COVID-19 vaccination with high CSF antibody response. Neurol. Sci. 2021, 42, 4397-9.
- Shibli R; Barnett O; Abu-Full Z; Gronich N; Najjar-Debbiny R; Doweck I, et al. Association between vaccination with the BNT162b2 mRNA COVID-19 vaccine and Bell's palsy: a population-based study. Lancet Reg. Health Eur 2021, 11, 100236.
- Klein NP; Lewis N; Goddard K; Fireman B; Zerbo O; Hanson KE; et al. Surveillance for adverse events after COVID-19 mRNA vaccination. Jama 2021, 326, 1390-9.
- Renoud L; Khouri C; Revol B; Lepelley M; Perez J; Roustit M; et al. Association of facial paralysis with mRNA COVID-19 vaccines: a disproportionality analysis using the World Health Organization pharmacovigilance database. JAMA Intern. Med. 2021, 181, 1243-5.
- Shemer A; Pras E; Einan-Lifshitz A; Dubinsky-Pertzov B; Hecht I. Association of COVID-19 vaccination and facial nerve palsy: a case-control study. JAMA Otolaryngol Head Neck Surg 2021, 147, 739-43.
- 2020 Korean Medicine Utilization Survey. Available online: https://www.koms.or.kr/main.do (accessed on 6 september 2022).
- Cha HJ; Kim BS; Sung KJ; Lee YR; Choi HK; Kim MJ; et al. Statistical Analysis of Outpatients Trends at Korean Medicine Hospitals of Daejeon University by Region before and after COVID-19. JKM 2021, 42, 26-43.
- Lee JE; Shin YJ; Shin SH. Comparative Analysis of Patients Visiting Department of Korean Internal Medicine in a Korean Medicine Hospital Before and During COVID-19-From July 2018 to June 2021 at Wonkwang University Jeonju Korean Medicine Hospital. J Int Korean Med 2021, 42, 1255-68.
- Lee YR; Cha HJ; Choi HK; Kim MJ; Kim BS; Sung KJ; et al. Statistical analysis of patients visiting department of acupuncture and moxibustion in Korean medicine hospital before and after COVID-19-Focusing on a Korean medicine hospital in Daejeon. JKM 2021, 42, 31-49.
- Kwon NH; Shin YJ; Kim CY; Koh PS; Yi WI; Joh BJ; et al. Comparative clinical study between Oriental medical and oriental-western medical treatment on bell’s palsy. Journal of Korean Acupuncture & Moxibustion Society 2008, 25, 19-28.
- Lee DH. Clinical efficacy of electroneurography in acute facial paralysis. J Audiol Otol 2016, 20, 8.
- Kim MW, Kim J. Early stage steroid treatment for acute facial paralysis in Korea. Korean J Otorhinolaryngol-Head Neck Surg 2016, 59, 346-52.
- Clinical practice Guideline of Korean Medicine for Facial palsy. Available online: https://nikom.or.kr/nikom/index.do (accessed on 6 september 2022).
- 2022 Health Insurance Health Insurance Medical Care Benefit. Available online: https://repository.hira.or.kr/handle/2019.oak/2964 (accessed on 6 september 2022).
- Yang JH. A Comparative Study on Hospital Choice Factors between First-visit and Revisit patients in General Hospitals. J. Digit. Converg 2017, 15, 231-8.
- Peitersen E. Bell's palsy: the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta oto-laryngologica 2002, 122, 4-30.
- Oh JY; Cho SJ; Choi JS. Changes in Health Care Utilization during the COVID-19 Pandemic. Health Policy and Management 2021, 31, 508-17.
- Shin JW; Moon SJ; Jeong SH. COVID-19 and medical care service utilization experience. Health and welfare Issue & Focus 2021, 400, 1-8.
- Han SH; Kang JK; Hong JS. A Study of Factors Related to the Subjective Health Status of Elderly Population in Korea. Health Policy and Management 2021, 31, 56-64.
- Valls-Solé J. Facial palsy, postparalytic facial syndrome, and hemifacial spasm. J. Mov. Disord 2002, 17, S49-S52.
- Kim SH; Lee HJ; Lee KS; Shin HW. Factors Affecting Patient Moving for Medical Service Using Multi-level Analysis. Korean J Hosp Manag 2014, 19, 9-20.
- Garro A; Nigrovic LE. Managing peripheral facial palsy. Annals of Emergency Medicine 2018, 71, 618-24.
- Shin JW; Jo BH; Choi BR; Kim HN; Moon SJ; Jin JH, et al. 2020 Medical service experience survey. Sejong: KIHASA 2020, 231-266.
- Yoon GJ. Infectious diseases and public health care examined through the COVID-19 response. Health and welfare Issue & Focus 2020, 377, 1-11.
- Lee SM; Yang SP; Kim ES; Lee MJ; Park JM; Nam DW; et al. Admission care for Bell's palsy patients: a qualitative report on patient experiences. J Acupunct Res 2013, 30, 11-23.
| Before COVID-19 | During COVID-19 | ||||
|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | ||
| Sex | |||||
| Male | 435 (48.5%) | 335 (46.8%) | 310 (44.5%) | 645 (45.6%) | |
| Female | 462 (51.5%) | 381 (53.2%) | 381 (55.5%) | 768 (54.4%) | |
| Age | |||||
| Under 20 | 42 (4.7%) | 24 (3.4%) | 22 (3.2%) | 46 (3.3%) | |
| 20s-30s | 210 (23.4%) | 191 (26.7%) | 164 (23.5%) | 355 (25.1%) | |
| 40s-50s | 362 (40.4%) | 266 (37.2%) | 242 (34.7%) | 508 (36.0%) | |
| Over 60 | 283 (31.5%) | 235 (32.8%) | 269 (38.6%) | 504 (35.7%) | |
| Lesion Site | |||||
| Left | 468 (52.2%) | 350 (48.9%) | 351 (50.4%) | 712 (50.4%) | |
| Right | 429 (47.8%) | 366 (51.1%) | 346 (49.6%) | 701 (49.6%) | |
| Before COVID-19 | During COVID-19 | |||
|---|---|---|---|---|
| 2019 | 2020 | 2021 | ||
| Fatigue and overwork | 198 (63.3%) | 184 (58.2%) | 118 (52.0%) | |
| Insomnia | 146 (46.6%) | 142 (44.9%) | 100 (44.1%) | |
| Stress | 162 (51.8%) | 156 (49.4%) | 104 (45.8%) | |
| On a diet | 12 (3.8%) | 9 (2.8%) | 8 (3.5%) | |
| Exposure to severe temperature differences | 66 (21.1%) | 43 (13.6%) | 35 (15.4%) | |
| Virus disease (ex. cold, enteritis) | 56 (17.9%) | 20 (6.3%) | 4 (1.8%) | |
| Surgery and injury | 14 (4.8%) | 9 (2.8%) | 7 (3.1%) | |
| COVID-19 vaccination | - | - | 24 (10.6%) | |
| Others | 2 (0.6%) | 6 (1.9%) | 15 (6.6%) | |
| Before COVID-19 | During COVID-19 | P-Value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Acutephase | 437 (48.7%) | 378 (52.8%) | 385 (55.2%) | 763 (54.0%) | X2=6.286 0.043 |
|
| Subacute phase | 327 (36.5%) | 243 (33.9%) | 212 (30.4%) | 455 (32.2%) | ||
| Chronic phase | 133 (14.8%) | 95 (13.3%) | 100 (14.3%) | 195 (13.8%) | ||
| Before COVID-19 | During COVID-19 | P-Value | |||||
|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | ||||
| Seoul | 481 (53. 6%) | 411 (57.4%) | 400 (57.4%) | 811 (57.4%) | X2=23.741 0.003 |
||
| Geonggi | 273 (30.4%) | 214 (29.9%) | 204 (29.3%) | 418 (29.6%) | |||
| Incheon | 32 (3.6%) | 22 (3.1%) | 23 (3.3%) | 45 (3.2%) | |||
| Ho-seo | 21 (2.3%) | 18 (2.5%) | 17 (2.4%) | 35 (2.5%) | |||
| Gwang Won | 27 (3.0%) | 17 (2.4%) | 22 (3.2%) | 39 (2.8%) | |||
| Yeongnam | 33 (3.7%) | 15 (2.1%) | 16 (2.3%) | 31 (2.2%) | |||
| Honam | 15 (1.7%) | 18 (2.5%) | 13 (1.9%) | 31 (2.2%) | |||
| Jeju | 7 (0.8%) | 1 (0.1%) | 2 (0.3%) | 3 (0.2%) | |||
| Foreign region | 8 (0. 9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |||
| Before COVID-19 | During COVID-19 | P-Value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Northeastern region | 287 (59.7%) | 275 (66.9%) | 269 (67.3%) | 544 (67.1%) | X2=23.741 0.003 |
|
| Northwestern region | 33 (6.9%) | 25 (6.1%) | 27 (6.8%) | 52 (6.4%) | ||
| Inner-city region | 30 (6.2%) | 29 (7.1%) | 25 (6.3%) | 54 (6.7%) | ||
| Southeastern region | 50 (10.4%) | 22 (5.4%) | 31 (7.6%) | 53 (6.5%) | ||
| Southwestern region | 81 (16.8%) | 60 (14. 6%) | 48 (12.0%) | 108 (13.3%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| After no treatment | 79 (8.8%) | 62 (8.7%) | 44 (6.4%) | 106 (7.5%) | X2=18.840 0.277 |
|
| After only Western Medicine treatment | 370 (41.2%) | 318 (44.4%) | 298 (42.8%) | 616 (43.6%) | ||
| After only Korean Medicine treatment | 102 (11.4%) | 77 (10.8%) | 68 (9.8%) | 145 (10.3%) | ||
| After both Western and Korean Medicine treatment | 346 (38.6%) | 259 (36.2%) | 287 (41.2%) | 546 (38.6%) | ||
| Before COVID-19 | During COVID-19 | P-value | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | Total | |||
| Only outpatient treatment | 250 (57.2%) | 246 (65.1%) | 288 (74.8%) | 534 (70.0%) | X2=23.741 0.003 |
|
| Both outpatient and inpatient treatment | 187 (42.8%) | 132 (34.9%) | 97 (25.2%) | 229 (30.0%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





