1. Introduction
Total hip arthroplasty (THA) is considered one of the most successful orthopedic procedures performed on patients with osteoarthritis (OA) [
1]. Fujita et al. [
2] report that improved postoperative activities of daily living (ADLs) and sports are important to improve satisfaction after THA. The ability to successfully perform common ADLs is important for safe mobility, social participation, and ultimately the quality of life.
In modern society, car usage is one of the most important ADLs. Shiomoto et al. [
3] report that getting into and out of a car is significantly correlated with the perception of a natural joint after THA. Previous studies on car use after THA have focused on patients' return to driving [
4,
5,
6]. To our knowledge, there are no studies that have investigated the characteristics of car use across THA patients, including those who do not drive.
Therefore, we performed a retrospective study, in patients with OA who underwent THA to assess: (1) how many of them use a car and the delay to using one post-surgery, (2) how comfortable they were while getting into and out of a car and (3) what factors affected their comfort in getting into and out of a car after THA.
2. Materials and Methods
After approval from the Institutional Review Board (IRB number: 21142-00), we retrospectively reviewed the clinical course of 517 patients who underwent THA for OA between January 2012 and December 2016. All THAs were performed using a posterolateral approach, with a uniform protocol for postoperative rehabilitation [
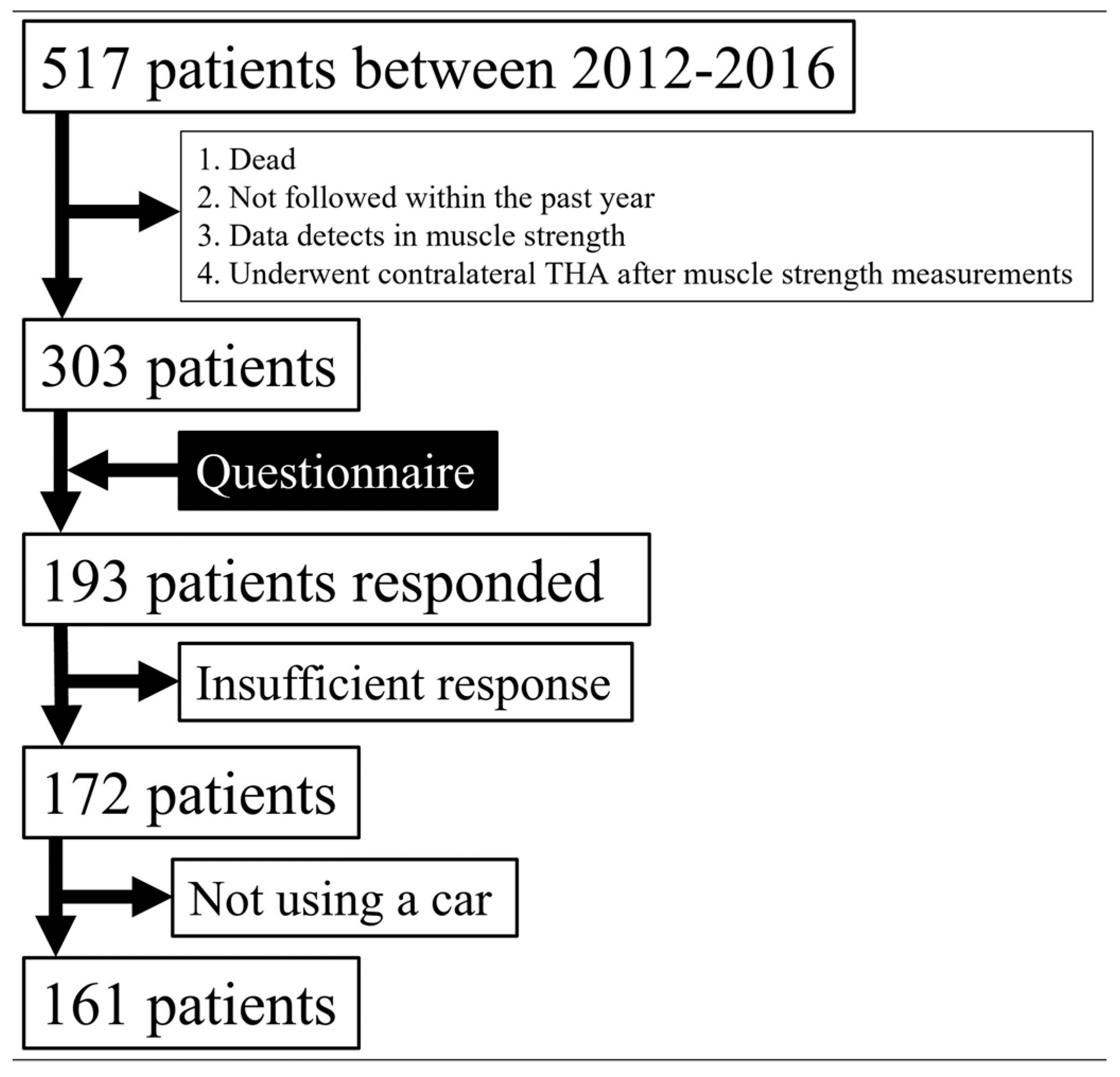
7]. Among them, 303 patients satisfied the following inclusion criteria: (1) at least one year elapsed since surgery, (2) evaluation by a surgeon within the past year, (3) no defects in muscle strength data, and (4) no contralateral THA after muscle strength measurements. A total of 303 THA patients received the study questionnaire in the mail, of which 193 (63.7%) returned the questionnaire with written informed consent. Of the respondents, 172 (56.1%) provided satisfactory responses and comprised the final study cohort (
Figure 1). All demographic and clinicopathological information was obtained from the patients' medical records. Data were handled following the ethical standards of the Declaration of Helsinki.
All participants were sent a 9-item questionnaire to collect the following information in 2020 (
Table 1): (1) whether the patient used a car, (2) whether the patient drove, (3) the timing of returning to car usage, (4) comfort level while getting into and out of a car, (5) the reasons for feeling uncomfortable when getting into and out of a car, and (6) the door side on which getting into and out of a car was uncomfortable, (7) which side was more uncomfortable, (8) satisfaction with pain level
8, and (9) satisfaction with function [
8].
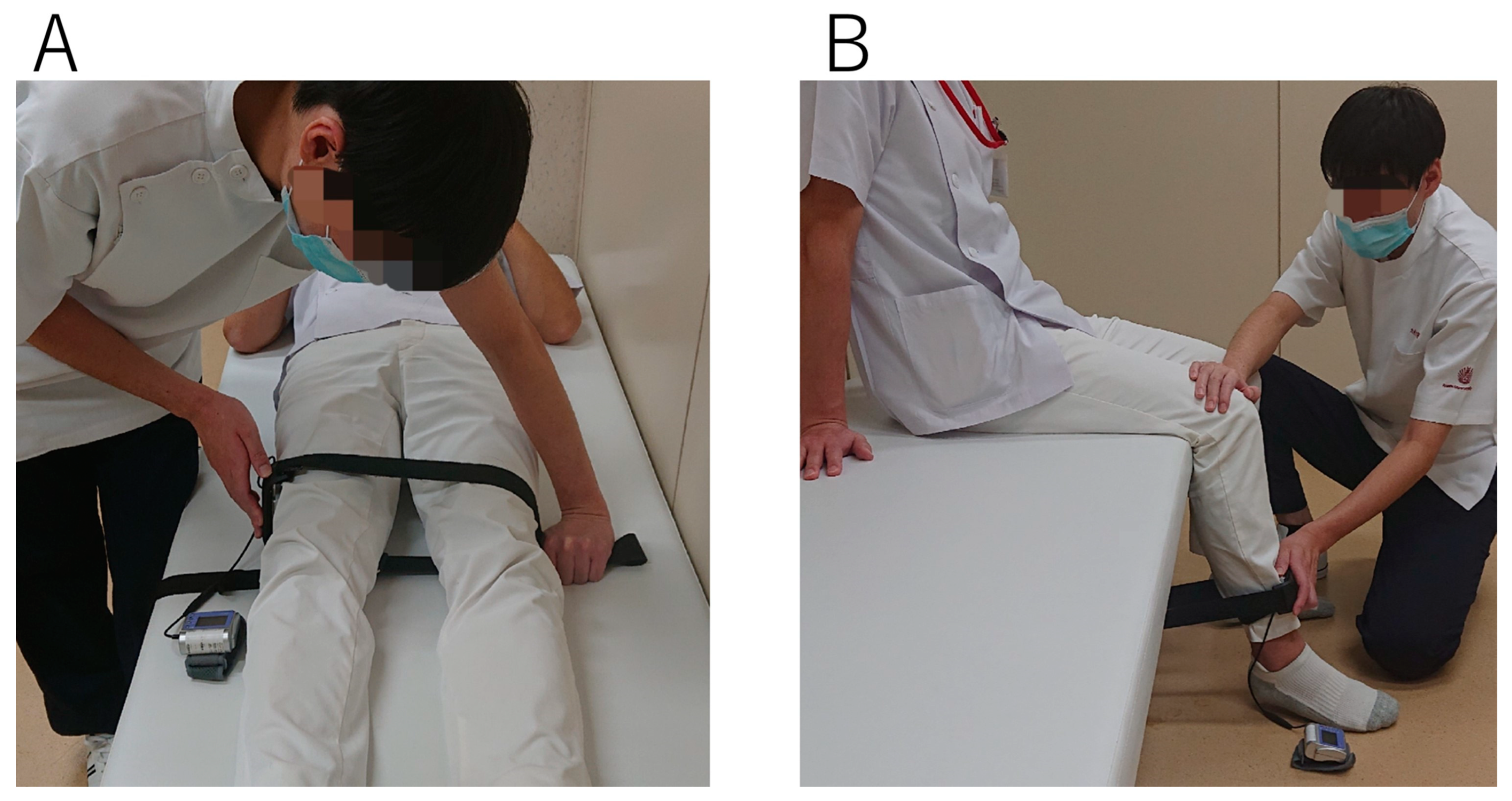
All patients underwent an assessment of maximal voluntary isometric muscle strength in concentric conditions using the hand-held dynamometer (HHD) (μ-Tas F1; ANIMA Inc, Tokyo, Japan) before surgery and at discharge (
Figure 2). Hip abductor and knee extensor strengths were quantified by well-trained physiotherapists with more than a year of experience in moment testing [
9,
10]. Two trials were performed after one practice in all examinations, with the highest peak torque (Nm/kg) used for the analysis.
Patients who responded "comfortable" were defined as the "comfort” group, and those who responded "somewhat uncomfortable," "very uncomfortable," or "impossible" were defined as the "discomfort” group. Patient characteristics, postoperative satisfaction, and muscle strengths were compared between “comfort” and “discomfort” groups using the Student’s t-test. Logistic regression analysis was performed to identify predictors associated with comfortable getting into and out of a car after THA. Before analysis, we selected the predictive factors with a p-value of <0.05 in univariate analyses [age, sex, body mass index (BMI), surgical side (unilateral or bilateral), contralateral hip (normal, OA or THA), and muscle strengths before THA and at discharge], and then a stepwise method was conducted to select the factors for exclusion of confounding factors. Logistic regression analysis was conducted using the factors selected by the stepwise method. All statistical analyses were performed using JMP® Pro 16 (SAS Institute Inc., Cary, NC, USA) with a significance level established at 0.05. Power analyses showed that the combined sample size of the two groups was 61, which provided 80% statistical power to detect the difference in muscle torque of HHD between the two groups [
9].
3. Results
Of the 172 patients, 161 used a car and 101 were drivers (
Figure 1). Of the 161 patients who used a car at a mean of 5.6 years after THA, 87 (54.0%) did so within 1 month after surgery, 52 (32.3%) within 1–3 months, 9 (5.6%) within 3–6 months, 11 (6.8%) within 6–12 months, and 2 (1%) after 12 months. Of the 161 patients, 114 (70.8%) were placed in the “comfort” group (
Table 2). In the "discomfort" group, 26 patients felt more uncomfortable using the door of the contralateral side, about three-fold more than the 8 patients who felt more uncomfortable using the door of the surgical side. In addition, 28 patients experienced more discomfort when getting into a car, almost twice as many as the 15 patients who experienced discomfort when getting out (
Table 3). The main reason for discomfort was muscle weakness, followed by pain, and limited range of motion (
Table 3). The "discomfort" group contained significantly more females and were less satisfied with pain and function (p < 0.05;
Table 4). Hip abduction muscle strength (surgical/ contralateral side) before surgery and at discharge (a mean of 3.3 weeks) averaged 0.44/0.57 Nm/kg and 0.47/0.61 Nm/kg, respectively, in patients with a mean age of 65 years. Knee joint extensor strength (surgical/contralateral side) averaged 0.74/0.94 Nm/kg and 0.75/0.99 Nm/kg, respectively; the "discomfort" group had significantly lower contralateral hip abduction and contralateral knee extension muscle strength before surgery and at discharge (p < 0.05;
Table 4). Multivariate analysis using significant factors (sex, and contralateral hip abductor and contralateral knee extensor muscle strength before surgery and at discharge) in univariate analysis showed that lower preoperative contralateral hip abductor muscle strength was the only significant predictor of discomfort when getting into and out of a car (p < 0.05;
Table 5).
4. Discussion
This study is the first to report on the characteristics of getting into and out of a car after THA. Approximately 94% of patients used a car at mid-term after THA. Of them, 71% of patients felt comfortable getting into and out of a car, with the preoperative contralateral hip abductor muscle strength being a significant predictor.
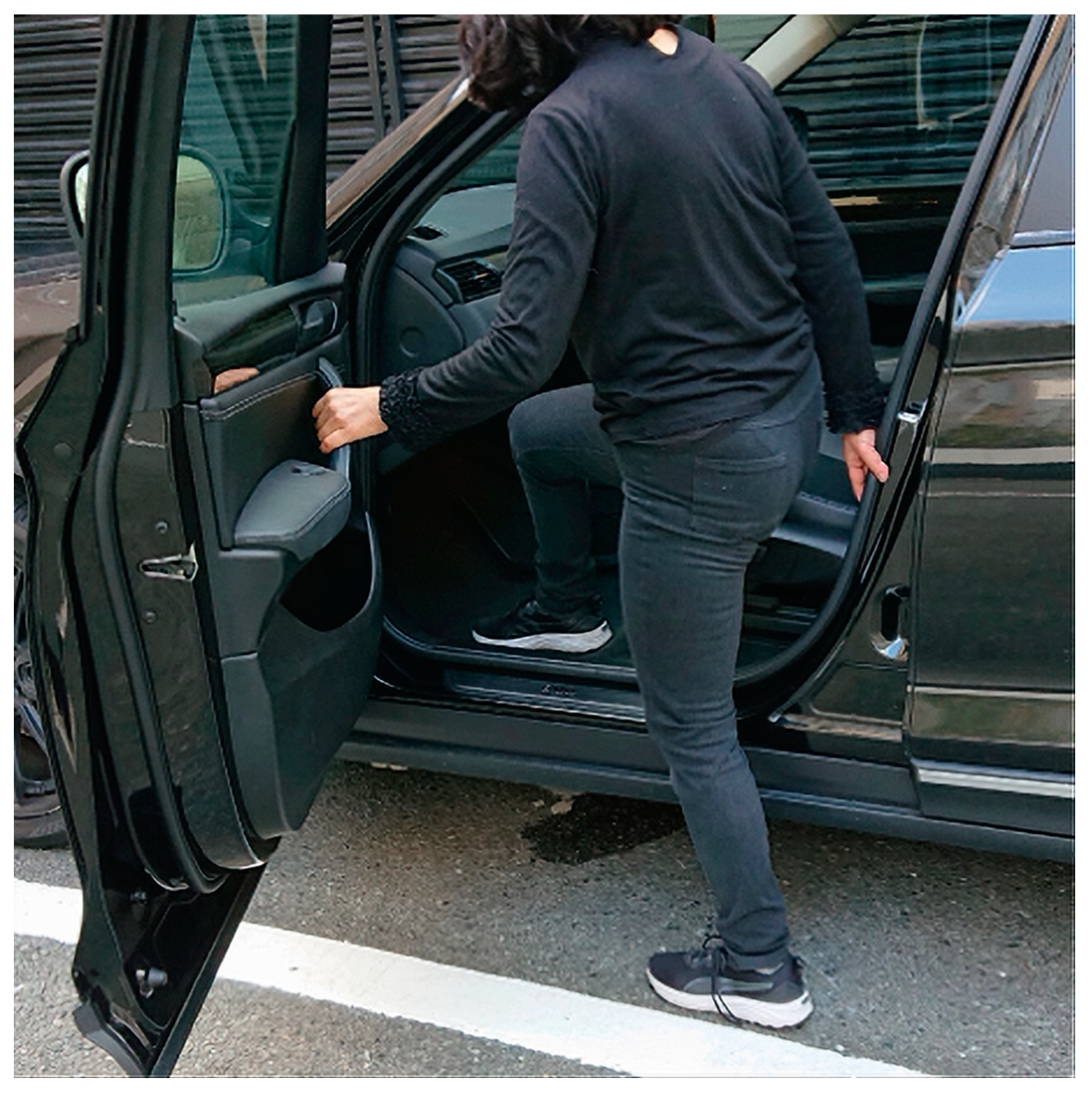
Twenty-nine percent of patients who received primary THA reported feeling uncomfortable getting into and out of a car. Patients in the "discomfort" group were about three-fold more likely to experience discomfort when using the door of the contralateral side than the door of the surgical side, and about twice as many patients experienced discomfort when getting into a car as when getting out. These findings may indicate that this cohort of patients were more likely to feel discomfort when using the contralateral side as the pivot limb than the surgical side, and found getting into a car more uncomfortable than getting out of a car (
Figure 3). The primary reason for discomfort was muscle weakness, followed by pain and limited range of motion. In addition, the patients had significantly lower pain and functional satisfaction compared to the comfortable group. Previous studies have reported the importance of functional improvement and pain relief in improving patients' ADLs and sports participation after THA [
2,
11,
12,
13]. This study also emphasized the importance of functional improvement and pain relief. The significantly higher proportion of females in the "discomfort" group was consistent with previous reports that demonstrated the association between sex and clinical outcomes after THA [
2,
11].
Patients in this study, with a mean age of 65 years, had 0.57 Nm/kg and 0.61 Nm/kg of isometric hip abduction muscle strength on the contralateral side before surgery and at discharge (mean 3.3 weeks postoperatively), respectively, which was comparable to the isometric hip abduction muscle strength (0.57 Nm/kg) of healthy participants of a similar age [
16]. Isometric hip abduction muscle strength on the surgical side was 0.44 Nm/kg and 0.47 Nm/kg before surgery and at discharge, respectively. Fukushi et al. [
9] reported isometric hip abduction muscle strength on the surgical side relative to the contralateral side, preoperatively and 1 month postoperatively, in THA patients with a mean age of 66 years to be 78% and 77%, respectively. These values are comparable to the 77% and 77% found in the present study, indicating that the current muscle strength data were adequate. Lower hip abductor muscle strength on the contralateral side preoperatively was a predictor of perceived feeling of discomfort concerning getting into and out of a car in the mid-term after THA. Ohmori et al. [
17] report that clinical outcomes after THA are influenced by preoperative contralateral limb strength, which is consistent with the findings of this study. These results suggest that it is important to prevent contralateral muscle weakness prior to THA. Furthermore, Moore et al. [
18] report that single-legged standing with contralateral lower extremity motion results in higher hip abductor muscle activation of the pivot limb. Thus, the hip abductor muscle strength of the pivot leg plays a significant role in getting into and out of a car, and a lower hip abductor muscle strength of the contralateral side may influence the discomfort felt by many patients when getting into and out of a car with the contralateral side as the pivot leg. Meanwhile, our recent study showed, in a 3D dynamic analysis using a motion capture method, that getting into and out of a car with the contralateral side as the pivot hip is more similar to the dynamic of a healthy patient than using the surgical side as pivot hip; furthermore, that strengthening of the abductor and extensor muscles of the surgical hip is important for a balanced motion when using the surgical hip as the pivot limb [
19]. This difference in findings may have been explained by the fact that the present study had included patients with OA and THA on the contralateral side and patients who required aids for walking in their study, unlike the patients included in the 3D dynamic analysis.
The current study has several limitations. Unreturned and missing questionnaire data impacted the study’s sample size. However, the overall 56% response rate was comparable with previous studies [
2,
3,
20]. In addition, the physical function data at the time of the questionnaire was not analyzed. Thus, the relationship between muscle strength and comfort in getting into and out of a car in the mid-term postoperative period was not assessed; however, this study was able to show that preoperative physical function predicted motion comfort in the mid-term postoperative period.
5. Conclusion
Approximately 94% of the patients were using a car at mid-term after THA, and 29% of them felt discomfort while getting into and out of a car, especially when using the contralateral side as the pivot limb and during entry. Muscle weakness was primarily attributed as the reason for this subjective impression. The predictor of discomfort concerning getting into and out of a car was a preoperative decline in contralateral hip abduction muscle strength, and prevention of this weakness prior to surgery was found to be important.
Author Contributions
T. H: methodology, investigation, and writing—original draft. S. H: conceptualization, formal analysis, review and editing, and funding acquisition. D. H: investigation and funding acquisition. T. F, D. F, S K, R. Y: investigation. K. K, Y. N: supervision. All authors contributed to the article and approved the final version.
Funding
This work was supported by a Grant from The General Insurance Association of Japan (22-1-005), ZENKYOREN (National Mutual Insurance Federation of Agricultural Cooperatives), a Grant-in-Aid for Scientific Research awarded by the Japan Society for the Promotion of Science [Grant Number JP21K21256], the Ogata Memorial Foundation, Inc. (No. 135), Shimadzu Science Foundation, Grant of The Clinical Research Promotion Foundation 2021 and Foundation for the Promotion of Clinical Medicine.
Institutional Review Board Statement
The study was approved by the Institutional Review Board of the Kyushu University Hospital (IRB number: 21142-00).
Informed Consent Statement
All participants gave their informed consent for inclusion before participation. Data were handled following the ethical standards of the Declaration of Helsinki.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
All authors have no competing interests to declare.
References
- Learmonth, ID; Young, C; Rorabeck, C. The operation of the century: total hip replacement. Lancet 2007;370:1508–19. [CrossRef]
- Fujita, T; Hamai, S; Shiomoto, K; Okazawa, K; Nasu, Y-K; Hara, D; et al. Analysis of factors influencing patient satisfaction after total hip arthroplasty in a Japanese cohort: the significant effect of postoperative physical activity. n.d.
- Shiomoto, K; Hamai, S; Motomura, G; Ikemura, S; Fujii, M; Nakashima, Y. Influencing Factors for Joint Perception After Total Hip Arthroplasty: Asian Cohort Study. Journal of Arthroplasty 2020;35:1307–14. [CrossRef]
- van der Velden, CA; Tolk, JJ; A Janssen, RP; Reijman, M; Surgery, O; Resident, O; et al. When is it safe to resume driving after total hip and total knee arthroplasty? a meta-analysis of literature on post-operative brake reaction times. Bone Joint J 2017:99–566. [CrossRef]
- Bäcker, HC; Krüger, D; Spies, S; Perka, C; Kirschbaum, SM; Hardt, S. Effect of total hip arthroplasty on brake reaction time and braking force. HIP International 2022;32:51–5. [CrossRef]
- Dugdale, EM; Siljander, MP; Trousdale, RT. Factors Associated With Early Return to Driving Following Total Joint Arthroplasty. Journal of Arthroplasty 2021;36:3392–400. [CrossRef]
- Nakashima, Y; Hirata, M; Akiyama, M; Itokawa, T; Yamamoto, T; Motomura, G; et al. Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop 2014;38:27–32. [CrossRef]
- Mahomed , N; Gandhi, R; Daltroy, L; Katz, JN. The Self-Administered Patient Satisfaction Scale for Primary Hip and Knee Arthroplasty. Arthritis 2011;2011:1–6. [CrossRef]
- Fukushi, J, ichi; Kawano, I; Motomura, G; Hamai, S; Kawaguchi, K, ichi; Nakashima, Y. Does hip center location affect the recovery of abductor moment after total hip arthroplasty? Orthopaedics and Traumatology: Surgery and Research 2018;104:1149–53. [CrossRef]
- Kiyohara, M; Hamai, S; Hara, D; Fujiyoshi, D; Harada, S; Kawaguchi, K; et al. Do component position and muscle strength affect the cup-head translation during gait after total hip arthroplasty? European Journal of Orthopaedic Surgery and Traumatology 2019;29:1263–9. [CrossRef]
- Wylde, V; Blom, A; Dieppe, P; Hewlett, S; Learmonth, I; Professor of Musculoskeletal Sciences, H; et al. Return to sport after joint replacement 2008;90:920–3. [CrossRef]
- Huch, K; Müller, KAC; Stürmer, T; Brenner, H; Puhl, W; Günther, KP. Sports activities 5 years after total knee or hip arthroplasty: The Ulm osteoarthritis study. Ann Rheum Dis 2005;64:1715–20. [CrossRef]
- Abe, H; Sakai, T; Nishii, T; Takao, M; Nakamura, N; Sugano, N. Jogging after total hip arthroplasty. American Journal of Sports Medicine 2014;42:131–7. [CrossRef]
- Hofstede, SN; Gademan, MGJ; Vliet Vlieland, TPM; Nelissen, RGHH; Marang-Van De Mheen, PJ. Preoperative predictors for outcomes after total hip replacement in patients with osteoarthritis: A systematic review. BMC Musculoskelet Disord 2016;17:1–11. [CrossRef]
- Rojanasopondist, P; Galea, VP; Connelly, JW; Matuszak, SJ; Rolfson, O; Bragdon, CR; et al. What preoperative factors are associated with not achieving a minimum clinically important difference after tha? Findings from an international multicenter study. Clin Orthop Relat Res 2019;477:1301–12. [CrossRef]
- Nankaku, M; Tsuboyama, T; Kakinoki, R; Akiyama, H; Nakamura, T. Prediction of ambulation ability following total hip arthroplasty. Journal of Orthopaedic Science 2011;16:359–63. [CrossRef]
- Ohmori, T; Kabata, T; Kajino, Y; Inoue, D; Kato, S; Tsuchiya, H. Contralateral Lower-Limb Functional Status Before Total Hip Arthroplasty: An Important Indicator for Postoperative Gait Speed. J Bone Joint Surg Am 2021;103:1093–103. [CrossRef]
- Moore, D; Semciw, AI; Pizzari, T. A Systematic Review and Meta-Analysis of Common Therapeutic Exercises That Generate Highest Muscle Activity in the Gluteus Medius and Gluteus Minimus Segments. Int J Sports Phys Ther 2020;15:856–81. [CrossRef]
- Harada, T; HHamai, S; Hara, D; Kawahara, S; Fujii, M; Ikemura, S; et al. Three-dimensional kinematics and kinetics of getting into and out of a car in patients after total hip arthroplasty. Gait Posture 2022;98:305–12. [CrossRef]
- Harada, T; Hamai, S; Shiomoto, K; Hara, D; Kawahara, S; Fujii, M; et al. Analysis of Factors That Influence Patient Satisfaction After Periacetabular Osteotomy: An Asian Cohort Study. Orthopedics 2022;45:297–303. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).