Submitted:
04 July 2023
Posted:
05 July 2023
You are already at the latest version
Abstract
Keywords:
2. INTRODUCTION
3. RELATED WORKS
4. DATASET
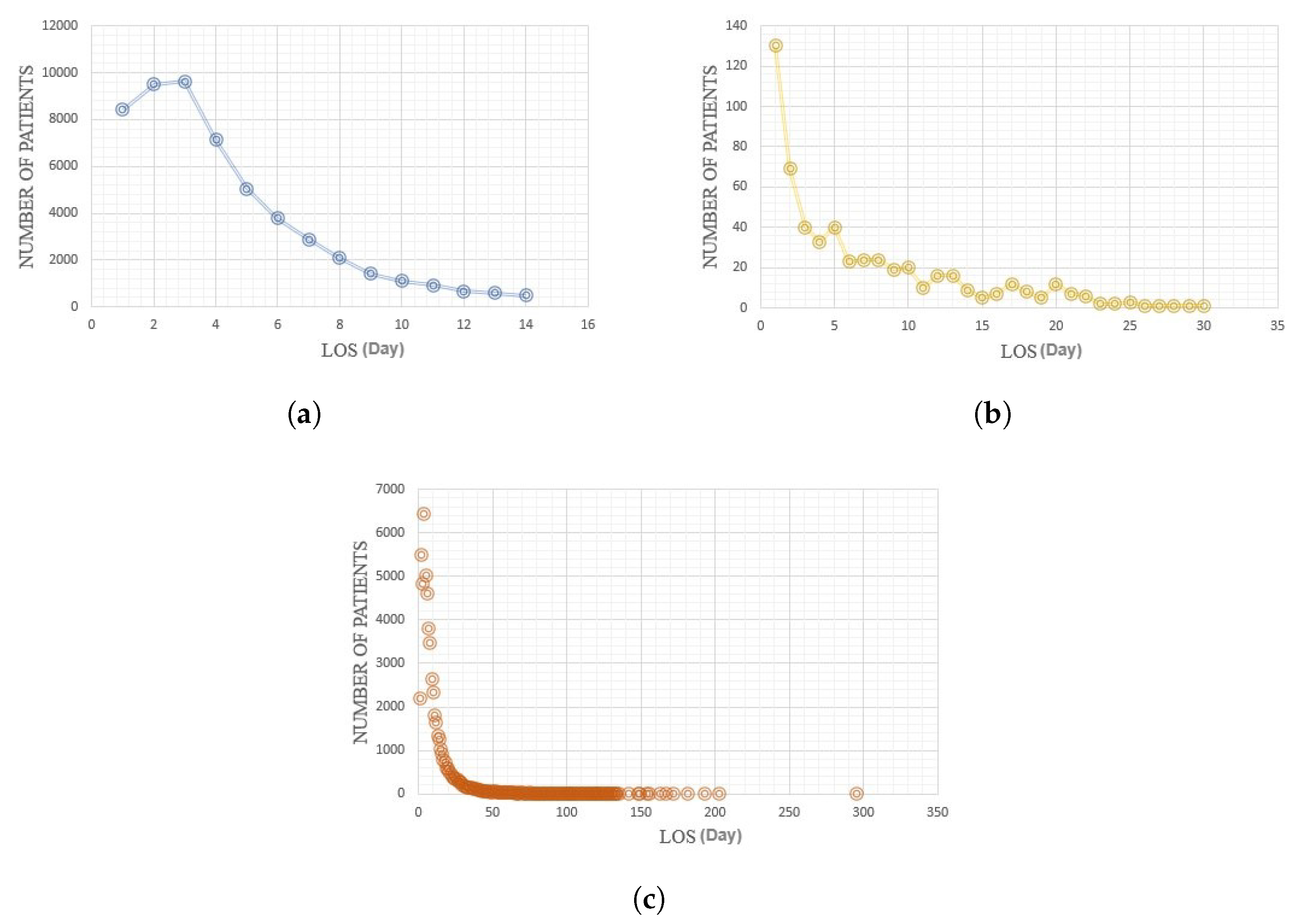
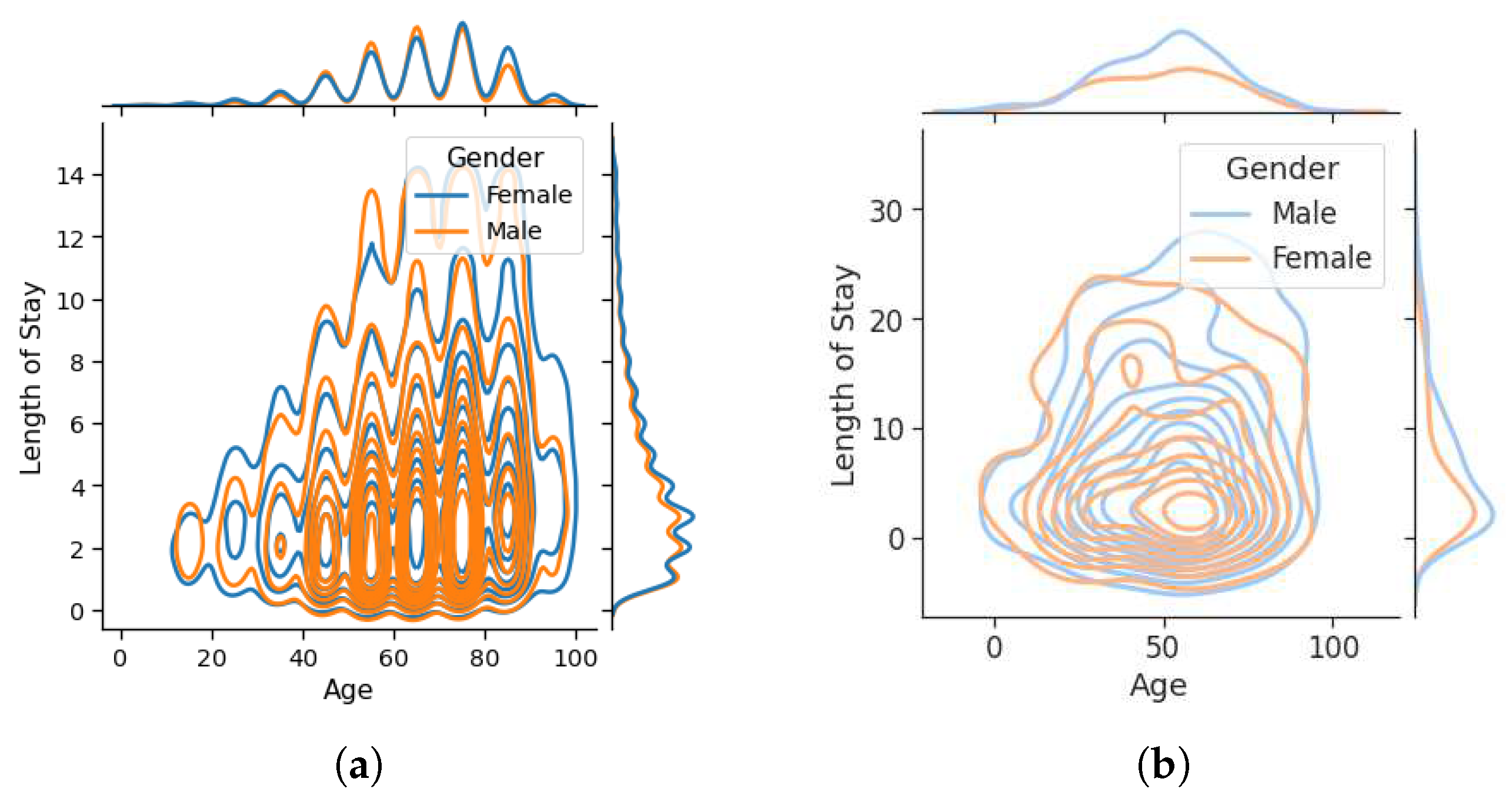
4.1. Diabetes
4.2. COVID-19
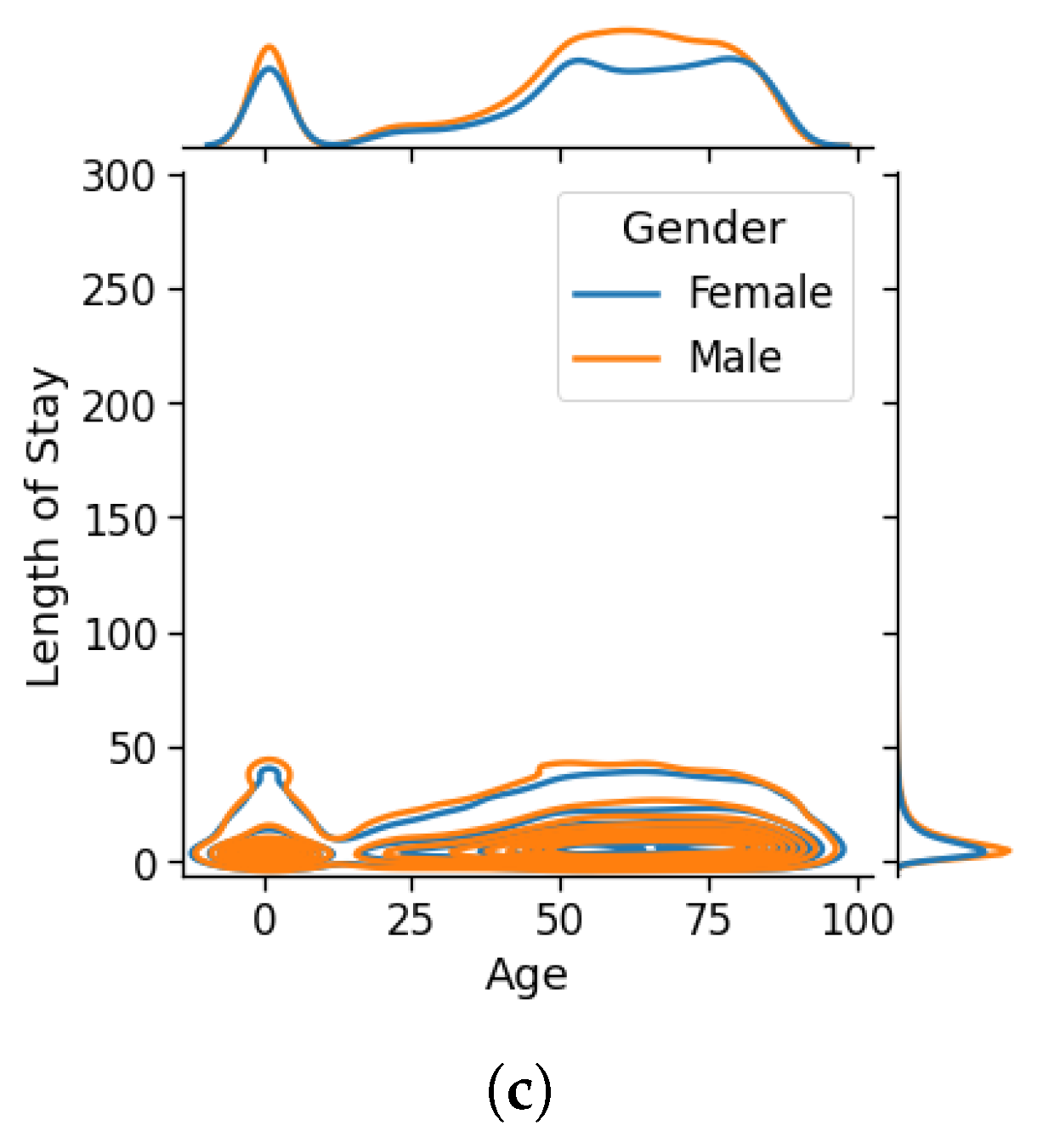
4.3. ICU
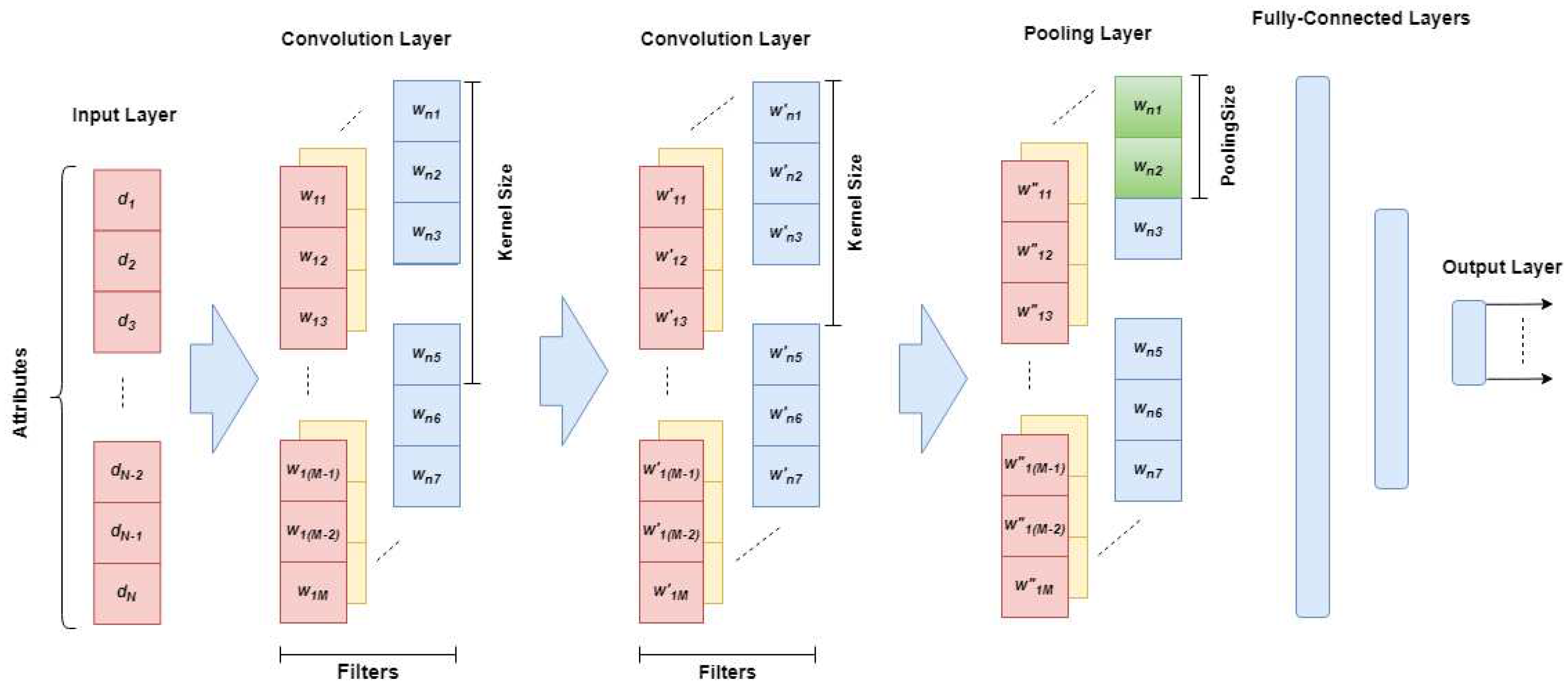
5. MODEL
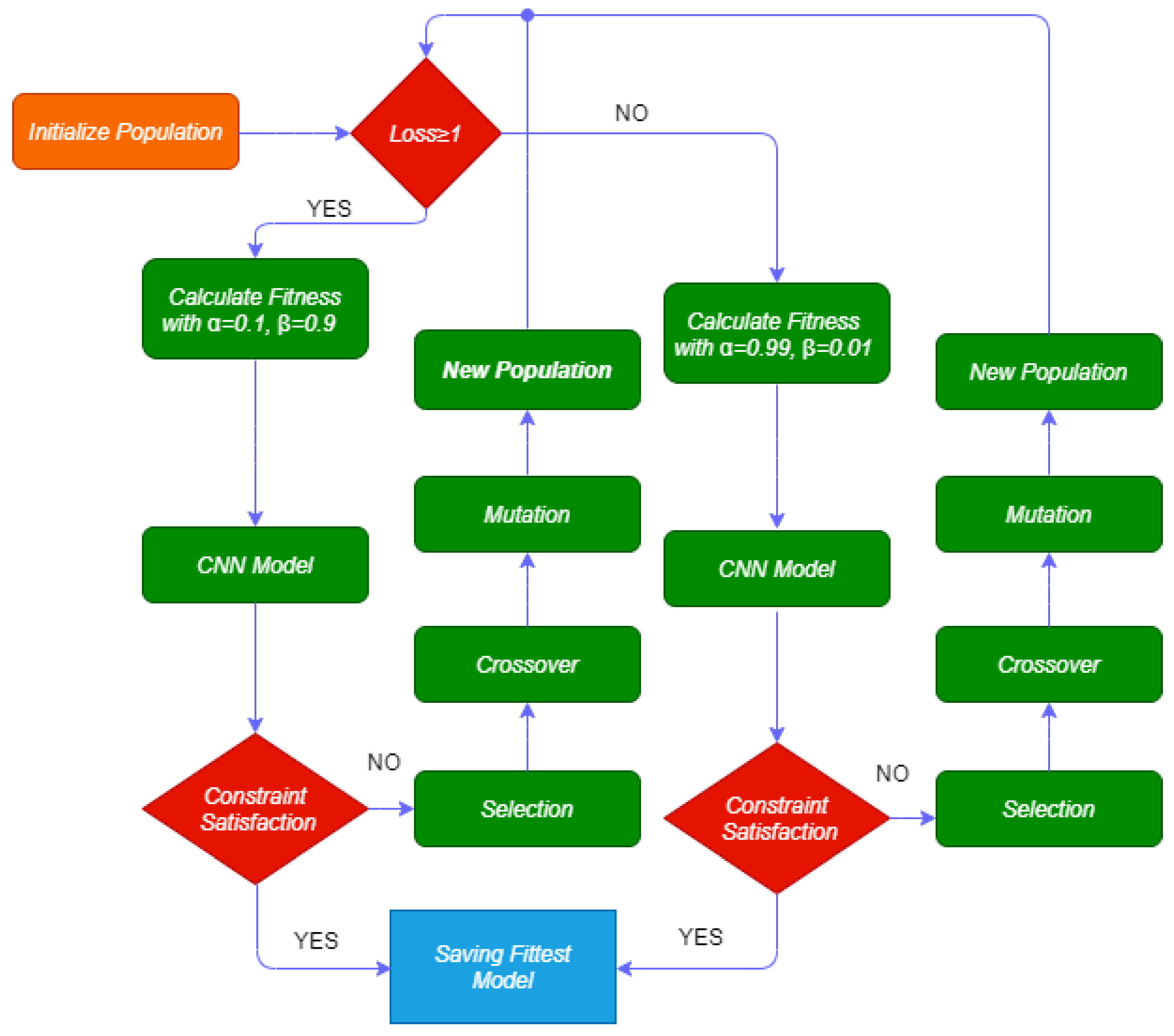
5.1. GAOCNN
- If the loss (l), is greater than or equal to 1, the Categorical Crossentropy Loss (CCL) varies between 1 and 10. So, we define alpha and beta as 0.1 and 0.9, respectively.
- If the loss (l), is less than 1, the CCL varies between 0.001 and 1. So, we define and as 0.99 and 0.01, respectively.
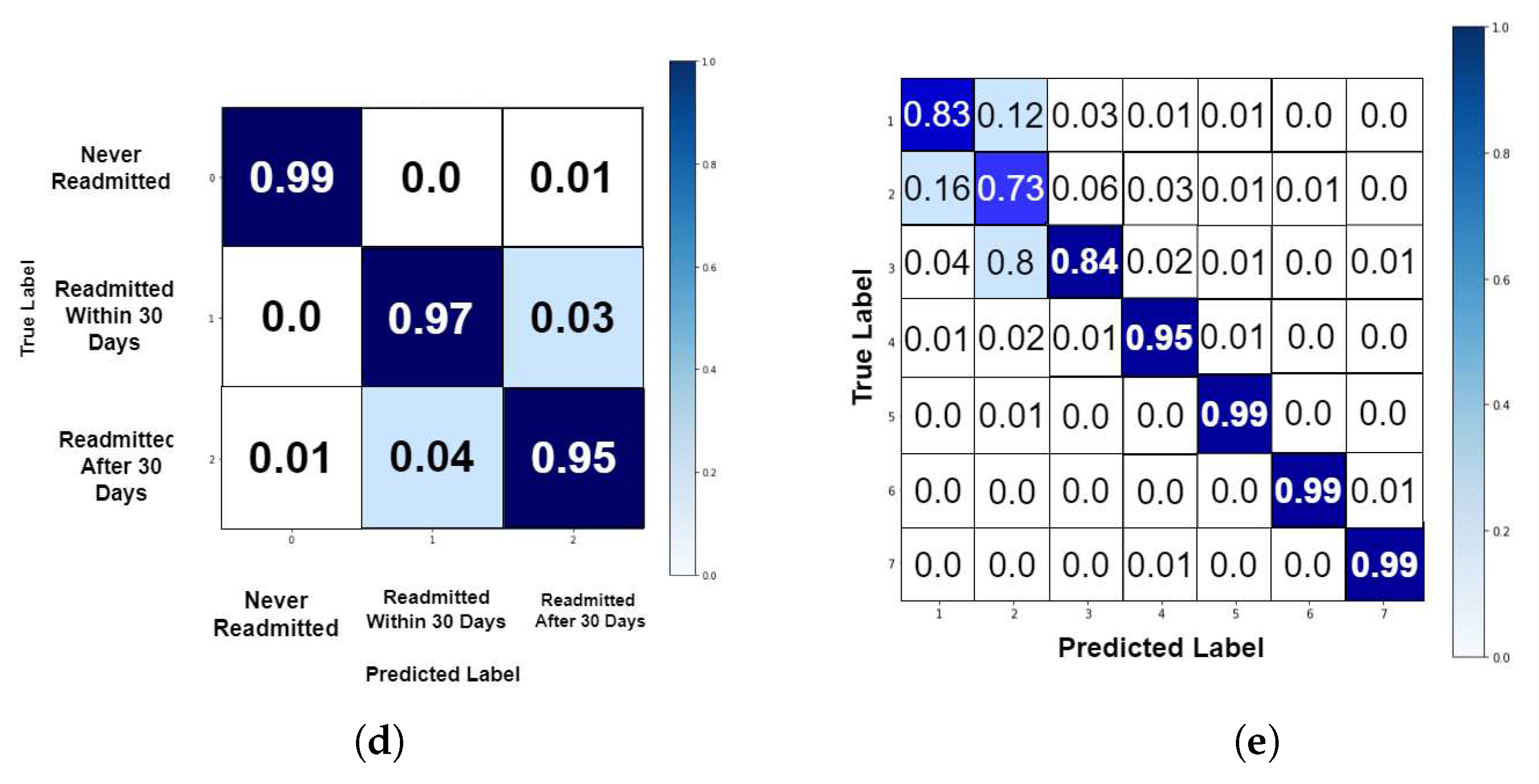
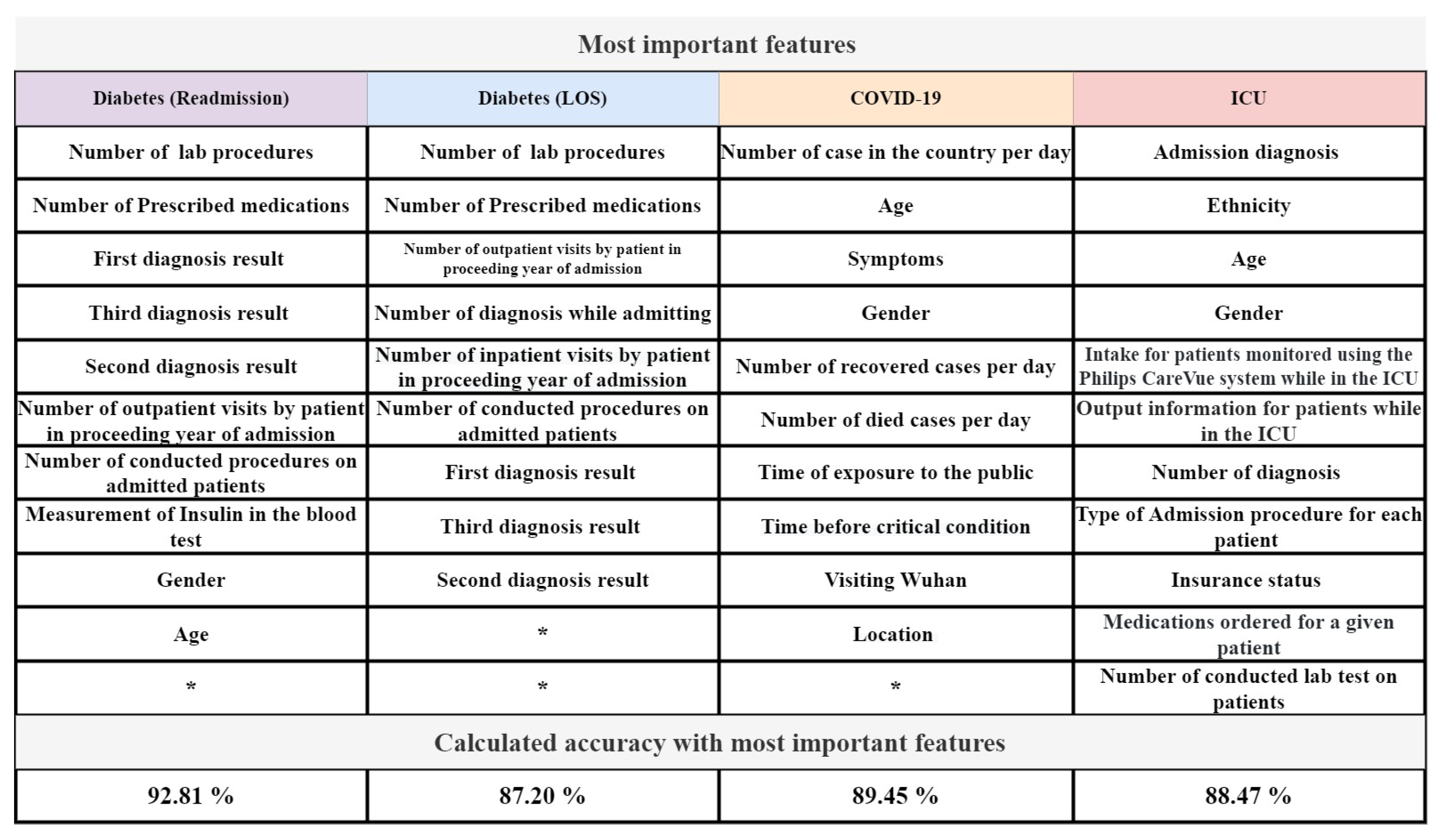
6. EXPERIMENTAL RESULT
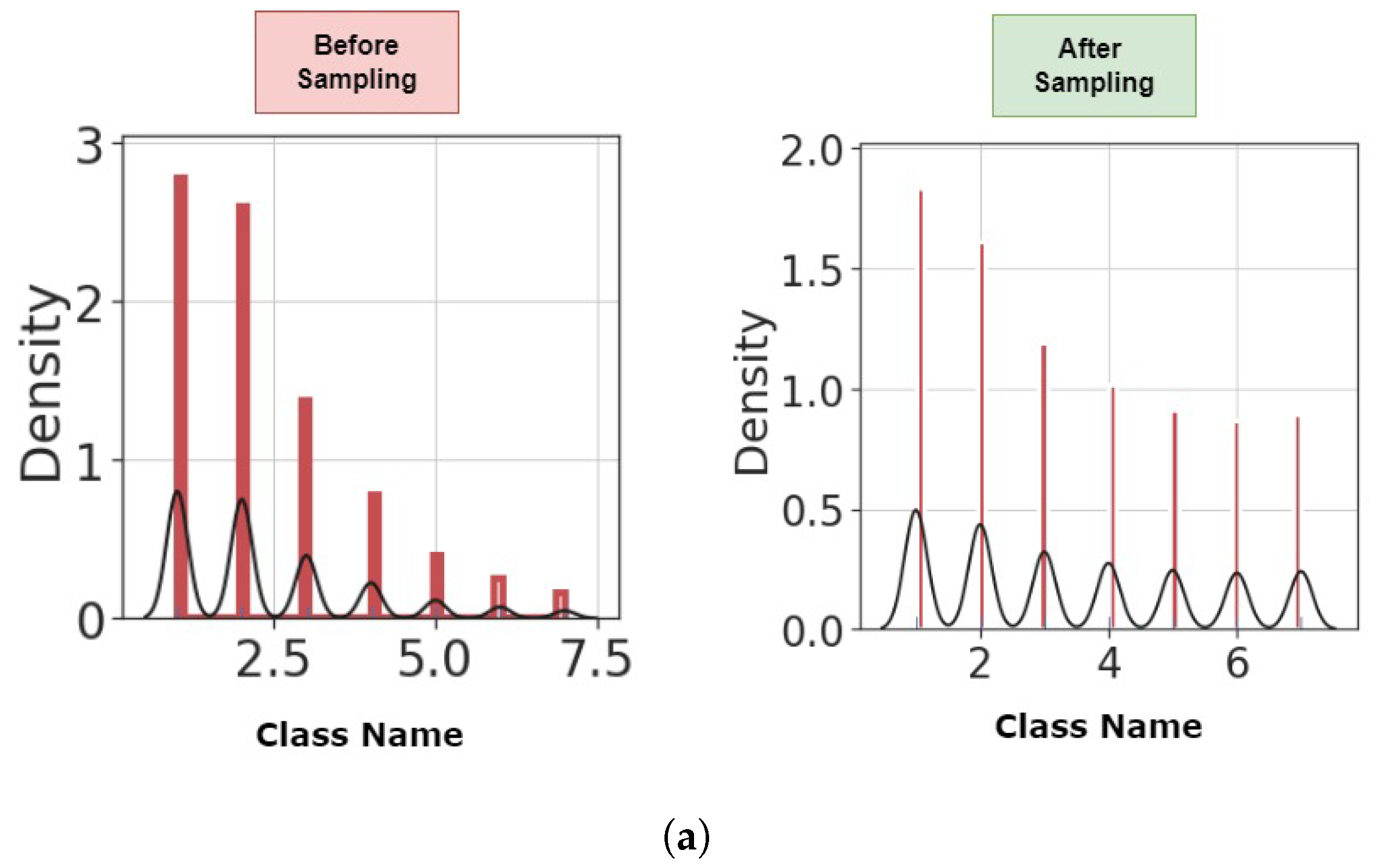
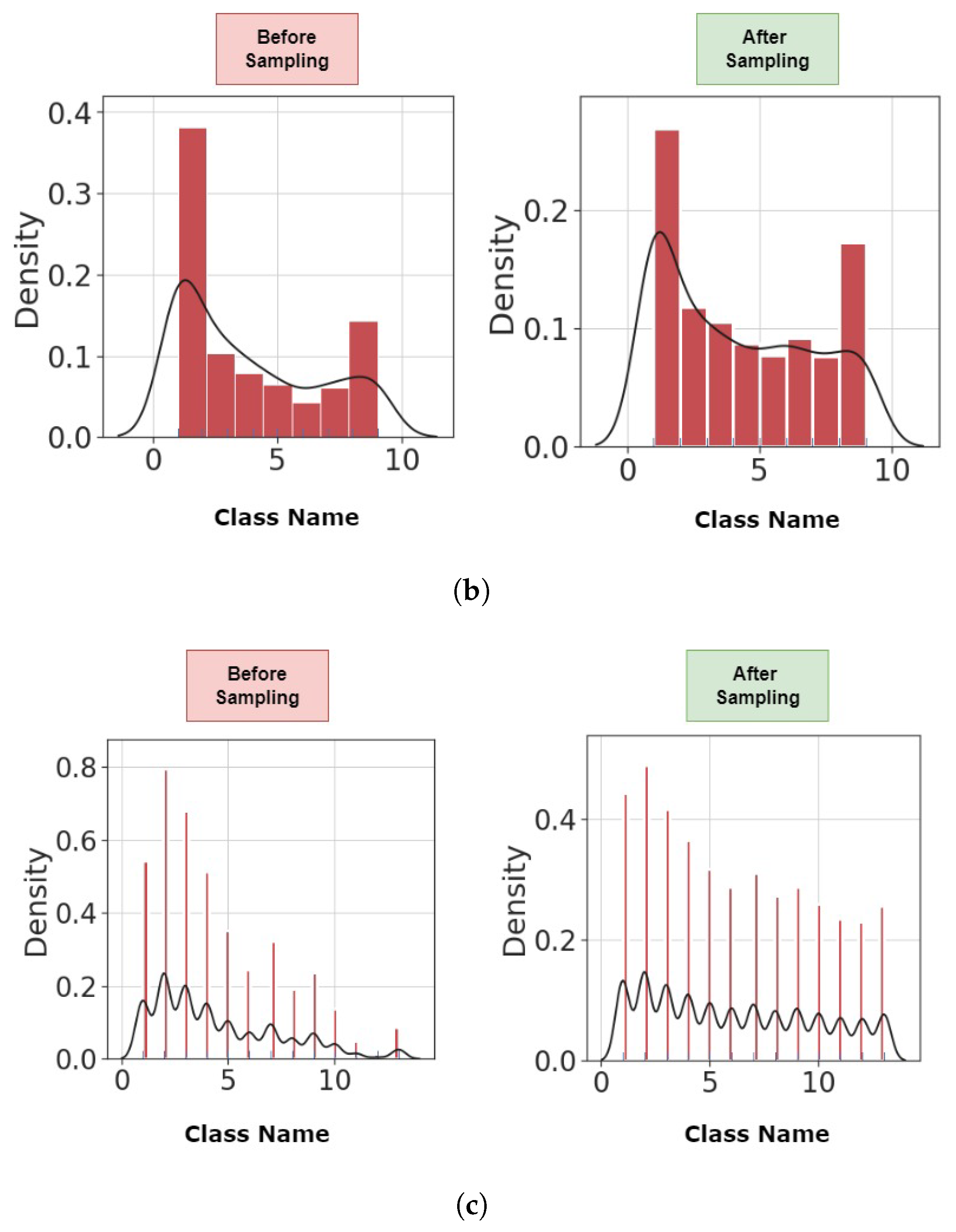
6.1. Preprocessing
6.2. Performance Analysis
| Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | F1-Measure (%) | Precision (%) |
|---|---|---|---|---|---|
| GAOCNN | 89.0 | 89.8 | 97.8 | 90.2 | 90.4 |
| VGG16 | 18.1 | 18.1 | 25.4 | 18.1 | 18.1 |
| ResNet | 17.7 | 17.7 | 20.8 | 17.7 | 17.7 |
| GoogLeNet | 28.6 | 2.3 | 35.6 | 4.5 | 67.9 |
| LR | 28.9 | 28.9 | 32.6 | 26.4 | 26.3 |
| RF | 79.9 | 79.9 | 92.7 | 79.7 | 79.6 |
| XGBoost | 78.8 | 78.8 | 92.6 | 78.3 | 77.9 |
| SVM | 36.5 | 33.5 | 42.3 | 32.1 | 31.9 |
| CNN + LR | 32.7 | 32.7 | 45.3 | 31.3 | 30.9 |
| CNN + RF | 80.0 | 80.0 | 93.4 | 79.7 | 79.6 |
| CNN + XGBoost | 78.8 | 78.8 | 94.4 | 78.3 | 77.9 |
| CNN + SVM | 36.2 | 36.2 | 43.3 | 34.8 | 34.5 |
| SGANs | 43.5 | 14.9 | 75.1 | 23.6 | 72.9 |
| Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | F1-Measure (%) | Precision (%) |
|---|---|---|---|---|---|
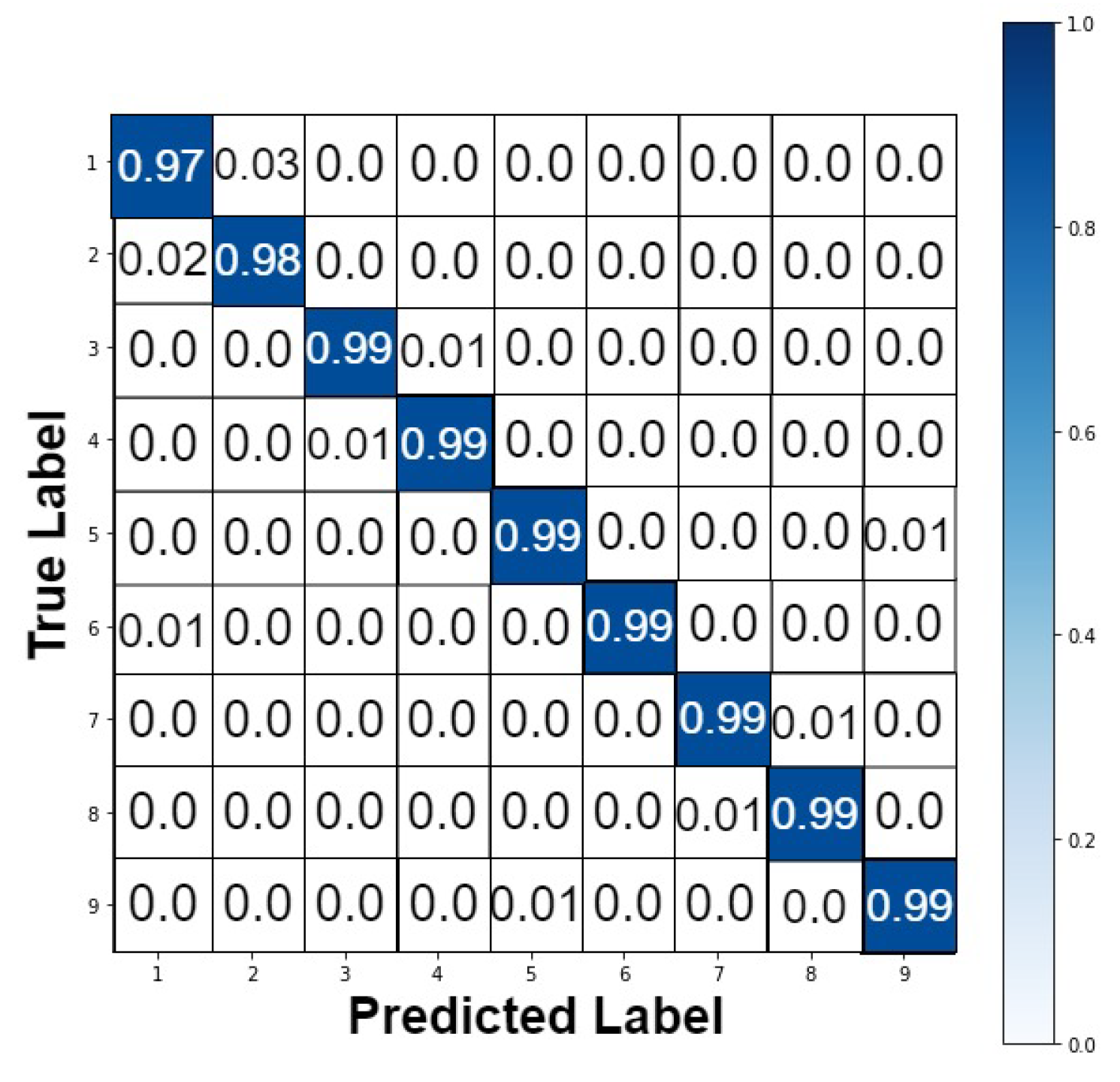
| GAOCNN | 99.4 | 99.4 | 99.8 | 99.4 | 99.4 |
| VGG16 | 14.1 | 14.6 | 20.5 | 14.6 | 14.6 |
| ResNet | 12.7 | 12.7 | 17.8 | 12.7 | 12.7 |
| LR | 92.1 | 92.1 | 98.8 | 92.1 | 92.3 |
| RF | 89.3 | 89.3 | 95.6 | 89.2 | 89.1 |
| XGBoost | 91.4 | 91.4 | 98.4 | 91.4 | 91.3 |
| SVM | 84.7 | 84.7 | 92.8 | 84.7 | 84.8 |
| CNN + LR | 70.3 | 70.3 | 89.9 | 70.2 | 70.6 |
| CNN + RF | 87.3 | 87.3 | 96.1 | 87.3 | 87.4 |
| CNN + XGBoost | 87.7 | 87.7 | 96.2 | 87.8 | 88.6 |
| CNN + SVM | 81.3 | 81.3 | 92.5 | 81.3 | 81.8 |
| SGANs | 93.5 | 93.3 | 98.8 | 93.6 | 93.9 |
| Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | F1-Measure (%) | Precision (%) |
|---|---|---|---|---|---|
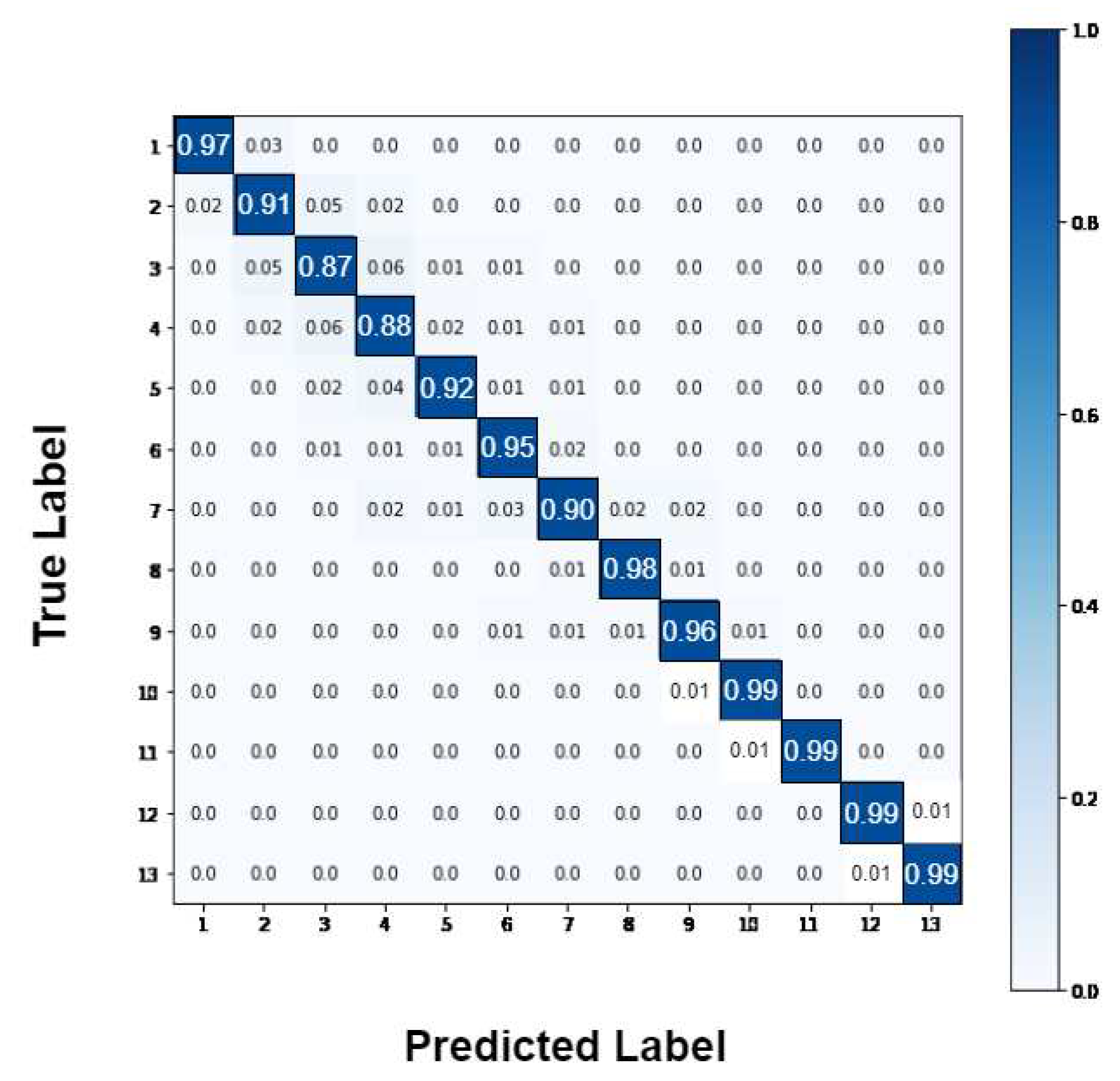
| GAOCNN | 94.1 | 94.0 | 98.8 | 94.2 | 94.5 |
| VGG16 | 10.1 | 10.1 | 20.6 | 10.1 | 10.1 |
| ResNet | 8.7 | 28.7 | 8.9 | 17.7 | 17.7 |
| GoogLeNet | 17.7 | 15.9 | 42.6 | 25.2 | 60.1 |
| LR | 43.9 | 43.9 | 65.1 | 38.4 | 36.2 |
| RF | 76.1 | 76.1 | 89.6 | 76.1 | 76.0 |
| XGBoost | 83.5 | 83.5 | 93.7 | 83.3 | 83.2 |
| SVM | 56.0 | 59.4 | 83.3 | 56.1 | 56.0 |
| CNN + LR | 43.6 | 43.6 | 72.7 | 42.4 | 41.8 |
| CNN + RF | 80.9 | 80.9 | 90.6 | 80.9 | 81.0 |
| CNN + XGBoost | 83.2 | 83.2 | 96.5 | 83.1 | 82.9 |
| CNN + SVM | 39.8 | 39.8 | 59.0 | 39.3 | 39.6 |
| SGANs | 56.1 | 45.7 | 92.6 | 54.5 | 67.7 |
| Model | Accuracy (%) | AUROC (%) |
|---|---|---|
| Tamin and Iswari ([50]) | 75.9 | - |
| Hammoudeh et al. ([18]) | 92 | 95 |
| Popel et al. ([45]) | 82.27 | - |
| Alturki et al. ([51]) | 94.8 | - |
| Goudjerkan and Jayabalan ([52]) | 95 | 95 |
| Seraphim et al. ([53]) | 86 | 66.7 |
| Norbrun ([54]) | 89.7 | 96 |
| GAOCNN | 97.2 | 99 |
| Model | Number of Classes | Accuracy (%) | AUROC (%) | Dataset |
|---|---|---|---|---|
| Gentimis et al. ([55]) | 2 | 79.8 | - | MIMIC-III |
| Steele and Thompson ([56]) | 2 | 87.7 | 88 | Diabetes |
| Alturki et al. ([51]) | 3 | 85.4 | - | Diabetes |
| Nallabasannagari et al. ([57]) | 2 | 66.2 | 88 | MIMIC-III |
| Wang et al. ([58]) | 2 | 68.3 | 73.3 | MIMIC-III |
| Wang et al. ([58]) | 2 | 91.2 | 71 | MIMIC-III |
| Etu et al. ([59]) | 2 | 85 | 93 | COVID-19 |
| Alabbad et al. ([60]) | 9 | 94.16 | - | COVID-19 |
| GAOCNN | 7 | 89 | 96 | Diabetes |
| GAOCNN | 13 | 94.1 | 99 | MIMIC-III |
| GAOCNN | 9 | 99.4 | 99 | COVID-19 |
7. DISCUSSION
8. CONCLUSIONS
References
- Desai, D.; Mehta, D.; Mathias, P.; Menon, G.; Schubart, U.K. Health care utilization and burden of diabetic ketoacidosis in the US over the past decade: a nationwide analysis. Diabetes care 2018, 41, 1631–1638. [Google Scholar]
- Friedberg, M.W.; Rosenthal, M.B.; Werner, R.M.; Volpp, K.G.; Schneider, E.C. Effects of a medical home and shared savings intervention on quality and utilization of care. JAMA internal medicine 2015, 175, 1362–1368. [Google Scholar]
- Mata-Cases, M.; Casajuana, M.; Franch-Nadal, J.; Casellas, A.; Castell, C.; Vinagre, I.; Mauricio, D.; Bolíbar, B. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia, Spain. The European Journal of Health Economics 2016, 17, 1001–1010. [Google Scholar]
- Huang, E.S.; Laiteerapong, N.; Liu, J.Y.; John, P.M.; Moffet, H.H.; Karter, A.J. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA internal medicine 2014, 174, 251–258. [Google Scholar]
- Riddle, M.C.; Herman, W.H. The cost of diabetes care—an elephant in the room. Diabetes Care 2018, 41, 929–932. [Google Scholar]
- Pasquini-Descomps, H.; Brender, N.; Maradan, D. Value for money in H1N1 influenza: a systematic review of the cost-effectiveness of pandemic interventions. Value in Health 2017, 20, 819–827. [Google Scholar]
- Tsai, Y.; Vogt, T.M.; Zhou, F. Patient characteristics and costs associated with COVID-19–related medical care among Medicare fee-for-service beneficiaries. Annals of Internal Medicine 2021. [Google Scholar]
- Gural, A. Algorithmic Techniques for Neural Network Training on Memory-Constrained Hardware; Stanford University, 2021.
- Faes, C.; Abrams, S.; Van Beckhoven, D.; Meyfroidt, G.; Vlieghe, E.; Hens, N.; et al. Time between symptom onset, hospitalisation and recovery or death: statistical analysis of Belgian COVID-19 patients. International journal of environmental research and public health 2020, 17, 7560. [Google Scholar]
- Muniyappa, R.; Gubbi, S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. American Journal of Physiology-Endocrinology and Metabolism 2020, 318, E736–E741. [Google Scholar]
- Tavakolian, A.; Hajati, F.; Rezaee, A.; Fasakhodi, A.O.; Uddin, S. Source code Optimized Parallel Inception: A fast COVID-19 screening software. Software Impacts 2022, p. 100337.
- Tavakolian, A.; Hajati, F.; Rezaee, A.; Fasakhodi, A.O.; Uddin, S. Fast COVID-19 versus H1N1 screening using Optimized Parallel Inception. Expert Systems with Applications 2022, p. 117551.
- Shinde, P.P.; Shah, S. A review of machine learning and deep learning applications. In Proceedings of the 2018 Fourth international conference on computing communication control and automation (ICCUBEA). IEEE; 2018; pp. 1–6. [Google Scholar]
- Desai, K.M.; Survase, S.A.; Saudagar, P.S.; Lele, S.; Singhal, R.S. Comparison of artificial neural network (ANN) and response surface methodology (RSM) in fermentation media optimization: case study of fermentative production of scleroglucan. Biochemical Engineering Journal 2008, 41, 266–273. [Google Scholar]
- Alloghani, M.; Aljaaf, A.; Hussain, A.; Baker, T.; Mustafina, J.; Al-Jumeily, D.; Khalaf, M. Implementation of machine learning algorithms to create diabetic patient re-admission profiles. BMC medical informatics and decision making 2019, 19, 1–16. [Google Scholar] [CrossRef]
- Mai, Q. A review of discriminant analysis in high dimensions. Wiley Interdisciplinary Reviews: Computational Statistics 2013, 5, 190–197. [Google Scholar] [CrossRef]
- Pranckevičius, T.; Marcinkevičius, V. Comparison of naive bayes, random forest, decision tree, support vector machines, and logistic regression classifiers for text reviews classification. Baltic Journal of Modern Computing 2017, 5, 221. [Google Scholar] [CrossRef]
- Hammoudeh, A.; Al-Naymat, G.; Ghannam, I.; Obied, N. Predicting hospital readmission among diabetics using deep learning. Procedia Computer Science 2018, 141, 484–489. [Google Scholar] [CrossRef]
- Mingle, D.; et al. Predicting diabetic readmission rates: moving beyond Hba1c. Current Trends in Biomedical Engineering & Biosciences 2017, 7, 555707. [Google Scholar]
- Voyant, C.; Notton, G.; Kalogirou, S.; Nivet, M.L.; Paoli, C.; Motte, F.; Fouilloy, A. Machine learning methods for solar radiation forecasting: A review. Renewable Energy 2017, 105, 569–582. [Google Scholar] [CrossRef]
- Chauhan, V.K.; Dahiya, K.; Sharma, A. Problem formulations and solvers in linear SVM: a review. Artificial Intelligence Review 2019, 52, 803–855. [Google Scholar] [CrossRef]
- Morton, A.; Marzban, E.; Giannoulis, G.; Patel, A.; Aparasu, R.; Kakadiaris, I.A. A comparison of supervised machine learning techniques for predicting short-term in-hospital length of stay among diabetic patients. In Proceedings of the 2014 13th International Conference on Machine Learning and Applications. IEEE; 2014; pp. 428–431. [Google Scholar]
- Yakovlev, A.; Metsker, O.; Kovalchuk, S.; Bologova, E. Prediction of in-hospital mortality and length of stay in acute coronary syndrome patients using machine-learning methods. Journal of the American College of Cardiology 2018, 71, A242–A242. [Google Scholar] [CrossRef]
- Tsai, P.F.J.; Chen, P.C.; Chen, Y.Y.; Song, H.Y.; Lin, H.M.; Lin, F.M.; Huang, Q.P. Length of hospital stay prediction at the admission stage for cardiology patients using artificial neural network. Journal of healthcare engineering 2016, 2016. [Google Scholar] [CrossRef]
- Schorr, E. Theoretical framework for determining hospital length of stay (LOS). In Proceedings of the BMC Proceedings. BioMed Central, 2012, Vol. 6, pp. 1–1.
- Mahboub, B.; Al Bataineh, M.T.; Alshraideh, H.; Hamoudi, R.; Salameh, L.; Shamayleh, A. Prediction of COVID-19 hospital length of stay and risk of death using artificial intelligence-based modeling. Frontiers in medicine 2021, 8. [Google Scholar] [CrossRef]
- Nemati, M.; Ansary, J.; Nemati, N. Machine-learning approaches in COVID-19 survival analysis and discharge-time likelihood prediction using clinical data. Patterns 2020, 1, 100074. [Google Scholar] [CrossRef]
- Ajit, A.; Acharya, K.; Samanta, A. A review of convolutional neural networks. In Proceedings of the 2020 International Conference on Emerging Trends in Information Technology and Engineering (ic-ETITE). IEEE; 2020; pp. 1–5. [Google Scholar]
- Strack, B.; DeShazo, J.P.; Gennings, C.; Olmo, J.L.; Ventura, S.; Cios, K.J.; Clore, J.N. Impact of HbA1c measurement on hospital readmission rates: analysis of 70,000 clinical database patient records. BioMed research international 2014, 2014. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care 2005, pp. 1130–1139.
- Xu, B.; Kraemer, M.U.; et al. Open access epidemiological data from the COVID-19 outbreak. 2020.
- Johnson, A.E.; Pollard, T.J.; Shen, L.; Li-Wei, H.L.; Feng, M.; Ghassemi, M.; Moody, B.; Szolovits, P.; Celi, L.A.; Mark, R.G. MIMIC-III, a freely accessible critical care database. Scientific data 2016, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Xue, B.; Zhang, M.; Yen, G.G.; Lv, J. Automatically designing CNN architectures using the genetic algorithm for image classification. IEEE transactions on cybernetics 2020, 50, 3840–3854. [Google Scholar] [CrossRef]
- Peng, Y.; Nagata, M.H. An empirical overview of nonlinearity and overfitting in machine learning using COVID-19 data. Chaos, Solitons & Fractals 2020, 139, 110055. [Google Scholar]
- Luo, G. A review of automatic selection methods for machine learning algorithms and hyper-parameter values. Network Modeling Analysis in Health Informatics and Bioinformatics 2016, 5, 1–16. [Google Scholar] [CrossRef]
- Isa, S.M.; Suwandi, R.; Andrean, Y.P. Optimizing the Hyperparameter of Feature Extraction and Machine Learning Classification Algorithms. Int. J. Adv. Comput. Sci. Appl 2019, 10, 69–76. [Google Scholar] [CrossRef]
- Kumar, A.; Kumar, D.; Jarial, S. A review on artificial bee colony algorithms and their applications to data clustering. Cybernetics and Information Technologies 2017, 17, 3–28. [Google Scholar] [CrossRef]
- García, S.; Luengo, J.; Herrera, F. Tutorial on practical tips of the most influential data preprocessing algorithms in data mining. Knowledge-Based Systems 2016, 98, 1–29. [Google Scholar] [CrossRef]
- Daghistani, T.A.; Elshawi, R.; Sakr, S.; Ahmed, A.M.; Al-Thwayee, A.; Al-Mallah, M.H. Predictors of in-hospital length of stay among cardiac patients: A machine learning approach. International journal of cardiology 2019, 288, 140–147. [Google Scholar] [CrossRef]
- Gowd, A.K.; Agarwalla, A.; Amin, N.H.; Romeo, A.A.; Nicholson, G.P.; Verma, N.N.; Liu, J.N. Construct validation of machine learning in the prediction of short-term postoperative complications following total shoulder arthroplasty. Journal of shoulder and elbow surgery 2019, 28, e410–e421. [Google Scholar] [CrossRef]
- Guo, A.; Lu, J.; Tan, H.; Kuang, Z.; Luo, Y.; Yang, T.; Xu, J.; Yu, J.; Wen, C.; Shen, A. Risk factors on admission associated with hospital length of stay in patients with COVID-19: a retrospective cohort study. Scientific Reports 2021, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.N.; Kumar, M.A.; et al. Enhanced fuzzy K-NN approach for handling missing values in medical data mining. Indian Journal of Science and Technology 2016, 9, 1–6. [Google Scholar]
- Rodríguez, P.; Bautista, M.A.; Gonzalez, J.; Escalera, S. Beyond one-hot encoding: Lower dimensional target embedding. Image and Vision Computing 2018, 75, 21–31. [Google Scholar] [CrossRef]
- Gikunda, P.K.; Jouandeau, N. State-of-the-art convolutional neural networks for smart farms: A review. In Proceedings of the Intelligent Computing-Proceedings of the Computing Conference. Springer; 2019; pp. 763–775. [Google Scholar]
- Popel, M.H.; Hasib, K.M.; Habib, S.A.; Shah, F.M. A hybrid under-sampling method (HUSBoost) to classify imbalanced data. In Proceedings of the 2018 21st International Conference of Computer and Information Technology (ICCIT). IEEE; 2018; pp. 1–7. [Google Scholar]
- Li, Y.; Xia, J.; Zhang, S.; Yan, J.; Ai, X.; Dai, K. An efficient intrusion detection system based on support vector machines and gradually feature removal method. Expert systems with applications 2012, 39, 424–430. [Google Scholar] [CrossRef]
- Yang, S.; Gu, L.; Li, X.; Jiang, T.; Ren, R. Crop classification method based on optimal feature selection and hybrid CNN-RF networks for multi-temporal remote sensing imagery. Remote Sensing 2020, 12, 3119. [Google Scholar] [CrossRef]
- Miao, X.; Wu, Y.; Wang, J.; Gao, Y.; Mao, X.; Yin, J. Generative semi-supervised learning for multivariate time series imputation. In Proceedings of the Proceedings of the AAAI Conference on Artificial Intelligence, 2021, Vol. 35, pp. 8983–8991.
- Balasch, A.; Beinhofer, M.; Zauner, G. The Relative Confusion Matrix, a Tool to Assess Classifiablility in Large Scale Picking Applications. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA). IEEE; 2020; pp. 8390–8396. [Google Scholar]
- Tamin, F.; Iswari, N.M.S. Implementation of C4. 5 algorithm to determine hospital readmission rate of diabetes patient. In Proceedings of the 2017 4th International Conference on New Media Studies (CONMEDIA). IEEE, 2017, pp. 15–18.
- Alturki, L.; Aloraini, K.; Aldughayshim, A.; Albahli, S. Predictors of Readmissions and Length of Stay for Diabetes Related Patients. In Proceedings of the 2019 IEEE/ACS 16th International Conference on Computer Systems and Applications (AICCSA). IEEE; 2019; pp. 1–8. [Google Scholar]
- Goudjerkan, T.; Jayabalan, M. Predicting 30-day hospital readmission for diabetes patients using multilayer perceptron. International Journal of Advanced Computer Science and Applications 2019, 10. [Google Scholar] [CrossRef]
- Seraphim, I.; Ravi, V.; Rajagopal, A. Prediction of Diabetes Readmission using Machine Learning 2020.
- Norbrun, G. Reduction of Hospital Readmissions in Patients with a Diagnosis of COPD: An Integrative Review 2021.
- Gentimis, T.; Ala’J, A.; Durante, A.; Cook, K.; Steele, R. Predicting hospital length of stay using neural networks on mimic iii data. In Proceedings of the 2017 IEEE 15th Intl Conf on Dependable, Autonomic and Secure Computing, 15th Intl Conf on Pervasive Intelligence and Computing, 3rd Intl Conf on Big Data Intelligence and Computing and Cyber Science and Technology Congress (DASC/PiCom/DataCom/CyberSciTech). IEEE; 2017; pp. 1194–1201. [Google Scholar]
- Steele, R.J.; Thompson, B. Data mining for generalizable pre-admission prediction of elective length of stay. In Proceedings of the 2019 IEEE 9th Annual Computing and Communication Workshop and Conference (CCWC). IEEE; 2019; pp. 0127–0133. [Google Scholar]
- Nallabasannagari, A.R.; Reddiboina, M.; Seltzer, R.; Zeffiro, T.; Sharma, A.; Bhandari, M. All Data Inclusive, Deep Learning Models to Predict Critical Events in the Medical Information Mart for Intensive Care III Database (MIMIC III). arXiv preprint. arXiv:2009.01366 2020.
- Wang, S.; McDermott, M.B.; Chauhan, G.; Ghassemi, M.; Hughes, M.C.; Naumann, T. Mimic-extract: A data extraction, preprocessing, and representation pipeline for mimic-iii. In Proceedings of the Proceedings of the ACM Conference on Health, Inference, and Learning, 2020; pp. 222–235.
- Etu, E.E.; Monplaisir, L.; Arslanturk, S.; Masoud, S.; Aguwa, C.; Markevych, I.; Miller, J. Prediction of Length of Stay in the Emergency Department for COVID-19 Patients: A Machine Learning Approach. IEEE Access 2022, 10, 42243–42251. [Google Scholar] [CrossRef]
- Alabbad, D.A.; Almuhaideb, A.M.; Alsunaidi, S.J.; Alqudaihi, K.S.; Alamoudi, F.A.; Alhobaishi, M.K.; Alaqeel, N.A.; Alshahrani, M.S. Machine learning model for predicting the length of stay in the intensive care unit for Covid-19 patients in the eastern province of Saudi Arabia. Informatics in Medicine Unlocked 2022, 30, 100937. [Google Scholar] [CrossRef]
- Déjean, S.; Ionescu, R.T.; Mothe, J.; Ullah, M.Z. Forward and backward feature selection for query performance prediction. In Proceedings of the Proceedings of the 35th annual ACM symposium on applied computing, 2020; pp. 690–697.

| Model | Accuracy (%) | Sensitivity (%) | Specificity (%) | F-Measure (%) | Precision (%) |
|---|---|---|---|---|---|
| GAOCNN | 97.2 | 96.7 | 99.3 | 96.9 | 97.1 |
| VGG16 | 38.0 | 38.2 | 37.8 | 45.6 | 38.2 |
| ResNet | 38.0 | 38.2 | 38 | 44.2 | 38.2 |
| GoogLeNet | 39.6 | 38.4 | 50.3 | 38.4 | 38.4 |
| LR | 86.8 | 86.8 | 93.4 | 86.8 | 86.8 |
| RF | 90.0 | 94.4 | 96.5 | 90.0 | 90.0 |
| XGBoost | 94.4 | 94.4 | 97.8 | 94.4 | 94.5 |
| SVM | 94.9 | 94.3 | 98.4 | 94.9 | 94.9 |
| CNN + LR | 87.5 | 86.5 | 94.2 | 87.5 | 87.4 |
| CNN + RF | 91.7 | 91.4 | 96.8 | 91.7 | 91.7 |
| CNN + XGBoost | 94.8 | 94.6 | 98.9 | 94.8 | 94.8 |
| CNN + SVM | 95.1 | 95.1 | 95.1 | 95.1 | 95.1 |
| SGANs | 58.9 | 51.7 | 52.6 | 56.9 | 63.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





