Submitted:
26 July 2023
Posted:
27 July 2023
You are already at the latest version
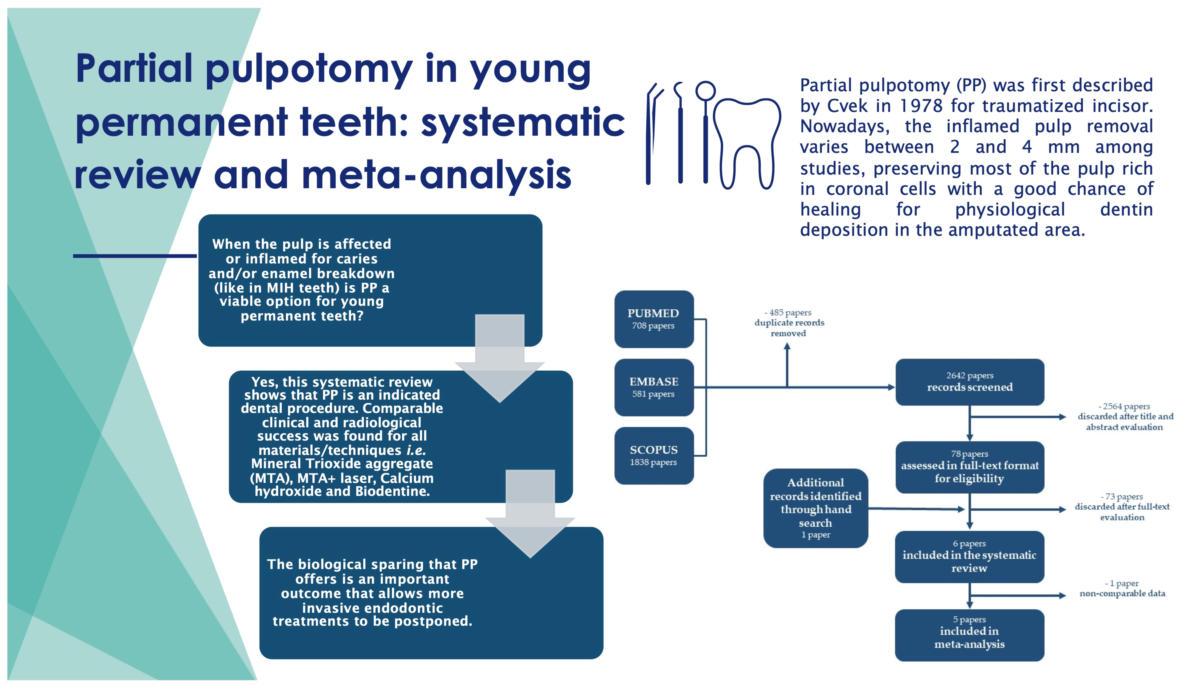
Abstract
Keywords:
1. Introduction
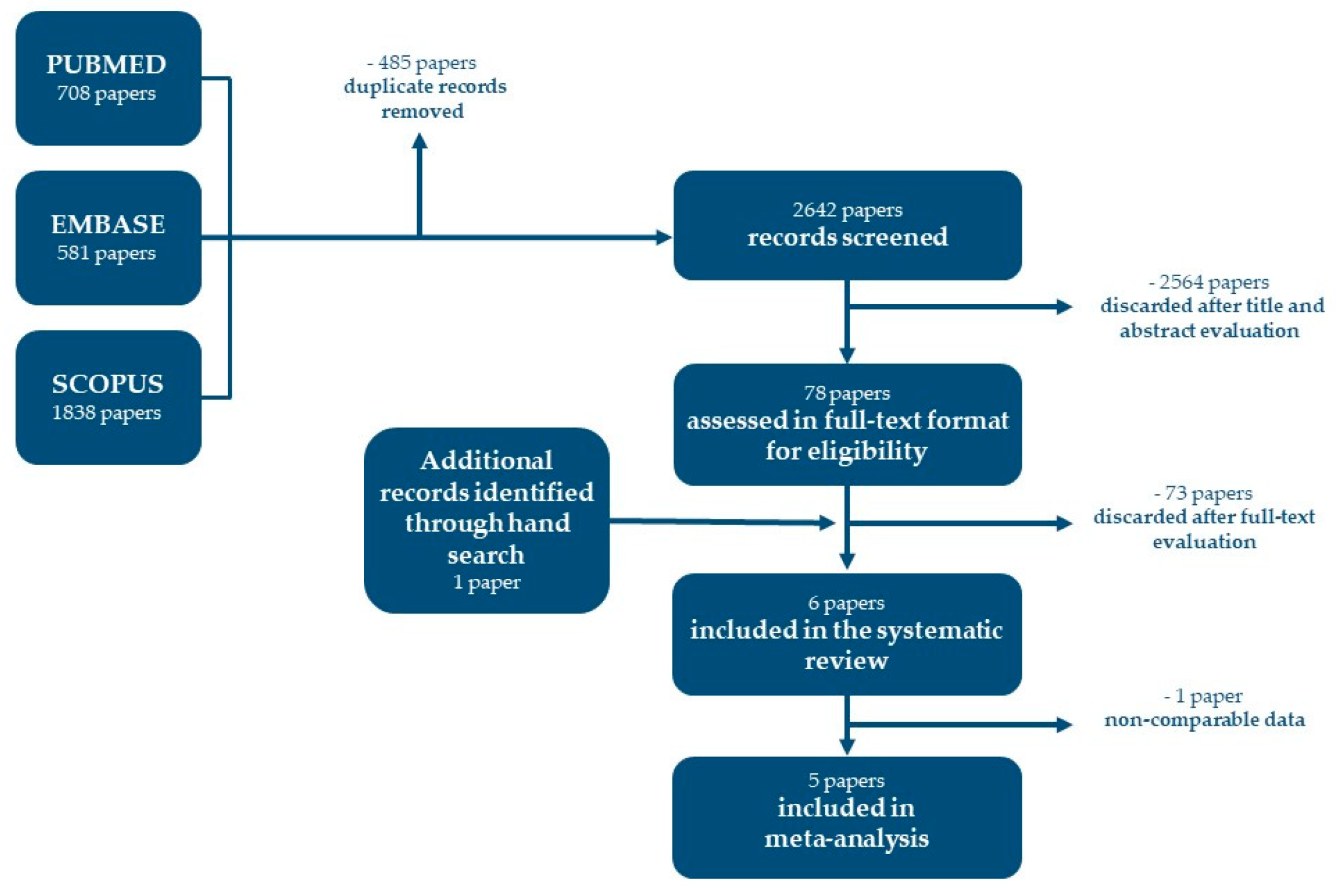
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Study Selection and Data Extraction
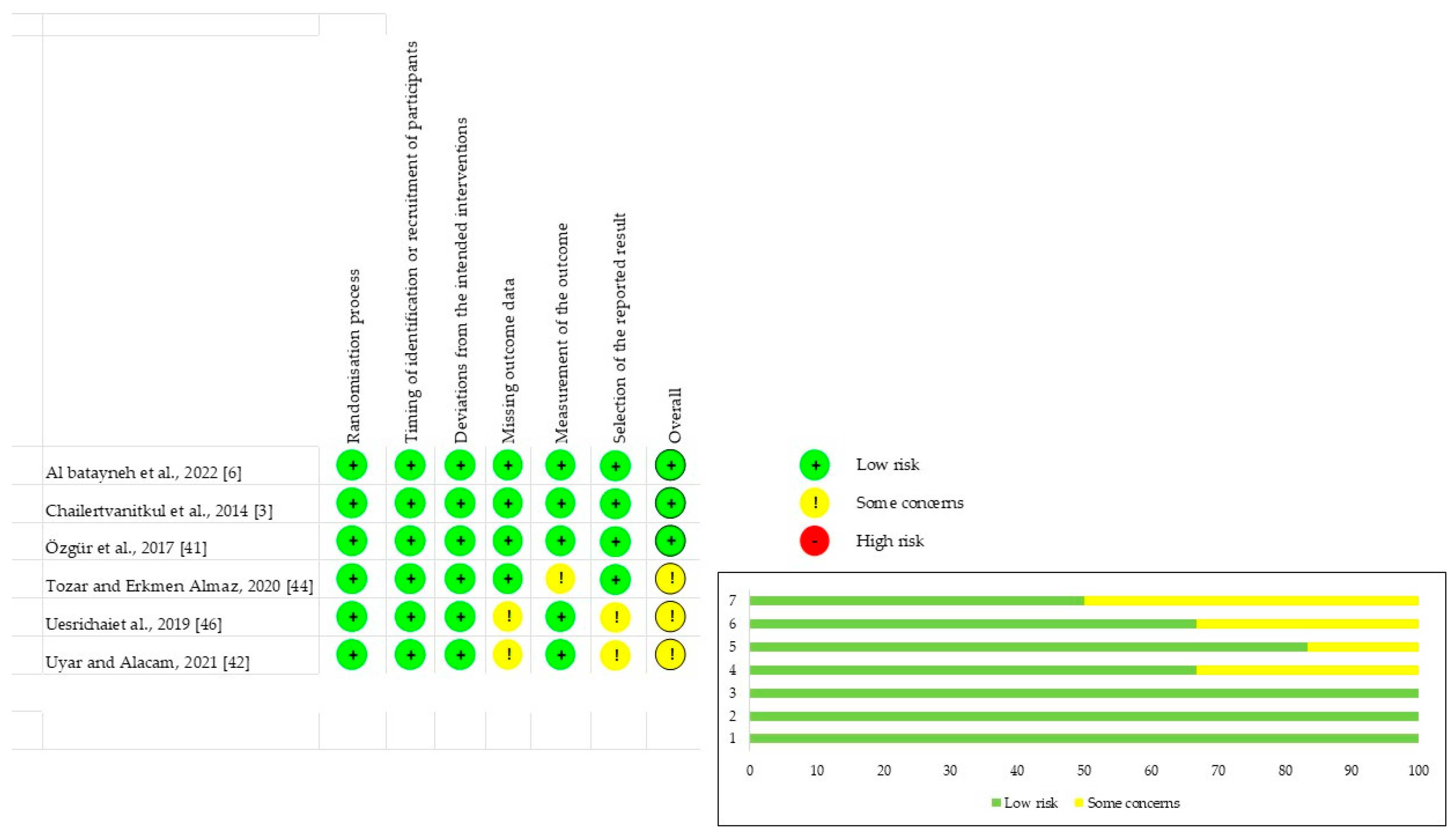
2.5. Risk of Bias
2.6. Outcome Measures
2.7. Heterogeneity
2.8. Synthesis of the Results
3. Results
3.1. Study Characteristics
3.2. Risk of Bias Assessment
3.3. Qualitative Synthesis
3.4. Quantitative Synthesis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Uribe, S.E.; Innes, N.; Maldupa, I. The global prevalence of early childhood caries: A systematic review with meta-analysis using the WHO diagnostic criteria. Int J Paediatr Dent 2021, 31, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Dong, B.; Yu, D.; Ren, Q.; Sun, Y. The prevalence of molar incisor hypomineralization: evidence from 70 studies. Int J Paediatr Dent 2018, 28, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Chailertvanitkul, P.; Paphangkorakit, J.; Sooksantisakoonchai, N.; Pumas, N.; Pairojamornyoot, W.; Leela-Apiradee, N.; Abbott, P.V. Randomized control trial comparing calcium hydroxide and mineral trioxide aggregate for partial pulpotomies in cariously exposed pulps of permanent molars. Int Endod J 2014, 47, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Pujar, P.; Subbareddy, V.V. Evaluation of the tooth brushing skills in children aged 6-12 years. Eur Arch Paediatr Dent 2013, 14, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Boustedt, K.; Dahlgren, J.; Twetman, S.; Roswall, J. Tooth brushing habits and prevalence of early childhood caries: a prospective cohort study. Eur Arch Paediatr Dent 2020, 21, 155–159. [Google Scholar] [CrossRef]
- Al-Batayneh, O.B.; Abdelghani, I.M. Outcome of vital pulp therapy in deeply carious molars affected with molar incisor hypomineralisation (MIH) defects: a randomized clinical trial. European Archives of pediatric dentistry : official journal of the European Academy of Paediatric Dentistry 2022, 23, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Ghanim, A.M.; Manton, D.J.; Morgan, M.V.; Marino, R.J.; Bailey, D.L. Trends of oral health care and dental treatment needs in relation to molar incisor hypomineralisation defects: a study amongst a group of Iraqi schoolchildren. Eur Arch Paediatr Dent 2012, 13, 171–178. [Google Scholar] [CrossRef]
- Ricucci, D.; Siqueira, J.F.; Li, Y.; Tay, F.R. Vital pulp therapy: histopathology and histobacteriology-based guidelines to treat teeth with deep caries and pulp exposure. Journal of Dentistry 2019, 86, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.J.X.; Yap, A.U. Vital pulp therapy in carious pulp-exposed permanent teeth: an umbrella review. Clin Oral Investig 2021, 25, 6743–6756. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.M.; Ricucci, D.; Saoud, T.M.; Sigurdsson, A.; Kahler, B. Vital pulp therapy of mature permanent teeth with irreversible pulpitis from the perspective of pulp biology. Aust Endod J 2020, 46, 154–166. [Google Scholar] [CrossRef]
- Alqaderi, H.E.; Al-Mutawa, S.A.; Qudeimat, M.A. MTA pulpotomy as an alternative to root canal treatment in children's permanent teeth in a dental public health setting. J Dent 2014, 42, 1390–1395. [Google Scholar] [CrossRef]
- Rodd, H.D.; Boissonade, F.M.; Day, P.F. Pulpal status of hypomineralized permanent molars. Pediatr Dent 2007, 29, 514–520. [Google Scholar]
- Tong, H.J.; Seremidi, K.; Stratigaki, E.; Kloukos, D.; Duggal, M.; Gizani, S. Deep dentine caries management of immature permanent posterior teeth with vital pulp: A systematic review and meta-analysis. J Dent 2022, 124, 104214. [Google Scholar] [CrossRef] [PubMed]
- Ghoddusi, J.; Forghani, M.; Parisay, I. New approaches in vital pulp therapy in permanent teeth. Iran Endod J 2014, 9, 15–22. [Google Scholar] [PubMed]
- Baume, L.J.; Holz, J. Long-term clinical assessment of direct pulp capping. Int Dent J 1981, 31, 251–260. [Google Scholar] [PubMed]
- Fong, C.D.; Davis, M.J. Partial pulpotomy for immature permanent teeth, its present and future. Pediatr Dent 2002, 24, 29–32. [Google Scholar]
- Witherspoon, D.E. Vital pulp therapy with new materials: new directions and treatment perspectives--permanent teeth. J Endod 2008, 34, S25–28. [Google Scholar] [CrossRef]
- Witherspoon, D.E.; Small, J.C.; Harris, G.Z. Mineral trioxide aggregate pulpotomies: a case series outcomes assessment. J Am Dent Assoc 2006, 137, 610–618. [Google Scholar] [CrossRef]
- Bogen, G.; Kim, J.S.; Bakland, L.K. Direct pulp capping with mineral trioxide aggregate: an observational study. J Am Dent Assoc 2008, 139, 305–315, quiz 305-315. [Google Scholar] [CrossRef]
- Cox, C.F.; Suzuki, S. Re-evaluating pulp protection: calcium hydroxide liners vs. cohesive hybridization. J Am Dent Assoc 1994, 125, 823–831. [Google Scholar] [CrossRef]
- Cox, C.F.; Subay, R.K.; Ostro, E.; Suzuki, S.; Suzuki, S.H. Tunnel defects in dentin bridges: their formation following direct pulp capping. Oper Dent 1996, 21, 4–11. [Google Scholar] [PubMed]
- Stanley, H.R. Pulp capping: conserving the dental pulp--can it be done? Is it worth it? Oral Surg Oral Med Oral Pathol 1989, 68, 628–639. [Google Scholar] [CrossRef] [PubMed]
- Schuurs, A.H.; Gruythuysen, R.J.; Wesselink, P.R. Pulp capping with adhesive resin-based composite vs. calcium hydroxide: a review. Endod Dent Traumatol 2000, 16, 240–250. [Google Scholar] [CrossRef]
- Palczewska-Komsa, M.; Kaczor-Wiankowska, K.; Nowicka, A. New Bioactive Calcium Silicate Cement Mineral Trioxide Aggregate Repair High Plasticity (MTA HP)-A Systematic Review. Materials (Basel) 2021, 14. [Google Scholar] [CrossRef]
- Aeinehchi, M.; Eslami, B.; Ghanbariha, M.; Saffar, A.S. Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J 2003, 36, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Moghaddame-Jafari, S.; Mantellini, M.G.; Botero, T.M.; McDonald, N.J.; Nor, J.E. Effect of ProRoot MTA on pulp cell apoptosis and proliferation in vitro. J Endod 2005, 31, 387–391. [Google Scholar] [CrossRef]
- Torabinejad, M.; Parirokh, M.; Dummer, P.M.H. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int Endod J 2018, 51, 284–317. [Google Scholar] [CrossRef]
- Parirokh, M.; Torabinejad, M.; Dummer, P.M.H. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J 2018, 51, 177–205. [Google Scholar] [CrossRef]
- Vanderweele, R.A.; Schwartz, S.A.; Beeson, T.J. Effect of blood contamination on retention characteristics of MTA when mixed with different liquids. J Endod 2006, 32, 421–424. [Google Scholar] [CrossRef]
- Torabinejad, M.; Hong, C.U.; McDonald, F.; Pitt Ford, T.R. Physical and chemical properties of a new root-end filling material. J Endod 1995, 21, 349–353. [Google Scholar] [CrossRef]
- Katge, F.A.; Patil, D.P. Comparative Analysis of 2 Calcium Silicate-based Cements (Biodentine and Mineral Trioxide Aggregate) as Direct Pulp-capping Agent in Young Permanent Molars: A Split Mouth Study. J Endod 2017, 43, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Slaboseviciute, M.; Vasiliauskaite, N.; Drukteinis, S.; Martens, L.; Rajasekharan, S. Discoloration Potential of Biodentine: A Systematic Review. Materials (Basel) 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M.; Singh, H.; Dhillon, J.S.; Batra, M.; Saini, M. MTA versus Biodentine: Review of Literature with a Comparative Analysis. J Clin Diagn Res 2017, 11, ZG01–ZG05. [Google Scholar] [CrossRef]
- Al-Hiyasat, A.S.; Ahmad, D.M.; Khader, Y.S. The effect of different calcium silicate-based pulp capping materials on tooth discoloration: an in vitro study. BMC Oral Health 2021, 21, 330. [Google Scholar] [CrossRef] [PubMed]
- Toomarian, L.; Fekrazad, R.; Sharifi, D.; Baghaei, M.; Rahimi, H.; Eslami, B. Histopathological evaluation of pulpotomy with Er,Cr:YSGG laser vs formocresol. Lasers Med Sci 2008, 23, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Marx, I.; Op't Hof, J. The Er,Cr:YSGG hydrokinetic laser system for dentistry--clinical applications. SADJ 2002, 57, 323–326. [Google Scholar]
- Aslantas, E.E.; Buzoglu, H.D.; Karapinar, S.P.; Cehreli, Z.C.; Muftuoglu, S.; Atilla, P.; Aksoy, Y. Age-related Changes in the Alkaline Phosphatase Activity of Healthy and Inflamed Human Dental Pulp. J Endod 2016, 42, 131–134. [Google Scholar] [CrossRef]
- Aslantas, E.E.; Buzoglu, H.D.; Muftuoglu, S.F.; Atilla, P.; Karapinar, S.P.; Aksoy, Y. Effects of aging and inflammation on catalase activity in human dental pulp. Arch Oral Biol 2022, 141, 105482. [Google Scholar] [CrossRef]
- WHO. SIXTY-FOURTH WORLD HEALTH ASSEMBLY - Youth and health risks 2011.
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. Rob 2: a revised tool for assessing the risk of bias in randomized trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Özgür, B.; Kargın, S.T.; Ölmez, M.S. Clinical evaluation of giomer- and resin-based fissure sealants on permanent molars affected by molar-incisor hypomineralization: a randomized clinical trial. BMC Oral Health 2022, 22, 275. [Google Scholar] [CrossRef]
- Uyar, D.S.; Alacam, A. Evaluation of partial pulpotomy treatment in cariously exposed immature permanent molars: Randomized controlled trial. Niger J Clin Pract 2021, 24, 1511–1519. [Google Scholar] [CrossRef]
- Özgür, B.; Uysal, S.; Güngör, H.C. Partial Pulpotomy in Immature Permanent Molars After Carious Exposures Using Different Hemorrhage Control and Capping Materials. Pediatric dentistry 2017, 39, 364–370. [Google Scholar]
- Tozar, K.N.; Erkmen Almaz, M. Evaluation of the Efficacy of Erbium, Chromium-doped Yttrium, Scandium, Gallium, and Garnet Laser in Partial Pulpotomy in Permanent Immature Molars: A Randomized Controlled Trial. Journal of Endodontics 2020, 46, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.M.; Kim, S.H.; Shin, Y.; Lee, H.S.; Lee, J.H.; Kim, G.T.; Song, J.S. A randomized controlled trial of ProRoot MTA, OrthoMTA and RetroMTA for pulpotomy in primary molars. Oral Dis 2015, 21, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Uesrichai, N.; Nirunsittirat, A.; Chuveera, P.; Srisuwan, T.; Sastraruji, T.; Chompu-inwai, P. Partial pulpotomy with two bioactive cements in permanent teeth of 6- to 18-year-old patients with signs and symptoms indicative of irreversible pulpitis: a noninferiority randomized controlled trial. International Endodontic Journal 2019, 52, 749–759. [Google Scholar] [CrossRef]
- Albaiti, S.S.; Albishri, R.F.; Alhowig, M.T.; Tayyar, W.I.; Alqurashi, N.F.; Alghamdi, F.T. Partial Pulpotomy as an Applicable Treatment Option for Cariously Exposed Posterior Permanent Teeth: A Systematic Review of Randomized Clinical Trials. Cureus 2022, 14, e26573. [Google Scholar] [CrossRef]
- Lin, G.S.S.; Yew, Y.Q.; Lee, H.Y.; Low, T.; Pillai, M.P.M.; Laer, T.S.; Wafa, S. Is pulpotomy a promising modality in treating permanent teeth? An umbrella review. Odontology 2022, 110, 393–409. [Google Scholar] [CrossRef]
- Ricucci, D.; Loghin, S.; Siqueira, J.F., Jr. Correlation between clinical and histologic pulp diagnoses. J Endod 2014, 40, 1932–1939. [Google Scholar] [CrossRef] [PubMed]
- Muliyar, S.; Shameem, K.A.; Thankachan, R.P.; Francis, P.G.; Jayapalan, C.S.; Hafiz, K.A. Microleakage in endodontics. J Int Oral Health 2014, 6, 99–104. [Google Scholar]
- Goel, N.; Jha, S.; Bhol, S.; Dash, B.P.; Sarangal, H.; Namdev, R. Molar Incisor Hypomineralization: Clinical Characteristics with Special Emphasis on Etiological Criteria. J Pharm Bioallied Sci 2021, 13, S651–S655. [Google Scholar] [CrossRef]
- Cho, S.Y.; Seo, D.G.; Lee, S.J.; Lee, J.; Lee, S.J.; Jung, I.Y. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod 2013, 39, 327–331. [Google Scholar] [CrossRef]
- Cabral, R.N.; Nyvad, B.; Soviero, V.; Freitas, E.; Leal, S.C. Reliability and validity of a new classification of MIH based on severity. Clin Oral Investig 2020, 24, 727–734. [Google Scholar] [CrossRef]
- Alanzi, A.; Faridoun, A.; Kavvadia, K.; Ghanim, A. Dentists' perception, knowledge, and clinical management of molar-incisor-hypomineralisation in Kuwait: a cross-sectional study. BMC Oral Health 2018, 18, 34. [Google Scholar] [CrossRef]
- Delgado, R.M.; Botelho, J.; Machado, V.; Mendes, J.J.; Lopes, L.B. Knowledge, perception, and clinical experiences on molar incisor hypomineralization amongst Portuguese dentists. BMC Oral Health 2022, 22, 250. [Google Scholar] [CrossRef]
- Gamboa, G.C.S.; Lee, G.H.M.; Ekambaram, M.; Yiu, C.K.Y. Knowledge, perceptions, and clinical experiences on molar incisor hypomineralization among dental care providers in Hong Kong. BMC Oral Health 2018, 18, 217. [Google Scholar] [CrossRef]
- European Society of Endodontology developed, b.; Duncan, H.F.; Galler, K.M.; Tomson, P.L.; Simon, S.; El-Karim, I.; Kundzina, R.; Krastl, G.; Dammaschke, T.; Fransson, H.; et al. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int Endod J 2019, 52, 923–934. [Google Scholar] [CrossRef]
- Therapy, A.A.o.E.S.C.o.V.P. AAE Position Statement on Vital Pulp Therapy. Guidelines & Position Statements AAE 2021.
- Chevalier, V.; Le Fur Bonnabesse, A.; Duncan, H.F. Frightened of the pulp? A qualitative analysis of undergraduate student confidence and stress during the management of deep caries and the exposed pulp. Int Endod J 2021, 54, 130–146. [Google Scholar] [CrossRef]
- Duncan, H.F. Present status and future directions-Vital pulp treatment and pulp preservation strategies. Int Endod J 2022, 55 Suppl 3, 497–511. [Google Scholar] [CrossRef]

| First Author (year) | Source | Location | Funding source |
|---|---|---|---|
| Al-batayneh et al., 2022 [6] | Eur Arch Paed Dent | Jordan | University grant |
| Chailertvanitkul et al., 2014 [3] | Int Endod J | Thailand | Not reported |
| Özgür et al., 2017 [41] | BMC Oral Health | Turkey | University grant |
| Tozar and Erkmen Almaz, 2020 [44] | J Endod | Turkey | University grant |
| Uesrichaiet al., 2019 [46] | Int Endod J | Thailand | University grant |
| Uyar and Alacam, 2021 [42] | Niger J Clin Pract | Turkey | None |
| Study | Age (Rage or Mean) | Patients (n) | Teeth (n) | Drop-Out of Teeth n (%) | Study Design | Final Restoration | Follow-Up (mo.) | Overall Success Rate at 12 mo. (n/total) | Conclusion | |
|---|---|---|---|---|---|---|---|---|---|---|
| Test | Control | |||||||||
| Al-batayneh et al., 2022 [6]* | 11±3.2 yy | 50 | 50 | 3/50 (6.0%) | PP vs IPC or FP | GIC, SSC | 3, 6, 12, 24 | PP 11/12 | IPC 2/25 | VTP is a valid option in severe carious lesions of permanent first molars with MIH over 24 mo. IPC had a higher success rate (95.8%) than PP or CP (85.7% for both). |
| FP 2/11 | ||||||||||
| Chailertvanitkul et al., 2014 [3] | 7-10 yy | 80 | 84 | 8/84 (9.5%) | MTA vs CH | Amalgam | 3, 6, 12, 24 | MTA 41/44 | CH 37/40 | PP using MTA or CH resulted in favourable treatment outcomes. Unfavorable outcomes increase for pulp exposure >5 mm |
| Özgür et al., 2017 [43] | 6-13 yy | 63 | 80 | 4/80 (5.0%) | MTA vs CH | CR | 6, 12, 18, 24 | MTA/SH 19/20 | CH/SH 19/20 | PP with MTA or CH produces comparable and favorable results in immature permanent teeth. |
| MTA/SS 20/20 | CH/SS 19/19 | |||||||||
| Tozar and Erkmen Almaz, 2020 [44] | 6-15 yy | 90 | 90 | 3/90 (3.3%) | MTA vs MTA + Laser Er, Cr: YSGG | GIC, CR | 1, 3, 6, 12 | MTA 40/45 | MTA+Laser 43/45 | The use of the laser did not contribute to the success rate compared to MTA alone. |
| Uesrichaiet al., 2019 [46] | 10 yy | 69 | 69 | 2/67 (3.0%) | MTA vs BD | C, SSC | 32.2±17.9 | MTA 34/37 | BD 26/30 | Permanent teeth with signs and symptoms of irreversible pulpitis were successfully treated with PP using MTA and BD. |
| Uyar and Alacam, 2021 [42] | 7.9 yy | 105 | 119 | 0/54 (0.0%) | MTA vs CH or BD | SSC | 3, 6, 12 | MTA 17/18 | CH 13/18 | PP treatment is a good option and has high success rates at 12 months with CH, MTA and BD. |
| BD 17/18 | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





