1. Introduction
The right to give birth safely is a fundamental human right [
1,
2]. Maternal mortality is a severe global health issue in Africa [
1]. According to United Nations (UN) data, around 287,000 women globally lose their lives annually due to maternal complications, amounting to roughly one death every two minutes [
3]. As defined by the World Health Organization (WHO), maternal death refers to the death of a woman during pregnancy or within 42 days of pregnancy completion due to complications or circumstances directly associated with the pregnancy [
4].
Despite worldwide interventions, preventable maternal deaths in Africa remain high, majorly caused by complications such as hemorrhage, eclampsia, sepsis, and delivery complications. HIV/AIDS often exacerbates these conditions[
5,
6]. The leading causes of maternal mortality in Africa are hemorrhage and eclampsia [
7]. Institutional delivery is vital as childbirth facilitated by trained healthcare professionals can significantly reduce maternal mortality. However, systemic issues like staffing shortages, accessibility, and service quality significantly challenge many African regions [
8,
9].
This study also explores the broader socioeconomic context of Africa by examining the effects of global events, such as the economic downturn of 2007, on maternal health outcomes [
10,
11].
The Millennium Development Goals (MDGs) aimed to achieve a 75% reduction in the maternal mortality rate (MMR) between 1990 and 2015 [
12,
13,
14,
15]. However, at a meeting in Luanda, Angola 2014, the Health Ministers of Africa acknowledged that only four African countries - Cape Verde, Equatorial Guinea, Eritrea, and Rwanda - had achieved this target [
16] The United Nations Sustainable Development Goal sets [
17] Achieving this goal requires strategic investments in healthcare infrastructure, educational enhancement, and significant policy changes [
18] These interventions should primarily focus on improving the accessibility and quality of maternal health services. Creating Maternal Health services accessible to the population is essential to reduce maternal mortality. As per the guidelines of the UN regarding emergency obstetric and neonatal care, there should be a minimum of 5 facilities providing such care for every 500,000 people. Out of these, at least one facility must be a comprehensive emergency obstetric and neonatal facility[
19]. Researchers and experts have utilized these indicators to monitor the progress of Maternal Health Services in Africa[
20,
21] and other continents[
22,
23,
24].
There is also a critical need to enhance women's access to the continuum of care, particularly post-natal care, and advocate for village-based healthcare systems to mitigate geographical barriers, thereby improving neonatal outcomes in remote areas[
25]. The present study uses data from the World Bank's public database to study the MMR trends across Africa and forecast future patterns using the ARIMA and Holt models [
26,
27]. Forecasting the MMR is crucial for policymakers, international organizations, and NGOs in planning health strategies [
28]. The findings of our study underline the urgent need for a holistic approach to improving maternal health in Africa, emphasizing data analysis, institutional delivery, and the effects of socioeconomic factors. The goal is to inspire additional research and policy discussions to help Africa progress toward achieving sustainable development goals in maternal health.
2. Materials and Methods
MMRs and population data were extracted from all African countries' World Bank mortality databases from 1990 to 2015[
17,
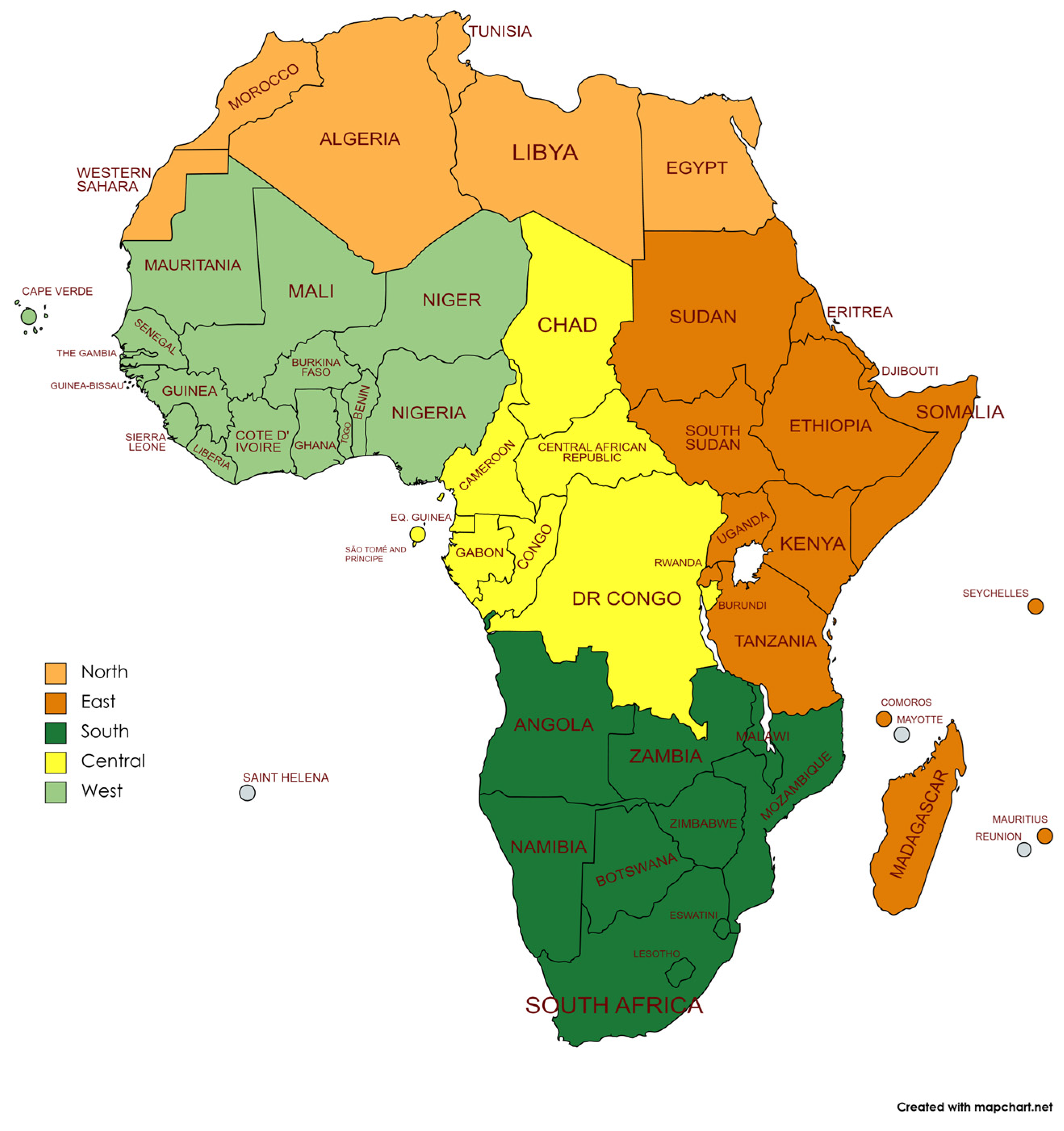
29]. Thus, we extracted the data from the database up to 2015, making it the latest year included in our analysis. We used the five regions of the African Union classification (
Figure 1)[
30,
31]. We excluded British and French territories from our analysis as they were not part of the African Union. We excluded Seychelles and Western Sahara from the analysis due to the lack of data.
The annual mortality rates for each region and Africa were estimated by weighting the region of each country's MMR with its population [
29]. The time series were evaluated for autocorrelation using the Durbin-Watson test. We used this test to evaluate two contrasting hypotheses: H0 (null hypothesis), stating that the residuals are not autocorrelated, and HA (alternative hypothesis), which suggests the existence of autocorrelation within the residuals. We performed a Joinpoint regression to detect changes in the trends. We estimated the annual percentage change (APC) to describe the magnitude of the change in each trend and calculated the 95% confidence intervals (95% CI).
We used Auto-Regressive Integrated Moving Average (ARIMA) models to predict MMR. MMR was the working variable to be forecasted. We computed separate models for each region. The ARIMA model involves three parameters, p, d, and q, where p is the model's auto-regressive (AR) part. P integrates the effect of lag value; d represents the number of differences needed for making the model stationary, and q is the moving average (MA) of the number of lagged forecast errors in the prediction equation[
32,
33]. We used Autocorrelation (ACF) and Partial Autocorrelation (PACF) graphs to check autocorrelation. We used the Bayesian Information Criteria (BIC) to select the best model. Finally, we applied the McLeod–Li test to check the stationarity of the model residuals. We first checked the stationarity of the data from 1990 onwards. After confirming stationarity, we used the autocorrelation function (ACF) and partial autocorrelation function (PACF) plots to determine appropriate values for the autoregressive (p) and moving average (q) components of the ARIMA model. We then fit the ARIMA model to the data and checked the residuals to ensure they were white noise.
We also used the Holt Exponential Smoothing method to forecast African maternal mortality trends [
34]. This method offers an approach for time series forecasting that considers both the level and the trend, making it particularly suitable for trends with non-stationary data. The model's appropriateness was assessed by scrutinizing the diagnostic results of residuals and determining the mean absolute percentage error (MAPE). The final model was then used to forecast the future maternal mortality trends in Africa.
We performed the computations using IBM SPSS v17 and Joinpoint Regression Program, Version 4.9.0.1, February 2022, from the Statistical Research and Applications Branch, National Cancer Institute of the United States. The Holt forecasting was performed in R (version 4.1.0) using the 'forecast' package (version 8.21)[
36,
37].
In this study, when 'Africa' is used alone, it refers to the entire African continent, including all associated islands, notably Madagascar and Cape Verde. However, when accompanied by directional terms such as 'North,' 'South,' 'East,' 'Central,' and 'West,' the term refers to the specific regions within the continent.
3. Results
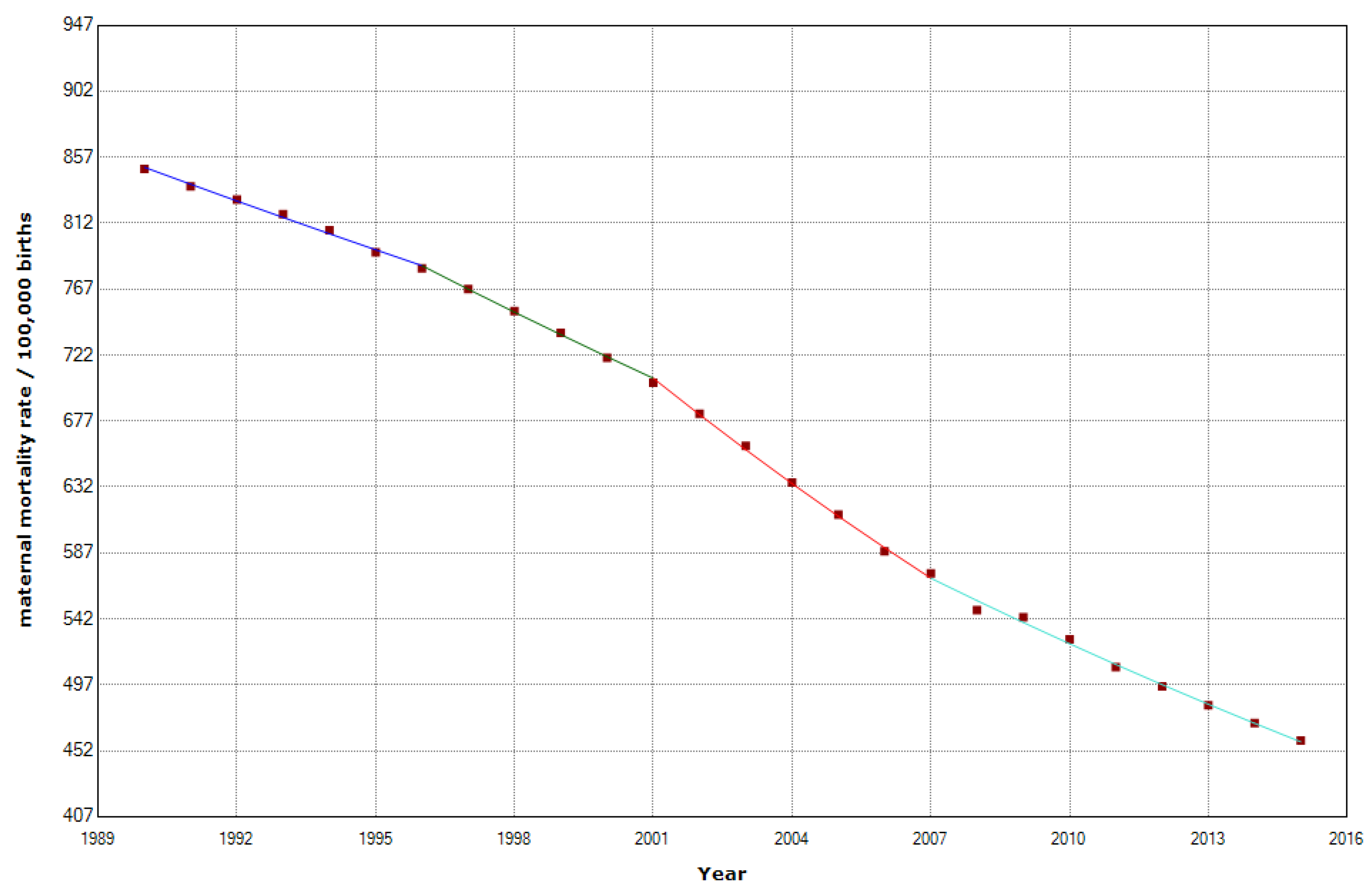
MMR declined from 788 deaths per 100,000 births in 1990 to 392 deaths per 100,000 births in 2015. (
Figure 2) However, 205,670 women still died in Africa in 2015. Most maternal deaths (203,000) occurred in sub-Saharan Africa [
17]. We have identified three join points in 1996, 2001, and 2007, indicating the presence of four distinct phases characterized by significant shifts in the maternal mortality trend.
Table 1 shows that there was a significant decline in MMR by a significant APC (−2.6%) (p < 0.001). In the first period, 1990-1996, a slight decrease with an APC of -1.4%. A series of stages followed in which the APC reduction of maternal mortality rates was progressively higher and higher. The accelerated trend was interrupted in 2007 when there was a slowdown in the APC. APC changed from -3.5% in 2001-2007 to -2.1% in 2007-2015.
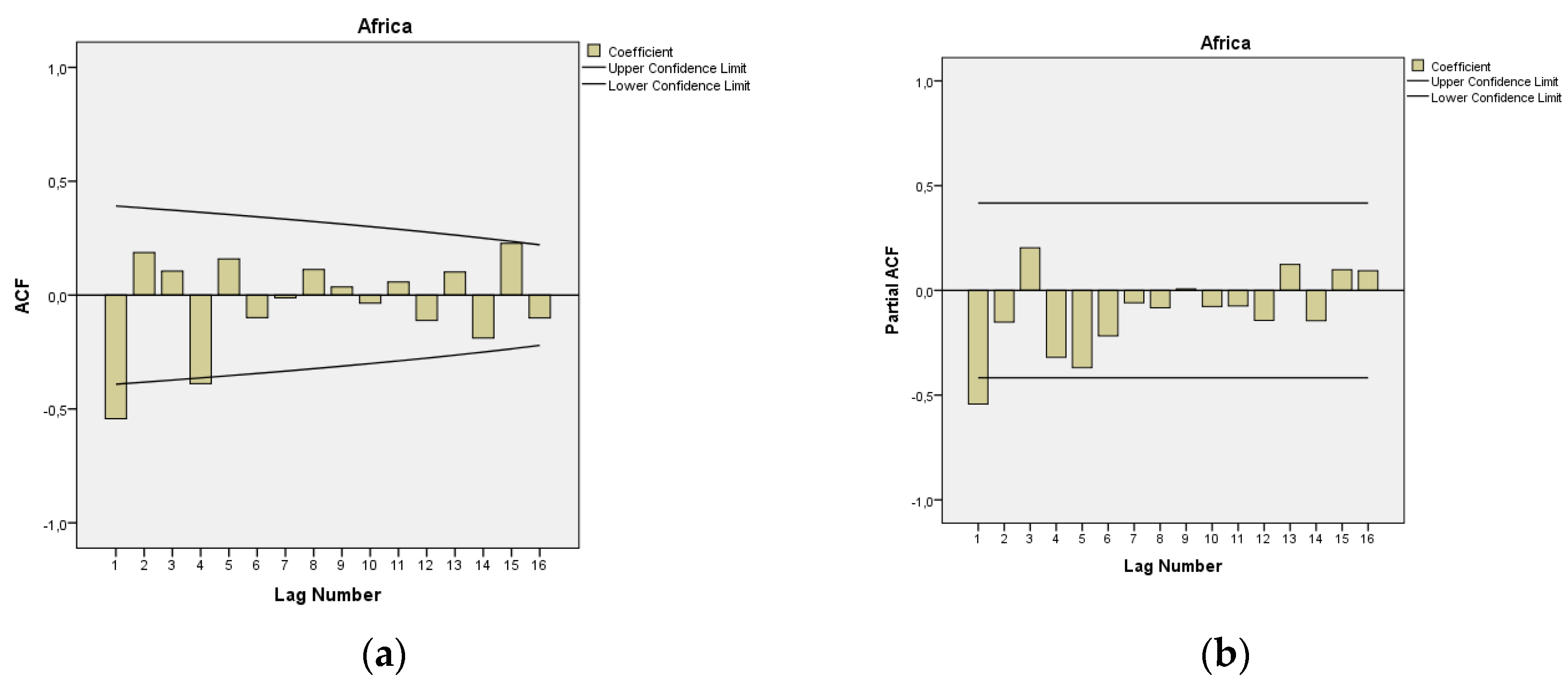
In
Figure 3, we present ACF and PACF of the temporal series of MMR in Africa. The ARIMA model of MMR in Africa was ARIMA (1,1,1). In the ARIMA model, the value of the Stationary R-squared was 0.277, and the normalized Bayesian information criterion (BIC) was 3.662.
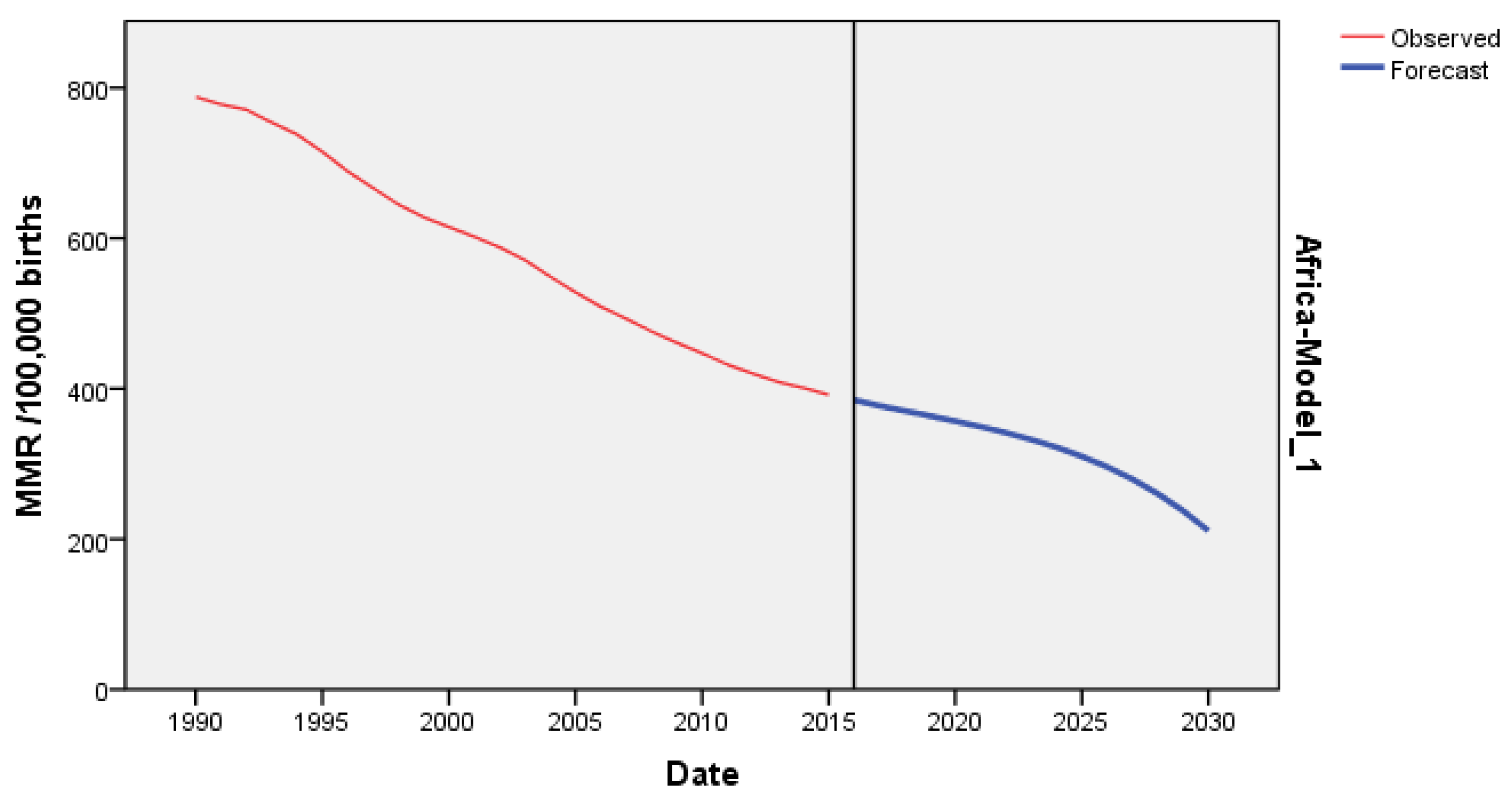
In
Figure 4, we present the forecasting of MMR for Africa till 2030. The predicted forecast of MMR in Africa for 2030 was 197 deaths per 100,000 births.
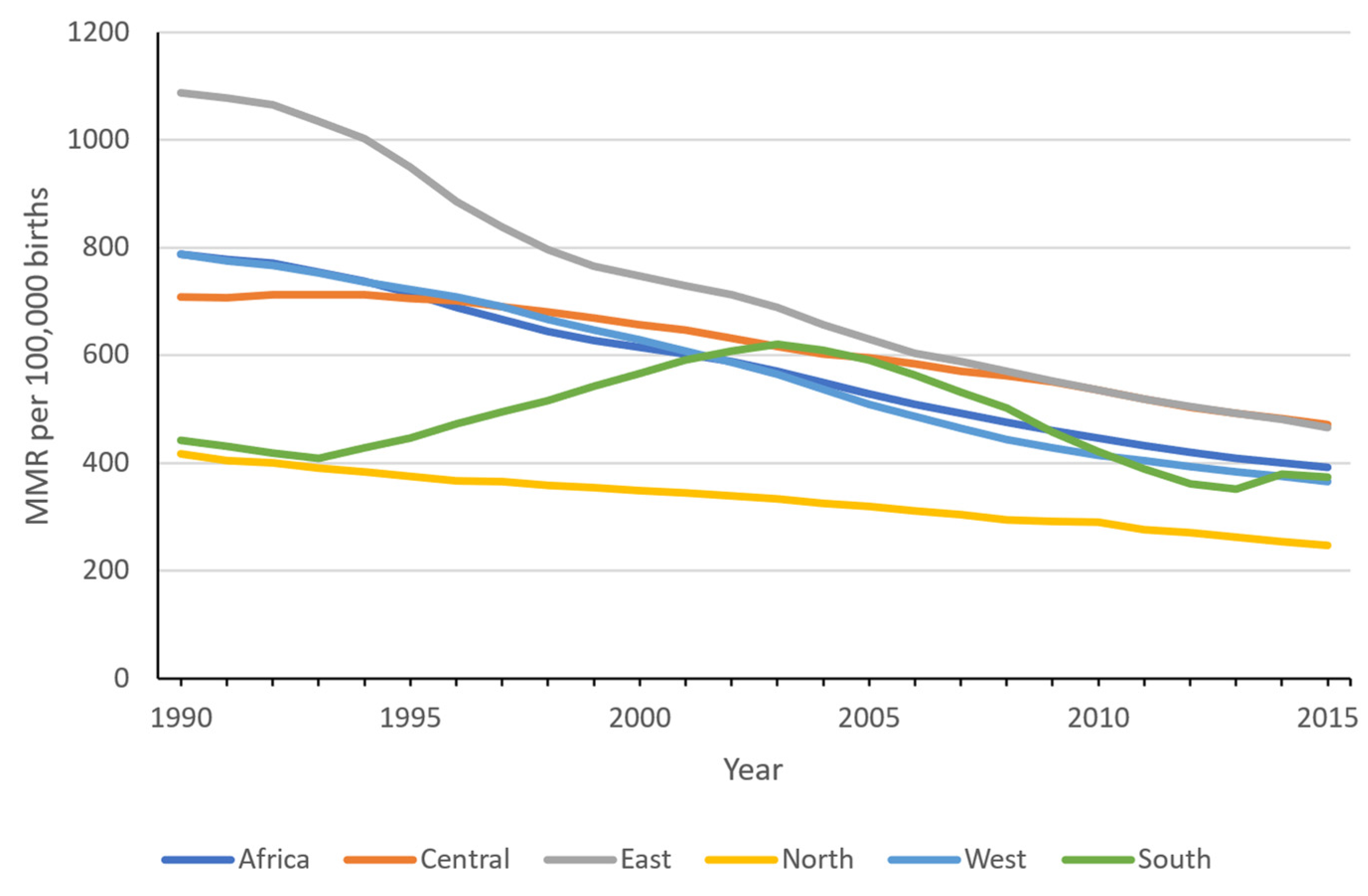
According to
Figure 5, there has been a noticeable change in the regional Maternal Mortality Ratio (MMR) over time. The gap between the regions with the highest and lowest MMR experienced a decline from 670 per 100,000 births in 1990 to 224 in 2015, indicating a reduction in interregional disparities as time progressed.
North and South Africa regions consistently remain with lower MMR throughout the period. There has been a convergence between Central and West Africa. Finally, the East African region, which started with extremely high levels, has experienced a sharp decline. Its rates tend to converge with those of the Southern Africa region.
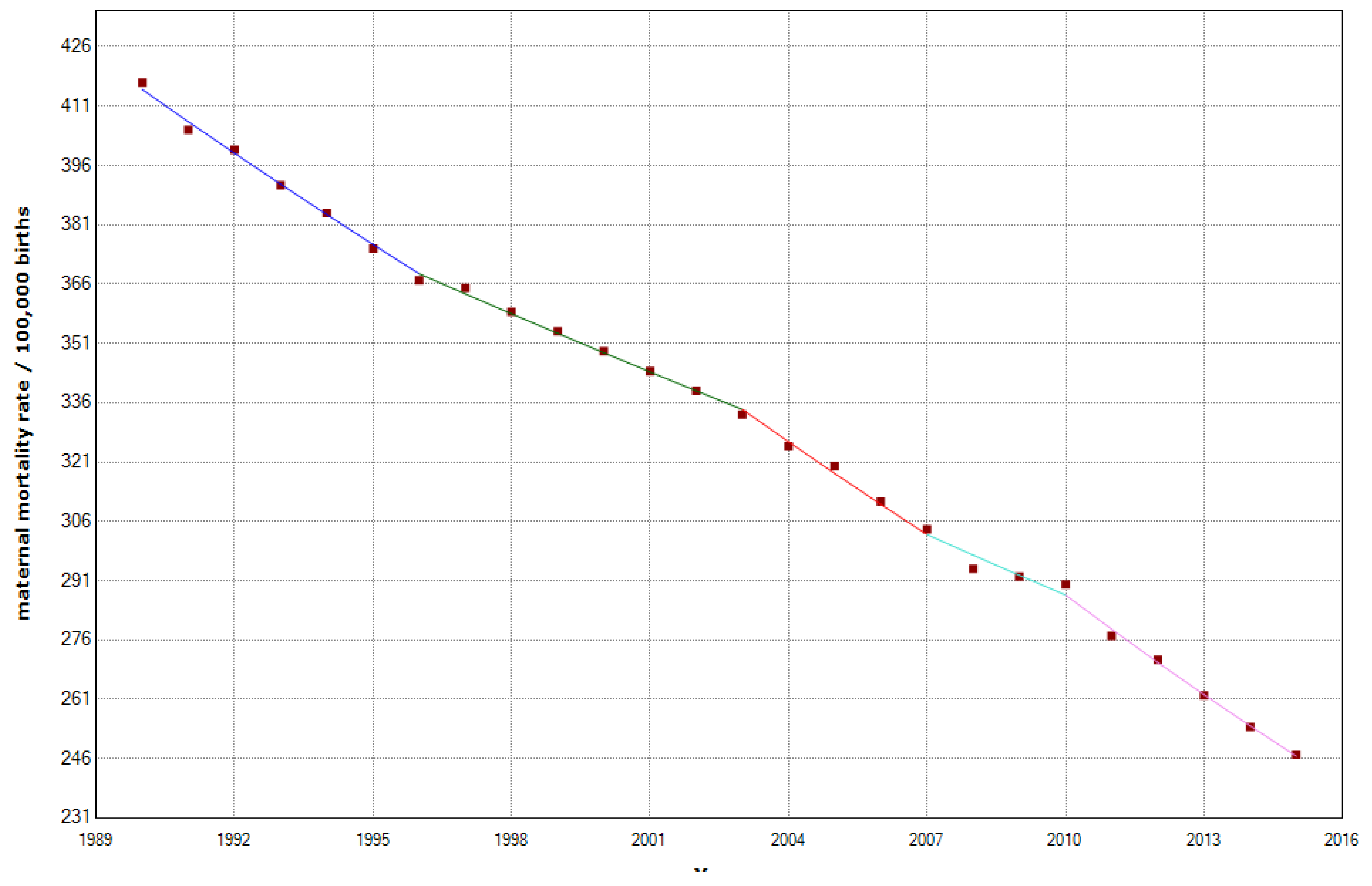
3.1. North Africa
The overall MMR decreased from 417 to 247 per 100,000 births in North Africa, which is a decrease of 40.8%. We recorded a statistically significant decrease in the MMR, with an APC of –1.9% (95% CI -2.0; -1.8). We detected four joinpoints in 1996, 2003, 2007, and 2010 (
Table 2,
Figure 6).
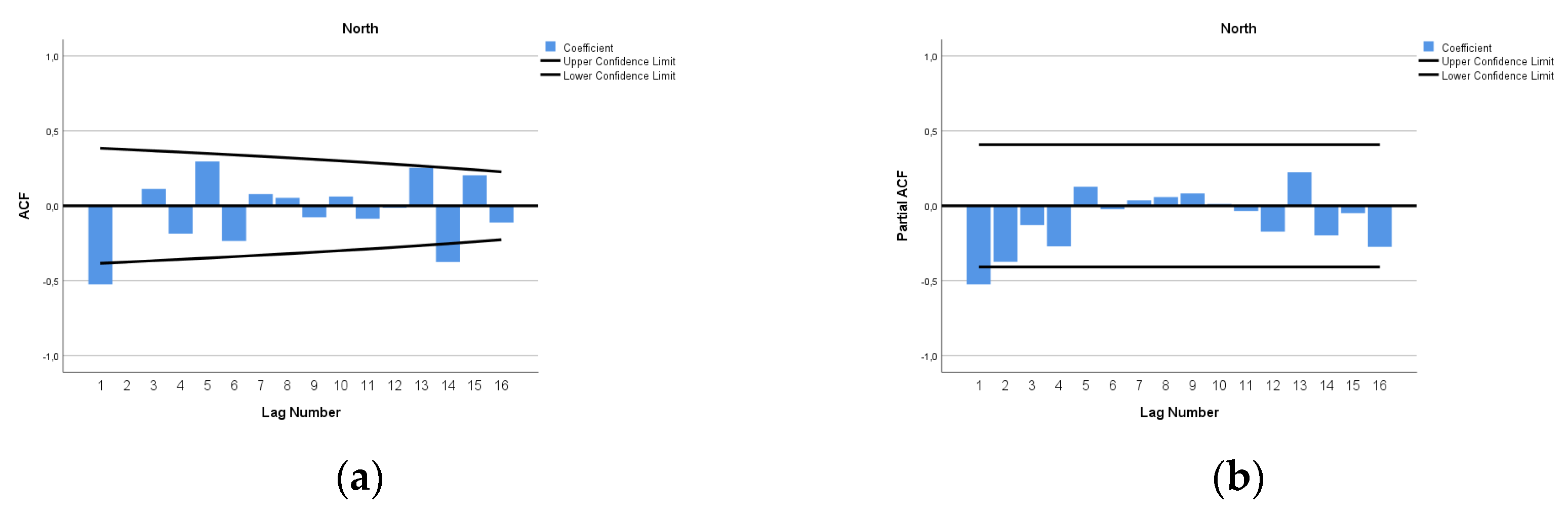
The ARIMA model of MMR in North Africa was (1,2,0). In
Figure 7, we present ACF and PACF of the temporal series of MMR in North Africa. In the ARIMA model, the value of the Stationary R-squared was 0.289, an R-squared of 0.994, and the normalized Bayesian information criterion (BIC) was 3.037.
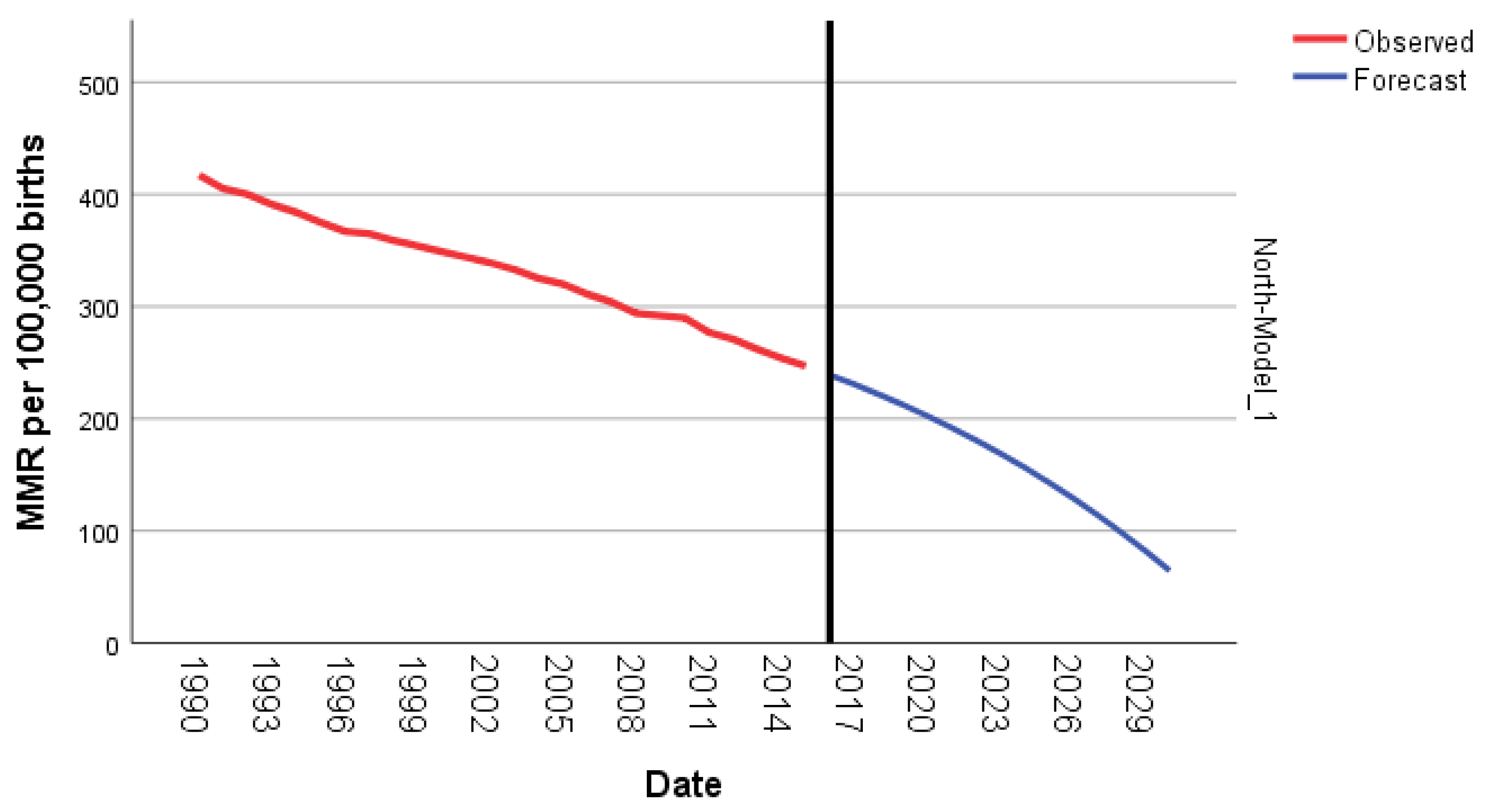
The predicted forecast of MMR in North Africa in 2030 is 65 deaths per 100,000 births. (
Figure 8)
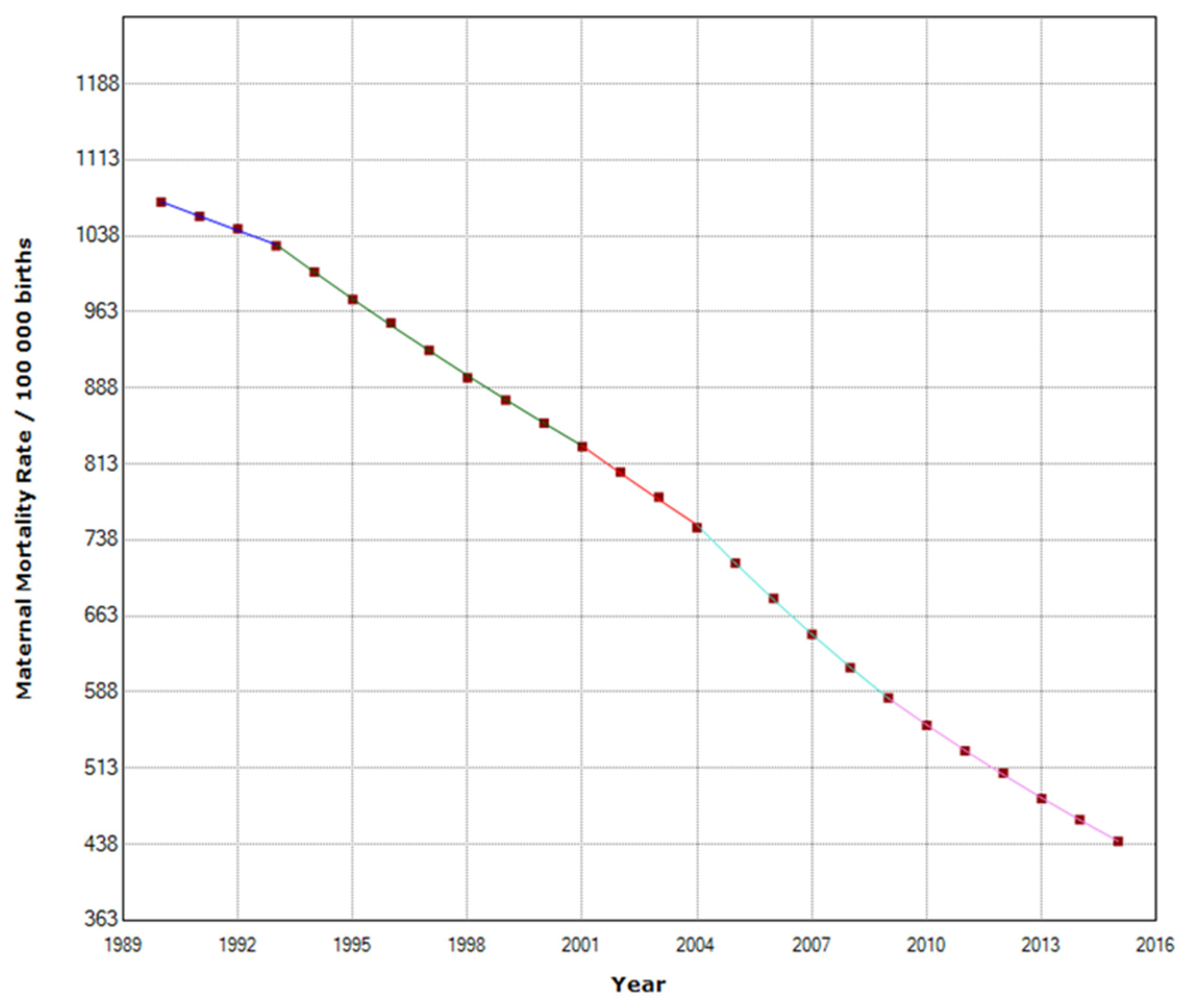
3.2. East Africa
In East Africa, MMR decreased from 1087 to 466 maternal deaths per 100,000 births (
Table 2). East Africa was the region with the highest decrease during the study period. MMR was reduced by 57.1%. Maternal mortality decreased annually by 3.6%, with four join points in 1993, 2001, 2004, and 2009. (
Figure 9)
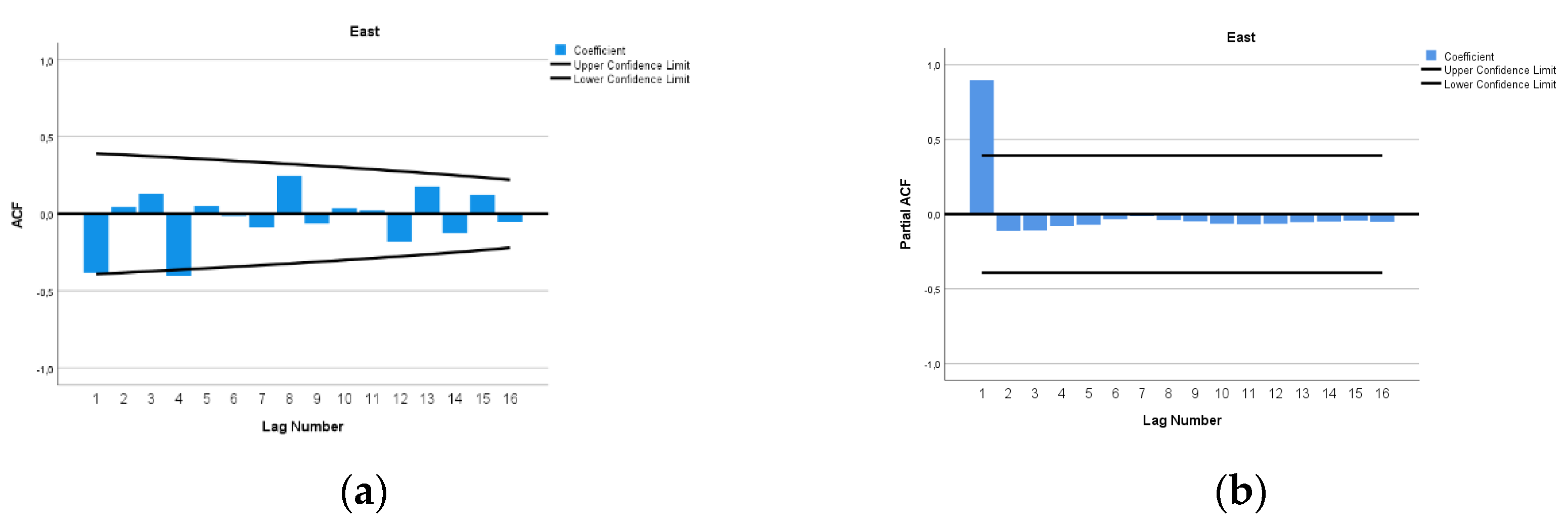
The ARIMA model of MMR in East Africa was (1,3,0). In
Figure 10, we present ACF and PACF of the temporal series of MMR in North Africa. In the ARIMA model, the value of the Stationary R-squared was 0.148, an R-squared of 0.997, and the normalized Bayesian information criterion (BIC) was 4.696.
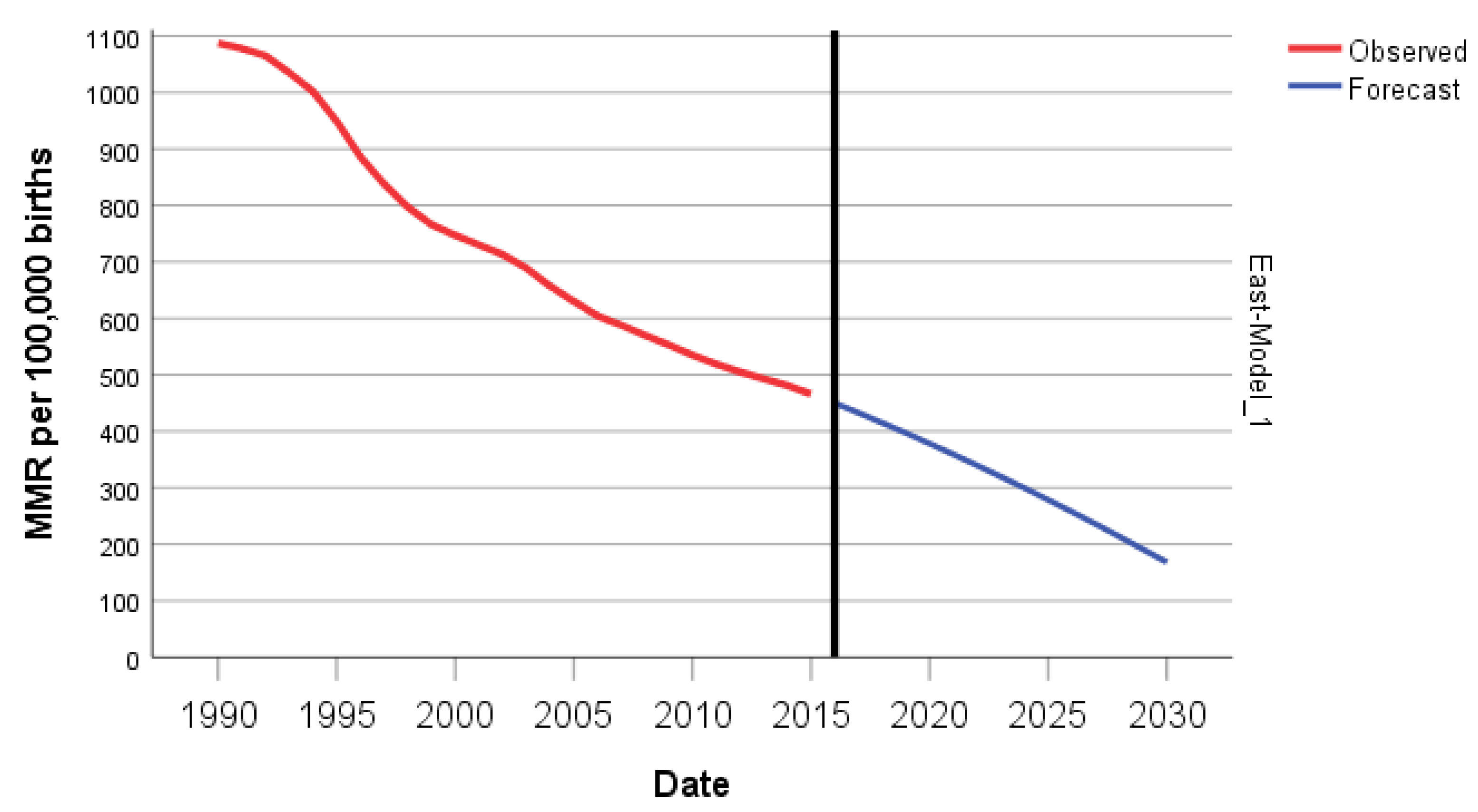
The predicted forecast of MMR in East Africa in 2030 is 168 deaths per 100,000 births. (
Figure 11)
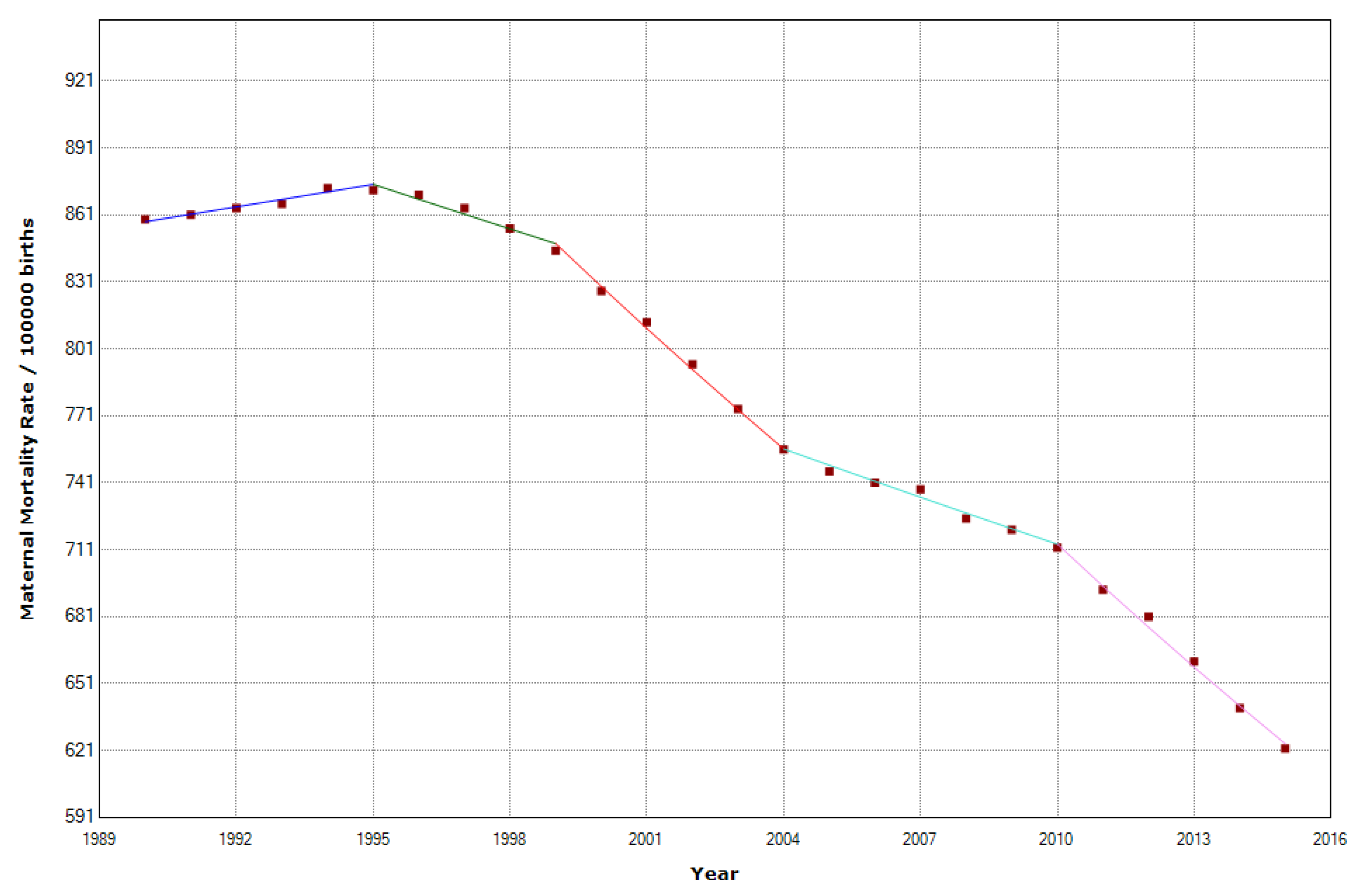
3.3. Central Africa
In Central Africa, there was a reduction of 33.5% in MMR, which moved from 708 in 1990 to 471 in 2015. The JoinPoint regression shows that in the Central African Region, there were four joinpoints. (
Table 2) From 1990-1995, maternal mortality increased by 0.4% per year; from 1995-1999, the MMR began to decline with an APC of -0.8%. After that, during 1999-2004, the APC accelerated with an APC of -2.3%. The decline slowed in 2004-2010 with an APC of -1% and accelerated again in 2010-2015 with an APC of -2.6%. (
Figure 12)
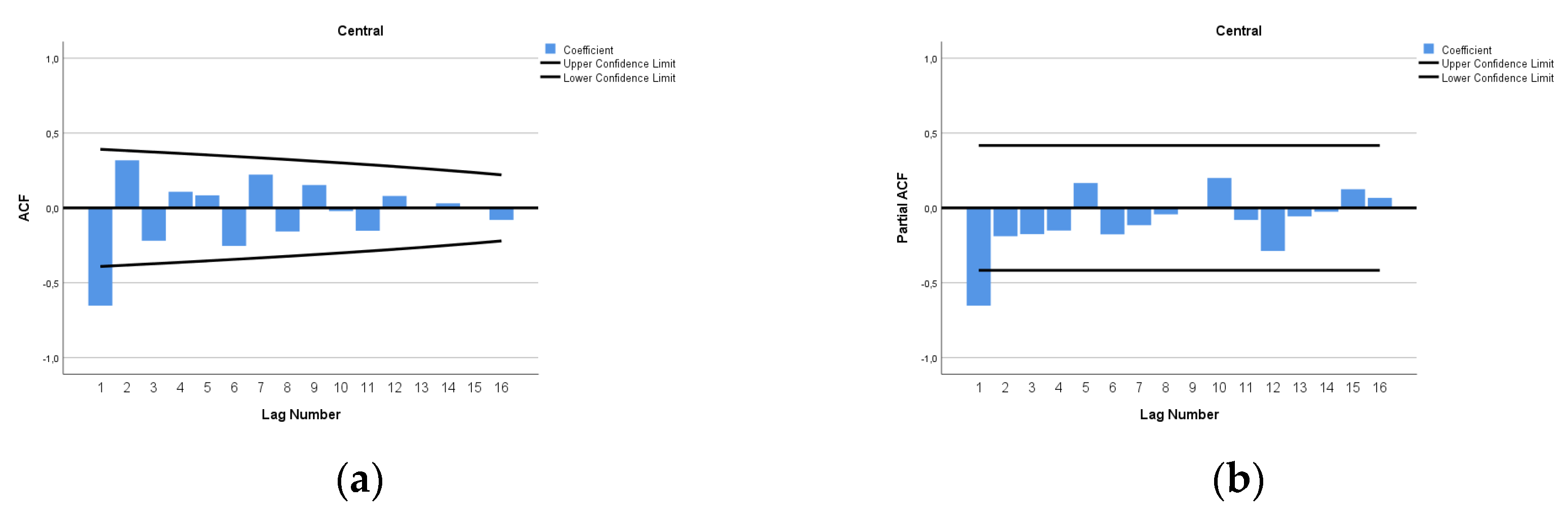
The ARIMA model of MMR in Central Africa was (1,2,0). In
Figure 13, we present ACF and PACF of the temporal series of MMR in Central Africa. In the ARIMA model, the value of the Stationary R-squared was 0.145, an R-squared of 0.998, and the normalized Bayesian information criterion (BIC) was 2.925.
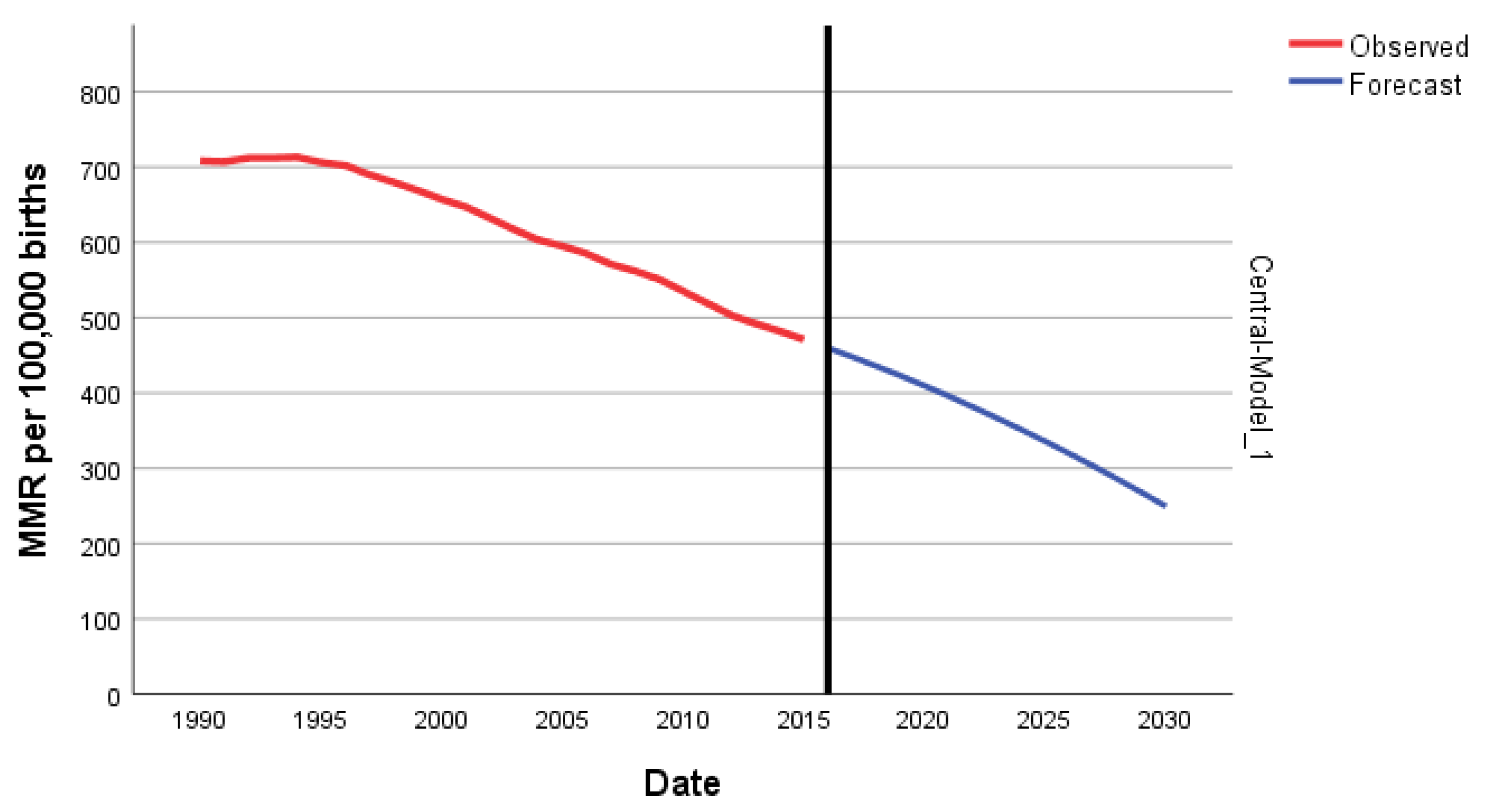
The predicted forecast of MMR in Central Africa in 2030 is 249 deaths per 100,000 births. (
Figure 14)
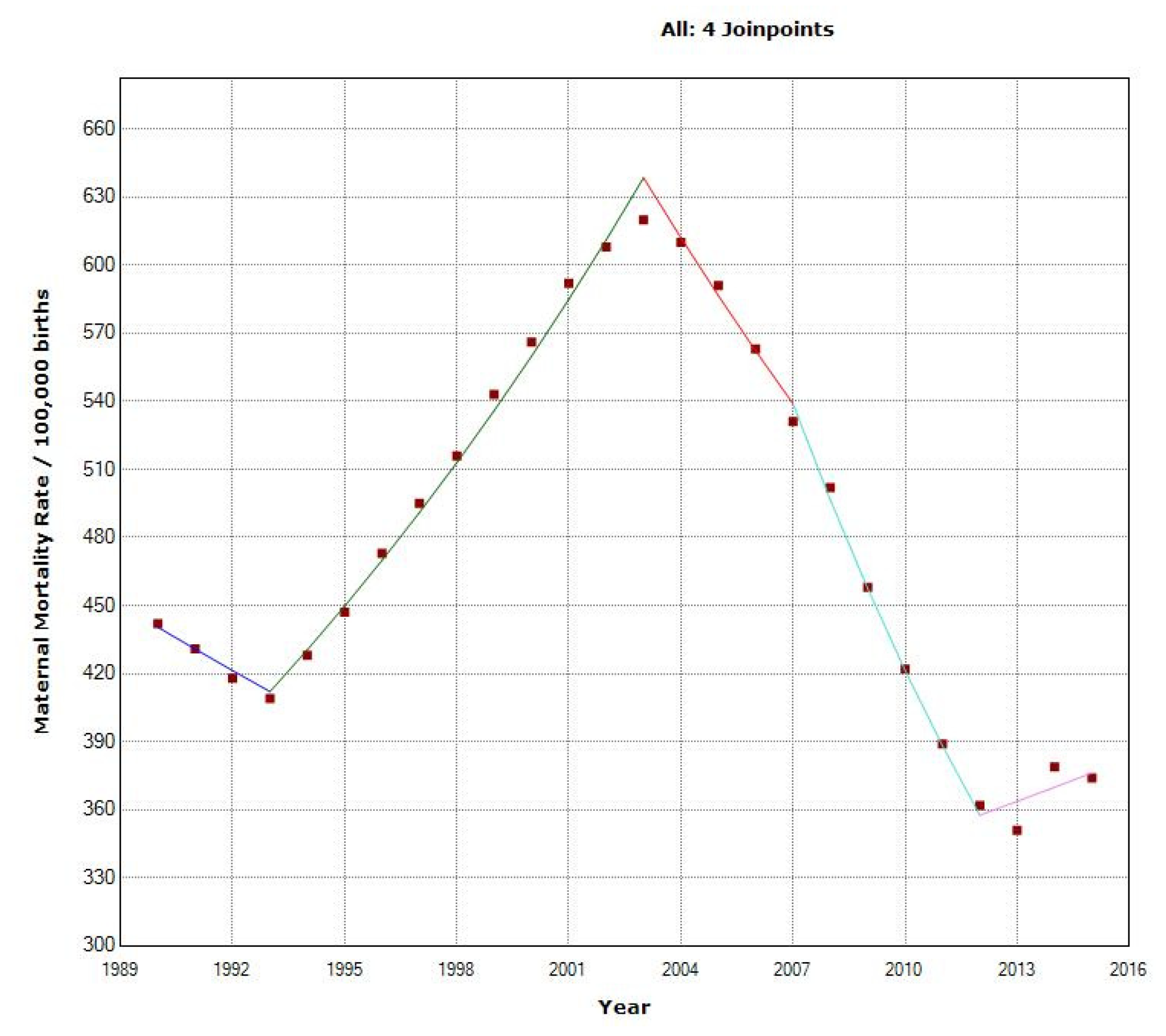
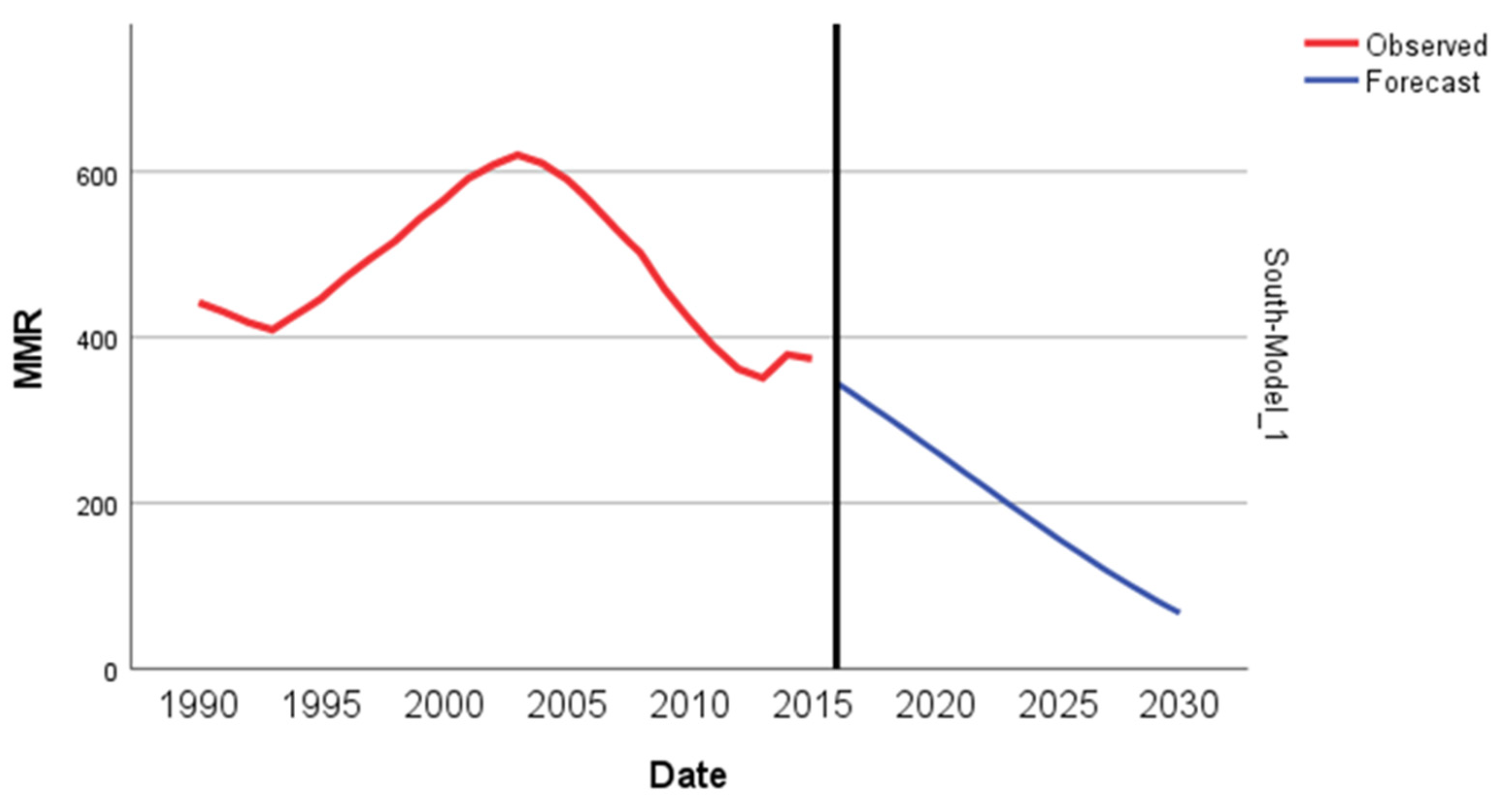
3.4 South Africa
The overall MMR decreased in the South African Region from 442 to 374 per 100,000. We recorded a -statistically significant decrease of –0.6% in the MMR, with four joinpoints in 1993, 2003, 2007, and 2012. (
Figure 15) In 1990-93, MMR decreased with an APC of -2.2%, then in the second period, 1993-2003, MMR increased, with an APC of 4,5%. Finally, in 2003-2007, back to an APC of -4.1%, and the period 2007-2012, with a high APC decrease of -7.9%, this is the highest period regional decrease detected in this study.
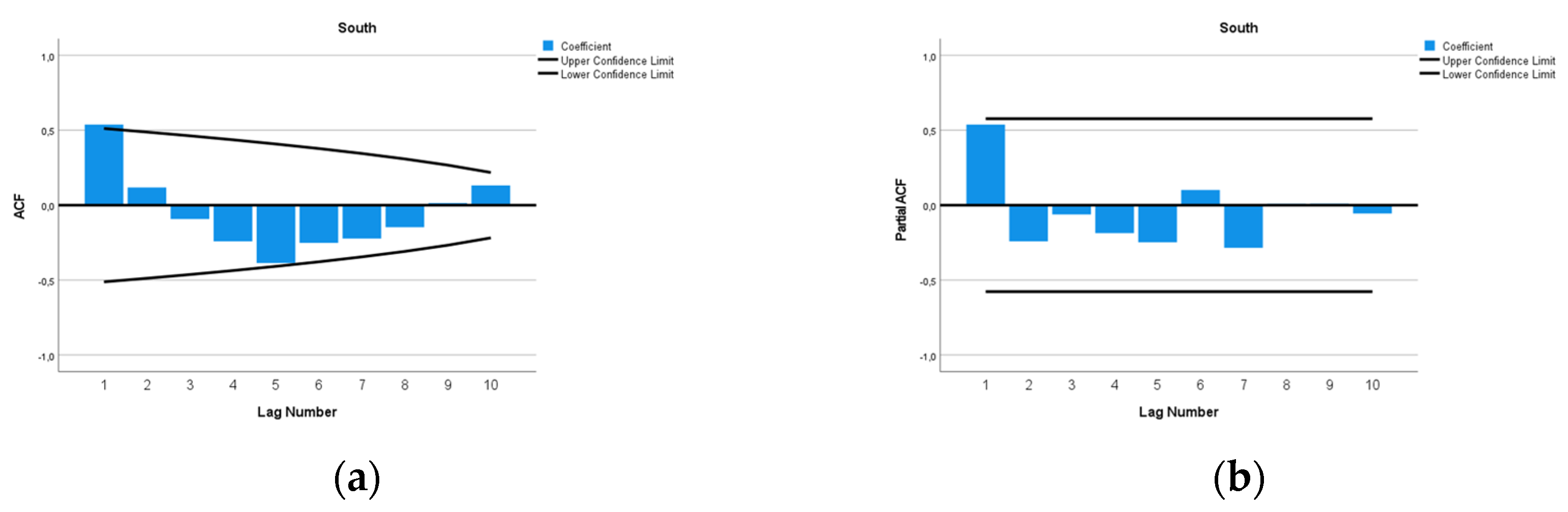
The ARIMA model of MMR in the South Africa region was ARIMA (0,1,1). This study analyzed the Maternal Mortality Rates (MMR) in South Africa from 1990 to 2015. The data exhibited a distinct pattern, with MMR increasing from 442 per 100,000 live births in 1990 to a peak of 620 per 100,000 live births in 2003. After 2003, the MMR decreased, reaching 374 per 100,000 live births in 2015. Given the observed 'V' pattern in the data, with a vertex in 2003, we decided to fit ARIMA models using data from 2003 onwards. The decision to make this estimation was grounded on the notable structural change observed in the data around 2003, indicating a shift in the dynamics of the MMR. We used a square root transformation of the data for a better fit. In
Figure 16, we present ACF and PACF of the temporal series of MMR in South Africa. In the ARIMA model, the value of the Stationary R-squared was 0.525, an R-squared of 0.966, and the normalized Bayesian information criterion (BIC) was 6.015.
The predicted forecast of MMR in the South Africa Region in 2030 is 67 deaths per 100,000 births. (
Figure 17)
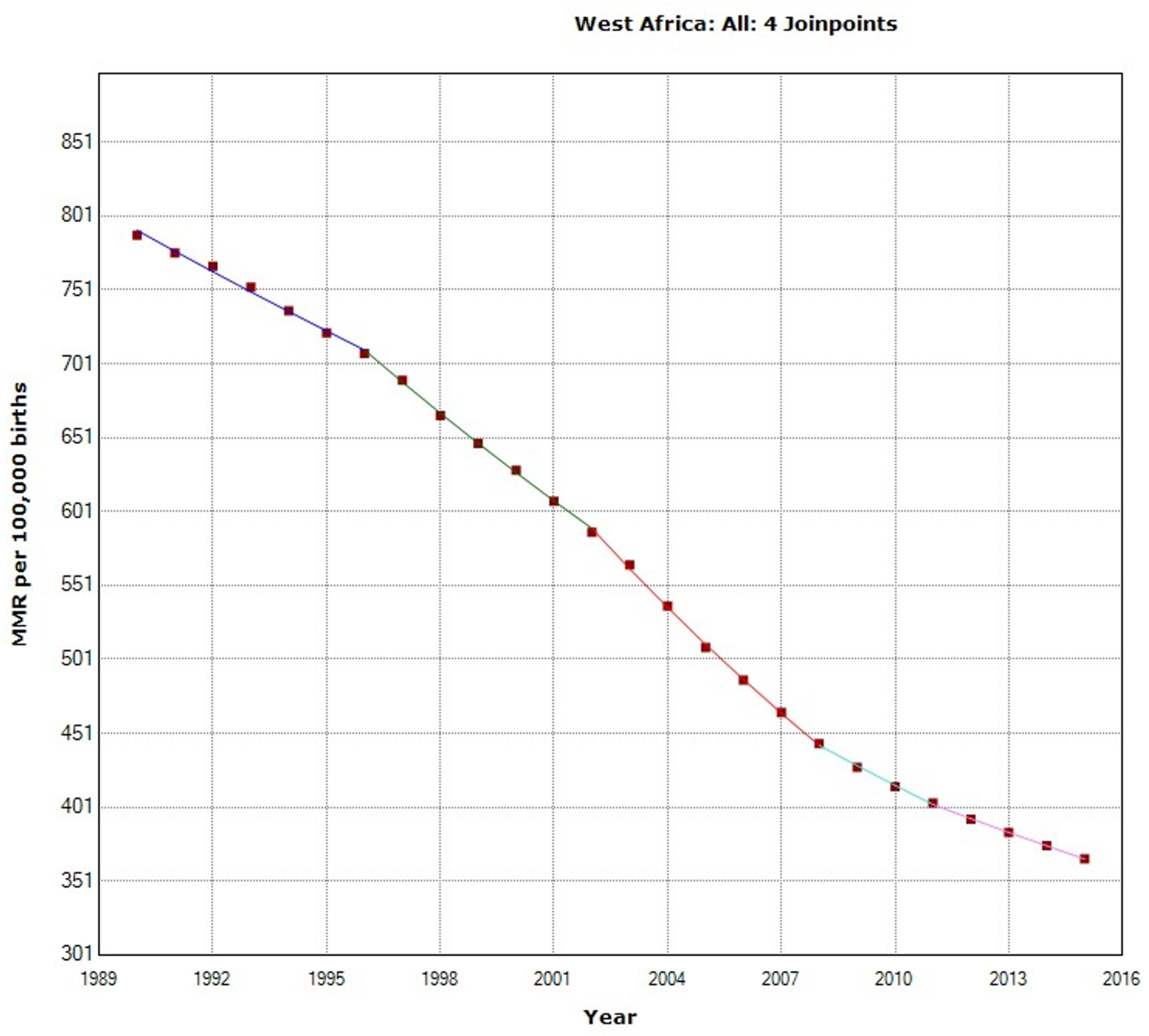
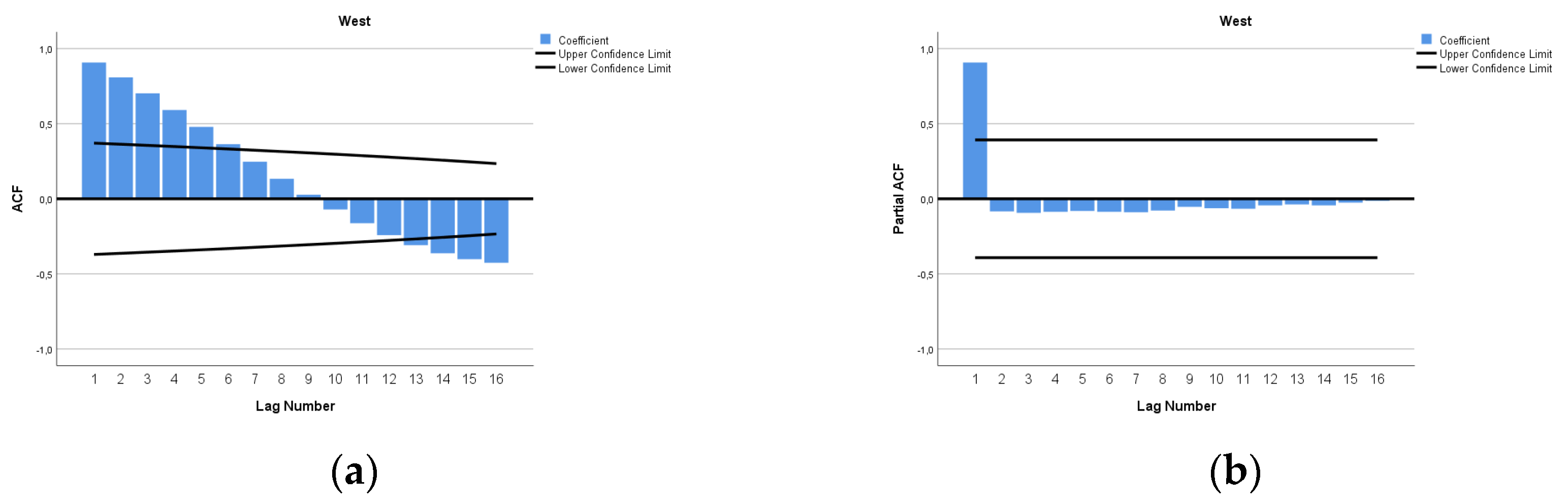
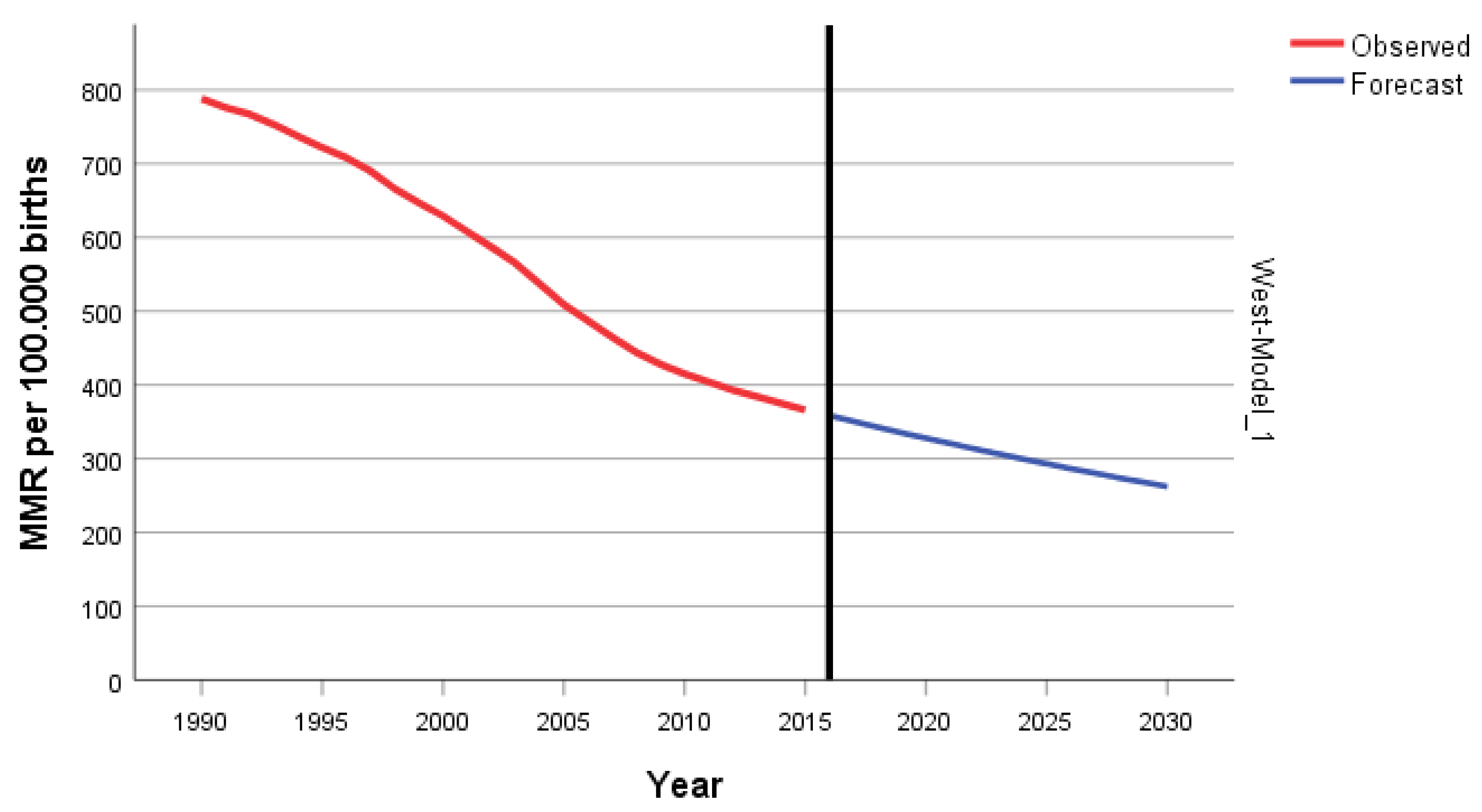
3.5. West Africa
In the West Africa Region, the overall MMR decreased by 53.6% from 788 to 366 during 1995-2015. We documented a statistically significant decrease in the MMR, with an APC of –2.6%, with four joinpoints in 1996,2002, 2008, and 2011 (
Figure 18).
The ARIMA Model for forecasting MMR in West Africa was ARIMA (1,2,3). In
Figure 19, we present ACF and PACF of the temporal series of MMR in North Africa. In the ARIMA model, the value of the Stationary R-squared was 0.226, an R-squared of 1, and the normalized Bayesian information criterion (BIC) was 2.952.
The predicted forecast of MMR in the West Africa Region in 2030 is 262 deaths per 100,000 births. (
Figure 20)
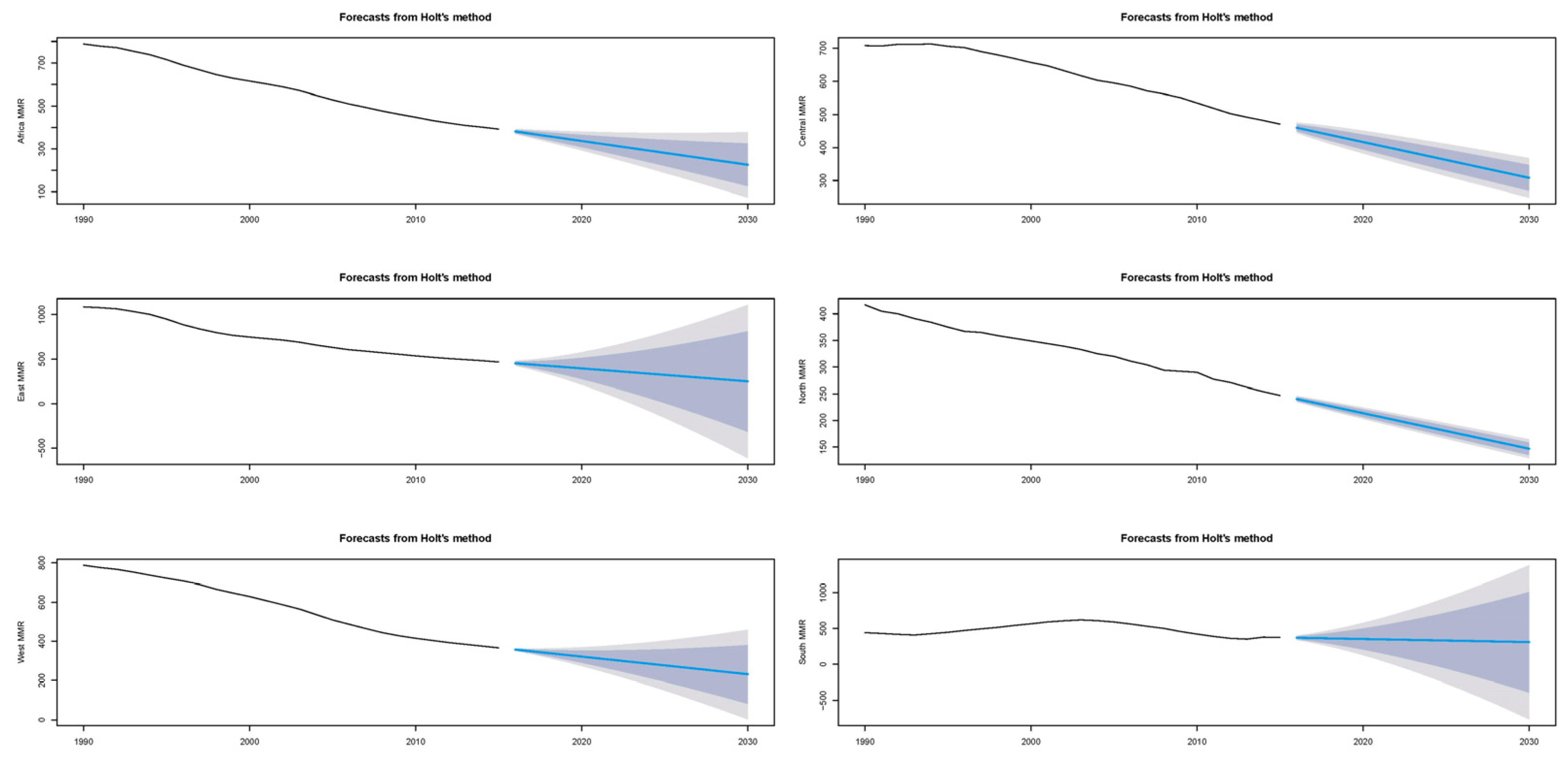
3.6. Holt forecasting.
We also performed forecasting by the Holt method (
Figure 21). The Holt Methods estimations are more conservative than those of ARIMA. The Holt Exponential Smoothing method forecasts MMR in Africa for 2030 as follows: According to our analysis, we expect the MMR for Africa to be 225 deaths per 100,000 births, accompanied by a Mean Absolute Percentage Error (MAPE) of 0.557.with a MAPE of 0.557; in Central Africa, an MMR of 308 and MAPE of 0.425; in East Africa, an MMR of 249 and MAPE of 0.766; in North Africa, an MMR of 147 and MAPE of 0.701; in West Africa, an MMR of 231 and MAPE of 0.394; and in South Africa, an MMR of 310 and MAPE of 2.361.
4. Discussion
Africa is the Region with the largest maternal mortality rate in the world, but the Region lacks accurate data. Researchers have employed various methods to estimate maternal mortality in Africa[
38]. However, the heterogeneity of these methods affects the results and makes it difficult to compare them.
Reproductive age mortality survey (RAMOS) studies combining data from institutional records and communities produced the most reliable national maternal mortality estimates. Many Subsaharian African countries rely on various surveys and census methods, such as Multiple Indicator Cluster Surveys, Demographic and Health Surveys, and population census, to estimate their MMR [
39]. The Data from international standardized sources may differ from some values collected at the national level via the routine data collection system[
40]. Nevertheless, we used this data because it was derived from standard and validated methodologies [
41]. The global African maternal mortality rate presented in our study, 392 per 100,000, is within the range of a meta-analysis conducted with studies published in Africa between 496 per 100,000 births (95% CI 216-776) [
42]. We have computed an estimation using the ARIMA and the Holt. MAPE measures the prediction accuracy of a forecasting method in statistics. It expresses the average absolute percent difference between actual and predicted values, with lower values indicating better model accuracy. In our results, the MAPE values vary across regions and are very high. Generally, a MAPE value of less than 10% is considered excellent, between 10 and 20% is good, and above 20% may indicate a less reliable model. The Holt Exponential Smoothing model appears to have a relatively high error in its MMR predictions for the specified regions; therefore, the ARIMA model is preferable.
This study's 25-year dataset provides a robust basis for projecting trends 15 years into the future, capitalizing on the ARIMA model's ability to detect long-term patterns [
43]. The limited time points, albeit fewer than recommendations of 50 to 100 observations [
44,
45], reflect an intentional balance to prioritize data relevance over volume, given the potential for substantial shifts and resulting noise in the underlying process. Starting from an earlier year, like 1965, would incorporate a period of effective decolonization in Africa, which could compromise future predictions. The lack of seasonality in the data aids models fitting, although multiple inflection points detected by Joinpoint analysis signify non-stationarity, requiring careful application of the ARIMA model. The 15-year forecast period comes with compounded errors and increased uncertainty, exacerbated by the potential for unanticipated structural changes. Such factors emphasize the need for a cautious interpretation of long-term forecasts, periodic re-evaluations, and confidence interval incorporation to gauge uncertainty[
46]. Additionally, integrating techniques like scenario planning or expert forecasting could enhance ARIMA's inherent limitations in addressing potential future events or changes.
Since the economic crisis 2007, we have observed a decline in maternal Mortality in Africa. We noted the diminishing reduction in the Northern, Central, and Western regions. The economic crisis impacted the East region but left the South region unscathed. As an integral component of the SDGs in 2015, the United Nations aimed to reduce the MMR to 70 out of every 100,000 live births by 2030. According to our forecasting, the only region that will reach the target will be North Africa. Reducing maternal deaths is among the most challenging SDG targets because Africa would need an 86 percent reduction in MMR, which is unrealistic given the present rate of decline [
41].
Institutional delivery, which refers to childbirth facilitated by trained healthcare professionals following safe and sterile protocols, is crucial to maternal health. Enhancing maternal understanding, perspective, and utilization of institutional delivery contributes significantly to decreasing maternal mortality and morbidity rates [
47]. In Africa, where many regions face considerable challenges in emergency obstetric care, the emphasis on institutional delivery becomes even more critical because there are widespread systemic issues in emergency obstetric care across Africa.
In South Africa, several studies have shown that in regions grappling with significant challenges in emergency obstetric care, the focus on institutional delivery is paramount due to prevalent systemic issues. Overburdened healthcare providers, notable personnel shortages, and problems with service delivery and infrastructure typify these issues. Compounded by limited access to vital resources such as operating theaters, intensive care units, and reliable emergency transport services, these challenges significantly amplify the risk of severe maternal outcomes. These circumstances underline systemic weaknesses, emphasizing the need for improvements in service coordination, staffing, performance indicators, and overall funding. [
48] Despite national policy guidelines advocating for decentralizing emergency obstetric care to Community Health Centers, services were centralized in hospitals to ensure patient safety[
49]. The use of comprehensive emergency obstetric and newborn care is related to waiting time for service and women's educational level [
49,
50]. That could suggest that improving women's education may increase the utilization of comprehensive emergency obstetric services. Therefore, future assessments of emergency obstetric care availability should consider facility opening hours, capacity, staffing, and the proven performance of essential functions rather than merely the venue of service provision. On the other hand, enhancing male education, improving wealth distribution, ensuring access to health facilities, promoting post-natal care, and improving the quality of antenatal and maternity care services could significantly increase the utilization of skilled delivery services in rural areas[
39]. In Uganda, unmarried and married youth who frequently attend antenatal care visits and attain higher education demonstrate increased utilization of health facilities during childbirth. [
39]. Conversely, health facility usage negatively correlates with higher parity, rural residence, and employment in the agriculture sector. In order to encourage the use of health facilities among youth, it is essential to promote regular antenatal care attendance, particularly for those with multiple children residing in rural areas. Policies should focus on improving access to mass media, enhancing youth education, and addressing economic disparities.
The African Union Summit in 2019 decided to increase domestic health resources.[
51] African countries are gradually increasing domestic health investments, with 35 of 55 African Union Member States (more than 64%) increasing the percentage of their GDP invested in health over the previous fiscal year. Out of the 55 member states in the African Union (AU), just two countries have successfully achieved Africa's objective of allocating a minimum of 15% of their government budget towards healthcare. However, these countries still fail to reach the recommended threshold of US
$86.30 per person, which is necessary to offer essential health services.[
51,
52,
53] Africa must financially commit to its health. The African Ministries of Health conference in Luanda 2014 emphasized the importance of improved transportation, communication technologies, effective community participation, and men's involvement in improving maternal health. They also emphasized the importance of investing in the development of human resources for health and the importance of adolescent health in the survival of mothers[
16].
The impact of the COVID-19 pandemic appears to pose substantial challenges to maternal health, particularly in Africa. Although detailed data is forthcoming, early indications suggest that the pandemic has significantly impacted maternal and child healthcare[
54]. The limited availability of skilled health professionals and medical equipment, service disruptions, and an increased reluctance among women to use available healthcare facilities contribute to this impact.[
55,
56]. Despite the absence of specific statistics on the pandemic's effects on maternal mortality, studies conducted in countries like Guinea, Nigeria, Tanzania, and Uganda hint at a decline in critical maternal and child health services, particularly in antenatal, intrapartum, and post-natal care [
57] This decline could potentially hinder progress toward reducing maternal mortality rates, posing a threat to achieving the related Sustainable Development Goal (SDG).
Author Contributions
Conceptualization, LO, FGG, and IAO; methodology, SGA, WOL, LGA, FGG; software, FGG.; validation, RAB, IAO; formal analysis, LO, WOL; investigation, LO, FGG, IAO; Data curation, LO, SGA; LGA, RAB, writing—original draft preparation, LO, WOL, SGA, RAB, LGA, FGG, IAO.RM; writing—review and editing, LO, WOL, SGA, RAB, RM, LGA, EAO, FGG, IAO; visualization, LO, WOL, SGA, RAB, LGA, EAO, FGG, IAO supervision, FGG, EAO, IAO. All authors have reviewed the manuscript in its published form and have provided their consent.
Figure 1.
Regions of the African Union, according to the African Union classification.
Figure 1.
Regions of the African Union, according to the African Union classification.
Figure 2.
Maternal Mortality trends in Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 2.
Maternal Mortality trends in Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 3.
Maternal Mortality in Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 3.
Maternal Mortality in Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 4.
Evolution and forecasting of MMR in Africa.
Figure 4.
Evolution and forecasting of MMR in Africa.
Figure 5.
Evolution of regional maternal Mortality rates (1990-2015).
Figure 5.
Evolution of regional maternal Mortality rates (1990-2015).
Figure 6.
Maternal mortality trends in North Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 6.
Maternal mortality trends in North Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 7.
Maternal Mortality in North Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 7.
Maternal Mortality in North Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 8.
Evolution and forecasting of MMR in North Africa.
Figure 8.
Evolution and forecasting of MMR in North Africa.
Figure 9.
Maternal mortality trends in East Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 9.
Maternal mortality trends in East Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 10.
Maternal Mortality in East Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 10.
Maternal Mortality in East Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 11.
Evolution and forecasting of MMR in East Africa.
Figure 11.
Evolution and forecasting of MMR in East Africa.
Figure 12.
Maternal mortality trends in Central Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 12.
Maternal mortality trends in Central Africa (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 13.
Maternal Mortality in Central Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 13.
Maternal Mortality in Central Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 14.
Evolution and forecasting of MMR in Central Africa.
Figure 14.
Evolution and forecasting of MMR in Central Africa.
Figure 15.
Maternal mortality trends in the South Africa Region (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 15.
Maternal mortality trends in the South Africa Region (1990-2015) indicate joinpoints at the transitions between colored lines.
Figure 16.
Maternal Mortality in Central Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 16.
Maternal Mortality in Central Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 17.
Evolution and forecasting of MMR in South Africa.
Figure 17.
Evolution and forecasting of MMR in South Africa.
Figure 18.
Maternal mortality trends in West Africa Region (1990-2015) indicating join points at the transitions between colored lines.
Figure 18.
Maternal mortality trends in West Africa Region (1990-2015) indicating join points at the transitions between colored lines.
Figure 19.
Maternal Mortality in West Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 19.
Maternal Mortality in West Africa (a) Autocorrelation (ACF) (b) and Partial Autocorrelation (PACF).
Figure 20.
ARIMA Predictions and Historical Trends of MMR in West Africa.
Figure 20.
ARIMA Predictions and Historical Trends of MMR in West Africa.
Figure 21.
Comparative Analysis and Projection of Maternal Mortality Ratio in Africa and its Regions Utilizing the Holt Method. (The blue shaded area signifies the 80% CI and the grey represents the 95% CI).
Figure 21.
Comparative Analysis and Projection of Maternal Mortality Ratio in Africa and its Regions Utilizing the Holt Method. (The blue shaded area signifies the 80% CI and the grey represents the 95% CI).
Table 1.
Joinpoint analysis maternal mortality rates in Africa, 1990–2015.
Table 1.
Joinpoint analysis maternal mortality rates in Africa, 1990–2015.
| Periods |
Years |
APC (95% CI) |
P |
| Total Period |
1990-2015 |
-2.6 (-2.7; -2.5) |
< 0.001 |
| Period 1 |
1990-1996 |
-1.4 (-1.6; -1.2) |
< 0.001 |
| Period 2 |
1996-2001 |
-2.0 (-2.4; -1.7) |
< 0.001 |
| Period 3 |
2001-2007 |
-3.5 (-3.8; -3.3) |
< 0.001 |
| Period 4 |
2007-2015 |
-2.7 (-2.8; -2.6) |
< 0.001 |
Table 2.
Joinpoint analysis maternal mortality rates in Africa, 1990–2015.
Table 2.
Joinpoint analysis maternal mortality rates in Africa, 1990–2015.
| Periods |
Years |
APC (95% CI) |
P |
| North |
|
|
|
| Total Period |
1990-2015 |
-1.9 (-2.0; -1.8) |
< 0.001 |
| Period 1 |
1990-1996 |
-2.0 (-2.1; -1.8) |
< 0.001 |
| Period 2 |
1996-2003 |
-1.4 (-1.5; -1.3) |
< 0.001 |
| Period 3 |
2003-2007 |
-2.5 (-2.8; -2.1) |
< 0.001 |
| Period 4 |
2007-2010 |
-1.7 (-2.6; -0.8) |
0.001 |
| Period 5 |
2010-2015 |
-3.0 (-3.2; -2.9) |
< 0.001 |
| East |
|
|
|
| Total Period |
1990-2015 |
-3.6 (-3.8; -3.4) |
< 0.001 |
| Period 1 |
1990-1993 |
-1.3 (-1.5; -1.1) |
< 0.001 |
| Period 2 |
1993-2001 |
-2.6 (-2.7; -2.6) |
< 0.001 |
| Period 3 |
2001-2004 |
-3.2 (-3.7; -2.8) |
< 0.001 |
| Period 4 |
2004-2009 |
-5.0 (-5.1; -4.9) |
< 0.001 |
| Period 5 |
2009-2015 |
-4.5 (-4.6; -4.4) |
< 0.001 |
| Central |
|
|
|
| Total Period |
1990-2015 |
-1.3 (-1.5; -1.1) |
< 0.001 |
| Period 1 |
1990-1995 |
0.4 (0.1; 0,6) |
0.005 |
| Period 2 |
1995-1999 |
-0.8 (-1.3; -0.2) |
0.009 |
| Period 3 |
1999-2004 |
-2.3 (-2.6; -1.9) |
< 0.001 |
| Period 4 |
2004-2010 |
-1.0 (-1.2; -0.7) |
< 0.001 |
| Period 5 |
2010-2015 |
-2.6 (-2.9; -2.4) |
< 0.001 |
| South |
|
|
|
| Total Period |
1990-2015 |
-2.6 (-2.8; -2.4) |
< 0.001 |
| Period 1 |
1990-1994 |
-1.4 (-1.8.; -0.9) |
< 0.001 |
| Period 2 |
1994-2003 |
-1.9 (-2.0; -1.7) |
< 0.001 |
| Period 3 |
2003-2012 |
-3.6 (-3.7; -3.5) |
< 0.001 |
| Period 4 |
2013-2015 |
-2.0 (-3.2; -0.8) |
0.004 |
| West |
|
|
|
| Total Period |
1990-2015 |
-3.3 (-3.5; -3.2) |
< 0.001 |
| Period 1 |
1990-1996 |
-1.8 (-1.9.; -1.6) |
< 0.001 |
| Period 2 |
1996-2002 |
-3.1 (-3.3; -2.9) |
< 0.001 |
| Period 3 |
2002-2008 |
-4.7 (-4.9; -4.5) |
< 0.001 |
| Period 4 |
2008-2011 |
-3.1 (-4.0; -2.2) |
< 0.001 |
| Period 5 |
2011-2015 |
-2.4 (-2.7; -2.1) |
< 0.001 |