1. Introduction
Vaginal bleeding in the initial stages of pregnancy should not be considered physiological, so it is advisable to carry out an adequate differential diagnosis to rule out any possible obstetric, gynecological or systemic pathology.
We carried out a study on metrorrhagia in the first trimester throughout the year 2015. All visits to the emergency room for this reason were collected and subsequent follow-up of the pregnancy was carried out, as well as a review of the characteristics of each pregnant woman.
Metrorrhagia or first trimester bleeding is defined as bleeding that occurs before 20 weeks of gestation [
1,
2]. Bleeding of genital origin during the initial stages of pregnancy is a frequent complication (20-30%). This bleeding in the context of an early pregnancy causes anxiety to the patient and is one of the most common reasons for consultation in the emergency services [
3]. The main causes of bleeding in the first trimester include voluntary termination of pregnancy, spontaneous abortion, ectopic pregnancy, gestational trophoblastic disease, and various non-obstetric causes such as cervicitis, vaginitis, trauma, cervical cancer, or polyps [
1].
The bleeding that occurs during the first trimester can lead to complications later during pregnancy. The development of any complication can be extremely distressing for the patient and her family. For the gynecologist, it is crucial to be able to identify the symptoms and be aware of the possible short- and long-term consequences of these complications that appear in the first weeks, in order to reassure, advise, and support the couple at a difficult time [
4,
5].
In this study, we reviewed all the patients who visited the emergency department in 2015 due to metrorrhagia during the first weeks of gestation. The aim of the study is to identify possible risk factors and maternal characteristics in order to act before complications develop. Once this data is reviewed and analyzed, we can use it to detect which patients are susceptible to complications and a worse evolution in order to anticipate and thus minimize poor outcomes.
Poor results and obstetric complications rise awareness for improving care and reducing perinatal morbidity and mortality. For this reason, many studies are aimed at identifying risk factors related to unfavorable results. In our study, and as previously stated by many other authors, we were able to describe increase in maternal age as a risk factor for unwanted outcomes [
6,
7,
8,
9,
10].
2. Materials and Methods
It is a descriptive, observational and retrospective study. It is based on the analysis of visits to the emergency department during the year 2015. We have selected the patients for study based on the reason for consultation and the confirmed diagnosis of first trimester bleeding after medical assessment. We collected maternal age in years at the first visit to the emergency room.
We monitored the pregnancy and followed up its evolution.
In order to assess the role of maternal age on the incidence of spontaneous first -trimester miscarriage, we studied those gestations that did not develop further than week 12. We included as first-trimester miscarriage cases of inevitable, missed, and incomplete miscarriage and ectopic pregnancy. Subsequently, we divided all the cases of first trimester miscarriage into age sub-groups to assess the impact of increased maternal age.
3. Results
To carry out the statistical analysis of the data, we reviewed visits to the emergency room in 2015. The total number of visits to the emergency room was 9451, 1161 of which were consultations for first-trimester bleeding. The final size of our sample consisted of 696 patients.
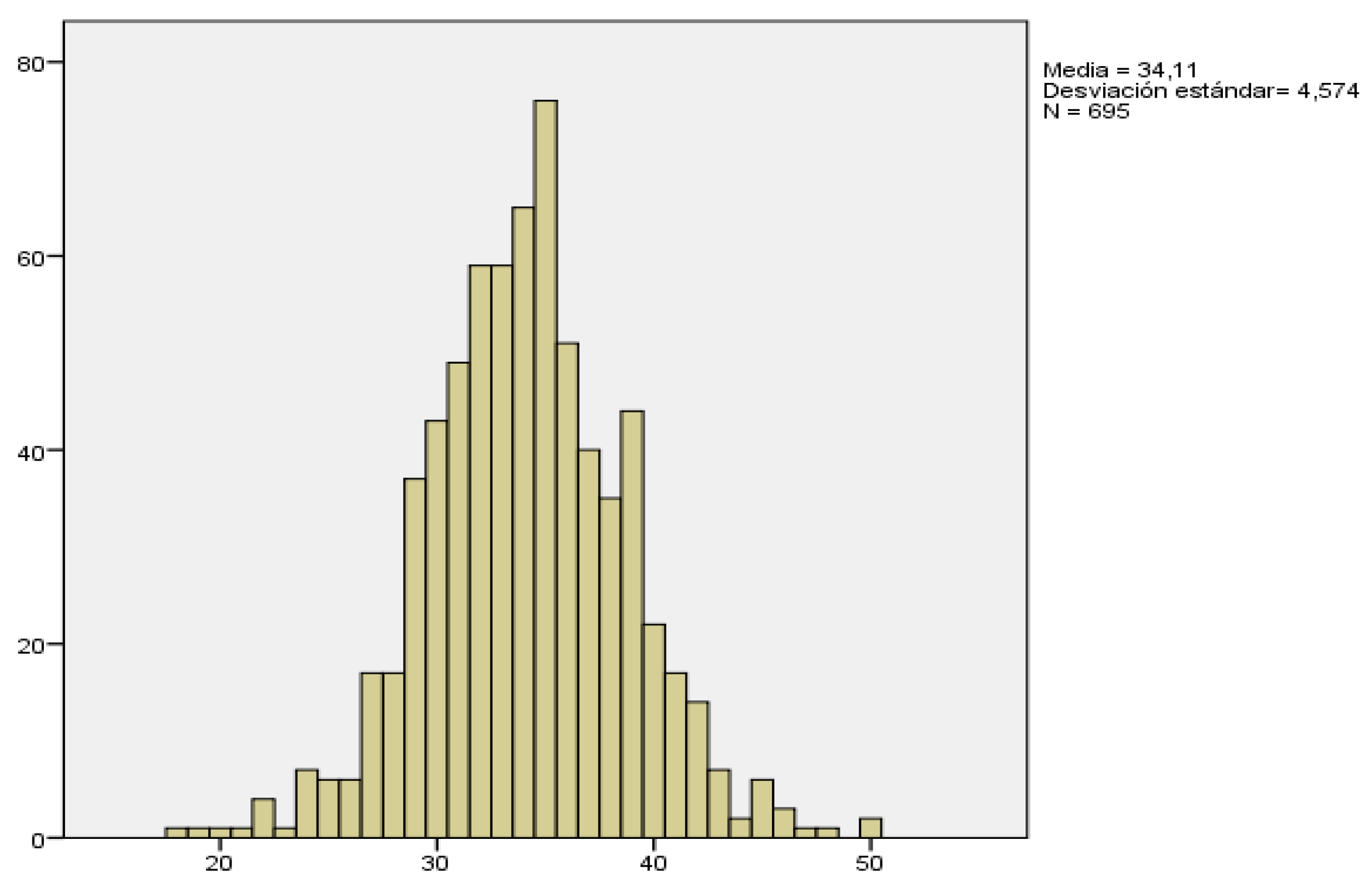
The mean age of pregnant women with metrorrhagia in the first weeks was 34.1 years with a median of 34 years, and an age range between 18 and 50 years.
The following table shows the descriptive parameters of this variable.
Table 1.
Descriptive study of maternal age.
Table 1.
Descriptive study of maternal age.
| |
Maternal Age |
| Population |
696 |
| Mean |
34,11 |
| Median |
34,00 |
| Percentile 25 |
31,00 |
| Percentile 75 |
37,00 |
| Minimal age |
18 |
| Maximal age |
50 |
Figure 1.
Maternal age distribution.
Figure 1.
Maternal age distribution.
In our study, we understand early gestational loss as that which occurs before and including week 12, up to week 12+6.
We evaluated a total of 654 patients, from the 696 women who initially consulted for bleeding in the first trimester. We were unable to follow up 44 of the patients since they did not consult again or continue the monitoring of their pregnancy in our hospital.
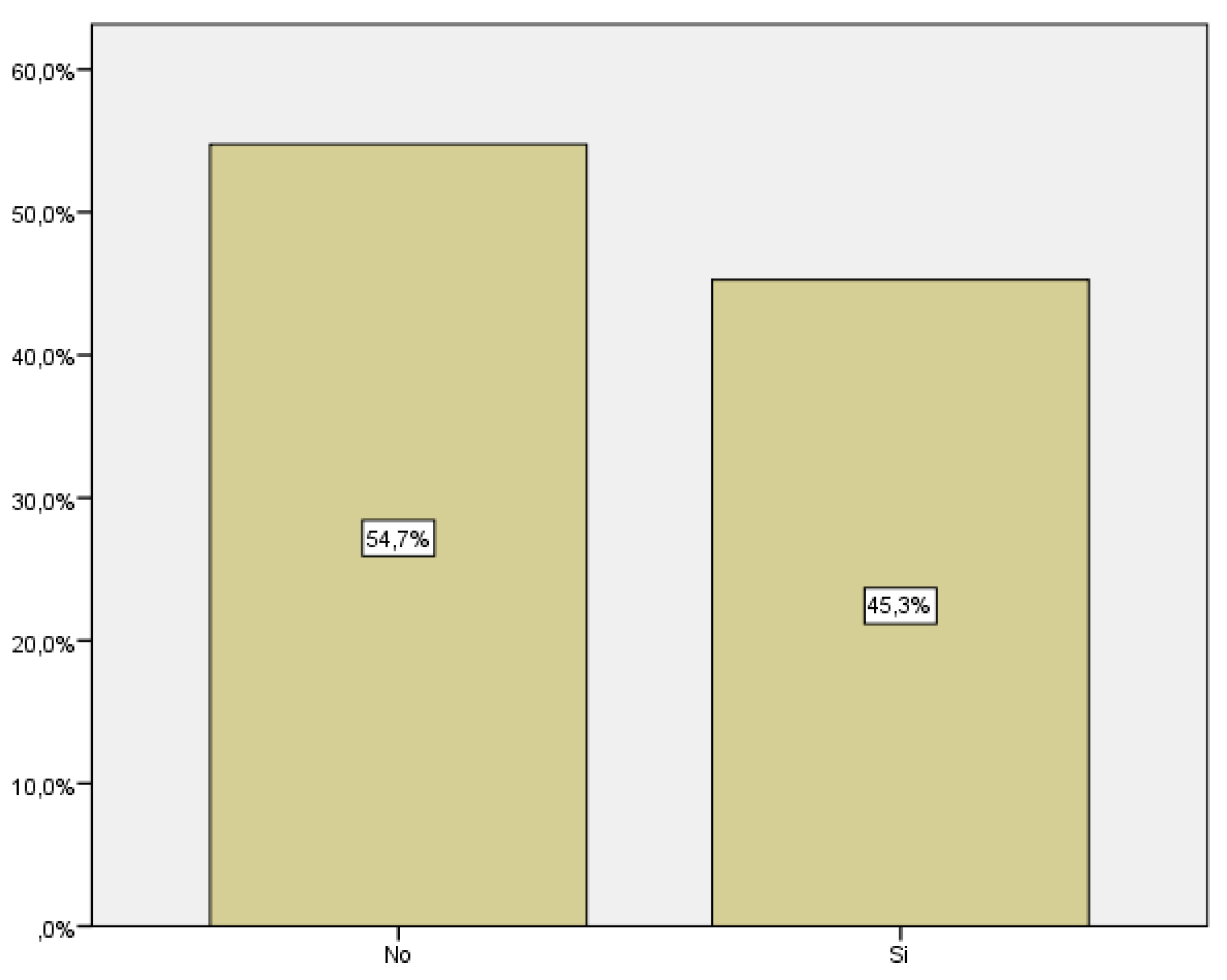
The total number of pregnancies that resulted in miscarriage was 296, which corresponds to 45.3% of the women who consulted for vaginal bleeding, in opposition to 54,7% (358 patients) that did not result in miscarriage.
Figure 2.
Distribution of first trimester miscarriage.
Figure 2.
Distribution of first trimester miscarriage.
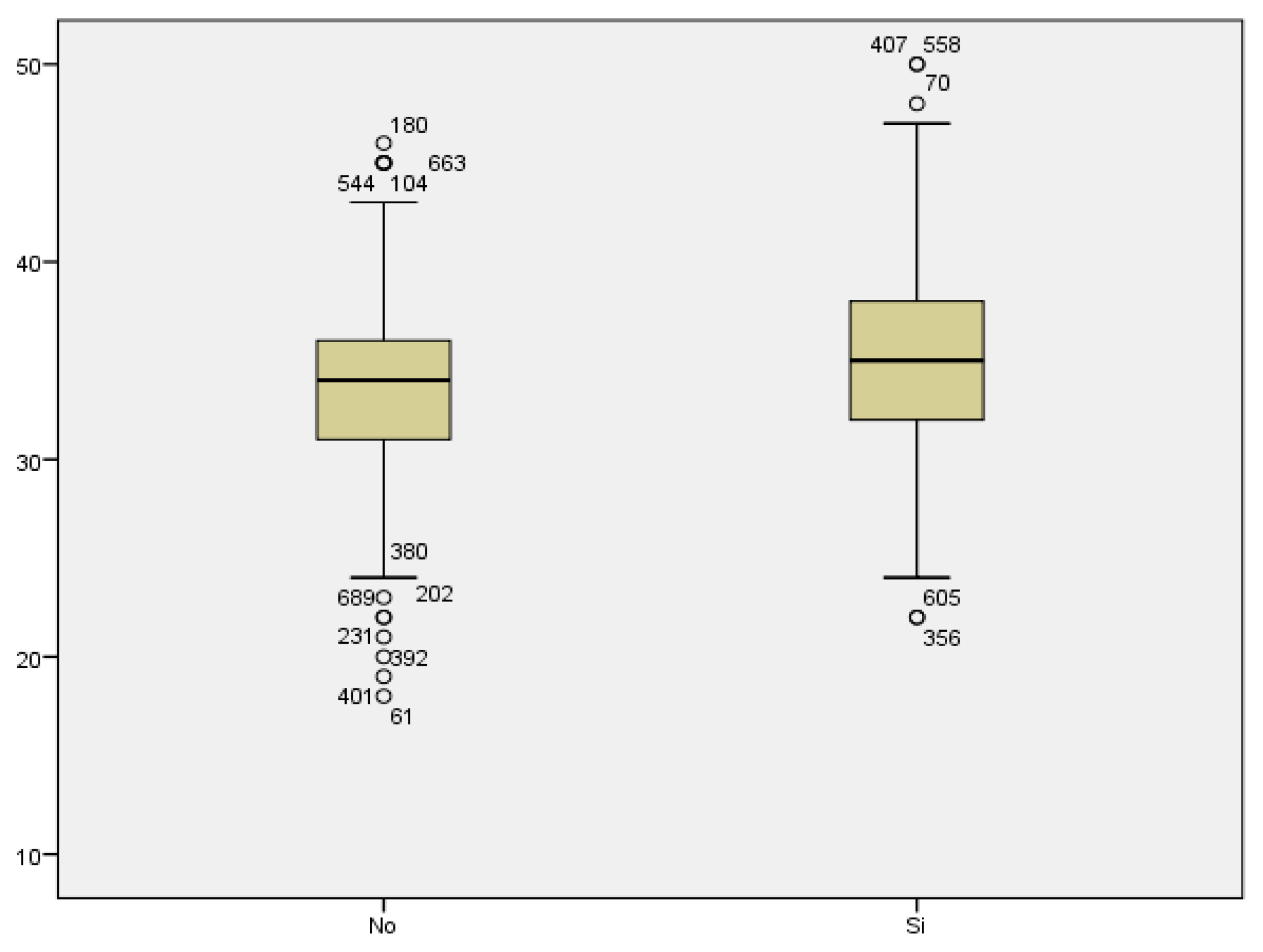
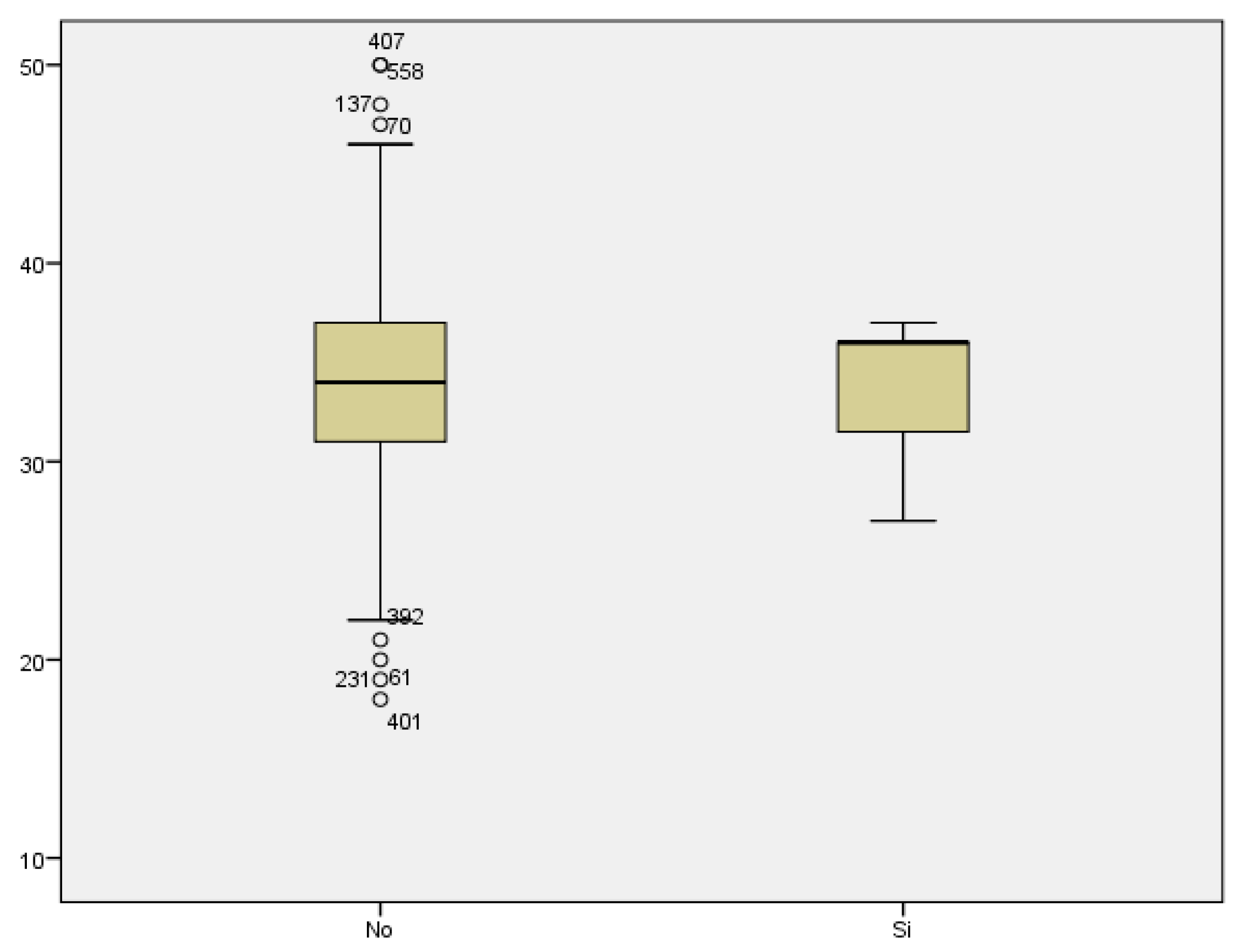
Data was collected to assess the association between maternal age and first trimester miscarriage (up to week 12+6 included). The mean age of women who did not experience a miscarriage was 33.37 years with a SD of ± 4.316, while the mean age of those whose pregnancy resulted in a first-trimester abortion was 35.01 years with a SD of ± 4,740.
Therefore, we can conclude that miscarriage was more frequent among older women, with a statistically significant difference (p< 0.0001).
Figure 3.
Bloxpot distribution of first trimester miscarriages in relation to maternal age.
Figure 3.
Bloxpot distribution of first trimester miscarriages in relation to maternal age.
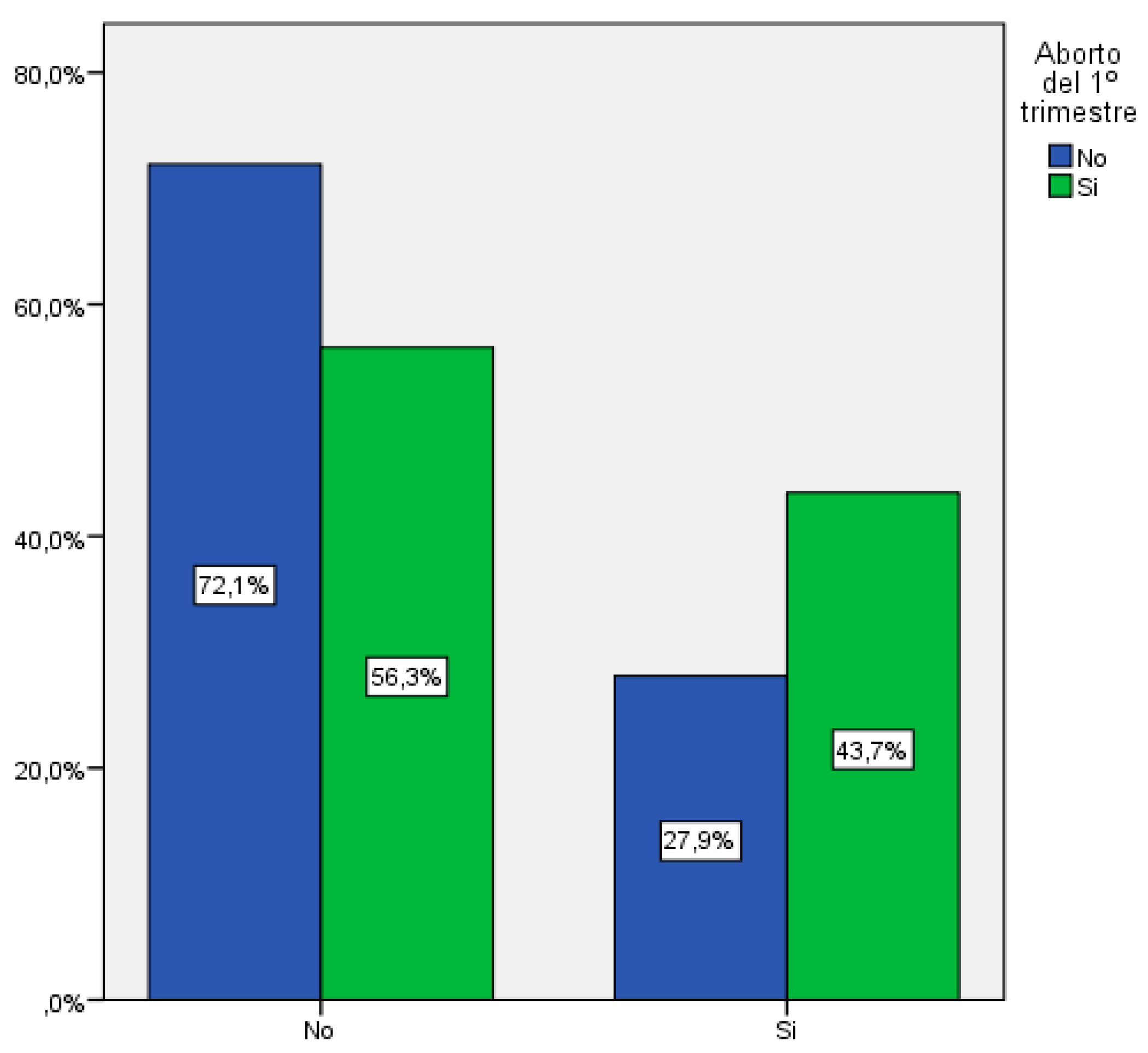
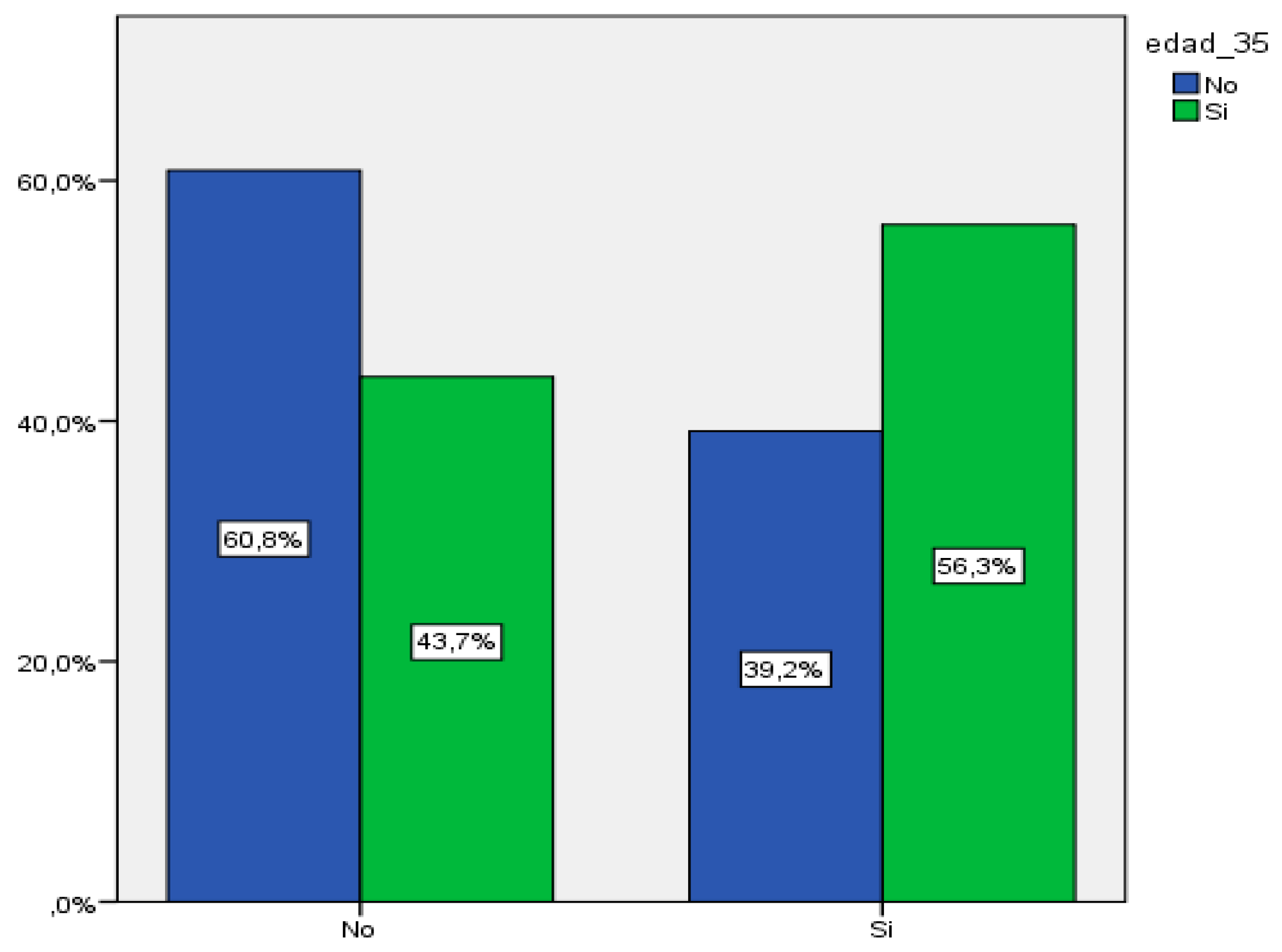
We subdivided the group of patients that experienced a miscarriage into age groups, in order to evaluate whether the prevalence of miscarriage increases with age.
Within the total number of miscarriages, 43.7% of them took place in women over 35 years of age.
Figure 4.
Distribution in those patients older than 35 years who ended in first trimester miscarriage.
Figure 4.
Distribution in those patients older than 35 years who ended in first trimester miscarriage.
If we take a look at the subgroup of women over 35 years of age who consulted for bleeding in the first weeks of pregnancy, we observe that 56.3% of these pregnancies resulted in a miscarriage. Hence, in this subgroup, the number of gestations that resulted in miscarriage was greater than the number of successful pregnancies.
Figure 5.
Distribution of first trimester miscarriages in women over 35 years of age.
Figure 5.
Distribution of first trimester miscarriages in women over 35 years of age.
Table 2.
Relationship between maternal age over 35 years and first trimester miscarriage.
Table 2.
Relationship between maternal age over 35 years and first trimester miscarriage.
| |
1st trimester miscarriage |
Total |
| No |
Yes |
| Age > 35 years |
No |
Count |
258 |
166 |
424 |
| % Age > 35 years |
60,8% |
39,2% |
100,0% |
| % 1st trimester miscarriage |
72,1% |
56,3% |
64,9% |
| Yes |
Count |
100 |
129 |
229 |
| % Age > 35 years |
43,7% |
56,3% |
100,0% |
| % 1st trimester miscarriage |
27,9% |
43,7% |
35,1% |
| Total |
Count |
358 |
295 |
653 |
| % Age > 35 years |
54,8% |
45,2% |
100,0% |
| % 1st trimester miscarriage |
100,0% |
100,0% |
100,0% |
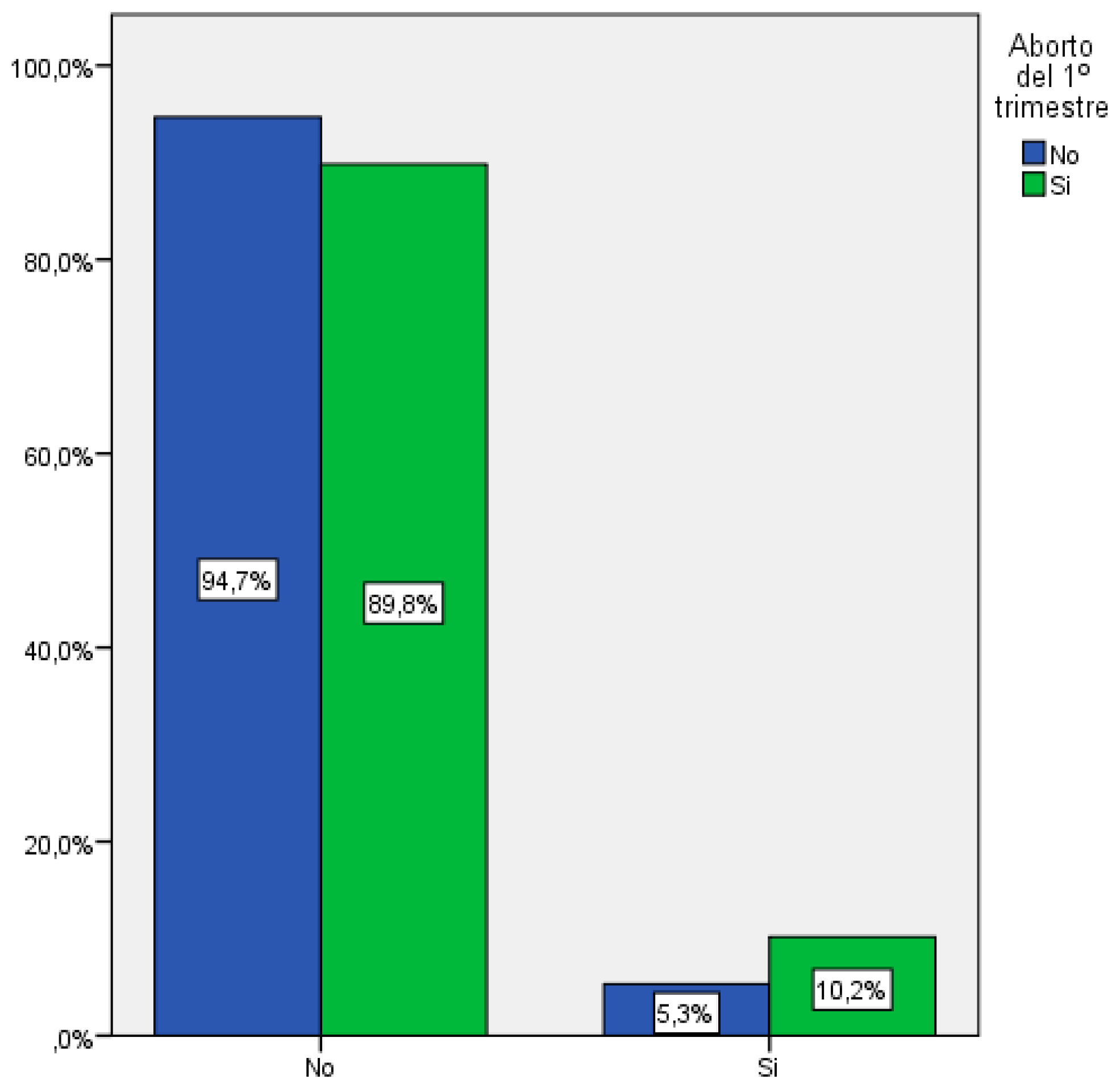
If we increase the age range to 40 years of age, 10.2% of the total number of miscarriages took place within this age group.
Figure 6.
Distribution in those patients older than 40 years who ended in first trimester miscarriage.
Figure 6.
Distribution in those patients older than 40 years who ended in first trimester miscarriage.
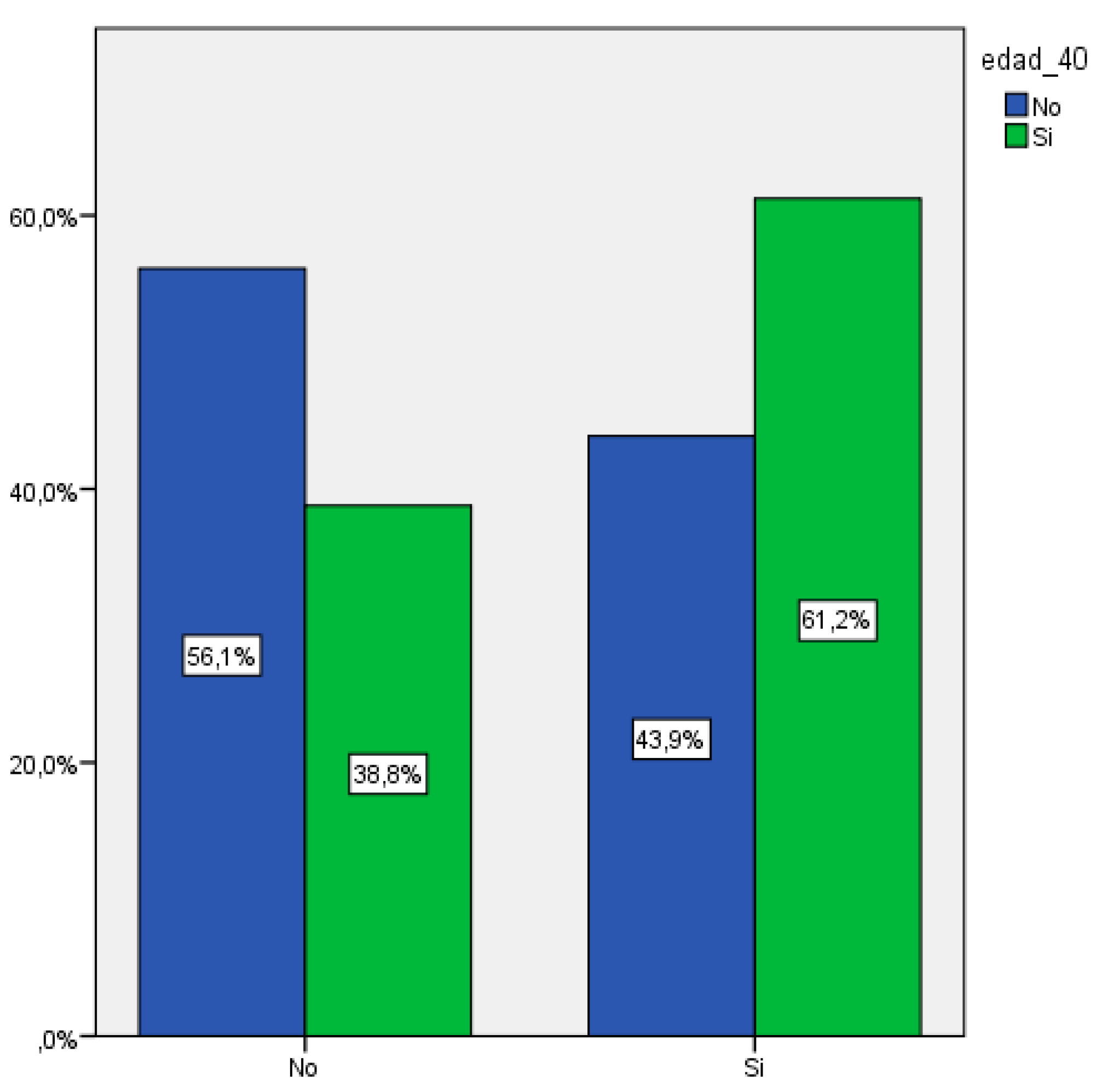
Looking now at the sub-group of women over 40 years of age, we observe that 61.2% of the patients who consulted for bleeding experienced a miscarriage, with a statistically significant difference (p<0.019). Therefore, the percentage of miscarriage increases as maternal age increases, so this case there is also a positive correlation between the increase in spontaneous abortions and the increase in maternal age.
Figure 7.
Distribution of first trimester miscarriages in women over 40 years of age.
Figure 7.
Distribution of first trimester miscarriages in women over 40 years of age.
Table 3.
Relationship between maternal age over 40 years and first trimester miscarriage.
Table 3.
Relationship between maternal age over 40 years and first trimester miscarriage.
| |
1st trimester miscarriage |
Total |
| No |
Yes |
| Age > 40 years |
No |
Count |
339 |
265 |
604 |
| % Age > 40 years |
56,1% |
43,9% |
100,0% |
| % 1st trimester miscarriage |
94,7% |
89,8% |
92,5% |
| Yes |
Count |
19 |
30 |
49 |
| % Age > 40 years |
38,8% |
61,2% |
100,0% |
| % 1st trimester miscarriage |
5,3% |
10,2% |
7,5% |
| Total |
Count |
358 |
295 |
653 |
| % Age > 40 years |
54,8% |
45,2% |
100,0% |
| % 1st trimester miscarriage |
100,0% |
100,0% |
100,0% |
| |
|
|
|
|
Table 4.
Summary of first trimester miscarriage with maternal age over 35 and over 40 years.
Table 4.
Summary of first trimester miscarriage with maternal age over 35 and over 40 years.
| 1st trimester miscarriage |
|---|
| |
|
% |
Signification (p) |
| More than 35 years |
Yes |
56,3 |
0,0001 |
| |
No |
39,2 |
|
| More than 40 years |
Yes |
61,2 |
0,019 |
| |
No |
43,9 |
|
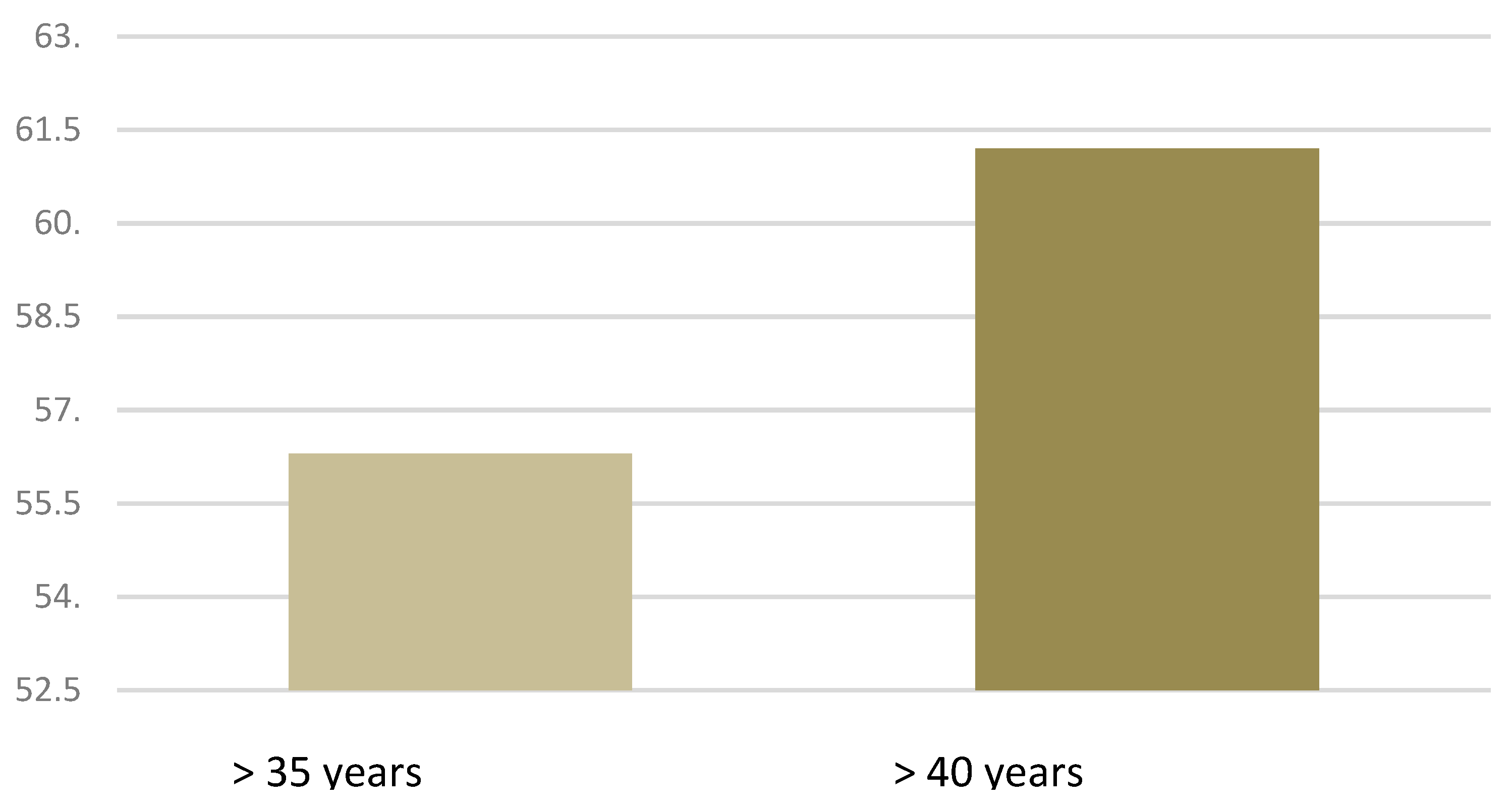
Figure 8.
Distribution of first trimester miscarriages in women over 35 and 40 years of age.
Figure 8.
Distribution of first trimester miscarriages in women over 35 and 40 years of age.
Regarding the cases of late pregnancy loss (above week 12+6), we assessed the average maternal age at which they occurred. We observed that the average age among patients who experienced a late abortion was 33.57 years ± 3.69 SD, compared to an average of 34.12 years ± 4.594 in those who did not. We did not find a statistically significant difference between both groups. In this case, older women did not have a significantly higher number of late abortions.
Figure 9.
Bloxpot distribution of late-term miscarriages according to maternal age.
Figure 9.
Bloxpot distribution of late-term miscarriages according to maternal age.
Table 5.
Relationship of maternal age with miscarriages.
Table 5.
Relationship of maternal age with miscarriages.
| Maternal Age |
|
|
|
|
| |
|
Media |
Typical deviation |
Signification (p) |
| 1st trimester miscarriage |
Yes |
35,01 |
4,740 |
0,0001 |
| |
No |
33,37 |
4,316 |
|
| Late abortion |
Yes |
33,57 |
3,69 |
0,752 |
| |
No |
34,12 |
4,594 |
|
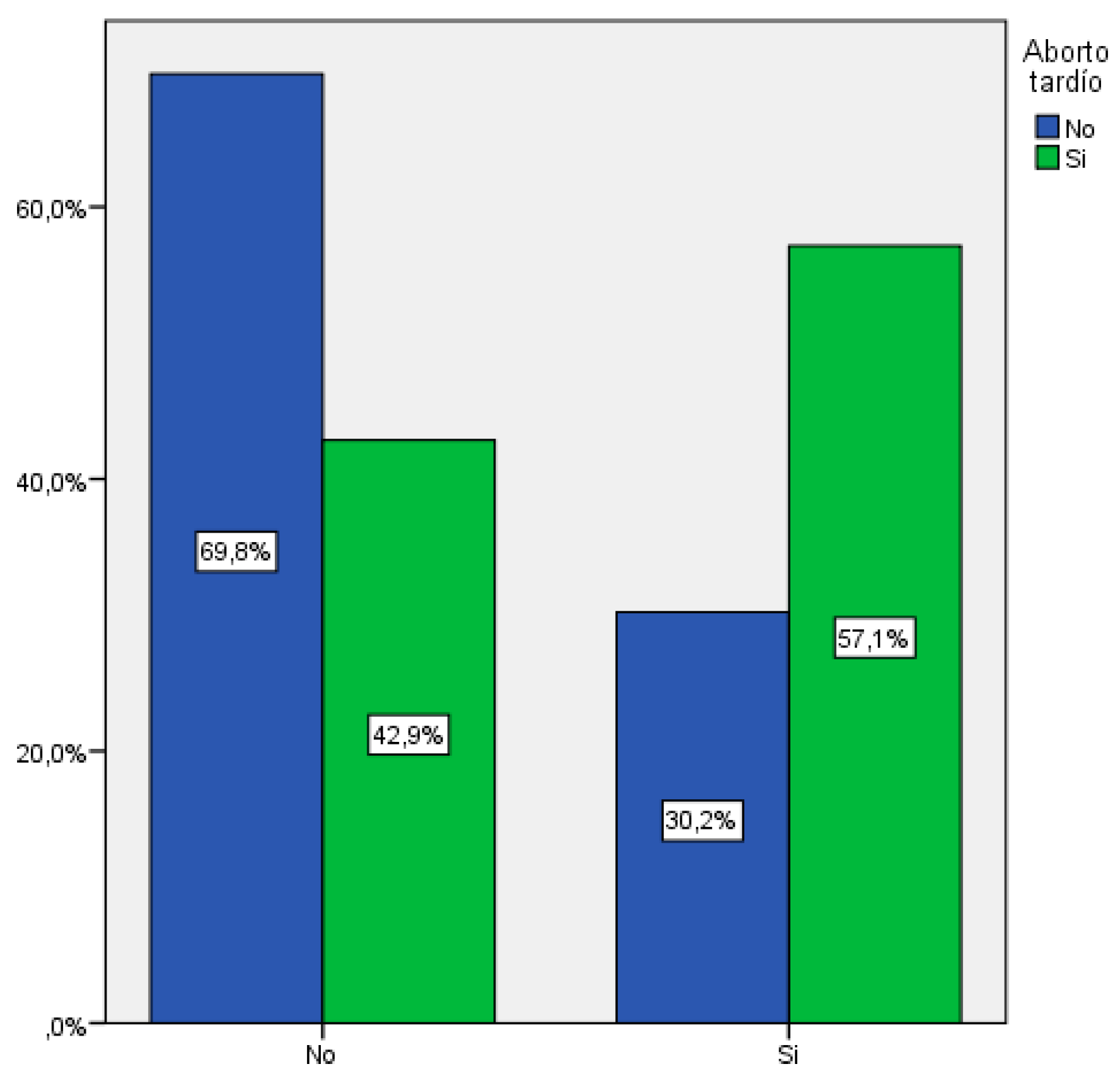
Among the 7 women who had a late-term abortion, 4 of them were older than 35 years, which corresponds to 57.1%. There was no statistically significant difference, with p<0.221.
Figure 10.
Distribution in those patients older than 35 years who ended in late abortion.
Figure 10.
Distribution in those patients older than 35 years who ended in late abortion.
Table 6.
Relationship between maternal age over 35 years and late abortion.
Table 6.
Relationship between maternal age over 35 years and late abortion.
| |
Late abortion |
Total |
| No |
Yes |
| Age > 35 years |
No |
Count |
194 |
3 |
197 |
| % Age > 35 years |
98,5% |
1,5% |
100,0% |
| % late abortion |
69,8% |
42,9% |
69,1% |
| Si |
Count |
84 |
4 |
88 |
| % Age > 35 years |
95,5% |
4,5% |
100,0% |
| % late abortion |
30,2% |
57,1% |
30,9% |
| Total |
Count |
278 |
7 |
285 |
| % Age > 35 years |
97,5% |
2,5% |
100,0% |
| % late abortion |
100,0% |
100,0% |
100,0% |
There is no statistically significant difference between the increase in maternal age and late abortion. If we look at the subgroup of maternal age over 40 years, we find that none of the 7 pregnancies that resulted in late abortion were older than 40.
Table 7.
Number of late abortions according to age range.
Table 7.
Number of late abortions according to age range.
| |
Late abortion |
| Total women |
7 |
| Older than 35 years |
4 |
| Older than 40 years |
0 |
Table 8.
Late abortion with maternal age greater than 35 and greater than 40 years.
Table 8.
Late abortion with maternal age greater than 35 and greater than 40 years.
| Late abortion |
|---|
| |
|
% |
Signification (p) |
| Older than 35 years |
Yes |
57,1 |
0,221 |
| |
No |
42,9 |
|
| Older than 40 years |
Yes |
0 |
0,449 |
| |
No |
100 |
|
4. Discussion
Poor results and obstetric complications rise awareness for improving care and reducing perinatal morbidity and mortality. For this reason, many studies are aimed at identifying risk factors related to unfavorable results.
From all the pregnant women who consulted for metrorrhagia in the first trimester, we observed a rate of miscarriage of 45.3%. If we compare this result with the miscarriage rate among the general obstetric population, regardless of the presence or absence of vaginal bleeding, the percentage of pregnancy loss is approximately 12-15% [
11].
Reviewing publications on first trimester miscarriage and its frequency, we found results that were in line with those obtained in our study. Approximately 50% of pregnancies that present with bleeding during the first weeks result in spontaneous miscarriage. On the other hand, studies that assess the evolution of pregnancies with first-trimester metrorrhagia observe a rate of pregnancy loss before week 28 between 41% and 67%, which include cases of miscarriage, ectopic pregnancies, and molar pregnancies [
12].
We observed that vaginal bleeding played a major role among pregnancies that resulted in a miscarriage. Thus, although bleeding in the early stages of pregnancy does not imply termination of pregnancy, it is strongly associated with poor outcomes.
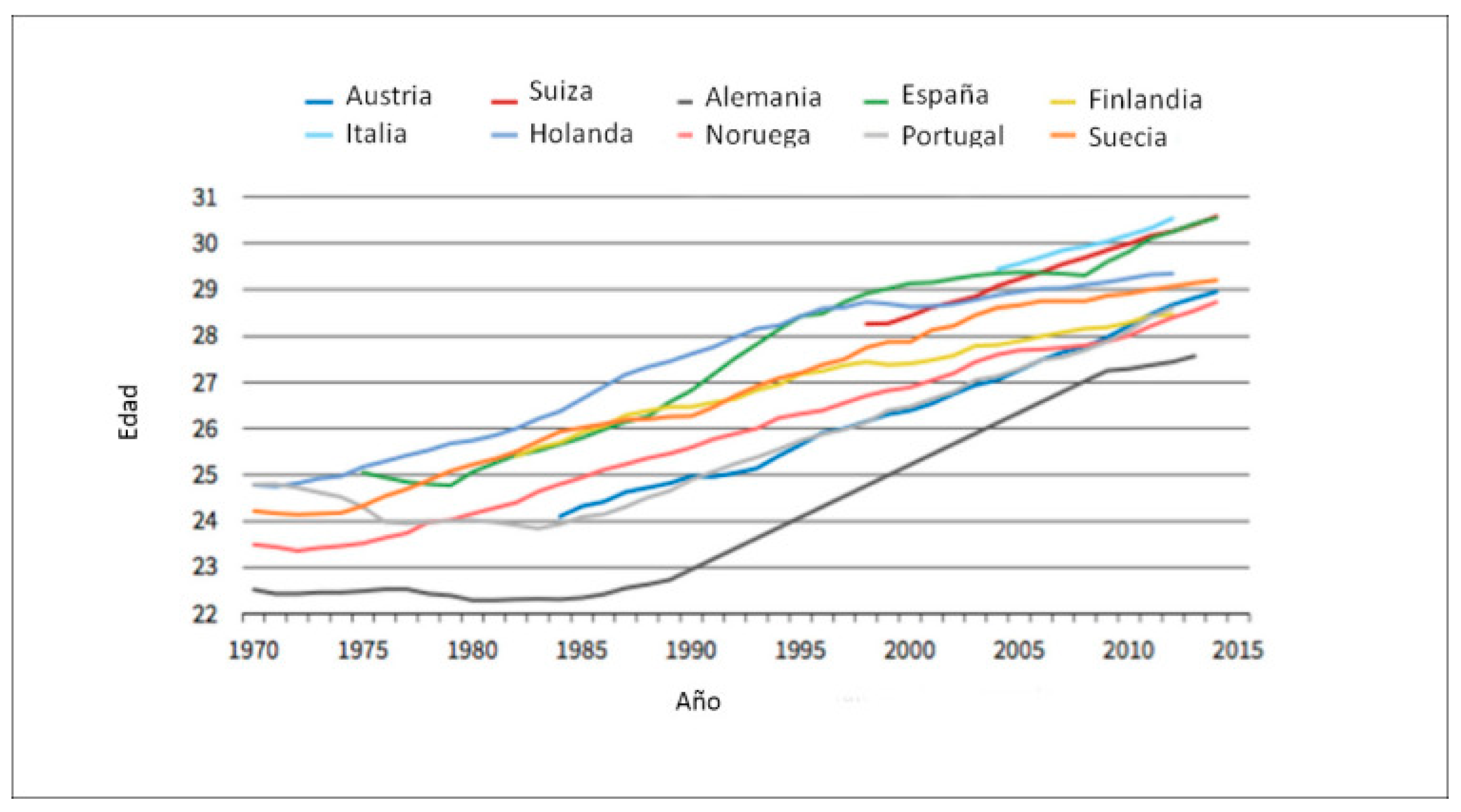
In recent decades we have observed a constant increase in maternal age at the time of first delivery.
We are also seeing a rise in the average maternal age in developed countries. In Spain, in 1978, the average age of pregnant women was 26 years. However, by 2017, the median maternal age had increased to 32 years [
9].
According to data from the European Economic Community, a progressive increase in maternal age is observed among all member countries, but especially in Spain, where the average age is 30.8 years, constituting the highest in all of Europe [
13].
The mean maternal age in our study was 34.1 years.
Figure 11.
Evolution of maternal age in Europe between 1970 and 2015.
Figure 11.
Evolution of maternal age in Europe between 1970 and 2015.
This graph shows the increase in the mean maternal age at the first pregnancy from 1970 to 2015 [
14].
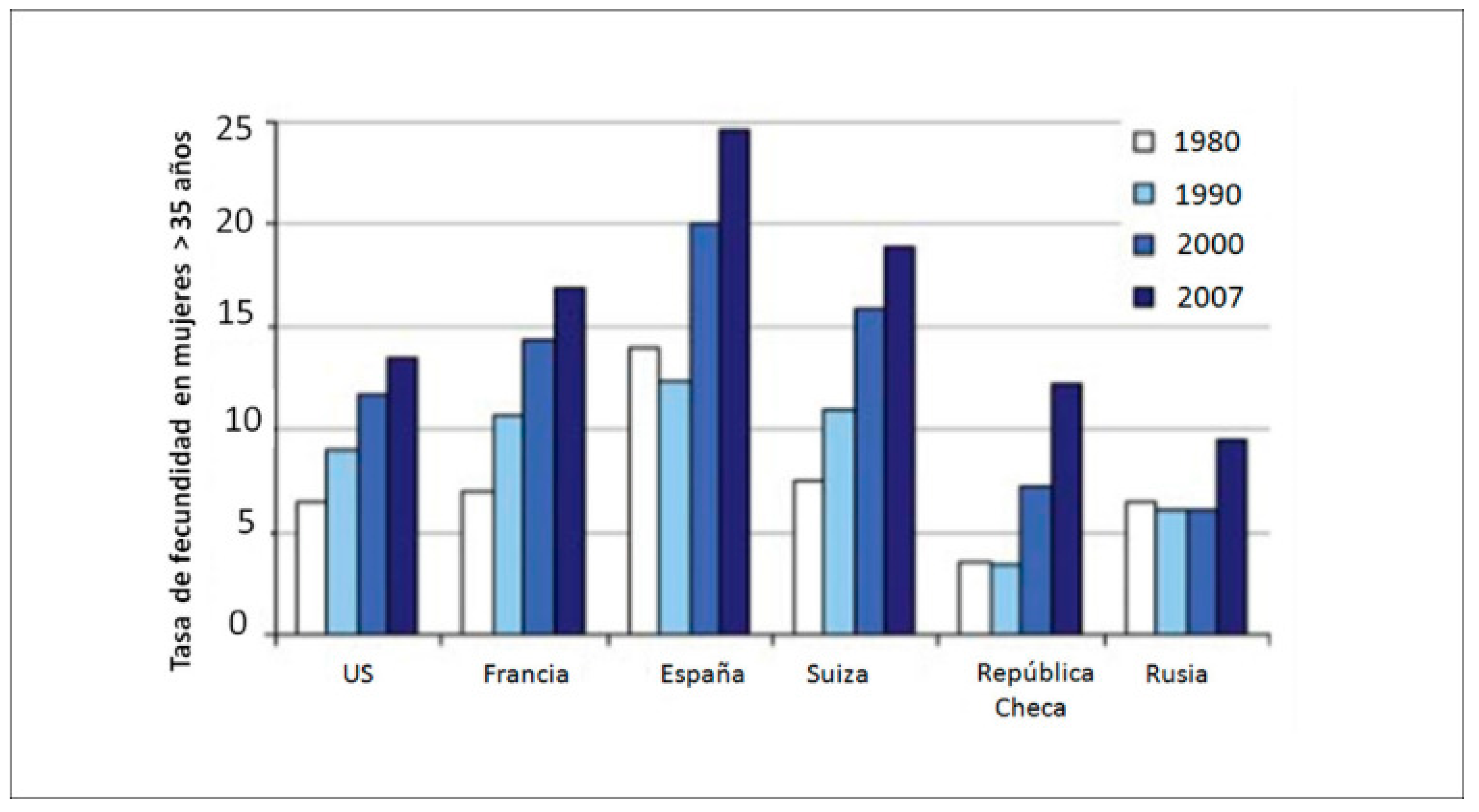
Figure 12.
Fertility rate in women older than 35 years between 1980 and 2007.
Figure 12.
Fertility rate in women older than 35 years between 1980 and 2007.
Nowadays, most part of births occurs in women over 30 years of age in many countries. A recent study shows that Spain occupies the first place in this trend, with 60% of women older than 30 years of age since 2002. Also, it is the only country in Europe where, since 2008, just over 50% of first births occur after that age [
14].
One of the events with which we have found a direct and exponential relationship with the increase in maternal age is the frequency of first trimester miscarriage. When we compared the mean age of women who miscarried with respect to those who did not, we observed that those who experienced an undesired outcome were older. To further extend the study, we established several age subgroups to assess whether this relationship increased as maternal age increased. We found a statistically significant relationship between first trimester miscarriage and maternal age in both groups, women over 35 and 40 years of age.
Reviewing and comparing our results with those previously published by other authors, we found the same conclusion: it has become apparent that there is a the correlation between the increase in maternal age and a poor outcome of the pregnancy.
In a similar study to ours, they studied gestations from week 11 and 14 until completion, and divided women over 35 years of age into two subgroups, one between 35-39 years and another over 40 years. They observed an increase in first trimester miscarriages as maternal age increased. In addition to pregnancy loss, they also described an increased incidence of several other complications of pregnancy such as chromosomal abnormalities, congenital malformations, stillbirth, and birth before 34 weeks of gestation [
15].
Advanced maternal age is an independent risk factor for poor obstetric outcomes. Age over 40 years is related to a considerable increase in risk, so it seems to be a good cut-off point to establish this age as advanced maternal age [
16].
A wide range of adverse gestational outcomes are associated with women of advanced maternal age. These include increased risks of spontaneous miscarriage, chromosomal abnormalities, stillbirth, fetal growth restriction, preterm delivery, preeclampsia, gestational diabetes mellitus, and cesarean section [
17].
A study conducted in a group of women over 40 years of age also shows that this age is an independent risk factor for adverse obstetric outcomes. Among the results obtained, they observed an increase in early pregnancy loss. This study especially highlights the increased risk to pregnant women, with a marked rise in associated pathologies [
18].
A recent study allocated the patients of study into several age subgroups in order to assess the influence of increasing maternal age on the obstetric outcome. The created a first group of women between 30 and 34 years of age, a second group of women between 35 and 39 years of age, and a third group of women over 40 years of age. Then, within each group, patients were further divided into nulliparous and multiparous women. The study concludes that most definitely advanced maternal age is associated with several adverse perinatal outcomes. At the same time, the risk of perinatal complications starts to increase from the age of 35 years but becomes significant in women over 40 years of age. [
19].
Other authors found the same results regarding increased maternal age, describing miscarriage rates of 39-51% between the ages of 40 and 42, and between 67 and 75% in women over the age of 43[
20].
Pregnancies in women over 40 years of age should be considered high-risk pregnancies and be carefully monitored with individualized care protocols [
18].
5. Strengths and limitations
Our study had several strengths. First, we collected the total number of patients who visited the emergency service in a whole a year and reviewed the reasons for consultation of each of them. Vaginal bleeding that occurs until week 12+6 has been established as first quarter metrorrhagia, which allows us to establish clear criteria for inclusion and exclusion.
Second, we have a good sample size with a total number of 696 pregnant women. Third, we performed an extensive analysis of each pregnant woman, reviewing her previous medical and obstetric-gynecological history (such as previous miscarriages or surgical interventions performed on the uterus), information on the monitoring of the current gestation (parameters of first trimester screening and analytical values, measurement of cervical length, obstetric complications) and delivery and newborn data (weeks of gestation, birth route, newborn weight, Apgar test value, etc.).
However, this study also has some limitations. As a first limitation, this is a retrospective study, therefore the data we used was limited to the information included in the digitized clinical history. Secondly, our study is solely based on visits to the emergency department of Hospital QuironSalud Málaga, and therefore the follow-up of the gestation and the subsequent analysis of obstetric history was performed on this same center. In consequence, data regarding patients who continued pregnancy follow-up in other centers was missing. We were able to retrieve some of the data that was lost by external monitoring from the collection of medical histories from the Andalusian Health System.
Another limitation we encountered was the absence of a control group with which to compare the results and assess the rate of complications among women who did not present with vaginal bleeding during the first trimester. Due to the high prevalence of first-trimester bleeding and its potential implications for the pregnancy, it would be interesting to further continue the study and perform it prospectively, allowing for the identification and monitoring of potential risk factors that could lead to poor gestational outcomes.
6. Conclusions
According to the results obtained in our study as well as the data previously published by different study groups, we know that increased maternal age is related to higher risk of first trimester miscarriages in pregnancies in which metrorrhagia occurs during the first trimester.
Pregnancies in older women, especially if we establish 40 years of age as the cut-off point, should be considered high-risk pregnancies and have individualized care and follow-up based on the characteristics and needs of each pregnant woman.
Author Contributions
Conceptualization, L.B.C, D.A.D. and E.G.M.; methodology, L.B.C, D.A.D and E.G.M.; software, L.B.C.; validation, D.A.D and E.G.M.; formal analysis, L.B.C.; investigation, L.B.C and D.A.D; data curation, L.B.C.; writing—original draft preparation, L.B.C; writing—review and editing, L.B.C, D.A.D, E.G.M and L.C.F; visualization, L.B.C, D.A.D. and E.G.M.; supervision, D.A.D and E.G.M.; translation, L.C.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We would like to thank all of the authors included in this original paper. This research contributes to the doctoral work of L.B.C. We would like to thank all the participants in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Martonffy, A.I.; Rindfleisch, K.; Lozeau, A.M.; Potter, B. First trimester complications. Prim. Care Clin. Off. Pract. 2012, 39, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Matamoros, C.M.; Rodríguez, O.M. Una actualización en aborto recurrente. Rev. Médica De Costa Rica Y Centroamérica 2011, 68, 423–433. [Google Scholar]
- Román, S.M. Hemorragias del primer trimestre del embarazo. Jano Med. Y Humanidades 2006, 48. [Google Scholar]
- Lamb, E.H. The impact of previous perinatal loss on subsequent pregnancy and parenting. J. Perinat. Educ. 2002, 11, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Griebel, C.P.; Halvorsen, J.; Golemon, T.B.; A Day, A. Management of spontaneous abortion. Am. Fam. Physician 2005, 72, 1243–1250. [Google Scholar] [PubMed]
- Benli, A.R.; Benli, N.C.; Usta, A.T.; Atakul, T.; Koroglu, M. Effect of Maternal Age on Pregnancy Outcome and Cesarean Delivery Rate. J. Clin. Med. Res. 2015, 7, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Xu, W.; Liu, Y.; Zhang, B.; Zhang, Y.; Yu, T.; Huang, T.; Zou, Y. Trends in maternal age and the relationship between advanced age and adverse pregnancy outcomes: a population-based register study in Wuhan, China, 2010–2017. Public Health 2022, 206, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Elçi, G.; Çakmak, A.; Elçi, E.; Sayan, S. The effect of advanced maternal age on perinatal outcomes in nulliparous pregnancies. JPME 2022, 50, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Montori, M.G.; Martínez, A.; Álvarez, C.L.; Cuchí, N.A.; Alcalá, P.M.; Ruiz-Martínez, S. Advanced maternal age and adverse pregnancy outcomes: A cohort study. Taiwan. J. Obstet. Gynecol. 2021, 60, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Saccone, G.; Gragnano, E.; Ilardi, B.; Marrone, V.; Strina, I.; Venturella, R.; Berghella, V.; Zullo, F. Maternal and perinatal complications according to maternal age: A systematic review and meta-analysis. Int. J. Gynecol. Obstet. 2022, 159, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Blohm, F.; Fridén, B.; Milsom, I. A prospective longitudinal population-based study of clinical miscarriage in an urban Swedish population. BJOG: Int. J. Obstet. Gynaecol. 2008, 115, 176–183. [Google Scholar] [CrossRef] [PubMed]
- De Poncheville, L.; Marret, H.; Perrotin, F.; Lansac, J.; Lansac, G.; Ouedraogo, C. Conducta ante las metrorragias del primer trimestre del embarazo. EMC-Ginecol.-Obstet. 2004, 40, 1–15. [Google Scholar] [CrossRef]
- Pérez, B.H.; Tejedor, J.G.; Cepeda, P.M.; Gómez, A.A. La edad materna como factor de riesgo obstétrico. Resultados perinatales en gestantes de edad avanzada. 2011, 54, 575–580. [Google Scholar] [CrossRef]
- Fuentes, A.; Sequeira, K.; Tapia-Pizarro, A. Efectos demográficos, clínicos y biológicos de la postergación de la maternidad. Revista Médica Clínica Las Condes 2021, 32, 146–160. [Google Scholar] [CrossRef]
- Frederiksen, L.E.M.; Ernst, A.; Brix, N.; Lauridsen, L.L.B.B.; Roos, L.; Ramlau-Hansen, C.H.M.; Ekelund, C.K. Risk of Adverse Pregnancy Outcomes at Advanced Maternal Age. Obstet. Gynecol. 2018, 131, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Nieto, M.C.; Barrabes, E.M.; Martínez, S.G.; Prat, M.G.; Zantop, B.S. Impact of aging on obstetric outcomes: defining advanced maternal age in Barcelona. BMC Pregnancy Childbirth 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Frick, A.P. Advanced maternal age and adverse pregnancy outcomes. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 70, 92–100. [Google Scholar] [CrossRef]
- Marozio, L.; Picardo, E.; Filippini, C.; Mainolfi, E.; Berchialla, P.; Cavallo, F.; Tancredi, A.; Benedetto, C. Maternal age over 40 years and pregnancy outcome: a hospital-based survey. J. Matern. Neonatal Med. 2019, 32, 1602–1608. [Google Scholar] [CrossRef]
- Radoń-Pokracka, M.; Adrianowicz, B.; Płonka, M.; Danił, P.; Nowak, M.; Huras, H. Evaluation of Pregnancy Outcomes at Advanced Maternal Age. Open Access Maced. J. Med Sci. 2019, 7, 1951–1956. [Google Scholar] [CrossRef] [PubMed]
- Serour, G.; Mansour, R.; Serour, A.; Aboulghar, M.; Amin, Y.; Kamal, O.; Al-Inany, H.; Aboulghar, M. Analysis of 2,386 consecutive cycles of in vitro fertilization or intracytoplasmic sperm injection using autologous oocytes in women aged 40 years and above. Fertil. Steril. 2010, 94, 1707–1712. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).