1. Introduction
The patellofemoral joint (PFJ) is a complex articulation between the patella and the femur [
1,
2]. The patella is the largest sesamoid of the human body. It is involved in the extensor mechanism bridging the quadriceps femoris to the proximal tibia, thus generating a transferring of forces necessary to knee extension [
3].
On the other hand, the femur, with its trochlear groove, accommodates the patella. At full knee extension, the patella lays above the trochlear groove. In contrast, as the knee reaches around 30° of flexion, the patella starts engaging the trochlear groove, progressively increasing lateral translation and lateral patellar tilt [
3,
4,
5]. We are therefore faced with a foul of force distribution. Anatomical structures, such as bone morphology and ligaments, combined with adequate neuro-muscular control, play a decisive role in controlling the patella-femoral kinematics [
6]. Here come the patellofemoral disorders.
2. Classification of Patellofemoral Disorders
The Lyonnaise school has perfected a simple, easily applicable classifying system for patellofemoral pathology by dividing it into three main groups [
7]:
Objective patellar instability: patients have experienced at least one episode of patellar dislocation and present at least one or more principal factors of instability. Patellar dislocation can occur during high-energy activities such as sports, and is frequently associated with hemarthrosis.
Potential patellar instability: patients never experienced a true patellar dislocation, although they report a rather generic feeling of instability. It may occur daily during low-demanding activities, such as walking and climbing stairs. These patients present one or more principal factors of instability.
Patellofemoral pain syndrome: pain is the main symptom, and it is mostly attributed to cartilage wear on either the patellar or femoral side. Imaging does not show any evident factor of instability, nor a clinical episode of patellar dislocation can be identified.
3. Principal Factors of Instability
Three main features were revealed to be relevant in knees with patellar instability that depend basically on anatomical parameters, thus on bone morphology [
7]:
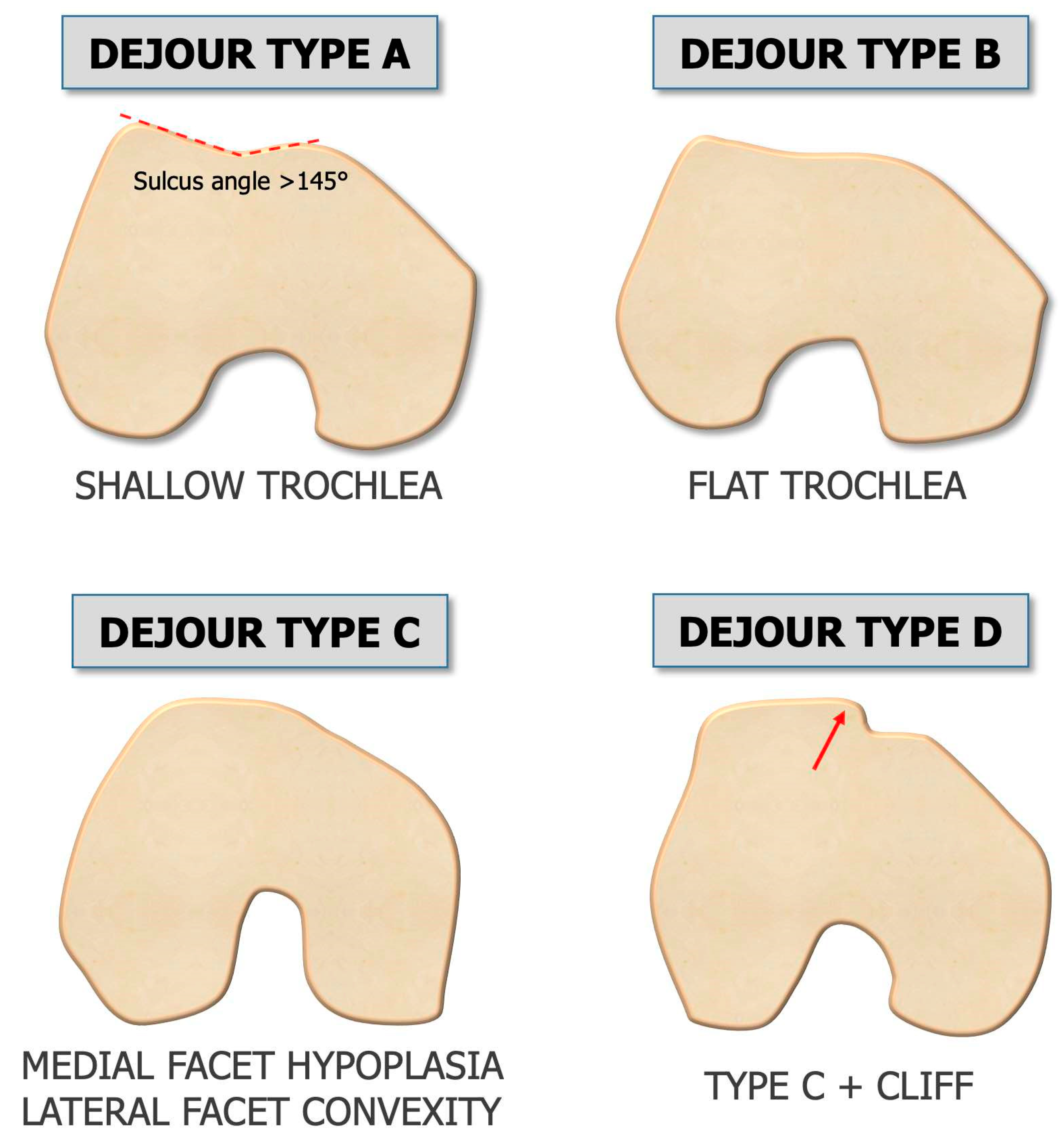
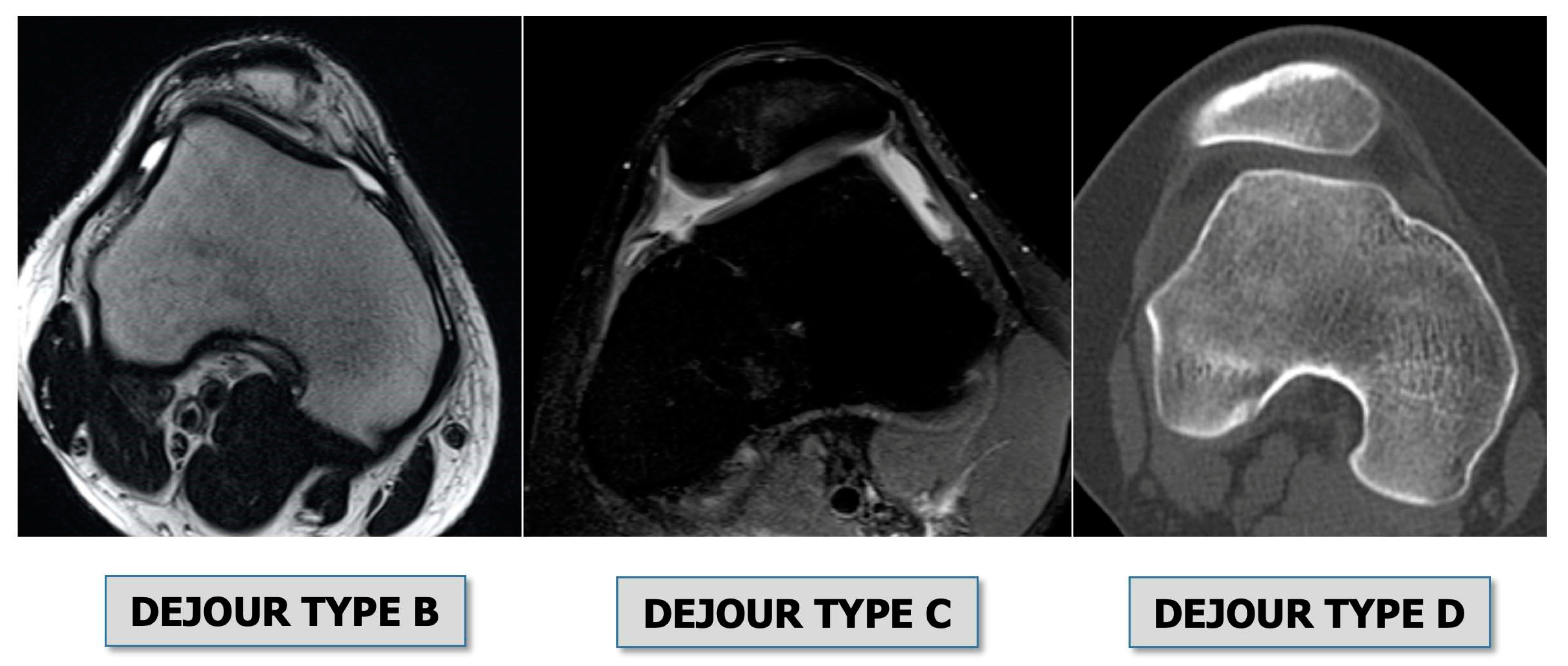
Trochlear dysplasia: indicates how the femoral trochlea is flat or convex (instead of concave), causing abnormal patellar tracking and loss of joint congruence (
Figure 1 and
Figure 2). Dejour classified trochlear dysplasia into four groups [
8]. This classification system requires an accurate lateral X-ray (congruent posterior condyles) and confirmation with axial imaging of the knee (CT scan or MRI). A certain degree of trochlear dysplasia was found in up to 96% of patients with objective or potential patellar instability [
7].
- 2.
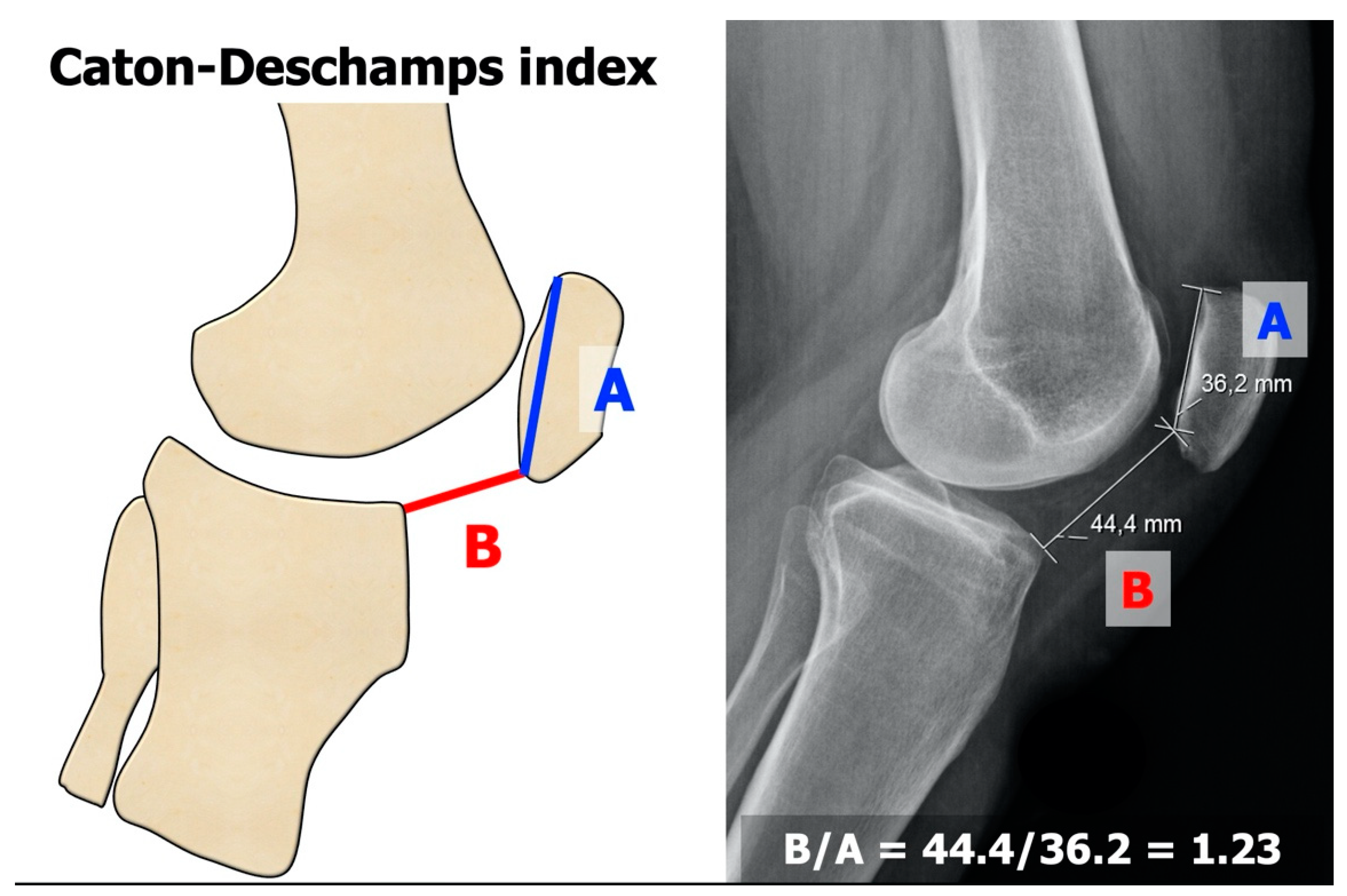
Patella alta: is defined as an excessive patellar height that prevents or limits the patellar engagement on the trochlea during flexion, thus predisposing to patellofemoral instability. It is easily measurable with the Caton-Deschamps Index (CDI) on an accurate lateral knee X-ray[
9,
10]. It is pathological when CDI is greater than or equal to 1.2 (
Figure 3). It is present in 30% of the patellar dislocations [
11].
- 3.
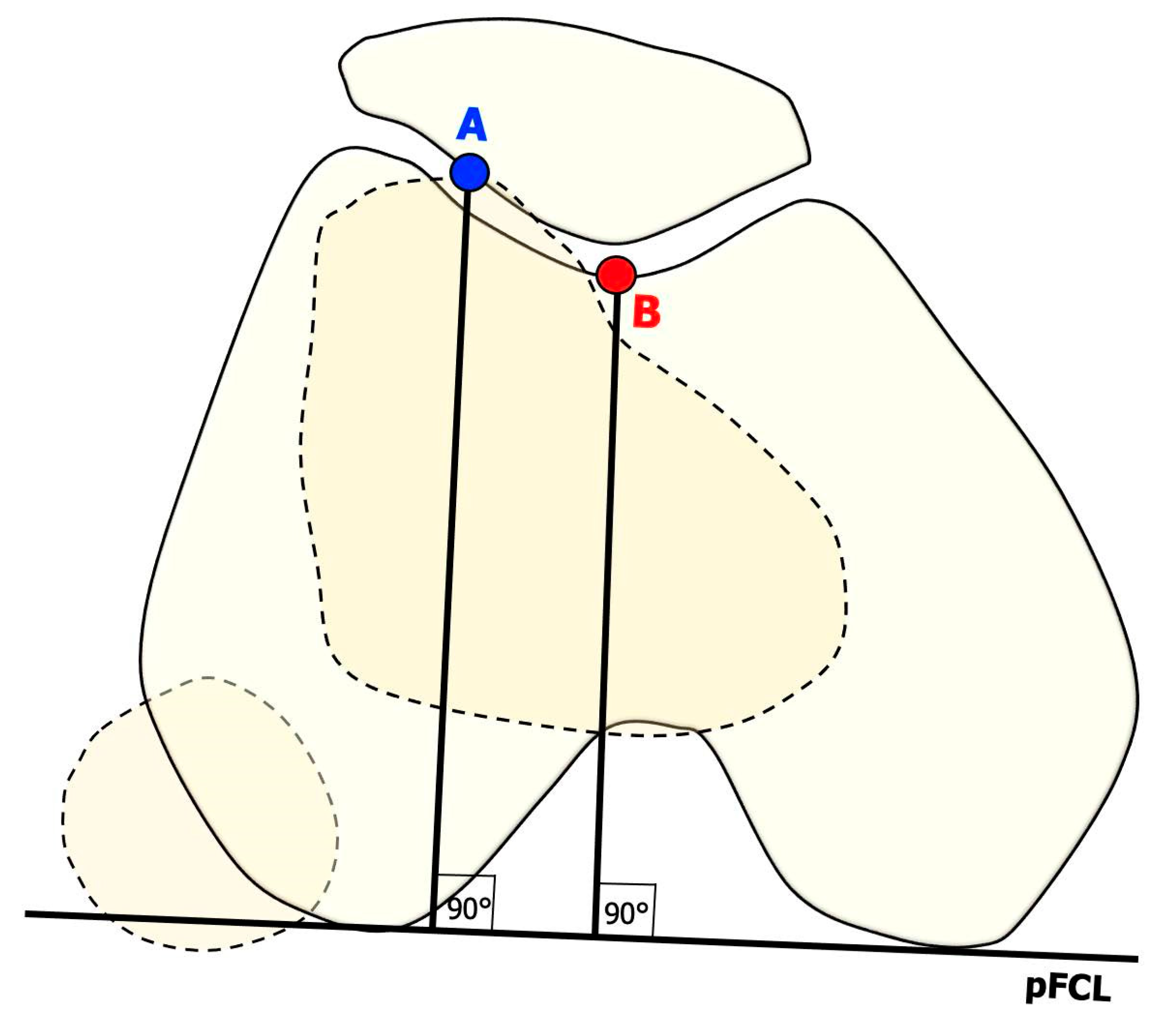
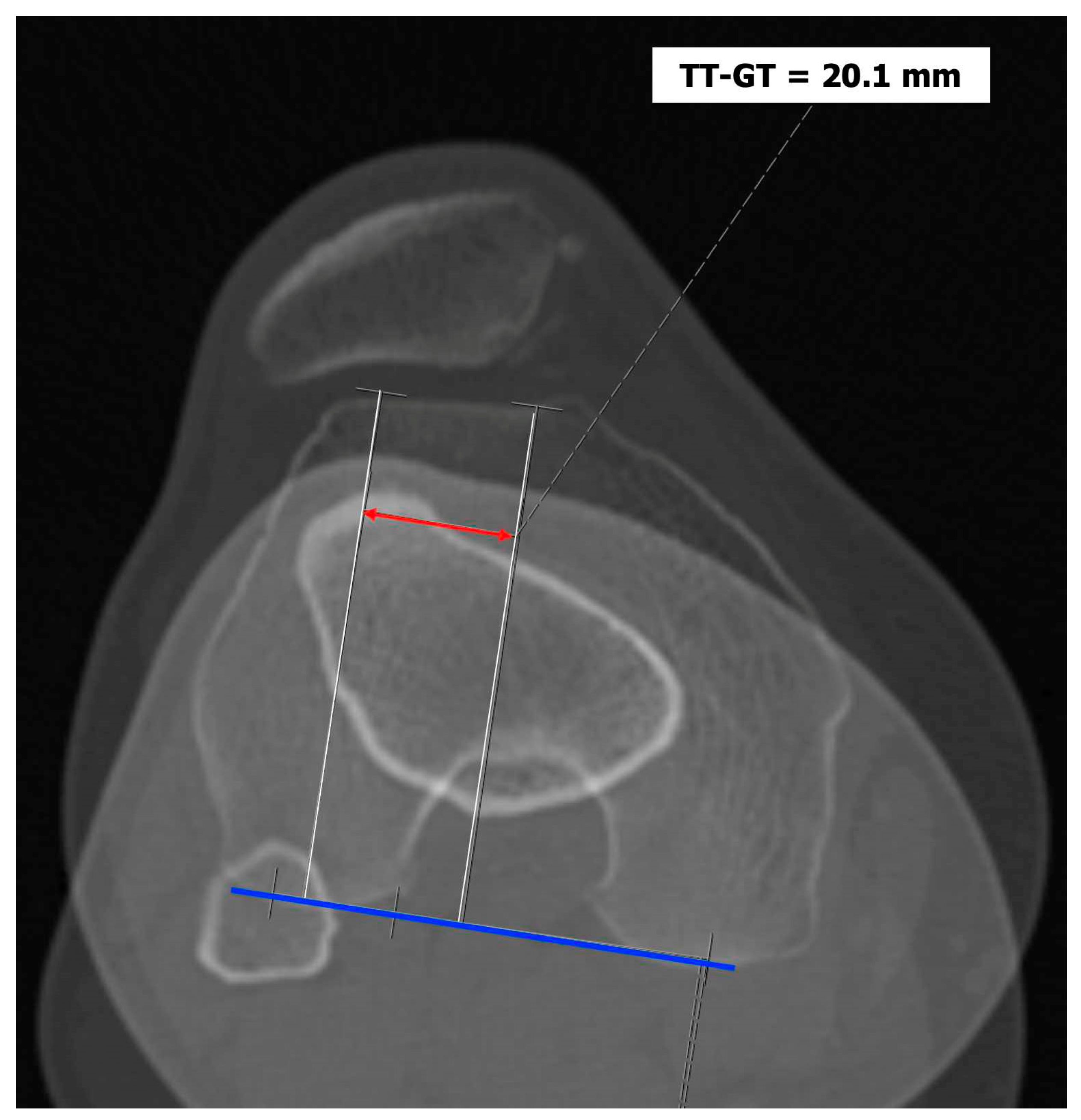
Tibial tuberosity-trochlear groove (TT-TG) distance [
12,
13]: it is defined as the transverse length between the most prominent point of the tibial tuberosity and the trochlear groove on the femur calculated on axial images (CT scan or MRI), representing axial malalignment of the extensor mechanism. The greater the distance, the greater the lateralizing force acting on the patella. It is pathological when TT-TG > 13mm on MRI or TT-TG > 20mm on CT scan (
Figure 4 and
Figure 5).
4. Patellofemoral Instability
When patients present an anatomical predisposition (at least one principal factor of instability), the patella may incur dislocation. In general, the patella dislocates laterally as the extensor mechanism's biomechanics pushes to the knee's lateral side. Other but rare cases of dislocations are classified depending on the patella's position, such as medial dislocation, which is usually iatrogenic, vertical intercondylar dislocation, or horizontal intra-articular dislocation [
14,
15].
Patellofemoral instability can be further classified according to the frequency of dislocation into:
Recurrent, where the patella dislocates frequently during knee flexion (two or more episodes are necessary) [
16];
Habitual, where the patella dislocates every time the knee flexes in early knee flexion (< 30°) and spontaneously relocates with the extension of the knee [
17].
Permanent, where the patella is permanently dislocated through all knee range of motion, never facing the trochlea [
18].
Dislocation is caused by a concomitance of factors, such as sports trauma, genetics, and age to which anatomical predisposition is added.
Patellofemoral dislocation accounts for 3% of knee traumas. The average annual incidence of primary patellar dislocation has been reported to be 5.8 cases per 100,000 in the general population, with the highest incidence occurring in the second decade of life (29 per 100,000) [
19]. It is more common in females and may be associated with other injuries within the knee [
20]. Recurrence rate can be up to 15-44%, and patients with a history of two or more dislocations have a 50% chance of recurrent dislocation episodes, meaning that an important slice of the population goes through primary patellar dislocation will not go through recurrence [
21].
5. Primary Dislocation: Diagnostic Framing
The patient suffering from primary patellar dislocation refers to the emergency room with a painful knee and possible flexion inability. After plain knee radiographs and an axial view of the patella, the physician perform the reduction maneuver. The patient may also arrive at the emergency room with the patella already relocated, only complaining of a painful, swollen knee. On physical examination, typical findings are medial side tenderness due to Medial Patello-Femoral Ligament (MPFL) rupture and swollen knee, which may require aspiration. Patellar dislocation is a common cause of knee hemarthrosis, especially in adolescents [
22].
On the X-rays, trauma surgeons must focus their attention on the following:
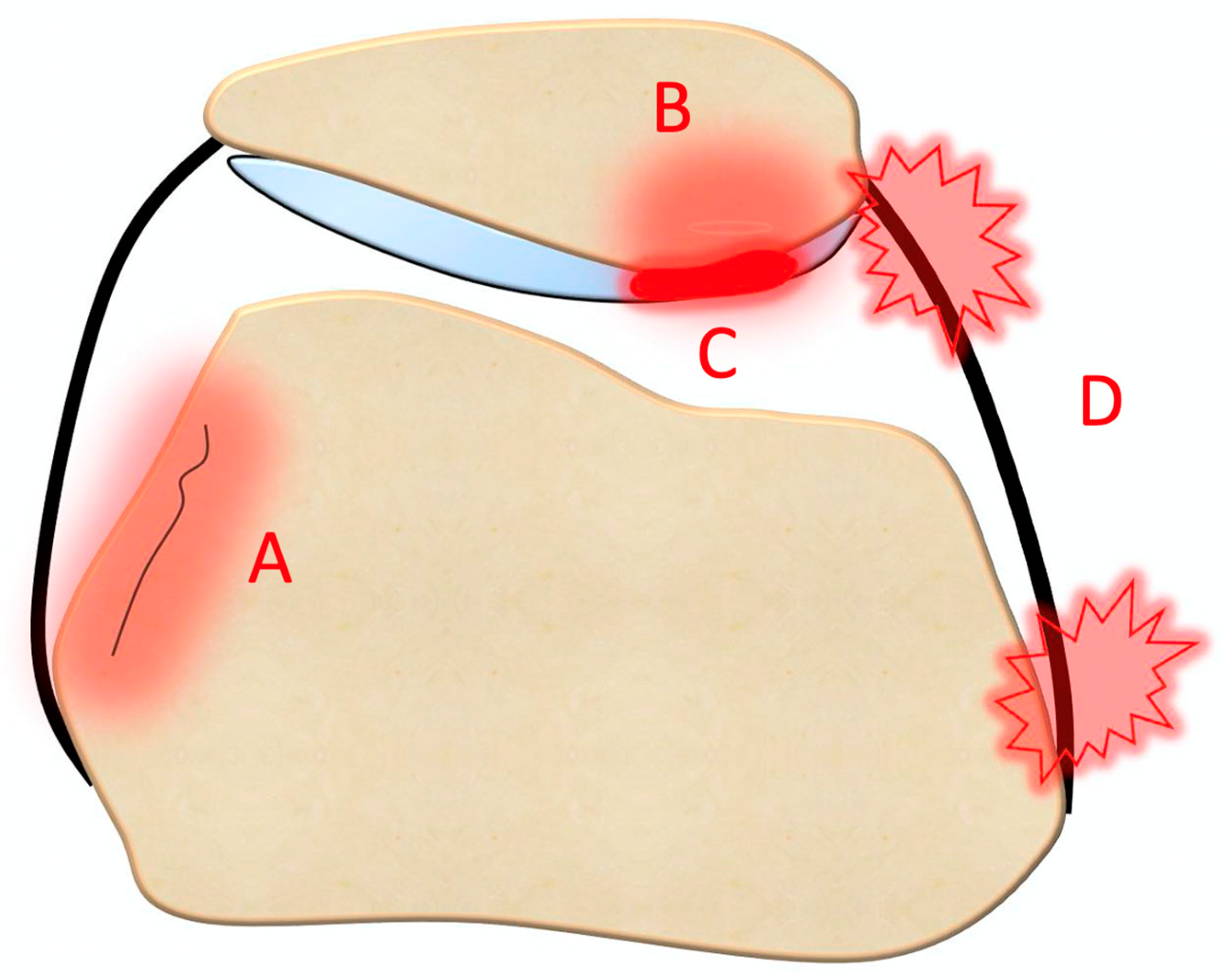
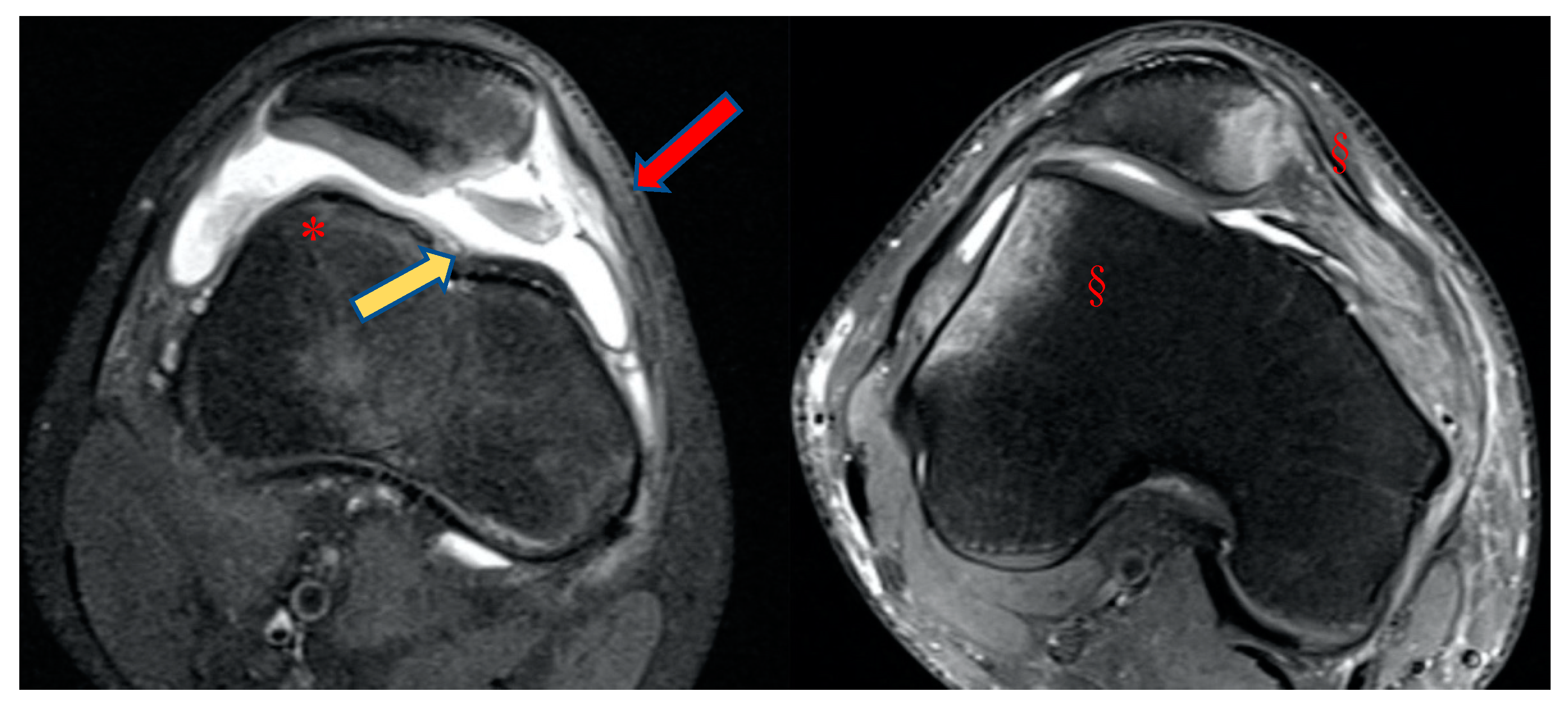
An MRI within few days after trauma is highly recommended in addition to plain radiograph [
24]. Indeed, MRI allows for the detection of (
Figure 6 and
Figure 7):
MRI remains necessary in case of suspected primary patellar dislocation to make a correct diagnosis, to assess concomitant osteocartilaginous injuries, and to evaluate principal factors of instability. Recognizing the abnormalities in bony anatomy after primary dislocation is essential to treating patellar dislocation.
After the first episode, a meticulous physical examination and sufficient imaging modalities are crucial to identify patients with high risk of recurrence [
27,
28]. Skeletally immature patients are also at higher risk of recurrence than adults. Balcarek et al. [
29] proposed the “Patellar Instability Severity Score” (PISS) as a practical tool for initial risk assessment, helping to discriminate between the patients at low risk of recurrence (PISS ≤ 3) and those at high risk of recurrence (PISS ≥ 4, associated with an up to five times greater risk of recurrent dislocation) (
Table 1). PISS is not a therapeutic algorithm; nevertheless, it may help the orthopedic surgeon in correctly informing the patient of his condition and to be more inclined to a conservative or surgical approach. In our opinion, it remains essential to choose a tailored approach to the patient and his condition, avoiding a so-called one-for-all approach.
6. Primary Dislocation: Treatment Options
6.1. Urgent surgery
Primary dislocation with a patellar osteochondral fragment is the only indication for urgent surgery. It consists of osteochondral fixation with pins or screws or darts, absorbable or not absorbable. The dimension of the osteochondral lesion should allow for the use of the fixation devices. MPFL reconstruction is not indicated. After surgery, an immediate rehabilitation protocol is essential. It includes full weight bearing, as the osteochondral lesion is not located in a loading zone, thereby minimizing any impact on the osteochondral fixation. Crutches are recommended for 30 days, while no brace is required. Isometric exercises for quadriceps should be performed. Additionally, a progressive passive motion from 0° to 100° is advised for 45 days. It's important to note that flexion of the knee can engage the patella on the trochlea, potentially affecting the osteochondral fixation. Therefore, passive motion should be stepwise to prevent any adverse effects on the fixation, while still necessary to avoid articular stiffness.
6.2. Conservative treatment
In case of dislocation without osteochondral lesions, surgery is not indicated. Arthrocentesis may relieve the patient’s symptoms. Arthrocentesis also reduces the tension on the capsule and MPFL, allowing for better patellar position and decreasing pain. After surgery, an immediate rehabilitation protocol is implemented to facilitate the recovery process. This protocol includes several components:
Firstly, ice therapy is applied to help reduce swelling and manage pain in the affected area. It is typically administered intermittently for short durations. Full weight bearing is encouraged unless the osteochondral lesion is situated in a loading zone. In such cases, partial weight bearing or non-weight bearing may be advised to protect the affected area. Crutches are utilized for a duration of 30 days to assist with mobility and alleviate pressure on the healing joint. Light patellar bracing is employed to limit tension on the medial patellofemoral ligament (MPFL), supporting its healing and stability during the initial stages of rehabilitation. Isometric exercises of the quadriceps are prescribed to maintain muscle strength and promote stability around the knee joint. Finally, progressive passive motion exercises ranging from 0° to 100° of flexion are performed over a period of 45 days. This gradual increase in motion helps prevent joint stiffness and improve range of motion, ensuring optimal recovery. Overall, this comprehensive rehabilitation protocol aims to promote healing, restore function, and minimize complications following surgery for patellar instability.
7. Primary Dislocation: Follow-up
Follow-up may be scheduled 45 days after injury, with complete imaging screening: X-rays MRI or CT scan. On this occasion, the orthopedic surgeon will assess the effects of the conservative treatment and explain the risk factors for recurrence to the patient by identifying and quantifying the principal factors of instability and PISS score. Return to sport is allowed three months after injury. In addition to the primary factors of instability, it is important for trauma surgeons to also focus on the so-called "secondary factors" of instability. These secondary factors encompass various aspects that can contribute to instability in the knee joint. One of these secondary factors is varus/valgus malalignment of the knee, which refers to the deviation of the knee joint from its normal alignment. This misalignment can put additional stress on the joint and contribute to instability. Another secondary factor is genu recurvatum, which is characterized by hyperextension of the knee joint beyond its normal range. This excessive extension can compromise the stability of the knee and increase the risk of instability. Torsional malalignment of the lower extremities is also an important secondary factor to consider. This involves abnormal rotation of the femur or tibia, such as increased femoral anteversion or increased internal torsion of the distal femur. These rotational abnormalities can affect the alignment and stability of the knee joint. Patellar dysplasia, classified by the Wiberg system [
30], is another secondary factor that can contribute to instability. Patellar dysplasia refers to abnormal development or shape of the patella, which can affect its tracking and stability within the patellofemoral joint. Lastly, abnormal pronation of the subtalar joint can also be a secondary factor of instability. Excessive inward rolling of the foot during walking or running can impact the alignment and stability of the entire lower extremity, including the knee joint.
While the principal factors of instability must be detected with an accurate instrumental evaluation (MRI or CT scan), the secondary factors of instability can initially be assessed clinically. The physical examination starts by analyzing walking and standing positions focusing on varus/valgus malalignment, torsional malalignment, and increased foot pronation. Any clinically evident torsional malalignment of the lower extremities, such as increased femoral anteversion or increased internal torsion of the distal femur, should be better defined by specific imaging evaluation (CT scan). Patellar dysplasia classified by Wiberg can be assessed on an axial view of the patella radiographs. Abnormal pronation of the subtalar joint may require correction with orthotics. It is also suggested to examine the patient sitting with lower legs hanging. In many cases, when asked to actively extend the leg, the patient with patellar instability may present a so-called J sign, which means the patella moves resembling an inverted J while extending the knee. The apprehension test is positive in the majority of patients with patellar instability: the physician gently pushes the patella toward lateral at 0° - 30° - 60° and 90° of flexion, with relaxed quadriceps. Avoidance or protective quadriceps contraction indicates a positive test [
31,
32].
Patellar instability at 0°-30° of knee flexion reflects insufficiency of passive stabilizers (mostly MPFL); instability at 0°-60° of knee flexion depends on insufficiency of passive and often of static stabilizers (pathological TT-TG, trochlear dysplasia, patella alta, and valgus knee). Patellar instability 0°-90° of knee flexion relies on complex rotational bony malalignment.
The study of primary and secondary factors of instability gives us a complete framework of primary patellar instability. In the absence of osteochondral fractures, treatment of primary patellar instability is usually conservative. If recurrence is highly probable (PISS ≥ 4) or important rotational malalignment is present, operative treatment should be considered. Understanding why the patient underwent primary patellar dislocation represents the task of the orthopedic surgeon, allowing them to adopt the best therapeutical approach.
8. Conclusions
Patellofemoral instability can lead to different types of dislocations, making it necessary to establish an accurate diagnosis for primary patellar dislocation. Utilizing MRI is crucial to assess the extent of damage and determine the appropriate treatment options. Additionally, thorough post-treatment follow-up is essential, involving the analysis of both primary and secondary factors of instability. The orthopedic surgeon's role is to understand the underlying cause of the patient's primary patellar dislocation.
Author Contributions
Conceptualization, D.M.M. and R.G.; methodology, L.M.; validation, R.G.; investigation, C.M. and D.A.; resources, C.M. and D.A.; writing—original draft preparation, D.M.M. and R.G.; writing—review and editing, L.M. and G.M.P.; supervision, L.M. and G.M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arendt, E.A.; Dejour, D. Patella instability: building bridges across the ocean a historic review. Knee Surgery, Sports Traumatol. Arthrosc. 2012, 21, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Flandry, F.; Hommel, G. Normal Anatomy and Biomechanics of the Knee. Sports Med. Arthrosc. Rev. 2011, 19, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.J.S.; Wanivenhaus, F.; Rodeo, S.A. The Basic Science of the Patella: Structure, Composition, and Function. J. Knee Surg. 2012, 25, 127–142. [Google Scholar] [CrossRef] [PubMed]
- van Kampen, A.; Huiskes, R. The three-dimensional tracking pattern of the human patella. J. Orthop. Res. 1990, 8, 372–382. [Google Scholar] [CrossRef]
- Nagamine, R.; Otani, T.; White, S.E.; McCarthy, D.S.; Whiteside, L.A. Patellar tracking measurement in the normal knee. J. Orthop. Res. 1995, 13, 115–122. [Google Scholar] [CrossRef]
- Wheatley, M.G.A.; Rainbow, M.J.; Clouthier, A.L. Patellofemoral Mechanics: a Review of Pathomechanics and Research Approaches. Curr. Rev. Musculoskelet. Med. 2020, 13, 326–337. [Google Scholar] [CrossRef]
- DeJour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef]
- Dejour, D. & Saggin, P. The sulcus deepening trochleoplasty-the Lyon’s procedure. Int. Orthop. 34, 311–316 (2010).
- Malghem, J.; Maldague, B. Patellofemoral joint: 30 degrees axial radiograph with lateral rotation of the leg. Radiology 1989, 170, 566–567. [Google Scholar] [CrossRef]
- Caton, J. [Method of measuring the height of the patella]. Acta Orthop. Belg. 1989, 55. [Google Scholar]
- Lewallen, L.; McIntosh, A.; Dahm, D. First-Time Patellofemoral Dislocation: Risk Factors for Recurrent Instability. J. Knee Surg. 2015, 28, 303–310. [Google Scholar] [CrossRef]
- Bayhan, I.A.; Kirat, A.; Alpay, Y.; Ozkul, B.; Kargin, D. Tibial tubercle–trochlear groove distance and angle are higher in children with patellar instability. Knee Surgery, Sports Traumatol. Arthrosc. 2018, 26, 3566–3571. [Google Scholar] [CrossRef] [PubMed]
- Polat, A.E.; Polat, B.; Gürpınar, T.; Sarı, E.; Çarkçı, E.; Erler, K. Tibial tubercle–trochlear groove (TT–TG) distance is a reliable measurement of increased rotational laxity in the knee with an anterior cruciate ligament injury. Knee 2020, 27, 1601–1607. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.A.; Shah, A.B.; Kamal, Y. Vertical Patellar Dislocation: Reduction by the Push Up and Rotate Method, A Case Report and Literature Review. Trauma Mon. 2016, 21. [Google Scholar] [CrossRef]
- Udogwu, U.N.; Sabatini, C.S. Vertical patellar dislocation: A pediatric case report and review of the literature. Orthop. Rev. 2018, 10, 7688. [Google Scholar] [CrossRef]
- Weber, A.E.; Nathani, A.; Dines, J.S.; Allen, A.A.; Shubin-Stein, B.E.; Arendt, E.A.; Bedi, A. An Algorithmic Approach to the Management of Recurrent Lateral Patellar Dislocation. J. Bone Jt. Surg. 2016, 98, 417–427. [Google Scholar] [CrossRef]
- Batra, S. & Arora, S. Habitual dislocation of patella: A review. Journal of Clinical Orthopaedics and Trauma 5, (2014).
- Noda, M.; Saegusa, Y.; Kashiwagi, N.; Seto, Y. Surgical Treatment for Permanent Dislocation of the Patella in Adults. Orthopedics 2011, 34, e948–51. [Google Scholar] [CrossRef]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and Natural History of Acute Patellar Dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef]
- Pagliazzi, G.; Napoli, F.; Previtali, D.; Filardo, G.; Zaffagnini, S.; Candrian, C. A Meta-analysis of Surgical Versus Nonsurgical Treatment of Primary Patella Dislocation. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 2469–2481. [Google Scholar] [CrossRef]
- Kita, K.; Tanaka, Y.; Toritsuka, Y.; Amano, H.; Uchida, R.; Takao, R.; Horibe, S. Factors Affecting the Outcomes of Double-Bundle Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocations Evaluated by Multivariate Analysis. Am. J. Sports Med. 2015, 43, 2988–2996. [Google Scholar] [CrossRef]
- Nikku, R., Nietosvaara, Y., Aalto, K. & Kallio, P. E. The mechanism of primary patellar dislocation: trauma history of 126 patients. Acta Orthop. 80, 432–434 (2009).
- Placella, G.; Tei, M.M.; Sebastiani, E.; Criscenti, G.; Speziali, A.; Mazzola, C.; Georgoulis, A.; Cerulli, G. Shape and size of the medial patellofemoral ligament for the best surgical reconstruction: a human cadaveric study. Knee Surgery, Sports Traumatol. Arthrosc. 2014, 22, 2327–2333. [Google Scholar] [CrossRef]
- Sillanpää, P. J. et al. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am. J. Sports Med. 37, 1513–1521 (2009).
- Elias, D.A.; White, L.M.; Fithian, D.C. Acute Lateral Patellar Dislocation at MR Imaging: Injury Patterns of Medial Patellar Soft-Tissue Restraints and Osteochondral Injuries of the Inferomedial Patella. Radiology 2002, 225, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Conlan, T.; Garth, W.P.; E Lemons, J. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J. Bone Jt. Surg. 1993, 75, 682–693. [Google Scholar] [CrossRef] [PubMed]
- Arendt, E.A.; Askenberger, M.; Agel, J.; Tompkins, M.A. Risk of Redislocation After Primary Patellar Dislocation: A Clinical Prediction Model Based on Magnetic Resonance Imaging Variables. Am. J. Sports Med. 2018, 46, 3385–3390. [Google Scholar] [CrossRef] [PubMed]
- Parikh, S.N.; Lykissas, M.G.; Gkiatas, I. Predicting Risk of Recurrent Patellar Dislocation. Curr. Rev. Musculoskelet. Med. 2018, 11, 253–260. [Google Scholar] [CrossRef]
- Balcarek, P. et al. Which patellae are likely to redislocate? Knee Surg. Sports Traumatol. Arthrosc. 22, 2308–2314 (2014).
- Panni, A.S.; Cerciello, S.; Maffulli, N.; Di Cesare, M.; Servien, E.; Neyret, P. Patellar shape can be a predisposing factor in patellar instability. Knee Surgery, Sports Traumatol. Arthrosc. 2010, 19, 663–670. [Google Scholar] [CrossRef]
- Fairbank, H. A. Internal Derangement of the Knee in Children and Adolescents: (Section of Orthopaedics). Proc. R. Soc. Med. 30, 427–32 (1937).
- Hughston, J. Subluxation of the patella - PubMed. J Bone Jt. Surg Am (1968).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).