Submitted:
29 June 2023
Posted:
30 June 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Admissions, beds endowment, population data and catchment area
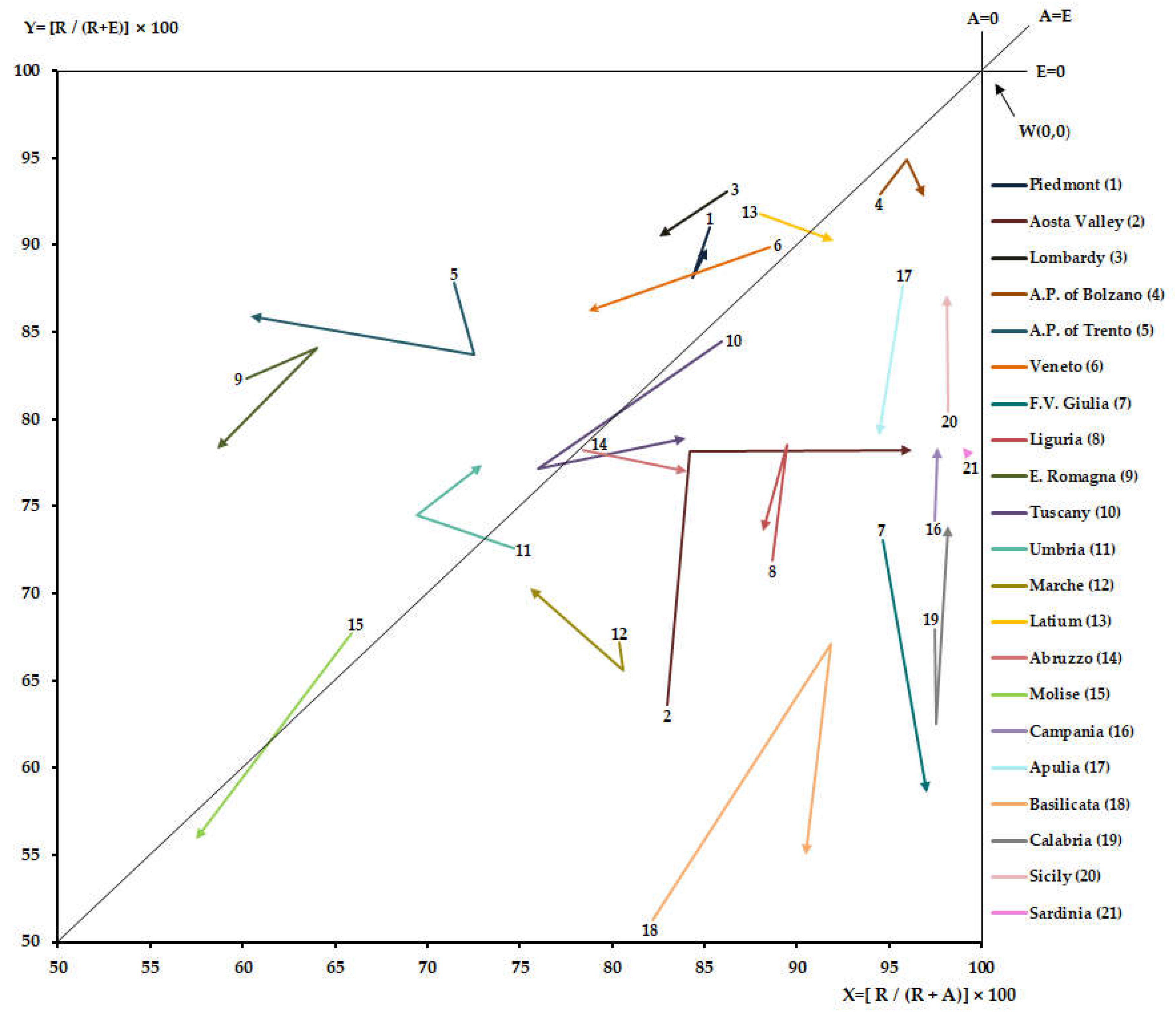
2.2. Gandy's Nomogram
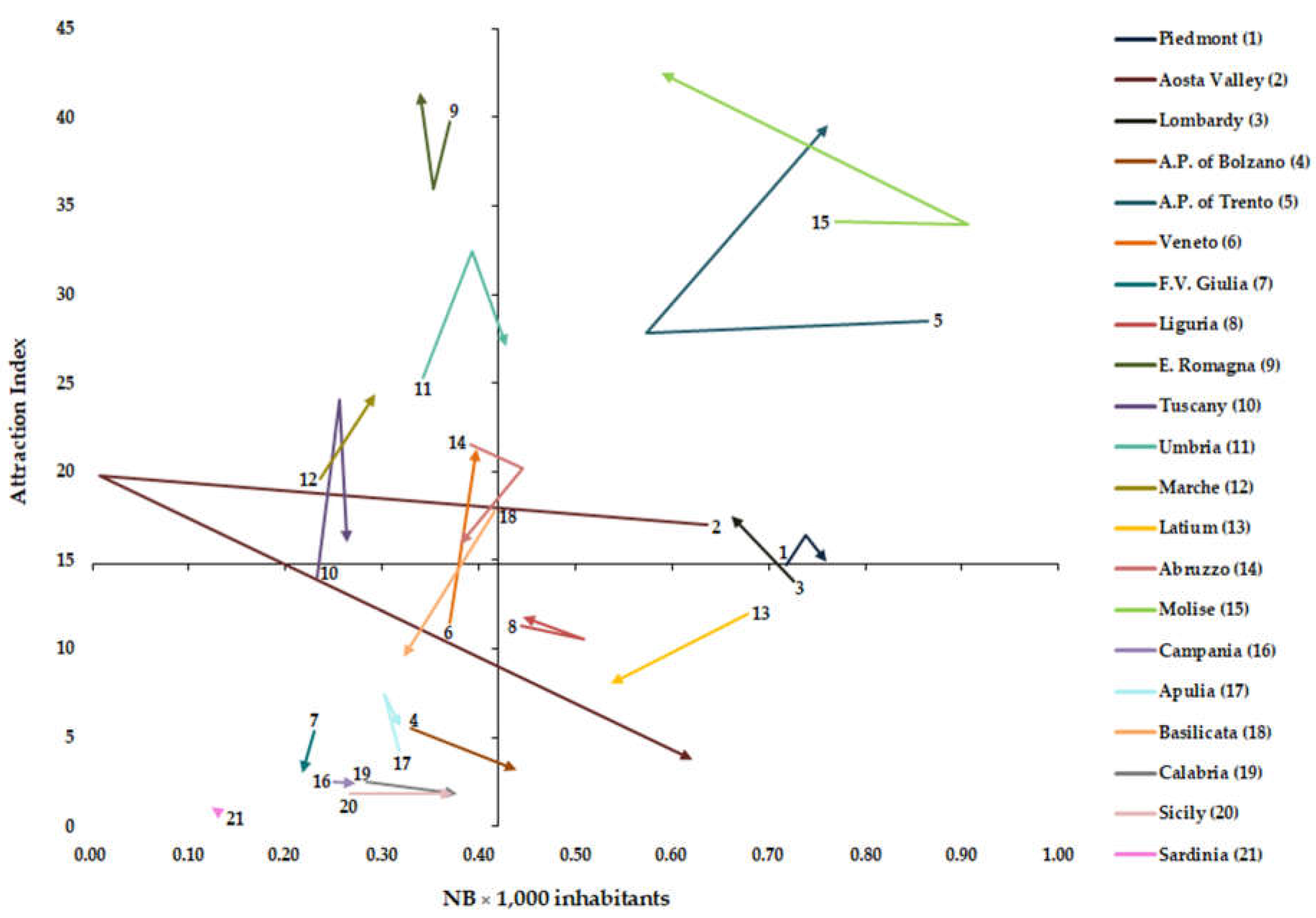
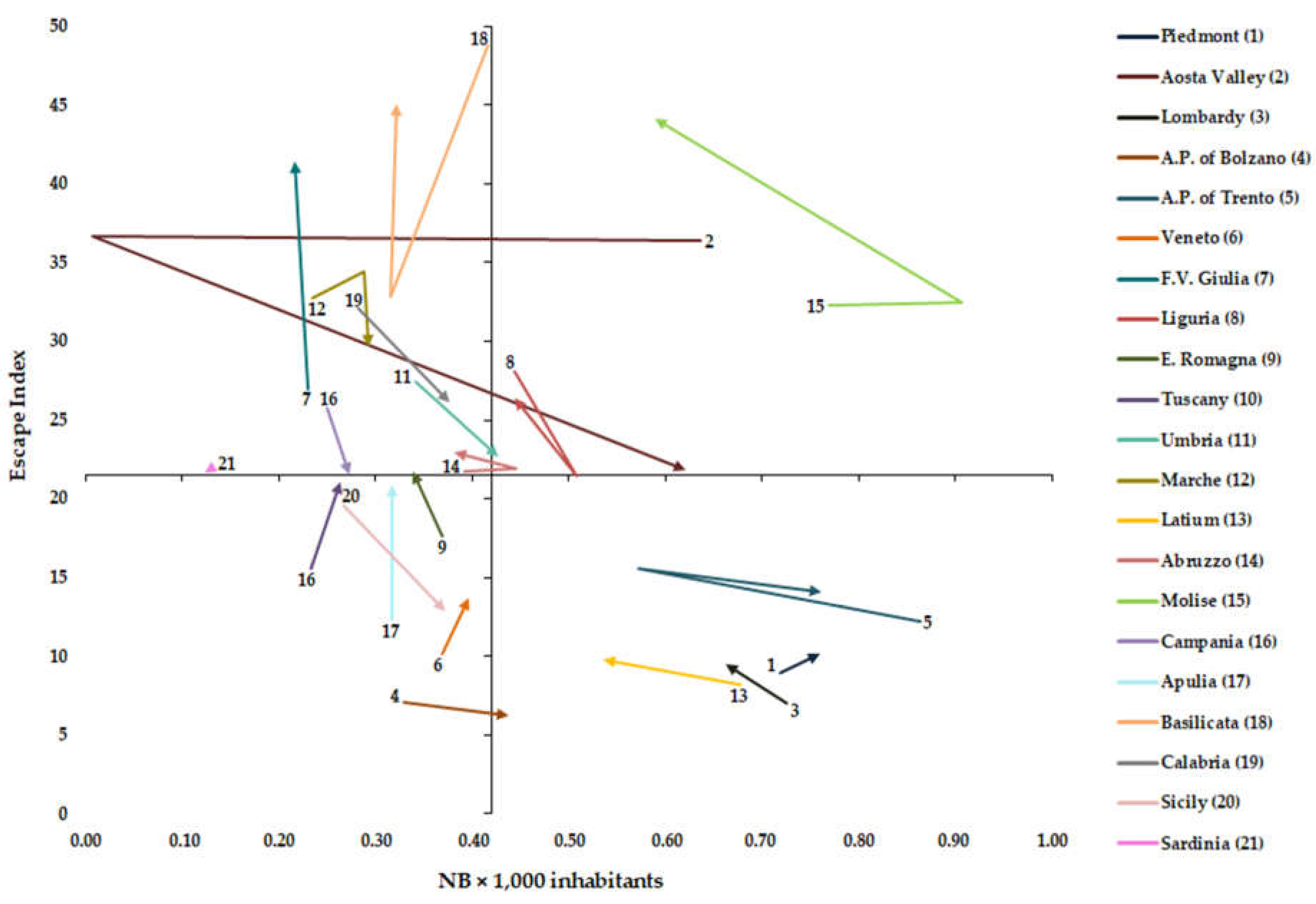
2.3. Attraction and Escape Indexes
2.4. Graphical representation of AI, EI and NB x 1,000 inhabitants:
2.5. Vectorial and statistical analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ricci, A.; Barzan, E.; Longo, F. How to identify the drivers of patient inter-regional mobility in beveridgean systems? Critical review and assessment matrix for policy design & managerial interventions. Health Serv. Manage. Res. 2021, 34, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Lunt, N.; Mannion, R. Patient mobility in the global marketplace. A multidisciplinary perspective. Int. J. Health Policy Manag. 2014, 2, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Horsfall, D. Medical tourism from the UK to Poland: How the market masks migration. J. Ethn. Migr. Stud. 2019, 46, 4211–4229. [Google Scholar] [CrossRef]
- Perna, R.; Cruz-Martínez, G.; Moreno Fuentes, F.J. Patient mobility within national borders. Drivers and politics of cross-border healthcare agreements in the Spanish decentralized system. Health Policy. 2022, 126, 1187–1193. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, Y. Analysis of the charateristics of Cross-Regional Patient Group and Differences in Hospital Service Utilization in Beijin. Int. J. Environ. Res. Public Health 2022, 19, 3227. [Google Scholar] [CrossRef]
- Diesenreiter, C.; Österle, A. Patients as EU citizens? The implementation and corporatist stakeholders’ perceptions of the EU cross-border health care directive in Austria. Health Policy 2021, 125, 1498–1505. [Google Scholar] [CrossRef]
- Pecoraro, F.; Luzi, D.; Clemente, F. The Impact of Hospital Accessibility on Interregional Patient Mobility in Italy. Stud Health Technol Inform. 2022, 25, 684–688. [Google Scholar] [CrossRef]
- Rotulo, A.; Paraskevopoulou, C.; Kondilis, E. The Effects of Health Sector Fiscal Decentralisation on Availability, Accessibility, and Utilisation of Healthcare Services: A Panel Data Analysis. Int J Health Policy Manag. 2021, 11, 2440–50. [Google Scholar] [CrossRef]
- Nante, N.; Guarducci, G.; Lorenzini, C.; Messina, G.; Carle, F.; Carbone, S.; Urbani, A. Inter-Regional Hospital Patients’ Mobility in Italy. Healthcare 2021, 9, 1182. [Google Scholar] [CrossRef]
- Fattore, G.; Petrarca, G.; Torbica, A. Traveling for care: Inter-regional mobility for aortic valve substitution in Italy. Health Policy 2014, 117, 90–97. [Google Scholar] [CrossRef]
- Aggarwal, A.; Lewis, D.; Mason, M.; Sullivan, R.; Van Der Meulen, J. Patient Mobility for Elective Secondary Health Care Services in Response to Patient Choice Policies: A Systematic Review. Med. Care Res. Rev. 2016, 74, 379–403. [Google Scholar] [CrossRef] [PubMed]
- Lega, F.; Sargiacomo, M.; Ianni, L. The rise of governmentality in the Italian National Health System: physiology or pathology of a decentralized and (ongoing) federalist system? Health Serv Manage Res. 2010, 23, 172–80. [Google Scholar] [CrossRef] [PubMed]
- Nante, N.; Messina, G.; Lispi, L.; Serafini, A.; Prisco, G.; Moirano, F. Mobility trends of Patients across Italian Regions: implications for planning and evaluation of hospital services. Ann Ig. 2016, 28, 328–38. [Google Scholar]
- Int J Health Policy Manag. 2015, 4, 363–72. [CrossRef]
- Balia, S.; Brau, R.; Moro, D. Choice of hospital and long-distances: Evidence from Italy. Reg. Sci. Urban Econ. 2020, 81, 103502. [Google Scholar] [CrossRef]
- Levaggi, R.; Zanola, R. Patients’ migration across regions: The case of Italy. Appl. Econ. 2004, 36, 1751–1757. [Google Scholar] [CrossRef]
- Ferré, F.; Seghieri, C.; Nuti, S. Women's choices of hospital for breast cancer surgery in Italy: Quality and equity implications. Health Policy. 2023, 131, 104781. [Google Scholar] [CrossRef]
- Pecoraro, F.; Accordino, F.; Cecconi, F.; Paolucci, M. Agent Based Modelling for Simulating the Interregional Patient Mobility in Italy. Stud Health Technol Inform. 2023, 302, 297–301. [Google Scholar] [CrossRef]
- Rubino, C.; Di Maria, C.; Abbruzzo, A.; Ferrante, M. Socio-economic inequality, interregional mobility and mortality among cancer patients: A mediation analysis approach. Socio-Econ. Plan. Sci. 2022, 82, 101247. [Google Scholar] [CrossRef]
- Beukers, P.D.C.; Kemp, R.G.M.; Varkevisser, M. Patient hospital choice for hip replacement: Empirical evidence from the Netherlands. Eur. J. Health Econ. 2013, 15, 927–936. [Google Scholar] [CrossRef]
- Ruwaard, S.; Douven, R.C.M.H. Hospital Choice for Cataract Treatments: The Winner Takes Most. Int. J. Health Policy Manag. 2018, 7, 1120–1129. [Google Scholar] [CrossRef] [PubMed]
- Nante, N.; Ricchiardi, G.; Al Farraj, O.; Morgagni, S.; Siliquini, R.; Moirana, F.; Messina, G.G.; Sassi, F. Hospital patient migration: Analysis using a utility index. In Public Health in Europe; Kirch, W., Ed.; Springer: Berlin/Heidelberg, Germany, 2004; pp. 293–316. [Google Scholar]
- Sivey, P. The effect of waiting time and distance on hospital choice for English cataract patients. Health Econ. 2012, 21, 444–56. [Google Scholar] [CrossRef]
- Moscelli, G.; Siciliani, L.; Gutacker, N.; Gravelle, H. Location, quality and choice of hospital: Evidence from England 2002-2013. Reg Sci Urban Econ. 2016, 60, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Pinto, C. Percived quality and formation of inter-regional networks of health care migration. Adv. Manag. Appl. Econ. 2017, 7, 93–111. Available online: https://www.scienpress.com/journal_focus.asp?main_id=55&Sub_id=IV&Issue=259775 (Accessed on 27 May 2023).
- Schnatz, P.F.; Murphy, J.L.; O'Sullivan, D.M.; Sorosky, J.I. Patient choice: comparing criteria for selecting an obstetrician-gynecologist based on image, gender, and professional attributes. Am J Obstet Gynecol. 2007, 197, 548.e1–7. [Google Scholar] [CrossRef] [PubMed]
- Howell, E.A.; Gardiner, B.; Concato, J. Do women prefer female obstetricians? Obstet Gynecol. 2002, 99, 1031–5. [Google Scholar] [CrossRef] [PubMed]
- Martini, G.; Levaggi, R.; Spinelli, D. Is there a bias in patient choices for hospital care? Evidence from three Italian regional health systems. Health Policy. 2022, 126, 668–679. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Beds per hospital facility. Available online: https://www.dati.salute.gov.it/dati/dettaglioDataset.jsp?menu=dati&idPag=114 (Accessed on 3 April 2023).
- ISTAT. Health for All—Italia. Update December 2022. Available online: http://www.istat.it/it/archivio/14562. (Accessed on 3 January 2023).
- Guarducci, G.; Messina, G.; Carbone, S.; Urbani, A.; Nante, N. Inter-Regional Patients’ Migration for Hospital Orthopedic Intensive Rehabilitation: The Italian Experience. Int. J. Environ. Res. Public Health 2022, 19, 13726. [Google Scholar] [CrossRef]
- Gandy, R.J. A graphical representation of the inter-relationship between districts. Hosp. Health Serv. Rev. 1979, 75, 50–51. [Google Scholar]
- Gandy, R.; Franci, A.; Gurrieri, C.; McClelland, R. Demonstrating Access to Public Services Diagrammatically. Int. J. Public Adm. 2011, 34, 516–527. [Google Scholar] [CrossRef]
- De Curtis, M.; Bortolan, F.; Diliberto, D.; Villani, L. Pediatric interregional healthcare mobility in Italy. Ital. J. Pediatr. 2021, 47, 1–7. [Google Scholar] [CrossRef]
- Griffiths, I.W. Principles of Biomechanics & Motion Analysis; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Blàsquez-Fernàndez, C.; Cantarero-Prieto, D.; Pascual-Sàez, M. Patient cross-border mobility: New findings and implications in Spanish regions. Econ. Sociol. 2017, 10, 11–21. [Google Scholar] [CrossRef]
- Berta, P.; Guerriero, C.; Levaggi, R. Hospitals’ strategic behaviours and patient mobility: Evidence from Italy. Socio-Econ. Plan. Sci. 2021, 77, 101030. [Google Scholar] [CrossRef]
- Rubino, C.; Di Maria, C.; Abbruzzo, A.; Ferrante, M. Socio-economic inequality, interregional mobility and mortality among cancer patients: A mediation analysis approach. Socio-Econ. Plan. Sci. 2022, 82, 101247. [Google Scholar] [CrossRef]
- Conference of the Regions and Autonomous Provinces. Health Pact 2019-2021. Available online: http://www.regioni.it/newsletter/n-3750/del-07-01-2020/patto-per-la-salute-2019-2021-il-testo-20616/ (Accessed on 10 June 2023).
- Berta, P.; Martini, G.; Spinelli, D.; Vittadini, G. The beaten paths effect on patient inter-regional mobility: An application to the Italian NHS. Papers in Regional Science. 2022, 101, 945–77. [Google Scholar] [CrossRef]
- Calovi, M.; Seghieri, C. Using a GIS to support the spatial reorganization of outpatient care services delivery in Italy. BMC Health Serv Res. 2018, 18, 883. [Google Scholar] [CrossRef]
- Seghieri, C.; Calovi, M.; Ferrè, F. Proximity and waiting times in choice models for outpatient cardiological visits in Italy. PLoS One. 2018, 13, e0203018. [Google Scholar] [CrossRef]
- Roh, C.Y.; Lee, K.H.; Fottler, M.D. Determinants of hospital choice of rural hospital patients: the impact of networks, service scopes, and market competition. J Med Syst. 2008, 32, 343–53. [Google Scholar] [CrossRef]
| Year | Residents | Mobility | Total | Total (ORD+DH) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ORD | DH | ORD/DH | ORD | DH | ORD/DH | ORD | DH | ORD/DH | ||
| 2011 | 263,884 | 47,550 | 5.55 | 44,067 | 5,733 | 7.69 | 307,951 | 53,283 | 5.78 | 361,234 |
| 2012 | 266,029 | 39,783 | 6.69 | 46,069 | 5,328 | 8.65 | 312,098 | 45,111 | 6.92 | 357,209 |
| 2013 | 269,373 | 36,419 | 7.40 | 48,132 | 4,452 | 10.81 | 317,505 | 40,871 | 7.77 | 358,376 |
| 2014 | 265,473 | 31,692 | 8.38 | 48,462 | 3,173 | 15.27 | 313,935 | 34,865 | 9.00 | 348,800 |
| 2015 | 267,010 | 30,812 | 8.67 | 50,466 | 3,236 | 15.60 | 317,476 | 34,048 | 9.32 | 351,524 |
| 2016 | 265,753 | 28,905 | 9.19 | 51,796 | 2,949 | 17.56 | 317,549 | 31,854 | 9.97 | 349,403 |
| 2017 | 263,474 | 27,716 | 9.51 | 51,579 | 3,001 | 17.19 | 315,053 | 30,717 | 10.26 | 345,770 |
| 2018 | 260,856 | 25,477 | 10.24 | 50,596 | 2,974 | 17.01 | 311,452 | 28,451 | 10.95 | 339,903 |
| 2019 | 261,481 | 25,524 | 10.24 | 49,386 | 3,092 | 15.97 | 310,867 | 28,616 | 10.86 | 339,483 |
| Region | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Piedmont | 0,72 | 0,75 | 0,75 | 0,74 | 0,74 | 0,74 | 0,74 | 0,75 | 0,76 | |
| Aosta Valley | 0,64 | 0,01 | 0,51 | 0,61 | 0,59 | 0,59 | 0,59 | 0,62 | 0,62 | |
| Lombardy | 0,73 | 0,67 | 0,65 | 0,65 | 0,66 | 0,67 | 0,66 | 0,66 | 0,66 | |
| A.P. of Bolzano | 0,33 | 0,33 | 0,34 | 0,37 | 0,37 | 0,43 | 0,42 | 0,44 | 0,35 | |
| A.P. of Trento | 0,86 | 0,57 | 0,80 | 0,75 | 0,69 | 0,69 | 0,71 | 0,70 | 0,76 | |
| Veneto | 0,37 | 0,37 | 0,37 | 0,37 | 0,38 | 0,40 | 0,40 | 0,40 | 0,40 | |
| F.V. Giulia | 0,23 | 0,22 | 0,24 | 0,24 | 0,23 | 0,24 | 0,23 | 0,23 | 0,22 | |
| Liguria | 0,44 | 0,41 | 0,48 | 0,51 | 0,43 | 0,46 | 0,45 | 0,45 | 0,44 | |
| E. Romagna | 0,37 | 0,37 | 0,36 | 0,35 | 0,35 | 0,35 | 0,34 | 0,34 | 0,34 | |
| Tuscany | 0,23 | 0,24 | 0,24 | 0,25 | 0,26 | 0,25 | 0,24 | 0,26 | 0,26 | |
| Umbria | 0,34 | 0,35 | 0,39 | 0,39 | 0,39 | 0,40 | 0,42 | 0,43 | 0,43 | |
| Marche | 0,24 | 0,24 | 0,25 | 0,25 | 0,26 | 0,29 | 0,29 | 0,29 | 0,29 | |
| Latium | 0,68 | 0,59 | 0,56 | 0,56 | 0,55 | 0,54 | 0,54 | 0,53 | 0,54 | |
| Abruzzo | 0,39 | 0,39 | 0,39 | 0,38 | 0,38 | 0,45 | 0,38 | 0,39 | 0,38 | |
| Molise | 0,77 | 0,75 | 0,91 | 0,78 | 0,77 | 0,77 | 0,65 | 0,65 | 0,59 | |
| Campania | 0,25 | 0,24 | 0,25 | 0,25 | 0,24 | 0,25 | 0,25 | 0,25 | 0,27 | |
| Apulia | 0,32 | 0,30 | 0,31 | 0,31 | 0,30 | 0,30 | 0,30 | 0,30 | 0,32 | |
| Basilicata | 0,42 | 0,33 | 0,34 | 0,34 | 0,34 | 0,32 | 0,32 | 0,32 | 0,32 | |
| Calabria | 0,28 | 0,26 | 0,32 | 0,41 | 0,37 | 0,36 | 0,40 | 0,41 | 0,38 | |
| Sicily | 0,27 | 0,29 | 0,31 | 0,32 | 0,32 | 0,32 | 0,32 | 0,35 | 0,37 | |
| Sardinia | 0,13 | 0,13 | 0,10 | 0,13 | 0,13 | 0,13 | 0,13 | 0,13 | 0,12 | |
| Italy | 0,49 | 0,48 | 0,48 | 0,49 | 0,46 | 0,49 | 0,49 | 0,49 | 0,50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





