Submitted:
29 June 2023
Posted:
29 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study design
2.2. Study population:
2.3. Pretreatment, isolation, and purification of nucleic acids:
2.4. Human papillomavirus testing:
2.5. Study outcomes:
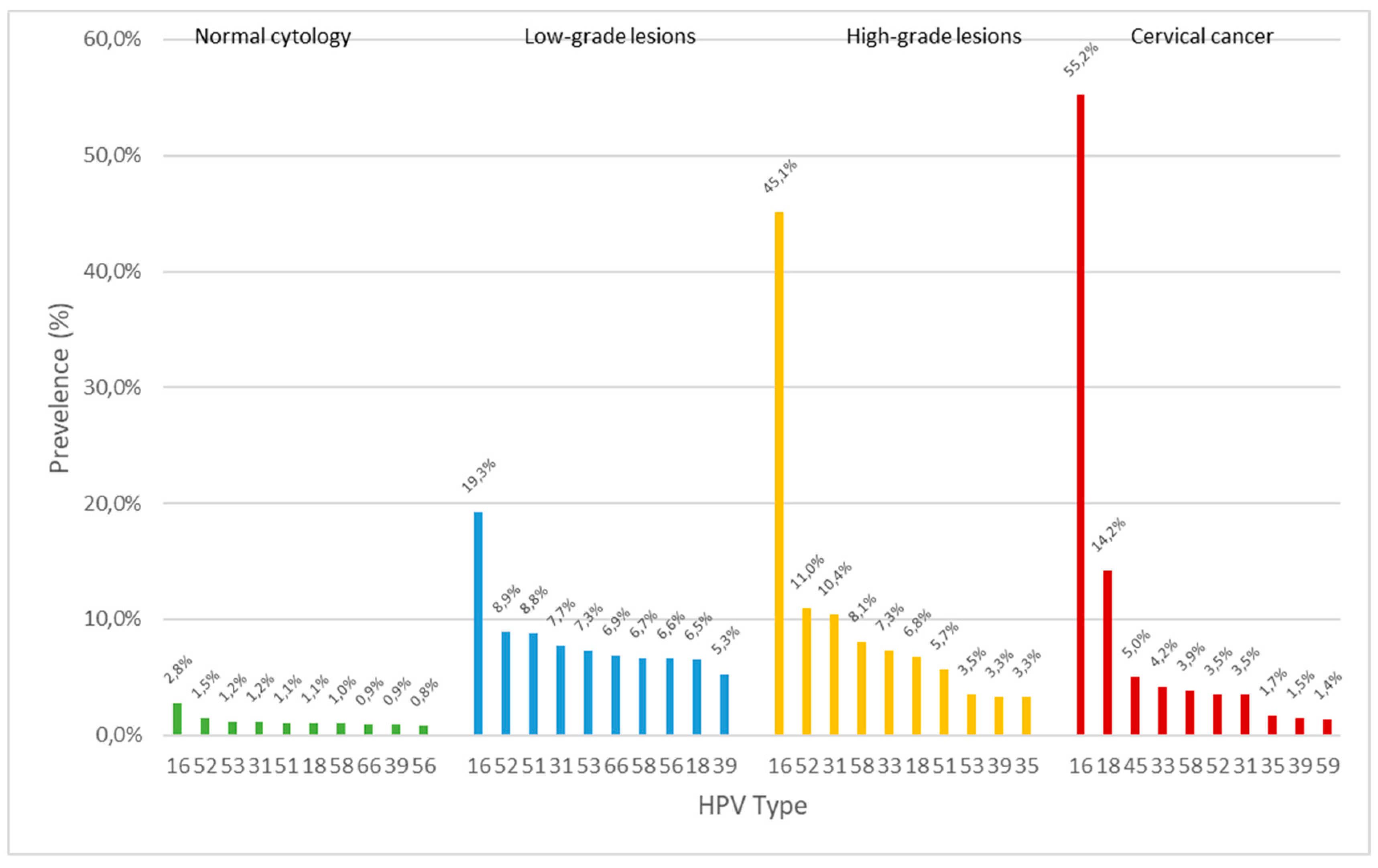
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12-9. [CrossRef]
- Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
- Petersen Z, Jaca A, Ginindza TG, Maseko G, Takatshana S, Ndlovu P, Zondi N, Zungu N, Varghese C, Hunting G, Parham G, Simelela P, Moyo S. Barriers to uptake of cervical cancer screening services in low-and-middle-income countries: a systematic review. BMC Womens Health. 2022 Dec 2;22(1):486. [CrossRef]
- Ronco, G.; Dillner, J.; Elfstrom, K.M.; Tunesi, S.; Snijders, P.J.; Arbyn, M.; Kitchener, H.; Segnan, N.; Gilham, C.; Giorgi-Rossi, P.; et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: Follow-up of four European randomised controlled trials. Lancet 2014, 383, 524–532. [CrossRef]
- Engesæter, B.; Groeneveld, L.F.; Skare, G.B.; Tropé, A. Annual Report of the Cervical Cancer Screening Program in Norway 2021. Kreftregisteret, Institute of Population-Based Cancer Research, Oslo, Norway. Production: Kreftregisteret. Available online: www.kreftregisteret.no/livmorhals (accessed June 2022).
- Norwegian Institute of Public Health (NIPH). "High vaccine uptake in the childhood immunisation programme." News. Published 07.04.2022. Available online: https://www.fhi.no/en/news/2022/high-vaccine-uptake-in-the-childhood-immunisation-programme/ (accessed June 2022).
- Kreftregisteret (The Cancer Registry of Norway). (n.d.). Livmorhalskreft [Cervical Cancer]. Available online: https://www.kreftregisteret.no/Temasider/kreftformer/Livmorhalskreft/ (accessed June 2023).
- zur Hausen, H. Papillomaviruses and cancer: From basic studies to clinical application. Nat. Rev. Cancer 2002, 2, 342–350. [CrossRef]
- Bosch FX. HPV vaccines and cervical cancer. Ann Oncol. 2008 Jul;19 Suppl 5:v48-51. [CrossRef]
- Joura EA, Ault KA, Bosch FX, Brown D, Cuzick J, Ferris D, Garland SM, Giuliano AR, Hernandez-Avila M, Huh W, Iversen OE, Kjaer SK, Luna J, Miller D, Monsonego J, Munoz N, Myers E, Paavonen J, Pitisuttithum P, Steben M, Wheeler CM, Perez G, Saah A, Luxembourg A, Sings HL, Velicer C. Attribution of 12 high-risk human papillomavirus genotypes to infection and cervical disease. Cancer Epidemiol Biomarkers Prev. 2014 Oct;23(10):1997-2008. [CrossRef]
- Serrano B, de Sanjosé S, Tous S, Quiros B, Muñoz N, Bosch X, Alemany L. Human papillomavirus genotype attribution for HPVs 6, 11, 16, 18, 31, 33, 45, 52 and 58 in female anogenital lesions. Eur J Cancer. 2015 Sep;51(13):1732-41. [CrossRef]
- de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, Tous S, Felix A, Bravo LE, Shin HR, Vallejos CS, de Ruiz PA, Lima MA, Guimera N, Clavero O, Alejo M, Llombart-Bosch A, Cheng-Yang C, Tatti SA, Kasamatsu E, Iljazovic E, Odida M, Prado R, Seoud M, Grce M, Usubutun A, Jain A, Suarez GA, Lombardi LE, Banjo A, Menéndez C, Domingo EJ, Velasco J, Nessa A, Chichareon SC, Qiao YL, Lerma E, Garland SM, Sasagawa T, Ferrera A, Hammouda D, Mariani L, Pelayo A, Steiner I, Oliva E, Meijer CJ, Al-Jassar WF, Cruz E, Wright TC, Puras A, Llave CL, Tzardi M, Agorastos T, Garcia-Barriola V, Clavel C, Ordi J, Andújar M, Castellsagué X, Sánchez GI, Nowakowski AM, Bornstein J, Muñoz N, Bosch FX; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010 Nov;11(11):1048-56. [CrossRef]
- Bonde, J.H.; Sandri, M.T.; Gary, D.S.; Andrews, J.C. Clinical Utility of Human Papillomavirus Genotyping in Cervical Cancer Screening: A Systematic Review. J. Low. Genit. Tract. Dis. 2020, 24, 1–13. [CrossRef]
- Arbyn, M.; Tommasino, M.; Depuydt, C.; Dillner, J. Are 20 human papillomavirus types causing cervical cancer? J. Pathol. 2014, 234, 431–435. [CrossRef]
- Kjaer SK, Nygård M, Sundström K, Munk C, Berger S, Dzabic M, Fridrich KE, Waldstrøm M, Sørbye SW, Bautista O, Group T, Luxembourg A. Long-term effectiveness of the nine-valent human papillomavirus vaccine in Scandinavian women: interim analysis after 8 years of follow-up. Hum Vaccin Immunother. 2021 Apr 3;17(4):943-949. [CrossRef]
- Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report 10 March 2023. Available online: https://hpvcentre.net/statistics/reports/XWX.pdf?t=1687952491692 (accessed June 2023).
- van den Brule AJ, Pol R, Fransen-Daalmeijer N, et al. GP5+/6+ PCR followed by reverse line blot analysis enables rapid and high-throughput identification of human papillomavirus genotypes. J Clin Microbiol 2002;40:779–87. [CrossRef]
- Snijders PJ, van den Brule AJ, Jacobs MV, et al. HPV DNA detection and typing in cervical scrapes. Methods Mol Med 2005;119:101–14. [CrossRef]
- Guan P, Howell-Jones R, Li N, Bruni L, de Sanjosé S, Franceschi S, Clifford GM. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012 Nov 15;131(10):2349-59. [CrossRef]
- So KA, Lee IH, Lee KH, Hong SR, Kim YJ, Seo HH, Kim TJ. Human papillomavirus genotype-specific risk in cervical carcinogenesis. J Gynecol Oncol. 2019 Jul;30(4):e52. [CrossRef]
- Nygård M, Hansen BT, Kjaer SK, Hortlund M, Tryggvadóttir L, Munk C, Lagheden C, Sigurdardottir LG, Campbell S, Liaw KL, Dillner J. Human papillomavirus genotype-specific risks for cervical intraepithelial lesions. Hum Vaccin Immunother. 2021 Apr 3;17(4):972-981. [CrossRef]
- Sundström K, Dillner J. How Many Human Papillomavirus Types Do We Need to Screen For? J Infect Dis. 2021 May 20;223(9):1510-1511. [CrossRef]
- Arbyn M, Weiderpass E, Bruni L, de Sanjose S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8:e191-203. [CrossRef]
- Gravdal, B.H., Lönnberg, S., Skare, G.B. et al. Cervical cancer in women under 30 years of age in Norway: a population-based cohort study. BMC Women's Health 21, 110 (2021). [CrossRef]
- Simopekka Vänskä and others, Differing Age-Specific Cervical Cancer Incidence Between Different Types of Human Papillomavirus: Implications for Predicting the Impact of Elimination Programs, American Journal of Epidemiology, Volume 190, Issue 4, April 2021, Pages 506–514. [CrossRef]
- Tjalma WA, Fiander A, Reich O, Powell N, Nowakowski AM, Kirschner B, Koiss R, O'Leary J, Joura EA, Rosenlund M, Colau B, Schledermann D, Kukk K, Damaskou V, Repanti M, Vladareanu R, Kolomiets L, Savicheva A, Shipitsyna E, Ordi J, Molijn A, Quint W, Raillard A, Rosillon D, De Souza SC, Jenkins D, Holl K; HERACLES/SCALE Study Group. Differences in human papillomavirus type distribution in high-grade cervical intraepithelial neoplasia and invasive cervical cancer in Europe. Int J Cancer. 2013 Feb 15;132(4):854-67. [CrossRef]
- Rad A, Sørbye SW, Dreyer G, Hovland S, Falang BM, Louw M, Skjeldestad FE. HPV types in cervical cancer tissue in South Africa: A head-to-head comparison by mRNA and DNA tests. Medicine (Baltimore). 2017 Nov;96(47):e8752. [CrossRef]
- Lehtinen M, Pimenoff VN, Nedjai B, Louvanto K, Verhoef L, Heideman DAM, El-Zein M, Widschwendter M, Dillner J. Assessing the risk of cervical neoplasia in the post-HPV vaccination era. Int J Cancer. 2023 Mar 15;152(6):1060-1068. [CrossRef]
- El-Zein M, Richardson L, Franco EL. Cervical cancer screening of HPV vaccinated populations: Cytology, molecular testing, both or none. J Clin Virol. 2016 Mar;76 Suppl 1(Suppl 1):S62-S68. [CrossRef]
- Lei J, Ploner A, Lehtinen M, Sparén P, Dillner J, Elfström KM. Impact of HPV vaccination on cervical screening performance: a population-based cohort study. Br J Cancer. 2020 Jul;123(1):155-160. [CrossRef]
- Baasland I, Romundstad PR, Eide ML, Jonassen CM. Clinical performance of Anyplex II HPV28 by human papillomavirus type and viral load in a referral population. PLoS One. 2019 Jan 23;14(1):e0210997. [CrossRef]
- Sorbye, S.W.; Fismen, S.; Gutteberg, T.J.; Mortensen, E.S.; Skjeldestad, F.E. HPV mRNA is more specific than HPV DNA in triage of women with minor cervical lesions. PLoS ONE 2014, 9, e112934. [CrossRef]
- Origoni, M.; Cristoforoni, P.; Carminati, G.; Stefani, C.; Costa, S.; Sandri, M.T.; Mariani, L.; Preti, M. E6/E7 mRNA testing for human papilloma virus-induced high-grade cervical intraepithelial disease (CIN2/CIN3): A promising perspective. Ecancermedicalscience 2015, 9, 533. [CrossRef]
- Westre, B.; Giske, A.; Guttormsen, H.; Sorbye, S.W.; Skjeldestad, F.E. 5-type HPV mRNA versus 14-type HPV DNA test: Test performance, over-diagnosis and overtreatment in triage of women with minor cervical lesions. BMC Clin. Pathol. 2016, 16, 9. [CrossRef]
- Sorbye, S.W.; Fismen, S.; Gutteberg, T.; Mortensen, E.S. Triage of women with minor cervical lesions: Data suggesting a “test and treat” approach for HPV E6/E7 mRNA testing. PLoS ONE 2010, 5, e12724. [CrossRef]
| HPV DNA Results | HPV mRNA Results | |||||
|---|---|---|---|---|---|---|
| Frequency | Percent | Cumulative Percent | Frequency | Percent | Cumulative | |
| Type | n | (%) | (%) | n | (%) | Percent (%) |
| HPV 16 | 89 | 50.0 | 50.0 | 90 | 50.6 | 50.6 |
| HPV 18 | 31 | 17.4 | 67.4 | 32 | 18.0 | 68.6 |
| HPV 45 | 13 | 7.3 | 74.7 | 13 | 7.3 | 75.9 |
| HPV 33 | 9 | 5.1 | 79.8 | 8 | 4.5 | 80.4 |
| HPV 35 | 8 | 4.5 | 84.3 | * | * | * |
| HPV 31 | 4 | 2.2 | 86.5 | 4 | 2.2 | 82.6 |
| HPV 39 | 2 | 1.1 | 87.6 | * | * | * |
| HPV 52 | 1 | 0.6 | 88.2 | 1 | 0.6 | 83.2 |
| HPV 58 | 1 | 0.6 | 88.8 | 1 | 0.6 | 83.8 |
| HPV 73 | 1 | 0.6 | 89.4 | * | * | * |
| Negative | 19 | 10.7 | 100.0 | 29 | 16.3 | 100.0 |
| Total | 178 | 100.0 | 178 | 100.0 | ||
| HPV mRNA | Total | |||
|---|---|---|---|---|
| Negative | Positive | |||
| HPV DNA | Negative | 16 | 3 | 19 |
| Positive | 13 | 146 | 159 | |
| Total | 29 | 149 | 178 | |
| Sample# | Biopsy (Year) |
Age CxCa Diagnosis |
Routine Screening (YES/NO) |
Last Normal Cytology (Years) |
First Abnormal Cytology (Years) |
Last Cytology Diagnosis |
Screening Failure (YES/NO) |
HPV Test LBC (NT/type) |
|---|---|---|---|---|---|---|---|---|
| 1 | 1996 | 38 | NO | 14 | 0 | Normal | NO | NT |
| 2 | 1996 | 34 | YES | 1 | 0 | ASC-H | YES | 16 |
| 3 | 1998 | 45 | YES | 5 | 5 | HSIL | YES | NT |
| 4 | 1998 | 57 | NO | 1 | 5 | ASC-US | YES | NT |
| 5 | 2005 | 63 | NO | 32 | 0 | Normal | NO | NT |
| 6 | 2006 | 56 | NO | 1 | 3 | ASC-H | YES | NT |
| 7 | 2007 | 78 | NO | 6 | 28 | Normal | YES | NT |
| 8 | 2010 | 67 | YES | 5 | 5 | HSIL | NO | NT |
| 9 | 2010 | 75 | NO | 3 | 0 | Normal | YES | NT |
| 10 | 2011 | 49 | YES | 0 | 0 | ASC-H | YES | NT |
| 11 | 2011 | 70 | NO | 8 | 28 | Normal | NO | NT |
| 12 | 2012 | 47 | NO | 1 | 4 | ASC-US | YES | NT |
| 13 | 2012 | 79 | NO | 0 | 0 | Normal | YES | NT |
| 14 | 2014 | 44 | NO | 3 | 0 | ASC-H | YES | 16 |
| 15 | 2015 | 55 | NO | 9 | 0 | HSIL | NO | NT |
| 16 | 2015 | 30 | YES | Missing | 1 | LSIL | NO | 16 |
| HPV Type (DNA/mRNA) |
Frequency n |
Percent (%) |
Cumulative Percent (%) |
Screen Detected n (%) |
Symptom Detected n (%) |
|
|---|---|---|---|---|---|---|
| HPV 16 | 94 | 52.8 | 52.8 | 41 (57.7) | 53 (49.5) | |
| HPV 18 | 32 | 18.0 | 70.8 | 19 (26.8) | 13 (12.1) | |
| HPV 45 | 13 | 7.3 | 78.1 | 2 (2.8) | 11 (10.3) | |
| HPV 33 | 9 | 5.1 | 83.2 | 3 (4.2) | 6 (5.6) | |
| HPV 35 | 8 | 4.5 | 87.7 | 1 (1.4) | 7 (6.5) | |
| HPV 31 | 4 | 2.2 | 89.9 | 1 (1.4) | 3 (2.8) | |
| HPV 39 | 2 | 1.1 | 91.0 | 0 (0.0) | 2 (1.9) | |
| HPV 52 | 1 | 0.6 | 91.6 | 0 (0.0) | 1 (0.9) | |
| HPV 58 | 1 | 0.6 | 92.2 | 0 (0.0) | 1 (0.9) | |
| HPV 73 | 1 | 0.6 | 92.8 | 1 (1.4) | 0 (0.0) | |
| Negative | 13 | 7.3 | 100.0 | 3 (4.2) | 10 (9.3) | |
| Total | 178 | 100.0 | 71 (100.0) | 107 (100.0) | ||
| HPV Type | Age Mean |
N | SD | Cumulative % |
|---|---|---|---|---|
| Negative | 59.9 | 13 | 13.28 | 7.3 |
| 16 | 45.3 | 94 | 15.29 | 60.1 |
| 18 | 44.3 | 32 | 11.37 | 78.1 |
| 45 | 45.5 | 13 | 10.49 | 85.4 |
| Other* | 51.6 | 26 | 15.49 | 100.0 |
| Total | 47.1 | 178 | 14.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




