1. Introduction
People from Black and Asian backgrounds are more likely to die from COVID-19 but less likely to be vaccinated [
1], contributing to concerns about low vaccine uptake exacerbating health inequalities already experienced by ethnic minority groups. The United Kingdom (UK) COVID-19 vaccine campaign started in December 2020 with primary care services (including General Practitioner (GP) practices and Community Pharmacies) leading vaccine delivery [
2]. The most recently released data on vaccination rates in adults shows that by March 2023, 75.8% of the general population have received at least three COVID-19 vaccinations [
1]. Whilst vaccine delivery has been successful in reaching a large number of people, vaccine uptake has been particularly low in ethnic minority groups (with 34.8% of Pakistani adults, 36.3% of Bangladeshi adults and 41.8% of Black African adults continuing to a fourth vaccination compared to 78.1% of White adults) [
1]. Now that we’ve moved into COVID-19 recovery, the government, healthcare professionals and communities face the challenge of building vaccine confidence and addressing health inequalities faced by ethnic minority groups.
Vaccine hesitancy has been defined by the World Health Organization (WHO) as a refusal or delay in vaccine acceptance [
3] and is not a new concept. In 2014 the WHO SAGE working group developed the ‘3 C’s’ model to categorise reasons for hesitancy into 3 areas: Convenience (access), Confidence (trust), and Complacency (perceived risk) [
4]. Whilst vaccine hesitancy has been conceptualised in the general population, less is known about vaccine hesitancy in people from ethnic minority backgrounds. During the COVID-19 pandemic rapid assessment of underlying factors leading to vaccine hesitancy in ethnic minority groups was undertaken and data demonstrated that factors associated with vaccine hesitancy were younger age, less education, lower gross annual income and living in areas of high deprivation [
5] [
6]. Research since the pandemic including a semi-structured interview study by Woodhead et al [
7] has further emphasized the role of wider inequalities beyond COVID-19 in vaccine mistrust, including socio-economic disadvantage and exposure to and anticipation of discrimination [
8,
9]. This supports findings from the work of medical sociologists including Harding, Maxwell and Nazroo, who suggest that we need to better understand structural factors (including socioeconomic position and experience of racism) in order to unpick the processes through which ethnic minority status leads to health inequalities [
10]. Understanding and addressing these processes is likely to lead to longer-term impacts to reduce vaccine inequalities than information alone. This is supported by the evidence on parental vaccination decisions which suggests that interventions focused on vaccine knowledge, education and messaging change vaccine attitudes and increase vaccination rates in the short-term. However, in the longer-term interventions solely focused on vaccine messaging may lead to dissatisfaction due to deeper-rooted beliefs driven by individual experiences and beliefs resulting from structural inequalities [
11,
12,
13,
14].
1.1. Theoretical underpinnings
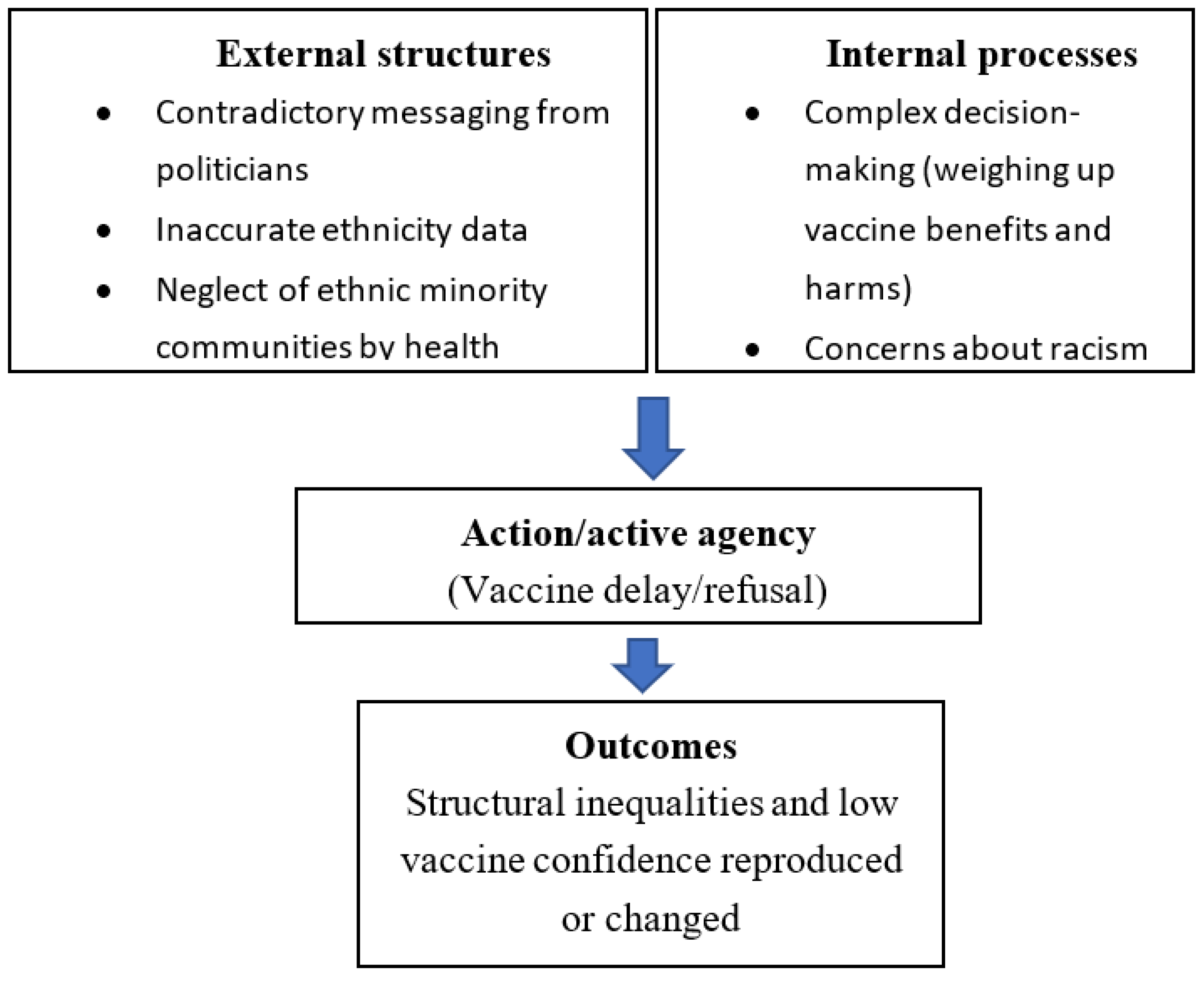
We will draw on structuration theory [
15] and realist social theory [
16,
17] to inform our understanding of how the social environment (‘social structures’) interact with human action (‘agency’) to influence vaccine acceptance by ethnic minority communities. The theory of structuration groups social structures into ‘external’ and ‘internal’ [
15,
18,
19]. External structures represent the social structures in which people operate and are mediated by institutional infrastructures and power relations, political & medical ‘authority’, social position and associated identity and network of social interactions, and race, racial inequality and racialized social environments where Black and other non-White group members are routinely stigmatized [
20]. Structural constraints and opportunities are created by health and social policies, and this impacts people’s ability to leverage resources and be active in their own health [
21]. Internal structures (or processes) refer to how and what people ‘know’ and can be analytically divided into ‘general dispositions’ (world-views, morals, principles and attitudes) and ‘conjuncturally-specific knowledge’ (knowledge specific to the immediate decision-making situation) [
15,
18,
19]. The action (active agency) produced can have intended and unintended impacts on internal and external structures, which may be reproduced or changed [
15,
22].
Within realist social theory, behaviour results from people (agents) actively and reflexively drawing upon both their attitudes and knowledge (internal structures) and social interactions (external structures) [
22]. Social interactions can also facilitate the sharing of common concerns, and make people reflect and act differently [
17].
1.2. Aim and objectives
The aim of the research study is to improve the understanding of COVID-19 vaccine confidence and structural factors influencing confidence in low uptake ethnic minority groups in London and surrounding areas.
The specific objectives are to:
Explore which structural factors influence decision-making, including external structures (education, employment, income, social identity, positioning and networks and experiences of structural racism) and internal structures (morals, values, attitudes and knowledge);
Explore actions which would enable primary care and public health campaigns to improve confidence in COVID-19 vaccination in ethnic minority groups.
2. Materials and Methods
2.1. Study design
This was a qualitative study consisting of focus groups and interviews with people from ethnic minority (non-White British) communities. Both focus groups and interviews were offered. Focus groups are particularly useful for gaining insights from minority ethnic groups because they help gain an understanding of group “norms”, values and “community” responses [
23,
24,
25,
26]. Two groups took part in focus groups and the remaining participants expressed a preference to be interviewed one-to-one.
2.2. Study setting
The interviews and focus groups were conducted online in London, UK from December 2021 to March 2022. Vaccine rollout in the UK started in December 2020. COVID-19 vaccine uptake data showed that the four ethnic minority groups with the lowest uptake were: Bangladeshi, African, Caribbean and Pakistani [
27,
28]. Data also showed that London was the lowest uptake area in England (64% of people aged over 16 years old had had at least one dose of the vaccine compared to an average of 89% in England) [
28].
At the start of the study in December 2021 new variants of the COVID-19 virus were emerging, and hospitalisations were increasing, particularly in Bangladeshi and Pakistani communities. A booster vaccine was being offered, with the aim of achieving a high uptake by January 2022. There was also discussion about mandatory vaccination for NHS and social care workers.
2.3. Patient and Public Involvement (PPI)
SP led a participatory community engagement project exploring under-representation in health by ethnic minority communities (“Diverse Voices”) in June 2021 which led to the formation of the PPI group supporting this study (CK, LW and AI) [
29]. The PPI representatives were part of the core research team and advised on the study design, recruitment strategy, research flyer, topic guide and interpretation of findings. Approaches were based on NIHR guidance on inclusive public involvement [
30,
31].
2.4. Sampling and recruitment
All ethnic groups apart from White British with current or previous concerns about COVID-19 vaccines, leading to delay or refusal to be vaccinated, were eligible to take part in the study. Interpreting services for Bengali and Urdu speakers were provided. Access and skills to use MS Teams or a telephone were needed. Eligible participants were identified and recruited through established Patient and Public Involvement (PPI) networks, community organizations and snowball sampling. Organizations in areas with larger Bangladeshi, Pakistani, African and Caribbean populations (including Newham, Tower Hamlets and Hackney) were contacted by email with the research flyer and asked to disseminate via email, newsletters and WhatsApp. Professionals were eligible if they worked in the NHS, Local Authorities or Voluntary and Community Organisations (VCSOs) providing COVID-19 vaccine information and access to ethnic minority communities in London. Professionals were identified from community outreach events and snowball sampling, and contacted by email with participant and consent information.
Ethical approval for the study was received from the University College London Research Ethics Committee (ID no 6761/002).
2.5. Data collection and analysis
Interviews were conducted by lead author SP, who is experienced in qualitative methods and working with ethnic minority communities. A topic guide (Supplement 1) was developed by SP, informed by the literature, PPI representatives and Co-Is. The topic guide covered the following areas: social background; experiences of the pandemic and offer of vaccination; access to vaccine information; factors influencing decision-making; comparison with other vaccines; and suggestions for improving COVID-19 vaccine information and access. Focus groups and interviews were conducted online and recorded using MS Teams to comply with guidance on minimising the spread of COVID-19. Focus groups lasted approximately 60-90 minutes and interviews ranged from 30-60 minutes. Participants were given a shopping voucher as a thank you for their time. All participants had sufficient English language skills to conduct the focus groups and interviews in English. Professional transcription services were used to transcribe recordings verbatim. SP anonymised the transcripts and checked the transcripts against the recordings for accuracy.
Transcripts were managed using NVivo 12 software [
32]. Inductive reflective thematic analysis informed by Braun and Clarke was used to analyse data (working from the data up) [
33]. This approach ensured that analytic categories were obtained gradually from the data and experiences of the participants themselves [
34]. Data analysis took place alongside data collection, so that early concepts were identified, and the topic guide updated accordingly to explore key issues in more detail. Led by SP, the process started with data familiarisation, followed by data coding when each phrase, line and paragraph of the transcripts was scrutinised in detail. Ideas and concepts were labelled with a code and codes were sorted so that data with similar content were located together in NVivo [
35]. Codes from a sample of transcripts were shared and discussed at two researchers’ meetings with SP and AK, a qualitative researcher with expertise in vaccine hesitancy. Analysis was informed by participatory action research approaches to ensure the findings were grounded in the experiences of the participants and people affected by the research question [
36]. An online 90-minute participatory workshop was therefore held with a small group (n=4) of PPI representatives and participants who responded to an email invitation to take part. Two anonymised transcripts were shared with the group in advance and co-production methods [
37,
38] were used to discuss and share ideas about the meaning emerging from sections of the transcripts. This included individuals documenting their ideas collectively using a digital white board (Jamboard [
39]).
Once codes had been shared and validated in the data meetings and workshop, they were grouped into initial themes by SP and shared with all co-authors. To go beyond description of the data and produce a more exploratory analysis, we produced a ‘first-level analysis’ summarising main themes and sub-themes from the thematic analysis, and an overall thematic framework examining connections between themes and existing structuration theory (illustrated in Table 2 and
Figure 1) [
35].
3. Results
This section may be divided by subheadings. It should provide a concise and precise description of the experimental results, their interpretation, as well as the experimental conclusions that can be drawn.
3.1. Participants
Focus groups and interviews were conducted with 22 participants online using MS Teams. Fourteen participants were members of the public and 8 were professionals involved in COVID-19 vaccination campaigns. Of the members of the public, the age of participants ranged from 21-67 years old. N=9 were female and n=5 were male. 10/14 (71.4%) were from African, Caribbean, Pakistani or Bangladeshi backgrounds. The remaining participants were mixed race (Caribbean/White British), Indian or preferred not to say. 13/14 (92.8%) of participants were in employment (4/14 or 28.6% in the NHS). Demographic characteristics are summarised in
Table 1.
3.2. First level analysis
The following overarching themes were identified:
Lack of information credibility and clarity
Discrimination and barriers to healthcare
Personal beliefs, characteristics and experiences influencing vaccine choice
Social networks and community cohesion
3.2.1. Lack of information credibility and clarity
Some participants lacked trust in official information and the government. This included trust in data on the number of deaths in different ethnic groups. Participants described how they did not share their ethnicity when asked, and their concern that if others did the same, this would result in inaccurate data.
“I find that it is a bit misleading. I don't know, I haven't seen enough reports that make me feel encouraged by the data that’s been given. As I said, when they ask me my own ethnicity, I always say unknown, I would prefer not to say, but for me the figures are not correct anyway. They're not really reflecting the fact that there may be other people who don’t put down their ethnicity or race, they just don’t do that. So I don't think the figures are really a true reflection of what is happening.” [P01, Ethnicity not disclosed, 57 years, Female]
Some participants expressed that they did trust the government, and rejected the idea that ethnic minority communities were not supported adequately.
“I trust the government information that they give. I don’t think there is any difference between member of the – of any community. If people, they want to pick up on this, saying that, you know, the government didn’t’ do enough for BME (Black and minority ethnic people) or whatever, I don’t think it’s true”. [P05, Pakistani, 36 years, Female]
Other participants described how inconsistency in government messaging led to contradiction and confusion, which undermined their trust in politicians.
“Compared to other countries that our government has been very inconsistent. One example I think I do have is like maybe New Zealand.. And I think it was a Scandinavian country, they were very clear they were very like, “Well, this is how we're doing it and this is why we're doing it.” And they spoke directly to the people. In the UK, it's the Prime Minister says this, and the health secretary is saying that and they’re just contradicting themselves. So that confuses people.” [P03, Mixed race African/Caribbean/White, 61 years, Female]
Lack of clarity about the information on vaccine benefits and safety was also up the benefits and risks more complicated.
“The problem with me is that they said that, if you’ve got underlying health conditions, take the vaccine, it’s going to protect you. Then, when you hear a story about people dying of the vaccine and then you say – and they said no, they took the vaccine but they had underlying health condition, that’s why they died. But surely the aim of the vaccine is to protect them so they don’t die, and if they’re going to die they might as well not have the vaccine and, you know? So I don’t know. It’s complicated.” [P07, Pakistani, 54 years, Female]
The complexity of decision-making was also described by professionals providing information on vaccination. Professionals described their experience of meeting people who analysed the risks and benefits of vaccination and did not see the benefit of vaccination if they were still able to catch the virus and experience symptoms.
“Often where people don’t follow – I talk a lot on webinars to people, individuals - and where they stop to basically listen is when you say, “Well, because you’re vaccinating to protect yourself from severe illness and death,” they can follow that. But if you then say, “Vaccination doesn’t mean that you can’t harbour the virus and that you may still be experiencing symptoms,” that’s when people, I think, make their own internal risk benefit analysis. And they come to the conclusion that that’s not a good enough reason.’ [P14, Consultant in Public Health]
3.2.2. Discrimination and barriers to healthcare
Professionals described their experiences doing community outreach events answering questions about COVID-19 vaccination from members of the public. One professional talked about a community event with young Black people and their families in east London. Attendees questioned why health professionals were holding events to talk to them about COVID-19 vaccination, when similar events and communication had not taken place on other issues, suggesting that these communities themselves feel underserved by health services.
“So I did quite a few webinars and actually did a face-to-face event with young black people in August 2021, and that was, again, really interesting. Young people with their parents came in and there was quite a lot of anger around, ‘you’re coming to talk to us about this vaccine’ – first of all, just concerns about the vaccine and actually that it was going to be harming people. But actually more than that, someone stood up and said, “Look, you’ve never bothered about anything else. Why are you coming to talk to us about the vaccines?” And I think that’s why I got involved in that. I thought it was a good opportunity that if we can really reach into underserved communities for this, then there should be no reason why we can’t do the same for other health conditions, whether it’s long-term conditions or childhood immunisations, etc.” [P16, GP and Clinical Advisor to NHS England]
Members of the public also called for more action to improve overall health instead of focusing on vaccination specifically and used examples of long-term conditions disproportionately affecting ethnic minority communities including diabetes.
“I think health needs to be helped, especially the ethnic minorities, especially we have a lot of, I think obesity is a huge problem with ethnic minorities and diabetes obviously is, and that’s kind of related. It’s not just COVID, it’s other things as well which can affect you in the long term with these diseases. So I think just improving your overall health instead of just saying, “Just have the vaccine and everything will be better,” because it won’t.” [P09, Indian, 42 years, Male]
The sentiment about neglect was echoed by other professionals who talked about the need to acknowledge and be honest about structural discrimination towards ethnic minority communities, and the challenges this presents with talking to people about vaccination.
“That question is, how do we respond to a legitimate accusation of 500 years of structural underfunding and racism with like a sentence? My kind of crass response to that is, you go, “Yeah, you’re right. You’re totally right, and this vaccine will help save your life. So I can’t fix this structural underfunding. All I can do is help you protect yourself from COVID.” But they’re right, like it’s a legitimate criticism, and I think to deny it is the worst thing you can do.” [P17, Head of Community Public Health for a Local Authority]
Professionals reported hearing members of the public express concerns about racism in vaccine development and deployment. One concern was that vaccines were deployed quickly in order to be tested on people of African descent.
“You know some people said things like “are you aware that they’ve developed it so fast because they want to test it on people of African descent first.” [P21, Chief Executive of a VCSO supporting Black communities]
Another professional described how people were reluctant to share their ethnicity because they were worried that they would be given a different, perhaps less safe, vaccine to people from a White background.
“I had one woman early on, say, “Why did you ask my ethnicity?” and I said, “So we can make sure it’s equally distributed.” And she looked at me and I was like, “Do you think there’s like a white cupboard and a black cupboard?” She was like, “Yeah, basically,” and told me a story of a friend of hers, who was also black, who was a carer, who had a person she was caring for was white. And so she had her vaccine because it came out of the same vial. So I think we have to be really respectful now, in particular, of people’s decisions.” [P17, Head of Community Public Health for a Local Authority]
Professionals reflected on the community engagement work that occurred during the vaccine campaign, including what had gone well and how this could be developed in future public health campaigns. Professionals suggested putting the same amount of resource into addressing other health problems which are commonly seen in ethnic minority communities, including diabetes and mental health.
“Other things that I think worked well outside when it came to the uptake of the vaccines, especially in ethnic minority communities, was a recognition of the historical injustice and this idea of trust. I think trust was a big issue. I found that in spaces where there was good uptake, when there was good engagement, there were places where professionals and practitioners acknowledged the historical wrongs and were willing to kind of say, ‘you know what, I understand why you do not trust us. We understand that you were wronged, we are partners on this journey together, I would like you to….‘ I think that actually did work well, especially you know, where communities were hesitant.’ [P18, Public Health Programme Lead for a Local Authority]
3.2.3. Personal beliefs, characteristics and experiences influencing vaccine choice
Religious beliefs, age and occupation emerged as personal factors participants considered in making their vaccine choices. Participants talked about how their religious beliefs influenced their values around taking the COVID vaccine. One participant described whether he becomes unwell from COVID-19 or not is determined by God rather than vaccination.
“in a different manner some people think, “Oh, if I’m going to die of COVID, I might as well take the vaccine and get less side-effects off it, off the severe form of the virus, and then at least I won’t die.” But whether you’re going to die or you’re not going to die, as a Muslim we leave that in the hands of God. So God decides who’s going to die and who’s going to live. So you know, it’s not in our hands. So you could take the double-jab, get COVID, get it severe and pass away. It can, it can happen. It’s happened to family members.” [P07, Pakistani, 54 years, Female]
Four (27%) members of the public interviewed worked in health and social care. They talked about their professional experiences during the pandemic including inadequate equipment, exposure to infection due to insufficient Personal Protective Equipment (PPE), and consultation on mandatory vaccination (which was later rejected). Participants expressed views against mandatory vaccination due to the policy disregarding healthcare workers’ personal, political and religious views.
“The problem with mandatory vaccination is that from my personal view, you're asking somebody to say we’re going to force you to put a chemical into your body against your will. And I think that’s how it should be presented, because ultimately that is what we’re asking people to do if we’re saying it’s mandatory. We’re saying you have to put this chemical into your body, regardless of your opinion, whether it’s personal or political or religious or spiritual, whatever it is. And I just think that’s completely wrong to do that.” [P09, Indian, 42 years, Male]
Participants described how mandatory vaccination forced healthcare workers to consider how much they wanted to stay in their roles in the NHS, compared to how strongly they felt about being vaccinated.
“for me, it’s not about information, it’s about how comfortable you are about putting something in your body. It’s just a question of are you comfortable or not, and at this point, I’m thinking about it but I’m actually thinking to myself that actually I’m ready to leave the NHS [laughs] rather than take it. Because it’s that serious where they're giving you this ultimatum that you take it or leave your job.” [P10, Black African, 43 years, Female]
3.2.4. Social networks and community cohesion
Participants described the roles of social media, family, friends, neighbours, community organisations and Community Champions in sharing vaccine information and contributing to vaccination choices.
Participants discussed the role of social media as a source of information in ethnic minority communities, how and why it was used, and the impact it had on decision-making about vaccination. Professionals expressed concerns that some people developed mistrust for the government and NHS due to having limited sources of information apart from word of mouth and social media. They also described the use of social media in spreading misinformation or information discrediting scientific findings.
“A lot of the webinars that I’ve been on, you can sense those undertones of mistrust in the Government and the NHS, exacerbated by a restricted channel of information and education that people have. Which means that people are more reliant on word-of-mouth and also, social media – WhatsApp videos, I think, has a lot to answer for. I think they’ve allowed fringe ideas to become very mainstreamed and spread very quickly. So that’s kind of what we were up against and a lot of that came out at the webinars that I’ve done since then, these myths that started right at the start.
And some of them are actually not necessarily myths. Some things are based on a couple of scientific reports that then got blown out of proportion. And even though they were disproven after a while, the damage was already done.” [P16, GP and Clinical Advisor to NHS England]
Members of the public also talked about relying on online information from social media due to it being easier to access, particularly during lockdown.
“When people are at home, because you cannot go out, the only source they get information from is the internet and social media and news, you know? Because you will only believe whatever you see on those. Like, you can get access of information from here.” [P06, Bangladeshi, 32 years, Male]
Members of the public talked about the way social media has replaced traditional media such as newspapers as a source of information and is perceived as a reliable source of news.
“If you look at Instagram just like a new generation of the newspaper, so you look at it as your daily news.” [P08, Bangladeshi, 21 years, Male]
Leaders of community organisations supporting ethnic minority communities talked about their approaches to discussing COVID-19 vaccination with the public. They described the need for respect for people’s age, beliefs, historical relationships with medications and concerns about vaccination.
“There was a respect in terms of age, there was a respect in terms of people’s belief system. Because what we recognised was that we had to do things in the context of people’s historical relationship with medicines and so forth, particularly when they were designed at such rapid speed. So people’s suspicions, we had to roll with that resistance. And what happened is the wonderful thing about being culturally informed and culturally aware was that we gained much more rich information about the individual because they were comfortable in conversing with us.” [P21, Chief Executive of a VCSO supporting Black communities]
Participants described family, friends and neighbours as their immediate contacts in their social networks. One participant talked about her neighbours in a block of flats in Tower Hamlets and their sense of collective feeling about not being vaccinated.
“There’s about three or four of us, sometimes. We’re like little old ladies, standing on the landing, talking about all sorts of issues, and the COVID and the vaccination and, you know? And I think, out of us, only one’s had it. You know? And the rest of them has the similar thing that I’ve got, you know what I mean? We just talk about the same thing and, the way I say I feel, that’s them, as well.” [P12, Black Caribbean, 67 years, Female]
Professionals who reflected on successes from community engagement programmes described the role of Community Champions in providing tailored simple information to the public in formats and channels that were known to be easier to access including WhatsApp.
“Champions programmes are where public health teams or the NHS (the statutory body) provides tailored, simple information to people in a form that is easy for them to digest and share…And in Newham, we’ve used WhatsApp as well as email and Zoom. I live in [London borough] and I’m a champion, and we get our information by email. And to be honest with you, I don’t share it, because it’s a lot of words and I have to cut and paste it into WhatsApp and I don’t. Whereas in Newham, we did one page infographics as JPEGs that people could send on, and we were told that they were really powerful. And the biggest lessons from that are – these are really like pedantic – but make stuff that’s easy for people to share. So put stuff in JPEG, not PDF, send it on WhatsApp, not email, and do it quickly when the information changes so that people trust it and they’re able to use it.” [P17, Head of Community Public Health for a Local Authority]
Second level analysis
Overarching themes from the first level analysis (lack of information credibility and clarity; discrimination and barriers to healthcare; personal beliefs, characteristics and experiences influencing vaccine choice; social networks and community cohesion) were mapped onto Stones’ structuration theory [
15,
18,
19]. Themes were grouped as either ‘external’ or ‘internal’, depending on whether they represent the external structural context in which people operate, or whether they represent the internal processes (morals, principles, attitudes and knowledge) that people use to make COVID-19 vaccination decisions. This is represented in the conceptual framework in
Figure 1.
4. Discussion
4.1. Key findings
This was a qualitative study aiming to improve the understanding of COVID-19 vaccine confidence and structural factors influencing confidence in low uptake of ethnic minority groups in London and surrounding areas. Reasons for low uptake are complex and multifactorial. We identified four overarching themes which influenced COVID-19 vaccine confidence: (i) lack of information credibility and clarity; (ii) discrimination and barriers to healthcare; (iii) personal beliefs, characteristics and experiences; and (iv) social networks and community cohesion.
Our findings on information credibility and clarity are consistent with existing literature on ethnicity data and public trust. In the UK, ethnicity data relating to the number of covid deaths and vaccinations were recorded using NHS healthcare records and self-report to health professionals. Researchers have highlighted inconsistencies and poor quality of ethnicity data collection [
40] due to people feeling less willing to share their ethnicity due to lack of explanation about why the data is being collected, concerns about racial discrimination and a feeling of ethnic categories not being representative [
40,
41,
42]. Our findings on public trust are consistent with evidence from studies in the UK and US, including co-produced research with UK ethnic minority communities, suggests that trust in organisations and individuals promoting COVID-19 vaccines is amongst one of the most important factors in determining uptake [
43].
Discrimination was a driver for lack of vaccine confidence due to neglect of ethnic minority communities from health services (particularly in the prevention and treatment of health conditions which are prevalent in ethnic minority communities), the impact of structural racism, and concerns about racism in vaccine development and deployment. There is emerging evidence on the role of racism and discrimination as a driver of ethnic health inequalities [
44,
45,
46], mediated through structured social and economic inequalities including in health behaviours, psychosocial stress, and differential access to material, social and healthcare resources [
45]. We also identified concerns about racism in vaccine development and deployment. This is consistent with research exploring the views of ethnic minority and vulnerable communities towards participation in COVID-19 trials, which found that African and Afro-Caribbean participants feared vaccines were developed to eradicate Black people [
47], and research with community organisations since the start of the COVID-19 vaccine programme which identified mistrust in vaccines due to previous unethical research (including the US Tuskegee syphilis study) [
48]. Asian, Black and Mixed ethnic groups are under-represented or incorrectly classified in UK COVID-19 clinical trials [
49] which is likely to further perpetuate these concerns.
Religious beliefs, age and occupation emerged as personal characteristics which influenced vaccine confidence, with some people believing that they could not protect themselves from COVID-19 through vaccination as it is “in the hands of God”. Cultural and religious influences have also been identified in previous studies, which have suggested that working with mosques and faith leaders may be effective in addressing vaccine confidence [
50]. Participants working in the NHS described being less willing to be vaccinated following the consultation on mandatory vaccination for health and social care staff and having a preference for losing their job rather than being forced to be vaccinated. Previous studies have suggested that ethnic minority healthcare workers are less likely to be vaccinated against COVID-19 than their White colleagues [
51], with reasons including fear around institutional pressure to be vaccinated [
7].
Participants described the roles of social media, family, friends, neighbours, community organisations and Community Champions as drivers of vaccine confidence. People had access to vaccine misinformation through social media, but also relied on it as a way of easily accessing up to date news and information. This is consistent with a 2020 study of sources of information across diverse ethnic groups in the UK which found that family and social media were sources of information for some people, and that negative WhatsApp messages spread rapidly among social networks [
50].
Representatives of community organisations described taking a listening approach as successful ways of engaging with the public, as well as respecting existing beliefs and values. Community Champions networks were identified as a successful way of sharing reliable vaccine information and improving vaccine confidence with local communities, particularly when shared in formats that were easily accessible. This is consistent with a study of barriers and facilitators to COVID-19 vaccine uptake in ethnic minorities in primary care which found that channelling information through local community organisations and Community Champions networks was a key factor in influencing uptake [
52].
The theory of structuration has previously been used in research on food security [
53,
54] to inform understanding of how systemic forces determine why Black and other ethnic minority groups are disproportionately at risk of food insecurity and other health inequities. Although other studies have highlighted the role of structural racism in reducing vaccine confidence in ethnic minority communities [
55,
56], to our knowledge, this is the first study to use structuration to explore vaccine inequalities in ethnic minority communities.
4.2. Strengths & limitations
The strengths of this study are the qualitative exploration of experiences and views and the diversity of the participants. Both members of the public and professionals were interviewed, and members of the public all self-identified as either currently or previously refusing vaccination (35% are unvaccinated). This provided insights into both the lived experience of having low COVID-19 vaccine confidence, and the experience of professionals providing vaccine information and supporting communities with access to vaccination. Professionals represented a range of organisations involved in vaccine roll-out including the NHS, public health, local authorities and community groups. We were able to interview people from ethnic minority backgrounds with the lowest vaccine uptake (African, Caribbean, Bangladeshi and Pakistani), and collect demographic data on country of birth, first language, vaccination status, education level and occupation. 27% of members of the public worked as healthcare professionals which revealed insights into the experience of working in the NHS during the covid pandemic, and views towards mandatory vaccination.
PPI involvement was a further strength, particularly the preparatory community engagement work [
29] which supported PPI involvement .A data validation workshop with participants and PPI ensured analysis took a participatory approach and the findings were grounded in lived experience.
Limitations of the study include the focus on one geographic area (London and the southeast) and the number of participants (n=15 members of the public and n=7 professionals). Although London is an area of high diversity and low COVID-19 vaccine uptake, this limits the generalisability of findings. The number of participants within each ethnic group was small limiting our ability to explore between-group differences in more depth and compare views of different groups. Data were collected from December 2021 to March 2022, a year after the start of vaccine rollout. Ethnic inequalities in vaccine uptake were established, part of the public discourse and interventions to improve vaccine uptake in ethnic minority groups had been implemented. The research has demonstrated that vaccine confidence is highly sensitive to social context and perceived risk, and the timing of the research may have influenced participants responses. Although interpreters were available all interviews were conducted in English, excluding people who may have had different experiences and views of COVID-19 vaccination due to language. All interviews were conducted by SP who is a female academic GP of Indian ethnicity. SP’s role as a healthcare professional could have reduced trust or resulted in social desirability bias.
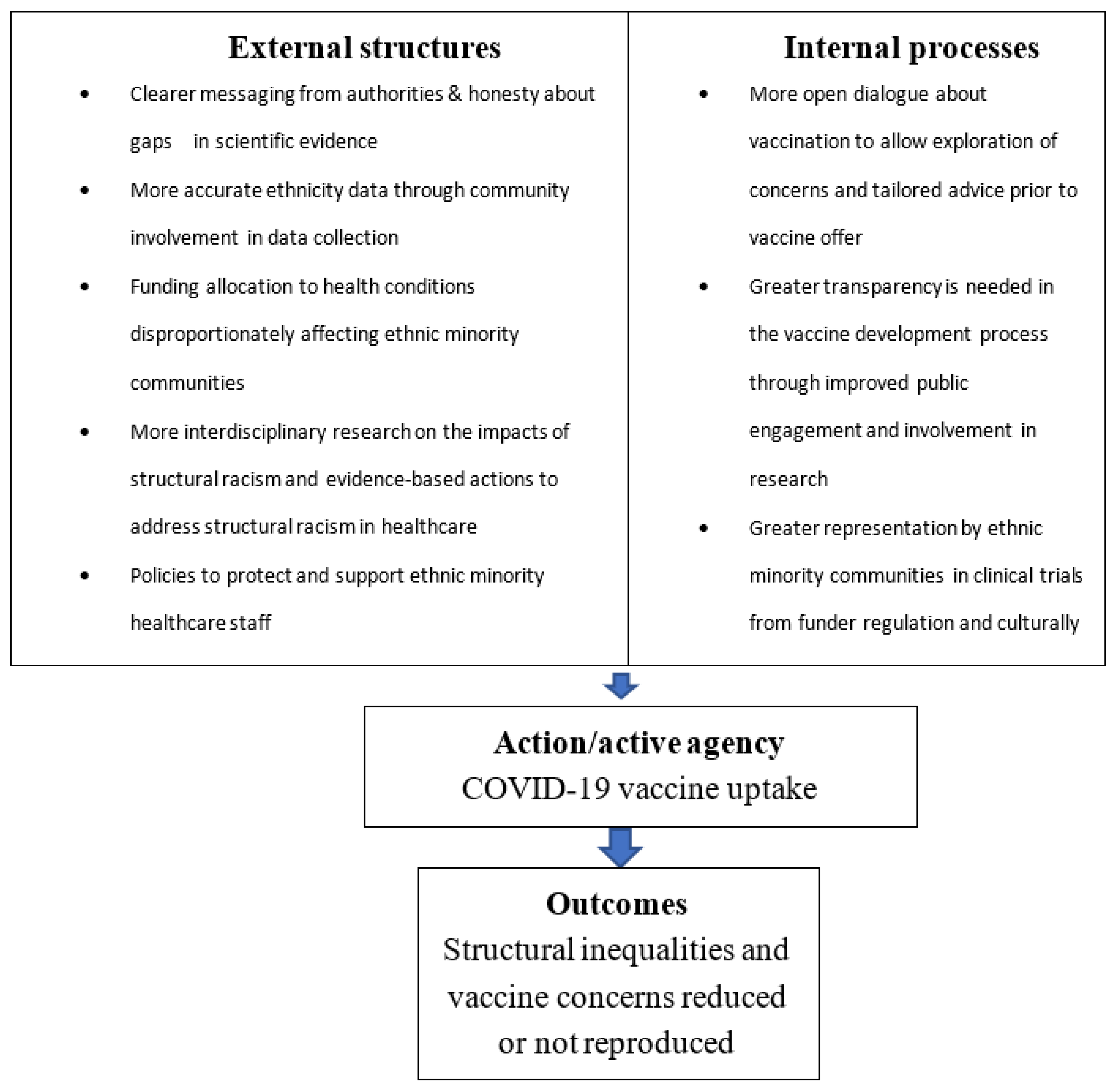
4.3. Implications for research, policy & practice
Participant views reflect the strengths of community organisations and Community Champions networks in supporting people from ethnic minority communities. However, there are several concerns influencing decisions to be vaccinated that are not addressed by these strategies. Barriers mediated by social structures cannot be addressed through community-led information and engagement alone.
Recommendations therefore address social factors which contribute to ethnic inequalities. The thematic framework based on structuration theory has been used to develop recommendations for policy-makers and healthcare professionals to improve confidence in COVID-19 vaccination in ethnic minority groups (see
Figure 2).
With regard to ethnicity data, improved collection and reporting processes are needed, including working with communities to design appropriate ethnicity categories and explaining rationale for data collection. Neglect of ethnic minority communities by health services needs to be rectified by creating more open dialogue about vaccination to allow exploration of concerns and tailored advice prior to vaccine offer. More funding and resource need to be allocated to clinical conditions disproportionately affecting ethnic minority communities or where ethnic minority communities experience poorer outcomes. In terms of vaccine development, greater transparency is needed in the vaccine development process through improved public engagement and involvement in research. Greater representation by ethnic minority communities in clinical trials could be achieved if regulations from research funders and culturally adapted recruitment processes are adopted. Another research recommendation is for more interdisciplinary research combining both health and sociological perspectives to understand structural inequalities (including the impacts of socioeconomic position and experience of racism and discrimination). To support the ethnic minority workforce in the NHS, workplace policies and practices are needed which support and protect staff wellbeing.
5. Conclusions
It may be possible to improve confidence in COVID-19 vaccination for some people from ethnic minority communities using culturally appropriate and accessible information via community organisations and Community Champions. However, the accumulated morals, views and attitudes and the external structures that shape them (including institutional infrastructures and power relations, political & medical ‘authority’, social position, identity and interactions, and race, racial inequality and racialized social environments) are less amenable to change through information-sharing alone. More research is needed to explore the impacts of external social structures on ethnic health inequalities and actions to address these and achieve ethnic health equity.
Supplementary Materials
The following supporting information can be downloaded at:
www.mdpi.com/xxx/s1, Figure S1: Thematic framework of factors influencing low COVID-19 vaccine confidence in ethnic minority communities (Adapted from Greenhalgh and Stones) ; Figure S2: Thematic framework of recommendations for increasing COVID-19 vaccine confidence in ethnic minority communities; Table S1: Demographic characteristics of members of the public
Author Contributions
Conceptualization, SP, SK, SM, CK, AI, PG; methodology, SP, SK, SM, CK, AI, PG; validation, SP, AK, CK, AI; formal analysis, SP, AK; data curation, SP; writing—original draft preparation, SP; writing—review and editing, SP, AK, SM, CK, AI, PG; administration, SP; funding acquisition, SP, SK, SM, CK, AI, PG. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Institute for Health and Care Research (NIHR) School for Primary Care Research (project reference 571). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Patient and Public Involvement (PPI) funding was supplemented by a UCL Biomedical Research Centre starter grant for PPI (project reference: BRC830).
Institutional Review Board Statement
This is a UCL research staff study which has been ethically approved by the UCL Research Ethics Committee (ID no 6761/002). Lead researcher: Dr Shoba Poduval. Email: s.poduval@ucl.ac.uk
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
We acknowledge the interview participants for the generosity of their time and perspectives.
Conflicts of Interest
PG receives support from the National Institute for Health Research (NIHR) Applied Research Collaborations West Midland and is a NIHR Senior Investigator. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Office for National Statistics. Coronavirus and vaccination rates in adults by socio-demographic characteristic and occupation, England: December 2020 to March 2023 2023 [Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/bulletins/coronavirusandvaccinationratesinadultsbysociodemographiccharacteristicandoccupationengland/december2020tomarch2023#sociodemographic-characteristics. 20 December.
- NHS England. COVID-19 vaccination deployment strategy and operational readiness. 2020.
- MacDonald, NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161-4. [CrossRef]
- World Health Organization. Report of the SAGE working group on vaccine hesitancy 2014.
- Office for National Statistics. Coronavirus and vaccine hesitancy, Great Britain: 13 January to 7 February 2021.
- NHS Race and Health Observatory. Maximising uptake of the COVID-19 vaccine for ethnic minority people. 2021.
- Woodhead C, Onwumere J, Rhead R, Bora-White M, Chui Z, Clifford N, et al. Race, ethnicity and COVID-19 vaccination: a qualitative study of UK healthcare staff. Ethnicity & health. 2021:1-20.
- Rhead RD, Chui Z, Bakolis I, Gazard B, Harwood H, MacCrimmon S, et al. Impact of workplace discrimination and harassment among National Health Service staff working in London trusts: results from the TIDES study. BJPsych Open. 2021;7(1):e10. [CrossRef]
- Kline R, Naqvi H, Razaq SA, Wilhelm R. NHS workforce race equality standard. 2016 Data analysis report for NHS Trusts. 2017.
- Nazroo, JY. Addressing inequalities in healthy life expectancy. 2015. [Google Scholar]
- Amin AB, Bednarczyk RA, Ray CE, Melchiori KJ, Graham J, Huntsinger JR, et al. Association of moral values with vaccine hesitancy. Nature Human Behaviour. 2017;1(12):873-80. [CrossRef]
- Opel DJ, Mangione-Smith R, Robinson JD, Heritage J, DeVere V, Salas HS, et al. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. American journal of public health. 2015;105(10):1998-2004. [CrossRef]
- Sales JM, Painter JE, Pazol K, Gargano LM, Orenstein W, Hughes JM, et al. Rural parents' vaccination-related attitudes and intention to vaccinate middle and high school children against influenza following educational influenza vaccination intervention. Human vaccines. 2011;7(11):1146-52. [CrossRef]
- Spleen AM, Kluhsman BC, Clark AD, Dignan MB, Lengerich EJ. An increase in HPV-related knowledge and vaccination intent among parental and non-parental caregivers of adolescent girls, age 9–17 years, in Appalachian Pennsylvania. Journal of Cancer Education. 2012;27(2):312-9. [CrossRef]
- Stones, R. Structuration theory: Bloomsbury Publishing; 2017.0230213642.
- Archer, MS. Realist social theory: The morphogenetic approach: Cambridge university press; 1995.0521484421.
- Donati, P. The ‘Relational Subject’ According to a Critical Realist Relational Sociology. Journal of Critical Realism. 2016;15(4):352-75. [CrossRef]
- Greenhalgh T, Stones R, Swinglehurst D. Choose and Book: A sociological analysis of ‘resistance’ to an expert system. Social Science & Medicine. 2014;104:210-9. [CrossRef]
- Greenhalgh T, Swinglehurst D, Stones R. Health Services and Delivery Research. Rethinking resistance to ‘big IT’: a sociological study of why and when healthcare staff do not use nationally mandated information and communication technologies. Southampton (UK): NIHR Journals Library.
- Misir, P. Dismantling Systemic Racism and Structuration Theory. In: Misir P, editor. COVID-19 and Health System Segregation in the US: Racial Health Disparities and Systemic Racism. Cham: Springer International Publishing; 2022. p. 101-17.
- Sen, A. The idea of justice. Journal of human development. 2008;9(3):331-42.
- Greenhalgh T, Stones R. Theorising big IT programmes in healthcare: Strong structuration theory meets actor-network theory. Social Science & Medicine. 2010;70(9):1285-94. [CrossRef]
- Greenwood N, Ellmers T, Holley J. The influence of ethnic group composition on focus group discussions. BMC Medical Research Methodology. 2014;14(1):107.
- Kidd PS, Parshall MB. Getting the focus and the group: enhancing analytical rigor in focus group research(1049-7323 (Print)).
- Focus Group Methodology: Principles and Practice. London2011. Available from: https://methods.sagepub.com/book/focus-group-methodology.
- Halcomb EJ, Gholizadeh L Fau - DiGiacomo M, DiGiacomo M Fau - Phillips J, Phillips J Fau - Davidson PM, Davidson PM. Literature review: considerations in undertaking focus group research with culturally and linguistically diverse groups. (0962-1067 (Print)),.
- NHS England. COVID-19 Vaccinations 2021 [Available from: https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/.
- Public Health England. Coronavirus (COVID-19) vaccinations in the United Kingdom 2021 [cited 2021 02 September]. Available from: https://coronavirus.data.gov.uk/details/vaccinations.
- Poduval S, Kaviraj C. Research Department of Primary Care and Population Health Blog2022. [cited 2022]. Available from: https://blogs.ucl.ac.uk/pcph-blog/2022/03/04/diverse-voices-a-ucl-community-engagement-project-on-diversity-in-health-research-participation/.
- National Institute for Health Research. Being inclusive in public involvement in health and care research 2021 [cited 2023 10 Jan ]. Available from: https://www.nihr.ac.uk/documents/being-inclusive-in-public-involvement-in-health-and-care-research/27365#how-to-cite-this-guidance.
- NIHR CLAHRC East Midlands Centre for BME Health. Toolkit for increasing participation of BAME groups in health and social care research. 2018.
- QSR International Pty Ltd. NVivo (Version 12) 2018 [cited 10 Jan 2023]. Available from: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home.
- Terry G, Hayfield N, Clarke V, Braun V. Thematic analysis. The SAGE handbook of qualitative research in psychology. 2017;2:17-37.
- Pope, C. Qualitative research in health care / edited by Catherine Pope, Nicholas Mays. Fourth edition. ed. Pope C, Mays N, editors: Hoboken, New Jersey : Wiley Blackwell; 2020.1-119-41086-X1-119-41088-6.
- Canesqui AM, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Studentes and Researchers. Botucatu, Brazil: Interface; 2010.
- Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health. 2006;60(10):854-7. [CrossRef]
- Co-Production Collective. coproductioncollective.co.uk 2021 [cited 2021 30 April]. Available from: https://www.coproductioncollective.co.uk/.
- West NARC. A map of resources for co-producing research in health and social care. 2020.
- Google. What's Jamboard? 2023 [Available from: https://support.google.com/jamboard/answer/7424836?hl=en.
- Routen A, Akbari A, Banerjee A, Katikireddi SV, Mathur R, McKee M, et al. Strategies to record and use ethnicity information in routine health data. Nature Medicine. 2022;28(7):1338-42. [CrossRef]
- Mathur R, Rentsch CT, Venkataraman K, Fatumo S, Jobe M, Angkurawaranon C, et al. How do we collect good-quality data on race and ethnicity and address the trust gap? Lancet. 2022;400(10368):2028-30. [CrossRef]
- Bignall T, Phillips J. Improving the recording of ethnicity in health datasets Wellcome; 2022.
- Change, Cf. Collaboration for change: Promoting vaccine uptake. 2021.
- Devakumar D, Selvarajah S, Abubakar I, Kim S-S, McKee M, Sabharwal NS, et al. Racism, xenophobia, discrimination, and the determination of health. The Lancet. 2022;400(10368):2097-108. [CrossRef]
- Selvarajah S, Corona Maioli S, Deivanayagam TA, de Morais Sato P, Devakumar D, Kim S-S, et al. Racism, xenophobia, and discrimination: mapping pathways to health outcomes. The Lancet. 2022;400(10368):2109-24. [CrossRef]
- Race and Health Observatory. Ethnic Inequalities in Healthcare: A Rapid Evidence Review. 2022.
- Ekezie W, Czyznikowska BM, Rohit S, Harrison J, Miah N, Campbell-Morris P, et al. The views of ethnic minority and vulnerable communities towards participation in COVID-19 vaccine trials. Journal of Public Health. 2021;43(2):e258-e60. [CrossRef]
- Kadambari S, Vanderslott S. Lessons about COVID-19 vaccine hesitancy among minority ethnic people in the UK. The Lancet Infectious Diseases. 2021;21(9):1204-6. [CrossRef]
- Murali M, Gumber L, Jethwa H, Ganesh D, Hartmann-Boyce J, Sood H, et al. Ethnic minority representation in UK COVID-19 trials: systematic review and meta-analysis. BMC Med. 2023;21(1):111. [CrossRef]
- Sides E, Jones LF, Kamal A, Thomas A, Syeda R, Kaissi A, et al. Attitudes towards coronavirus (COVID-19) vaccine and sources of information across diverse ethnic groups in the UK: a qualitative study from June to October 2020. BMJ Open. 2022;12(9):e060992. [CrossRef]
- Gogoi M, Wobi F, Qureshi I, Al-Oraibi A, Hassan O, Chaloner J, et al. "The vaccination is positive; I don't think it's the panacea": A qualitative study on COVID-19 vaccine attitudes among ethnically diverse healthcare workers in the United Kingdom. PLoS One. 2022;17(9):e0273687. [CrossRef]
- Magee L, Knights F, McKechnie DGJ, Al-bedaery R, Razai MS. Facilitators and barriers to COVID-19 vaccination uptake among ethnic minorities: A qualitative study in primary care. PLOS ONE. 2022;17(7):e0270504. [CrossRef]
- Regnier-Davies J, Edge S, Austin N. The intersection of structure and agency within charitable community food programs in Toronto, Canada, during the COVID-19 pandemic: cultivating systemic change. Critical Public Health. 2023;33(3):355-62. [CrossRef]
- Dean WR, Sharkey JR, Johnson CM. The Possibilities and Limits of Personal Agency. Food, Culture & Society. 2016;19(1):129-49. [CrossRef]
- Corbie-Smith, G. Vaccine Hesitancy Is a Scapegoat for Structural Racism. JAMA Health Forum. 2021;2(3):e210434-e. [CrossRef]
- Hussain B, Latif A, Timmons S, Nkhoma K, Nellums LB. Overcoming COVID-19 vaccine hesitancy among ethnic minorities: A systematic review of UK studies. Vaccine. 2022;40(25):3413-32. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).