1. Introduction
Orthodontic malocclusion is a common dental condition that has persisted throughout history, encompassing various forms of dental deformities, such as crowded teeth and dysfunctional occlusion [
1]. The field of orthodontics comprises trained specialists who specialize in the diagnosis and treatment of individuals with dental malocclusions. Prior to commencing orthodontic treatment, a clinician must accurately diagnose the patient and devise a customized treatment plan. This plan involves the formulation of objectives aimed at attaining the highest standards of esthetics, occlusion, and long-term stability. Once these steps are completed by the orthodontist, the treatment plan is presented to the patient. In delivering the treatment plan, there is an inevitable question that comes to the patient’s mind: “How long will the braces take?” The duration of the treatment is a critical piece of information that is often most valued by the patient. Providing a credible and realistic estimate of treatment duration is of great importance, as it forms a key component of the orthodontic informed consent process, payments plan, and significantly influences patient satisfaction [
2,
3].
Establishing an estimate of the orthodontic treatment duration begins when diagnostic records are obtained from the patient [
4]. These records include dental models, photographs, and radiographs such as cephalometric and panoramic radiographs [
5]. A wide range of quantitative measurements are obtained from these records such as cephalometric values, tooth-size-arch-length discrepancy (TSALD), molar classification, etc. Seasoned orthodontists have years-worth of expertise allowing them to plan and predict orthodontic treatment duration confidently and efficiently. However, orthodontic residents and recently certified orthodontists do not have this advantage. Although they are prepared with the technical skills to do so, it requires more time and experience.
Several studies have been developed to identify certain pre-treatment factors and their effects on orthodontic treatment duration. Aljehani et al. conducted a study that assessed the effectiveness of the American Board of Orthodontics Discrepancy Index (DI) in predicting duration of orthodontic treatment [
6]. The DI form was used to quantitatively define the complexity of an orthodontic case. They concluded that there is a positive weak correlation between DI and treatment time. Vu et al. performed a similar study that evaluated the effectiveness of the DI and the treatment complexity index (TCI), created for patients treated with fixed edgewise appliances, in predicting orthodontic treatment duration [
7]. They found that the average treatment time at an orthodontic clinic was 29.10 months. It was concluded that increases in TCI or DI were significantly associated with longer treatment durations. For instance, a higher TCI score was associated with the use of headgear therapy and resulted in an average increase in 6.10 months in treatment length [
7]. Finally, Mavreas et al. conducted a systematic review to investigate various factors that can affect duration of orthodontic therapy [
8]. A total of 41 articles were included in the study. They concluded that certain treatment complexities such as extractions, impacted maxillary canines, and compliance of patients contribute to an increase length of orthodontic therapy. Each article reviewed in this study focused specifically on comparing a specific treatment complexity to a control. For example, Vig et al. collected data to compare mean treatment duration of extraction versus non-extraction cases. The results showed a 5-month average increase in treatment duration in extraction cases [
9]. It can be concluded from these studies that in order to predict duration of orthodontic therapy, accurate and complete pre-treatment data is required.
Recent advancements in the field of artificial intelligence (AI) and machine learning (ML) offer clinicians a supplemental tool to aid in predicting orthodontic treatment duration. AI is a broad term for the technological systems that gather large data samples and exports information that is used to help or improve a human’s decision-making process. Over the last few years, there has been a rapid emergence of AI and ML systems [
10]. Various algorithms of ML systems have been developed that include but not limited to artificial neural networks (ANNs), ML, convolutional neural networks (CNNs), and deep learning (DL) [4,11-14]. These studies have focused on utilizing ML algorithms to predict extraction vs non-extraction treatment, extraction pattern, and anchorage planning [
15,
16]. These studies have shown ML systems can determine extraction treatment (>90%) and extraction patterns (>84%) with reasonably high accuracy [
14,
15]. Dharmasena et al. conducted a study that utilized two ML algorithms (Naïve Bayes and Random Forest) to predict the continuation or discontinuation of orthodontic treatment [
17]. They analyzed a total of 310 records and concluded that the Random Forest algorithm had highest accuracy in predicting continuation or discontinuation of orthodontic treatment. The variable duration of active treatment (>5 years) was concluded to be the main factor in discontinuation of treatment.
Perhaps the most relevant study to ours examined the implementation of a ML algorithm to predict orthodontic treatment duration [
18]. This study evaluated the accuracy and comparison of ML algorithms in predicting orthodontic treatment duration. It included 9 different ML algorithms and 8 pre-treatment variables. The study concluded that decision tree models outperformed other methods (mean square error of 54.08) and revealed that age, malocclusion, and crowding were the most influential predictors. However, this study and other existing studies on this topic have relied on a limited number of independent variables, such as DI or specific questionnaires. In contrast, our study is unique in its incorporation of cephalometric data for the purpose of predicting orthodontic treatment duration and represents a novel contribution to the field. We hypothesize that ML algorithms have the capacity to predict orthodontic treatment duration in a manner comparable to that of clinicians.
2. Materials and Methods
2.1. Study Sample
The data for this retrospective study consisted of 478 patients who received orthodontic treatment at Indiana University School of Dentistry (IUSD) Graduate Orthodontic Clinic. Inclusion criteria consisted of patients who: (1) received and completed comprehensive orthodontic treatment at IUSD, (2) presented with a first molar to first molar permanent dentition, and (3) had complete pretreatment and posttreatment records. Exclusion criteria consisted of: (1) non-IUSD patients, (2) limited care treatments, (3) interdisciplinary cases, (4) early debonds, (5) phase I treatments, and (6) orthognathic surgery patients. The patient sample included 315 (66%) females and 163 (34%) males. 49% of the patients were treated without any extraction, while 51% were treated with extractions. There was a total of 119 (25%) patients that received treatment during the COVID pandemic. Molar classification consisted of 181 (38%) Class I, 217 (45%) Class II, and 80 (17%) Class III patients.
2.2. Data Collection
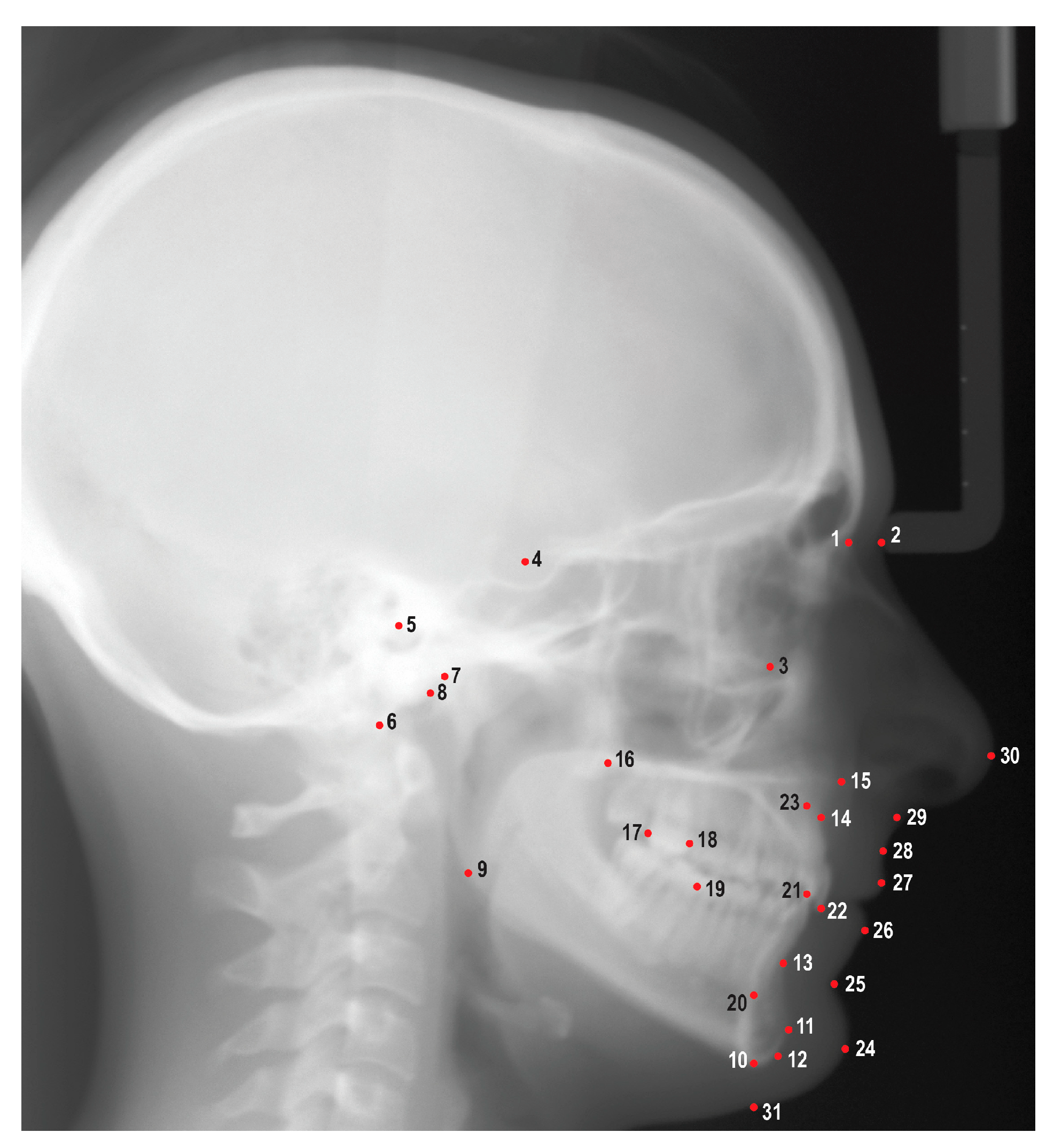
An experienced orthodontic faculty member (HT) and three orthodontic residents (JV, TM, LL) attended three calibration sessions prior to reviewing and tracing the cephalometric radiographs. A total of 31 cephalometric landmarks were identified using Dolphin Imaging Software (Patterson Dental, Saint Paul, MN) (
Figure 1). These cephalometric landmarks were used to generate a cephalometric analysis that included 46 linear and angular measurements (
Table 1). Demographic and treatment information including age, gender, race, ethnicity, actual treatment time, additional appliances, and COVID factor were gathered from the IUSD electronic practice management software (Axium, Exan Software, Las Vegas, NV). Additional appliances factor included impacted canines, expanders, and headgear. COVID factor was included if patient was being treated during the pandemic when IUSD limited elective dental appointments (March 2020 – June 2020). Maxillary/mandibular TSALD and molar classifications were collected by utilizing pretreatment photographs and digital casts. TSALD was categorized into no crowding/spacing (<1mm), mild crowding/spacing (1-3mm), moderate crowding/spacing (4-7mm), and severe crowding/spacing (>8mm).
2.3. Reliability Assessment
In order to evaluate the agreement among examiners, as well as the repeatability within examiners, a total of twenty patient records were randomly selected for each resident. These records were subsequently retraced to assess intra-examiner repeatability and inter-examiner agreement by using the intraclass correlation coefficient (ICCs).
2.4. Training and testing the models
Following the data collection, the statistician randomly distributed the patient sample into a training set, which comprised of two-thirds of the total sample, and a test set, which constituted one-third of the total sample. The aforementioned training and test sets were used to both train and test each of the designated ML algorithms.
A total of 8 traditional regression models and a small multilayer perceptron (MLP), namely a neural network, were used to predict the orthodontic treatment duration. The implemented models include 4 linear models (Linear regression, Lasso, Ridge, and Elastic Net), 2 tree-based models (XGBoost and Random Forest), 2 kernel-based models (Support Vector Machine (SVM) and Gaussian Process Regression), and a neural network (MLP Regressor). Since the dataset contains both numeric and categorical values with different feature scales, tree-based methods are a natural choice. To explore both linear and non-linear relationship between covariate and treatment months, we extended ML methods to linear and kernel-based methods. For the sake of completeness, we added a small neural network to the pack although the size of the dataset is quite small for this data hungry approach. Finally, we performed automated hyperparameter tuning using python Hyperopt package for each model.
Due to the number of numerical features in this study, it was determined to test and train the ML methods utilizing both the raw data and normalized data set. Normalization is an important step when training traditional ML methods. It is particularly important for kernel-based methods like SVM as they are sensitive to outliers, and normalization mitigates the effect of outliers. Linear models also benefit from normalization and the model interpretability becomes easier as the features now reside in common scale. Normalization makes sure the variance and scale in some features do not overshadow the relative importance from other features. For these reasons we determined to employ min-max normalization on the data and the raw data, separately.
2.5. Statistical Analysis
Descriptive statistics were provided for normalized and raw data groups for both true and absolute differences. For both normalized and scaling analyses, means with 95% confidence intervals were provided for differences between the actual, and each initial measurement were provided for both true and absolute differences. Mean absolute error (MAE), root mean square error (RMSE), and mean error (ME) were calculated to further evaluate the accuracy of the ML algorithms. One-sample t-test was used to test for the difference from zero. One-way analysis of variance (ANOVA) with a random effect was used to test for the differences between the 9 methods for both normalized and raw data groups. For both groups, intraclass correlation coefficients (ICCs) and Bland Altman plots were used to measure the agreement between actual and final measurements. All the tests were conducted at 5% significance level. All the analyses were done using SAS 9.4 software (SAS Institute Inc., Cary, NC).
3. Results
3.1. Reliability Analysis
The reliability analysis conducted in this study assessed the repeatability and agreement of 50 measurable pre-diagnostic variables and the results were given in
Table 2. The findings indicate that 80% of these variables demonstrated excellent (ICCs>0.90) or good (0.75<ICCs<0.90) intra-examiner repeatability, highlighting the consistent and reliable nature of the measurements performed by the same examiner [
19]. Furthermore, inter-examiner agreement was evaluated, with 86% of the variables showing excellent or good agreement between different examiners. These results provide evidence of the robustness and consistency of the measurements, supporting the reliability of the data used in the study.
3.2. Descriptive Statistics
The study encompassed a sample population with a mean age of 16.00 ± 9.32 years. The average duration of treatment was found to be 30.12 ± 9.32 months. Moreover, the mean ANB value for the sample was determined to be 3.29° ± 2.06, while the average SN-MP measurement stood at 32.66° ± 5.98. Furthermore, a comparative analysis revealed that the average treatment time for cases involving extraction was 33.46 ± 8.94 months, whereas non-extraction cases exhibited an average treatment time of 26.58 ± 8.38 months.
Table 3 provides the complete results for the descriptive statistics including mean, standard deviation, minimum and maximum values.
3.3. Predictive Features
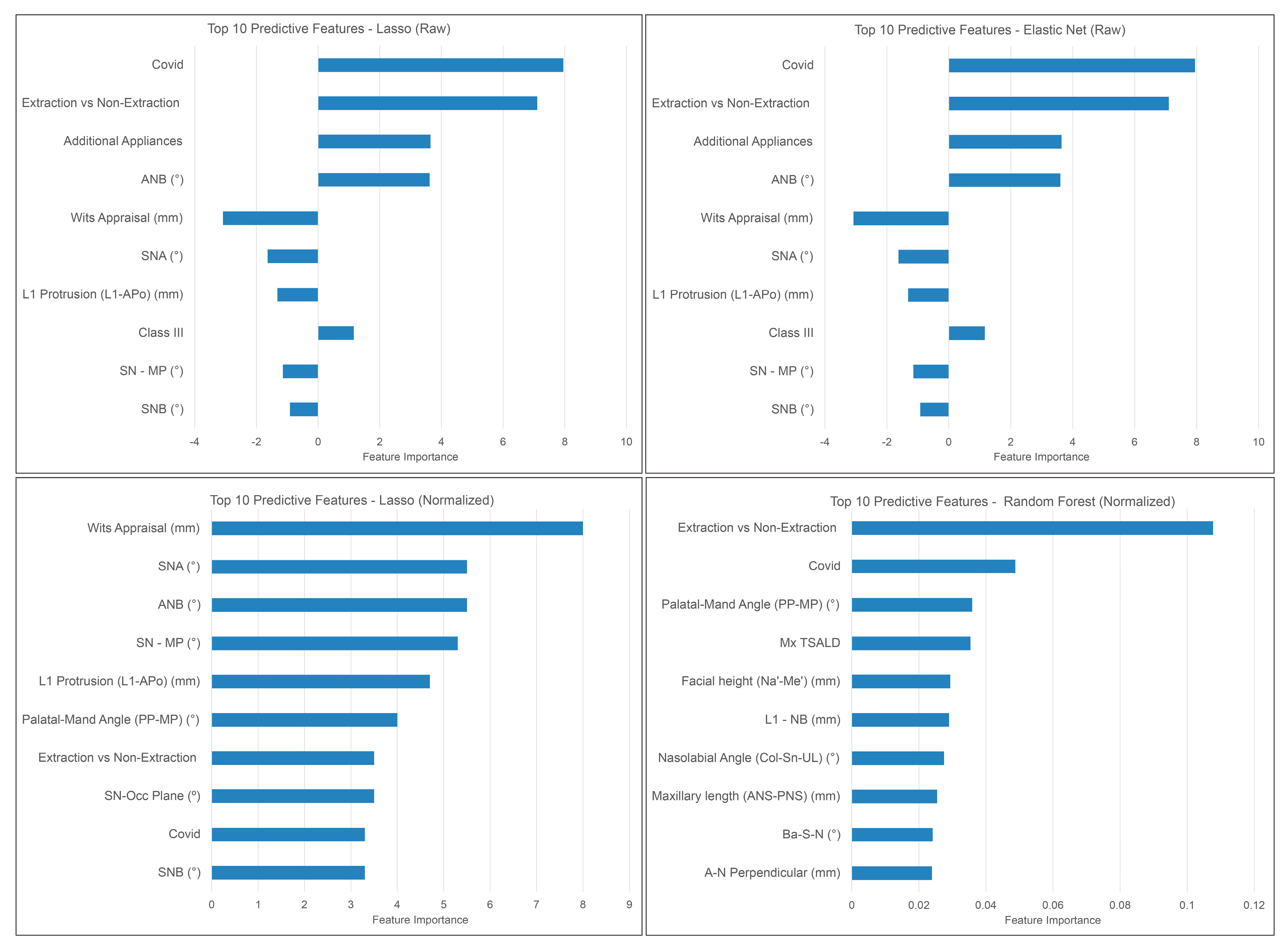
Figure 4 shows the most predictive features picked up by the top performing ML models: Elastic net, Random Forest, and Lasso. Extraction decision, the impact of COVID-19, and the utilization of additional appliances consistently emerged as the most influential features in predicting orthodontic treatment duration. These features exhibited notable consistency in their appearance across multiple ML models, reinforcing their significance in accurately estimating treatment duration.
3.4. Method comparison
Table 5 represents the ANOVA comparing performance of the tested models in predicting the actual orthodontic treatment duration. A significant difference exists between Gaussian process, SVM, and MLP regressor when compared to the remaining ML algorithms. This disparity suggests notable variations in their predictive capabilities or performance outcomes.
4. Discussion
The study aimed to assess and analyze the feasibility of developing a reasonably accurate ML model for predicting orthodontic treatment duration based on pretreatment diagnostic variables. Estimating treatment duration in orthodontics requires extensive expertise and discipline-specific knowledge. The development of such a model holds significant potential in optimizing treatment planning and facilitating effective communication between orthodontists and patients. By offering a ML model that can provide reliable predictions, informed consent for patients can be enhanced, leading to increased levels of patient satisfaction. In addition to providing precise treatment estimates, it is equally essential to establish an accurate range.
The present study revealed a mean treatment duration of 30.12 ± 9.32 months. Notably, Vu et al. reported comparable treatment durations of 29.10 ± 10.99 months within an orthodontic department [
7]. Specifically, extraction cases exhibited an average treatment time of 33.15 months, whereas non-extraction cases had an average treatment time of 26.90 months. Similar trends were observed in the investigation conducted by Holman et al., wherein extraction cases had an extended average treatment time of 30 months, while non-extraction cases exhibited a shorter average treatment duration of 26 months [
20]. Moreover, patients undergoing orthodontic treatment during the COVID pandemic experienced an average treatment time increase of 3 months. This finding aligns with the study conducted by Morosan, which reported a comparable treatment delay of 2 months [
21].
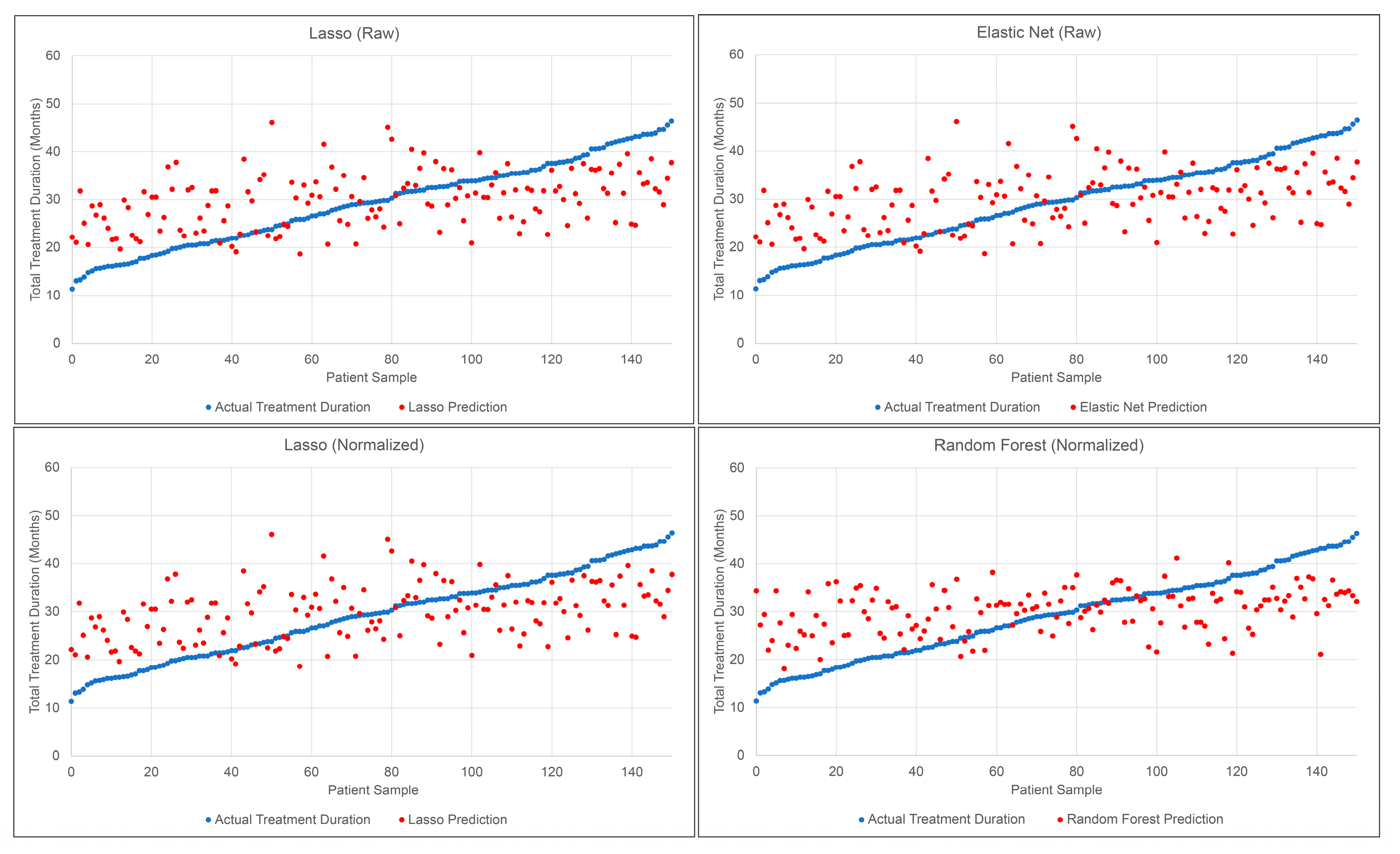
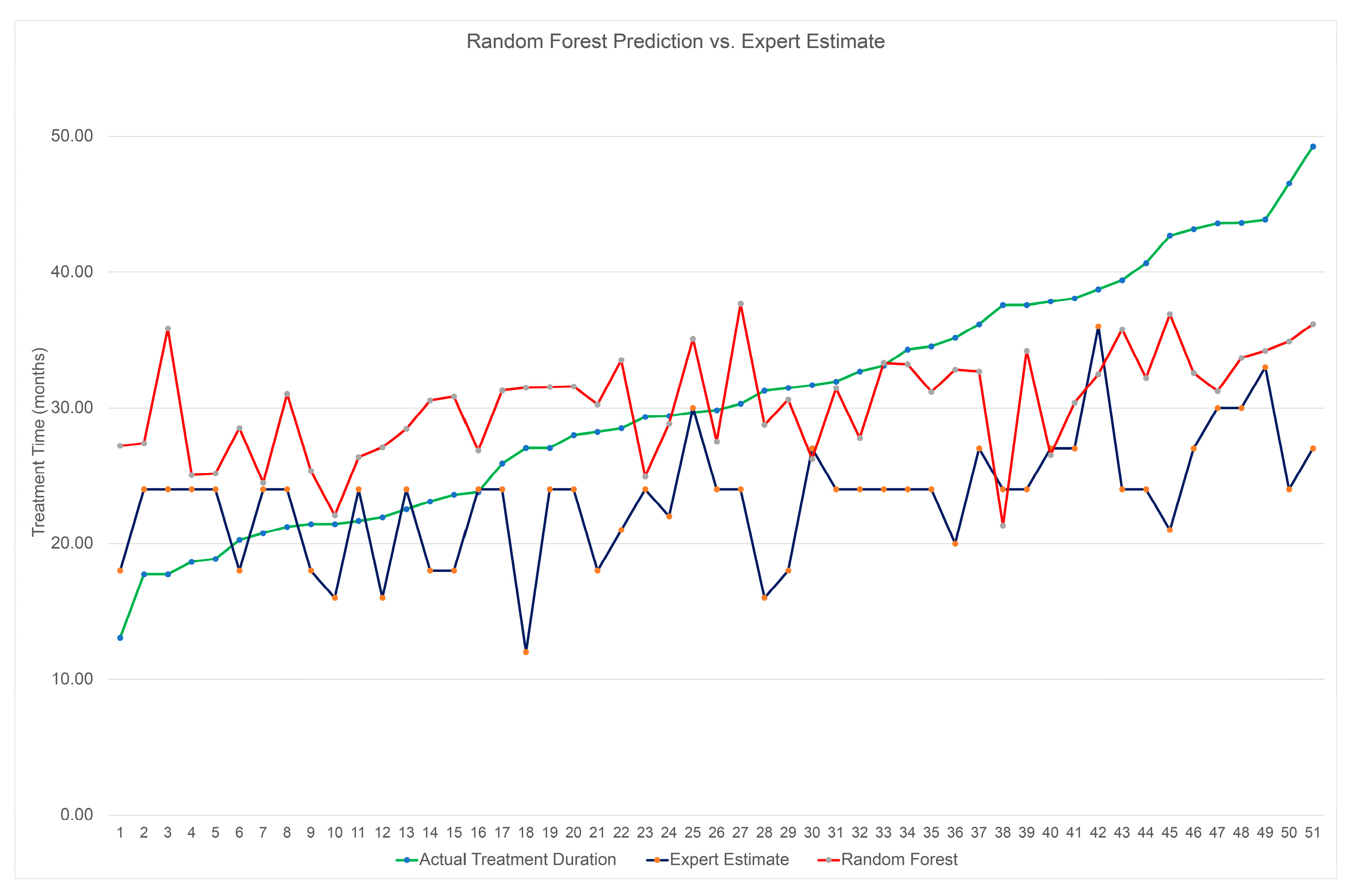
A comprehensive evaluation was conducted in this study to assess the performance of different ML models in predicting orthodontic treatment duration. ML models were able to predict the actual orthodontic treatment duration within ± 7.27 months. A consistent pattern was observed among the ML models, with a tendency to overestimate shorter treatment times while underestimating longer treatment times. This behavior may stem from the algorithms' inclination to converge treatment time predictions towards the average total treatment duration of the patient sample. In order to evaluate the clinical performance of the ML models, it is essential to establish a benchmark against which their predictive accuracy can be evaluated. The benchmark was established from a subset of 148 patients that had received expert-estimated treatment time prior to commencing orthodontic treatment. The analysis of expert predictions against the actual treatment time revealed a MAE of ± 9.66 months. Notably, the expert predictions demonstrated a 25% decrease in accuracy compared to the best ML models. This emphasizes the fact that predicting orthodontic treatment duration is a challenging task for both ML models and clinicians.
The ML models employed in this study were evaluated to identify the most influential features for treatment duration prediction. The analysis of the best performing ML models revealed that extraction decision, COVID-19 impact, additional appliances, intermaxillary relationship, lower incisor position, and vertical skeletal pattern were the features accorded the highest weights in treatment time prediction. This observation aligns with the findings of Fisher et al., who also identified extraction decision, lower incisor position, and vertical skeletal pattern as significant factors impacting orthodontic treatment duration [
22]. Similarly, Mavreas et al. reported an extended treatment duration associated with additional appliances and extraction treatment. Interestingly, our study and that of Mavreas both indicated that molar classification and age did not exert significant effects on treatment time [
8]. The inclusion criteria encompassed all patients with permanent dentition, potentially diminishing the influence of age when the ML models assigned importance to specific features. Moreover, the majority of patients in our sample shared a similar age range. Regarding molar classification, its impact may have been limited due to the absence of malocclusion severity among the pre-treatment variables. For example, patients classified as a quarter-step Class II received equivalent weight as those classified as a full-step Class II.
Our findings revealed notable variations in the performance of the methods, with Elastic Net, Lasso, and Random Forest models emerging as the top performers. Conversely, the MLP regressor, Gaussian process, and SVM models exhibited comparatively poorer predictive capabilities. Notably, linear regression and tree-based models exhibited superior performance, while kernel-based and deep learning models yielded slightly less accurate predictions. Several factors, including sample size, feature selection, and regularization techniques, likely contributed to these disparities. In the context of limited sample sizes, the simplicity and reduced risk of overfitting in linear models make them more likely to outperform non-linear models. This advantage stems from the stable and reliable estimations of variable relationships that linear models can provide.
It is essential to recognize that orthodontic treatment duration is influenced by various factors, encompassing both pre-diagnostic measurable data and factors that arise during the course of treatment. The pre-diagnostic data, obtained through clinical examinations and cephalometric analyses, contribute to the complexity of each case, ultimately impacting the duration of treatment. This study primarily focuses on analyzing these pre-diagnostic variables. However, it is crucial to acknowledge that additional factors that arise during treatment, such as patient compliance, treatment-related emergencies, and missed appointments, can significantly influence the overall treatment duration. Beckwith’s study found that factors such as broken brackets, poor oral hygiene, and missed appointments had a significant increase in orthodontic treatment duration [
23]. Furthermore, the MAE values obtained in this study may provide insight into the extent to which these treatment-related factors can affect the treatment duration. By examining the MAE values, we can gain a better understanding of the interplay between pre-diagnostic factors and the additional factors that emerge during treatment, contributing to a comprehensive assessment of orthodontic treatment duration.
This study is limited by its inability to account for these factors. Furthermore, the sample size represents another limitation, as ML methods tend to exhibit improved performance when provided with larger datasets. Future investigations should prioritize enlarging the sample size and exploring the potential benefits of incorporating image detection of cephalometric radiographs, which could mitigate concerns regarding intra-examiner reliability and inter-examiner agreement.
5. Conclusions
All tested ML models were able to predict orthodontic treatment duration within a clinically acceptable range. Although ML models had similar accuracy, linear models and Random Forest were the most predictive models, while SVM regressor and Gaussian process regression were the least. Extraction decision, COVID factor, intermaxillary relationship, lower incisor position and additional appliances were found to be the most predictive features in determining treatment time.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org., Figure S1: Bland-Altman plots showing the agreement between actual and predicted treatment durations using raw data. Figure S2: Bland-Altman plots showing the agreement between actual and predicted treatment durations using normalized data.
Author Contributions
JV: Conceptualization, methodology, investigation, writing – original draft preparation, data curation, visualization, and optimized data collection. SB: Conceptualization, methodology, writing – original draft, organized and ran ML algorithms, and organized results. SA: Data curation and writing – original draft. LL: Resources and data collection. TM: Resources and data collection. SB: Statistical analysis and writing – original draft. GE: Statistical analysis. DA: Conceptualization, resources, writing – review and editing, visualization, and supervision. HT: Conceptualization, methodology, formal analysis, writing – original draft, project administration, supervision, and manuscript preparation.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved as a non-human subject's research (NHSR) by the Institution Review Board (IRB) of Indiana University (Protocol #11487).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data was gathered from the Indiana University School of Dentistry, Department of Orthodontics.
Acknowledgments
This study was made possible through the invaluable contributions of the orthodontic residents, esteemed faculty members, dedicated technical team, and the patient records at the Indiana University School of Dentistry.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Proffit, W.R.; Fields, H.W.; Larson, B.E.; Sarver, D.M. Contemporary Orthodontics; Elsevier: 2019; Volume 6th.
- Pachêco-Pereira, C.; Pereira, J.R.; Dick, B.D.; Perez, A.; Flores-Mir, C. Factors associated with patient and parent satisfaction after orthodontic treatment: A systematic review. American Journal of Orthodontics and Dentofacial Orthopedics 2015, 148, 652–659. [Google Scholar] [CrossRef]
- Jharwal, V.; Trehan, M.; Rathore, N.; Rathee, P.; Agarwal, D.; Mathur, N. Informed consent for braces. Int J Clin Pediatr Dent 2014, 7, 105–108. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Al-Ehaideb, A.; Vishwanathaiah, S.; Maganur, P.C.; Patil, S.; Naik, S.; Baeshen, H.A.; Sarode, S.S. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making - A systematic review. J Dent Sci 2021, 16, 482–492. [Google Scholar] [CrossRef]
- Rischen, R.J.; Breuning, K.H.; Bronkhorst, E.M.; Kuijpers-Jagtman, A.M. Records needed for orthodontic diagnosis and treatment planning: a systematic review. PLoS one 2013, 8, e74186. [Google Scholar] [CrossRef]
- Aljehani, D.; Baeshen, H.A. Effectiveness of the American Board of Orthodontics Discrepancy Index in predicting Treatment Time. J Contemp Dent Pract 2018, 19, 647–650. [Google Scholar]
- Vu, C.Q.; Roberts, W.E.; Hartsfield, J.K., Jr.; Ofner, S. Treatment complexity index for assessing the relationship of treatment duration and outcomes in a graduate orthodontics clinic. Am J Orthod Dentofacial Orthop 2008, 133, 9–e1. [Google Scholar] [CrossRef]
- Mavreas, D.; Athanasiou, A.E. Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod 2008, 30, 386–395. [Google Scholar] [CrossRef]
- Vig, K.W.; Weyant, R.; Vayda, D.; O'Brien, K.; Bennett, E. Orthodontic process and outcome: efficacy studies--strategies for developing process and outcome measures: a new era in orthodontics. Clin Orthod Res 1998, 1, 147–155. [Google Scholar] [CrossRef]
- Chen, Y.W.; Stanley, K.; Att, W. Artificial intelligence in dentistry: current applications and future perspectives. Quintessence Int 2020, 51, 248–257. [Google Scholar] [CrossRef]
- Arık, S.; Ibragimov, B.; Xing, L. Fully automated quantitative cephalometry using convolutional neural networks. J Med Imaging (Bellingham) 2017, 4, 014501. [Google Scholar] [CrossRef]
- Xie, X.; Wang, L.; Wang, A. Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. Angle Orthod 2010, 80, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Kök, H.; Acilar, A.M.; İzgi, M.S. Usage and comparison of artificial intelligence algorithms for determination of growth and development by cervical vertebrae stages in orthodontics. Prog Orthod 2019, 20, 41. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.-K.; Kim, T.-W. New approach for the diagnosis of extractions with neural network machine learning. American Journal of Orthodontics and Dentofacial Orthopedics 2016, 149, 127–133. [Google Scholar] [CrossRef]
- Li, P.; Kong, D.; Tang, T.; Su, D.; Yang, P.; Wang, H.; Zhao, Z.; Liu, Y. Orthodontic Treatment Planning based on Artificial Neural Networks. Sci Rep 2019, 9, 2037. [Google Scholar] [CrossRef] [PubMed]
- Leavitt, L.; Volovic, J.; Steinhaeur, L.; Mason, T.; Eckert, G.; Dean, J.A.; Dundar, M.M.; Turkkahraman, H. Can we predict orthodontic extraction patterns by using machine learning? Orthodontics & Craniofacial Research 2023.
- Dharmasena, R.; Nawarathna, L.; Nawarathna, R. Predicting cessation of orthodontic treatments using a classification-based approach. Biom Biostat Int J 2020, 9, 68–74. [Google Scholar] [CrossRef]
- Elnagar, M.H.; Pan, A.Y.; Handono, A.; Sanchez, F.; Talaat, S.; Bourauel, C.; Kaboudan, A.; Kusnoto, B. Utilization of Machine Learning Methods for Predicting Orthodontic Treatment Length. Oral 2022, 2, 263–273. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Holman, J.K.; Hans, M.G.; Nelson, S.; Powers, M.P. An assessment of extraction versus nonextraction orthodontic treatment using the peer assessment rating (PAR) index. Angle Orthod 1998, 68, 527–534. [Google Scholar] [CrossRef]
- Morosan, H. Orthodontic treatment in times of Covid-19. J Med Life 2021, 14, 205–209. [Google Scholar] [CrossRef]
- Fisher, M.A.; Wenger, R.M.; Hans, M.G. Pretreatment characteristics associated with orthodontic treatment duration. American Journal of Orthodontics and Dentofacial Orthopedics 2010, 137, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Beckwith, F.R.; Ackerman, R.J.; Cobb, C.M.; Tira, D.E. An evaluation of factors affecting duration of orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics 1999, 115, 439–447. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
Cephalometric landmarks used in this study. 1: Nasion (N), 2: Soft tissue nasion (N’), 3: Orbitale (Or), 4: Sella (S), 5: Porion (Po), 6: Basion (Ba), 7: Condylion (Co), 8: Articulare (Ar), 9: Gonion (Go), 10: Menton (Me), 11: Pogonion (Pog), 12: Gnathion (Gn), 13: B point (B), 14: A point (A), 15: Anterior nasal spine (ANS), 16: Posterior nasal spine (PNS), 17: Distal of upper first molar (U6d), 18: Mesial of upper first molar (U6m), 19: Mesial of lower first molar (L6m), 20: Lower incisor root apex (L1a), 21: Lower incisor incisal edge (L1i), 22: Upper incisor incisal edge (U1i), 23: Upper incisor root apex (U1a), 24: Soft tissue pogonion (Pog’), 25: Soft tissue B point (B’), 26: Lower lip (Li), 27: Upper lip (Ls), 28: Soft tissue A point (A’), 29: Subnasale (Sn), 30: Pronasale (Pn), 31: Soft tissue menton (Me’).
Figure 1.
Cephalometric landmarks used in this study. 1: Nasion (N), 2: Soft tissue nasion (N’), 3: Orbitale (Or), 4: Sella (S), 5: Porion (Po), 6: Basion (Ba), 7: Condylion (Co), 8: Articulare (Ar), 9: Gonion (Go), 10: Menton (Me), 11: Pogonion (Pog), 12: Gnathion (Gn), 13: B point (B), 14: A point (A), 15: Anterior nasal spine (ANS), 16: Posterior nasal spine (PNS), 17: Distal of upper first molar (U6d), 18: Mesial of upper first molar (U6m), 19: Mesial of lower first molar (L6m), 20: Lower incisor root apex (L1a), 21: Lower incisor incisal edge (L1i), 22: Upper incisor incisal edge (U1i), 23: Upper incisor root apex (U1a), 24: Soft tissue pogonion (Pog’), 25: Soft tissue B point (B’), 26: Lower lip (Li), 27: Upper lip (Ls), 28: Soft tissue A point (A’), 29: Subnasale (Sn), 30: Pronasale (Pn), 31: Soft tissue menton (Me’).
Figure 2.
Actual treatment time vs ML predictions for the test set.
Figure 2.
Actual treatment time vs ML predictions for the test set.
Figure 3.
Comparison of expert estimate, RF prediction, and actual treatment duration.
Figure 3.
Comparison of expert estimate, RF prediction, and actual treatment duration.
Figure 4.
Most predictive features picked up by the top performing ML methods.
Figure 4.
Most predictive features picked up by the top performing ML methods.
Table 1.
Cephalometric variables and their definitions.
Table 1.
Cephalometric variables and their definitions.
| Category |
Measurements |
Definitions |
| Maxilla to Cranial Base |
SNA (˚) |
The angle formed by connecting sella, nasion, and A-point |
| SN-Palatal Plane (˚) |
The angle formed from the intersection of sella-nasion line and a line drawn connecting anterior nasal spine to posterior nasal spine |
| |
SN-Occlusal Plane (˚) |
The angle formed from sella-nasion and occlusal plane |
| |
A-N Perpendicular (mm) |
The linear distance from A point to the nasion perpendicular. |
| Mandible to Cranial Base |
SNB (˚) |
The angle formed by connecting sella, nasion, and B-point |
| SNPg (˚) |
The angle formed by connecting sella, naison, and pogonion |
| FMA: MP-FH (˚) |
The angle formed from the intersection of porion-orbitale line and a line drawn connecting gonion to gnathion |
| SN-MP (˚) |
The angle formed from the intersection of sella-nasion line and a line drawn connecting gonion to gnathion |
| Mandibular Plane to Occlusal Plane (˚) |
The angle formed by mandibular plane and occlusal plane |
| B-N Perpendicular (mm) |
The linear distance from B point to nasion perpendicular |
| Pog-N Perpendicular (mm) |
The linear distance from pogonion to nasion perpendicular |
| Y-Axis: SGn-SN (˚) |
The angle formed by connecting nasion, sella, and gnathion |
| Maxilla to Mandible |
ANB (˚) |
The difference between SNA and SNB |
| Palatal-Mandibular Angle (PP-MP) (˚) |
The angle formed from palatal plane and mandibular plane |
| Wits Appraisal (mm) |
The distance between A point to Occlusal plane and B point to Occlusal plane |
| Maxillary Length: ANS-PNS (mm) |
The linear measurement between anterior nasal spine and posterior nasal spine |
| Mandibular Length: Co-Gn (mm) |
The linear measurement between condylion and gnathion |
| Cranial Base |
Cranial Base Flexure Angle: Ba-S-N (˚) |
The angle formed by connecting basion, sella, and nasion |
| Upper Incisors to Maxilla |
U1-SN (˚) |
The angle formed from a line connecting sella to nasion and a line connecting the upper incisor incisal tip to the root apex |
| U1-NA (˚) |
The angle formed from a line connecting nasion to A-point and a line connecting the upper incisor incisal tip to the root apex |
| U1-NA (mm) |
The linear measurement from the labial surface of the upper incisor to the line connecting nasion to A-point |
| |
U1-Palatal Plane (˚) |
The angle formed by the position of maxillary incisor to palatal plane |
| |
U1 Protrusion (U1-APo) (mm) |
The distance from maxillary incisor to the A point-pogonion reference line |
| Lower Incisors to Mandible |
L1-MP (˚) |
The angle formed from a line connecting the lower incisor incisal tip to the root apex and a line connecting gonion to gnathion |
| L1-NB (˚) |
The angle formed from a line connecting the lower incisor incisal tip to the root apex and a line connecting nasion to B-point |
| L1-NB (mm) |
The linear measurement from the labial surface of the lower incisor incisal to the line connecting nasion to B-point |
| |
L1 Protrusion (L1-Apo) (mm) |
The distance from mandibular incisor to the A point-pogonion reference line |
| Incisors to Each Other |
Interincisal Angle (˚) |
The angle formed from a line connecting the lower incisor incisal tip to the apex and a line connecting the upper incisor incisal tip to the root apex |
| |
Overjet (mm) |
The horizontal distance from maxillary incisor tip to mandibular incisor tip |
| |
Overbite (mm) |
The vertical distance from maxillary incisor tip to mandibular incisor tip |
| Soft Tissue |
Upper Lip to E-Plane (mm) |
The linear distance from upper lip to a line connecting soft tissue pogonion and pronasale |
| Lower Lip to E-Plane (mm) |
The linear distance from lower lip to a line connecting soft tissue pogonion and pronasale |
| ILG (HP) (mm) |
The vertical distance from stomion superius to stomion inferius |
| Nasolabial Angle (Pn-Sn-UL) (˚) |
The angle formed by pronasale, subnasale, and upper lip |
| H-Angle (Pg’UL-Pg’Na’) (˚) |
The angle formed by soft tissue pogonion-upper lip to soft tissue pogonion-soft tissue nasion |
| Facial Height (Na’-Me’) (mm) |
The linear measurement from soft tissue nasion and soft tissue menton |
| Soft Tissue Upper Face Height: G'-Sn' (mm) |
The linear measurement between soft tissue glabella and soft tissue subnasale |
| Soft Tissue Lower Face Height: Sn'-Me' (mm) |
The linear measurement between soft tissue subnasale and soft tissue pogonion |
| Hard Tissue Upper Face Height: N-ANS (mm) |
The linear measurement between nasion and anterior nasal spine |
| Hard Tissue Lower Face Height: ANS-Me (mm) |
The linear measurement between anterior nasal spine and menton |
| UFH (N-ANS/(N-ANS+ANS-Me)) (%) |
The ratio of the upper face height to facial height |
| LFH (ANS-Me/(N-ANS+ANS-Me)) (%) |
The ratio of lower face heigh to facial height |
| Posterior Face Height: Ar-Go (mm) |
The linear measurement between articulare and gonion |
| |
PFH:AFH (Co-Go:N-Me) (%) |
The ratio of posterior facial height to anterior facial height |
| Profile |
Convexity: NA-APo (˚) |
The angle formed by connecting nasion, A-point, and pogonion |
| Facial Angle: FH-NPo (˚) |
The angle formed from a line connecting porion to orbitale and a line connecting nasion to pogonion |
Table 2.
The results of the reliability analyses.
Table 2.
The results of the reliability analyses.
| |
Threshold |
Agreement |
Quantity |
Percent |
| |
0 < ICCs <0.50 |
Poor |
3 |
6% |
| Intra-examiner repeatability |
0.50 < ICCs < 0.75 |
Moderate |
7 |
14% |
| |
0.75 < ICCs < 0.90 |
Good |
14 |
28% |
| |
ICCs > 0.9 |
Excellent |
26 |
52% |
| |
0 < ICCs <0.50 |
Poor |
1 |
2% |
| Inter-examiner agreement |
0.50 < ICCs < 0.75 |
Moderate |
6 |
12% |
| |
0.75 < ICCs < 0.90 |
Good |
27 |
54% |
| |
ICCs > 0.9 |
Excellent |
16 |
32% |
Table 3.
Descriptive statistics for the pre-treatment variables.
Table 3.
Descriptive statistics for the pre-treatment variables.
| Variable |
Mean |
SD |
Min |
Max |
| Treatment Time (Months) |
30.12 |
9.32 |
11.37 |
51.80 |
| Age (Years) |
16.00 |
5.61 |
9.00 |
50.00 |
| SNA (°) |
82.55 |
4.14 |
71.00 |
94.90 |
| SN-Palatal Plane (°) |
7.52 |
3.71 |
-2.80 |
19.20 |
| SN-Occlusal Plane (º) |
15.62 |
4.85 |
-1.50 |
29.00 |
| A-N Perpendicular (mm) |
0.49 |
3.72 |
-9.60 |
12.00 |
| SNB (°) |
79.25 |
4.14 |
67.40 |
92.90 |
| SNPg (°) |
79.78 |
4.18 |
66.50 |
93.00 |
| FMA (MP-FH) (°) |
27.28 |
5.54 |
11.00 |
45.50 |
| SN - MP (°) |
32.66 |
5.98 |
14.80 |
51.70 |
| Mandibular Plane to Occlusal Plane (°) |
18.25 |
4.52 |
4.80 |
35.10 |
| B-N Perpendicular (mm) |
-4.36 |
6.09 |
-22.10 |
13.20 |
| Pog-N Perpendicular (mm) |
-4.09 |
7.01 |
-24.80 |
15.70 |
| Y-Axis (SGn-SN) (°) |
67.84 |
4.27 |
56.20 |
83.90 |
| ANB (°) |
3.29 |
2.06 |
-3.70 |
11.10 |
| Palatal-Mandibular Plane Angle (PP-MP) (°) |
26.35 |
6.08 |
2.10 |
43.10 |
| Wits Appraisal (mm) |
-0.15 |
3.06 |
-9.50 |
8.90 |
| Maxillary length (ANS-PNS) (mm) |
49.47 |
3.85 |
38.20 |
65.40 |
| Mandibular length (Co-Gn) (mm) |
113.10 |
8.20 |
93.40 |
158.40 |
| Ba-S-N (°) |
130.91 |
5.71 |
114.30 |
153.90 |
| U1 - SN (°) |
107.44 |
9.60 |
67.30 |
134.50 |
| U1 - NA (°) |
24.89 |
8.80 |
-14.10 |
51.50 |
| U1 - NA (mm) |
5.55 |
3.22 |
-7.50 |
17.70 |
| U1 - Palatal Plane (°) |
114.96 |
8.82 |
80.40 |
140.50 |
| U1 Protrusion (U1-APo) (mm) |
7.74 |
3.74 |
-2.40 |
20.90 |
| L1 - MP (°) |
92.19 |
7.70 |
65.50 |
112.80 |
| L1 - NB (°) |
26.70 |
8.35 |
4.80 |
51.30 |
| L1 - NB (mm) |
5.60 |
3.21 |
-1.30 |
17.10 |
| L1 Protrusion (L1-APo) (mm) |
3.35 |
3.41 |
-5.20 |
13.60 |
| Interincisal Angle (U1-L1) (°) |
125.12 |
14.53 |
89.50 |
171.60 |
| Upper Lip to E-Plane (mm) |
-1.60 |
3.12 |
-12.90 |
8.50 |
| Lower Lip to E-Plane (mm) |
0.37 |
3.64 |
-9.80 |
13.80 |
| Interlabial gap (HP) (mm) |
1.19 |
1.40 |
-1.10 |
8.80 |
| Nasolabial Angle (Col-Sn-UL) (°) |
106.58 |
11.27 |
68.00 |
132.60 |
| Holdaway Angle (Pg'UL-Pg'Na') (°) |
17.34 |
4.91 |
0.60 |
36.70 |
| Facial height (Na'-Me') (mm) |
112.97 |
7.60 |
79.90 |
137.20 |
| Soft tissue Upper Facial Height (G'-Sn') (mm) |
63.96 |
4.82 |
49.60 |
76.80 |
| Soft tissue Lower Facial Height (Sn'-Me') (mm) |
69.64 |
6.18 |
53.60 |
87.10 |
| Upper Face Height (N-ANS) (mm) |
49.13 |
3.41 |
38.50 |
59.60 |
| Lower Face Height (ANS-Me) (mm) |
63.37 |
6.34 |
44.90 |
94.20 |
| UFH (N-ANS/(N-ANS+ANS-Me)) (%) |
43.75 |
2.56 |
36.40 |
50.10 |
| LFH (ANS-Me/(N-ANS+ANS-Me)) (%) |
56.25 |
2.56 |
49.90 |
63.60 |
| Posterior Face Height (Ar-Go) (mm) |
42.89 |
5.24 |
29.70 |
62.70 |
| PFH:AFH (Co-Go : N-Me) (%) |
51.74 |
4.84 |
37.40 |
67.30 |
| Convexity (NA-APo) (°) |
5.65 |
5.30 |
-8.20 |
26.30 |
| Facial Angle (FH-NPo) (°) |
87.76 |
3.83 |
75.30 |
98.20 |
| Overjet (mm) |
4.48 |
2.33 |
-2.30 |
18.20 |
| Overbite (mm) |
2.17 |
2.19 |
-6.30 |
10.20 |
Table 4.
Results for the ML predictions and performance assessments.
Table 4.
Results for the ML predictions and performance assessments.
| |
Raw Data |
Normalized Data |
| |
MAE |
RMSE |
ME |
ICC |
MAE |
RMSE |
ME |
ICC |
| XGBoost |
8.70 |
10.56 |
-0.29 |
0.97 |
8.43 |
10.40 |
-0.45 |
0.97 |
| Random Forest |
7.75 |
9.63 |
-0.65 |
0.97 |
7.27 |
8.79 |
-0.46 |
0.96 |
| Lasso |
7.27 |
8.73 |
-0.13 |
0.96 |
7.27 |
8.73 |
-0.13 |
0.96 |
| Ridge |
7.30 |
8.76 |
-0.29 |
0.96 |
7.29 |
8.73 |
-0.16 |
0.96 |
| Linear Regression |
7.30 |
8.76 |
-0.29 |
0.96 |
7.31 |
8.77 |
-0.36 |
0.96 |
| Elastic Net |
7.27 |
8.73 |
-0.13 |
0.96 |
7.27 |
8.73 |
-0.13 |
0.96 |
| Gaussian Process |
29.77 |
31.27 |
29.77 |
0.99 |
8.62 |
11.02 |
3.42 |
0.98 |
| Support Vector |
7.66 |
9.13 |
1.18 |
0.96 |
10.24 |
12.47 |
0.07 |
0.98 |
| MLP Regressor |
13.04 |
15.69 |
12.63 |
0.99 |
8.52 |
10.57 |
-3.20 |
0.97 |
Table 5.
ANOVA comparison for the ML models performance.
Table 5.
ANOVA comparison for the ML models performance.
| Methods |
Estimate |
Standard Error |
P-value |
| Elastic < Gaussian |
-1.35 |
0.47 |
<0.01 |
| Elastic & Lasso |
0.00 |
0.47 |
1.00 |
| Elastic & Linear |
-0.03 |
0.47 |
0.94 |
| Elastic < MLP |
-1.25 |
0.47 |
0.01 |
| Elastic & Random |
0.00 |
0.47 |
1.00 |
| Elastic & Ridge |
-0.01 |
0.47 |
0.97 |
| Elastic < SVM |
-2.96 |
0.47 |
<0.01 |
| Elastic < XGBoost |
-1.16 |
0.47 |
0.01 |
| Gaussian > Lasso |
1.35 |
0.47 |
<0.01 |
| Gaussian > Linear |
1.31 |
0.47 |
0.01 |
| Gaussian & MLP |
0.10 |
0.47 |
0.83 |
| Gaussian > Random |
1.35 |
0.47 |
<0.01 |
| Gaussian > Ridge |
1.33 |
0.47 |
<0.01 |
| Gaussian < SVM |
-1.62 |
0.47 |
<0.01 |
| Gaussian & XGBoost |
0.19 |
0.47 |
0.68 |
| Lasso & Linear |
-0.03 |
0.47 |
0.94 |
| Lasso < MLP |
-1.25 |
0.47 |
0.01 |
| Lasso & Random |
0.00 |
0.47 |
1.00 |
| Lasso & Ridge |
-0.01 |
0.47 |
0.97 |
| Lasso < SVM |
-2.96 |
0.47 |
<0.01 |
| Lasso < XGBoost |
-1.16 |
0.47 |
0.01 |
| Linear < MLP |
-1.21 |
0.47 |
0.01 |
| Linear & Random |
0.03 |
0.47 |
0.94 |
| Linear & Ridge |
0.02 |
0.47 |
0.97 |
| Linear < SVM |
-2.93 |
0.47 |
<0.01 |
| Linear < XGBoost |
-1.12 |
0.47 |
0.02 |
| MLP > Random |
1.25 |
0.47 |
0.01 |
| MLP > Ridge |
1.23 |
0.47 |
0.01 |
| MLP < SVM |
-1.72 |
0.47 |
<0.01 |
| MLP & XGBoost |
0.09 |
0.47 |
0.85 |
| Random & Ridge |
-0.01 |
0.47 |
0.97 |
| Random < SVM |
-2.96 |
0.47 |
<0.01 |
| Random < XGBoost |
-1.16 |
0.47 |
0.01 |
| Ridge < SVM |
-2.95 |
0.47 |
<0.01 |
| Ridge < XGBoost |
-1.14 |
0.47 |
0.01 |
| SVM > XGBoost |
1.81 |
0.47 |
<0.01 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).