1. Introduction
Chronic diseases are long-term conditions with persistent effects, are more common in older people and can usually be controlled but not cured [
1]. People with chronic diseases frequently have more than one chronic disease. Arthritis, asthma, back pain, cancer, cardiovascular disease, chronic obstructive pulmonary disease, diabetes, chronic kidney disease, mental health conditions, and osteoporosis are the most commonly reported chronic conditions [
2]. Chronic diseases account for many hospital readmissions because they are associated with high rates of mortality and morbidity, as well as the need for continuous treatment and monitoring [
1,
3]. Since chronic diseases necessitate specialized home care to meet patients' needs or administer therapy programs, and most caregivers and families lack the time or skills to care for patients, patients with chronic diseases have the highest rate of readmission [
4,
5].
Although some other factors contribute to readmission, such as increasing age, male gender, diagnosis of congestive heart failure or diabetes, severe illness, visual impairment, prolonged length of stay, high prior utilization, having a low SES (socioeconomic status), living alone, and receiving limited social support, hospital readmissions can indicate problems with caregiving during transfers between care settings or from a facility to home.
The annual cost of hospital readmissions is estimated to be around
$26 billion in the US [
6], with heart failure (HF) and chronic obstructive pulmonary disease (COPD) accounting for 9% of all medical admissions [
5]. While not all readmissions are entirely avoidable, it is widely accepted that a portion of unplanned readmissions can be avoided by addressing several barriers that patients face before, during, and after admission and discharge. As a result, targeted and specific efforts to prevent readmissions among minority and vulnerable populations are required [
9].
Healthcare experts, providers, and policy-makers are attempting to find new ways to reduce healthcare costs while lowering readmission rates. Improving the care process and delivery, information systems, and analytics research can be crucial in recommending new and innovative health strategies and solutions [
4]. Recent federal efforts in information systems and analytics research have focused on reducing hospital readmissions in chronic disease, such as implementing social determinants of health screening protocols to identify patients at high risk for readmissions, retrospective analyses to examine the prediction of rehospitalization, data analytics and risk stratification tools, developing e-health systems for remote patient monitoring (RPM), and electronic health records.
The Internet of Things (IoT), sensors, wearables, social media, mobile apps, and genomics are also being used to lower readmission rates. Readmission rates are changing with advances in AI and analytics [
4]. AI refers to intelligent systems that analyze their surroundings and take action to achieve specific goals. Machine learning (ML) techniques, robotics, algorithms, and automated decision-support systems are all used in these systems. AI-based technology in various forms is currently being used in healthcare. Artificial intelligence and machine learning have already outperformed traditional prediction models for several medical applications, according to new methods from the field of Intensive care [
10]. Healthcare providers can use AI to identify patients by leveraging advanced analytics, real-time monitoring, and decision support systems.
As AI makes predictions particularly sensitive to environmental conditions, such as the data samples used, there are concerns about the biases and robustness of new AI techniques caused by these technologies' preliminary design [
10]. As a result, there are increasing recommendations and guidelines dealing with the ethical AI issue. AI must be confined to fundamental rights, values of society, and the moral values of explicability, prevention of harm, fairness, and human autonomy [
10], in addition to sticking to rules and regulations and being technically robust.
The paper is organized as follows.
Section 2 explores the economic impact of chronic illness readmissions and highlights the financial implications for healthcare systems. Building upon this understanding,
Section 3 proposes a comprehensive taxonomy of AI technologies specifically designed to tackle the challenge of reducing hospital readmissions. In
Section 4, we critically assess the limitations of existing systems, identifying potential improvements. To provide insights into the latest advancements,
Section 5 highlights emerging trends in AI technologies.
Section 6 takes a deep dive into a case study analysis, demonstrating the practical application of AI systems to address concerns in this domain. This analysis is followed by detailed recommendations in
Section 7, outlining strategies for optimizing the future use of AI systems. Finally, in
Section 8, we present the conclusion, summarizing the essential findings and emphasizing the potential impact of continued advancements in AI technology for reducing hospital readmissions.
2. The Economic Burden of Hospital Readmission for Chronic Diseases
Individuals with multiple chronic conditions incur a significant and disproportionate portion of the total cost of healthcare. This high cost is due to the high number of hospital admissions per year related to patients having complex chronic illnesses with multiple conditions, resulting in higher healthcare costs [
11]. Identifying patients with an increased risk of readmission and their potential financial impact is essential to reducing readmissions. The economic burden of being readmitted to hospitals for progressive illnesses is well-documented in the medical literature. Recurrent hospitalizations for illnesses like congestive heart failure, chronic obstructive pulmonary disease, diabetes, and kidney disease are expensive and have a negative financial impact, as numerous studies show.
Readmission in chronic diseases is associated with several costs, including direct healthcare costs, such as hospital stays, diagnostic tests, medications, procedures, and consultations [
12], prolonged expenditures on hospitalization due to complications or disease exacerbations, unplanned healthcare utilization significantly increasing the financial burden, long-term medication and treatment costs for poor disease management [
13], etc.
In addition to these regular costs, each chronic disease carries other expenses. The readmission cost for particular diseases can vary depending on several variables, including the severity level of the condition, adverse effects, length of hospital stay, and necessary treatments.
The more severe COPD (chronic obstructive pulmonary disease) frequently raises healthcare costs by requiring more inpatient hospitalizations, emergency room visits, office visits, and prescription medications [
11]. Congestive heart failure (CHF), pneumonia (PNA), acute myocardial infarction (AMI), anxiety disorders, cerebrovascular disease, CHF, coronary artery disease, depressive disorders, osteoarthritis, osteoporosis, sleep apnea, and type 2 diabetes are some of the comorbidities that COPD includes, which increases utilization and associated costs. Poor lung function also appears to be a factor in COPD-related healthcare costs. Diabetes-related hospital readmissions can result in additional expenses like prolonged hospital stays, medication adjustments, laboratory tests, and potential complications management, all of which can raise healthcare costs. Costs for ER visits, hospital stays, medication changes, diagnostic exams, and follow-up care may result from readmissions for asthma [
11]. These costs may raise the total financial burden. As a result of extended hospital stays, cardiac procedures, medications, rehabilitation programs, and ongoing management to ward off new complications, hospital readmissions for heart disease can be costly. While readmissions for depression may not incur high direct costs such as surgeries or procedures, they can still contribute to expenses such as psychiatric consultations, medication or therapy adjustments, and potentially more extended hospital stays for severe cases. Hospital readmissions for Alzheimer's disease may incur costs for diagnostic evaluations, medication adjustments, specialized care, safety measures, and caregiver support during hospital stays and after discharge.
Reducing hospital readmissions for chronic diseases is essential for economic relief; strategies like care coordination, patient education, transitional care, and remote monitoring improve management can mitigate the financial impact of readmissions and improve the overall management of chronic conditions.
3. Taxonomy of AI Technologies in Reducing Hospital Readmission
Artificial intelligence (AI) AI technology integration in healthcare has the ability to transform clinical procedures, advance diagnostics, simplify workflows, and boost patient outcomes. Precision diagnosis, proactive disease prevention, personalized treatment plans, real-time monitoring and intervention, improved medical imaging, streamlined healthcare workflows, ethical considerations, and the potential future implications of AI in healthcare are the areas of AI that are used in healthcare [
14]. AI can be used to effectively reduce hospital readmissions by identifying patients who are at risk for readmission.
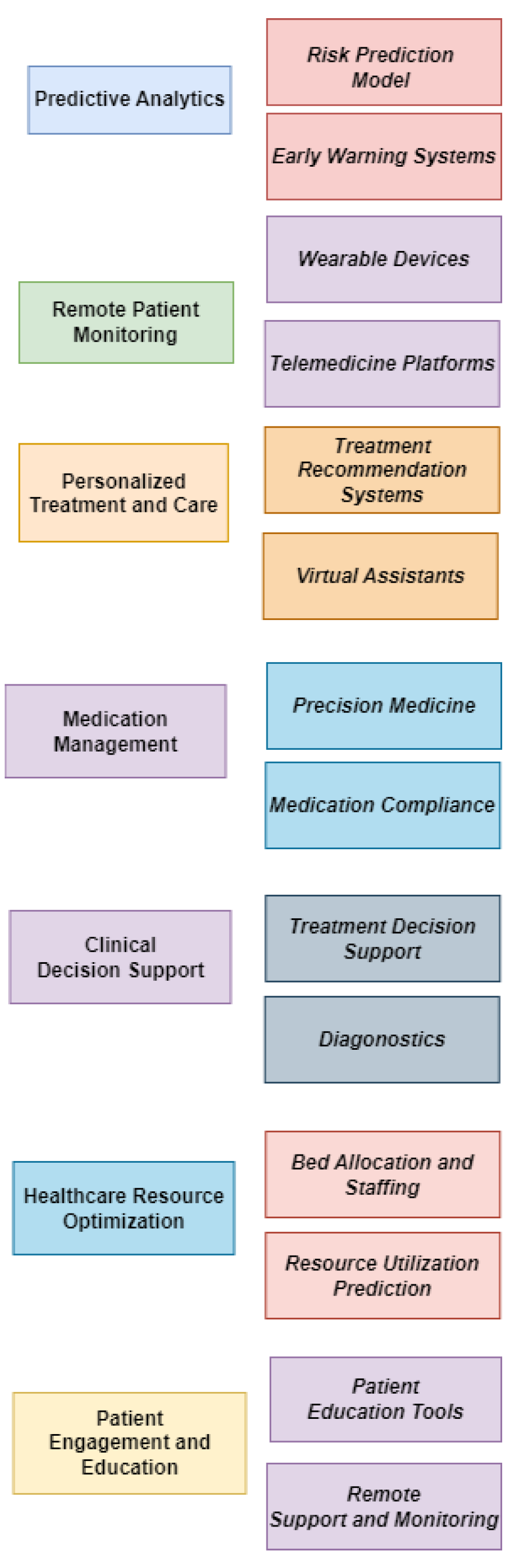
Figure 1 categorizes different AI applications based on specific functions and capabilities.
AI in healthcare targets personalized treatment and early disease detection through extensive analysis of patient data. The first segment employs predictive analytics to identify individuals at high risk of specific conditions, aiming to prevent diseases. The second segment analyzes patient data, including genetics, biomarkers, and therapy response, to develop customized treatment plans. Several applications of AI play an influential role in reducing hospital readmission rates.
AI-Driven Diagnostics use AI algorithms such as machine learning and deep learning techniques to analyze vast volumes of medical data, including photos, test findings, and patient records for early detection of ailments like cancer, heart disease, and neurological problems [
14]. Early detection improves prognosis and treatment outcomes [
14]. AI can enhance predictive performance by incorporating novel or richer data sets, including laboratory results, comorbidity records, and medication history. It can fully utilize the valuable information hidden in electronic medical record (EMR) data, particularly patients' historical knowledge and their comparison to previous admissions, to identify necessary details related to the patient's condition, treatment plans, and discharge instructions [
15]. NLP enables AI systems to analyze and extract such information.
Precision Medicine, which tailors medical interventions to individual patients based on their genetics, lifestyle, and environment, has advanced with the help of AI by analyzing extensive genetic and clinical data to identify biomarkers, predict disease vulnerability, and recommend personalized treatment plans. This approach can revolutionize disease management, optimize drug selection, minimize side effects, and improve patient care and outcomes [
14], thus reducing the risk of complications and readmissions.
Healthcare operations and workflow management are also changing due to AI technologies. AI-powered intelligent automation can automate tasks like patient triage, appointment scheduling, and electronic health record administration, which relieves administrative pressure on healthcare workers and frees them up to devote more time to patient care [
14].
AI has made the drug discovery and development process easy by identifying prospective therapeutic targets, forecasting drug effectiveness, and enhancing drug candidates, hastening the development of novel treatments [
14].
AI-powered remote monitoring systems enable continuous monitoring of patients' conditions and detect early warning signs, reducing hospital readmission. In this context, Telehealth minimizes the need for in-person visits by facilitating virtual consultations and follow-up care, enhancing patient access to healthcare professionals.
Poor medication adherence is a significant factor in hospital readmissions. AI technologies can help address poor medication adherence issues by providing medication reminders, tracking adherence, and alerting healthcare providers and patients about missed doses or potential interactions.
AI transforms healthcare delivery by enabling personalized treatment plans, facilitating early disease detection, leveraging predictive analytics, and empowering virtual assistants [
14]. Although AI technologies play a significant role, challenges related to data protection, algorithmic transparency, and ethical considerations must be overcome through collaboration between healthcare providers, researchers, legislators, and technology specialists. Collaborative efforts between healthcare providers, AI developers, and policy-makers are crucial to ensure AI's responsible and effective deployment in reducing hospital readmissions [
14].
4. Limitations in Current Solutions
There are various challenges which are associated with current AI solutions. Some of the prominent ones are ethical considerations in AI adoption for readmission reduction, Data Privacy and security concerns, algorithm bias and fairness issues, explainability and interpretability, legal and regulatory implications, integration with existing healthcare systems, adoption and acceptance by healthcare professionals, and cost and resource considerations.
The use of AI raises questions about its algorithms, including biased training data, ambiguous correlations, a lack of comprehension, errors, and the possibility of unfair results. Since machine learning (ML) algorithms heavily rely on the training data, they will unintentionally pick up and reproduce biases against minorities or other vulnerable groups in society in their outputs [
16]. Although it might seem like a good idea to remove sensitive factors like race, age, or gender from the model, non-sensitive characteristics like postal codes can still serve as proxies and correlate with these factors, perpetuating bias. Additionally, ML classifiers tend to improve with more data, but minorities frequently have disproportionately less data available. As a result, classifiers perform worse for smaller groups and models developed for majorities may not accurately apply to minorities.
AI algorithms like machine learning and deep learning are associated with many biases, including bias in model design, training data, clinician interactions, and patient interactions. These biases are frequently caused by a lack of dataset for disease diagnoses, such as a low number of images to detect diabetic retinopathy, an uneven distribution of different groups for classifying different stages of diseases, and some sensitive categories such as gender, race, age, sexual orientation, ability, or belief [
20]. These data and system biases can impact the AI algorithms' fair and inclusive outcomes. Furthermore, these biases draw attention to several social and demographic variables that affect how people access and are represented in the healthcare system [
20].
As a result of these biases in training data, the fairness of decision-making and the outcomes produced by AI systems has been called into question. The AI system must be reliable and generalizable to produce fair results and become trustworthy [
19]. To obtain accurate patient outcomes and justified resource allocation, fairness must be ensured to identify ethical issues created. It must be integrated into the model design [
19]. As a result, recurrent readmissions caused by disease misclassification or misdiagnosis will be reduced, and clinical resources will be allocated and used appropriately.
Algorithms frequently use strong correlations rather than proven causal relationships to make decisions. Making decisions based solely on correlations without considering the ethical implications and context can result in biased and unfair outcomes. AI will be challenging if there is a lack of transparency, such that humans cannot represent them [
17]. They may even have far-reaching effects. As a result, the importance of AI systems being understandable has increased. For an algorithm to be considered intelligent, its decisions must be answerable to and comprehendible by humans, especially in critical areas where AI decisions have a significant impact.
Since AI is probabilistic, it is susceptible to error. This might happen due to biases, errors, or the model's incapacity to faithfully reflect real-world scenarios. Therefore, it is crucial to carefully assess and consider AI systems' constraints and potential adverse effects. Because the underlying data used to train AI algorithms may contain biases, using AI systems can result in unfair results. Such prejudices may lead to the unfair treatment or disadvantage of particular people or groups [
18]. Addressing and mitigating these issues is imperative to ensure that AI systems support equality and fairness in decision-making.
Accessing and analyzing patient data is crucial for using AI technologies to lower hospital readmission rates. Since sensitive health information must be protected from unauthorized access or breaches, this raises questions concerning data privacy and security. Maintaining patient confidence and adhering to applicable privacy laws make protecting patient data essential.
On the other hand, the explainability and interpretability of AI models are essential challenges in developing and using AI-based hospital readmission solutions. These challenges arise because many AI models are complex and opaque, making it difficult to understand how they make their predictions. This can make it difficult to trust the predictions of AI models and make it challenging to use AI models to inform clinical decision-making. In addition, many AI models lack transparency resulting in unable to understand the way they make predictions. Sometimes this is due to the proprietary nature of the algorithms behind these models and the unwillingness of the model developers to share how they work. The challenges also stem from the fact that there are a limited number of tools available for explaining AI models. Some available tools can help identify the most critical features behind those AI models' predictions. Still, they cannot always completely understand how these models work.
As a result, the challenges arising from the explainability and interpretability of AI models in terms of AI-based hospital readmission solutions can have a number of negative consequences. These consequences can start from reduced trust in AL models, increased bias, and increased patient harm. For instance, discrepancies in healthcare delivery may result if an AI model suggests various treatment options for different demographic groups without a convincing reason.
The use of AI technologies to reduce readmissions creates legal and regulatory issues. To safeguard patient rights and ensure the secure processing of patient data, compliance with healthcare standards, such as HIPAA (Health Insurance Portability and Accountability Act), is essential. Healthcare organizations must understand the legal system to ensure compliance with applicable laws and rules governing the implementation of AI.
Integrating AI technologies into current healthcare operations and systems can be challenging. Compatibility problems, data interoperability problems, and workflow disruptions might occur during the implementation process. To enable seamless collaboration between AI technologies and current infrastructure, healthcare organizations must carefully plan and strategize the integration of AI systems.
The acceptance and involvement of healthcare professionals are essential for the effective use of AI technology for readmission reduction. The adoption and use of these technologies may be hampered by a lack of knowledge of AI, scepticism, and resistance to change. Healthcare workers should receive training, education, and support to ensure their active participation and acceptance of AI technologies.
AI technology adoption and upkeep can be expensive, requiring investment in infrastructure, data storage, algorithm development, and training. Healthcare organizations must also save money for routine system maintenance, updates, and employee training. It is essential to thoroughly assess AI solutions' affordability and long-term viability for readmission reduction.
AI has revolutionized the healthcare sector by accurately analyzing and interpreting large datasets that would otherwise require human intelligence, such as problem-solving, data interpretation, and decision-making. Various clinical and patient-facing applications are already in the healthcare sector, including GP at Hand for assessing known symptoms and risk factors to provide informed medical information, Corti for managing and optimizing the emergency dispatch process, and many others. These AI-based applications are being developed and are increasingly used to relieve strain on healthcare staff, reduce costs, and improve patients' lives.
While the potential benefits of artificial intelligence in healthcare are significant, it is crucial to acknowledge the complex ethical concerns that arise with its implementation. These concerns must be carefully identified and addressed using evidence-based methods to ensure the responsible and ethical use of AI in healthcare. However, there are no universally accepted frameworks for addressing these ethical concerns surrounding implementing AI-based systems. As a result, research is required to ensure the ethical design and implementation of AI in healthcare [
19].
There has not been enough discussion of the ethical concerns with artificial intelligence, such as biases, patient privacy, building trust, and potential risks like dataset shift, confounder fitting, unintentional bias, generalization to new populations, and detrimental effects on health outcomes. It is critical to develop information systems capable of detecting and responding to unfairness [
19].
Discrimination issues in the healthcare industry, such as the Racial Equality Directive and the Goods and Services Directive, must also be addressed to ensure patients' fundamental rights based on constitutionally protected characteristics such as age, disability, gender transition, pregnancy and maternity, race, religion or belief, sex, and gender identity [
20]. This ensures that all patients are treated equally, and those receiving treatment will not be denied care or readmitted based on those protected characteristics. Healthcare services and insurance plans must be designed in such a way that inequalities are avoided. Readmission can be reduced, and equality is ensured by considering the requirements of all patients and providing fair access to quality care, resulting in improved health outcomes. In order to protect patients' privacy and safety, AI systems designed for readmission management in the healthcare sector should be monitored and evaluated regularly.
AI models should not be created in a way that compromises autonomy. These models must not force a patient to act with intentionality, understanding, or the absence of coercive influences that might unnecessarily influence their actions when receiving healthcare. Patients must be informed about the nature, risks, consequences, and alternatives associated with medical intervention, even though they cannot comprehend how AI algorithms work. They would therefore be competent to decide whether to readmit a patient with a particular chronic condition.
In some chronic conditions, using AI to conclude could result in mistakes or harm to the patients. Therefore, there must be clear guidelines on how to use these products, and the makers of AI systems must be held accountable for the harm caused by flaws in their creations. Mechanisms for ensuring transparent accountability for the results of AI-driven readmission management must be in place.
By reviewing numerous medical records and recommending appropriate treatments, AI supports clinical decision-making and enables data translation into actionable intelligence. It addresses the moral problems that result from their use. Therefore, it is essential to address and discuss medical ethics, identify risks and threats to each principle, and develop mitigation strategies. Thus, ethical standards for using big data and AI technologies in healthcare should be established by the bioethics community, the medical community, and the government [
21,
22]. AI will therefore be able to decrease readmissions to hospitals, enhance medication adherence, and improve resource allocation.
5. The Emerging Trends of AI Technologies in Reducing Hospital Readmission
This section examines the emerging trends of AI technologies in recusing hospital readmission for chronic diseases. Explainable AI, Natural Language Processing, Federated Learning, Precision Medicine and Genomics, Social Determinants of Health (SDOH), Continuous Monitoring and Remote Care all have potential in this context.
Explainable AI: There is a rising focus on creating explainable AI models as AI algorithms get more complicated and smarter [
23]. Healthcare providers will be able to comprehend and have faith in the decision-making process because of Explainable AI's goal of producing transparent and understandable findings. This can improve patient acceptance and enable greater AI technology incorporation into hospital procedures.
Natural Language Processing (NLP): Understanding and producing human language is the focus of NLP, an area of AI developing quickly. NLP can be used to analyze unstructured clinical notes, doctor-patient dialogues, and patient-generated data in the context of readmission reduction to extract insightful information [
24]. It makes it possible to identify important clinical characteristics, stratify risks more precisely, and use personalized therapies.
Federated Learning: Federated learning is a decentralized method of AI training that enables the collaborative development of models across several healthcare organizations without disclosing private patient information. This method tackles privacy issues while gaining the advantages of a vast and varied dataset. Federated learning has the potential to enhance the precision and generalizability of AI readmission reduction models, as proven in some recent study [
25].
Precision Medicine and Genomics: Based on each patient's particular genetic, environmental, and lifestyle characteristics, precision medicine tries to customize medical treatments for them. The analysis of genomics data and the discovery of genetic markers linked to disease progression and readmission risk can be significantly aided by AI technology [
26]. Precision medicine methods and AI integration can lead to more individualized interventions and better patient outcomes.
Social Determinants of Health (SDOH) Integration: Socioeconomic position, housing quality, and access to care are just a few examples of the social determinants of health that significantly impact patient health outcomes and readmission risks. To acquire a thorough picture of patients' circumstances and uncover social aspects that contribute to readmissions, AI technologies can assist in integrating SDOH data with clinical data [
27]. AI can support initiatives to lower readmissions in vulnerable populations by targeting social determinants of health.
Continuous Monitoring and Remote Care: AI technologies are enabling continuous monitoring patients' health conditions in the hospital and at home [
28]. Real-time data on vital signs, exercise levels, and other important health parameters can be gathered through wearable technology and remote sensors. AI algorithms may analyze this data, which can also identify early indicators of deterioration and send timely alerts to healthcare professionals, enabling proactive treatments to reduce readmissions.
These new patterns and developments in AI technology have tremendous potential to cut down on chronic disease-related hospital readmissions. Healthcare practitioners can create more accurate predictions, give individualized interventions, and enhance patient outcomes by utilizing explainable AI, NLP, federated learning, precision medicine, and SDOH integration. The possibilities of AI technology in readmission reduction methods will be further strengthened by continued research and development in these fields.
6. Analyze the Challenges of AI-based Solutions for Hospital Readmission from a Case Study Perspective
This section presents the challenges and solutions for AI-based frameworks regarding hospital readmission from a fictional case study analysis perspective. We designed an AI-based readmission-reducing framework named "Smart Health" in ABC Hospital for patients with COPD. The framework used predictive analytics algorithms to tailor their care plans and identify high-risk patients. The framework's goal was to reduce the readmission rates for COPD patients and improve resource allocation and care strategies. It includes several components and processes.
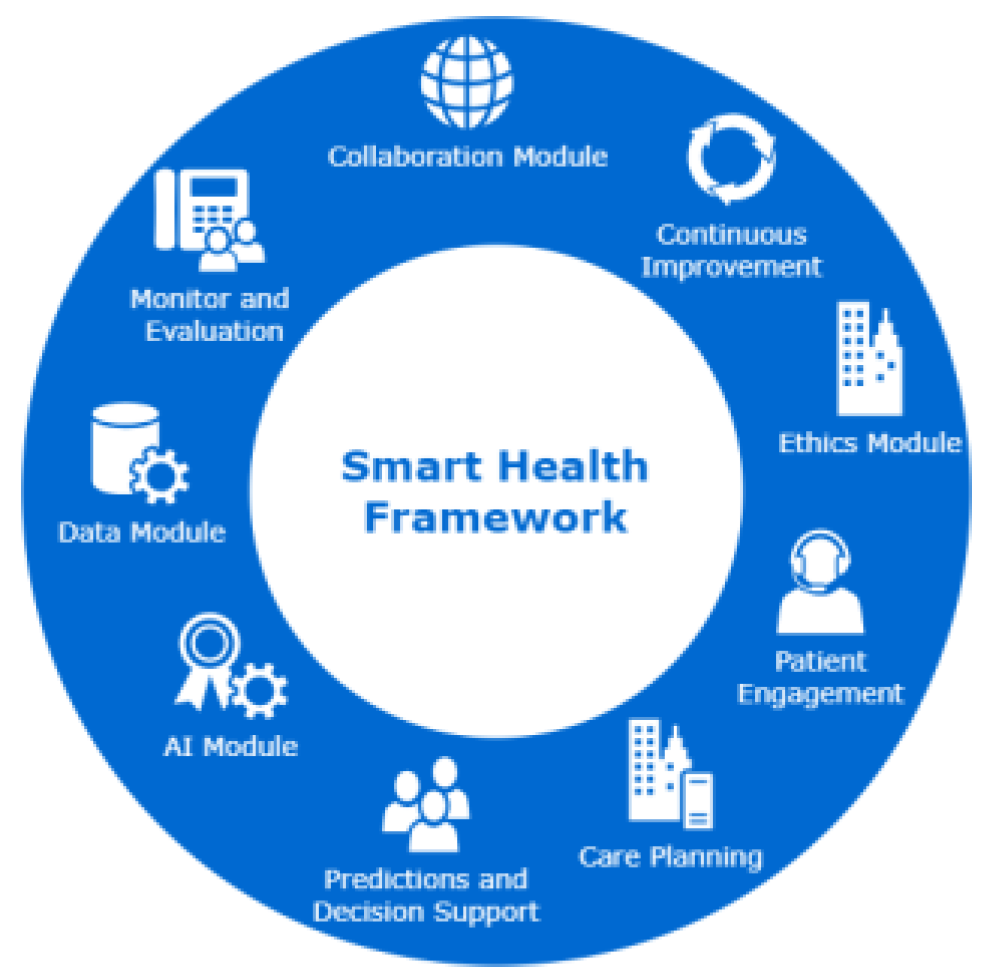
Figure 2 depicts the framework.
The Data Module is responsible for data collection and integration. It ensures patient data collection from various sources, such as Electronic Health Records (EHRs), wearable devices and remote monitoring systems. It also maintains data quality and consistency by implementing data cleaning and preprocessing techniques. Then it integrates the collected data into a centralized repository or warehouse to facilitate continuous analysis.
The AI Module has a few components. They are AI algorithm development, feature engineering, model validation and evaluation, implementation, and integration.
AI algorithm development component selects appropriate machine learning algorithms to develop predictive analytics algorithms. Then it trains the algorithms using the collected patient data from the Data module. The algorithms are optimized by iteratively adjusting model parameters and evaluating performance metrics. The feature engineering component identifies relevant features and variables that contribute to predicting readmission risk in COPD patients. Then it performs feature engineering to create new features or transform existing ones to enhance the predictive power of the algorithms.
The model validation and evaluation component ensures the validation of the performance of the developed algorithms and applies appropriate evaluation metrics, such as accuracy, precision, recall, and area under the curve (AUC), to assess the algorithms' predictive accuracy. It also performs cross-validation techniques to ensure the generalizability and robustness of the models. Then in the implementation and integration stage, the AI algorithms are integrated into the hospital's existing infrastructure, such as the electronic medical record system or clinical decision support systems. Appropriate application programming interfaces (APIs) are developed to enable seamless data flow and interaction between the AI system and other clinical systems. It ensures compatibility and interoperability with existing technologies and workflows.
The Predictions and Decision Support Module applies the trained algorithms to the data collected to identify individuals at high risk of readmission for COPD patients. It defines the parameters and factors considered in assessing the readmission risk level. It also determines the threshold for identifying high-risk patients based on the algorithm outputs. It integrates the AI-powered decision support system into the clinical workflow, providing healthcare providers with timely and actionable insights to guide their decision-making. It also enables alerts or notifications for high-risk patients, facilitating early interventions and personalized care planning.
The Personalized Care Planning module develops personalized care plans for high-risk patients using the identified readmission risk factors from the Predictions and Decision Support Module. It customizes interventions and treatment strategies to address each patient's specific needs and challenges. It collaborates with multidisciplinary healthcare teams to ensure comprehensive and coordinated care delivery.
The Patient Engagement module implements strategies to improve care coordination and communication among healthcare providers, patients, and caregivers. It utilizes AI-powered tools like mobile apps or virtual assistants to facilitate remote patient monitoring, education, and self-management. It Engages patients actively through personalized health coaching, adherence reminders, and timely interventions.
The Monitoring and Evaluation module establishes mechanisms for continuous monitoring and evaluation of the program's effectiveness and impact. It collects readmission rates, patient outcomes, patient satisfaction, and resource utilization data. It analyzes the collected data to assess the program's success in achieving its goals and objectives.
The Continuous Improvement module regularly evaluates the program's performance and identifies areas for improvement. It gathers feedback from healthcare providers, patients, and stakeholders to refine the algorithms, processes, and interventions. It also ensures following the latest information about AI technology advancements. It considers integrating relevant innovations to enhance the program's effectiveness.
The Ethics module establishes and follows ethical guidelines to ensure patient privacy and confidentiality throughout the program. It implements appropriate data governance measures, secure data storage, and access controls to protect patient information. It complies with relevant regulations and guidelines, such as the Health Insurance Portability and Accountability Act (HIPAA) and General Data Protection Regulation (GDPR) regarding data privacy and protection.
The Collaboration module fosters collaboration with other healthcare organizations, research institutions, and industry partners. Share experiences, insights, and best practices with the broader healthcare community through publications, presentations, and forums.
The Smart Health project faced several challenges. Some prominent ones are Algorithmic Bias and Fairness, data privacy and security concerns, and explainability and interpretability. In the case of Algorithmic Bias and Fairness, it was challenging to collect data from diverse patients and train the module with varied and representative training datasets. To address the challenge of algorithmic bias and fairness, the team employed several key strategies. It is described in
Table 1.
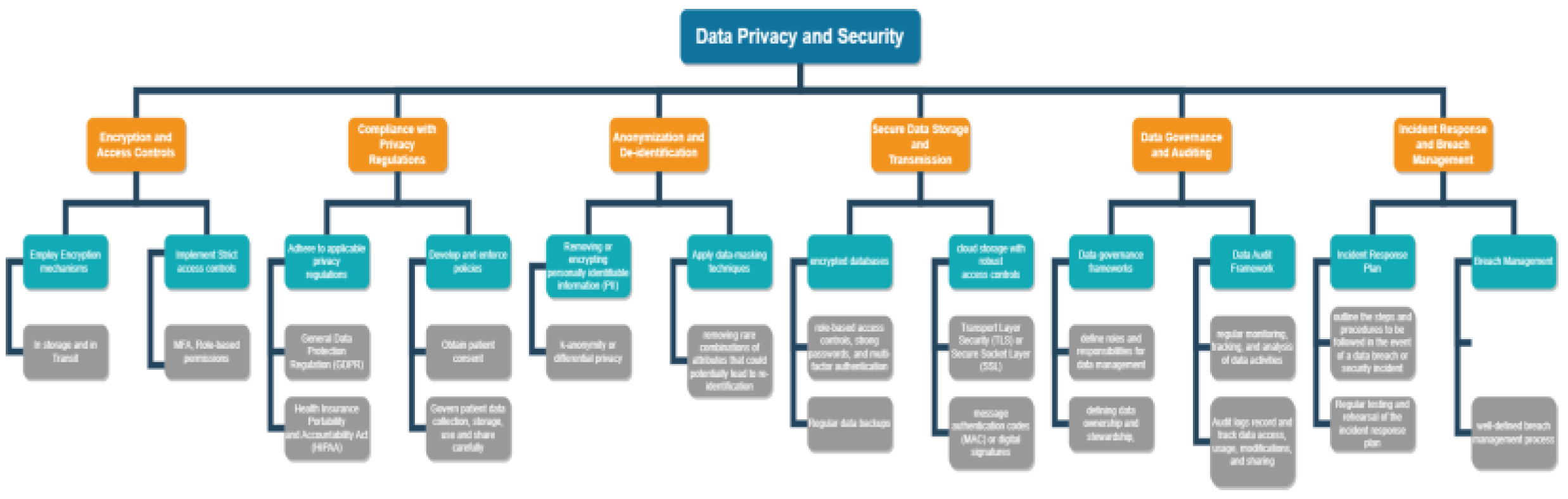
The team also faced data privacy and security concerns, which are generally associated with AI technologies while deployed in the healthcare industry. To deal with these challenges, the team implements several measures depicted in
Figure 3.
The team implemented encryption and access controls to ensure only authorized personnel can access sensitive patient information. It implemented compliance with privacy regulations such as the General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA). The team developed and enforced policies and procedures to govern patient data collection, storage, use, and sharing, including obtaining appropriate patient consent.
The project also used anonymization and de-identification of patient data used for AI algorithms. It ensured removing or modifying information such as names, addresses, social security numbers, and other direct identifiers linking the data to a specific individual. It employed advanced anonymization methods, such as k-anonymity or differential privacy. It applies data masking techniques for de-identification, for example, replacing specific values with general categories or ranges.
Secure Data Storage and Transmission have been implemented by encrypting databases, role-based access controls, strong passwords, multi-factor authentication and regular data backups. Secure communication protocols encrypt data during transmission, such as Transport Layer Security (TLS) and Secure Socket Layer (SSL). Message authentication codes (MAC) and digital signatures are employed to verify the integrity of the transmitted data and ensure it has not been tampered with.
A data governance framework has been developed to define roles and responsibilities for data management, establish data standards and guidelines, and ensure compliance with privacy regulations and ethical considerations. It also confirmed defining data ownership and stewardship. Data auditing is implemented through regular monitoring, tracking, and analysis of data activities to ensure compliance, data quality, and adherence to policies and procedures. Audit logs have been implemented to record and track data access, usage, modifications, and sharing within the AI-powered readmission reduction program. Regular audits and reviews of these logs help detect unauthorized access, suspicious activities, or breaches, allowing for prompt action to mitigate risks.
An incident response plan has been developed and implemented to outline the steps and procedures to be followed during a data breach or security incident. The team has implemented a well-defined breach management process, including notifying affected individuals, regulatory authorities, and other stakeholders.
The team's third challenge was the Explainability and Interpretability of the AI Models. The team employed a multidisciplinary approach involving clinicians, data scientists, policy-makers, and patients to address these challenges. The team ensured collaboration, ongoing research, and iterative improvements to overcome these challenges and maximize the potential benefits of AI technologies in reducing hospital readmissions for COPD patients. Some of the key strategies employed are:
Table 2.
Strategies to Ensure Explainability and Interpretability of the AI Models.
Table 2.
Strategies to Ensure Explainability and Interpretability of the AI Models.
| Strategy |
Details |
| Appropriate model selection and design |
The team used AI models that inherently offer interpretability, such as rule-based systems or decision trees. |
| Feature Importance and Visualization |
The team used visualization tools to provide insights into the features or variables contributing most significantly to the model's predictions. |
| Rule Extraction and Explanation Generation |
The team developed techniques to extract understandable rules or explanations from applied AI models. This allowed the healthcare providers to comprehend the underlying decision logic and trace the reasoning behind the model's predictions, promoting transparency and trust. |
| Local Explanations |
The team provided local explanations at each patient's level to help healthcare professionals comprehend how the model's predictions relate to particular patient features or clinical circumstances. It aided medical professionals in customizing treatment regimens and reaching knowledgeable conclusions that consider each patient's specific requirements and circumstances. |
| Model Documentation and Reporting |
The team documented the development process, training data, and model architecture to facilitate transparency and reproducibility. |
| Collaborative Approach |
To close the knowledge gap between technical skills and clinical understanding, the team established a culture of collaboration between data scientists and healthcare professionals. They engaged in ongoing discussions with healthcare professionals as part of the model-building process, gained insight into the clinical setting, and customized models to meet the unique clinical requirements of COPD patients. |
The team engaged in several strategies to deal with implementation and workflow integration challenges. Some of these are stakeholder engagement, needs assessment and workflow analysis, customization and adaptation, staff training and support, interoperability and data integration, pilot testing and evaluation, continuous monitoring and evaluation change management:
During the deployment phase, the team worked closely with patients, administrators, healthcare providers, and IT personnel. Together, they established goals, identified potential obstacles, and defined roles and responsibilities. To promote shared knowledge of the execution strategy, nurture support, and gain buy-in, they ensured that stakeholders were included and regularly communicated with.
The team also thoroughly evaluated the workflows and processes in the healthcare organization. They pinpointed areas where AI technologies could improve readmission reduction efficacy and efficiency. To assist in smooth integration, the researchers examined how AI technologies may fit into the existing workflows and identified potential opportunities for optimization or redesign.
The team ensures that existing infrastructure and data systems are seamlessly integrated with AI technologies. They created data integration protocols that allow transmitting pertinent patient data to AI systems from EHRs or other sources. To ensure that AI algorithms are as accurate and effective as possible, emphasize the need for consistent, high-quality data.
The team conducted pilot studies to determine the viability and effect of applying AI technology in lowering readmissions. They assessed the AI system's functionality, usability, and interaction with the current process. Before stepping up the implementation, they gathered feedback from healthcare professionals and patients to pinpoint areas that needed improvement and refinement.
The team put in place procedures for ongoing evaluation of the effectiveness of the AI system and its influence on readmission reduction. They analyzed important parameters like readmission rates, patient outcomes, and provider satisfaction to gauge the system's efficiency. They assessed the implementation procedure regularly and made the necessary adjustments to improve workflow integration and results.
The team put change management concepts into practice to overcome resistance and encourage acceptance among healthcare professionals and personnel. They addressed concerns and offered help during the transition. They explained the advantages and beneficial effects of AI technologies on lowering readmissions.
The team faced ethical and privacy concerns related to patient privacy, informed consent, and data security. They have implemented several key strategies to deal with such challenges. Some of these challenges are dealt with when they handle the challenge of date privacy and security concerns and model exploitability, such as Ethical Frameworks and Guidelines, Data Governance and Security, De-identification and Anonymization, Algorithmic Transparency and Explainability, Continuous Monitoring and Auditing, Education and Training. Some of the novel strategies are described in
Table 3.
7. Recommendations and Future Work
In this section, we summarize the recommendations that have been observed in the case study analysis. We classified our recommendations under a few crucial points as follows.
One of the most critical ethical concerns with AI-based systems is bias in training data. Therefore, procedures should be used to detect bias and guarantee fairness. The first and most important solution is to eliminate discrimination. Bias in training data can be avoided by using data gathered from various sources and backgrounds and data preprocessing techniques. Bias can also be decreased by routinely updating training data. In AI, a number of statistical measures are available to detect bias. Bias mitigation techniques, such as oversampling, under-sampling, regularization, and others, can be used if bias is found in training data. The fairness of the AI model would be ensured if bias could be avoided.
AI models ought to be understandable and comprehensible. As a result, patients and healthcare professionals will be able to trust the system because they will be able to comprehend what is happening and how AI is making a decision. Since AI algorithms handle a lot of sensitive patient data, the government must impose fundamental ethical standards to protect privacy and security.
Policy-makers must create regulatory frameworks that handle the particular difficulties and moral questions raised by the implementation of AI in healthcare. These frameworks should include data security, privacy, accountability, and algorithmic transparency rules. Along with ensuring adherence to current healthcare laws and guidelines, they should be adaptable enough to consider the quick development of AI technology.
Policies should emphasize the value of data control and protection. Certain rules should be set regarding collecting, storing, sharing, and anonymizing patient data. This includes thinking about how to get informed permission, protect data, and reduce the possibility of re-identification. To promote equity and inclusivity in AI models, policies should also address concerns about data bias and prejudice.
Implementing AI technologies for readmission reduction requires a stable and expandable data infrastructure. Businesses should spend money on platforms for inte-grating data that can gather and synchronize information from many sources, including electronic health records, wearable technology, and remote monitoring systems. To enable accurate and timely analysis for AI-driven insights, it is essential to ensure data interoperability, quality, and security. To ensure ethical data use and compliance with privacy laws, organizations should implement data governance rules and procedures.
Organizations should establish strong data governance frameworks that prioritize patient consent, data security, and confidentiality; patients should have control over their personal health data and be informed about how AI technologies utilize their in-formation; and patient-centered approaches should prioritize ethical considerations and privacy protection.
The requirement for human oversight and responsibility in the implementation of AI for readmission reduction should be emphasized by policy-makers. To ensure that healthcare professionals retain control over clinical decisions and are responsible for patient outcomes, guidelines should clearly define the roles and responsibilities of these professionals while adopting AI technologies.
Building confidence among healthcare professionals, patients, and regulatory authorities depends on how easily AI algorithms can be understood and how transparent they are. Research should continue to create methods and approaches to make AI models more understandable so that medical professionals may comprehend the underlying thought and decision-making processes. As a result, doctors would be able to verify AI-generated recommendations and encourage the ethical and responsible ap-plication of AI technologies to readmission reduction.
Policy-makers should fund collaborative research efforts and knowledge-sharing initiatives to encourage innovation, standardization, and best practices in AI adoption for readmission reduction. This may entail providing funds for research initiatives, setting up collaborative networks, and developing online forums for exchanging ideas, difficulties, and triumphs. To advance evidence-based AI solutions and guarantee their successful translation into clinical practice, policies should support the formation of research partnerships between academia, healthcare providers, and technology corpo-rations.
While AI technologies can potentially decrease hospital readmissions, longer-term research is required to evaluate their effects on patient outcomes outside the immediate post-discharge period. Additional studies should look into how long-lasting AI innovations are and how well they work to cut readmission rates. Evidence-based healthcare decision-making will be influenced by knowledge of AI technologies' long-term ad-vantages and potential hazards.
Based on unique patient features, AI technologies have the ability to give personalized interventions and treatment strategies. Further study should look at ways to create adaptable AI models that can learn and change when fresh patient data becomes available. This will enable more effective readmission reduction efforts through per-sonalized risk classification, customized interventions, and dynamic treatment plan adjustment.
Applying AI technologies to reduce readmissions necessitates careful consideration of sustainability over the long term and cost-benefit dynamics. Organizations should carry out in-depth cost-benefit studies to determine the costs associated with using AI technology. The initial investment expenses, infrastructure needs, possible cost savings from fewer readmissions, and improvements in patient outcomes are a few examples of the aspects that should be considered in this study. To ensure the long-term viability of AI implementations, it is crucial to identify sustainable funding methods and payment procedures.
Healthcare organizations can make fact-based judgements about implementing AI technology to lower hospital readmissions by completing a thorough cost-effectiveness analysis. Implementing AI interventions that benefit patients and healthcare systems will be made possible by clearly understanding the financial ramifications, cost savings, Return on Investment (ROI), and alignment with value-based care principles.
Conduct a thorough cost study considering all pertinent costs related to implementing AI technologies. In addition to the immediate costs of buying AI systems and software, this study should consider the expenses of employee training, data integration, infrastructure updates, and ongoing maintenance. A thorough understanding of the costs will give the organization a complete picture of the financial resources needed for a successful deployment.
Reducing the number of preventable readmissions will help save money, which is one of the main goals of adopting AI technologies in readmission reduction. Healthcare organizations should calculate the potential cost savings from fewer hospital readmis-sions. This estimate should account for decreased costs for hospital stays, procedures, examinations, and other medical interventions. Cost reductions could also translate into less strain on medical staff and resources.
An estimation of the financial profits made in relation to the initial investment is given by ROI. Negative ROI suggests that the expenses outweigh the benefits, whereas positive ROI shows that the investment has led to cost savings or revenue increase. Organizations can decide the scalability and sustainability of AI interventions through ROI analysis.
Value-based care aims to provide the best patient outcomes at the lowest possible price. AI innovations that improve patient outcomes and decrease readmissions are consistent with value-based care tenets. Economic analyses should examine how these technologies can support value-based payment models and evaluate how well AI in-terventions correspond with value-based care objectives.
Sensitivity analysis aids in locating essential variables that have a significant im-pact on estimations of cost-effectiveness and ROI. Organizations can improve their understanding of the reliability of their economic evaluation and make better judgements by testing various hypotheses and scenarios.
While initial expenses could be high, long-term advantages like fewer readmis-sions and better patient outcomes can lead to significant savings over time. Strategic planning and decision-making need to balance potential long-term rewards with short-term expenses.
Reduced hospital readmissions can be achieved in large part by providing person-centered or patient-centred care. It is crucial to carefully consider the value of incorporating patients in the development and application of AI technology. It is essential to research methods for fostering patient empowerment, involvement, and collaborative decision-making. We offer suggestions for creating user-friendly AI interfaces, making sure AI applications for readmission reduction are culturally and linguistically sensitive, and addressing health inequities.
By giving clear and intelligible information regarding AI technologies and their role in lowering readmissions, healthcare organizations should place a priority on patient empowerment and education. In order to help patients, make wise decisions and actively engage in their own care, patients should be informed about the advantages, restrictions, and potential hazards of AI interventions. Patient participation and un-derstanding can be facilitated by educational materials, interactive tools, and us-er-friendly interfaces.
Healthcare providers and patients should be able to make decisions together with the help of AI technologies. When creating individualized treatment plans or care strategies, patients should have the chance to share their perspectives, tastes, and objectives. AI technologies may make suggestions based on evidence while taking into account the preferences, values, and unique circumstances of each patient, promoting group decision-making and raising patient happiness.
Establishing systems for gathering patient feedback and incorporating it into the iterative development of AI technologies is something that organizations should do. Patient feedback can be used to pinpoint problem areas, polish algorithms, and increase user experience. Insights from regular feedback surveys, focus groups, or patient ad-visory councils can be extremely helpful in guiding the development and personalization of AI interventions.
Even after a patient leaves the hospital, AI technology can help with ongoing assistance and follow-up care. Patients can adhere to treatment plans, control their conditions, and seek prompt treatments when necessary with remote monitoring tools, virtual consultations, and personalized reminders. Organizations should set up open lines of contact for continuing assistance so that patients can get in touch with them with queries, grievances, or updates.
Strategies for scalability and generalizability must be taken into account for AI technology to have a significant influence on lowering hospital readmissions. Scalability, which enables growth to bigger patient populations or other healthcare venues, should be considered while designing implementations. Considering variations in patient demographics, healthcare infrastructure, and care delivery paradigms, solutions should be adaptive to various contexts. Scalability and generalizability of AI implementations can be facilitated by utilizing cloud-based technologies, modular designs, and interoperable systems.
It is essential to create thorough deployment roadmaps for AI technology in order to reduce hospital readmissions. These roadmaps should list the processes, materials, and timetables needed for an effective adoption. Stakeholder engagement, infrastruc-tural requirements, data gathering and administration, training and education, and as-sessment plans should all be taken into account. Healthcare organizations may develop well-defined implementation roadmaps to ensure a methodical and organized approach to deploying AI technologies.
8. Conclusions
Chronic diseases heavily burden people, healthcare systems, and the economy through increased direct healthcare costs, prolonged expenses, and additional long-term medication and treatment costs. Healthcare professionals, suppliers, and policy-makers have looked to artificial intelligence (AI) as a potential remedy to this problem. AI is a disruptive and transformative technology that can identify disease patterns, predict disease trajectories, and reduce future disease events or functional outcomes, which lowers hospital readmission rates. It can deliver and access accurate health information, increase the effectiveness of health system workflows, and more.
AI offers opportunities to lower readmission rates through early diagnosis, precision medicine, individualized treatment plans, automated and remote monitoring, and addressing poor medication adherence. While biases in training data and algorithmic decisions have all the advantages, the lack of accountability and comprehensibility of erroneous conclusions in AI systems and the potential for unintended implications highlight the importance of carefully evaluating and considering AI limitations. Ethical considerations are crucial for the responsible use of AI to ensure fairness, human autonomy, harm prevention, and explainability principles in lowering hospital readmissions. Frameworks that address these ethical issues and offer solutions must be created. If the ethical problems associated with AI deployment can be resolved, the potential of AI to enhance patient care, lower readmission rates, and lessen the financial burden of chronic diseases could be primarily utilized.
References
- Alluhaidan, A. et al. (2015) 'Designing patient-centered mHealth technology intervention to reduce hospital readmission for heart-failure patients', 2015 48th Hawaii International Conference on System Sciences [Preprint]. [CrossRef]
- RevCycleIntelligence (2019) 3 strategies to reduce hospital readmission rates, costs, RevCycleIntelligence. Available at: https://revcycleintelligence.com/news/3-strategies-to-reduce-hospital-readmission-rates-costs (Accessed: 15 June 2023).
- Philbin, E.F. and DiSalvo, TG (1999) 'Prediction of hospital readmission for heart failure: Development of a simple risk score based on administrative data', Journal of the American College of Cardiology, 33(6), pp. 1560–1566. [CrossRef]
- Bardhan, I. , Chen, H. and Karahanna, E. (no date) 'Connecting systems, data, and people: A multidisciplinary research roadmap for chronic disease management', MIS Quarterly: Management Information Systems, 44(1), pp. 185–200. [CrossRef]
- Zolbanin, H.M. and Delen, D. (2018) 'Processing Electronic Medical Records to improve predictive analytics outcomes for hospital readmissions', Decision Support Systems, 112, pp. 98–110. [CrossRef]
- Upadhyay, S. , Stephenson, A.L. and Smith, D.G. (2019) 'Readmission rates and Their Impact on Hospital Financial Performance: A Study of Washington Hospitals', INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 56, p. 004695801986038. [CrossRef]
- Arbaje, A.I. et al. (2008) 'Post-discharge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries', The Gerontologist, 48(4), pp. 495–504. [CrossRef]
- Press, V.G. , Konetzka, R.T. and White, S.R. (2018) 'Insights about the economic impact of chronic obstructive pulmonary disease readmissions post implementation of the hospital readmission reduction program', Current Opinion in Pulmonary Medicine, 24(2), pp. 138–146. [CrossRef]
- Betancourt JR, Tan-McGrory A, Kenst KS. Guide to Preventing Readmissions among Racially and Ethnically Diverse Medicare Beneficiaries. Prepared by the Disparities Solutions Center, Mongan Institute for Health Policy at Massachusetts General Hospital. Baltimore, MD: Centers for Medicare & Medicaid Services Office of Minority Health; September 2015. (Accessed: 22 June 2023).
- Beil, M. et al. (2019) 'Ethical considerations about Artificial Intelligence for prognostication in Intensive Care', Intensive Care Medicine Experimental, 7(1). [CrossRef]
- Friedman, B. , Jiang, H.J. and Elixhauser, A. (2008a) 'Costly Hospital Readmissions and Complex Chronic Illness', INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 45(4), pp. 408–421. [CrossRef]
- Joynt, K.E. and Jha, A.K. (2012) 'Thirty-day readmissions — truth and consequences', New England Journal of Medicine, 366(15), pp. 1366–1369. [CrossRef]
- Higashi, T. et al. (2007) 'Relationship between number of medical conditions and quality of care', New England Journal of Medicine, 356(24), pp. 2496–2504. [CrossRef]
- Harry, A. (2023) 'The Future of Medicine: Harnessing the Power of AI for Revolutionizing Healthcare', International Journal of Multidisciplinary Sciences and Arts, 2(1), pp. 37–48.
- Zolbanin, H.M. and Delen, D. (2018) 'Processing Electronic Medical Records to improve predictive analytics outcomes for hospital readmissions', Decision Support Systems, 112, pp. 98–110. [CrossRef]
- van Giffen, B. , Herhausen, D. and Fahse, T. (2022) 'Overcoming the pitfalls and perils of algorithms: A classification of machine learning biases and mitigation methods', Journal of Business Research, 144, pp. 93–106. [CrossRef]
- Artificial Intelligence: Examples of ethical dilemmas (no date) UNESCO.org. Available at: https://www.unesco.org/en/artificial-intelligence/recommendation-ethics/cases (Accessed: 27 June 2023).
- Lee, N.T. , Resnick, P. and Barton, G. (2022) Algorithmic bias detection and mitigation: Best practices and policies to reduce consumer harms, Brookings. Available at: https://www.brookings.edu/research/algorithmic-bias-detection-and-mitigation-best-practices-and-policies-to-reduce-consumer-harms/ (Accessed: 27 June 2023).
- Karimian, G. , Petelos, E. and Evers, S.M. (2022) 'The ethical issues of the application of artificial intelligence in Healthcare: A systematic scoping review', AI and Ethics, 2(4), pp. 539–551. [CrossRef]
- Schonberger, D. (2019)' Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications', International Journal of Law and Information Technology [Preprint].
- Anom, B.Y. (2020) 'Ethics of Big Data and Artificial Intelligence in medicine', Ethics, Medicine and Public Health, 15, p. 10 0568. [CrossRef]
- Ahamed, F. , and Farid, F. (2018) 'Applying Internet of Things and Machine-Learning for Personalized Healthcare: Issues and Challenges', International Conference on Machine Learning and Data Engineering (iCMLDE), Sydney, NSW, Australia, 2018, pp. 19-21. [CrossRef]
- Mohanty, S. D. , Lekan, D., McCoy, T. P., Jenkins, M., & Manda, P. (2022). Machine learning for predicting readmission risk among the frail: Explainable AI for healthcare. Patterns, 3(1).
- Arenson, M. , Hogan, J., Xu, L., Lynch, R., Lee, Y. T. H., Choi, J. D.,... & Patzer, R. E. (2023). Predicting Kidney Transplant Recipient Cohorts’ 30-Day Rehospitalization Using Clinical Notes and Electronic Health Care Record Data. Kidney International Reports, 8(3), 489-498.
- Houssein, E. H. , & Sayed, A. ( 2023). Boosted federated learning based on improved Particle Swarm Optimization for healthcare IoT devices. Computers in Biology and Medicine, 107195.
- Quazi, S. (2022). Artificial intelligence and machine learning in precision and genomic medicine. Medical Oncology, 39(8), 120.
- Obuobi, S. , Chua, R. F., Besser, S. A., & Tabit, C. E. (2021). Social determinants of health and hospital readmissions: can the HOSPITAL risk score be improved by the inclusion of social factors?. BMC Health Services Research, 21, 1-8.
- Park, C. , Otobo, E., Ullman, J., Rogers, J., Fasihuddin, F., Garg, S.,... & Atreja, A. (2019). Impact on readmission reduction among heart failure patients using digital health monitoring: feasibility and adoptability study. JMIR medical informatics, 7(4), e13353.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).