Submitted:
26 July 2023
Posted:
27 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
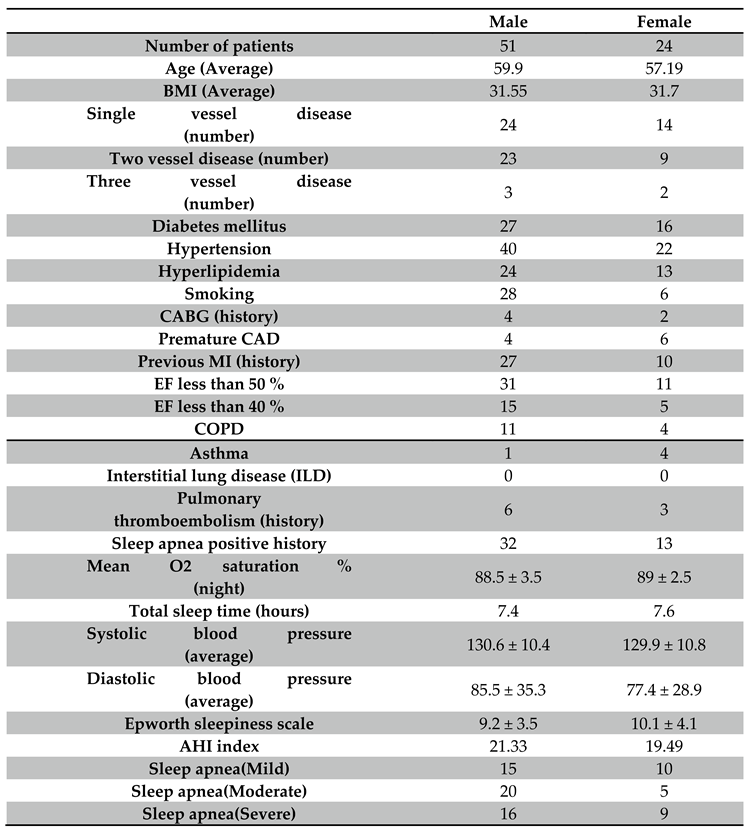
2. Material and methods
2.1. Inclusion and exclusions criteria:
2.2. Sleep apnea diagnosis:
2.3. QT dispersion and TpTe measurements:
2.4. Statistical analysis:
3. Results
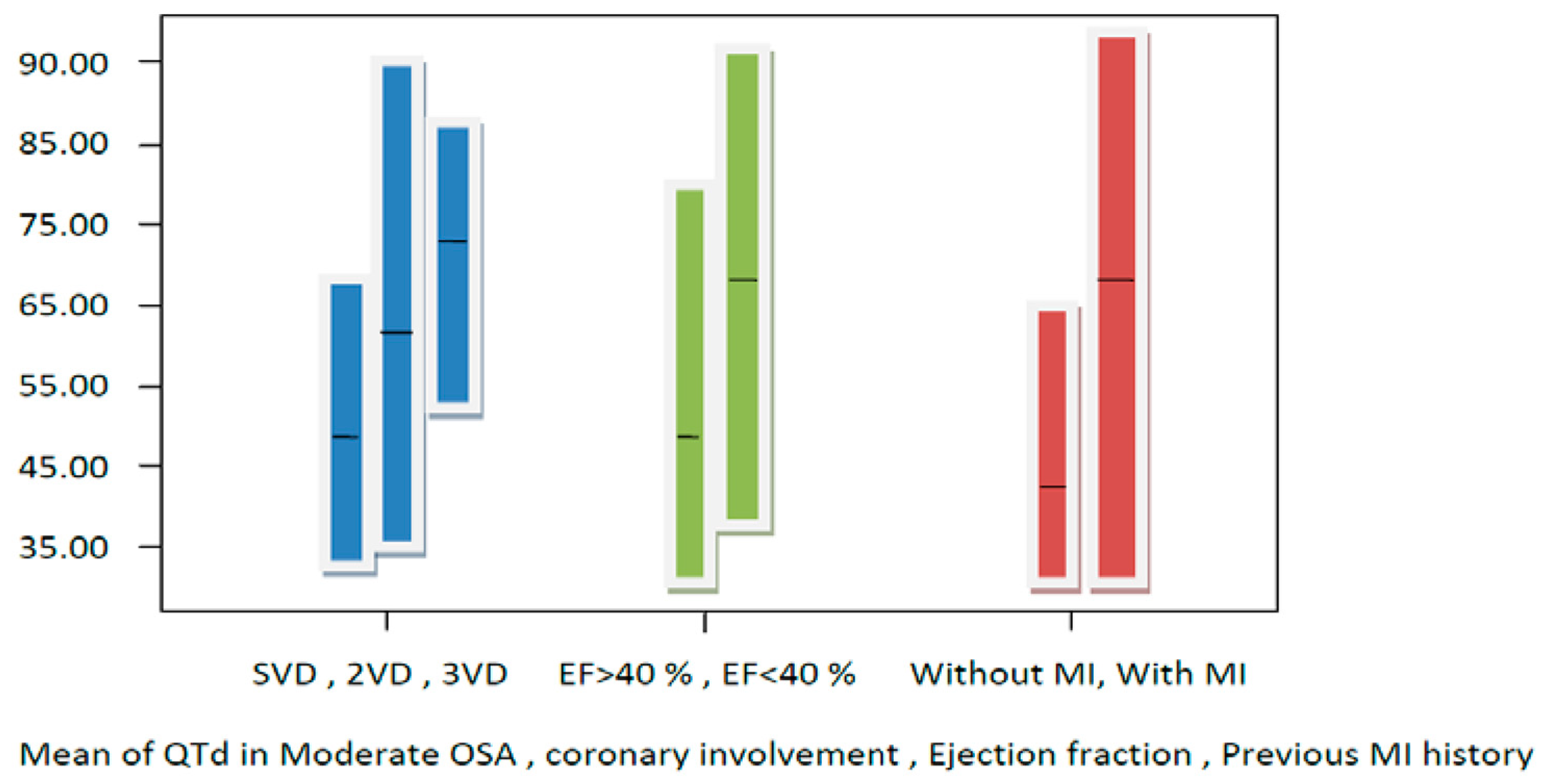
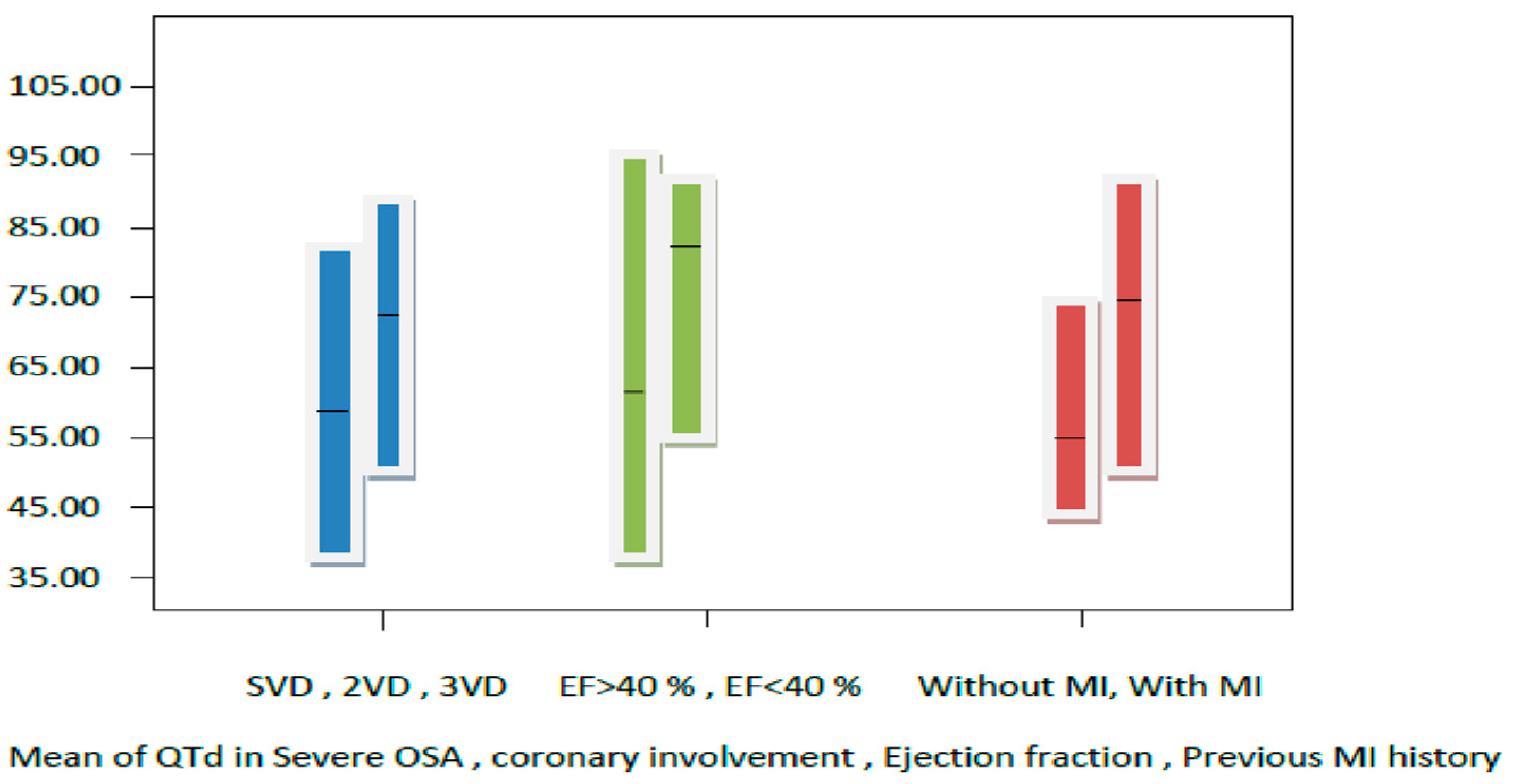
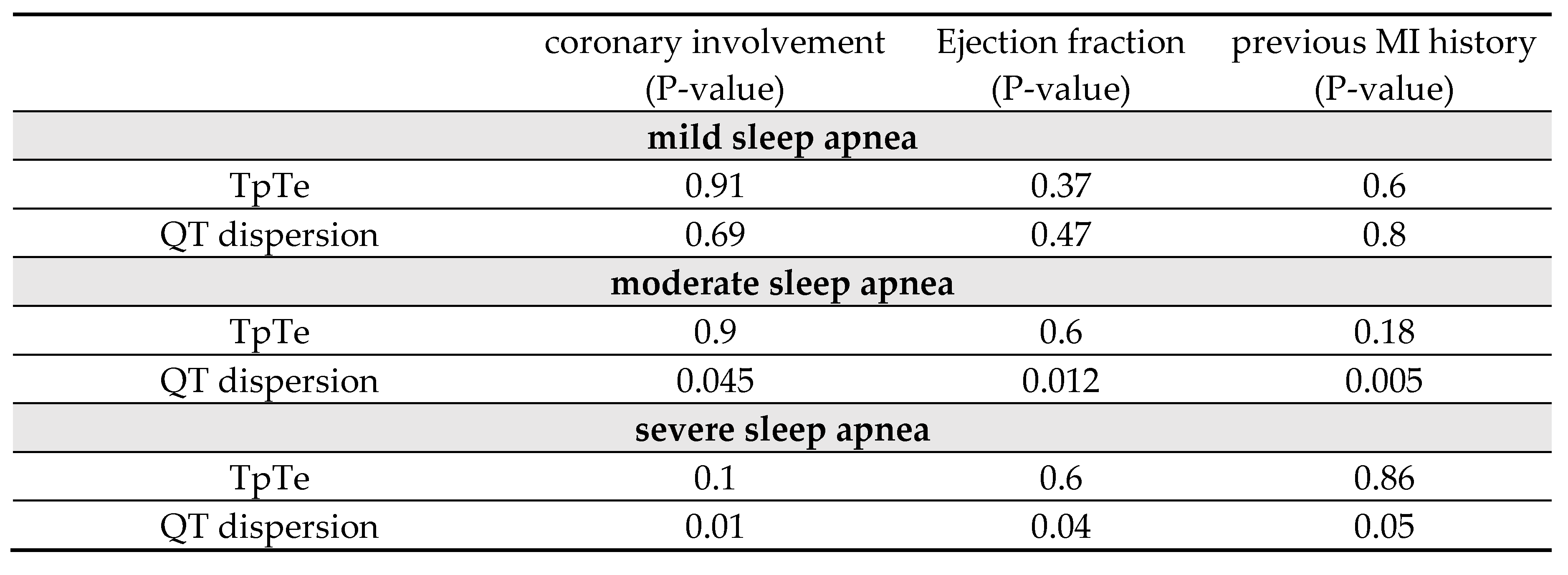
3.1. Comparison of QT dispersion and TpTe in OSA patients with CAD severity:
3.2. Comparing QT dispersion and TpTe in OSA patients with an ejection fraction of less than or over 40 %:
4. Discussion
5. Conclusion
Shortcoming and future directions
Contribution
Acknowledgments
Statement of Conflict of Interest
References
- Young T, Palta M, Dempsey J, Skatrud J, Weber S and Badr S. The occurrence of sleep disordered breathing among middle-aged adults.N Engl J Med. 1993;328:1230–1235. [CrossRef]
- Grimm W and Becker HF. Obesity, sleep apnea syndrome, and rhythmogenic risk. Herz. 2006 May;31(3):213-8.
- Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, Shamsuzzaman AS and Somers VK. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation 2003;107:2589–94.
- Gami AS, Olson EJ, Shen WK, Wright RS, Ballman KV, Hodge DO, Herges RM, Howard DE and Somers VK. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am CollCardiol 2013;62:610–16.
- Lattimore JDL, Celermajer DS and Wilcox I. Obstuctive sleep apnea and cardiovascular disease. J Am CollCardiol. 2003;41:1429–1437.
- Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, O’Connor GT, Boland LL, Schwartz JE and Samet JM. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J RespirCrit Care Med. 2001;163:19– 25.
- Caples SM, Wolk R, and Somers VK, “InGuence of cardiac function and failure on sleep- disordered breathing: evidence for a causative role,” Journal of Applied Physiology, vol. 99, no. 6, pp. 2433–2439, 2005.
- Kaneko Y, Floras JS, Usui K, Plante J, Tkacova R, Kubo T, Ando S and Bradley TD. “Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apneas,” New England Journal ofMedicine, vol. 348, no. 13, pp. 1233–1241, 2003. [CrossRef]
- Bazett HC. An analysis of the time-relations of electrocardiograms. Ann Noninvasive Electrocardiol 1997; 2: 177-94.
- Eslami V, Safi M, Taherkhani M, Adibi A and Movahed MR. Evaluation of QT, QT Dispersion, and T-Wave Peak to End Time Changes After Primary Percutaneous Coronary Intervention in patients presenting with acute ST-Elevation myocardial infarction. J INVASIVE CARDIOL 2013;25(5):232-234.
- Nakamura T, Chin K, Hosokawa R, Takahashi K, Sumi K, Ohi M and Mishima M. Corrected QT dispersionand cardiac sympathetic function in patients with obstructive sleep apnea-hypopnea syndrome. Chest. 2004;125:2107– 2114.
- Kilicaslan F, Tokatli A, Ozdag F, Uzun M, Uz O, Isilak Z, Yiginer O, Yalcin M, Guney MS and Cebeci BS. “Tp-e interval, Tpe/QT ratio, and Tp-e/QTc ratio are prolonged in patients with moderate and severe obstructive sleep apnea,” Pacing and Clinical Electrophysiology, vol. 35, no. 8, pp. 966–972, 2012. [CrossRef]
- Topilski I, Rogowski O, Rosso R, Justo D, Copperman Y, Glikson M, Belhassen B, Hochenberg M and Viskin S. The morphology of the QT interval predicts torsade de pointes during acquired bradyarrhythmias. J Am Coll Cardiol. 2007 Jan 23;49(3):320-8. [CrossRef]
- Alonso-Fernández A, García-Río F, Racionero MA, Pino JM, Ortuño F, Martínez I and Villamor J.Cardiac rhythm disturbances and ST segment depression episodes in patients with obstuctive sleep apnea-hypopnea syndrome and its mechanisms. Chest. 2005;127:15–22.
- Yamashita J, Nomura M, Uehara K, Nakaya Y, Uemura E, Iga A, Sawa Y, Nishikado A, Saito K and Ito S.. Influence of sleep apnea on autonomic nervous activity and QT dispersion in patients with essential hypertension and old myocardial infarction. J Electrocardiology. 2004;37:31–40. [CrossRef]
- Dursunoglu D, Dursunoglu N, Evrengül H, Ozkurt S, Kiliç M, Fisekci F, Kuru O and Delen O. QT interval dispersion in obstructive sleep apnea syndrome patients without hypertension. EurRespir J. 2005;25:677–681.
- Pontiroli AE, Pizzocri P, Saibene A, Girola A, Koprivec D and Fragasso G Left ventricular hypertrophy and QT interval is obesity and in hypertension: effects of weight loss and of normalization of blood pressure. Int J Obesity. 2004;28:118–123.
- Tasci S, Manka R, Scholtyssek S, Lentini S, Troatz C, Stoffel-Wagner B and Lüderitz B. “NT-pro-BNP inobstructive sleep apnea syndrome is decreased by nasal continuous positive airway pressure,” Clinical Research inCardiology, vol. 95, no. 1, pp. 23–30, 2006.
- Strehmel R, Valo M, and Teupe C. “Natriuretic peptide and high-sensitive troponin t concentrations correlate with effectiveness of short-term cpap in patients with obstructive sleep apnea and coronary artery disease,” Clinical MedicineInsights: Circulatory, Respiratory and Pulmonary Medicine, vol. 10, pp. 33–39, 2016. [CrossRef]
- Jarrah MI, Yassin AM, Ibdah RK, Ibnian AM, Eyadeh AA and Khassawneh BY. “Screening for obstructive sleep apnea amongpatients undergoing coronary catheterization in Jordan” Vascular Health and Risk Management 2019:15 109–113.
- Konishi T, Kashiwagi Y, Funayama N, Yamamoto T, Murakami H, Hotta D and Tanaka S. “Obstructive sleep apnea is associated with increased coronary plaque instability: an optical frequency domain imaging study” Heart and Vessels (2019) 34:1266–1279.
- Rivera-Pérez SJ, Martinez D, Araujo GN, Goncalves SC, Lazzaretti LK, Wainstein RV, Wainstein MV and Ribeiro JP. “Severity of obstructive sleep apnea and extension of coronary artery disease” Sleep and Breathing (2019) 23:747–752.
- Umut Somuncu M, Bulut U, Karakurt H, Utkusavas A, Akbay E and Kartal Kilinc F. “The Relationship Between Obstructive Sleep Apnea and Coronary Plaque: A Coronary Computed Tomographic Angiography Study” Acta Cardiol Sin 2019;35:325_334.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





