1. Introduction
Osteoarthritis (OA) emerged as a common chronic musculoskeletal disorder, becoming a common medical condition affecting the joints. In particular, osteoarthritis affects all races, sexes and ages but is best known in obese and elderly people1. Osteoarthritis has multiple risk factors, which can be categorized into two main types: modifiable risk factors and nonmodifiable risk factors. Modifiable risk factors include previous joint injury, obesity, metabolic syndrome, and daily lifestyle factors (such as occupational stress or overexertion). Nonmodifiable risk factors encompass genetics, increasing age, and female gender. The person who has risk factors should undergo regular health check-ups to enable timely interventions during the early stages and ensure the best treatment approach, thus avoiding potential long-term consequences1-5.
In the human body, meniscus is known to facilitate joint stability, maintain normal knee function, lubricate joints, and distribute body loads6-8. Osteoarthritis develops when the protective cartilage covering the ends of bones gradually wears down, leading to the bones rubbing against each other. This friction causes common symptoms such as joint swelling, pain, and stiffness4,5. In general, partial, or complete loss of function of the meniscus causes knee osteoarthritis9,10. Various imaging techniques can aid in diagnosing OA and providing treatment recommendations. Plain radiographs (X-rays) are commonly used and can show characteristic features of OA, including joint space narrowing, osteophytosis (bone spurs), subchondral sclerosis (increased bone density beneath the cartilage), and cyst formation4,5. Diagnostic ultrasound and MRI may also be employed to visualize soft tissues and assess the severity of joint damage4,5,8. Osteoarthritis can affect various joints throughout the body, including the wrist and finger joints, ankle and toe joints, hip joint, cervical spine, and lumbar spine. However, the most commonly affected joint is the knee joint. Knee arthritis includes self-reported knee arthritis, radiographic definition of knee arthritis and symptomatic knee arthritis (self-reported joint pain, stiffness, pain, and radiographic evidence)11.
In worldwide, osteoarthritis is considered the fourth leading cause of disability and functional impairment12,13. In developed and developing countries, osteoarthritis can cause a significant deterioration in the quality of life for people over 65 years of age due to joint pain and disability3,14-17. In an earlier Australian study, in Caucasians, the prevalence of symptomatic osteoarthritis was about 10% in men and 20% in women aged 45 years and older18, but for radiographic OA, the incidence can be increased range from 27% to 80% in a research was conducted in USA19. Besides that, the population prevalence of knee osteoarthritis at 40 years old and above accounts for 34%, with a higher incidence rate among females compared to males in Ho Chi Minh city, Vietnam20. The treatment of osteoarthritis is increasingly becoming a burden on society, not only in terms of direct healthcare costs but also in indirect costs resulting from the rising prevalence of the disease coupled with population aging21. This is a significant public health issue that requires attention, as the disease leads to functional impairment and becomes an economic burden on society aspects16.
Currently, interventions for patients with osteoarthritis include lifestyle modifications, medication-based approaches, and surgical interventions. About lifestyle modifications, such as maintaining a healthy weight, engaging in low-impact exercises, protecting joints from injuries, avoiding repetitive joint stress, following a balanced diet, and managing overall health conditions, can significantly reduce the risk of developing osteoarthritis and promote optimal joint health22. Medication-based approaches include pain relievers, symptomatic slow-acting drugs for osteoarthritis (SYSADOAs), non-steroidal anti-inflammatory drugs (NSAIDs), and intra-articular corticosteroid injections. Surgical interventions involve partial or total joint replacement23. In reality, non-steroidal anti-inflammatory drugs (NSAIDs) are the most commonly used medication due to their effectiveness in reducing pain and inflammation. However, they do carry a significant risk of adverse effects on cardiovascular issues and gastrointestinal systems24.
Glucosamine is a SYSADOA medication prescribed for patients with mild to moderate osteoarthritis. It plays a role in the synthesis and metabolism of joint cartilage, promoting the production of essential components and increasing the production of synovial fluid, which enhances lubrication. As a result, it effectively reduces the symptoms of the disease, such as swelling, pain, and joint stiffness, while also slowing down its progression2. Glucosamine offers a cost-effective treatment option with favorable outcomes25. The glucosamine Sulfate crystalline form, in particular, has been proven to be more cost-effective in the treatment of joint inflammation compared to other formulations. By incorporating glucosamine into the treatment plan, healthcare providers can provide patients with an effective therapy that not only alleviates symptoms but also helps prevent further deterioration of the condition. This leads to improved overall treatment outcomes at a lower cost. The use of glucosamine as a therapeutic option highlights its potential in managing osteoarthritis and its cost-effectiveness compared to alternative treatments26. Its ability to target the underlying processes of joint degeneration and provide symptomatic relief makes it a valuable addition to the treatment regimen for patients with mild to moderate osteoarthritis2,27,28. However, the clinical effectiveness of glucosamine, as demonstrated in published research studies, remains inconclusive, leading to significant debates and difficulties in decision-making by reimbursement agencies.
The issue at hand is not only finding a highly effective and cost-efficient treatment method but, more importantly, identifying the most efficient treatment sequence for osteoarthritis while minimizing costs and reducing the potential adverse effects of medications.
Research also aims to identify the optimal integration of crystalline glucosamine Sulfate into the standardized treatment, following the most favorable sequence. Through this research, we aim to provide healthcare professionals and policymakers with a comprehensive framework for evaluating and comparing treatment regimens, allowing them to make informed decisions based on cost-effectiveness analysis.
2. Materials and Methods
A comprehensive economic evaluation was conducted, considering both the clinical outcomes and the associated costs. The study employed a Markov model with standard treatment 1 (including pain relievers, one type of NSAID, intra-articular corticosteroid injections, and surgery) and standard treatment 2 (including pain relievers, two types of NSAIDs, intra-articular corticosteroid injections, and surgery) as the benchmarks to compare cost-effectiveness with the protocol supplemented with crystalline glucosamine Sulfate at different stages. The study participants consisted of a group of mild to moderate osteoarthritis patients above the age of 40, without any severe accompanying conditions. The study period spanned the lifetime horizon of the individuals, lasting for a 6-month cycle length. The data was derived from a comprehensive review of literature based on publicly available databases and data from the Vietnam Drug Administration (DAV). The evaluation of effectiveness was based on the quality-adjusted life years (QALYs), which adjusted the additional years of life gained for quality of life, and the cost effectiveness was assessed using the incremental cost-effectiveness ratio (ICER) from a societal perspective. All costs and outcomes in the study were discounted at 3%.
ICER (Incremental Cost-Effectiveness Ratio) is an essential tool in health economics that assists policymakers in evaluating the efficiency and rationality of different treatment sequences based on their cost and benefits. In the research model, ICER is calculated by comparing the costs and quality-adjusted life years (QALYs) of each treatment sequence.
2.1. Model structure
The study utilized Markov model to evaluate and compare the cost-effectiveness of treatment regimens against standard treatment. The methodology involved constructing models that represented the various treatment pathways and their corresponding probabilities, costs, and outcomes. By considering factors such as treatment efficacy, adverse effects, and cost, the model could provide valuable insights into the cost-effectiveness of different treatment regimens. This model was reviewed and consulted with local experts.
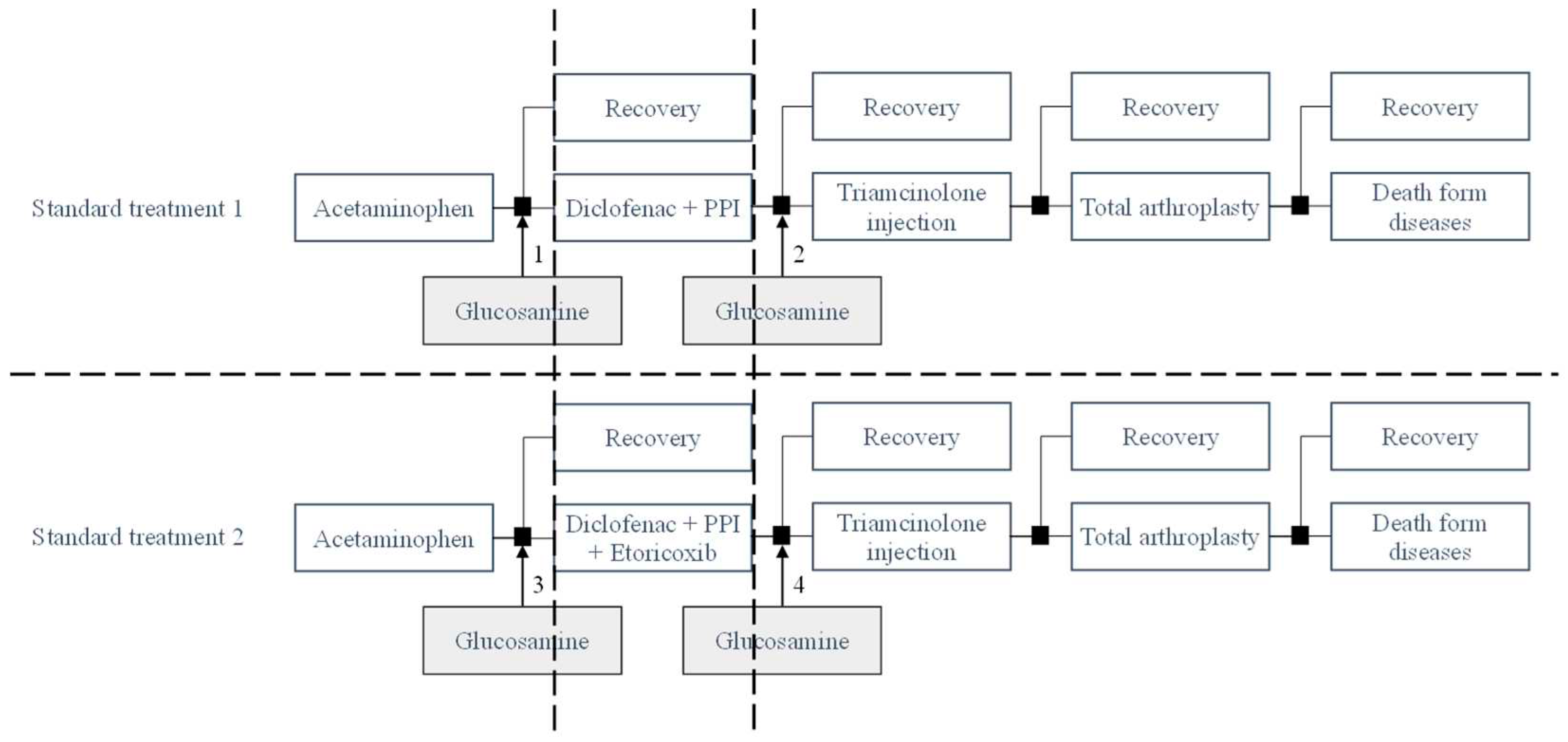
The standard treatment regimen in this study adhered to the following treatment sequence:
Standard treatment 1 (PD): Pain relievers (Acetaminophen), Non-steroidal anti-inflammatory drugs (NSAIDs): Diclofenac combined with proton pump inhibitor (PPI), Intra-articular corticosteroid injection (Triamcinolone) and finally, total arthroplasty surgery.
Standard treatment 2 (PDE): Standard treatment 1 + Etoricoxib. The specific treatment sequence was as follows: Acetaminophen - Diclofenac + PPI - Etoricoxib – Triamcinolone - total arthroplasty surgery.
Taking the milestone as standard treatment 1 and standard treatment 2, in each standard regimen, Crystalline Glucosamine Sulfate was supplemented before and after NSAIDs, forming different treatment sequences for cost-effectiveness comparison. In treatment 1, Glucosamine was used before initiating the use of NSAIDs (Nonsteroidal Anti-Inflammatory Drugs). Glucosamine is commonly used to alleviate pain and slow down the progression of joint degeneration, while NSAIDs are typically used to reduce inflammation and pain. By using glucosamine before NSAIDs, the objective was to enhance the effectiveness of slowing down the disease progression and reduce the necessity of NSAIDs during the treatment process. In treatment 2, Glucosamine was used after the administration of NSAIDs. The objective was to evaluate the differences in the extent of disease progression retardation and cost-effectiveness of treatment when glucosamine is utilized as a supplementary approach following the use of NSAIDs. Utilizing Glucosamine after NSAIDs may provide additional benefits in slowing down the progression of joint degeneration after inflammation and pain reduction with NSAIDs. The disparity between these two treatment sequences compared to the standard treatment protocol could lie in the effectiveness of slowing down joint degeneration, the level of pain and inflammation reduction, as well as the cost and convenience of utilizing these methods. However, to obtain an accurate assessment of the differences between these two treatment sequences, evaluation based on specific research data is required.
Figure 1.
Model structure.
Figure 1.
Model structure.
Regimen 1 (PGD): the addition of crystalline Glucosamine Sulfate before Diclofenac + PPI in standard treatment 1; Regimen 2 (PDG): the addition of crystalline Glucosamine Sulfate after Diclofenac + PPI in standard treatment 1
Regimen 3 (PGDE): the addition of crystalline Glucosamine Sulfate before Diclofenac + PPI + Etoricoxib in standard treatment 2; Regimen 4 (PDEG): the addition of crystalline Glucosamine Sulfate after Diclofenac + PPI+ Etoricoxib in standard treatment 2
In each cycle of the model, patients could achieve a stable state with the same level of treatment or transition to the next treatment state when the medication was unresponsive and the pain remained unimproved, necessitating intervention with escalated treatment measures. The patients in the study commenced treatment with Acetaminophen and ended in a deceased state. The transition rate, which represents the conversion rate between stages within each cycle of the model, was utilized to calculate the number of Quality-Adjusted Life Years (QALYs) in each phase. The main assumption of the study was that patients only received the prescribed treatment modality in each specific state.
2.2. Model assumptions
The main assumption in our study is that patients are only treated as prescribed by doctors at certain stages as in the proposed model. The risks of possible complications and side effects are assumed to be unchanged over time. The patients who received treatment were recovery or moved to the next health stage. Once the patient has moved to the next stage of illness, it is not possible to return to the previous state of illness.
Regarding the literature review of economic evaluation studies for osteoarthritis of the knee, all studies including ours hypothesized that self-treatment or adverse effects disease subtype will only be considered as a disease stage in our model. This is due to the nature of osteoarthritis where it is difficult to define specific stages. the adverse events were not included.
In Vietnam, the majority of people who begin to have symptoms and are recorded as having osteoarthritis are at the age of 40 or older20. Therefore, the target population selected for this study is 40 years old and older. In addition, knee osteoarthritis is a chronic disease, so in this study, QALYs based on status of patients was estimated as health outcome of this model. This life-year gained is estimated to be equal to the number of years of life of a person from 40 years old to the average life expectancy of Vietnamese people in 202129.
2.3. Model Input
Data were collected through a literature review based on studies available in Vietnam. The missing data will be searched and summarized through world studies, i.e. meta-analysis, systematic review, randomized controlled trial (RCT), and real-world evidence studies. The data are selected from data in studies in countries with the same socio-economic conditions as Vietnam or with countries similar to Vietnam. The 3% discount rate was applied to both costs and outcome. The data is summarized in
Table 1.
2.4. Cost variables
The cost data included for calculation comprises:
Direct medical costs: These encompass expenses related to direct healthcare services such as medication costs, laboratory tests, consultations, and hospital bed utilization during the treatment of osteoarthritis. Medication costs within the model were computed on the maximum dosage as per patients based on the Ministry of Health's diagnostic and treatment guidelines.
Direct non-medical costs: These encompass expenses incurred by patients that are not directly related to healthcare services but are associated with the treatment and management of osteoarthritis. This include costs for meals, transportation, travel to healthcare facilities30. Consumer Price Index (CPI) of Vietnam was used to convert past monetary values to the present31.
Indirect costs: These include costs incurred due to work absenteeism and reduced productivity caused by pain. Pain and functional limitations can significantly impact the patient's ability to work effectively, leading to loss of income and decreased work productivity. In this study, the cost was estimated from the knee joint recovery post-surgery multiply by Vietnam's Gross Domestic Product (GDP) per capita per month. The knee joint recovery post-surgery (1 month) was estimated from Hien TT. et al., 202232.
According to the World Bank, Vietnam's Gross Domestic Product per capita in 2021 was 3,756 USD33. Based on a currency exchange rate of 1 USD equivalent to 23,486 Vietnam Dong (VND) (May 2023), Vietnam's GDP per capita in 2021 would be approximately 88,213,416 VND33. At present, the willingness to pay threshold in Vietnam is determined based on per capita GDP. When the ICER (Incremental Cost-Effectiveness Ratio) is lower than the per capita GDP, the expenditure is considered highly cost-effective. When the ICER is greater than 1 GDP but less than 3 times the per capita GDP, the expenditure is considered cost-effective. If the ICER exceeds 3 times the per capita GDP, the expenditure is deemed not cost-effective.
2.5. Efficacy of pain relief
All efficacy data are assumed through data collected from RCTs worldwide because of limited data available in Vietnam. From selected studies34-38, data on the clinical effectiveness of a group of patients with osteoarthritis, exhibiting characteristics relevant to the Vietnamese population, was gathered. The collected results regarding pain reduction efficacy were transformed into transition rates for utilization within the model's calculations. Specifically, the clinical effectiveness of Acetaminophen, Diclofenac + PPI, Etoricoxib, Crystalline Glucosamine Sulfate, Triamcinolone injection, and Total arthroplasty were as follows previous studies.
2.6. Adverse events
While commonly used for pain and joint-related issues, acetaminophen, diclofenac, etoricoxib, and triamcinolone injection have potential adverse effects that should be considered. Acetaminophen, although generally considered safe when used as directed, can cause gastrointestinal disturbances such as stomach upset. In high doses or with prolonged use, it can lead to liver toxicity, which poses a significant concern. Although rare, allergic reactions to acetaminophen have been reported. Diclofenac and Etoricoxib, a nonsteroidal anti-inflammatory drug (NSAID), carries its own set of adverse effects. Gastrointestinal ulcers or bleeding can occur, particularly with long-term use or high doses. Furthermore, diclofenac is associated with cardiovascular risks, including an increased likelihood of high blood pressure, heart attack, or stroke. Renal toxicity and allergic reactions, manifesting as skin rash, swelling, or difficulty breathing, are also possible adverse effects34. In the case of triamcinolone injection, local injection site reactions, such as pain, swelling, or infection, are possible. There may be a temporary flare-up of joint pain or inflammation following the injection36. In this study, the adverse events were not included.
2.7. Health outcomes
The utility of each health state was assessed based on the effectiveness of the respective medications in alleviating pain. The utility index score of oral medications was obtained from Latimer et al., (2009)39. The utility of patient using Glucosamine was retrieved from study of Olivier Bruyère et al., (2019)40. For joint replacement surgery, a utility index score of 0.76 was derived from the David Feeny's study (2004)41. The utility index score of 0.64 for injectable medications was sourced from Losina's study (2013)42, which obtained data from the Osteoarthritis Research Society International. The pain subscale from the Western Ontario and McMaster Universities OA Index (WOMAC) served as the primary measure of clinical efficacy36.
2.8. Sensitivity analysis.
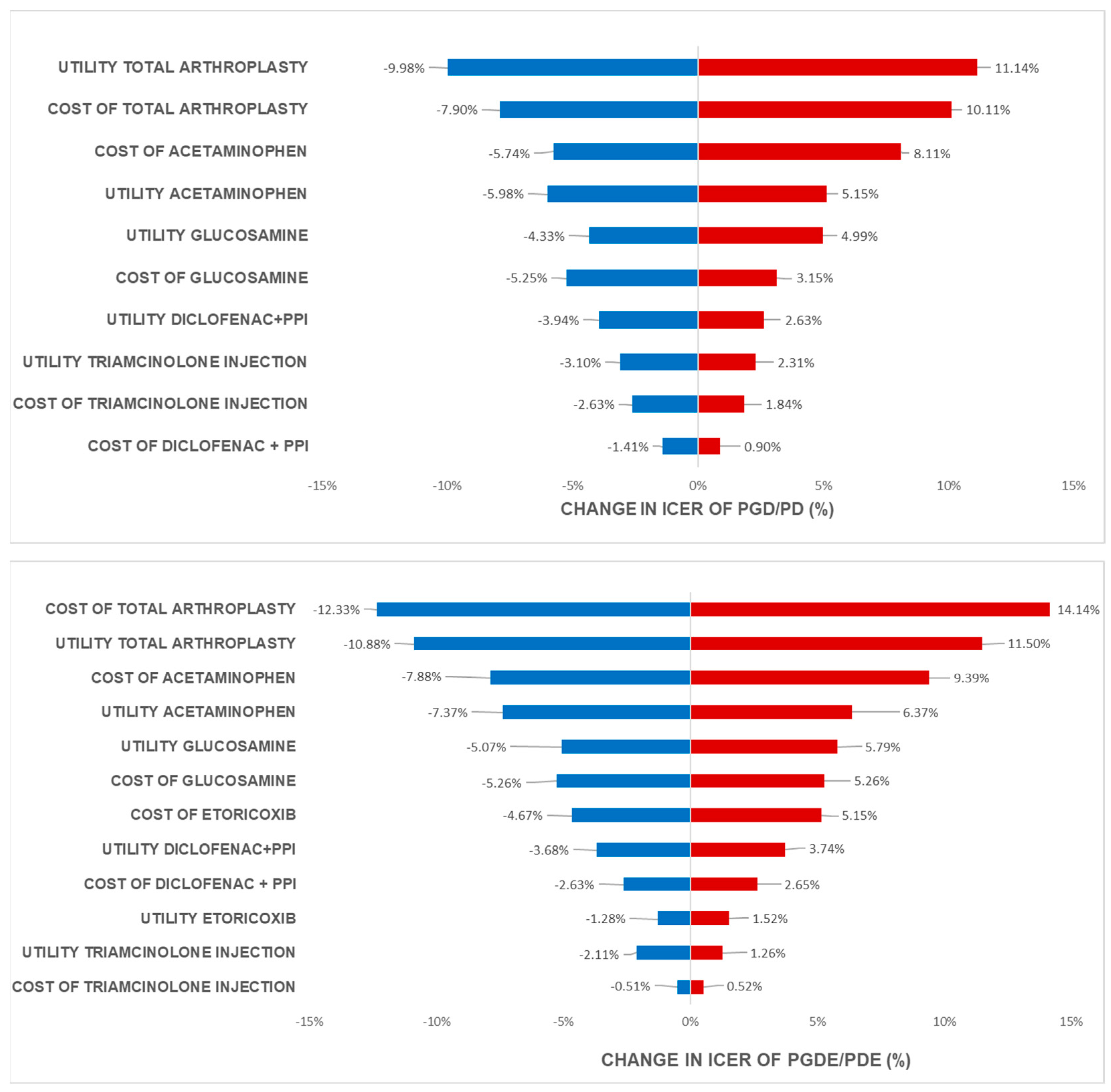
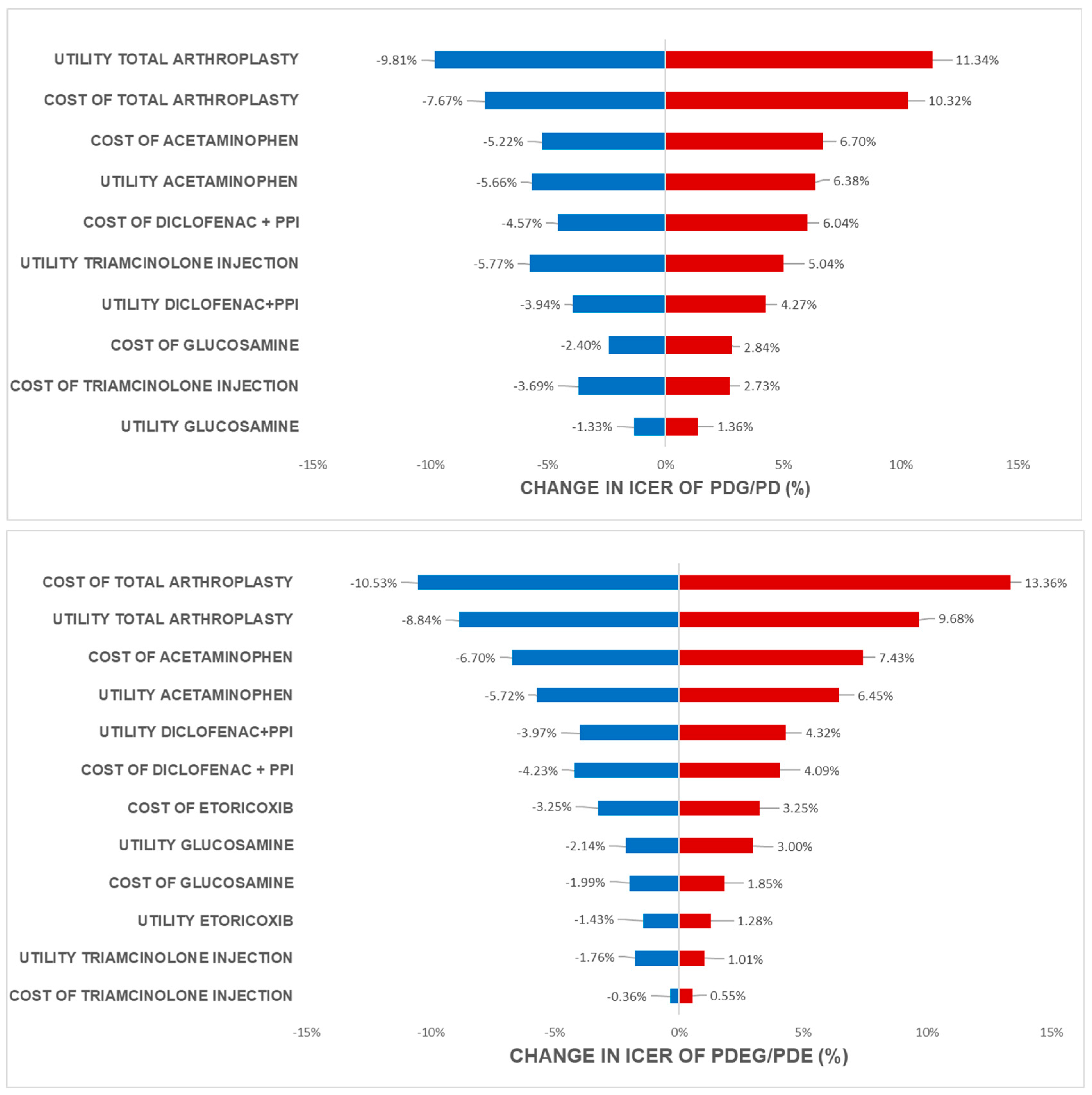
The one-way analysis with results were presented as Tornado diagram was applied to analyze the effect of parameters to the ICER values when parameters value were changed.
Table 1.
Input data.
| Component |
Estimate |
Sources |
|
1. Transition probabilities
|
| Acetaminophen |
0.3380 |
Herrero-Beaumont et al., (2007)37. |
| Diclofenac + PPI |
0.8647 |
Zacher et al., (2003)35. |
| Triamcinolone injection |
0.0392 |
McAlindon et al., (2017)36. |
| Total arthroplasty |
0.5122 |
Fortin et al., (1999)38. |
| Etoricoxib |
0.5657 |
Cannon et al. (2006)34. |
| Crystalline Glucosamine Sulfate |
0.3857 |
Herrero-Beaumont et al., (2007)37. |
|
2. Costs – VND (USD)
|
| Costs of treatment |
Acetaminophen (3,000 mg/day)
500 mg - 6 times/day |
588,600
(25.06) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
Diclofenac (150 mg/day)
50 mg - 3 times/day |
60,210
(2.56) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
Omeprazole (20 mg/day)
20 mg - 1 times/day |
344,700
(14.68) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
Etoricoxib (60 mg/day)
30-60 mg - 1-2 times/day |
785,700
(33.45) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
| Crystalline glucosamine sulfate (1500 mg/day) 500 mg – 3 times/day |
186,300
(7.93) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
| Triamcinolone injection (40mg every 3 months) - 80 mg/2ml |
19,400
(0.83) |
Vietnam Drug Administration, Ministry of Health, Vietnam43
|
| Total Knee Arthroplasty (TKA) |
88,712,500
(3,777.25) |
Decree 39/2018/TT-BYT, Ministry of Health, Vietnam44
|
| Direct non-medical costs (VND) |
| Food costs per person (1 month) |
2,700,000
(114.96) |
Research Center for Employment Relations (ERC)45
|
| Transportation costs per person (1 month) |
2,953,620
(125.76) |
Wilbert B. et al., (2005)30. |
| Indirect costs |
Cost of absenteeism
(1 month-absent for Knee Joint Recovery Post-Surgery) |
7,342,373
(312.63) |
Hien Thu Trinh et al., (2022)32
|
|
3. Utilities
|
| Utility Acetaminophen |
0.7010 |
Latimer et al., (2009)39. |
| Utility Diclofenac + PPI |
0.7230 |
Latimer et al., (2009)39. |
| Utility Etoricoxib |
0.7230 |
Latimer et al., (2009)39. |
| Utility Glucosamine |
0.6760 |
Olivier Bruyère et al., (2019)40. |
| Utility Triamcinolone injection |
0.6400 |
Losina et al., (2013)42. |
| Utility total knee arthroplasty |
0.7600 |
David Feeny et al., (2004)41. |
3. Results
3.1. Base case
The base-case of standard treatment 1
The standard treatment 1 had a cost of 314,758,471 VND and a Quality-Adjusted Life Year (QALY) of 56.9374.
When Glucosamine was added to the standard treatment 1 before using Diclofenac plus PPI, an increase in both cost and effectiveness was observed. The additional crystalline Glucosamine Sulfate treatment before NSAIDs had a cost of 348,133,295 VND and a QALY of 100.7445. This indicated that the supplementation of Glucosamine increased the treatment cost compared to the standard treatment 1 but also improved treatment effectiveness based on QALY. The cost difference between the additional treatment and the standard treatment was 33,374,824 VND, while the QALY difference was 43.8071. To assess the economic efficiency of adding Glucosamine, the Incremental Cost-Effectiveness Ratio (ICER) was calculated, defined as the cost difference divided by the QALY difference. The ICER of 761,858 VND/QALY suggested a relatively moderate cost to achieve an additional QALY when using the additional Glucosamine treatment before NSAIDs compared to the standard treatment 1. Moreover, it is noteworthy that the obtained ICER was lower than the threshold of 1 GDP per capita in Vietnam. This implied that the supplementation of Glucosamine before NSAIDs could be considered economically efficient.
When supplementing Crystalline Glucosamine Sulfate to the standard treatment 1 (after Diclofenac plus PPI), the cost was 339,027,398 VND with a corresponding Quality-Adjusted Life Year (QALY) of 92.7119. Compared to the standard treatment 1, there was a cost difference of 24,268,927 VND and a QALY difference of 35.7745. This indicates that the additional Glucosamine treatment after NSAIDs had a slightly higher cost but also improved the treatment effectiveness in terms of QALYs to a reasonable extent. The Incremental Cost-Effectiveness Ratio (ICER) was calculated to be 678,386 VND/QALY.
In addition, when comparing the administration of Glucosamine before NSAIDs with its administration after NSAIDs, it was observed that the former had a slightly higher cost but also higher QALYs. The calculated ICER for this case was 1,133,615 VND/QALY, indicating the cost needed to achieve an additional QALY.
The base case of standard treatment 2
In standard treatment 2, which includes the addition of Etoricoxib compared to the standard treatment 1, it was observed that the cost increased when Etoricoxib was introduced (367,478,671 VND). However, at the same time, the QALYs doubled, increasing from 56.9374 to 129.8038. The Incremental Cost-Effectiveness Ratio (ICER) for this comparison was 723,519 VND/QALY.
The outcomes of incorporating Glucosamine into the standard treatment 2 showed similarities to those observed in the standard treatment 1. Incorporating Crystalline Glucosamine Sulfate into the standard treatment 2 before using Diclofenac plus PPI led to notable increases in both cost and effectiveness. The addition of Crystalline Glucosamine Sulfate before NSAIDs resulted in a cost of 443,969,715 VND and a QALY of 230.6720. This indicates that while the supplementation of Glucosamine increased the treatment cost compared to the standard treatment 2, it also significantly improved treatment effectiveness in terms of QALY. The cost difference between the additional treatment and the standard treatment amounted to 76,491,044 VND, with a QALY difference of 100.8682 (a substantial increase in QALY). The calculated ICER was 758,326 VND/QALY, the ICER was found to be lower than the threshold of 1 GDP per capita in Vietnam.
Besides that, when adding Crystalline Glucosamine Sulfate into the standard treatment 2 (after NSAIDs), the treatment cost amounted to 425,013,733 VND and QALY was 211.3288. Compared to the standard treatment 2, the cost difference was 57,535,061 VND, accompanied by a QALY difference of 81.5250. This suggests that the additional Glucosamine treatment incurred a slightly higher cost while yielding improved QALY outcomes. The resulting ICER was calculated at 705,735 VND/QALY.
Moreover, when comparing the adding Glucosamine before NSAIDs into treatment versus the adding Glucosamine after NSAIDs, the QALYs was decreased from 230.6720 to 211.3288. The ICER was 979,981 VND/QALY.
All the results were summarized in
Table 2 below.
3.2. Sensitivity analyses
Based on the analysis of one-way sensitivity using tornado diagrams in all four scenarios of adding Glucosamine to standard treatment 1 and standard treatment 2 when glucosamine was adding before NSAIDs (
Figure 2) and before NSAIDs (
Figure 3), the factor that had the most significant impact on ICER was cost and utility of total knee arthroplasty because of high cost of knee replacement and the relief of pain after total knee arthroplasty. The next factor affected by ICER was cost and utility of acetaminophen use and other oral medications. Almost all these medications help the patient relief pain during the whole period of disease.
This shows that the cost and efficacy of Glucosamine have a substantial impact on the cost-effectiveness analysis compared to the standard treatment sequence. Furthermore, the cost and utility of the final treatment methods in the treatment sequence (Triamcinolone injection) have minimal effect on the analysis results because the proportion of patients transitioning to advanced treatment methods is low. The earlier treatment methods have a higher proportion of patients using them, leading to a higher level of impact on ICER. The later advanced treatment methods in the sequence have a lower impact on ICER outcomes. The one-way sensitivity also showed the same trend when cost and utility of glucosamine in patients who use glucosamine before NSAIDs were better than who use glucosamine after NSAIDs in osteoarthritis treatment.
4. Discussion
In order to identify an optimal treatment sequence for joint degeneration, it is crucial to analyze both the effects of symptom reduction, disease progression prevention, and the minimization of adverse effects while maintaining cost-effectiveness. The model serves as a valuable analytical tool to assess the cost-effectiveness of various treatment methods over an extended period of time. Based on the cost-effectiveness analysis conducted within the context of Vietnam's readiness-to-pay threshold, all treatment sequences that involved the supplementation of crystalline Glucosamine Sulfate into the standard treatment demonstrated favorable cost-effectiveness. This suggests that incorporating crystalline Glucosamine Sulfate into the standard treatment for osteoarthritis can provide economic benefits compared to the standard treatment sequence.
According to research, the treatment sequence could affect the treatment outcomes of patients. Initiating the use of Crystalline Glucosamine Sulfate before NSAIDs could be considered a dominant strategy in the treatment of osteoarthritis. By doing so, Glucosamine can leverage its benefits in reducing pain symptoms and improving joint function from the early stages of the disease, thereby enhancing the patient's quality of life. This can help prevent the rapid progression of the disease and reduce the risk of more complex treatment methods, such as joint replacement surgery, a major and costly surgical procedure. One strength of Crystalline Glucosamine Sulfate compared to other treatment methods is its lower incidence of side effects. While other treatment methods may cause adverse effects such as gastric ulcers, digestive and cardiovascular disturbances, Glucosamine have fewer side effects and is considered safer in the majority of cases46-48. Furthermore, the early use of Glucosamine can also help reduce the need for NSAIDs. This is significant importance as prolonged use of NSAIDs can lead to adverse effects, especially for patients at high risk of gastrointestinal and cardiovascular issues49.
The results from this study are consistent with the results from several previous studies on the cost-effectiveness of Glucosamine such as: Scholtissen et al. (2010)49 demonstrated that Glucosamine is cost-effectiveness compared to Paracetamol and placebo. Bruyère et al. (2019, 2021)40,50 concluded that Crystalline Glucosamine Sulfate is cost-effective compared to placebo and other forms of Glucosamine at 3-month, 6-month, and 3-year time points. Additionally, Segal et al. (2004)51, B.D. Zhang et al. (2012)26 and Luksameesate et al.(2022)52 also demonstrated the cost-effectiveness that Glucosamine achieves in the treatment of osteoarthritis. This indicates the feasibility of Crystalline Glucosamine Sulfate in improving cost-effectiveness compared to other treatment methods. Furthermore, Black et al. (2009)53 and Chaiyakunapruk N et al. (2010)54 stated that Glucosamine is clinically effective but does not achieve the desired cost-effectiveness. The observed difference could be attributed to varying state management policies and the differences in the structure of the research model.
The study had a number of limitations that should be considered. Firstly, not all treatment methods and medications used in the management of joint degeneration were included in the study. The focus was primarily on the commonly employed methods in clinical practice, which were considered appropriate for incorporation into the research model. Secondly, the study relied on a comprehensive literature review approach, which involved gathering information from various data sources. This was necessary due to the limited availability of data specific to Vietnam. Therefore, data from different countries were included to compensate for the lack of local data. However, it is important to note that this approach may introduce potential variations in terms of social conditions, lifestyles, and policies between countries. Additionally, the study selectively chose literature sources from neighboring countries with similarities in social context, lifestyles, and policies, which were deemed relevant for reference purposes. This approach aimed to provide valuable insights; however, it is crucial to acknowledge that the applicability of findings to the specific context of Vietnam may be influenced by these variations. These limitations highlight the need for further research that encompasses a broader range of treatment methods, utilizes local data, and considers the specific socio-cultural and policy contexts of Vietnam. Such studies would contribute to a more comprehensive understanding of the effectiveness and cost-effectiveness of treatments for joint degeneration in the Vietnamese population.
5. Conclusions
In conclusion, the study provided evidence that the addition of Crystalline Glucosamine Sulfate to the standard treatment, regardless of the stage of osteoarthritis, results in cost-effective outcomes within the acceptable willingness-to-pay threshold in Vietnam. Moreover, the study highlights that early supplementation of Glucosamine leads to a significant reduction in the Incremental Cost-Effectiveness Ratio (ICER) and substantially improves the cost-effectiveness of joint degeneration treatment compared to supplementation at later stages.
6. Abbreviations
OA: osteoarthritis; GDP: gross domestic product; DAV: Vietnam Drug Administration. ESCEO: European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases; SYSADOA: symptomatic slow acting drugs for osteoarthritis; QALY: quality-adjusted life-year; DALY: disability-adjusted life year; ICER: Incremental Cost-Effectiveness Ratio; WOMAC: Western Ontario and McMaster Universities Arthritis Index; NSAID(s): non-steroidal anti-inflammatory drug(s)
Author Contributions
Conceptualization, Vo, N.X. and Bui, T.T.; methodology, Vo, N.X.; software, Che, U.T.T. and Ngo, T.T.T.; validation, Vo, N.X. and Bui, T.T.; formal analysis, Vo, N.X., Bui, T.T., Che, U.T.T. and Ngo, T.T.T.; investigation, Vo, N.X.; resources, Vo, N.X., Bui, T.T., Che, U.T.T. and Ngo, T.T.T.; data curation, Che, U.T.T. and Ngo, T.T.T.; writing—original draft preparation, Che, U.T.T.; Ngo, T.T.T. and Bui, T.T.; writing—review and editing, Vo, N.X.; and Bui, T.T.; visualization, Vo, N.X. and Bui, T.T.; supervision, Vo, N.X.; project administration, Vo, N.X. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
All the authors declare no conflict of interest.
Ethical approval
This research did not include trials conducted on living humans which were performed by any of participated authors.
References
- Freitag J, Bates D, Boyd R, et al. Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy - a review. BMC Musculoskelet Disord 2016, 17, 230. [CrossRef] [PubMed]
- Reginster JY, Deroisy R, Rovati LC, et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Lancet. 2001, 357, 251–6. [Google Scholar] [CrossRef] [PubMed]
- Nyvang J, Hedstrom M, Gleissman SA. It's not just a knee, but a whole life: A qualitative descriptive study on patients' experiences of living with knee osteoarthritis and their expectations for knee arthroplasty. Int J Qual Stud Health Well-being 2016, 11, 30193. [CrossRef] [PubMed]
- Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain. 2002, 100, 55–64. [Google Scholar] [CrossRef]
- Murphy L, Helmick CG. The impact of osteoarthritis in the United States: a population-health perspective: A population-based review of the fourth most common cause of hospitalization in U.S. adults. Orthop Nurs. 2012, 31, 85–91. [Google Scholar] [CrossRef]
- Fibel KH, Hillstrom HJ, Halpern BC. State-of-the-Art management of knee osteoarthritis. World J Clin Cases. 2015, 3, 89–101. [Google Scholar] [CrossRef]
- McCorry MC, Puetzer JL, Bonassar LJ. Characterization of mesenchymal stem cells and fibrochondrocytes in three-dimensional co-culture: analysis of cell shape, matrix production, and mechanical performance. Stem Cell Res Ther. 2016, 7, 39. [Google Scholar] [CrossRef]
- Peterfy CG, Gold G, Eckstein F, Cicuttini F, Dardzinski B, Stevens R. MRI protocols for whole-organ assessment of the knee in osteoarthritis. Osteoarthritis Cartilage 2006, 14 Suppl. A, A95–A111. [CrossRef]
- Edd SN, Giori NJ, Andriacchi TP. The role of inflammation in the initiation of osteoarthritis after meniscal damage. J Biomech. Jun 1 2015, 48, 1420–6. [Google Scholar] [CrossRef]
- Waddell DD, Bert JM. The use of hyaluronan after arthroscopic surgery of the knee. Arthroscopy. 2010, 26, 105–11. [Google Scholar] [CrossRef]
- Uth K, Trifonov D. Stem cell application for osteoarthritis in the knee joint: A minireview. World J Stem Cells. 2014, 6, 629–36. [Google Scholar] [CrossRef]
- Anderson JA, Little D, Toth AP, et al. Stem cell therapies for knee cartilage repair: the current status of preclinical and clinical studies. Am J Sports Med. 2014, 42, 2253–61. [Google Scholar] [CrossRef] [PubMed]
- Kane P, Frederick R, Tucker B, et al. Surgical restoration/repair of articular cartilage injuries in athletes. Phys Sportsmed. 2013, 41, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Gupta PK, Das AK, Chullikana A, Majumdar AS. Mesenchymal stem cells for cartilage repair in osteoarthritis. Stem Cell Res Ther. 2012, 3, 25. [Google Scholar] [CrossRef] [PubMed]
- Smith B, Sigal IR, Grande DA. Immunology and cartilage regeneration. Immunol Res. 2015, 63, 181–6. [Google Scholar] [CrossRef]
- Greene MA, Loeser RF. Aging-related inflammation in osteoarthritis. Osteoarthritis Cartilage. 2015, 23, 1966–71. [Google Scholar] [CrossRef]
- Chen WH, Lo WC, Hsu WC, et al. Synergistic anabolic actions of hyaluronic acid and platelet-rich plasma on cartilage regeneration in osteoarthritis therapy. Biomaterials. 2014, 35, 9599–607. [Google Scholar] [CrossRef]
- March LM, Schwarz JM, Carfrae BH, Bagge E. Clinical validation of self-reported osteoarthritis. Osteoarthritis Cartilage. 1998, 6, 87–93. [Google Scholar] [CrossRef]
- Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008, 58, 26–35. [Google Scholar] [CrossRef]
- Ho-Pham LT, Lai TQ, Mai LD, Doan MC, Pham HN, Nguyen TV. Prevalence of radiographic osteoarthritis of the knee and its relationship to self-reported pain. PLoS One 2014, 9, e94563. [Google Scholar] [CrossRef]
- National and state medical expenditures and lost earnings attributable to arthritis and other rheumatic conditions--United States, 2003. MMWR Morb Mortal Wkly Rep. 2007, 56, 4–7.
- Focht, BC. Move to Improve: How Knee Osteoarthritis Patients Can Use Exercise to Enhance Quality of Life. ACSMs Health Fit J. 2012, 16, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Guidelines for the diagnosis and treatment of musculoskeletal disorders 124 (2016).
- Laura, A. Perry R, PharmD, BCPS; Charles Mosler, RPh, PharmD, CGP, FASCP; Ashton Atkins, PharmD; Megan Minehart, PharmD. Cardiovascular Risk Associated With NSAIDs and COX-2 Inhibitors. US Pharmacist. 2014, 39, 35–38. [Google Scholar]
- N. Zhao MC, J.B. Wong, C. Wang. Economic burden of medications and nutraceuticals in knee osteoarthritis. Wang. Economic burden of medications and nutraceuticals in knee osteoarthritis. Osteoarthritis and Cartilage 2015, 23. [Google Scholar] [CrossRef]
- Zhang B-D LZJ, Zhang H-T, He M-T, Li D-S. Cost-effectiveness analysis on the treatment of knee osteoarthritis by glucosamine hydrochloride and glucosamine sulfate. Chinese journal of tissue engineering research. 2012, 16, 9867–9872. [Google Scholar] [CrossRef]
- Cohen M, Wolfe R, Mai T, Lewis D. A randomized, double blind, placebo controlled trial of a topical cream containing glucosamine sulfate, chondroitin sulfate, and camphor for osteoarthritis of the knee. J Rheumatol. 2003, 30, 523–8. [Google Scholar]
- Pavelká K, Gatterová J, Olejarová M, Machacek S, Giacovelli G, Rovati LC. Glucosamine sulfate use and delay of progression of knee osteoarthritis: a 3-year, randomized, placebo-controlled, double-blind study. Arch Intern Med. 2002, 162, 2113–23. [Google Scholar] [CrossRef] [PubMed]
- Bank, W. Life expectancy at birth, total (years) - Vietnam. Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?
- van den Hout WB, de Jong Z, Munneke M, Hazes JM, Breedveld FC, Vliet Vlieland TP. Cost-utility and cost-effectiveness analyses of a long-term, high-intensity exercise program compared with conventional physical therapy in patients with rheumatoid arthritis. Arthritis Rheum. 2005, 53, 39–47. [Google Scholar] [CrossRef]
- Bank, W. Consumer Price Index in Vietnam. World Bank. Available online: https://data.worldbank.org/indicator/FP.CPI.TOTL? (accessed on 16 May 2023).
- Hien, TT. , Lien T. K. N. Evaluation of the rehabilitation results of patients with knee osteoarthritis after general knee replacement operation. Vietnam Medical Journal. 2022, 519, 368–372. [Google Scholar] [CrossRef]
- BANK, TW. GDP per capita (current US$) - Vietnam. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD? (accessed on 1 July 2023).
- Cannon CP, Curtis SP, FitzGerald GA, et al. Cardiovascular outcomes with etoricoxib and diclofenac in patients with osteoarthritis and rheumatoid arthritis in the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) programme: a randomised comparison. Lancet. 2006, 368, 1771–81. [Google Scholar] [CrossRef]
- Zacher J, Feldman D, Gerli R, et al. A comparison of the therapeutic efficacy and tolerability of etoricoxib and diclofenac in patients with osteoarthritis. Curr Med Res Opin. 2003, 19, 725–36. [Google Scholar] [CrossRef] [PubMed]
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial. Jama. 2017, 317, 1967–1975. [Google Scholar] [CrossRef] [PubMed]
- Herrero-Beaumont G, Ivorra JA, Del Carmen Trabado M, et al. Glucosamine sulfate in the treatment of knee osteoarthritis symptoms: a randomized, double-blind, placebo-controlled study using acetaminophen as a side comparator. Arthritis Rheum. 2007, 56, 555–67. [Google Scholar] [CrossRef]
- Fortin PR, Clarke AE, Joseph L, et al. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999, 42, 1722–8. [Google Scholar] [CrossRef]
- Latimer N, Lord J, Grant RL, et al. Cost effectiveness of COX 2 selective inhibitors and traditional NSAIDs alone or in combination with a proton pump inhibitor for people with osteoarthritis. BMJ 2009, 339, b2538. [CrossRef] [PubMed]
- Bruyere O, Reginster JY, Honvo G, Detilleux J. Cost-effectiveness evaluation of glucosamine for osteoarthritis based on simulation of individual patient data obtained from aggregated data in published studies. Aging Clin Exp Res. 2019, 31, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Feeny D, Wu L, Eng K. Comparing short form 6D, standard gamble, and Health Utilities Index Mark 2 and Mark 3 utility scores: results from total hip arthroplasty patients. Qual Life Res. 2004, 13, 1659–70. [Google Scholar] [CrossRef] [PubMed]
- Losina E, Daigle ME, Suter LG, et al. Disease-modifying drugs for knee osteoarthritis: can they be cost-effective? Osteoarthritis Cartilage. 2013, 21, 655–67. [Google Scholar] [CrossRef]
- MOH_Vietnam. Drug Prices. Available online: https://dichvucong.dav.gov.vn/congbogiathuoc/index (accessed on 12 May 2023).
- Determining the price of medical examination and treatment services covered by health insurance among patients of the same class nationwide and guiding the application of prices and payment of medical examination and treatment expenses in some cases (2018).
- (ERC) RCfER. Living Wage Report, Rural Vietnam, Soc Trang to Thai Binh. Available online: https://www.isealalliance.org/sites/default/files/resource/2017-12/Rural_Vietnam_Living_Wage_Benchmark_Report.pdf (accessed on 16 May 2023).
- Moreno A, Vargas E, Soto J, Rejas J. [Cost-effectiveness analysis of the use of celecoxib for the treatment of osteoarthritis]. Análisis coste-efectividad del empleo de celecoxib en el tratamiento de la artrosis. Gac Sanit. 2003, 17, 27–36. [Google Scholar] [CrossRef]
- Sawitzke AD, Shi H, Finco MF, et al. Clinical efficacy and safety of glucosamine, chondroitin sulphate, their combination, celecoxib or placebo taken to treat osteoarthritis of the knee: 2-year results from GAIT. Ann Rheum Dis. 2010, 69, 1459–64. [Google Scholar] [CrossRef]
- 48. Bruyère O, Altman RD, Reginster JY. Efficacy and safety of glucosamine sulfate in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Semin Arthritis Rheum 2016, 45 Suppl. 4, S12–S17. [CrossRef]
- Scholtissen S, Bruyère O, Neuprez A, et al. Glucosamine sulphate in the treatment of knee osteoarthritis: cost-effectiveness comparison with paracetamol. Int J Clin Pract. 2010, 64, 756–62. [Google Scholar] [CrossRef]
- Bruyère O, Detilleux J, Reginster JY. Cost-Effectiveness Assessment of Different Glucosamines in Patients with Knee Osteoarthritis: A Simulation Model Adapted to Germany. Curr Aging Sci. 2021, 14, 242–248. [Google Scholar] [CrossRef]
- Segal L, Day SE, Chapman AB, Osborne RH. Can we reduce disease burden from osteoarthritis? Med J Aust. 2004, 180, S11–7. [Google Scholar] [CrossRef]
- Luksameesate P, Tanavalee A, Taychakhoonavudh S. An economic evaluation of knee osteoarthritis treatments in Thailand. Front Pharmacol. 2022, 13, 926431. [Google Scholar] [CrossRef] [PubMed]
- Black C, Clar C, Henderson R, et al. The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation. Health Technol Assess. 2009, 13, 1–148. [Google Scholar] [CrossRef]
- 54. Chaiyakunapruk N, Saokaew, S., and Pansang, S. Cost-effectiveness analysis of glucosamine sulphate for the treatment of osteoarthritis in Thailand. Value Health 2010, 13. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).