Introduction
Cancer is a significant global health concern and remains one of the leading causes of death worldwide. It is characterized by the uncontrolled growth and spread of abnormal cells in the body. With its diverse forms and varying degrees of severity, cancer poses a substantial burden on individuals, families, and healthcare systems globally. Understanding the factors contributing to cancer mortality is crucial for developing effective prevention, early detection, and treatment strategies 1-3. The mortality rate associated with cancer is alarmingly high, impacting millions of lives each year. Lung cancer stands out as a prominent example, with its staggering mortality and morbidity rates. Lung cancer accounts for a substantial portion of cancer-related deaths, particularly among smokers. The prevalence of lung cancer mortality highlights the urgent need for comprehensive tobacco control measures and interventions to reduce the burden of this devastating disease 1,2,4.
Tobacco use is widely recognized as a major contributing factor to the development of various types of cancer. Smoking tobacco, in particular, is strongly associated with an increased risk of lung cancer, as well as other malignancies such as oral, throat, esophageal, pancreatic, and bladder cancers. The harmful chemicals present in tobacco products, including carcinogens such as nicotine, tar, and various toxins, have been linked to DNA damage and the initiation and progression of cancerous cells 2,4-6.
Efforts to mitigate the impact of tobacco use on cancer mortality involve comprehensive tobacco control strategies. These include implementing stringent tobacco control policies, increasing public awareness about the risks of tobacco use, offering smoking cessation programs and resources, and providing support for individuals to quit smoking 4. By addressing tobacco use as a primary risk factor for cancer, healthcare professionals, policymakers, and public health organizations can work collaboratively to reduce the prevalence of cancer-related mortality and improve overall health outcomes 4,7,8.
Nicotine dependence is a significant barrier that hinders individuals, including those diagnosed with cancer and other diseases, from successfully quitting tobacco use. Nicotine, a highly addictive substance found in tobacco products, leads to the development of dependence and makes quitting smoking a challenging endeavor. This dependence on nicotine often becomes a major reason why patients with cancer and other health conditions struggle to quit tobacco use, despite being aware of the detrimental effects on their health 4,7,9-11.
For patients with cancer, nicotine dependence poses additional risks and complexities. The adverse health consequences of continued tobacco use can compromise their treatment outcomes and overall prognosis. Smoking during cancer treatment has been associated with reduced treatment effectiveness, increased risk of complications, poorer response to therapy, and heightened mortality rates. Despite these grave risks, many patients find it incredibly difficult to break free from the grip of nicotine addiction 4,9,11. Moreover, nicotine dependence extends beyond cancer patients and affects individuals with various other diseases as well. Those living with chronic conditions such as cardiovascular diseases, respiratory disorders, and psychiatric illnesses often struggle to quit tobacco use due to the powerful hold of nicotine addiction. Nicotine's impact on the brain's reward system and withdrawal symptoms experienced when attempting to quit make it a formidable challenge for patients to overcome 4,9,11-13.
To address this issue, healthcare providers play a crucial role in supporting patients with cancer and other diseases to quit tobacco use. Tailored interventions, such as medication-assisted treatments and behavioral therapies, should be implemented to address both the physical and psychological aspects of nicotine dependence. Providing education, counseling, and ongoing support is vital in helping patients understand the risks of tobacco use and empowering them to overcome nicotine addiction 8,11,13,14.
By acknowledging nicotine dependence as a major obstacle in quitting tobacco use among patients with cancer and other diseases, healthcare providers can offer tailored interventions and support systems to enhance cessation efforts. By addressing nicotine addiction alongside the treatment of the underlying condition, healthcare professionals can significantly improve patient outcomes and overall well-being.
Background About Tobacco Use and Addition
Worldwide tobacco use, production, and consumption are continuing. Of approximately 1.5 billion smokers in the world, about half of them will die from diseases caused by smoking 4,15,16. Tobacco use has been recognized as a chief avoidable cause of multiple cancers, cardiovascular disease, stroke, complications of pregnancy and chronic obstructive pulmonary disease. Smoking cessation reduces the morbidity and mortality associated with such diseases 4,6,15.
Approximately, one third of the adult male population globally smokes. Smoking related-diseases kill 1 in 10 adults globally. Every eight seconds, someone dies from tobacco use. If current trends continue, smoking is estimated to kill one in 6 people worldwide. Smoking prevalence is on the rise in the developing world, whereas, it is decreasing in developed nations. In the developing world, tobacco consumption is rising by 3.4% per year 8,15,16. Tobacco use is the most preventable cause of death worldwide. It causes more than 435,000 deaths each year in the United States; 45 million (21%) adult Americans are smokers 17-19. Despite the harmful consequences of tobacco use and the population’s awareness of these health problems, approximately 1,200 children and adolescents become new cigarette smokers each day. Even with recommendations to stop smoking, smokers with life-threatening medical problems such as acute coronary syndrome or asthma are unable to quit. In 2015, only 4 to 7 percent of 19 million American adults who attempted to quit smoking were successful. In the United States, unfortunately, 80% of smokers who attempt to quit by themselves relapse within the first month of abstinence; only 3% remain abstinent at 6 months 17-20. These quitting attempt failures may relate to nicotine dependence and/or insufficient motivating factors such as the individual’s confidence in their ability, readiness, and self-efficacy to quit tobacco use 11,13,16,21,22.
Nicotine dependence is a complex phenomenon that involves various neurobiological mechanisms. When nicotine enters the body through smoking or other forms of tobacco use, it quickly reaches the brain and binds to specific receptors known as nicotinic acetylcholine receptors (nAChRs). These receptors are predominantly located in areas of the brain associated with reward, motivation, and reinforcement, such as the ventral tegmental area (VTA) and the nucleus accumbens (NAc). The binding of nicotine to nAChRs triggers the release of several neurotransmitters, including dopamine, serotonin, and norepinephrine, which contribute to the rewarding effects of nicotine 5,9,22,23. Over time, repeated nicotine exposure leads to neuroadaptive changes in the brain. The brain's reward circuitry becomes sensitized to nicotine, leading to an increased motivation to seek and use the drug. This process involves long-term potentiation (LTP) in the synaptic connections between neurons, particularly in the mesolimbic dopamine pathway. The increased release of dopamine in response to nicotine reinforces the association between smoking and pleasurable feelings, making it a highly rewarding behavior. Furthermore, chronic nicotine exposure causes downregulation of nAChRs, reducing their sensitivity to nicotine 5,9,23. This desensitization leads to a decrease in the pleasurable effects of nicotine, promoting the need for higher doses to achieve the same level of reward. The down-regulation of nAChRs is accompanied by changes in other neurotransmitter systems, including glutamate, GABA, and endogenous opioids, which further contribute to the development and maintenance of nicotine dependence 5,9,11,23.
Understanding the neurobiology of nicotine dependence is crucial for developing effective treatments and interventions to help individuals quit smoking. By targeting the specific neural pathways and receptors involved in nicotine addiction, researchers can develop medications and behavioral therapies that address the underlying mechanisms of dependence. Additionally, unraveling the complex interplay between nicotine and the brain can shed light on the development of alternative strategies for smoking cessation and addiction prevention 5,9,11,13,23.
The treatment of nicotine dependence encompasses various approaches, with pharmacological treatment and self-efficacy being two major avenues of intervention. Pharmacological treatment plays a crucial role in aiding individuals in their journey to quit smoking. Nicotine replacement therapy (NRT) is a commonly used pharmacological approach that helps reduce withdrawal symptoms and cravings. NRT involves providing nicotine to the body through different forms such as patches, gum, lozenges, nasal sprays, or inhalers. By delivering controlled amounts of nicotine without the harmful toxins found in tobacco smoke, NRT helps individuals gradually wean off nicotine and manage their addiction 11,13,22. Additionally, certain prescription medications can be used to treat nicotine dependence. One commonly prescribed medication is bupropion, an antidepressant that has been found to help reduce nicotine cravings and withdrawal symptoms. Another medication, varenicline, acts by blocking nicotine receptors in the brain, reducing the pleasurable effects of smoking and making it easier to quit 11,13,22.
In addition to pharmacological interventions, self-efficacy plays a vital role in the treatment of nicotine dependence. Self-efficacy refers to an individual's belief in their ability to quit smoking and resist the urge to smoke 11,13. Behavioral therapies and counseling can help individuals enhance their self-efficacy by providing support, guidance, and strategies to cope with triggers and cravings. These therapies may include cognitive-behavioral techniques, motivational interviewing, and relapse prevention strategies, all aimed at empowering individuals to take control of their addiction and make lasting behavioral changes 5,13,24. Self-efficacy theory has been studied in nursing to assess its effects on health promotion in various health activities such as smoking cessation, cancer prevention, education related to pre- and post-operative care for cardiac surgeries and changing behavior related to drug dependence. Many studies have found that self-efficacy has an important role in improvement of individual performance and change in their adverse behaviors. Moreover, self-efficacy is considered to have an important role in influencing and changing many adverse behaviors including smoking cessation 11,13,21,24.
Combining pharmacological treatment with behavioral therapies and self-efficacy interventions has been shown to be the most effective approach in treating nicotine dependence. This comprehensive approach addresses both the physiological and psychological aspects of addiction, increasing the chances of successful smoking cessation and long-term recovery. It is important for individuals seeking treatment to consult with healthcare professionals who can tailor the treatment plan to their specific needs and provide ongoing support throughout the quitting process 9,11,13,22.
Study Purpose
The purpose of this literature review article is to discuss the neurobiology of nicotine dependence, which is important for understanding tobacco addiction and its treatment for reducing or treating nicotine dependence. Specifically, this paper will discuss: nicotine dependence, the mechanism of nicotine addiction, the neurobiology of nicotine dependence, and brief description of therapeutic approaches to nicotine addiction treatment.
Literature Overview regarding Neurobiology of Nicotine Dependence
Definition of Nicotine Dependence
The term "drug dependence" refers to a socio-psycho-biological syndrome where the use of a particular psychoactive drug takes precedence over other behaviors. Nicotine, a psychoactive drug found in tobacco, is known to reinforce tobacco use. It leads to both psychic and physical dependence. Psychic dependence involves a strong desire for the drug to experience pleasure or avoid discomfort, while physical dependence is characterized by withdrawal symptoms when the drug is discontinued. Different drugs exhibit specific withdrawal syndromes with distinct psychological and physical symptoms 5,11,22,23,25.
The concept of "nicotine addiction" has been acknowledged for decades. Early reports the Advisory Committee to the Surgeon General in 1964 referred to tobacco use as "habituating," and subsequent guideline in 1979 identified smoking as a prototype of substance-abuse dependency. In 1988, the Surgeon General's report unequivocally stated that cigarettes and other tobacco products were highly addictive substances. The terms "dependence" and "addiction" are used interchangeably to describe the neurochemical and psychological processes involved in drug use, including nicotine. While "nicotine addiction" is less commonly used, "nicotine dependence" is a more prevalent term in the literature 9,11,22,25.
In 1988, the Surgeon General established criteria for drug dependence (
Table 1) , comprising primary and secondary criteria
25. Primary criteria define drug dependence and encompass the psychoactive effects of nicotine. Secondary criteria are used to characterize drug dependence and include the development of tolerance, cravings, continued use despite harmful effects, and a high likelihood of relapse after quitting. These criteria serve as guidelines for understanding and assessing nicotine dependence
9,22,25
That Nicotine Use is Addicting
Understanding the pharmacology of nicotine and the neurobiology of nicotine dependence is important for health care providers to help tobacco users quit and prevent relapse. Since 1964, the term, drug habit, was dropped and replaced by drug dependence. The term tobacco addiction began to be used in the literature in the early 1900s 25. The scientific evidences support the idea of nicotine as an addictive drug. This evidence is inferred from experimental studies (e.g., studies that examine the effect of nicotine on mice), clinical studies, and from the theoretical background of the characteristics and actions of nicotine and the diagnostic criteria of addiction. For instance, the US Department of Health and Human Services (USDHHS) in 1988 25 concluded that nicotine has pharmacological effects and produces addiction similar to other addictive drugs such as heroin and cocaine. Scientific evidence demonstrates that nicotine is a psychoactive drug. Nicotine affects all of the human body, particularly the brain. Repeated exposure to nicotine develops neuroadaptation that leads to nicotine tolerance and addiction 9,11,22,25.
There are much evidences that explain the role of nicotine in sustaining tobacco use. The addictive properties of smoking in spite of smoking-related diseases, is one of the major explanation why smokers are unable to quit smoking 9. Benowitz (2008) described the evidence for tobacco addiction: First, tobacco users who smoke are unable to quit easily. Tobacco users who have smoking-related diseases such as cardiovascular disease and cancer fail to quit smoking even after multiple serious quit attempts. On average, most tobacco users who try to stop smoking need four attempts to do so. Approximately 97% of smokers’ unaided quit attempts fail to achieve long-term abstinence. Half of smokers are unable to stop smoking, even though they know that continuing smoking may kill them. Secondly, nicotine is a pharmacologic agent that has physiological and psychological effects on the human body. Nicotine has effects on mood and cognitive function that contribute to tobacco addiction. Smokers report positive effects such as pleasure, relaxation and improved performance, which triggers them to smoke. Finally, maintaining abstinence from tobacco, avoiding nicotine withdrawal symptoms, craving nicotine and preventing relapse can be facilitated by treatment with nicotine replacement medications 9,22.
In addition, the nicotine dependence meets many criteria used to diagnose drug addiction. Nicotine use meets all of the Surgeon General’s primary criteria for drug addiction (
Table 1)
25. According to the DSM-IV criteria, tobacco use is considered a drug addiction when at least three of seven criteria are met within the same 12-month period (
Table 2).
Benowitz (2008) noted that three of these criteria are relevant to tobacco use: nicotine is often taken in larger amounts or over a longer period than was intended, unsuccessful efforts to cut down or control tobacco use, and continuing to use nicotine despite the development of physical or psychological problems that are likely to have been caused or exacerbated by tobacco 9,22. Cohen, McChargue, Garlan, Prensky and Emery (2003) stated that the DSM-IV criteria for the development of tolerance to nicotine and the experience of withdrawal are also relevant to tobacco use 26.
Etiological Risk Factors for Nicotine Dependence
Tobacco addiction is due to the psychological and neurobiological effects of nicotine found in tobacco products. Repeated tobacco use in some specific situations (certain environments, emotional states, and psychosocial stimuli such as depressed mood and anxiety) automatically triggers smokers’ desire for more tobacco use 9,11,22,26. Hatsukami, Stead and Gupta (2008) argued that in addition to the physiological contribution of nicotine dependence, there are many other factors that play an important role in nicotine addiction. These factors include the environmental culture: availability of tobacco products, bans on tobacco use, cost of tobacco, social acceptability, and modeling, for example, parental or peer smoking. They also include the characteristics of the individual: e.g., genes, comorbid psychiatric disorders, and personality features 23. Data show there is variation in genes such as cholinergic nicotine receptor genes, dopamine pathway (dopamine D2 and D4) receptor genes and dopamine transport genes 23. In addition to neurobiological and psychosocial factors, the genetic factor is a risk factor for nicotine dependence. Nicotine dependence also varies across gender 11,23,26. The proportion of tobacco users among men is much higher than among women in some countries such as Japan and Greece, but not in others, such as the United States and the United Kingdom 26,27.
Neurobiology of Nicotine Dependence
Tobacco addiction is a complex neuro-psycho-pharmacological disorder. Addiction is a process involving multiple molecular and brain components. One of the major challenges that face neuroscientists is to piece together the chemical and molecular alterations of the brain in response to addictive drugs 9,11,28,29.
There are several chemical compounds in tobacco; nicotine is the main source of tobacco addiction. It is the most pharmacologically active substance in tobacco. All tobacco forms contain nicotine. Nicotine is a weak base, which mean that half of nicotine is ionized and the other half is non-ionized 9,22,23. When a person smokes, nicotine is absorbed from the tobacco and is carried into the lungs. Nicotine is rapidly absorbed in the lung because of the large surface area of the alveoli and related to weak base, relatively high pH of the lung fluid (7.4) 9,23,25. Then nicotine is carried into the pulmonary venous circulation. Then, it reaches the arterial circulation. Absorbed nicotine diffuses readily into brain tissue and binds to nicotinic acetylcholine receptors (nAChR) 9. The rapid delivery of nicotine to the brain increases its psychoactive rewards, which is associated with drug dependence 9,22.
Nicotine increases activity in the prefrontal cortex, thalamus, corticobasal ganglia-thalamic brain circuits and visual system. When nicotine binds to nicotine receptors, changes in the states of the channels will occur. These changes include the resting (an activated) state (channel open) and two desensitization states (channel closed). Both transition and persistent desensitization states of nicotine receptors lead to nicotine tolerance 9,22.
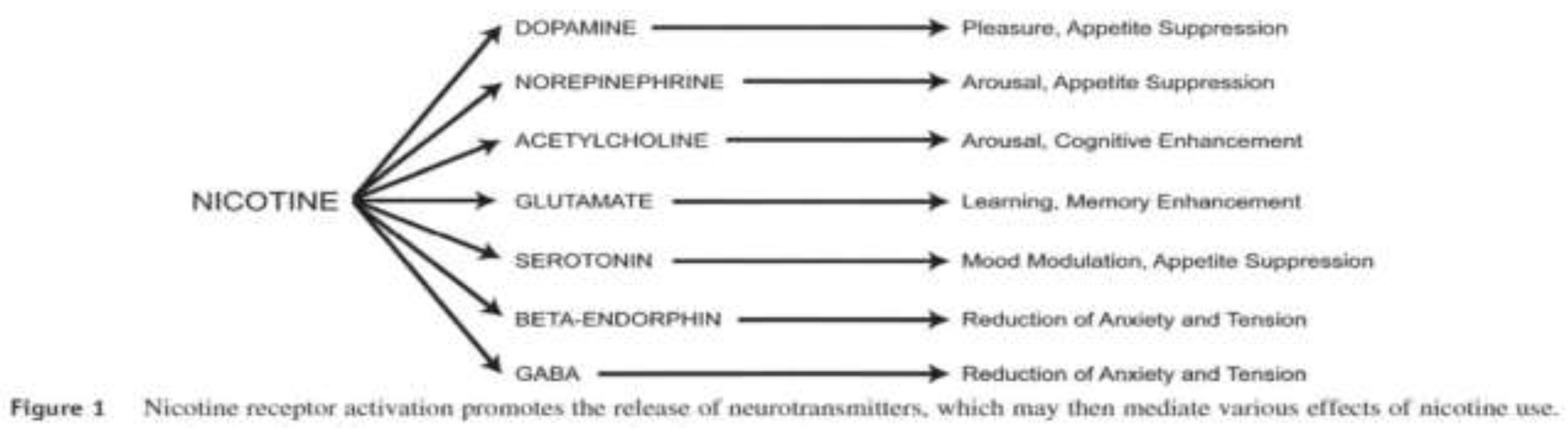
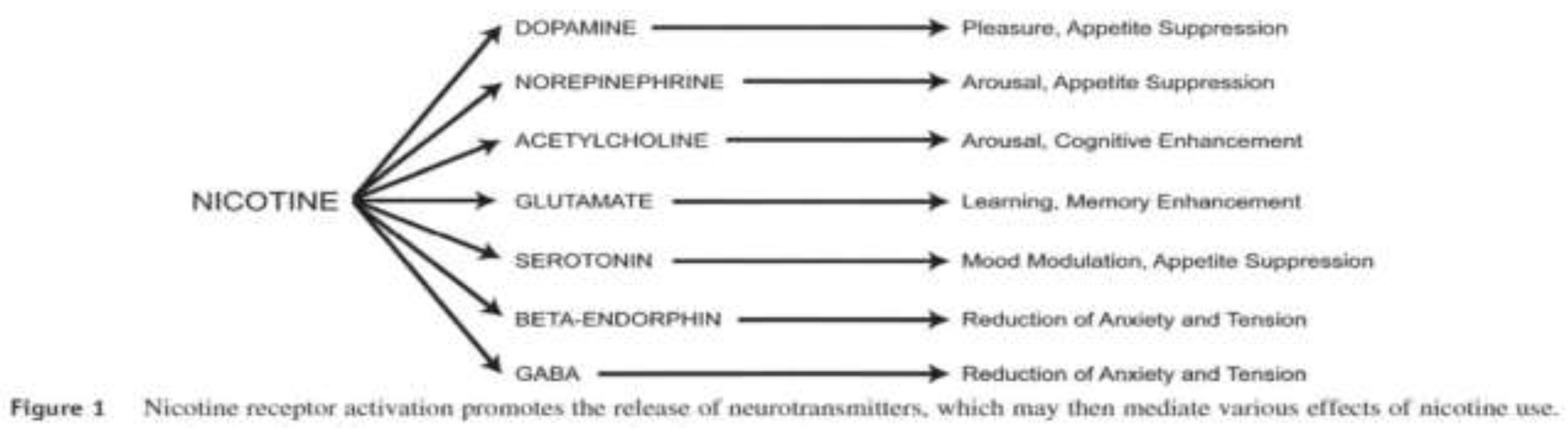
Nicotine acts presynaptically to facilitate release of many brain neurotransmitters, including norepinephrine, acetylcholine, serotonin, γ-aminobutyric acid (GABA), glutamate, endorphins and the most important neurotransmitter, dopamine. Dopamine produces a pleasurable sensation, which leads to the reinforcing effects of nicotine and other drugs of abuse. These neurotransmitters mediate various addiction behaviors. These neurotransmitters lead to reduction of anxiety, pleasure, arousal, cognitive enhancement, mood modulation, performance enhancement, and analgesic and weight-loss effects (Figure 1) 9.
Repeated exposure to nicotine contributes to neuroadaptation, from which the phenomenon of tolerance develops. Tolerance is the state which occurs after repeating doses of a drug, and then given a dose of the drug will not produce the same effect. The dose produces less of an effect than before, and increasing doses are required. Neuroadaptation occurs to attain homoeostasis resulting from the activation of the nAChRs sites and increased concentration of neurotransmitters. Chronic nicotine exposure leads to up-regulatation of some subtypes of nAChRs, an increase in numbers of nAChRs, and produces desensitized (inactivated) nicotine receptors, which are critical for the development of nicotine tolerance 5,9,22,23. In addition, chronic exposure to nicotine reduces brain monoamine oxidase A and B activity. This results in increased monoaminergic neurotransmitter levels such as dopamine and norepinephrine in the synapses, which plays a major role in augmenting the effects of nicotine and contributing to nicotine dependence 9,22,23.
Craving and withdrawal symptoms occur during periods of nicotine abstinence, i.e. night time sleep, when the desensitized α4β2 nAChRs become unoccupied. This explains the daily smoking behavior aimed to maintain the body nearly saturated with nicotine, thus occupying (desensitized) brain nAChRs. Smokers then start smoking soon after they wake up. When smoking, nicotine binds with nicotine receptors, craving and withdrawal are avoided and alleviated through maintaining nAChR desensitization 5,9,22,23.
When smokers stop smoking, the release of neurotransmitters, particularly dopamine, decreases and the body develops a homeostatic response. This causes withdrawal symptoms on abstinence from nicotine. For example, in the state of dopamine deficiency, smokers are unable to experience pleasure 9,23. Nicotine withdrawal symptoms include negative affect such as irritability, restlessness, frustration or anger, anxiety, difficulty concentrating, depressed mood, insomnia, increased appetite or weight gain, decreased heart rate 9,11,23. Other possible symptoms can include constipation, cough, dizziness, increased dreaming and mouth sores. The withdrawal symptoms cause impairment in social, occupational, or other areas of functioning 11,30,31.
Nicotine withdrawal symptoms begin within 1 to 2 days of cessation, peak during the first week, and gradually decrease to pre-cessation levels within approximately 4 weeks 9,12,22. Other studies have shown that nicotine withdrawal symptoms might persist for several months after quitting smoking. Nicotine withdrawal symptoms might increase over the 6 months after quitting, and then decrease or become sustained 9,26,30,31.
Nicotine dependence is produced by a combination of positive reinforcements such as enhanced mood and experience of pleasure and by avoidance of negative reinforcements of nicotine such as relief of withdrawal symptoms. In addition to the direct pharmacologic actions of nicotine, environmental conditioning is involved in the development of nicotine dependence. Environmental conditioning such as the smell of a cigarette, a meal, cup of coffee, talking on the phone, or drinking with friends are common triggers for smoking 9,12,22,26. All drug-taking behavior is learned, a result of conditioning. Conditioning is a major risk factor for relapse to tobacco use after smoking cessation 9,11,12,22.
Prevention, Control, and Treatment of Tobacco Use
Prevention and Control of Nicotine Dependence and Tobacco Use
Cigarette smoking has been universally accepted as a major cause of serious disease and death all over the world. Recent research demonstrates the hazards of smoking and its contribution to many diseases. The intensity of nicotine dependence is dependent upon various factors such as age of starting smoking, form of tobacco use, cigarette consumption per day, and duration of tobacco use 4,7,32. There are many risk factors for nicotine addiction such as psychosocial, environmental, and economic factors for the smoker and society at large. There are many risk factors that can be controlled. Knowledge of the etiological risk factors for nicotine dependence and the neurobiology of nicotine are basic requirements for understanding prevention, control and treatment of nicotine dependence 4,7,11,32.
Health institutions and government agencies collaborate to control tobacco use and to create communities free of tobacco. Smoking cessation programs and policies are established to protect people from the hazards of smoking. These policies vary from country to country. Some have used the WHO Tobacco Convention to legally counter the tobacco industry’s aggressive efforts to get new smokers initiated 4,15,16.
Many countries commonly use tobacco control regulations. These regulations include: raising cigarettes taxes, restricting smoking in public places and on public transportation, prohibiting tobacco advertising, restricting the sale of tobacco products to minors, and putting warning labels about the health hazards of nicotine addiction on tobacco packets 4,16,33,34. There are penalties for persons who violate these regulations. In addition to these regulations, many smoking cessation programs have been initiated. These programs use media campaigns through television ads, radio, official newspapers, billboards, and publications to fight tobacco use, promote health awareness of the hazards of smoking and nicotine dependence, to help people quit smoking 15,16,33,34.
Treatment of Tobacco Use and Nicotine Dependence
Fiore, et al. (2008) described the “5 As” model for treating tobacco use and dependence (Ask-screening all patients for tobacco use, Advice to quit, Assess willingness to quit, Assist with quitting and Arrange follow up) 12. The treatment strategies for this model are as follows: if the patient is willing to quit, the clinician should assist the tobacco user to quit smoking by offering medication and providing counseling or additional treatment based on the tobacco user’s needs and arrange for follow up contacts to prevent relapse. For the patient who is unwilling to make a quit attempt, clinicians are advised to motivate their patients to quit smoking in the future 11-13.
In United States, the USDHHS collaborates with federal agencies and nonprofit organizations in publishing and updating clinical practice guidelines. The USDHHS has published more than 25 reports about the treatment of tobacco use, management of nicotine withdrawal symptoms and prevention of relapse 25. These treatment guidelines have concluded that tobacco dependence is a chronic disease that requires serious interventions to quit 4,12,25. Combinations of counseling and medication are recommended to achieve effective treatment and increase long-term smoking cessation rates 11-13. According to the United Kingdom and US Public Health Service guidelines, all smokers should be considered for pharmacotherapy. It can improve quit rates by 2- to 3-fold 23.
There are many effective medications available for tobacco dependence. These pharmacologic treatments are approved by the US Food and Drug Administration (FDA) 11,22,23. Fiore et al. (2008) listed seven first-line medications (five nicotine replacement therapies (NRT) and two non-NRT). These medications include: Bupropion SR, nicotine gum, nicotine inhaler, nicotine lozenges, nicotine nasal spray, nicotine patch, and Varenicline 12. NRT acts to relieve craving and withdrawal symptoms when the tobacco user quits. NRT reduces the amount and speed of nicotine delivery, reduces reinforcement from smoking and reduces tobacco toxicity 11,12. There is evidence that NRT can be effective in both men and women, but using NRT is contraindicated during pregnancy 12. Non-NRT include agents such as Bupropion and Nortriptyline. Bupropion is an antidepressant drug. It functions as a non-competitive antagonist of the nicotinic acetylcholine receptor. It blocks the reuptake of dopamine and noradrenaline. Nortriptyline is a reuptake inhibitor for noradrenaline and serotonin 11,22,23.
Recently, a new drug has been released, Varenicline, a specific α4 β2 nicotinic receptor partial agonist which acts on dopamine stimulation and blocks nicotine receptors. α4 β2 nAChR partial agonists aim to reduce craving and withdrawal symptoms. It is an effective pharmacotherapeutic tool for quitting tobacco use and reducing risk for relapse 11,22,23.
Many trials are in progress examining a nicotine vaccine, which stimulates the immune system to develop antinicotine antibodies. The results of these trials showed that the nicotine vaccine reduces the distribution of nicotine to the brain in rats. A second clinical trial is ongoing on testing a selective Cannabinoid CB1 receptor antagonist. This drug can block nicotine-induced dopamine release in the nucleus accumbens and reduces nicotine-seeking behavior 23,28,29.
Counseling is an important non-pharmacological intervention for quitting smoking. Teaching smokers about the benefits of smoking cessation, problem solving skills and providing cognitive behavioral therapy and social support as part of treatment can motivate tobacco users to quit 13,16,28,29. The established benefits of counseling can be further enhanced by referring tobacco users to specialists in smoking cessation or to telephone quit lines when smoking cessation specialists are unavailable 13,16,23,28,29.
Research implications and recommendations
The comprehensive literature review article on the neurobiology of nicotine dependence and its implications for tobacco use treatment carries significant research implications and recommendations for healthcare providers. The study's findings highlight the importance of understanding the neurobiological mechanisms underlying nicotine addiction to enhance clinical practice and patient care. Healthcare providers can use this knowledge to develop more effective strategies for tobacco use treatment and smoking cessation interventions.
Firstly, healthcare providers should consider integrating the neurobiological aspects of nicotine dependence into their patient consultations. By educating patients about the addictive nature of nicotine and its impact on the brain, providers can foster a deeper understanding of the challenges individuals face when attempting to quit smoking. This knowledge can increase patient motivation and engagement in treatment, paving the way for more successful outcomes.
Additionally, healthcare providers should adopt a personalized approach to treatment based on the neurobiological profile of each patient. Recognizing that individuals may have unique neurobiological factors influencing their nicotine addiction can help tailor interventions accordingly. By considering factors such as genetic predispositions or variations in neurotransmitter pathways, healthcare providers can offer more targeted pharmacological and behavioral interventions, ultimately improving treatment efficacy.
Furthermore, the research underscores the importance of comprehensive and multidimensional treatment approaches. Healthcare providers should encourage a combination of pharmacological interventions, such as nicotine replacement therapy or prescription medications, with behavioral therapies and counseling. This integrated approach addresses both the physical and psychological aspects of nicotine addiction, providing individuals with a higher likelihood of successful smoking cessation and long-term recovery.
In conclusion, healthcare providers should leverage the insights gained from the neurobiology of nicotine dependence to enhance their practice. By integrating this knowledge into patient consultations, personalizing treatment plans, and embracing comprehensive approaches, providers can significantly contribute to improving tobacco use treatment outcomes and supporting individuals in their journey towards smoking cessation.
Conclusion
The literature review article on the neurobiology of nicotine dependence provides insights into the complex relationship between neurobiology and addiction. It reveals the intricate neural pathways involved in nicotine addiction, shedding light on its physiological and psychological aspects. Understanding the neurobiological basis of nicotine dependence can help healthcare providers enhance their approach to tobacco use treatment and smoking cessation. Implications of the research suggest that healthcare providers should discuss the neurobiology of nicotine addiction with patients to increase awareness and motivation to quit smoking. Personalized treatment approaches based on individual neurobiological profiles can lead to more effective interventions. The study highlights the importance of comprehensive treatment strategies that combine pharmacological interventions and behavioral therapies to address the physical and psychological aspects of nicotine addiction. By embracing these implications, healthcare providers can support individuals in their journey to quit smoking and improve overall well-being. The insights gained from this research contribute to evidence-based practices, guiding healthcare providers to enhance the success rates of tobacco use treatment. Ultimately, this research has the potential to positively impact public health by reducing tobacco-related morbidity and mortality.
Acknowledgments
This study is supported via funding from Prince Sattam Bin Abdulziz University project number (PSAU/2023/R/1444).
References
- Arem H, Loftfield E. Cancer epidemiology: A survey of modifiable risk factors for prevention and survivorship. American journal of lifestyle medicine. 2018;12(3):200-210. [CrossRef]
- McGuire S. World cancer report 2014. Geneva, Switzerland: World Health Organization, international agency for research on cancer, WHO Press, 2015. Advances in nutrition. 2016;7(2):418-419. [CrossRef]
- Kumar SB, Chawla B, Bisht S, Yadav RK, Dada R. Tobacco use increases oxidative DNA damage in sperm-possible etiology of childhood cancer. Asian Pacific Journal of Cancer Prevention. 2015;16(16):6967-6972. [CrossRef]
- Health UDo, Services H. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease …; 2014. [CrossRef]
- Broms U. Nicotine Dependence and Smoking Behaviour: A genetic and epidemiological study. 2008.
- Quach BC, Bray MJ, Gaddis NC, et al. Expanding the genetic architecture of nicotine dependence and its shared genetics with multiple traits. Nature communications. 2020;11(1):5562. [CrossRef]
- 7Le Foll B, Piper ME, Fowler CD, et al. Tobacco and nicotine use. Nature Reviews Disease Primers. 2022;8(1):19.
- Guindon GE, Boisclair D. Past, current and future trends in tobacco use. 2003.
- Benowitz NL. Neurobiology of nicotine addiction: implications for smoking cessation treatment. The American journal of medicine. 2008;121(4):S3-S10. [CrossRef]
- Huang Z, Wu D, Qu X, Li M, Zou J, Tan S. BDNF and nicotine dependence: associations and potential mechanisms. Reviews in the Neurosciences. 2021;32(1):79-91. [CrossRef]
- Elshatarat RA, Saleh ZT. Treatment of nicotine dependence. Journal of Drug Addiction, Education, and Eradication. 2015;11(3/4):213.
- Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update US Public Health Service Clinical Practice Guideline executive summary. Respiratory care. 2008;53(9):1217-1222.
- Elshatarat RA, Yacoub MI, Khraim FM, Saleh ZT, Afaneh TR. Self-efficacy in treating tobacco use: A review article. Proceedings of Singapore Healthcare. 2016;25(4):243-248. [CrossRef]
- Jaén CR, Benowitz NL, Curry SJ, et al. A clinical practice guideline for treating tobacco use and dependence: 2008 update. Am J Prev Med. 2008;35(2):158-176.
- Organization WH. WHO report on the global tobacco epidemic, 2011: warning about the dangers of tobacco. World Health Organization; 2011.
- Organization WH. WHO report on the global tobacco epidemic, 2021: addressing new and emerging products. World Health Organization; 2021.
- Organization WH. WHO global report on trends in prevalence of tobacco smoking 2015. World Health Organization; 2015.
- Organization WH. WHO global report on trends in prevalence of tobacco smoking 2000-2025. World Health Organization; 2018.
- BPsyc TS, Anandan A, Lim CC, et al. Global prevalence of heated tobacco product use, 2015-2022: a systematic review and meta-analysis. Addiction. 2023. [CrossRef]
- Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011–2015. Morbidity and mortality weekly report. 2016;65(14):361-367. [CrossRef]
- Hays JT, Ebbert JO, Sood A. Treating tobacco dependence in light of the 2008 US Department of Health and Human Services clinical practice guideline. Paper presented at: Mayo Clinic Proceedings2009.
- Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clinical Pharmacology & Therapeutics. 2008;83(4):531-541. [CrossRef]
- Hatsukami DK, Stead LF, Gupta PC. Tobacco addiction. The Lancet. 2008;371(9629):2027-2038. [CrossRef]
- Liehr PR. Middle range theory for nursing. 2018. [CrossRef]
- Health UDo, Services H. The health and consequences of smoking. Nicotine addiction: a report of the surgeon general. US Department of Health and Human Services. 1988.
- Cohen LM, McChargue DE, Cortez-Garland M, Prensky EH, Emery S. The etiology and treatment of nicotine dependence: A biopsychosocial perspective. Faculty Publications, Department of Psychology. 2003:306. [CrossRef]
- Health UDo, Services H. The health consequences of smoking: a report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and …; 2004.
- Baker TB, Mermelstein R, Collins LM, et al. New methods for tobacco dependence treatment research. Annals of Behavioral Medicine. 2011;41(2):192-207. [CrossRef]
- Rose JE. New findings on nicotine addiction and treatment. The motivational impact of nicotine and its role in tobacco use. 2009:131-141. [CrossRef]
- Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine & tobacco research. 2007;9(3):315-327. [CrossRef]
- Klemperer EM, Hughes JR, Peasley-Miklus CE, et al. Possible new symptoms of tobacco withdrawal III: Reduced positive affect—A review and meta-analysis. Nicotine and Tobacco Research. 2021;23(2):259-266. [CrossRef]
- 3Bonnie RJ, Stratton K, Kwan LY. The effects of tobacco use on health. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products: National Academies Press (US); 2015.
- Peruga A, López MJ, Martinez C, Fernández E. Tobacco control policies in the 21st century: achievements and open challenges. Molecular oncology. 2021;15(3):744-752. [CrossRef]
- Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tobacco control. 2012;21(2):172-180. [CrossRef]
Table 1.
The Surgeon General's Report: Criteria for Drug Dependence.
Table 1.
The Surgeon General's Report: Criteria for Drug Dependence.
| Primary criteria |
Highly controlled or compulsive use
Psychoactive effects
Drug-reinforced behavior
Additional criteria
Addictive behavior often involves:
Stereotypic patterns of use
Use despite harmful effects
Relapse following abstinence
Recurrent drug cravings
Dependence-producing drugs often produce:
Tolerance
Physical dependence
Pleasant (euphoriant) effects
|
Data from the US Department of Health and Human Services (1988).
|
Table 2.
Criteria for drug dependence *.
Table 2.
Criteria for drug dependence *.
| A maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by ≥3 of the following criteria occurring at any time in the same 12-month period: |
1. Tolerance, as defined by either of the following:
a. Need for markedly increased amounts of the substance to achieve intoxication or desired effect
b. Markedly diminished effect with continued use of the same amount of the substance
2. Withdrawal, as manifested by either of the following:
a. The characteristic withdrawal syndrome for the substance
b. The same (or closely related) substance is taken to relieve or avoid withdrawal symptoms
3. The substance is often taken in larger amounts or over a longer period than was intended
4. There is a persistent desire or unsuccessful efforts to cut down or control substance use
5. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects
6. Important social, occupational, or recreational activities are given up or reduced because of substance use
7. The substance use is continued despite knowledge of having had a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance
|
* Criteria from the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV).
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).