Submitted:
30 June 2023
Posted:
03 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
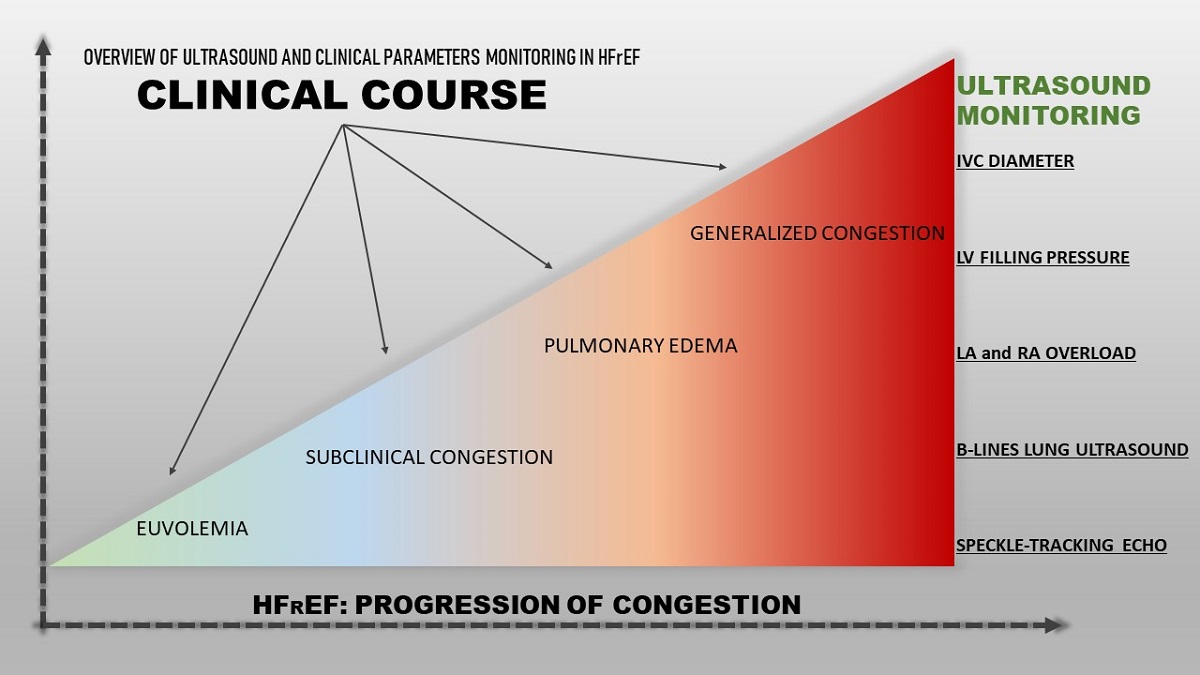
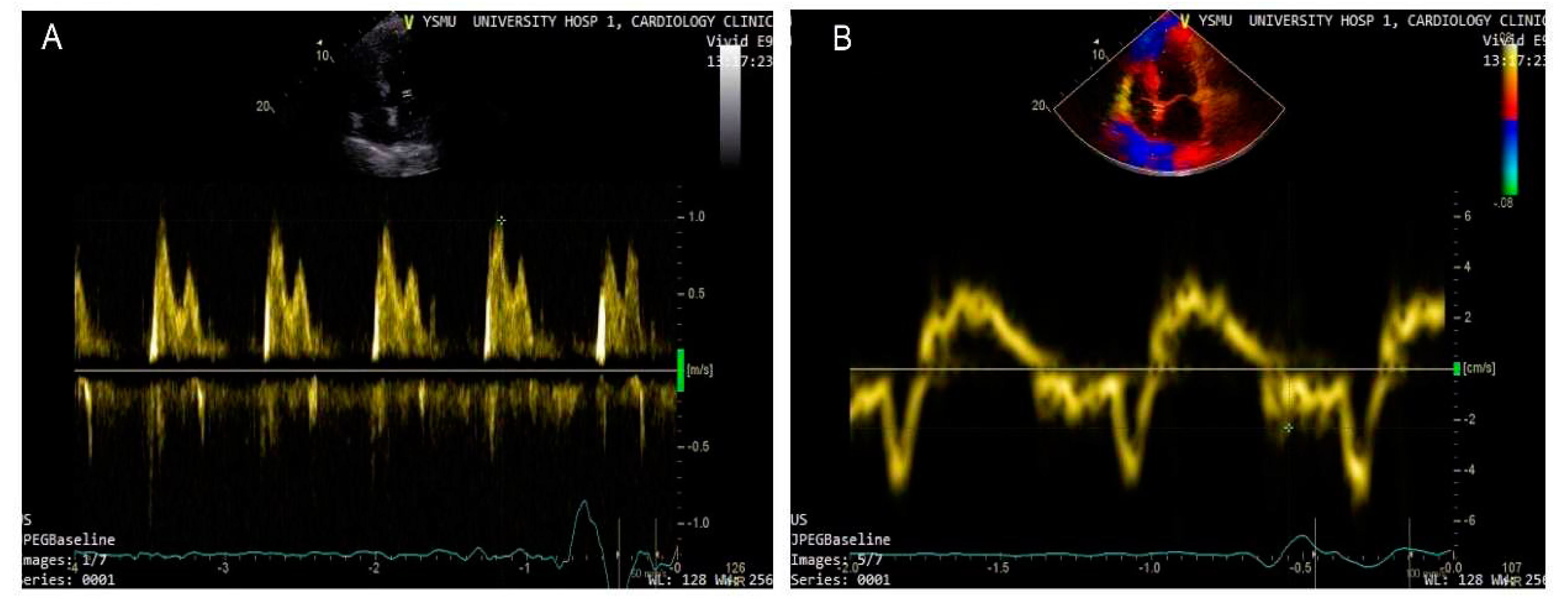
2. Left ventricular decompensation: natriuretic peptides and basic echocardiography
3. Speckle tracking
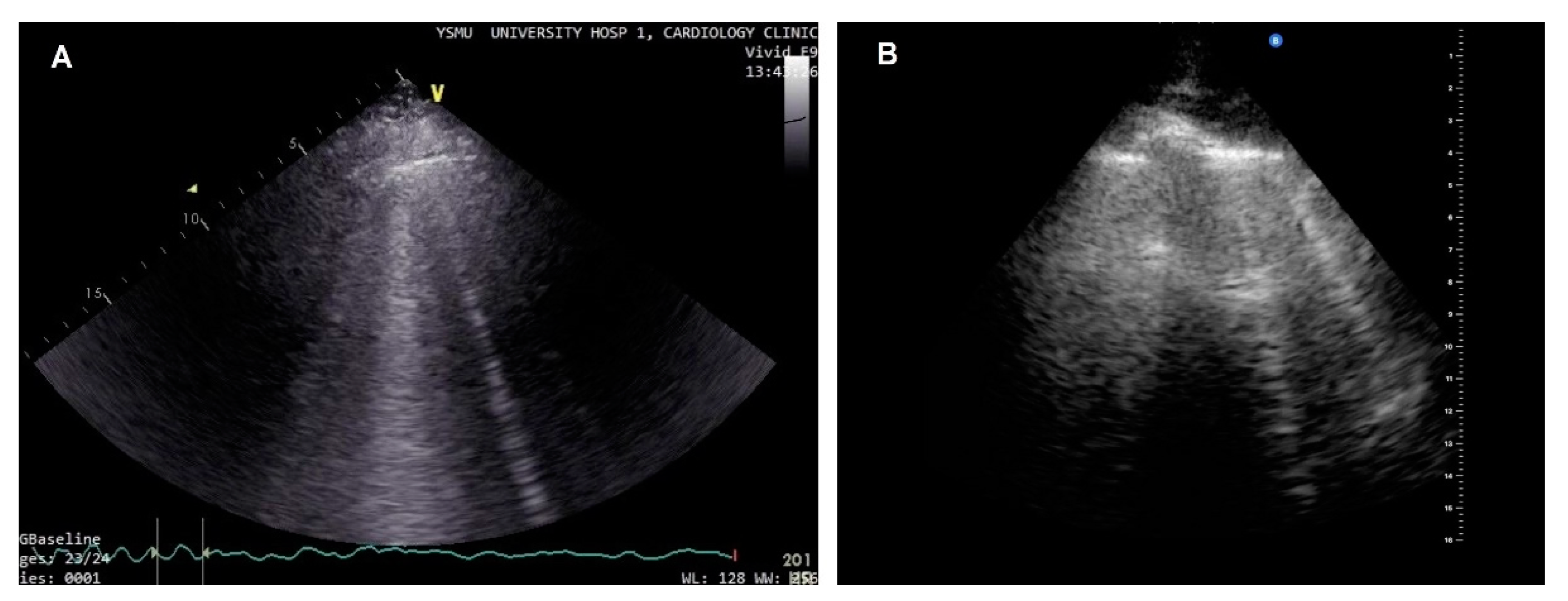
4. Lung ultrasound
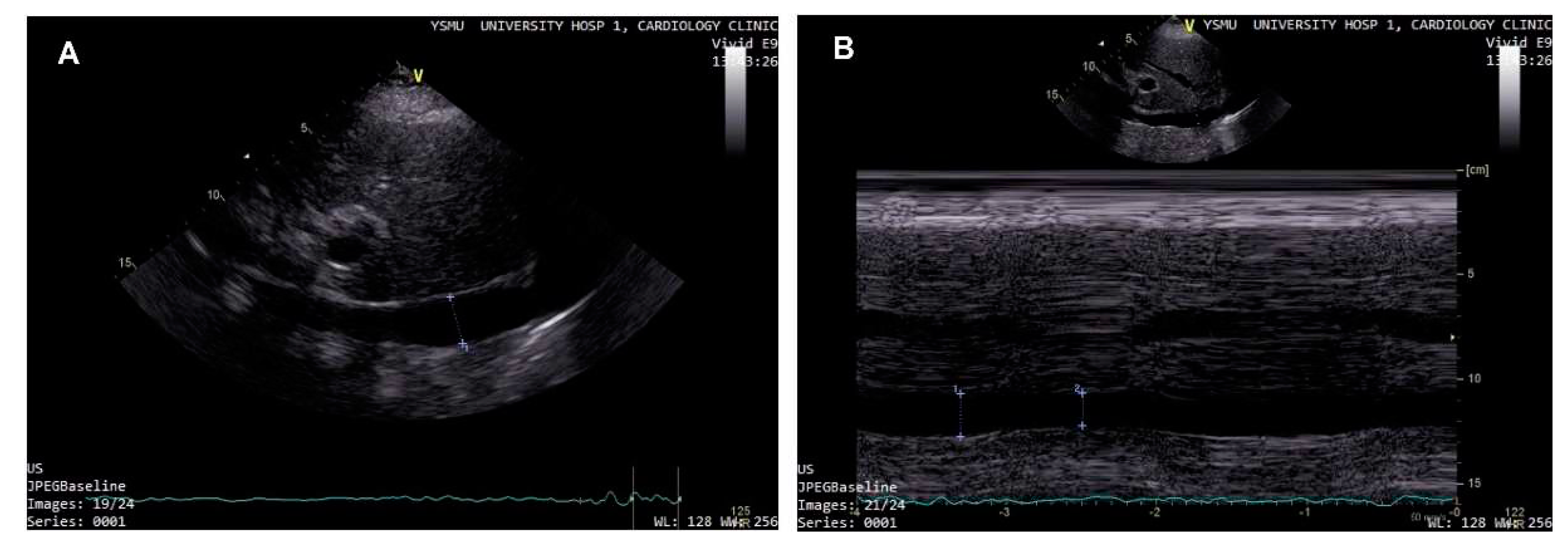
5. Right ventricular HF decompensation
6. Conclusions
- Several important echocardiographic parameters beyond EF can be routinely used as part of an algorithm for prediction of decompensations in chronic HF patients.
- Integration of multiple parameters, which can be easily determined by lung ultrasound and cardiovascular ultrasound, including LV filling pressure, central venous pressure, left and right atrial remodelling, enables to move beyond considering only LV systolic function.
- Complex cardiovascular ultrasound assessment allows to obtain more precise parameters of HF deterioration and enables to identify patients, who require a personalized treatment approach.
Funding
Data Availability Statement
Conflicts of Interest
References
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; et al. American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA Guideline for the Management of Heart Failure. J Am Coll Cardiol. 2013, 62, 147–239. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology ( ESC ) Developed with the special contribution. Eur Heart J 2016, 128, 1–85. [Google Scholar]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; et al. American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation. 2016, 26, 38–360. [Google Scholar]
- Maggioni, A.P.; Dahlström, U.; Filippatos, G.; et al. Heart Failure Association of ESC (HFA). EURObservational research programme: The heart failure Pilot survey (ESC-HF Pilot). Eur J Heart Fail. 2010, 12, 1076–1084. [Google Scholar] [CrossRef]
- Orso, F.; Fabbri, G.; Maggioni A Pietro. Epidemiology of Heart Failure. Handb Exp Pharmacol 2017, 243, 15–33. [Google Scholar]
- Savarese, G.; Musella, F.; Amore, C.D.; et al. Changes of Natriuretic Peptides Predict Hospital Admissions in Patients With Chronic Heart Failure. JACC Hear Fail. 2014, 2, 148–58. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.; Metra, M.; Adamo, M.; et al. ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Murphy, N.; Shanks, M.; Alderman, P. Management of Heart Failure With Outpatient Technology. J Nurse Pract. 2019, 15, 12–8. [Google Scholar] [CrossRef]
- Damy, T.; Kallvikbacka-Bennett, A.; Zhang, J.; et al. Does the physical examination still have a role in patients with suspected heart failure? Eur J Heart Fail. 2011, 13, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Čerlinskaitė, K.; Mebazaa, A.; Cinotti R, et al. Readmission following both cardiac and non-cardiac acute dyspnoea is associated with a striking risk of death. ESC Heart Fail. 2021, 8, 2473–2484. [Google Scholar] [CrossRef] [PubMed]
- Lindmark, K.; Boman, K.; Stålhammar, J.; et al. Recurrent heart failure hospitalizations increase the risk of cardiovascular and all-cause mortality in patients with heart failure in Sweden: a real-world study. ESC Heart Fail. 2021, 8, 2144–2153. [Google Scholar] [CrossRef] [PubMed]
- Mangi, M.A.; Rehman, H.; Rafique, M.; Illovsky, M. Ambulatory Heart Failure Monitoring : A Systemic Review Common methods for HF monitoring. Cureus. 2017, 9, 1174. [Google Scholar]
- Tribouilloy, C.; Rusinaru, D.; Mahjoub, H.; Goissen, T.; Lévy, F.; Peltier, M. Impact of echocardiography in patients hospitalized for heart failure: a prospective observational study. Arch Cardiovasc Dis. 2008, 101, 465–73. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Follath, F.; Ponikowski, P. , et al, European Society of Cardiology; European Society of Intensive Care Medicine. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail. 2010, 12, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Adamson, P.B. Pathophysiology of the transition from chronic compensated and acute decompensated heart failure: New insights from continuous monitoring devices. Curr Heart Fail Rep. 2009, 6, 287–292. [Google Scholar] [CrossRef]
- Lampert, B.C.; Emani, S. Remote hemodynamic monitoring for ambulatory left ventricular assist device patients. J Thorac Dis. 2015, 7, 2165–2171. [Google Scholar] [CrossRef] [PubMed]
- Dokainish, H.; Nguyen, J.S.; Bobek, J.; Goswami, R.; Lakkis, N.M. Assessment of the American Society of Echocardiography-European Association of Echocardiography guidelines for diastolic function in patients with depressed ejection fraction: an echocardiographic and invasive haemodynamic study. Eur J Echocardiogr. 2011, 12, 857–64. [Google Scholar] [CrossRef]
- Zile, M.R.; Claggett, B.L.; Prescott, M.F.; et al. Prognostic Implications of Changes in N-Terminal Pro-B-Type Natriuretic Peptide in Patients With Heart Failure. J Am Coll Cardiol. 2016, 68, 2425–2436. [Google Scholar] [CrossRef]
- O’Connor, C.; Fiuzat, M.; Mulder, H.; et al. Clinical factors related to morbidity and mortality in high-risk heart failure patients: the GUIDE-IT predictive model and risk score. Eur J Heart Fail. 2019, 21, 770–8. [Google Scholar] [CrossRef]
- Rocca, H.B.; Wijk, S.S. Biomarkers Natriuretic Peptides in Chronic Heart Failure. Card Fail Rev. 2019, 5, 44–49. [Google Scholar] [CrossRef]
- Madamanchi, C.; Alhosaini, H.; Sumida, A.; Runge, M.S. Obesity and natriuretic peptides, BNP and NT-proBNP: mechanisms and diagnostic implications for heart failure. Int J Cardiol. 2014, 176, 611–7. [Google Scholar] [CrossRef]
- Horwich, T.B.; Hamilton, M.A.; Fonarow, G.C. B-type natriuretic peptide levels in obese patients with advanced heart failure. J Am Coll Cardiol. 2006, 47, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Mehra, M.R.; Uber, P.A.; Park, M.H.; et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J Am Coll Cardiol. 2004, 43, 1590–5. [Google Scholar] [CrossRef] [PubMed]
- Breathett, K.; Allen, L.A.; Udelson, J.; Davis, G.; Bristow, M. Changes in Left Ventricular Ejection Fraction Predict Survival and Hospitalization in Heart Failure With Reduced Ejection Fraction. Circ Heart Fail. 2016, 9, e002962. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H. Methods used for the assessment of LV systolic function: common currency or tower of Babel? Heart. 2013, 99, 1078–1086. [Google Scholar] [CrossRef] [PubMed]
- Marwick, T.H. The role of echocardiography in heart failure. J Nucl Med. 2015, 56 (Suppl. 4), 31S–38S. [Google Scholar] [CrossRef]
- Pastore, M.C.; Mandoli, G.E.; Aboumarie, H.S.; et al. Basic and advanced echocardiography in advanced heart failure : an overview. Heart Fail Rev. 2019, 25, 937–948. [Google Scholar] [CrossRef]
- Savarese, G.; Lund, L. Global Public Health Burden of Heart Failure. Card Fail Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- Galderisi, M.; Cosyns, B.; Edvardsen, T.; et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: An expert consensus document of the European Association of Cardiovascular Imag. Eur Heart J Cardiovasc Imaging. 2017, 18, 1301–1310. [Google Scholar] [CrossRef]
- Di Tullio, M.R.; Qian, M.; Thompson, J.L.P.; et al. Left atrial volume and cardiovascular outcomes in systolic heart failure: effect of antithrombotic treatment. ESC Hear Fail. 2018, 5, 800–808. [Google Scholar] [CrossRef]
- Romano, G.; Magro, S.; Agnese, V.; et al. Echocardiography to estimate high filling pressure in patients with heart failure and reduced ejection fraction. ESC Heart Fail. 2020, 7, 2268–2277. [Google Scholar] [CrossRef] [PubMed]
- Hammoudi, N.; Achkar, M.; Laveau, F.; et al. Left atrial volume predicts abnormal exercise left ventricular filling pressure. Eur J Heart Fail. 2014, 16, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography : An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef] [PubMed]
- Cameli, M.; Pastore, M.C.; Mandoli, G.E.; Nistor, D. Prognosis and Risk Stratification of Patients With Advanced Heart Failure (from PROBE). Am J Cardiol. 2019, 124, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Benfari, G.; Miller, W.L.; Antoine, C.; et al. Diastolic Determinants of Excess Mortality in Heart Failure With Reduced Ejection Fraction. JACC Hear Fail. 2019, 7, 808–17. [Google Scholar] [CrossRef]
- Ommen, S.R.; Nishimura, R.A.; Appleton, C.P.; et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000, 102, 1788–1794. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Marwick, T.H. Use and Limitations of E/e' to Assess Left Ventricular Filling Pressure by Echocardiography. J Cardiovasc Ultrasound. 2011, 19, 169–173. [Google Scholar] [CrossRef]
- Lancellotti, P.; Galderisi, M.; Edvardsen, T.; et al. Echo-Doppler estimation of left ventricular filling pressure: results of the multicentre EACVI Euro-Filling study. Eur Heart J Cardiovasc Imaging. 2017, 18, 961–968. [Google Scholar] [CrossRef]
- Jones, R.; Varian, F.; Alabed, S.; et al. Meta-analysis of echocardiographic quantification of left ventricular filling pressure. ESC Heart Fail. 2021, 8, 566–576. [Google Scholar] [CrossRef]
- Obokata, M.; Kane, G.C.; Reddy, Y.N.; Olson, T.P.; Melenovsky, V.; Borlaug, B.A. Role of Diastolic Stress Testing in the Evaluation for Heart Failure With Preserved Ejection Fraction: A Simultaneous Invasive-Echocardiographic Study. Circulation. 2017, 135, 825–838. [Google Scholar] [CrossRef]
- Hummel, Y.M.; Liu, L.C.Y.; Lam, C.S.P.; et al. Echocardiographic estimation of left ventricular and pulmonary pressures in patients with heart failure and preserved ejection fraction: a study utilizing simultaneous echocardiography and invasive measurements. Eur J Heart Fail. 2017, 19, 1651–1660. [Google Scholar] [CrossRef]
- Marini, C.; Fragasso, G.; Italia, L.; et al. Lung ultrasound-guided therapy reduces acute decompensation events in chronic heart failure. Heart. 2020, 106, 1934–1939. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, J.J.; Pellicori, P.; Flockton, R.; et al. The prevalence and clinical associations of ultrasound measures of congestion in patients at risk of developing heart failure. Eur J Heart Fail. 2021, 23, 1831–1840. [Google Scholar] [CrossRef]
- Ballo, P.; Guarini, G.; Simioniuc, A.; et al. Prognostic value of pulsed tissue Doppler imaging for the assessment of left ventricular systolic function in patients with nonischemic dilated cardiomyopathy. Echocardiography. 2012, 29, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Pellicori, P.; Carubelli, V.; Zhang, J.; et al. IVC Diameter in patients with chronic heart failure: relationships and prognostic significance. JACC Cardiovasc Imaging. 2013, 6, 16–28. [Google Scholar] [CrossRef]
- Jung, I.H.; Park, J.H.; Lee, J.; et al. Left Ventricular Global Longitudinal Strain as a Predictor for Left Ventricular Reverse Remodeling in Dilated Cardiomyopathy. J Cardiovasc Imaging. 2020, 28, 137–149. [Google Scholar] [CrossRef]
- Kaufmann, D.; Szwoch, M.; Kwiatkowska, J.; Raczak, G.; Daniłowicz-Szymanowicz, L. Global longitudinal strain can predict heart failure exacerbation in stable outpatients with ischemic left ventricular systolic dysfunction. PLoS One. 2019, 14, e0225829. [Google Scholar] [CrossRef]
- Nahum, J.; Bensaid, A.; Dussault, C.; et al. Impact of longitudinal myocardial deformation on the prognosis of chronic heart failure patients. Circ Cardiovasc Imaging. 2010, 3, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Sengeløv, M.; Jørgensen, P.G.; Jensen, J.S.; et al. Global Longitudinal Strain Is a Superior Predictor of All-Cause Mortality in Heart Failure with Reduced Ejection Fraction. JACC Cardiovasc Imaging. 2015, 8, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Hasselberg, N.E.; Haugaa, K.H.; Sarvari, S.I.; et al. Left ventricular global longitudinal strain is associated with exercise capacity in failing hearts with preserved and reduced ejection fraction. Eur Heart J Cardiovasc Imaging. 2015, 16, 217–24. [Google Scholar] [CrossRef]
- Modin, D.; Andersen, D.M.; Biering-Sørensen, T. Echo and heart failure: when do people need an echo, and when do they need natriuretic peptides? Echo Res Pract. 2018, 5, R65–R79. [Google Scholar] [CrossRef]
- Carluccio, E.; Biagioli, P.; Mengoni, A.; et al. Left Atrial Reservoir Function and Outcome in Heart Failure With Reduced Ejection Fraction. Circ Cardiovasc Imaging. 2018, 11, e007696. [Google Scholar] [CrossRef]
- Guler, A.; Tigen, K.M.; Dundar, C.; et al. Left atrial deformation and nonischemic dilated cardiomyopathy. A 2D speckle-tracking imaging study. Herz. 2014, 39, 251–7. [Google Scholar] [CrossRef]
- Cameli, M.; Mandoli, G.E.; Loiacono, F.; Dini, F.L.; Henein, M.; Mondillo, S. Left atrial strain: a new parameter for assessment of left ventricular filling pressure. Heart Fail Rev. 2016, 21, 65–76. [Google Scholar] [CrossRef]
- Picano, E.; Pellikka, P.A. Clinical update Ultrasound of extravascular lung water : a new standard for pulmonary congestion. Eur Heart J. 2016, 37, 2097–104. [Google Scholar] [CrossRef]
- Volpicelli, G.; Lichtenstein, D.A.; Kirkpatrick, A.W.; et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012, 38, 577–91. [Google Scholar] [CrossRef] [PubMed]
- Coiro, S.; Rossignol, P.; Ambrosio, G.; et al. Prognostic value of residual pulmonary congestion at discharge assessed by lung ultrasound imaging in heart failure. Eur J Heart Fail. 2015, 17, 1172–1181. [Google Scholar] [CrossRef] [PubMed]
- Gargani, L.; Pang, P.S.; Frassi, F.; et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure : a lung ultrasound study. Cardiovasc Ultrasound. 2015, 13, 40. [Google Scholar] [CrossRef]
- Miglioranza, M.H.; Picano, E.; Badano, L.P.; et al. Pulmonary congestion evaluated by lung ultrasound predicts decompensation in heart failure outpatients. Int J Cardiol. 2017, 240, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Platz, E.; Lewis, E.F.; Uno, H.; et al. Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J. 2016, 37, 1244–1251. [Google Scholar] [CrossRef]
- Chaudhry, S.I.; Wang, Y.; Concato, J.; Concato, J.; Gill, T.M.; Krumholz, H.M. Patterns of weight change preceding hospitalization for heart failure. Circulation 2007, 116, 1549–1554. [Google Scholar] [CrossRef] [PubMed]
- Bui, A.L.; Fonarow, G.C. Home monitoring for heart failure management. J Am Coll Cardiol. 2012, 59, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Riegel, B.; Moser, D.K.; Anker, S.D.; et al. State of the science: Promoting self-care in persons with heart failure: A scientific statement from the american heart association. Circulation 2009, 120, 1141–63. [Google Scholar] [CrossRef]
- Goldberg, L.R.; Piette, J.D.; Walsh, M.N.; et al. Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the Weight Monitoring in Heart Failure (WHARF) trial. Am Heart J. 2003, 146, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Mullens, W.; Damman, K.; Harjola, V.-P.; et al. The use of diuretics in heart failure with congestion — a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019, 21, 137–155. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; et al. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef]
- Grant, A.D.M.; Smedira, N.G.; Starling, R.C.; Marwick, T.H. Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol. 2012, 60, 521–528. [Google Scholar] [CrossRef]
- Meluzín, J.; Špinarová, L.; Dušek, L.; Toman, J.; Hude, P.; Krejčí, J. Prognostic importance of the right ventricular function assessed by Doppler tissue imaging. Eur J Echocardiogr. 2003, 4, 262–271. [Google Scholar] [CrossRef]
- Almodares, Q.; Wallentin Guron, C.; Thurin, A.; et al. Larger right atrium than left atrium is associated with all-cause mortality in elderly patients with heart failure. Echocardiography. 2017, 34, 662–667. [Google Scholar] [CrossRef]
- Kato, T.S.; Stevens, G.R.; Jiang, J.; et al. Risk stratification of ambulatory patients with advanced heart failure undergoing evaluation for heart transplantation. J Hear Lung Transplant. 2013, 32, 333–340. [Google Scholar] [CrossRef]
- Kircher, B.J.; Himelman, R.B.; Schiller, N.B. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990, 66, 493–6. [Google Scholar] [CrossRef] [PubMed]
- Nath, J.; Vacek, J.L.; Heidenreich, P.A. A dilated inferior vena cava is a marker of poor survival. Am Heart J. 2006, 151, 730–5. [Google Scholar] [CrossRef] [PubMed]
- Curbelo, J.; Rodriguez-Cortes, P.; Aguilera, M.; Gil-Martinez, P.; Martín, D.; Fernandez, C.S. Comparison between inferior vena cava ultrasound, lung ultrasound, bioelectric impedance analysis and natriuretic peptides in chronic heart failure. Curr Med Res Opin. 2019, 35, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Razi, R.; Estrada, J.R.; Doll, J.; Spencer, K.T. Echocardiography At The “Point Of Care” Bedside Hand-Carried Ultrasound by Internal Medicine Residents Versus Traditional Clinical Assessment for the Identification of Systolic Dysfunction in Patients Admitted with Decompensated Heart Failure. J Am Soc Echocardiogr. 2011, 24, 1319–1324. [Google Scholar] [CrossRef] [PubMed]
- Dalen, H.; Gundersen, G.H.; Skjetne, K.; et al. Feasibility and reliability of pocket-size ultrasound examinations of the pleural cavities and vena cava inferior performed by nurses in an outpatient heart failure clinic. Eur J Cardiovasc Nurs. 2015, 14, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, G.H.; Norekval, T.M.; Haug, H.H.; et al. Adding point of care ultrasound to assess volume status in heart failure patients in a nurse-led outpatient clinic. A randomised study. Heart. 2016, 102, 29–34. [Google Scholar] [CrossRef]
- Saha, N.M.; Barbat, J.J.; Fedson, S.; Anderson, A.; Rich, J.D.; Spencer, K.T. Outpatient Use of Focused Cardiac Ultrasound to Assess the Inferior Vena Cava in Patients With Heart Failure. Am J Cardiol. 2015, 116, 1224–1228. [Google Scholar] [CrossRef]
- Curbelo, J.; Aguilera, M.; Rodriguez-Cortes, P.; Gil-Martinez, P.; Fernandez, C.S. Usefulness of inferior vena cava ultrasonography in outpatients with chronic heart failure. Clin Cardiol. 2018, 41, 510–517. [Google Scholar] [CrossRef]
- Lee, H.F.; Hsu, L.A.; Chang, C.J.; et al. Prognostic significance of dilated inferior vena cava in advanced decompensated heart failure. Int J Cardiovasc Imaging. 2014, 30, 1289–1295. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




