Submitted:
04 July 2023
Posted:
06 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
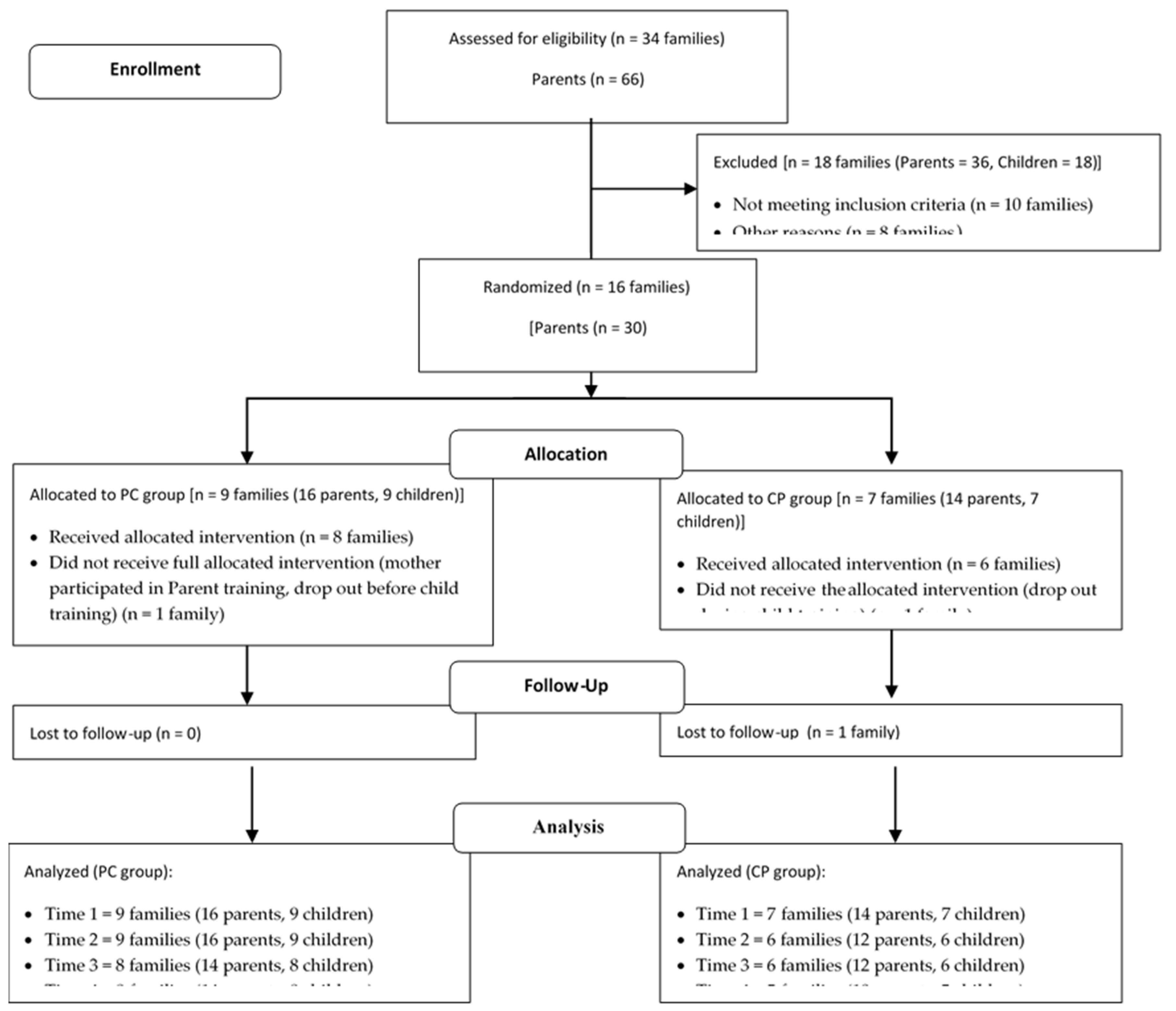
2.1. Trial Design
2.2. Eligibility Criteria for Participants
2.3. Participant Recruitment
2.4. Ethics
2.5. Intervention Procedure
2.5.1. Parent Psychoeducational Training Program
2.5.2. Child Training Program
2.5.3. Randomization
2.6. Measures and procedure
2.6.1. Primary Measures
2.6.2. Procedure
2.6.3. Feasibility and Acceptability Measures
2.7. Statistical Analysis
3. Results
3.1. Demographics
3.2. Main Analysis
3.3. Feasibility and Acceptability Outcomes
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Sessions | Content |
|---|---|
| Session 1 | Attention deficits and concurrent difficulties Neurobiological background |
| Session 2 | Parenting Stress Stress management strategies |
| Session 3 | Positive attention and Praise Effective instructions/commands |
| Session 4 | Contingency management system |
| Session 5 | Executive functions I Strategies for the enhancement of executive functions |
| Session 6 | Executive functions II Strategies for the enhancement of executive functions |
| Session 7 | Emotional control Self-monitoring and self-regulation Strategies for the enhancement of children’s emotional control and self-regulation |
| Session 8 | Wrap-up and review of the sessions and content covered through the parent training program |
References
- Amso, D.; Scerif, G. The Attentive Brain: Insights from Developmental Cognitive Neuroscience. Nat. Rev. Neurosci. 2015, 16, 606–619. [Google Scholar] [CrossRef] [PubMed]
- Tarver, J.; Daley, D.; Sayal, K. Attention-Deficit Hyperactivity Disorder (ADHD): An Updated Review of the Essential Facts. Child Care Health Dev. 2014, 40, 762–774. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Executive Functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Yang, H.-J.; Chen, V.C.; Lee, W.-T.; Teng, M.-J.; Lin, C.-H.; Gossop, M. Meta-Analysis of Quality of Life in Children and Adolescents with ADHD: By Both Parent Proxy-Report and Child Self-Report Using PedsQLTM. Res. Dev. Disabil. 2016, 51–52, 160–172. [Google Scholar] [CrossRef]
- Franke, B.; Michelini, G.; Asherson, P.; Banaschewski, T.; Bilbow, A.; Buitelaar, J.K.; Cormand, B.; Faraone, S.V.; Ginsberg, Y.; Haavik, J.; et al. Live Fast, Die Young? A Review on the Developmental Trajectories of ADHD across the Lifespan. Eur. Neuropsychopharmacol. 2018, 28, 1059–1088. [Google Scholar] [CrossRef]
- Ramos, A.A.; Hamdan, A.C.; Machado, L. A Meta-Analysis on Verbal Working Memory in Children and Adolescents with ADHD. Clin. Neuropsychol. 2020, 34, 873–898. [Google Scholar] [CrossRef]
- Pievsky, M.A.; McGrath, R.E. The Neurocognitive Profile of Attention-Deficit/Hyperactivity Disorder: A Review of Meta-Analyses. Arch. Clin. Neuropsychol. 2018, 33, 143–157. [Google Scholar] [CrossRef]
- Graziano, P.A.; Garcia, A. Attention-Deficit Hyperactivity Disorder and Children’s Emotion Dysregulation: A Meta-Analysis. Clin. Psychol. Rev. 2016, 46, 106–123. [Google Scholar] [CrossRef]
- Sjöwall, D.; Roth, L.; Lindqvist, S.; Thorell, L.B. Multiple Deficits in ADHD: Executive Dysfunction, Delay Aversion, Reaction Time Variability, and Emotional Deficits. J. Child Psychol. Psychiatry 2013, 54, 619–627. [Google Scholar] [CrossRef]
- Fleming, M.; Fitton, C.A.; Steiner, M.F.C.; McLay, J.S.; Clark, D.; King, A.; Mackay, D.F.; Pell, J.P. Educational and Health Outcomes of Children Treated for Attention-Deficit/Hyperactivity Disorder. JAMA Pediatr. 2017, 171, e170691. [Google Scholar] [CrossRef]
- Arnold, L.E.; Hodgkins, P.; Kahle, J.; Madhoo, M.; Kewley, G. Long-Term Outcomes of ADHD: Academic Achievement and Performance. J. Atten. Disord. 2020, 24, 73–85. [Google Scholar] [CrossRef]
- Ros, R.; Graziano, P.A. Social Functioning in Children With or At Risk for Attention Deficit/Hyperactivity Disorder: A Meta-Analytic Review. J. Clin. Child Adolesc. Psychol. 2018, 47, 213–235. [Google Scholar] [CrossRef]
- Mikami, A.Y.; Miller, M.; Lerner, M.D. Social Functioning in Youth with Attention-Deficit/Hyperactivity Disorder and Autism Spectrum Disorder: Transdiagnostic Commonalities and Differences. Clin. Psychol. Rev. 2019, 68, 54–70. [Google Scholar] [CrossRef] [PubMed]
- Azazy, S.; Nour Eldein, H.; Salama, H.; Ismail, M. Quality of Life and Family Function of Parents of Children with Attention Deficit Hyperactivity Disorder. East. Mediterr. Health J. 2018, 24, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Peasgood, T.; Bhardwaj, A.; Biggs, K.; Brazier, J.E.; Coghill, D.; Cooper, C.L.; Daley, D.; De Silva, C.; Harpin, V.; Hodgkins, P.; et al. The Impact of ADHD on the Health and Well-Being of ADHD Children and Their Siblings. Eur. Child Adolesc. Psychiatry 2016, 25, 1217–1231. [Google Scholar] [CrossRef] [PubMed]
- Craig, F.; Operto, F.F.; De Giacomo, A.; Margari, L.; Frolli, A.; Conson, M.; Ivagnes, S.; Monaco, M.; Margari, F. Parenting Stress among Parents of Children with Neurodevelopmental Disorders. Psychiatry Res. 2016, 242, 121–129. [Google Scholar] [CrossRef]
- Leitch, S.; Sciberras, E.; Post, B.; Gerner, B.; Rinehart, N.; Nicholson, J.M.; Evans, S. Experience of Stress in Parents of Children with ADHD: A Qualitative Study. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1690091. [Google Scholar] [CrossRef] [PubMed]
- Deater-Deckard, K. Parenting Stress and Child Adjustment: Some Old Hypotheses and New Questions. Clin. Psychol. Sci. Pract. 1998, 5, 314–332. [Google Scholar] [CrossRef]
- Abidin, R.R. Introduction to the Special Issue: The Stresses of Parenting. J. Clin. Child Psychol. 1990, 19, 298–301. [Google Scholar] [CrossRef]
- Abidin, R.R. The Determinants of Parenting Behavior. J. Clin. Child Psychol. 1992, 21, 407–412. [Google Scholar] [CrossRef]
- Bloomfield, L.; Kendall, S. Parenting Self-Efficacy, Parenting Stress and Child Behaviour before and after a Parenting Programme. Prim. Health Care Res. Dev. 2012, 13, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Albanese, A.M.; Russo, G.R.; Geller, P.A. The Role of Parental Self-efficacy in Parent and Child Well-being: A Systematic Review of Associated Outcomes. Child Care Health Dev. 2019, 45, 333–363. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, L.; Feder, M.; Abar, B.; Winsler, A. Relations between Parenting Stress, Parenting Style, and Child Executive Functioning for Children with ADHD or Autism. J. Child Fam. Stud. 2016, 25, 3644–3656. [Google Scholar] [CrossRef]
- Corcoran, J. Parents’ Experience of Raising a Child with Attention Deficit Disorder. ADHD Rep. 2017, 25, 6–10. [Google Scholar] [CrossRef]
- Theule, J.; Cheung, K.; Aberdeen, K. Children’s ADHD Interventions and Parenting Stress: A Meta-Analysis. J. Child Fam. Stud. 2018, 27, 2744–2756. [Google Scholar] [CrossRef]
- Modesto-Lowe, V.; Danforth, J.S.; Brooks, D. ADHD: Does Parenting Style Matter? Clin. Pediatr. (Phila.) 2008, 47, 865–872. [Google Scholar] [CrossRef]
- Theule, J.; Wiener, J.; Tannock, R.; Jenkins, J.M. Parenting Stress in Families of Children With ADHD: A Meta-Analysis. J. Emot. Behav. Disord. 2013, 21, 3–17. [Google Scholar] [CrossRef]
- Corcoran, J.; Schildt, B.; Hochbrueckner, R.; Abell, J. Parents of Children with Attention Deficit/Hyperactivity Disorder: A Meta-Synthesis, Part I. Child Adolesc. Soc. Work J. 2017, 34, 281–335. [Google Scholar] [CrossRef]
- Sanders, M.R.; Woolley, M.L. The Relationship between Maternal Self-Efficacy and Parenting Practices: Implications for Parent Training: Self-Efficacy and Parenting Practices. Child Care Health Dev. 2005, 31, 65–73. [Google Scholar] [CrossRef]
- Marino, R.L.D.F.; Teixeira, M.C.T.V.; Cantiere, C.N.; Ribeiro, A.D.F.; Micieli, A.P.R.; Carreiro, L.R.R. Parenting Styles and Mental Health in Parents of Children with ADHD. Rev. Interam. Psicol. J. Psychol. 2019, 53, 417–430. [Google Scholar] [CrossRef]
- Muñoz-Silva, A.; Lago-Urbano, R.; Sanchez-Garcia, M.; Carmona-Márquez, J. Child/Adolescent’s ADHD and Parenting Stress: The Mediating Role of Family Impact and Conduct Problems. Front. Psychol. 2017, 8, 2252. [Google Scholar] [CrossRef] [PubMed]
- Theule, J.; Wiener, J.; Rogers, M.A.; Marton, I. Predicting Parenting Stress in Families of Children with ADHD: Parent and Contextual Factors. J. Child Fam. Stud. 2011, 20, 640–647. [Google Scholar] [CrossRef]
- Perez Algorta, G.; Kragh, C.A.; Arnold, L.E.; Molina, B.S.G.; Hinshaw, S.P.; Swanson, J.M.; Hechtman, L.; Copley, L.M.; Lowe, M.; Jensen, P.S. Maternal ADHD Symptoms, Personality, and Parenting Stress: Differences Between Mothers of Children With ADHD and Mothers of Comparison Children. J. Atten. Disord. 2018, 22, 1266–1277. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Adamo, N.; Del Giovane, C.; Mohr-Jensen, C.; Hayes, A.J.; Carucci, S.; Atkinson, L.Z.; Tessari, L.; Banaschewski, T.; Coghill, D.; et al. Comparative Efficacy and Tolerability of Medications for Attention-Deficit Hyperactivity Disorder in Children, Adolescents, and Adults: A Systematic Review and Network Meta-Analysis. Lancet Psychiatry 2018, 5, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.W.; Owens, J.S.; Bunford, N. Evidence-Based Psychosocial Treatments for Children and Adolescents with Attention-Deficit/Hyperactivity Disorder. J. Clin. Child Adolesc. Psychol. 2014, 43, 527–551. [Google Scholar] [CrossRef] [PubMed]
- Pelham, W.E.; Fabiano, G.A.; Waxmonsky, J.G.; Greiner, A.R.; Gnagy, E.M.; Pelham, W.E.; Coxe, S.; Verley, J.; Bhatia, I.; Hart, K.; et al. Treatment Sequencing for Childhood ADHD: A Multiple-Randomization Study of Adaptive Medication and Behavioral Interventions. J. Clin. Child Adolesc. Psychol. 2016, 45, 396–415. [Google Scholar] [CrossRef]
- Pelham, W.E.; Altszuler, A.R. Combined Treatment for Children with Attention-Deficit/Hyperactivity Disorder: Brief History, the Multimodal Treatment for Attention-Deficit/Hyperactivity Disorder Study, and the Past 20 Years of Research. J. Dev. Behav. Pediatr. 2020, 41, S88–S98. [Google Scholar] [CrossRef]
- Storebø, O.J.; Ramstad, E.; Krogh, H.B.; Nilausen, T.D.; Skoog, M.; Holmskov, M.; Rosendal, S.; Groth, C.; Magnusson, F.L.; Moreira-Maia, C.R.; et al. Methylphenidate for Children and Adolescents with Attention Deficit Hyperactivity Disorder (ADHD). Cochrane Database Syst. Rev. 2015, 2016. [Google Scholar] [CrossRef]
- Van De Loo-Neus, G.H.H.; Rommelse, N.; Buitelaar, J.K. To Stop or Not to Stop? How Long Should Medication Treatment of Attention-Deficit Hyperactivity Disorder Be Extended? Eur. Neuropsychopharmacol. 2011, 21, 584–599. [Google Scholar] [CrossRef]
- Keilow, M.; Holm, A.; Fallesen, P. Medical Treatment of Attention Deficit/Hyperactivity Disorder (ADHD) and Children’s Academic Performance. PLOS ONE 2018, 13, e0207905. [Google Scholar] [CrossRef]
- Tsujii, N.; Okada, T.; Usami, M.; Kuwabara, H.; Fujita, J.; Negoro, H.; Kawamura, M.; Iida, J.; Saito, T. Effect of Continuing and Discontinuing Medications on Quality of Life After Symptomatic Remission in Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-Analysis. J. Clin. Psychiatry 2020, 81. [Google Scholar] [CrossRef] [PubMed]
- Ferrin, M.; Perez-Ayala, V.; El-Abd, S.; Lax-Pericall, T.; Jacobs, B.; Bilbow, A.; Taylor, E. A Randomized Controlled Trial Evaluating the Efficacy of a Psychoeducation Program for Families of Children and Adolescents With ADHD in the United Kingdom: Results After a 6-Month Follow-Up. J. Atten. Disord. 2020, 24, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Ferrin, M.; Moreno-Granados, J.M.; Salcedo-Marin, M.D.; Ruiz-Veguilla, M.; Perez-Ayala, V.; Taylor, E. Evaluation of a Psychoeducation Programme for Parents of Children and Adolescents with ADHD: Immediate and Long-Term Effects Using a Blind Randomized Controlled Trial. Eur. Child Adolesc. Psychiatry 2014, 23, 637–647. [Google Scholar] [CrossRef]
- Barkley, R.A. Defiant Children: A Clinician’s Manual for Assessment and Parent Training, 3rd Ed; 3rd ed.; Guilford Press: New York, NY, US, 2013; pp. xii, 228; ISBN 978-1-4625-0950-8. [Google Scholar]
- Kazdin, A.E. Parent Management Training: Treatment for Oppositional, Aggressive, and Antisocial Behavior in Children and Adolescents; Parent management training: Treatment for oppositional, aggressive, and antisocial behavior in children and adolescents; Oxford University Press: New York, NY, US, 2005; pp. ix, 410; ISBN 978-0-19-515429-0. [Google Scholar]
- Dekkers, T.J.; Hornstra, R.; Van Der Oord, S.; Luman, M.; Hoekstra, P.J.; Groenman, A.P.; Van Den Hoofdakker, B.J. Meta-Analysis: Which Components of Parent Training Work for Children With Attention-Deficit/Hyperactivity Disorder? J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 478–494. [Google Scholar] [CrossRef]
- Gümüs, F.; Ergün, G.; Dikeç, G. Effect of Psychoeducation on Stress in Parents of Children With Attention-Deficit/Hyperactivity Disorder: A Randomized Controlled Study. J. Psychosoc. Nurs. Ment. Health Serv. 2020, 58, 34–41. [Google Scholar] [CrossRef]
- Chen, V.C.-H.; Yeh, C.-J.; Lee, T.-C.; Chou, J.-Y.; Shao, W.-C.; Shih, D.-H.; Chen, C.-I.; Lee, P.-C. Symptoms of Attention Deficit Hyperactivity Disorder and Quality of Life of Mothers of School-Aged Children: The Roles of Child, Mother, and Family Variables. Kaohsiung J. Med. Sci. 2014, 30, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Coates, J.; Taylor, J.A.; Sayal, K. Parenting Interventions for ADHD: A Systematic Literature Review and Meta-Analysis. J. Atten. Disord. 2015, 19, 831–843. [Google Scholar] [CrossRef]
- Yao, A.; Shimada, K.; Kasaba, R.; Tomoda, A. Beneficial Effects of Behavioral Parent Training on Inhibitory Control in Children With Attention-Deficit/Hyperactivity Disorder: A Small-Scale Randomized Controlled Trial. Front. Psychiatry 2022, 13, 859249. [Google Scholar] [CrossRef]
- Loren, R.E.A.; Vaughn, A.J.; Langberg, J.M.; Cyran, J.E.M.; Proano-Raps, T.; Smolyansky, B.H.; Tamm, L.; Epstein, J.N. Effects of an 8-Session Behavioral Parent Training Group for Parents of Children With ADHD on Child Impairment and Parenting Confidence. J. Atten. Disord. 2015, 19, 158–166. [Google Scholar] [CrossRef]
- Daley, D.; Van Der Oord, S.; Ferrin, M.; Danckaerts, M.; Doepfner, M.; Cortese, S.; Sonuga-Barke, E.J.S. Behavioral Interventions in Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis of Randomized Controlled Trials Across Multiple Outcome Domains. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 835–847. [Google Scholar] [CrossRef]
- Lee, P.; Niew, W.; Yang, H.; Chen, V.C.; Lin, K. A Meta-Analysis of Behavioral Parent Training for Children with Attention Deficit Hyperactivity Disorder. Res. Dev. Disabil. 2012, 33, 2040–2049. [Google Scholar] [CrossRef] [PubMed]
- Heath, C.L.; Curtis, D.F.; Fan, W.; McPherson, R. The Association Between Parenting Stress, Parenting Self-Efficacy, and the Clinical Significance of Child ADHD Symptom Change Following Behavior Therapy. Child Psychiatry Hum. Dev. 2015, 46, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Larsen, L.B.; Daley, D.; Lange, A.-M.; Sonuga-Barke, E.; Thomsen, P.H.; Rask, C.U. Effect of Parent Training on Health-Related Quality of Life in Preschool Children With Attention-Deficit/Hyperactivity Disorder: A Secondary Analysis of Data From a Randomized Controlled Trial. J. Am. Acad. Child Adolesc. Psychiatry 2021, 60, 734–744.e3. [Google Scholar] [CrossRef] [PubMed]
- Dimitropoulou, P.; Pachiti, I. Determinants of Treatment Response to State-of-the-Art Interventions for Attention Deficits: Child Temperament, Cognitive Profiles and Family Dynamics; clinicaltrials.gov. 2022. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children | Fifth Edition; Pearson: Bloomington, MN, US, 2014. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children-Fifth Edition. Technical and Interpretive Manual Supplement: Special Group Validity Studies with Other Measures and Additional Tables; Pearson: Bloomington, MN, US, 2014. [Google Scholar]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated Guidelines for Reporting Parallel Group Randomised Trials. J. Clin. Epidemiol. 2010, 63, e1–e37. [Google Scholar] [CrossRef] [PubMed]
- Cortese, S.; Ferrin, M.; Brandeis, D.; Buitelaar, J.; Daley, D.; Dittmann, R.W.; Holtmann, M.; Santosh, P.; Stevenson, J.; Stringaris, A.; et al. Cognitive Training for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes From Randomized Controlled Trials. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Kirby, J.R.; Kim, H.-J.; Silvestri, R. Cognitive Constructs and Individual Differences Underlying ADHD and Dyslexia: A Cognitive Mosaic Approach. In Cognition, Intelligence, and Achievement: A tribute to J. P. Das; Papadopoulos, T.C., Parilla, R.K., Kirby, J.R., Eds.; Elsevier Academic Press, 2015; pp. 197–223 ISBN 978-0-12-410388-7.
- Rapport, M.D.; Orban, S.A.; Kofler, M.J.; Friedman, L.M.; Bolden, J. Executive Function Training for Children with ADHD. In Attention-Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment; Barkley, R.A., Ed.; Guilford Press: New York, NY, US, 2015; pp. 1131–1171. [Google Scholar]
- Jolles, D.D.; Crone, E.A. Training the Developing Brain: A Neurocognitive Perspective. Front. Hum. Neurosci. 2012, 6. [Google Scholar] [CrossRef]
- DuPaul, G.J.; Power, T.J.; Anastopoulos, A.D.; Reid, R. ADHD Rating Scale—IV: Checklists, Norms, and Clinical Interpretation; The Guilford Press: New York, NY, US, 1998; ISBN 978-1-57230-423-9. [Google Scholar]
- Kalantzi-Azizi, A.; Ageli, K.; Efstathiou, G. Greek ADHD Rating Scale–IV; Hellenic Grammata: Athens, Greece, 2005. [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR; American Psychiatric Association, Ed.; 4th ed., text revision; American Psychiatric Association: Washington, DC, 2000; ISBN 978-0-89042-024-9.
- Abidin, R.R. Parenting Stress Index: Manual, Administration Booklet, [and] Research Update; Pediatric Psychology Press: Charlottesville, VA, US, 1983. [Google Scholar]
- Abidin, R.R. Parenting Stress Index, Third Edition: Professional Manual; Psychological Assessment Resources, Inc: Odessa, FL, US, 1995. [Google Scholar]
- Leze, E. Clinical genetic evaluation and developmental examination of children born with preimplantation genetic diagnosis: evaluation of parental stress. Ph.D. thesis, National and Kapodistrian University of Athens (NKUA): Athens, Greece, 2013.
- Gibaud-Wallston, J.; Wandersman, L.P. Development and Utility of the Parenting Sense of Competence Scale 1978.
- Johnston, C.; Mash, E.J. A Measure of Parenting Satisfaction and Efficacy. J. Clin. Child Psychol. 1989, 18, 167–175. [Google Scholar] [CrossRef]
- Brislin, R.W. Back-Translation for Cross-Cultural Research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Brislin, R.W. The Wording and Translation of Research Instruments. In Field methods in cross-cultural research; Sage Publications, Inc: Thousand Oaks, CA, US, 1986; pp. 137–164. ISBN 978-0-8039-2549-6. [Google Scholar]
- Ozolins, U.; Hale, S.; Cheng, X.; Hyatt, A.; Schofield, P. Translation and Back-Translation Methodology in Health Research – a Critique. Expert Rev. Pharmacoecon. Outcomes Res. 2020, 20, 69–77. [Google Scholar] [CrossRef]
- Robinson, C.C.; Mandleco, B.; Olsen, S.F.; Hart, C.H. The Parenting Styles and Dimensions Questionnaire (PSDQ). In Handbook of family measurement techniques (Vol. 3). Instruments and index; Perlmutter, B.F., Touliatos, J., Holden, G.W., Eds.; Sage: Thousand Oaks, CA, 2001; Vol. 3, pp. 319–321. [Google Scholar]
- Baumrind, D. Child Care Practices Anteceding Three Patterns of Preschool Behavior. Genet. Psychol. Monogr. 1967, 75, 43–88. [Google Scholar]
- Maridaki-Kassotaki, A. Greek father’s parental typology according to child rearing practice: Adaptation and standardization of the “Parenting Styles and Dimensions Questionnaire (PSDQ). ” Epistimes Agogis 2009, 4, 23–33. [Google Scholar]
- Antonopoulou, K.; Tsitsas, G. Investigation of the Greek mother’s typology: Standardization of the Parenting Styles and Dimensions Questionnaire (PSDQ). Epistimes Agogis 2011, 2, 51–60. [Google Scholar]
- Brestan, E.V.; Jacobs, J.R.; Rayfield, A.D.; Eyberg, S.M. A Consumer Satisfaction Measure for Parent–Child Treatments and Its Relation to Measures of Child Behavior Change. Behav. Ther. 1999, 30, 17–30. [Google Scholar] [CrossRef]
- Eyberg, S. Consumer Satisfaction Measures for Assessing Parent Training Programs. In Innovations in clinical practice: A source book, Vol. 12; VandeCreek, L., Knapp, S., Jackson, T.L., Eds.; Professional Resource Press/Professional Resource Exchange: Sarasota, FL, US, 1993; pp. 377–382. ISBN 978-0-943158-98-3. [Google Scholar]
- Kazdin, A.E. Acceptability of Alternative Treatments for Deviant Child Behavior. J. Appl. Behav. Anal. 1980, 13, 259–273. [Google Scholar] [CrossRef]
- Webster-Stratton, C. The Incredible Years: Parents, Teachers, and Children Training Series. Resid. Treat. Child. Youth 2001, 18, 31–45. [Google Scholar] [CrossRef]
- Diggle, P.; Heagerty, P.; Liang, K.-Y.; Zeger, S.L. (Eds.) In Analysis of Longitudinal Data, 2nd. ed; OUP Oxford, 2002; ISBN 978-0-19-852484-7.
- IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp.
- R Core Team (2020). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria.
- Akaike, H. Information Theory and an Extension of Maximum Likelihood Principle. Proc. 2nd Int. Symp. Inf. Theory 1973, 267–281. [Google Scholar]
- Akaike, H. A New Look at the Statistical Model Identification. In Selected Papers of Hirotugu Akaike; Parzen, E., Tanabe, K., Kitagawa, G., Eds.; Springer Series in Statistics; Springer: New York, NY, 1998; pp. 215–222; ISBN 978-1-4612-1694-0. [Google Scholar]
- Stone, M. Comments on Model Selection Criteria of Akaike and Schwarz. J. R. Stat. Soc. Ser. B Methodol. 1979, 41, 276–278. [Google Scholar] [CrossRef]
- Haack, L.M.; Villodas, M.T.; McBurnett, K.; Hinshaw, S.; Pfiffner, L.J. Parenting Mediates Symptoms and Impairment in Children With ADHD-Inattentive Type. J. Clin. Child Adolesc. Psychol. 2016, 45, 155–166. [Google Scholar] [CrossRef]
- Mofokeng, M.; Van Der Wath, A.E. Challenges Experienced by Parents Living with a Child with Attention Deficit Hyperactivity Disorder. J. Child Adolesc. Ment. Health 2017, 29, 137–145. [Google Scholar] [CrossRef]
- Dey, M.; Paz Castro, R.; Haug, S.; Schaub, M.P. Quality of Life of Parents of Mentally-Ill Children: A Systematic Review and Meta-Analysis. Epidemiol. Psychiatr. Sci. 2019, 28, 563–577. [Google Scholar] [CrossRef]
- Wiener, J.; Biondic, D.; Grimbos, T.; Herbert, M. Parenting Stress of Parents of Adolescents with Attention-Deficit Hyperactivity Disorder. J. Abnorm. Child Psychol. 2016, 44, 561–574. [Google Scholar] [CrossRef] [PubMed]
- Sollie, H.; Mørch, W.-T.; Larsson, B. Parent and Family Characteristics and Their Associates in a Follow-Up of Outpatient Children with ADHD. J. Child Fam. Stud. 2016, 25, 2571–2584. [Google Scholar] [CrossRef]
- Primack, B.A.; Hendricks, K.M.; Longacre, M.R.; Adachi-Mejia, A.M.; Weiss, J.E.; Titus, L.J.; Beach, M.L.; Dalton, M.A. Parental Efficacy and Child Behavior in a Community Sample of Children with and without Attention-Deficit Hyperactivity Disorder (ADHD). ADHD Atten. Deficit Hyperact. Disord. 2012, 4, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Cussen, A.; Sciberras, E.; Ukoumunne, O.C.; Efron, D. Relationship between Symptoms of Attention-Deficit/Hyperactivity Disorder and Family Functioning: A Community-Based Study. Eur. J. Pediatr. 2012, 171, 271–280. [Google Scholar] [CrossRef]
- Gau, S.S.-F.; Chang, J.P.-C. Maternal Parenting Styles and Mother–Child Relationship among Adolescents with and without Persistent Attention-Deficit/Hyperactivity Disorder. Res. Dev. Disabil. 2013, 34, 1581–1594. [Google Scholar] [CrossRef] [PubMed]
- Kopala-Sibley, D.C.; Jelinek, C.; Kessel, E.M.; Frost, A.; Allmann, A.E.S.; Klein, D.N. Parental Depressive History, Parenting Styles, and Child Psychopathology over 6 Years: The Contribution of Each Parent’s Depressive History to the Other’s Parenting Styles. Dev. Psychopathol. 2017, 29, 1469–1482. [Google Scholar] [CrossRef]
- Allmann, A.E.S.; Klein, D.N.; Kopala-Sibley, D.C. Bidirectional and Transactional Relationships between Parenting Styles and Child Symptoms of ADHD, ODD, Depression, and Anxiety over 6 Years. Dev. Psychopathol. 2022, 34, 1400–1411. [Google Scholar] [CrossRef]
- Daley, D.; Van Der Oord, S.; Ferrin, M.; Danckaerts, M.; Doepfner, M.; Cortese, S.; Sonuga-Barke, E.J.S. Behavioral Interventions in Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis of Randomized Controlled Trials Across Multiple Outcome Domains. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 835–847. [Google Scholar] [CrossRef]
- Si, Y.; Ma, J.L.C.; Zhang, J. Factors Influencing Parenting Stress among Chinese Families of Children with Attention-Deficit/Hyperactivity Disorder. Child. Youth Serv. Rev. 2020, 116, 105148. [Google Scholar] [CrossRef]
- Crnic, K.; Ross, E. Parenting Stress and Parental Efficacy. In Parental Stress and Early Child Development; Deater-Deckard, K., Panneton, R., Eds.; Springer International Publishing: Cham, 2017; pp. 263–284; ISBN 978-3-319-55374-0. [Google Scholar]
- Ciesielski, H.A.; Loren, R.E.A.; Tamm, L. Behavioral Parent Training for ADHD Reduces Situational Severity of Child Noncompliance and Related Parental Stress. J. Atten. Disord. 2020, 24, 758–767. [Google Scholar] [CrossRef]
- Rimestad, M.L.; Lambek, R.; Zacher Christiansen, H.; Hougaard, E. Short- and Long-Term Effects of Parent Training for Preschool Children With or at Risk of ADHD: A Systematic Review and Meta-Analysis. J. Atten. Disord. 2019, 23, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.; Johnston, C. Maternal ADHD Symptoms and Parenting Stress: The Roles of Parenting Self-Efficacy Beliefs and Neuroticism. J. Atten. Disord. 2019, 23, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Johnston, C. The Relationship Between ADHD Symptoms and Competence as Reported by Both Self and Others. J. Atten. Disord. 2012, 16, 418–426. [Google Scholar] [CrossRef] [PubMed]
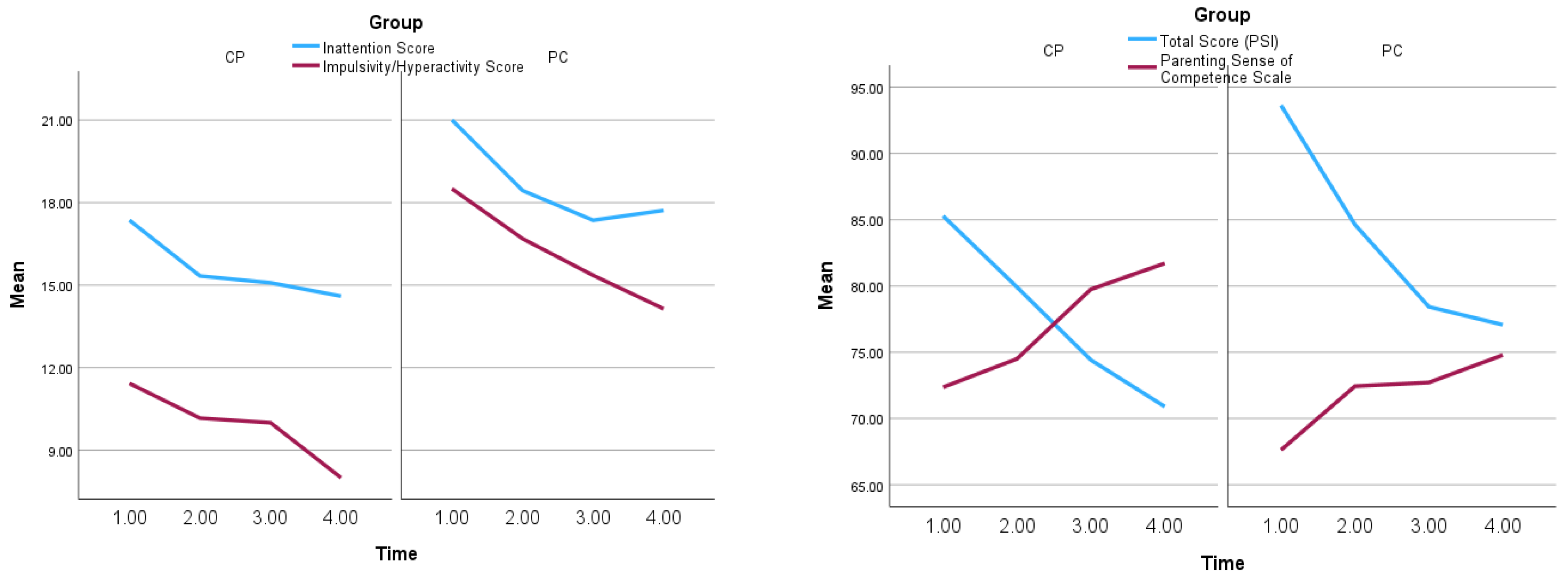
| Group | Scale | Subscale | Time 1 (n=30) | Time 2 (n=28) | Time 3 (n=26) | Time 4 (n=24) |
|---|---|---|---|---|---|---|
| PC | Parenting Styles and Dimensions Questionnaire | Democratic | 4.03 (0.74) | 4.16 (0.47) | 4.16 (0.57) | 4.15 (0.57) |
| Authoritarian* | 1.98 (0.51) | 1.94 (0.52) | 1.88 (0.61) | 1.67 (0.49) | ||
| Permissive** | 3.11 (0.65) | 3.09 (0.55) | 3.03 (0.54) | 2.66 (0.65) | ||
| Strict | 3.84 (0.52) | 3.88 (0.48) | 3.73 (0.5) | 3.71 (0.59) | ||
| Parenting Stress Index-Short Form (PSI-SF) | Parental Distress | 29.25 (8.19) | 26.25 (9.07) | 25.07 (9.41) | 25.93 (10.21) | |
| Parent-Child Dysfunctional Interaction** |
29.25 (8.64) | 25.88 (7.35) | 25.29 (7.28) | 23.14 (7.39) | ||
| Difficult Child*** | 35.13 (8.38) | 32.5 (7.85) | 28.07 (7.64) | 28 (7.54) | ||
| Total Score* | 93.63 (22.7) | 84.63 (20.61) | 78.43 (21.69) | 77.07 (22.43) | ||
| Parenting Sense of Competence (PSOC) | Total Score* | 67.63 (8.16) | 72.44 (9.42) | 72.71 (9.43) | 74.79 (11.41) | |
| ADHD Rating Scale-IV | Inattention* | 21 (3.37) | 18.44 (4.27) | 17.36 (4.27) | 17.71 (4.81) | |
| Impulsivity/ Hyperactivity* |
18.5 (5.09) | 16.69 (6.02) | 15.36 (4.77) | 14.14 (5.78) | ||
| CP | Parenting Styles and Dimensions Questionnaire | Democratic* | 4.18 (0.51) | 4.15 (0.44) | 4.38 (0.51) | 4.3 (0.55) |
| Authoritarian | 1.64 (0.62) | 1.67 (0.48) | 1.4 (0.35) | 1.47 (0.43) | ||
| Permissive** | 3.14 (0.49) | 3.18 (0.4) | 2.83 (0.61) | 2.78 (0.69) | ||
| Strict | 3.55 (0.5) | 3.5 (0.55) | 3.19 (0.54) | 3.45 (0.71) | ||
| Parenting Stress Index-Short Form (PSI-SF) | Parental Distress | 27.5 (6.6) | 27.58 (6.43) | 27.25 (6.45) | 25.4 (7.52) | |
| Parent-Child Dysfunctional Interaction** |
25.36 (6.83) | 23 (4.67) | 20.83 (5.8) | 21.6 (5.72) | ||
| Difficult Child*** | 32.43 (5.5) | 29.33 (8.04) | 26.33 (6.44) | 23.9 (5.69) | ||
| Total Score** | 85.29 (16.69) | 79.92 (10.77) | 74.42 (13.94) | 70.9 (13.63) | ||
| Parenting Sense of Competence (PSOC) | Total Score*** | 72.36 (9.08) | 74.5 (8.6) | 79.75 (7.48) | 81.7 (7.57) | |
| ADHD Rating Scale-IV | Inattention | 17.36 (4.96) | 15.33 (5.47) | 15.08 (4.32) | 14.6 (6.38) | |
| Impulsivity/ Hyperactivity |
11.43 (4.11) | 10.17 (4.57) | 10 (3.88) | 8 (4.16) |
| Dependent Variable | ||||
|---|---|---|---|---|
| Parameters | Parenting Stress |
Parenting Sense of Competence | Inattention | Impulsivity/ Hyperactivity |
| Intercept | 91.54 | 70.01 | 18.42 | 13.05 |
| Group (PC:1, CP:0) |
5.56 | -5.94* | 2.84 | 6.60*** |
| Time (1-4) |
-5.31*** | 3.10*** | -1.11*** | -1.47*** |
| Correlation Structure | Autoregressive, AR (1) | Autoregressive, AR (1) | Compound symmetry |
Compound symmetry |
| Evaluation of Parent Training_Final Questionnaire | ||||
|---|---|---|---|---|
| Sessions attended | Satisfaction Score | Program’s Usefulness Score | Trainers’ Assessment Score | |
| Mean (std) | 6.20 (0.77) | 40.60 (2.35) | 63.80 (4.24) | 39.33 (2.05) |
| Satisfaction Score | 0.439 | |||
| Program’s Usefulness Score | 0.035 | .735** | ||
| Trainers’ Assessment Score | 0.045 | .560* | .646** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





