2. Materials and Methods
Medical records of all cats and dogs diagnosed with partial colonic agenesis between January 2016 and May 2022 at the Veterinary Teaching Hospital of Alfort, Paris, France, were retrospectively searched from the database. Inclusion criteria was presence of a short colon diagnosed using contrast radiography, ultrasonography, endoscopy, or a combination of these modalities.
Partial colonic agenesis was defined as a colon length below 20 cm for cats, measured during colonoscopy or on positive contrast abdominal radiographs. In dogs, there is an extreme variability in body weight and size that affects the colon length with values ranging from 30 cm in dogs weighing 5 kg to 99 cm in dogs weighing 60 kg [
13,
14]. As such, a threshold of 25 cm was defined for smaller dogs (between 8 and 14 kg, 2 cases) and 45 cm for larger dogs (between 15 and 30 kg, 3 cases). We did not record dogs heavier than 30 kg in this study. Two cases with an extremely short colon on abdominal ultrasound did not have endoscopy performed yet were also included (one cat and one dog). Information was collected regarding signalment, clinical signs, age at presentation, clinical signs duration, diagnostic tests, treatments, and outcome. Hematologic data (scil Vet abc, IDEXX ProCyte Dx), serum biochemical analysis (Scil VetScan, IDEXX catalyst), electrolytes, B9 and B12 vitamin profile and stool analysis from patients at presentation or at the referring veterinarian were assessed. Abdominal ultrasonography, abdominal radiographs and endoscopic images were reviewed. Abdominal ultrasonography was performed with an Affinity 70, Phillips Medical System, using both microconvex and linear probes. Normal ranges for ultrasonographic measures were defined according to the current literature [
15,
16,
17] ; among others, colonic wall was considered thickened above 1.5 mm for dogs and cats and lymph nodes were considered enlarged over 5 mm for dogs and 4 mm for cats. Subjective assessment based on lymph nodes echogenicity and shape was also taken into consideration for equivocal cases. Endoscopic evaluation was performed with an Olympus Evis Exera III Gif-h190 gastrointestinal videoscope and according to the WSAVA endoscopic recommendations [
18]. At least 6 colonic biopsies were performed. Histological specimen were also evaluated according to the WSAVA criteria [
18]. Medical treatment and outcomes were compared when available. The ratio between the duration of clinical signs (in months) and the age (in months) was calculated. A ratio over 0.75 was considered consistent with clinical signs lasting since the adoption (referred thereafter as
group A), whereas a ratio below 0.5 was considered to represent emerging clinical signs (referred thereafter as
group B). Cases for which no primary colonic lesion but the partial colonic agenesis was detected were described together as
subgroup C (see below).
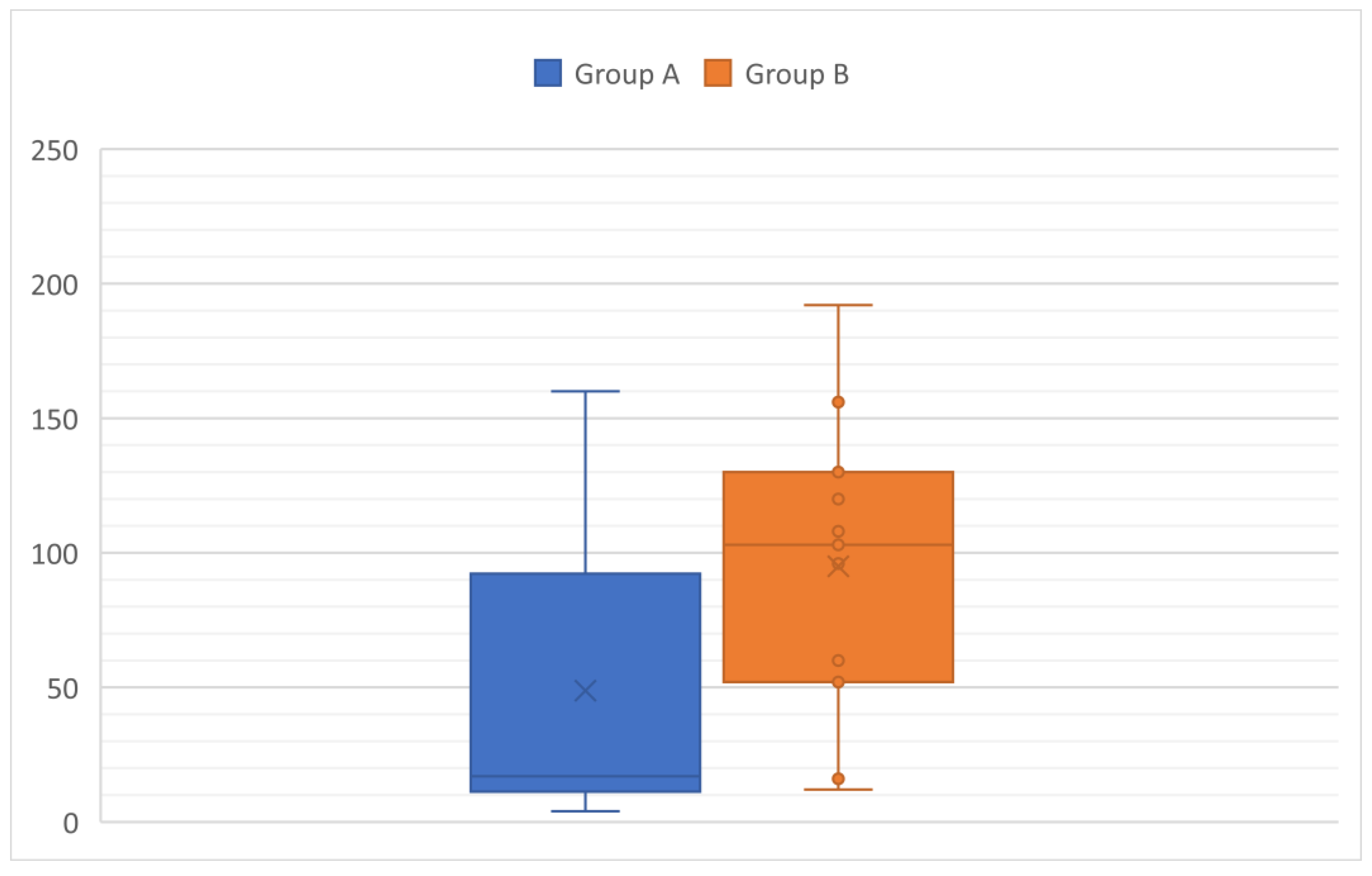
Data were expressed by standard descriptive statistics and presented as mean or median and range (minimum-maximum). The student’s t-test was used to compare age between group A and B. Categorial variables were compared among groups using the chi-squared test. Each of which initially included variables that were significant at P < .05 in simple logistic regression. Statistical analyses were performed using available statistical software (BiostatGV).
4. Discussion
To the authors’ knowledge, this is the first study describing congenital partial colonic agenesis in a cohort of dogs and cats. In this study, there was no sex predisposition and too few cases to detect breed overrepresentation. However, cats included in the Group C were mostly purebreed cats.
In terms of frequency, clinical signs included diarrhea, hematochezia, weight loss or failure to thrive, vomiting, mucoid stools, dyschezia and dysorexia. No clinical signs nor specific associations of clinical signs were found to be specific in the diagnosis of a partial colonic agenesis. Likewise, CBC, biochemistry and electrolytes were non-specific. Mild anemia, monocytosis and mild neutrophilia were occasionally present and likely secondary to chronic inflammation. Five cases had mild eosinophilia that was not explained by parasitism or by an eosinophilic infiltrate in the colon. Biochemical abnormalities were seldom. Apart from 1 dog that had panhypoproteinemia due to PLE, all biochemical abnormalities remained mild and were considered non-specific (chronic inflammation, dehydration, suspected reactive hepatitis) in the context of gastro-intestinal disease. Cobalamin and folic acid abnormalities were variable and could not be predictive of a partial colonic agenesis or of any group. No association was found between hypocobalaminemia and ileocolic valve malformation. One cat had low TLI consistent with exocrine pancreatic insufficiency (EPI). In this case, EPI did not seem to explain the dyschezia [
19], therefore motivating colonoscopy that led to the diagnosis of partial colonic agenesis.
Abdominal ultrasonography seems to be a useful tool in the diagnosis of partial colonic agenesis, leading to the diagnosis in 14 of 17 cats. However, diagnosis of partial colonic agenesis was more challenging in dogs because abdominal ultrasonography identified it in only 1 case, suggesting a lack of sensitivity of this modality for diagnosing this disease in dogs. This apparent discrepancy can be explained by the position of the ileocecocolic junction is an indicator of the colon size and that it can be challenging to localize in dogs. The ileocolic junction and the cecum are typically located to the right of the midline, along with the duodenum [
20]. This localization might be modified in case of partial colonic agenesis. On canine abdominal ultrasound, the junction can be challenging to identify because the cecum is most commonly gas-filled. On the contrary, in cats, it can be more easily recognized [
15]. Thus, an abnormal position of the ileocolic junction in association with a subjective short colon length might be more easily recognized in feline cases and increases the suspicion of partial colonic agenesis. Unfortunately, due to the retrospective nature of the study, the imaging criteria that led the radiologist to suspect a short colon were not available. Thickening of the colonic wall and local adenomegaly were seen in 17 and 14 cases of 22, respectively, but are unspecific findings in cases of colic diarrhea. Few cases had other abdominal ultrasound abnormalities outside of the colon or associated lymph nodes and were more common in group B (12/16 in group B). They may thus by secondary to a concomitant disease.
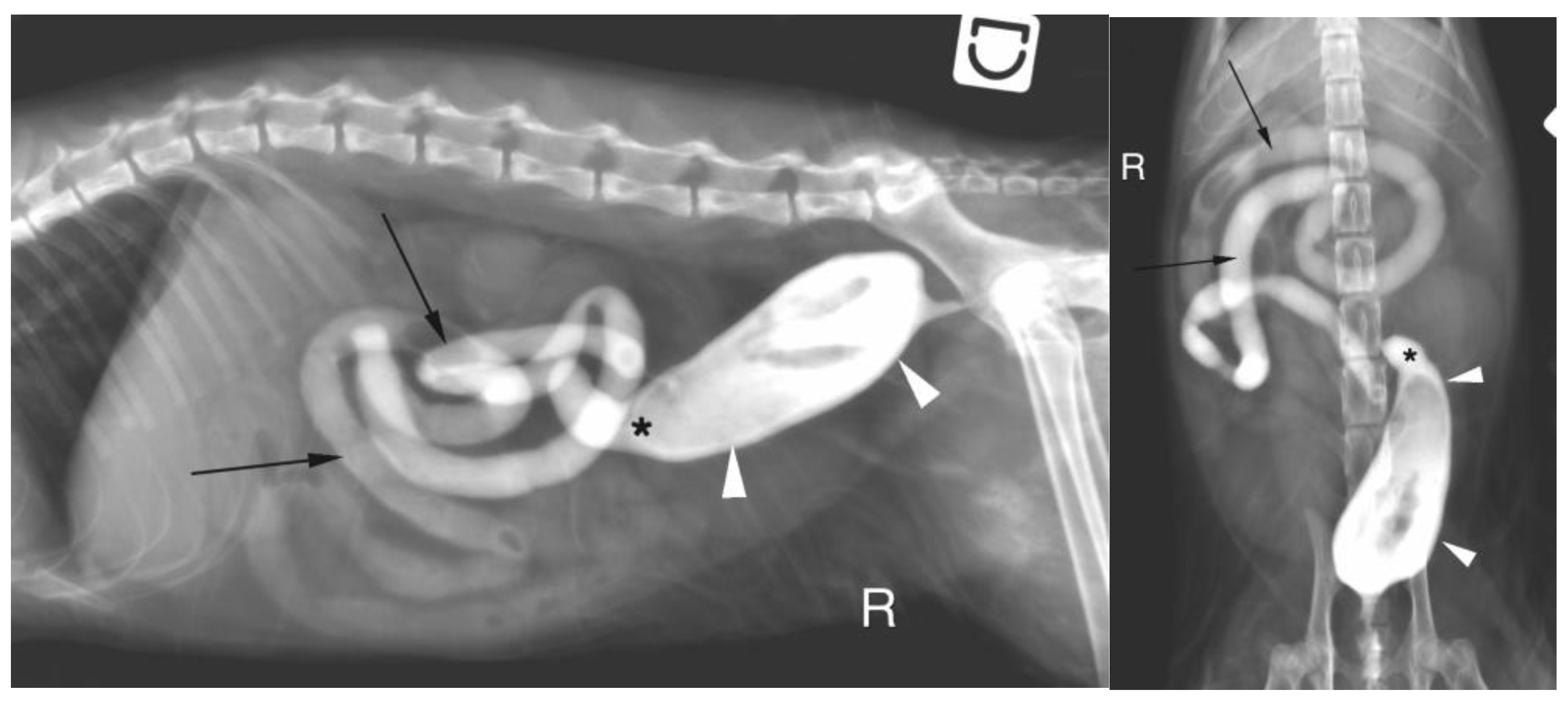
Abdominal radiography was performed in few cases and raised the suspicion of partial colonic agenesis in only half of them. This difference might be due to the difficulty in identifying the oral part of the colon on abdominal radiograph because its filling with air or stool is variable. Positive colonography has not been investigated extensively in this study. However, as the ileocolic junction was clearly identified in the 2 cases with colonography, it might be a useful and easily accessible tool to diagnose partial colonic agenesis in small animals.
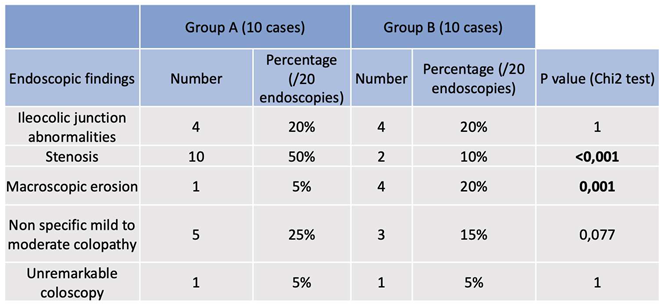
Colonoscopy allowed the diagnosis in most cases. Partial colonic agenesis was associated with other anatomical malformation in 8 cases and included absence of the cecum or abnormal ileocolic junction (Image 3). Focal stenosis was also identified in 12 cases. Marked macroscopic signs of active colonic disease were identified in 5 cases and corresponded to a diagnosis of granulomatous inflammation or IBD. In most cases however, the colic mucosa was macroscopically normal or only slightly modified, especially in group A.
Two different subtypes of presentation were identified in this study: 1 with clinical signs that lasted since a young age or adoption, and 1 with clinical signs that developed during adulthood. In cases where clinical signs developed in adult individuals, a concomitant affection was present in all cases and included IBD, PLE, LGITL, and granulomatous colitis. It is likely that these diseases were responsible for the clinical signs and that the partial colonic agenesis was an incidental finding. However, it might also have been a predisposing factor to the development of these diseases. Indeed, in these 11 cases, an infectious origin was suspected or confirmed in 4 cases (granulomatous infiltrate). A partial colonic agenesis might then have increased to sensitivity of the colon to infectious agent.
In cases where clinical signs started young or at adoption, an infectious agent was found in 3 cases and included 1 trichomonosis and 2 granulomatous infiltrates. In the 9 remaining cases (subgroup C), 7 were submitted to a histologic analysis that showed variable degree of lymphoplasmacytic inflammation. Eight out of these 9 cases developed a colic stenosis. This complication has previously been described in 1 case report of short colon [
12]. In this case, the cat had chronic and progressive signs of diarrhea and developed dyschezia. Colonoscopy identified stenosis with mild to moderate lymphoplasmacytic infiltration and fibrosis, as well as absence of an ileocolic papilla. It is then possible that, in these individuals, partial colonic agenesis might have led to a persistent colic inflammation which predisposed to secondary fibrosis and stenosis. In dogs and cats, rectal strictures can indeed be secondary to diarrhea and the associated colonic inflammation [
21] and in humans, stenosis is a well-known complications of Crohn’s disease with fibrosis and inflammation involved in the pathogenesis [
22]. Furthermore, in the subgroup C, the length of the colon was significantly shorter than in the other cats of the cohort. However, overlap exists, and it remains unclear why some individuals might develop severe clinical signs whereas some remained free of clinical signs for several years. In cats and dogs who underwent small intestinal resection, secondary morphological modifications allow an increase of the villous mucosal surface area following the length reduction [
23,
24]. It seems to be also the case when the resection affects the colon with an adaptative response and villi elongation in the small intestine after sub-total colectomy in dogs [
25]. In all our cases with clinical signs since adoption (with the exclusion of infectious cases) the histological analysis revealed only mild to moderate lymphoplasmacytic infiltration. It is then possible that a histological compensatory adaptation was lacking in this group and could explain the early presentation. Comparison with asymptomatic cases of partial colonic agenesis would be required to answer this question.
The outcomes were highly variable in our cases. Because many of them were lost to follow-up, it is difficult to draw conclusions on the potential benefits of the treatments initiated (
Table 8). However, in some cases, management of the clinical signs seemed to be more difficult than in animals exhibiting a colopathy without partial colonic agenesis.
Partial colonic agenesis might be part of a wider syndrome of short bowel. Indeed, congenital short bowel is described [
26] and was associated with marked weight loss and intermittent diarrhea. In our study, the small intestinal length could not be evaluated. However, weight loss, when present, was usually mild as most BCS were higher than 3/9. Furthermore, 1 case underwent necropsy that did not show any small intestinal shortening.
Congenital partial colonic agenesis is described in humans. It is a rare condition, more common in males and in which the colon is partially or completely replaced by a dilated pouch. It is however often associated with anorectal malformations [
27] and usually terminates in a fistulous communication with the genitourinary tract [
28].
This study has some limitation. Firstly, a precise reference range of the normal colonic length according to the animal weight is lacking in the literature. It may vary according to the animal’s size and may differ if the measure has been performed on dead or alive individuals. Secondly, because of its retrospective nature, diagnostic criteria were not standardised and varied. Many of our cases were lost to follow-up and treatment efficiency could not be assessed precisely. Reviewing the abdominal ultrasounds was retrospectively performed on fixed images which might have troubled the identification of abnormalities. In addition, at the time of presentation, no specific attention was focused on the research of a shorten colon and subtle indicator might thus have been missed. Finally, Fluorescence in situ Hybridation (FISH) analysis could have been done to exclude invasive bacteria within the colonic mucosa.
Figure 1.
Age at presentation according to the group (A: animals with clinical signs lasting since the adoption and B: animals with a progressive or acute onset of clinical signs during adulthood).
Figure 1.
Age at presentation according to the group (A: animals with clinical signs lasting since the adoption and B: animals with a progressive or acute onset of clinical signs during adulthood).
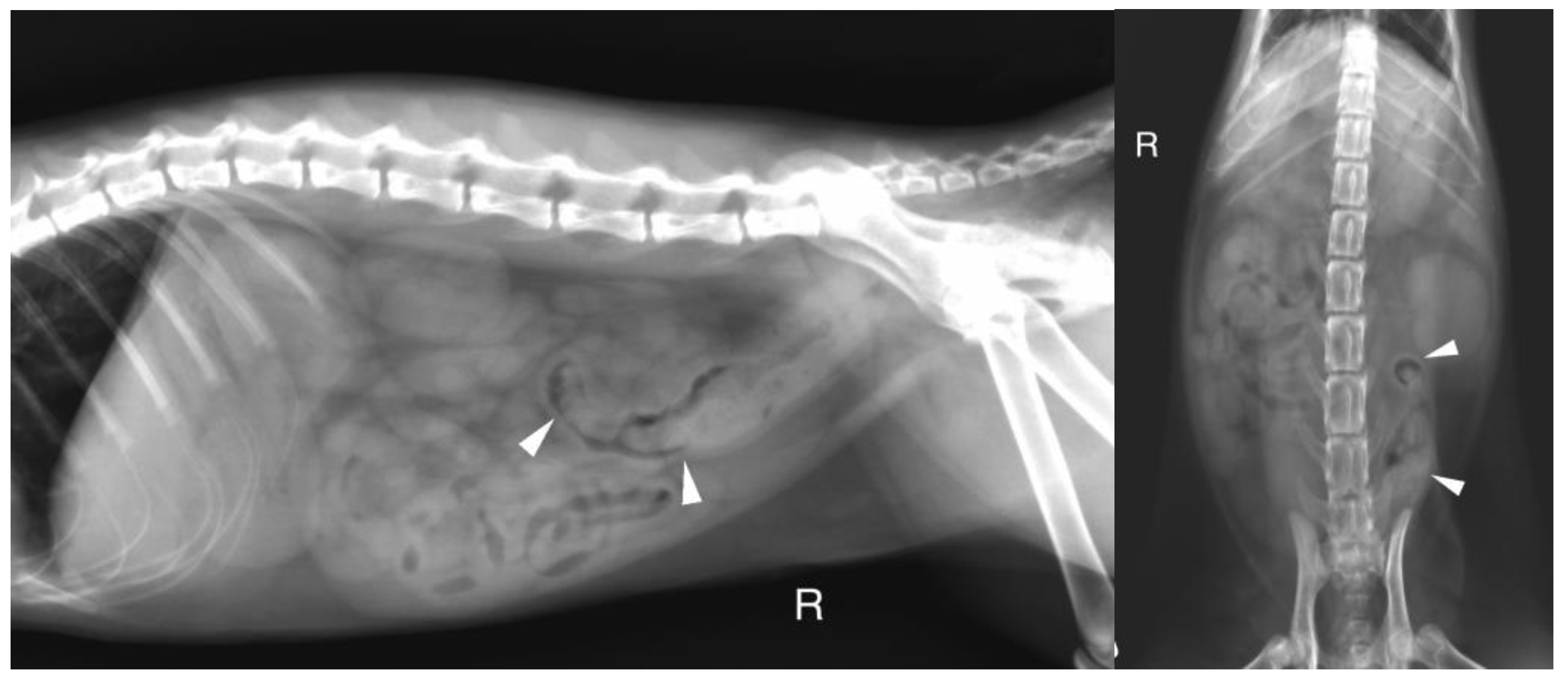
Figure 2.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of case 11, a 6 months old Scottish cat. The descending colon is shorter than expected and abruptly end in the mid left abdomen (white arrow heads). No other parts of the colon are identified.
Figure 2.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of case 11, a 6 months old Scottish cat. The descending colon is shorter than expected and abruptly end in the mid left abdomen (white arrow heads). No other parts of the colon are identified.
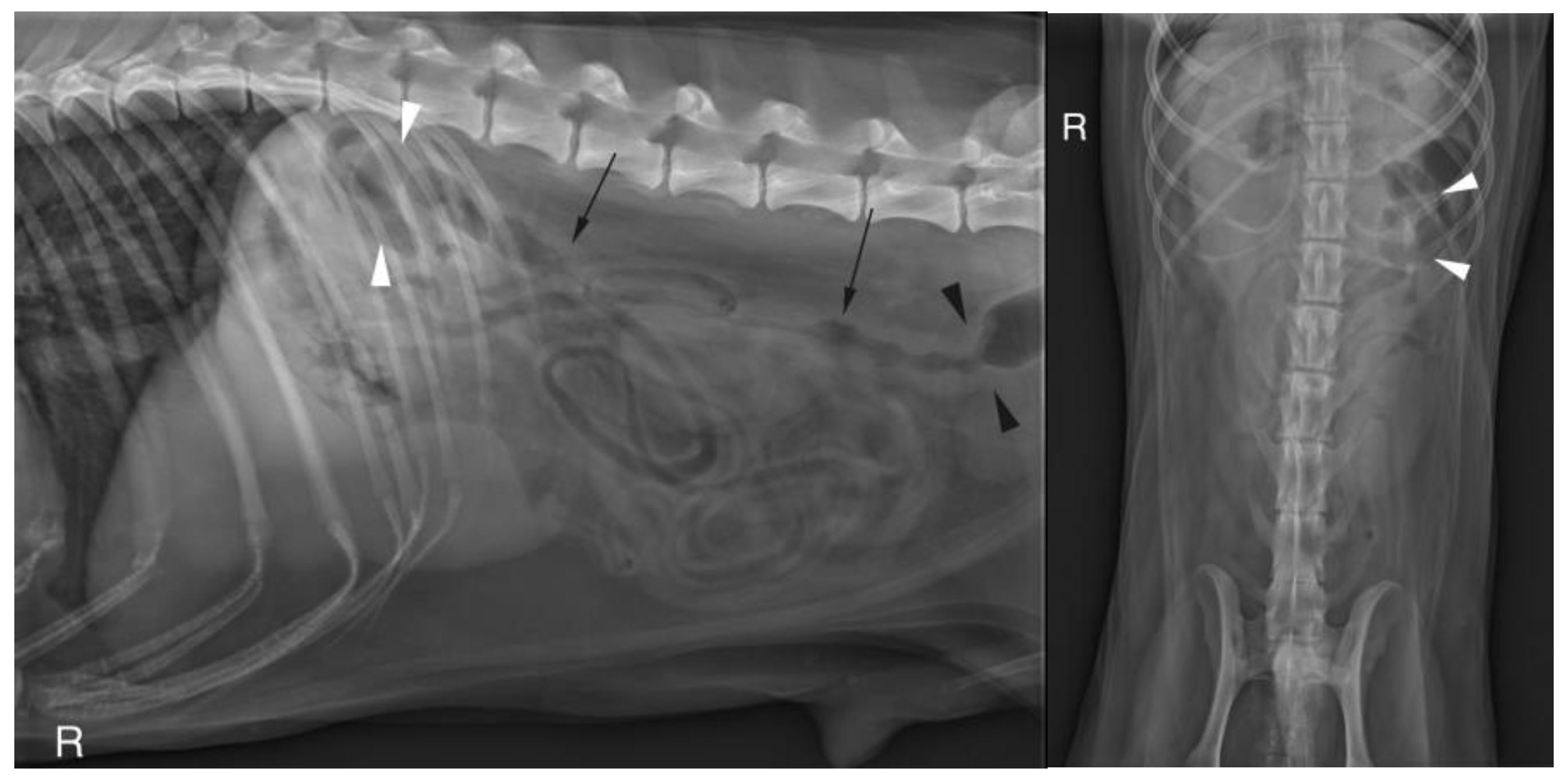
Figure 3.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of case 18, an 8 years-old Colley dog. The cecum is malpositioned in the left cranial and dorsal abdomen (white arrow heads), in continuity with the descending colon on the lateral view (black arrows). A focal narrowing of the aboral part of the descending colon is observed before it enters the pelvis (black arrow heads).
Figure 3.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of case 18, an 8 years-old Colley dog. The cecum is malpositioned in the left cranial and dorsal abdomen (white arrow heads), in continuity with the descending colon on the lateral view (black arrows). A focal narrowing of the aboral part of the descending colon is observed before it enters the pelvis (black arrow heads).
Figure 4.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of the same cat as on image 2, during positive retrograde colonography. The descending colon is shorter than expected (white arrow heads), the ileocolic junction is identified as a narrowing of the colonic lumen orally (asterisk). Contrast medium is also visible within the small intestine (black arrows). The cecum is not identified.
Figure 4.
A. Right lateral radiograph and B. Ventro-dorsal radiograph of the abdomen of the same cat as on image 2, during positive retrograde colonography. The descending colon is shorter than expected (white arrow heads), the ileocolic junction is identified as a narrowing of the colonic lumen orally (asterisk). Contrast medium is also visible within the small intestine (black arrows). The cecum is not identified.
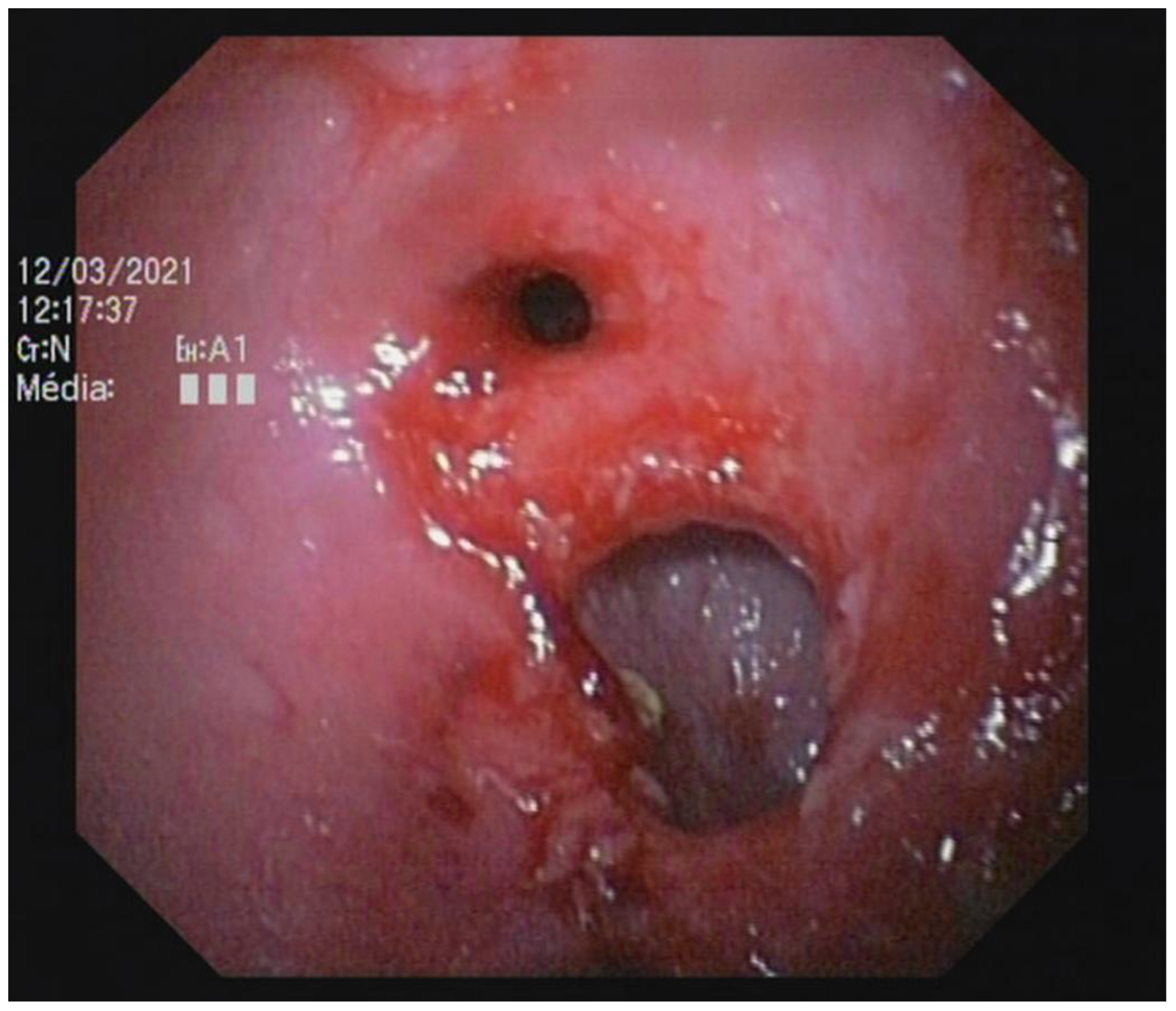
Figure 5.
Abnormal ileocolic junction in a cat (Case 10).
Figure 5.
Abnormal ileocolic junction in a cat (Case 10).
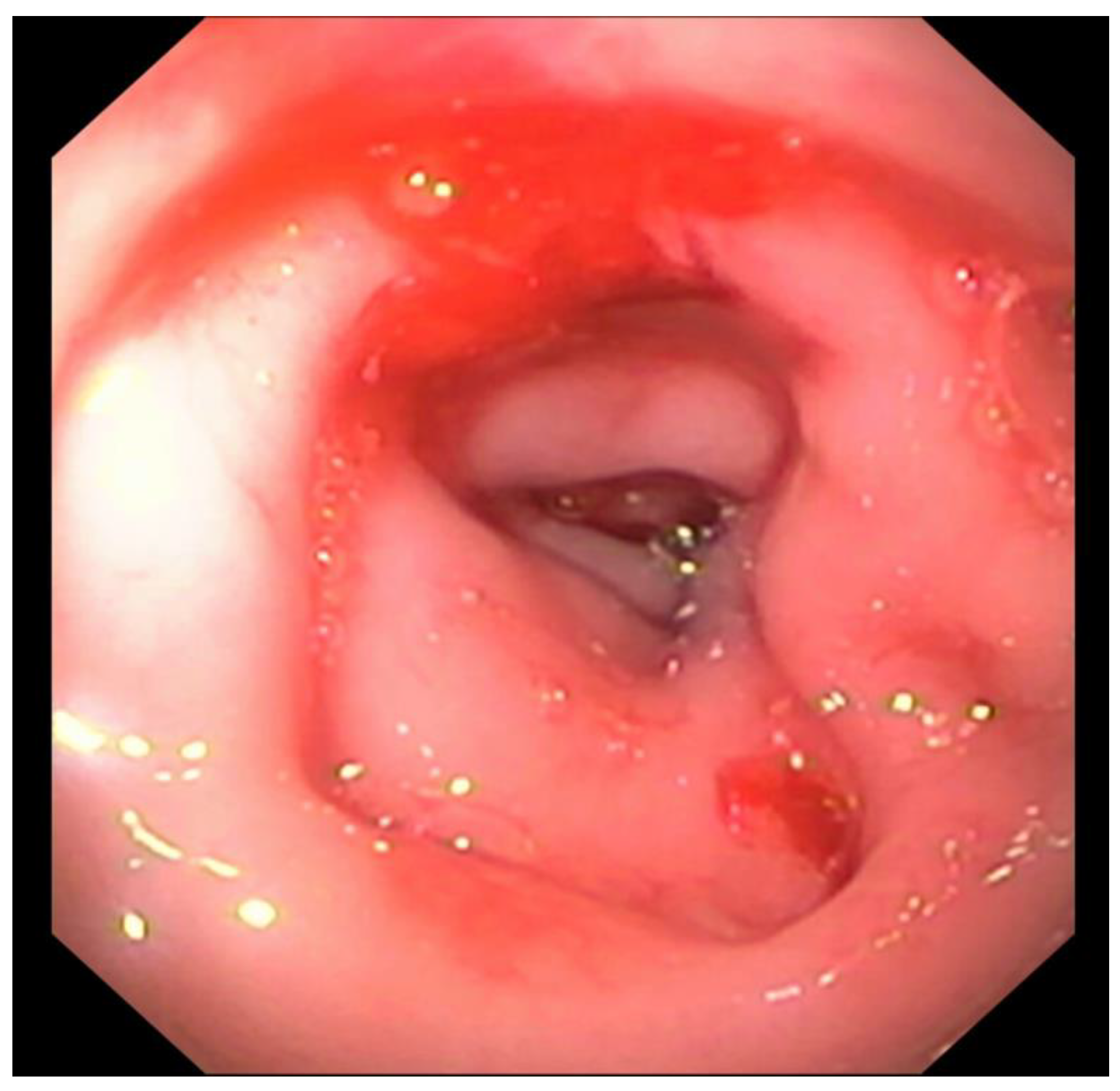
Figure 6.
Focal colonic stenosis in a cat (Case 15).
Figure 6.
Focal colonic stenosis in a cat (Case 15).
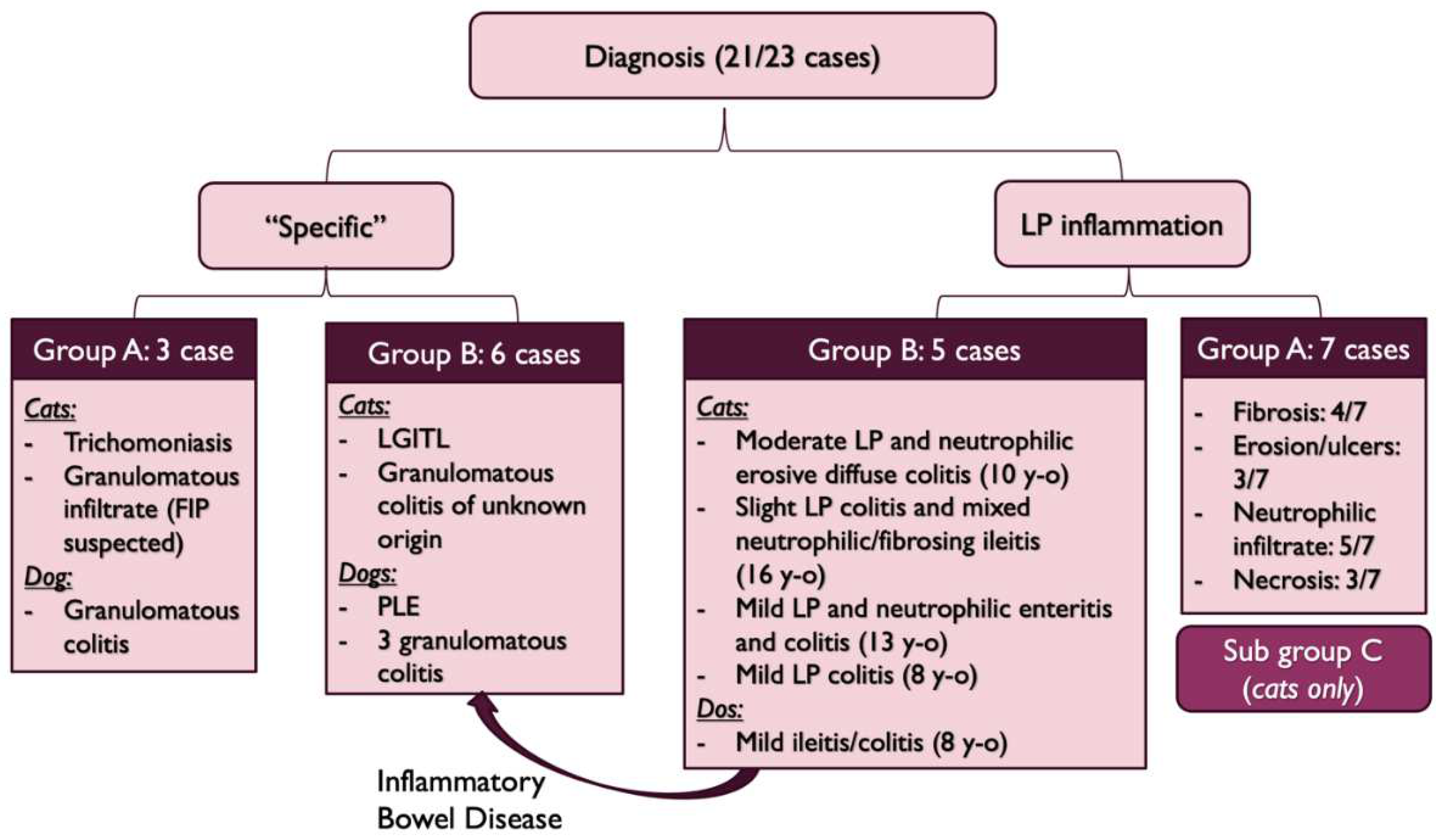
Figure 7.
Diagnosis repartition (FIP: Feline Infectious Peritonitis, LGITL: Low Grade Intestinal T-cell Lymphoma, PLE: Protein-Losing-Enteropathy, y-o: years-old, LP: lymphoplasmacytic).
Figure 7.
Diagnosis repartition (FIP: Feline Infectious Peritonitis, LGITL: Low Grade Intestinal T-cell Lymphoma, PLE: Protein-Losing-Enteropathy, y-o: years-old, LP: lymphoplasmacytic).
Figure 8.
Colectomy in a cat with partial colonic agenesis: the total length was estimated to 8 cm.
Figure 8.
Colectomy in a cat with partial colonic agenesis: the total length was estimated to 8 cm.
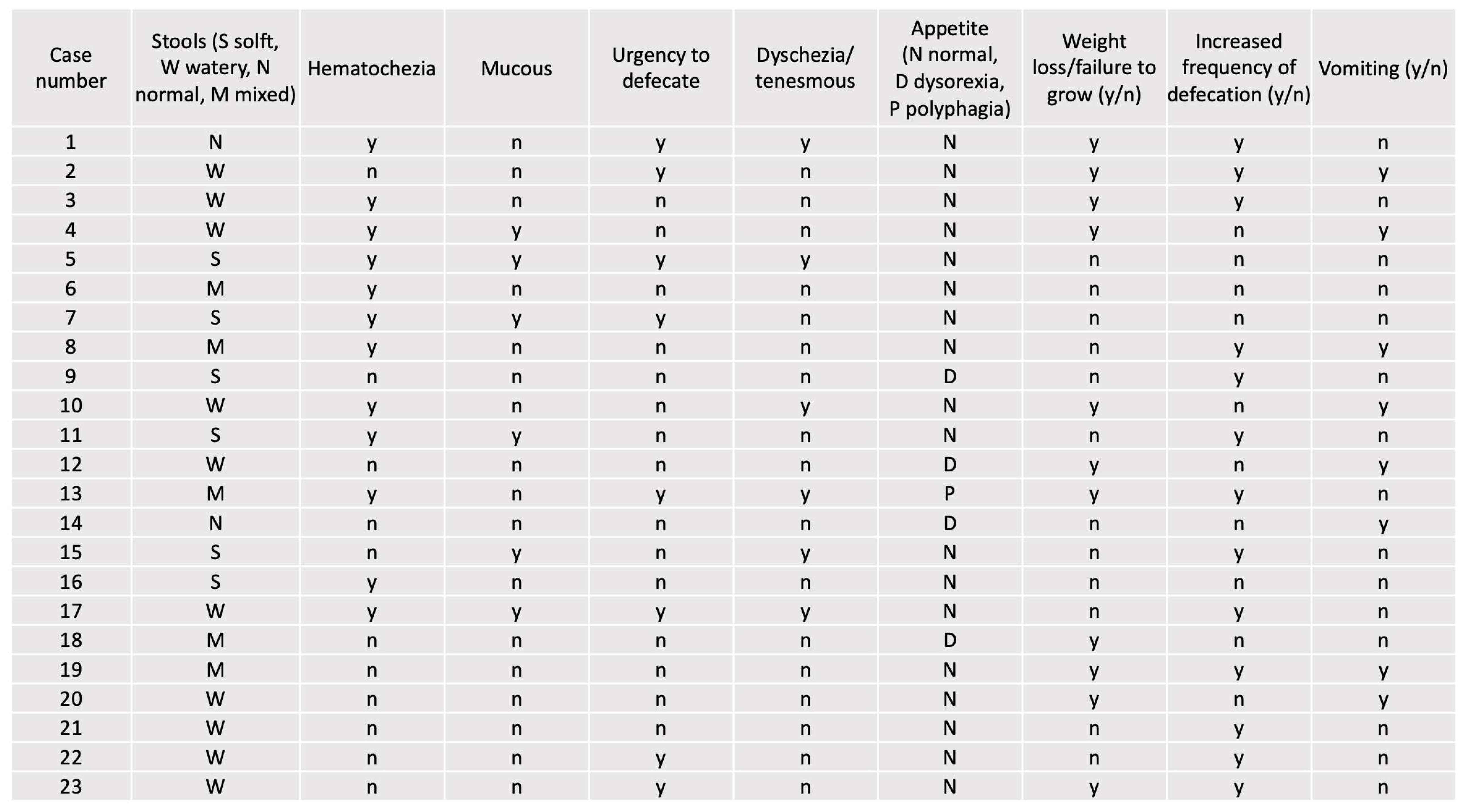
Table 2.
Clinical signs in both groups (y = yes; n = no).
Table 2.
Clinical signs in both groups (y = yes; n = no).
Table 3.
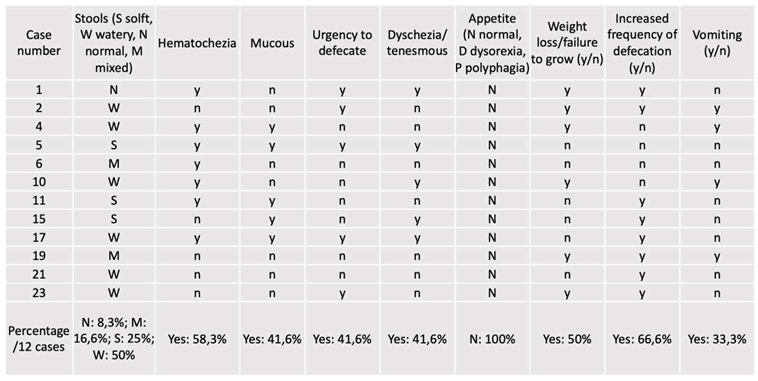
Clinical signs in group A (y = yes; n = no).
Table 3.
Clinical signs in group A (y = yes; n = no).
Table 4.
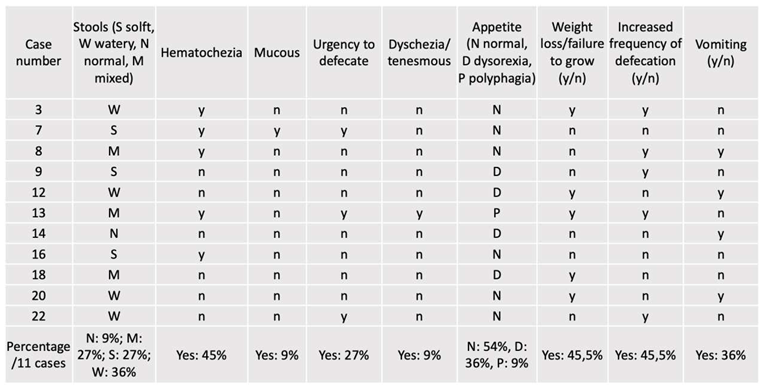
Clinical signs in group B (y = yes; n = no).
Table 4.
Clinical signs in group B (y = yes; n = no).
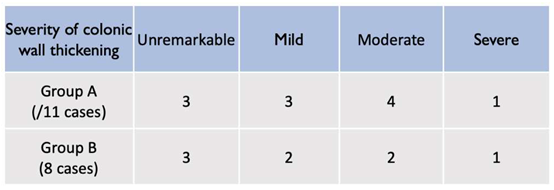
Table 5.
Severity of colonic wall thickening at diagnosis (abdominal ultrasound).
Table 5.
Severity of colonic wall thickening at diagnosis (abdominal ultrasound).
Table 6.
Endoscopic findings according to the presentation.
Table 6.
Endoscopic findings according to the presentation.
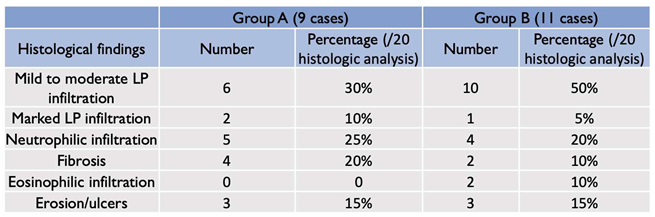
Table 7.
Histologic findings according to the presentation (LP: lymphoplasmacytic) (established according to the WSAVA criteria [
18].
Table 7.
Histologic findings according to the presentation (LP: lymphoplasmacytic) (established according to the WSAVA criteria [
18].
Table 8.
Diagnosis, treatments and outcomes (LP: lymphoplasmacytic, FIP: Feline Infectious Peritonitis, IBD: Inflammatory Bowel Disease, PLE: Protein-Losing-Enteropathy, LGITL: Low Grade Intestinal T-cell Lymphoma, D: dog, C: cat). Cases are referenced according to
Table 1.
Table 8.
Diagnosis, treatments and outcomes (LP: lymphoplasmacytic, FIP: Feline Infectious Peritonitis, IBD: Inflammatory Bowel Disease, PLE: Protein-Losing-Enteropathy, LGITL: Low Grade Intestinal T-cell Lymphoma, D: dog, C: cat). Cases are referenced according to
Table 1.
| Group |
Case Number |
Diagnosis |
Treatment |
Outcome |
| |
1 |
Sub group C and stenosis (C) |
Colectomy |
Died in the post operative period |
| A |
2 |
Sub group C and stenosis (C) |
Bougienage, amoxicillin/clavulanic acid, metronidazole, prednisolone 0.5 mg/kg/d, probiotics, pancreatic enzymes supplementation, cobalamine, diosmectite, hyperdigestible diet |
Lost to follow-ups |
| |
3 |
Tritrichomonosis (C) |
Ronidazole |
Lost to follow-ups |
| |
4 |
Sub group C and stenosis (C) |
Metronidazole, prednisolone 0.7 mg/kg/d, hyperdigestible diet |
Lost to follow-ups |
| |
6 |
Sub group C and stenosis (C) |
Colonic stent and bougienage, titanoreine, prednisolone 1 mg/kg/d, metronidazole, pancreatic enzymes, hyperdigestible diet, diosmectite |
Marked improvement |
| |
7 |
Sub group C with variable degree of LP inflammation (C) |
Prendnisolone 0.5 mg/kg/d |
Lost to follow up |
| |
10 |
Short colon with stenosis. Granulomatous infiltrate (FIP suspected) (C) |
Colectomy then prednisolone 1.5 mg/kg, smectite if needed, metronidazole and GS 441524 |
Mild improvement |
| |
11 |
Sub group C and stenosis (C) |
Metronidazole, Lactulose and a/d food |
Marked improvement |
| |
13 |
Sub group C and stenosis (C) |
Metronidazole, prednisolone 0.7 mg/kg/d, hyperdigestible diet |
Lost to follow-ups |
| |
15 |
Sub group C and stenosis (C) |
Prednisolone 0.75 mg/kg/d, marbofloxacin, fiber, hyperdigestible diet |
Recent inclusion |
| |
17 |
Sub group C and stenosis (C) |
Fiber enriched diet, metronidazole, prednisolone 1 mg/kg/d |
Recent inclusion |
| |
19 |
Granulomatous colitis (D) |
Marbofloxacin |
Improvement |
| B |
5 |
IBD (C) |
Prednisolone 0.5 mg/kg and amoxicillin/clavulanic acid (antibiogram) 3 weeks |
Lost to follow up |
| |
8 |
Granulomatous inflammation of unknown origin (C) |
Prednisolonone 2 mg/kg/d, smectite, TMPS, |
Died within 2 weeks of hypovolemic shock |
| 9 |
LGITL in ileum (C) |
Prednisolonone 2 mg/kg/d, chlorambucil 20 mg/m2 every 2 weeks |
Marked improvement |
| 12 |
LP colitis (C) |
Prednisolone 0.5 mg/kg and hyperdigestible diet |
Marked improvement |
| 14 |
IBD with cholecystitis (C) |
Marbofloxacin, amoxicillin/clavulanic acid, prednisolone 0.65 mg/kg/d after cholelithiasis removal. |
Marked improvement |
| 16 |
IBD with stenotic areas (C) |
Prednisolone, marbofloxacine, hyperdigestible diet |
Recent inclusion |
| 18 |
IBD with stenotic areas (D) |
Smectite, homemade eviction diet, fortiflora, tylosine, prednisolone 0.5 mg/kg/d 15 days. |
Marked improvement. Colonic ADK diagnosed 6 months after |
| 20 |
Granulomatous colitis (D) |
Enrofloxacine, fenebendazole, diosmectite |
Died of septic choc after aspiration pneumonia |
| 21 |
Granulomatous colitis (D) |
Marbofloxacine 4 mg/kg for 6 weeks |
Marked improvement |
| 22 |
PLE (D) |
Prednisolone 2 mg/kg/d, cobalamine, ciclosporine 5 mg/kg/d, clopidogrel, metronidazole, ULF diet |
Improvement with normal stools |
| 23 |
Granulomatous colitis (D) |
Enrofloxacine, hyperdigestible diet, diosmectite |
Marked improvement |