Introduction
Gaucher Disease (GD), is probably the most common lysosomal storage disease [
1] and can greatly affect patient’s health-related quality of life. The most severe symptoms include bone pain and persistent tiredness, which can disrupt their ability to attend school, work, and participate in social events. Its etiology is an autosomal recessive mutation causing a defect in the lysosomal enzyme β-glucosidase, leading to the accumulation of the non-degraded glucocerebroside in macrophages, mainly in the reticuloendothelial-system (spleen, liver and bone marrow)
. There are three clinical presentation groups: Type I is an adult chronic form that is non-neuropathic and the most common. Type II is an acute neuronopathic, and the most severe form, type III, is a juvenile sub-acute neuronopathic form [
2]. This differentiation is important, as symptomatic expressions are more common in severe neuronopathic forms of the disease. Bone involvement can occur in any bone, particularly of the proximal and distal femur, proximal tibia, and proximal humerus, and manifest in the form of pathological fractures, vertebral compression fractures and osteolytic lesions [
3,
4]. Osteonecrosis leading to osteoarthritis of large joints is relatively common in GD, with an increased incidence of hip joint osteoarthritis due to avascular necrosis (AVN) of the femoral head [
5]. While the introduction of enzyme replacement therapy (ERT) has led to a substantial reduction in AVN development [
6], adult patients previously diagnosed with Gaucher Disease before Enzyme Replacement Therapy was availability could still develop it while on therapy. Total hip arthroplasty (THA) is occasionally offered for symptomatic patients at younger ages [
7].
Anesthetic management concerns are raised during the pre-anesthesia planning phase due to theoretically higher risks from vital structures deposition. The airway management concerns for anesthesia can have an implication for securing the patient’s airway and oxygenation and are based on
reported respiratory dysfunction, hypoxemia, and altered pulmonary function tests [
8,
9,
10,
11,
12,
13]
, with possible bodily posture affection due to both pre-existing neurological symptoms and to potential adverse reactions to dopaminergic agents [
14]. Hemodynamic stability during anesthesia can be impacted in the presence of cardiac affections, and the presence of valvulopathies and arterial calcification have been reported [
15,
16] and could be fatally progressive. Hematological aspects have an implication in hemodynamic stability and also affect selection of the anesthesia induction technique or special monitoring methods, including higher infection rates, anemia, thrombocytopenia, abnormal platelet aggregation, coagulation factor deficiency, and seen in these patients [
17,
18,
19], leading to concerns for disproportionate or massive bleeding and surgical site infection. These conditions may present difficulties in the consideration of both general (GA) and neuraxial anesthesia (NA), their perceived likelihood of success, and the risk of complications.
A correspondence by Ioscovich et al. described a series of 14 patients that underwent THA. Pulmonary hypertension was seen present in a relatively large percentage (44%) of patients. Five of the operations (21%) were performed with preoperative platelet counts <80 × 103 mm
−3. General anesthesia was provided for fifty-three percent of patients without airway management difficulties. The requirement for blood product transfusion occurred in 68% of surgeries. Although all patients received preoperative antibiotic prophylaxis; postoperative wound infections were reported in thirty seven percent, significantly higher than that reported for the general population at the same institution (2%) and in the medical literature (0.3 – 2%) [
17] . In a series of 32 type I adult Gaucher patients, seven patients (22%) had abnormal platelet aggregation [
20]. Although small sized samples such as retrospective case series and case reports exist, supporting the former anesthesia concerns, comparative studies have yet not been conducted heretofore. We hypothesized that the anesthetic management of patients with Gaucher disease undergoing hip arthroplasty would be more challenging than for non GD patients. The Gaucher Disease Unit is the world’s largest referral center for GD, following more than 900 patients over 3 decades, and it has allowed us to conduct a control-matched
retrospective-cohort study with the purpose to analyze whether difficult anesthesia initiation, intraoperative course, hemodynamic management, and postoperative complications are associated to Gaucher Disease diagnosis.
Methods
Study Design and AIMS
This is a retrospective-cohort study conducted at a tertiary-care academic health center and was approved by the local Research Ethics Board (No. 0007-19-SZMC) on Feb. 26th, 2019. The aim was to evaluate the association between diagnosed Gaucher Disease and difficult anesthetic management, and also the anesthetic and surgical clinical outcomes to guide the professional to tailor his preoperative anesthetic plan safely and to avoid potentially foreseeable complications.
Study Population
This study included all patients with GD, who underwent Total Hip Replacement at a single medical center between March, 1st, 1997 and March, 1st, 2019 to comply with our power analysis requirements. Inclusion criteria were: (1) Elective total hip arthroplasty (primary or revision) ; (2) a confirmed diagnosis of GD [
1] ; (3) age 18 years or older. A concurrent control-group (CG) was created by computer-generated control-matching for the same time period from SZMC’s medical records, using as matching-criteria: age, gender and surgical procedure (primary and revision surgeries were both matched independently).
Sample size and Statistical Analysis
Sample size was based on literature’s reported incidence of difficult anesthetic intraoperative ma
nagement [
21,
22,
23]
. Assuming an incidence of the primary outcome in the CG of approximately 58%, and expecting a 50% increase in the exposure group to 87%, it was estimated that 26 patients in the Gaucher Disease group and 56 in the CG would be required for statistical significance with a type-1 error of less than 0.05, and a power of 0.8, with
an intended matching ratio of 1:2 (two control patients per exposed patient
). Based on the local historical yearly procedures for GD patients
, we expected to find approximately 1-2 THA surgeries for GD patients per year, obtaining approval for data collection for our retrospective review. Two-tailed P-values were used, considering significance as p-value <0.05. Descriptive variables are reported as
frequency (%), and mean±SD. Qualitative variables were analyzed using the chi-sq
uare test or Fisher's exact test. Quantitative variables comparison between the two groups was done by the
parametric t-test for normal distribution data or Mann-Whitney for non-normal distribution data.
Data Collection
Data were extracted from clinical files, including demographic, GD-related data, comorbidities, intraoperative data such as type of surgery and anesthesia, vital signs, perioperative blood products consumption, duration of surgery and anesthesia, and postoperative outcomes such as the incidence of infections, lengths-of-stay in recovery room and in the hospital, and transfer to the intensive care units and mortality.
Outcome Measures:
The primary outcome was the composite requirement-rate of more than one attempt at any-type anesthesia induction technique, including general anesthesia with endotracheal intubation or any-type of neuraxial anesthesia procedure. Secondary outcomes included (1) number of attempts of endotracheal intubation (2) number of attempts of neuraxial anesthesia, (3) volume of intraoperative crystalloids and colloids infused, (4) mean intraoperative change in hemoglobin and platelet levels, (5) use of invasive monitoring such as intra-arterial blood pressure or central venous pressure measurements (6) duration of surgery and anesthesia, (7) perioperative blood products transfusion incidence and volume (8) prolonged length-of-stay in recovery room, (9) intensive care unit (ICU) transfer, (10) prolonged length-of-stay in hospital, (11) postoperative prolonged antibiotic treatment beyond a single prophylactic dose, (12) thromboembolic events incidence (13) 30-day in-hospital all-cause mortality rate
Results
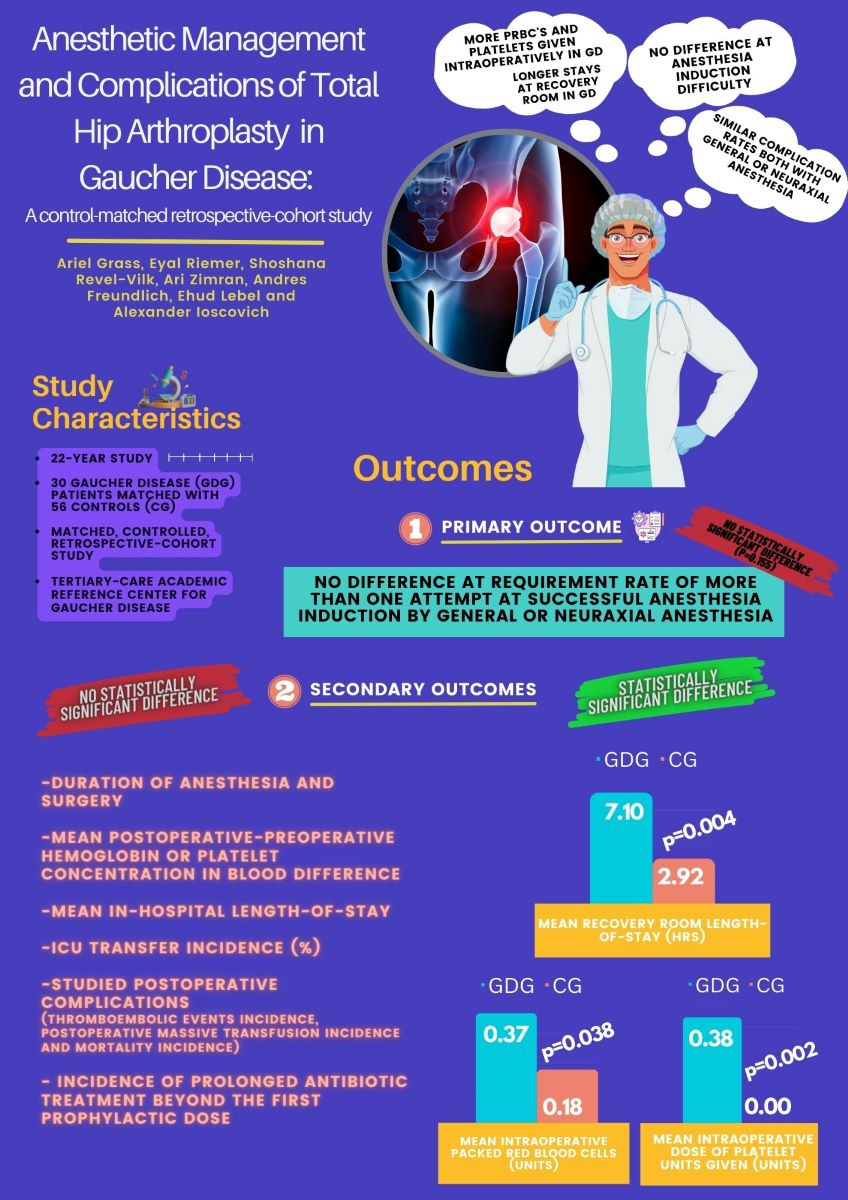
A total of 30 patients with Gaucher Disease and 56 matched controls were identified meeting the inclusion criteria over a 22-year period. Although Total Hip Replacement being uncommon in young non-GD patients (CG), matching quality was deemed satisfactory, with a final matching ratio of 1:1.87 attained, maintaining an age-similarity matching criteria of maximum 15 years instead of increasing the maximum allowed age difference with the CG.
Patient and Clinical Characteristics
The age, sex, weight, body mass index, primary-to-revision THA, type of
anesthesia, preoperative hemoglobin level and platelet counts were similar in both groups (
Table 1). The most frequent GD mutations were N370S/N370S (the most common and milder genotype among patients with type 1 GD presented in 16/28 [57.1%]), while none had a neuronopathic (type-3) diagnosis.
Anesthesia Induction
For the primary outcome, requirement-rate of more than one attempt at any-type anesthesia techniques was not significantly different between both groups, having occurred in one patient with GD (3.3%) and 9 controls (16.1%) ; (p=0.155), neither the total num
ber of any-type anesthesia attempts, 1.03 vs 1.16 respectively. The independent incidences of requiring more than one attempt at endotracheal intubation or neuraxial anesthesia were neither different (
(1.0 vs 1.0) ; (p= 1.000) and (5.6% vs 12.2%) ; (p= 0.656) respectively).
Both the decision to use invasive monitoring techniques, and the selection of neuraxial over general anesthesia were not significantly different in the Gaucher Disease
group for the study period (Table 2)
Surgical and Hemodynamic Management
Both duration of anesthesia and duration of surgery were longer in the GD group, however, these were not significantly different. Platelet transfusion occurred intraoperatively in significantly more cases in the GD group, presenting in 5 patients (16.7%), and in none of the CG (p=0.004). Accordingly, the mean intraoperative dose of platelet units given (U) was higher as well (0.38 vs 0.0) ; p=0.002)). There were no differences in the mean postoperative-preoperative hemoglobin difference, platelet levels, or the amounts of crystalloids or colloids given. Although the intraoperative transfusion incidence of packed Red Blood Cells (pRBC) was higher in patients with GD (26.7%) than in CG patients (10.7%), this was not significant. Nevertheless, there was a significantly higher mean amount of packed Red Blood Cells units given intraoperatively to the GD group vs the CG (0.37 vs 0.18) ; (p=0.038)). Intraoperative change in hemoglobin and platelet levels were not significantly different. Additional intraoperative data can be seen in
Table 3.
Postoperative Complications
Mean Recovery Room length-of-stay was significantly longer in the Gaucher group (426 vs 175 mins; p=0.004), but the mean in-hospital length-of-stay and the incidence of transfer to the Intensive Care Unit (%) were similar. The incidence of postoperative platelets administration was significantly higher in the Gaucher Disease group (3/30 [10%] vs 0/56 [0%]; p=0.040) with a mean amount of platelets transfused significantly higher as well (0.87 ± 4.38 (0-24) vs 0 ± 0.00 (0-0) ; p=0.017). The incidence of postoperativ
e requirements of
packed Red Blood Cells was lower in the GD group but not statistically significant, while the mean number of units given were similar in both groups. For the studied postoperative complications, the thromboembolic events incidence, postoperative
massive transfusion incidence and mortality incidence were non-significantly different between the GD group and the CG. Similarly, the incidence of prolonged antibiotic treatment beyond the first prophylactic dose was not significantly different. Additional statistical data are presented in
Table 4.
Discussion
To our knowledge this study is the first large control-matched retrospective-cohort study during a long observation period of 22-years, addressing anesthetic induction success, intraoperative management, and complications in the GD population undergoing THA.
Anesthetic Technique
The current study evaluated challenges of anesthesia for patients with Gaucher Disease as compared to those not affected by Gaucher Disease, while undergoing hip joint arthroplasty.
This study’s findings come to reinforce previous literature reports[
24]
, neither finding a
significant difference in the composite primary outcome, on the difficulty to succeed at a first initiation attempt of anesthesia by either endotracheal intubation or neuraxial anesthesia versus the control-group, nor on each technique’s independent analysis. Gaucher Disease patients who underwent the procedure under general anesthesia did not present greater difficulty in ventilating and establishing a secure airway with an endotracheal tube than control patients, and no patient required more than one intubation attempt. Although the theoretical concern of anesthetic induction and maintenance conditions being affected by Glucosylceramide deposits and the presence of neurological signs, no particular preference by staff anesthetists for GA or any neuraxial technique was found for the study period.
First, these results contrast airway concerns based on priorly reported presence of neurological symptoms in these patients such as trismus and opisthotonic posturing, limb stiffness, bulbar signs, convulsions [
14], the theoretical concerns of upper airway glycolipid pharyngolaryngeal infiltration, and of lower safe-apnea time due to reported lung pathology in the form of interstitial lung disease and hepatopulmonary Syndrome [
25,
26], and ventilatory reserve affection from reductions in functional residual capacity, total lung capacity, and alveolar-capillary diffusion abnormality [
8]. Second, the authors acknowledge the potential of bias in this airway management finding due to the documentation method used at this center, since the anesthetic chart requests marking the field "Difficulty at endotracheal intubation?". If present, marking omissions could possibly mean either a negative response or rather the lack of documentation of this finding. It was chosen to assume a lack of marking as a lack of difficulty, i.e. as success in a single attempt, considering in our center documentation of difficult intubation is commonly registered when present. Additional difficult intubations not reported cannot be ruled out, while this would apply to both study groups. In patients in whom neuraxial anesthesia was performed, no significant difference could be seen in the number of attempts. In the Gaucher group, there was only one patient (0.03%) who required more than one attempt, compared to five patients (0.09%) in the CG. Those findings suggest that airway and spine conditions might not significantly impact anesthetic success, supported by the lack of association to perioperative anesthetic complications. This could be interpreted
as a lack of significant Glucosylceramide deposition in glottic/supraglottic soft tissues and those superficial to the lumbar spine if existent. A second possibility could be meticulous anesthesiologist preparation. The same is true for neuraxial anesthesia (NXA) as an expected difficulty in performing neuraxial anesthesia due to osteopathological changes, the suspicion of an increased risk of bleeding and postprocedural epidural hematoma development in the context of a suspected coagulation abnormality could be worrisome and deterring to anesthetists. Additionally, the potential affection of accessory muscles that neuraxial anesthesia can occasionally cause when reaching higher spinal nerves blockage under a possible reduced respiratory reserve could cause apprehension. These factors, however, did not seem to affect the clinical decision to perform NXA, nor technical difficulty or complications.
In both cases, this suggests that a higher index of suspicion for anesthesia complications may not be particularly required. One should consider these findings cautiously, specifically the retrospective nature of the study. Prospective studies may substantiate these findings, although this might be difficult while considering the paucity of this illness. As for the secondary outcomes, the duration of anesthesia was not significantly longer among Gaucher patients. Although this study did not analyze specific intraoperative oxygenation or mechanical ventilation parameters, it did not find an association between Gaucher Disease and postoperative pulmonary complications, nor with other significant complications.
Blood Products
Due to a lack of GD-specific intraoperative blood transfusion guidelines, the decision to administer packed Red Blood Cells was taken by treating anesthesiologists according to the same criteria used for any patient without GD based on his professional criteria. The packed Red Blood Cell intraoperative transfused amount was significantly higher in the GD group while postoperatively was not significantly lower. Intraoperatively, approximately 1-in-4 GD patients received packed Red Blood Cells in contrast to approximately 1 in 10 in the CG (p-value : 0.07). Postoperatively this was inverted, with approximately 1 in 4 Gaucher patients receiving packed Red Blood Cells during their recovery room stay, compared with approximately 1-in-2 control patients. An average of 0.57 ± 1.22 units were given postoperatively per Gaucher Disease patient, compared with an average of 0.88 ± 1.48 per control patient (p = 0.133). Among possible reasons for this contrasting finding, the simpler explanation might be the better hemodynamic optimization of GD patients from higher intraoperative administration, therefore, leaving them more properly compensated postoperatively than the control group. Unfortunately, blood loss data collection for the study period was challenging from imprecise blood loss documentation narrowing further contextualization. Another alternative explanation proposed is a more defensive approach by the anesthesia staff, from bleeding concerns related to the disease, thus lowering the threshold for packed Red Blood Cell administration in GD patients compared with a more conservative approach with control patients. That is, pRBCs being given to GD patients for milder bleeding, as opposed to control patients, in which a more conservative approach would have been practiced, waiting for more extensive bleeding prior to deciding on the administration. Such a theory could explain the reversal of this trend, with control patients needing more blood products postoperatively than GD patients. In addition, it can be seen that there was one patient in the study group and two patients in the control group who were subjected to a massive blood transfusion protocol, defined as the requirement of 5 or more packed Red Blood Cell units, not meeting statistical significance. To date, no work has been described in literature reviewing specific intraoperative massive blood transfusion criteria for Gaucher Disease patients. Platelet doses were given exclusively to Gaucher patients, thus this finding was statistically significant for the study group. These results are consistent with the reported hematological manifestations of GD: lower levels of coagulation factors, hypersplenism with consequent thrombocytopenia, and impaired platelet function as potential contributors to increased surgical blood loss. It should be noted that most of these patients had a preliminary platelet administration protocol designated by the hematologist following their GD management, which was delivered in writing to the anesthesia staff from the Gaucher clinic ahead of time.
Extended Antibiotic Coverage
All patients received prophylactic antibiotic therapy as is conventional for these surgeries [
27]. Patients for whom antibiotic therapy was prolonged more than the conventional first prophylactic dose, or alternatively for whom antibiotic therapy was reinitiated later in their hospitalization, were flagged as having received prolonged antibiotic therapy. Gaucher patients had almost double the therapy period than the CG, almost reaching significance (P-value:0.063). Allegedly, two possible explanations could be raised for this finding: First, a more cautious approach in light of the suspected increased infection risk (especially in splenectomized patients), and second, the postoperative diagnosis of an infectious process (such as pneumonia). Patient's chart data supports that the prolongation of antibiotic treatment was mostly associated with the presence of signs of infection (eg. fever, and surgical wound findings), making the second explanation more plausible.
Other Findings
The most common genotype observed was N370S/N370S, which is consistent with literature. While typically clinically milder, due to its high frequency, most patients presenting with severe manifestations do belong to this group, being under-represented. In this study, none of the patients in the GD group that presented AVN and underwent THA had neuronopathic type-3- Gaucher Disease. It is worth noting that the profile of patients presenting with AVN before and after the Enzime Replacement Therapy initiation era could differ in the future. Recovery room length-of-stay was significantly longer in GD patients. (mean. Diff : 251 mins.). These patients may have required prolonged care for a justified clinical reason, or rather a cautious approach was likely taken with GD patients by recovery room staff for longer monitoring time from concerns for postoperative complications even in the absence of a particular clinical condition requiring a specific treatment. There may be room for further research into the causes of this increased delay in the GD group.
Limitations of This Study
The study limitations are its retrospective nature, the impossibility of concluding causation, and the low number of patients that could be included in the Gaucher Disease group being an infrequent disease, and too in the CG with the selected matching criteria. Being that age was matched, we are aware that an early age CG might not be representative of the more common daily practice older Total Hip Replacement cohort commonly due to osteoarthritis alone, with the selected younger comparator group probably being potentially affected by additional unknown confounders. These could lead to more or less differences than if compared with older populations and needs to be considered. Further studies are required to confirm these results. While prospective studies are required, Gaucher Disease's rarity however would significantly limit such possibility.
Conclusions
This observational control-matched cohort-study did not demonstrate an association with the rate of difficult anesthesia induction nor a significantly higher risk of complications, suggesting that GD patients can safely undergo either GA or Neuraxial Anesthesia for Hip Joint Arthroplasty. There was an association to the Gaucher Disease group of higher intraoperative packed red blood cell administration, an increased incidence of platelet transfusion both intraoperatively and postoperatively, and also a longer mean recovery room length of stay. The ideal preoperative, intraoperative and postoperative transfusion criteria remains to be defined in this population. It might be prudent for anesthesiologists whenever possible to assess a patient's coagulation status and blood coagulation tests preoperatively. Preoperative parameters can be improved through optimal ERT therapy and specialist management, and referring GD patients to a specialized center, can provide significant value in optimizing them before anesthesia and surgical procedures.
Cover Letter
Anesthetic management and complications of Total Hip Arthroplasty in Gaucher Disease: A control-matched retrospective-cohort study.
Author Contributions
All authors had full access to the data in the study, are in agreement with the content of the manuscript and take responsibility for the integrity of the data and the accuracy of the data analysis. The content has not been published or submitted for publication elsewhere. All authors have contributed significantly: Conceptualization, A.G. and A.I.; Methodology, A.G., E.R., E.L., S.R., A.Z., A.I.; Investigation, E.R.; Formal Analysis, E.R.; Resources, A.G. and E.R.; Data Curation, E.R.; Writing - Original Draft, A.G. and E.R.; Writing - Review & Editing, A.G., S.R., A.Z., A.F., E.L., A.I.; Visualization, A.G. and A.F.; Supervision, A.I.; Project Administration, A.G. Accountability: Agreement to be accountable for the article and to ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved: A.G., E.R., A.Z., S.R., A.F., E.L., A.I.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
This retrospective-cohort study was conducted at a tertiary-care academic health center and was approved by the local Research Ethics Board (No. 0007-19-SZMC).
Acknowledgements
No sources of support were involved in the development of this work and manuscript.
Conflicts of Interest
Ariel Grass, Eyal Riemer, Shoshana Revel-Vilk, Ari Zimran, Andres Freundlich, Ehud Lebel and Alexander Ioscovich declared no financial support or relationships that may pose conflict of interest with this manuscript. The authors declare no conflict of interest in relation to the manuscript.
Authorship Declaration
All authors meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and are in agreement with the manuscript
References
- Revel-Vilk S, Szer J and Zimran A: Gaucher disease and related lysosomal storage diseases. In: Williams Hematology. Kaushansky K, Lichtman M, Prchal J, et al. (eds.) McGraw-Hill, New York, 2021.
- Rosai J, Ackerman LV. Rosai and Ackerman’s surgical pathology Vol. 2. Vol. 2. Edinburgh [etc.: Mosby Elsevier; 2011.
- Grabowski GA, Andria G, Baldellou A, et al. Pediatric non-neuronopathic Gaucher disease: presentation, diagnosis and assessment. Consensus statements. Eur J Pediatr. 2004 Feb;163(2):58-66. Epub 2003 Dec 16. [CrossRef] [PubMed]
- Montfort M, Chabás A, Vilageliu L, Grinberg D. Functional analysis of 13 mutant alleles identified in Gaucher disease patients: Pathogenic changes and “modifier” polymorphisms. Human Mutation 2005 ; 26: 276. [CrossRef]
- Oliveri, B., González, D., Quiroga, F., Silva, C.,. Rozenfeld, P.. A Comprehensive Study of Bone Manifestations in Adult Gaucher Disease Type 1 Patients in Argentina. Calcif Tissue Int 104, 650–657 (2019). https://doi-org.szmc.idm.oclc.org/10.1007/s00223-019-00536-x.
- Pastores GM, Elstein D, Hrebícek M, Zimran A. Effect of miglustat on bone disease in adults with type 1 Gaucher disease: a pooled analysis of three multinational, open-label studies. Clin Ther. 2007 Aug;29(8):1645-54. [CrossRef] [PubMed]
- Johannson HR, Zywiel MG, Marker DR, Jones LC, McGrath MS, Mont MA. Osteonecrosis is not a predictor of poor outcomes in primary total hip arthroplasty: a systematic literature review. Int Orthop. 2011 Apr;35(4):465-73. Epub 2010 Feb 25. PMID: 20182877; PMCID: PMC3066310. [CrossRef]
- Kerem E, Elstein D, Abrahamov A, et al. Pulmonary function abnormalities in type I Gaucher disease. Eur Respir J. 1996 Feb;9(2):340–345. [CrossRef] [PubMed]
- Elstein D, Klutstein MW, Lahad A, Abrahamov A, Hadas-Halpern I, Zimran A. Echocardiographic assessment of pulmonary hypertension in Gaucher’s disease. Lancet. 1998 May 23;351(9115):1544–1546. PMID: 10326537. [CrossRef]
- Balwani M, Fuerstman L, Kornreich R, Edelmann L, Desnick RJ. Type 1 Gaucher disease: significant disease manifestations in "asymptomatic" homozygotes. Arch Intern Med. 2010 Sep 13;170(16):1463-9. Erratum in: Arch Intern Med. 2010 Nov 8;170(20):1833. PMID: 20837833; PMCID: PMC3098047. [CrossRef]
- Kita T, Kitamura S, Takeda K, Fukumitsu K, Kinouchi K. [Anesthetic management involving difficult intubation in a child with Gaucher disease]. Masui. 1998 Jan;47(1):69–73. PMID: 9492502.
- Goitein O, Elstein D, Abrahamov A, et al. Lung involvement and enzyme replacement therapy in Gaucher’s disease. QJM. 2001 Aug;94(8):407–415. [CrossRef] [PubMed]
- Miller A, Brown LK, Pastores GM, Desnick RJ. Pulmonary involvement in type 1 gaucher disease: Functional and exercise findings in patients with and without clinical interstitial lung disease. Clinical Genetics 2003 ; 63: 368–76. [CrossRef]
- Goker-Alpan O, Schiffmann R, LaMarca M, Nussbaum R, McInerney-Leo A, Sidransky E. Parkinsonism among Gaucher disease carriers. J Med Genet. 2004 Dec;41(12):937–940. PMCID: PMC1735652. [CrossRef]
- Talluto CJ, Silverman NH. Aortic and mitral valve stenosis with regurgitation: not due to rheumatic heart disease. Echocardiography. 2011 Feb;28(2):E24-7. Epub 2010 Aug 17. [CrossRef] [PubMed]
- Perić Z, Kardum-Skelin I, Puskarić BJ, Letilović T, Vrhovac R, Jaksić B. An unusual presentation of Gaucher’s disease: aortic valve fibrosis in a patient homozygous for a rare G377S mutation. Coll Antropol. 2010 Mar;34(1):275–278. PMID: 20432762.
- Ioscovich A, Briskin A, Lebel E, et al. Anaesthesia for total hip replacement in Gaucher’s disease. Eur J Anaesthesiol. 2006 Mar;23(3):265–266. [CrossRef] [PubMed]
- Gillis S, Hyam E, Abrahamov A, Elstein D, Zimran A. Platelet function abnormalities in Gaucher disease patients. Am J Hematol. 1999 Jun;61(2):103–106. PMID: 10367788.
- Deghady A, Marzouk I, El-Shayeb A, Wali Y. Coagulation abnormalities in type 1 Gaucher disease in children. Pediatr Hematol Oncol. 2006 Jul-Aug;23(5):411-7. Department of Clinical Pathology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt. [CrossRef]
- Simo-Moyo J, Ducloy JC, Theeten G, Ducloy AS, Krivosic-Horber R, Monnier JC, Dufour P, Plantier I. Prise en charge anesthésiologique d'une femme enceinte atteinte d'une maladie de Gaucher de type I. A propos d'un cas [Anesthetic management of a pregnant woman with type I Gaucher's disease. Apropos of a case]. Cah Anesthesiol. 1994;42(2):169-72. French. [PubMed]
- Taboada M, Doldan P, Calvo A, et al. Comparison of tracheal intubation conditions in operating room and Intensive Care Unit. Anesthesiology. 2018;129(2):321-328. [CrossRef]
- Sidiropoulou, T., Christodoulaki, K. and Siristatidis, C., 2021. Pre-Procedural Lumbar Neuraxial Ultrasound—A Systematic Review of Randomized Controlled Trials and Meta-Analysis. Healthcare, 9(4), p.479. [CrossRef]
- Chin, K., Perlas, A., Chan, V., Brown-Shreves, D., Koshkin, A. and Vaishnav, V., 2011. Ultrasound Imaging Facilitates Spinal Anesthesia in Adults with Difficult Surface Anatomic Landmarks. Anesthesiology, 115(1), pp.94-101. [CrossRef]
- Ioscovich A, Elstein Y, Halpern S, Vatashsky E, Grisaru-Granovsky S, Elstein D. Anesthesia for obstetric patients with Gaucher disease: survey and review. Int J Obstet Anesth. 2004 Oct;13(4):244–250. [CrossRef] [PubMed]
- Balwani M, Fuerstman L, Kornreich R, Edelmann L, Desnick RJ. Type 1 Gaucher disease: significant disease manifestations in "asymptomatic" homozygotes. Arch Intern Med. 2010 Sep 13;170(16):1463-9. Erratum in: Arch Intern Med. 2010 Nov 8;170(20):1833. PMID: 20837833; PMCID: PMC3098047. [CrossRef]
- Elstein D, Klutstein MW, Lahad A, Abrahamov A, Hadas-Halpern I, Zimran A. Echocardiographic assessment of pulmonary hypertension in Gaucher’s disease. Lancet. 1998 May 23;351(9115):1544–1546. PMID: 10326537. [CrossRef]
- Gradl G, Horn C, Postl LK, Miethke T, Gollwitzer H. Antibiotische Infektionsprophylaxe in der Primär- und Revisionsendoprothetik der Hüfte: Was ist erwiesen? [Antibiotic prophylaxis in primary and revision hip arthroplasty: what is the evidence?]. Orthopade. 2011 Jun;40(6):520-7. German. [CrossRef] [PubMed]
Table 1.
Characteristics of the research groups
Table 1.
Characteristics of the research groups
| |
Gaucher (n=30) |
Control (n=56) |
P-Value |
|
Age (№ ± SD [range]) |
48.2 ± 12.96 (17-67) |
49.93 ± 12.32 (24-68) |
0.544 |
|
Women/Men (№ [%]) |
13 [43%] /17 [57%] |
26 [46%] (30 [54%]) |
0.365 |
|
Weight (№ ± SD [range]) |
73.38 ± 11.26 (41-90) |
77.89 ± 16.9 (49-120) |
0.230
|
|
Body Mass Index (№ ± SD [range]) |
27.04 ± 2.52 (22.40 - 31.23) |
31.61± 6.78 (23.56 - 42.25) |
0.085 |
| History of AVN |
25 of 30 [83.3%] |
10 of 55 [18.2%] |
0.001 |
| Primary/Revision |
20 [67%] /10 [33%] |
41 [73%] / (15 [27%]) |
0.524 |
|
Preoperative Hemoglobin levels (№ ± SD [range]) |
13.03 ± 1.98 (6.9-16.2) |
13.23 ± 1.84 (7.7-18) |
0.661 |
|
Preoperative Platelet counts (№ ± SD [range]) |
219750 ± 134283.96
(21000-679000) |
262060.71 ± 117820.58
(149000-1011000) |
0.144 |
Table 2.
Types of anesthesia and invasive monitoring used
Table 2.
Types of anesthesia and invasive monitoring used
| |
All patients
(n = 86) |
Gaucher
(n = 30) |
Control
(n = 56) |
p-Value |
| Arterial line used. № (%) |
5 (5.8%) |
2 (6.7%) |
3 (5.4%) |
1.00 |
| Central venous line access used. № (%) |
2 (2.3%) |
2 (6.7%) |
0 (0.0%) |
0.119 |
| Performance of any Neuraxial Anesthesia technique. № (%) |
58 (68%) |
18 (60%) |
40 (71.4%) |
0.576 |
Table 3.
Intraoperative data: Duration, crystalloids blood products usage, and laboratory results.
Table 3.
Intraoperative data: Duration, crystalloids blood products usage, and laboratory results.
| |
Gaucher (n = 30) |
Control (n = 56) |
P-Value |
| Duration of anesthesia (mins ± SD ) |
180 ± 80 |
160 ± 55 |
0.230 |
|
Duration of surgery (mins ± SD) |
141 ± 76
|
120 ± 49
|
0.171 |
| Mean Crystalloids given (mL ± SD [range])) |
2350 ± 1328.92 [0,
5000]
|
2261.11 ± 966.5 [600, 4500] |
0.749 |
| Mean Colloids given (mL ± SD [range])) |
444.44 ± 481.69 [0,
1500]
|
700 ± 388.06 [500,
1800]
|
0.089 |
| Intraoperative massive transfusion incidence (%) |
3.3% (1/30) |
0% (0/56) |
0.349 |
| Intraoperative pRBC transfusion incidence (%) |
26.7% (8/30) |
10.7% (6/56) |
0.070 |
| Intraoperative mean pRBC units given (№ ± SD [range])) |
0.37 ± 1.39 [0, 5] |
0.18 ± 0.54 [0, 2] |
0.038 |
| Mean Hemoglobin change, Preoperative-Postoperative (g/dL ± SD [range])) |
-2.49 ± 1.69 [-4.9, 2.4] |
-2.58 ± 1.50 [-6.5, 1.2] |
0.794 |
| Intraoperative platelets transfusion Incidence (%) |
16.7% (5/30) |
0.0% (0/56) |
0.004 |
| Intraoperative mean platelet units given (U ± SD [range])) |
0.38 ± 2.9 (0, 12) |
0.0 ± 0.0 (0, 0) |
0.002 |
| Mean Platelet change Preoperative-Postoperative (u/uL ± SD [range])) |
-29773.37 ± 73366.01
[-216000, 169000]
|
-24150 ± 68826.07
[-245000, 202000]
|
0.734 |
Table 4.
Postoperative outcomes and complications.
Table 4.
Postoperative outcomes and complications.
| |
Gaucher (n = 30) |
Control (n = 56) |
P-Value |
| Mean Recovery Room Length of stay (mins ± SD [range])) |
426 ± 412 [70, 1185] |
175 ± 140 [0 - 1020] |
0.004 |
| Mean Hospital length of stay (days ± SD [range])) |
9.97 ± 3.61 [4, 19] |
11.75 ± 11.76 [4, 71] |
0.449 |
|
PACU Morphine dose given (mg ± SD [range]) |
11.79 ± 3.82 [8 - 20] |
11.68 ± 4.68 [4, 20] |
0.929 |
| Incidence of Transfer to ICU (%) |
6.7% (2/30) |
1.8% (1/56) |
0.278 |
| Incidence of a Thromboembolic event (%) |
6.7% (2/30 ) |
0.0% (0/56 ) |
0.119 |
| Mortality (%) |
0% (0/30) |
0% (0/56) |
1.000 |
| Postoperative massive transfusion incidence (%) |
3.3% (1/30) |
3.6% (2/56) |
1.000 |
| Postoperative pRBC administration incidence (%) |
23.3% (7/30) |
42.9% (24/56) |
0.072 |
| Postoperatively mean pRBC units given (№ ± SD [range]) |
0.57 ± 1.22 [0, 5] |
0.88 ± 1.48 [0, 8] |
0.133 |
| Postoperative platelets administration incidence (%) |
10% (3/30) |
0% (0/56) |
0.040 |
| Postoperative mean platelets units given (№) |
0.87 |
0.00 |
0.017 |
| Incidence of prolonged antibiotic treatment beyond a single prophylactic dose (%) |
46.7% (14/30) |
26.8% (15/56) |
0.063 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).