1. Introduction
Non-thyroidal-illness syndrome (NTIS) is a condition present in acute and chronic illnesses, in the absence of thyroid disease, and is considered an adaptive response rather than a real hypothyroidism [
1]. The most common picture is a low deiodination of free thyroxine (fT4), leading to reduced circulating levels of free triiodothyronine (fT3), which leads to the so-called “low-fT3 syndrome”, but with the prolongation of illness, is also involved low fT4 secretion [
2]. In acute conditions, this picture can be observed after starvation and critical illness, such as sepsis or major surgery, while low fT3 is commonly observed in chronic kidney and liver diseases, heart failure, and chronic inflammatory diseases[
3]. A key role seems to be exerted by increased cytokines levels [
4], but other mechanisms can be involved, such as alterations in plasma thyroid hormones transporter, clearance, and modifications of membrane transporters. It is also claimed the role of selenium since this element is involved in the mechanism of deiodination [
5]. Thyroid hormone replacement therapy is usually not requested, but this topic is still under debate[
6,
7]. Indeed, a tissue-specific response is described; some data suggest that, at cellular levels, a reduced fT3 bioavailability can be hazardous and express a “maladaptive” rather than “adaptive” response. Among these consequences, intracellular oxidative stress has been hypothesized [
8,
9].
Oxidative stress (OS) could exacerbate NTIS condition in a vicious cycle, due to deiodinase alteration and the negative effects of low T3 on antioxidant levels or activity [
10]. Chronic inflammation and OS exert reciprocal influences leading to a worse clinical course of such conditions [
11]. Accordingly, based on experimental and clinical studies, thyroid hormone (TH) levels in NTIS do not necessarily reflect their serum low concentrations and their intracellular levels; moreover, tissue-specific thyroid hormone transport, receptor binding, and hormone metabolism are reported [
12]. Interestingly, muscle is one of the main targets of thyroid hormones and it is not surprising that many alterations are seen in NTIS condition.
Different regulations of deiodinases 2 and 3 (DIO2 and DIO3) modulate T3 intracellular levels with a subtle tuning to compensate for the systemic TH unbalance [
13]. We have previously described as TH influence antioxidant systems, and their evaluation in chronic disease can represent an index of tissue effects of these hormones.
In our previous study, we reported that in chronic kidney disease (CKD), total antioxidant capacity (TAC) significantly correlated with the irisin levels [
14]. The irisin is a 112 amino acid protein of 12 kDa molecular weight, identified for its ability to induce the browning of white adipose tissue, protect from insulin resistance and increase energy expenditure [
15,
16].
Superoxide dismutases (SODs) are an important class of enzymes that protect against the formation of oxidants [
17]. A unique extracellular antioxidant enzyme with a key function in the vasculature in the prevention of oxidants-mediated tissue damage is extra-cellular superoxide dismutase (ec-SOD), also known as SOD3. The ec-SOD discovered in 1982 by Marklund [
18] is different from mitochondrial MnSOD (SOD2) or cytosolic CuZnSOD (SOD1) isoforms, although closer to the latter, it contains a heparin-binding domain that allows its binding to the glycosaminoglycans of extracellular matrix. In particular, in the arterial wall, it constitutes the primary endogenous defence against vascular superoxide anion, being critical for endothelial health in the protection of nitric oxide. The endothelium-bound ec-SOD can be assessed in patients by measuring an increase in plasma superoxide scavenging activity triggered by an injection of heparin in the patient leading to transient competition with heparan sulfate groups in the extracellular matrix and consequent increase in ec-SOD plasma levels.
Few data are reported on ec-SOD in hemodialysis subjects [
19,
20], but its relationships with thyroid hormones are not already investigated. An interesting model to evaluate ec-SOD is represented by hemodialytic patients since an acute release of ec-SOD in the blood is induced by the heparin administered before starting the dialysis procedure.
Therefore, this study was designed to evaluate, in an observational cohort study, as the primary endpoint the levels of ec-SOD in two models of NTIS: 1) chronic kidney disease during haemodialytic treatment, started from a short period (“acute hemodialytic patients”, AH) or 2) patients treated for a long period (“chronic hemodialytic patients”, CH). This observational study has as secondary endpoint to measure the ec-SOD activity in correlation with thyroid hormones, to establish the possible effects of NTIS in the modulation of antioxidant systems.
2. Materials and Methods
2.1. Patients enrollments
Patients with end stage renal disease (ERDS) on maintenance hemodialysis were considered eligible. Patients with ESRD on maintenance hemodialysis at the Italian Fondazione Teaching Hospital “Agostino Gemelli IRCCS” three times a week were screened. Exclusion criteria were as follows: advanced heart failure (according to the criteria of the European Society of Cardiology), diagnosis of dementia based on DSM-IV criteria, history of alcohol or substance abuse, previous diagnosis of psychotic disorders, and clinical instability requiring hospital admission. According to the administration of hemodialysis in the first period of treatment or for a longer time, two groups were identified:
- -
Group Acute Hemodialysis (AH): 1-3 months of treatment
- -
Group Chronic Hemodialysis (CH): 12-336 months of treatment
All enrolled patients were given an explanation of the purposes and nature of the study, and written informed consent was obtained. Our centre Institutional Board (School of Medicine, Catholic University) approved the study protocol.
All patients received 4-h bicarbonate hemodialysis three times a week, according to the schedule employed in the hemodialysis Unit (HU). The blood flow ranged from 250 to 300 mL/min, with a dialysiate rate flow of 500 mL/min. Patients of group AH performed hemodialysis via venous central catheter (CVC); patients of Group CH via CVC or arteriovenous fistulae. All Patients were treated with high-permeability membranes. Membranes were not reused. The inter-dialytic weight gain (IDWG) and pre-dialysis systolic blood pressure of 10 consecutive hemodialysis sessions (the same used to record IDH) were recorded and mean median values were calculated [
21]
2.2. Sample collection
Between 08.00 and 09.00 a.m. before starting hemodialysis treatment, at fasting a venous withdrawal was performed; the blood sample was collected, through the arteriovenous fistula (in CH) or the central venous catheter (both in AH and CH) immediately during the “short interval” (48 after the last dialysis “basal 2”) or “extended interval” (72 h after the last dialysis “basal 1”) to evaluate differences in the basal level of ec-SOD linked to the duration of intervals between dialytic procedures; in the day of a short interval, we also collected samples at 5 and 10 min after heparin administration preceding the starting of hemodialysis and at the end of the same. All samples were collected in a test tube containing heparin as an anticoagulant and immediately centrifuged (4°C at 2500× g for 10 min) were subsequently aliquoted in 2 ml and stored at -80°C until assayed.
2.3. Hormonal and metabolic parameters
We also collected an aliquot for the determination of the following metabolic and hormonal parameters: glucose, creatinine, uric acid, total and HDL cholesterol, albumin, transaminases, fT3, fT4, TSH.
Plasma concentrations of glucose, creatinine, uric acid, total cholesterol, HDL-cholesterol, albumin, and transaminases were measured by using enzymatic assays and an Olympus AU2700 chemistry analyzer (Olympus America Inc., Center Valley, PA). The intra-and inter-assay coefficients of variation (CV) for total cholesterol and uric acid were <1.5% and <2.5%, respectively. The intra- and inter-assay CV for HDL-cholesterol were <2.5% and <3.0%, respectively.
Serum concentrations of TSH, fT3, and fT4 were measured by using immunochemiluminometric assays on a Roche Modular E170 analyzer (Roche Diagnostics, Indianapolis, IN, USA). The intra-assay and inter-assay CV for all hormones were, respectively, <5.0 and <7.0%. The normal fT3 range in our laboratory measurements was 2.5-3.2 pg/ml. Thus, low fT3 levels were considered if under 2.5 pg/ml. Moreover, a “severe low fT3” was furtherly defined as an fT3 level under the median of the low fT3 population.
2.4. Oxidative parameters
Total antioxidant capacity (TAC) was evaluated using the method of Rice-Evans, modified in our laboratory as below described [
17,
22,
23]. This assay is based on inhibition, determined by antioxidants, of the absorbance of the radical cation 2,2′-azinobis (3-ethylbenzothiazoline-6 sulfonate) (ABTS
●+) formed by interaction between ABTS (150 μM) and ferrylmyoglobin radical species, generated by activation of metmyoglobin (2.5 μM) with H
2O
2 (75 μM). Aliquots of the frozen plasma were thawed at room temperature and 10 μl of the samples were tested immediately. The manual procedure was used with only minor modifications, as previously described [
22]. The reaction was started directly in the cuvette through H
2O
2 addition after 1 min equilibration of all other reagents and followed for 10 min, monitoring at 734 nm, typical of the spectroscopically detectable ABTS
●+. The presence of chain-breaking antioxidants induces a lag time (the “Lag phase”) in the accumulation of ABTS
●+ proportional to the concentration of the antioxidants and expressed as the length of such a Lag phase (sec). This assay mainly measures non-protein and non-enzymatic antioxidants that are primarily extracellular chain-breaking antioxidants, such as ascorbate, urate, and glutathione. Trolox, a water-soluble tocopherol analogue, was used as a reference standard. Absorbance was measured with a Hewlett-Packard 8450A UV/Vis spectrophotometer (Palo Alto, CA) equipped with a cuvette stirring apparatus and a constant temperature cell holder.
The ec-SOD activity was measured by a modified nitrite method [
24]. Briefly, superoxide generated by hypoxanthine and xanthine oxidase was changed by hydroxylamine to nitrite anion which was measured spectrophotometrically at 550 nm by the use of a chromogen. The amount of ec-SOD required to inhibit 50% nitrite anion generation was defined as 1 U of ec-SOD activity.
2.5. Statistical analysis
Descriptive analyses were performed using frequencies and percentages for categorical data and mean and standard deviation (SD) for continuous data. Skewness and kurtosis were used to investigate the distribution of the collected quantitative data and the Saphiro-Wilk test was used to investigate normal distribution. Inferential statistics were performed using the Student t-test or Wilcoxon rank-sum test (Mann-Whitney) or sign-rank test, for unpaired and paired data respectively, for quantitative data accordingly to the normalcy of the distribution, applying Fisher correction. to investigate differences between groups and within the groups for the ec-SOD activity values after heparin infusion (at 5 and 10 minutes and at the end of treatment) vs basal values (basal 2 short). In the CH group ec-SOD activities were compared with the levels of fT3. Paired or unpaired tests were deployed accordingly. Pearson bivariate correlations were performed to check multi-collinearity between fT3 levels and ec-SOD activities. Statistical significance was set at p<0.05. I performed statistical analysis with STATA 17.0 software (Stata Corporation, College Station, TX, USA).
3. Results
Fifty-six patients were screened and 46 were included in the study. Thirty (65.22%) were males and the mean age was 68.27 years (SD 14.42), with an overall hemodialysis time of 55.25 months (SD 68.9). According to the treatment duration, ten patients were allocated to the AH group and 36 to the CH group.
Metabolic parameters in AH and CH groups are described and compared in
Table 1.
Hormonal parameters and antioxidants activity in both groups are described and compared in
Table 2.
All data are in the normal range according to our clinical biochemistry parameters, except for creatinine as expected, with significantly higher values in chronic patients. Albumin and GPT values are higher in the AH group, with a statistically significant difference from the other group. Hormonal parameters reported in
Table 2 show significant variations among chronic and acute patients, with significantly higher levels of ec-SOD and LAG lower levels in the chronic group.
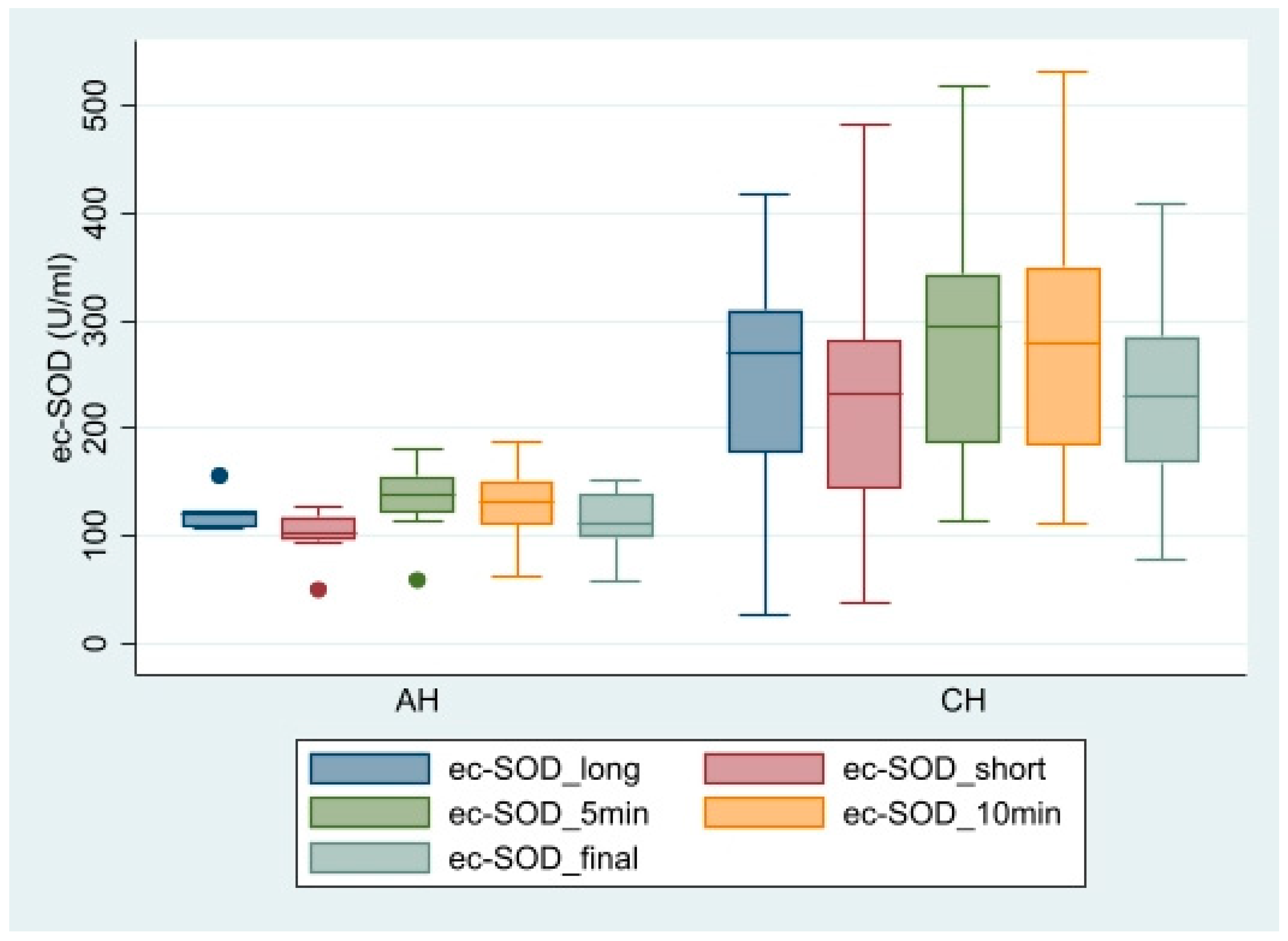
Figure 1 shows the pattern of ec-SOD release after heparin infusion in AH vs CH patients.
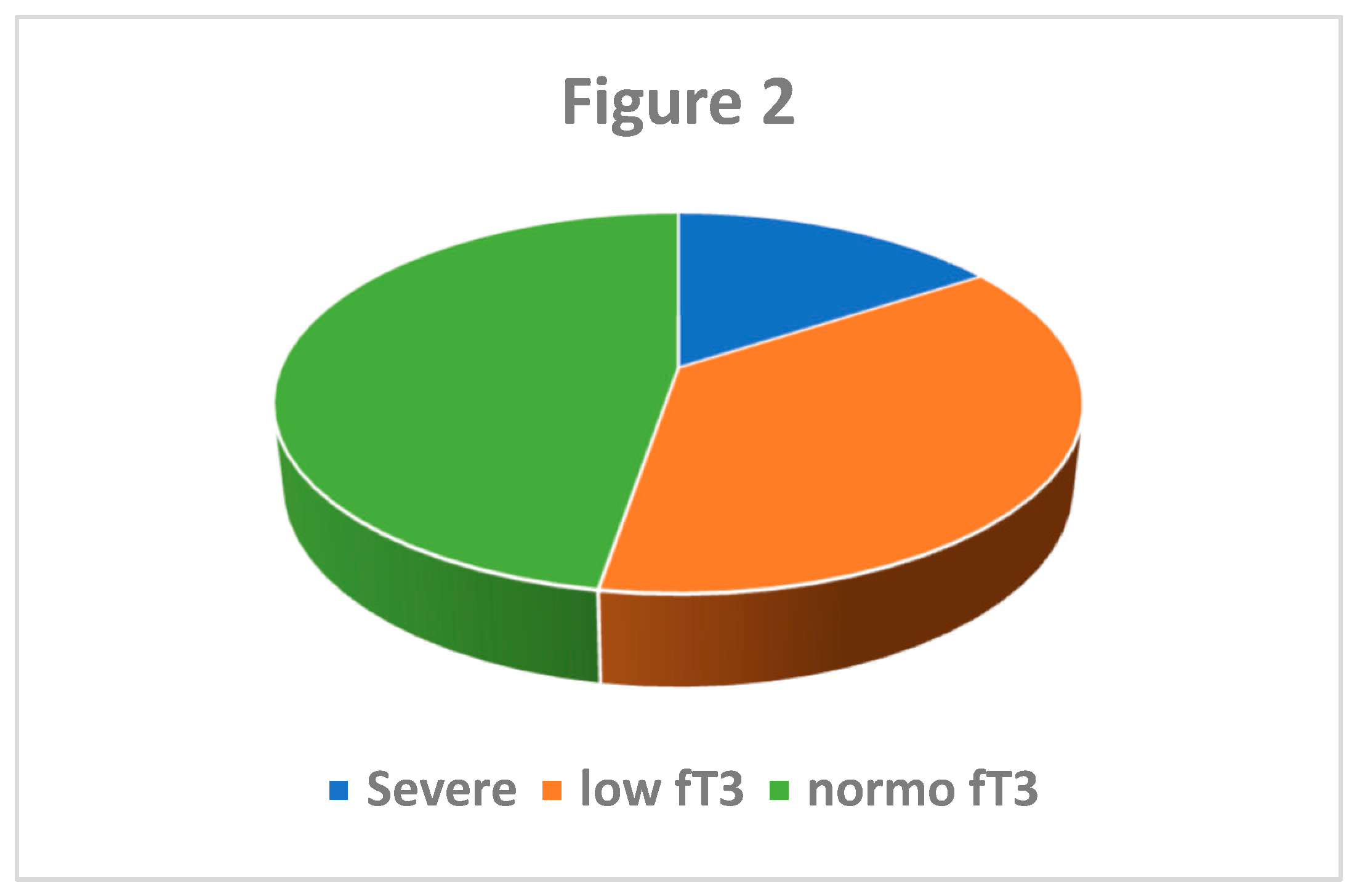
Interesting data were observed when classified CH patients according to fT3 levels. Nineteen patients (52.78%) had low level of fT3, and a quarter of those (26.32%) had severe NTIS (<1.8 pg/ml, median of low-T3 values).
Figure 2 shows the distribution of fT3 categories (severe NTIS: <= 1.8 pg/ml, 1.8 pg/ml < low fT3 <2.4 pg/ml; normal fT3 >= 2.4 pg/ml).
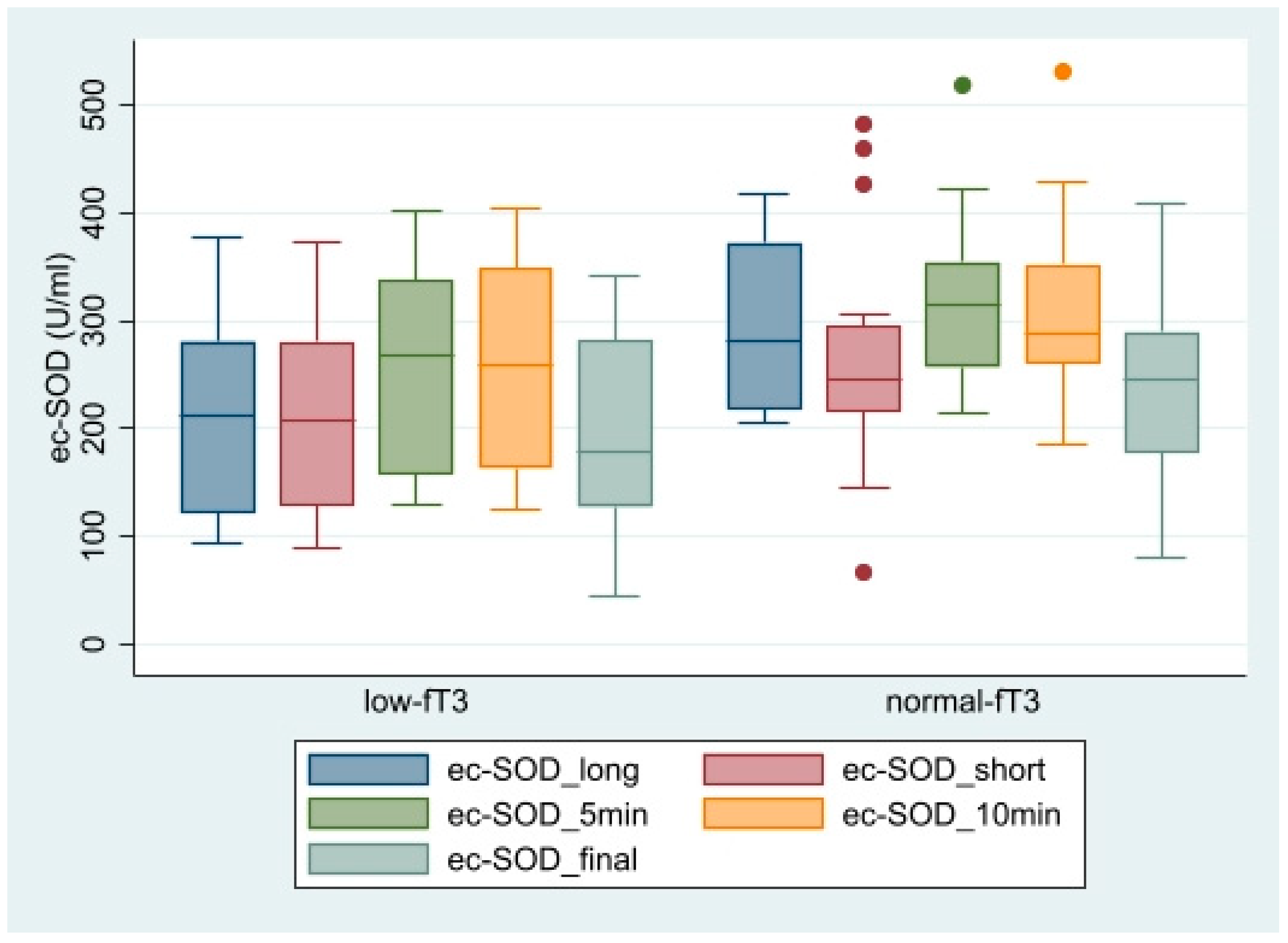
Figure 2 shows the ec-SOD levels after heparin infusion in CH patients divided according to the presence of low T3 condition.
Basal ec-SOD differed between low- and normal-T3 groups only for the basal 1 (long), but the increase after heparin was significantly correlated with T3 levels. In
Table 3 the different patterns of ec-SOD release after heparin are described and compared in the two subgroups.
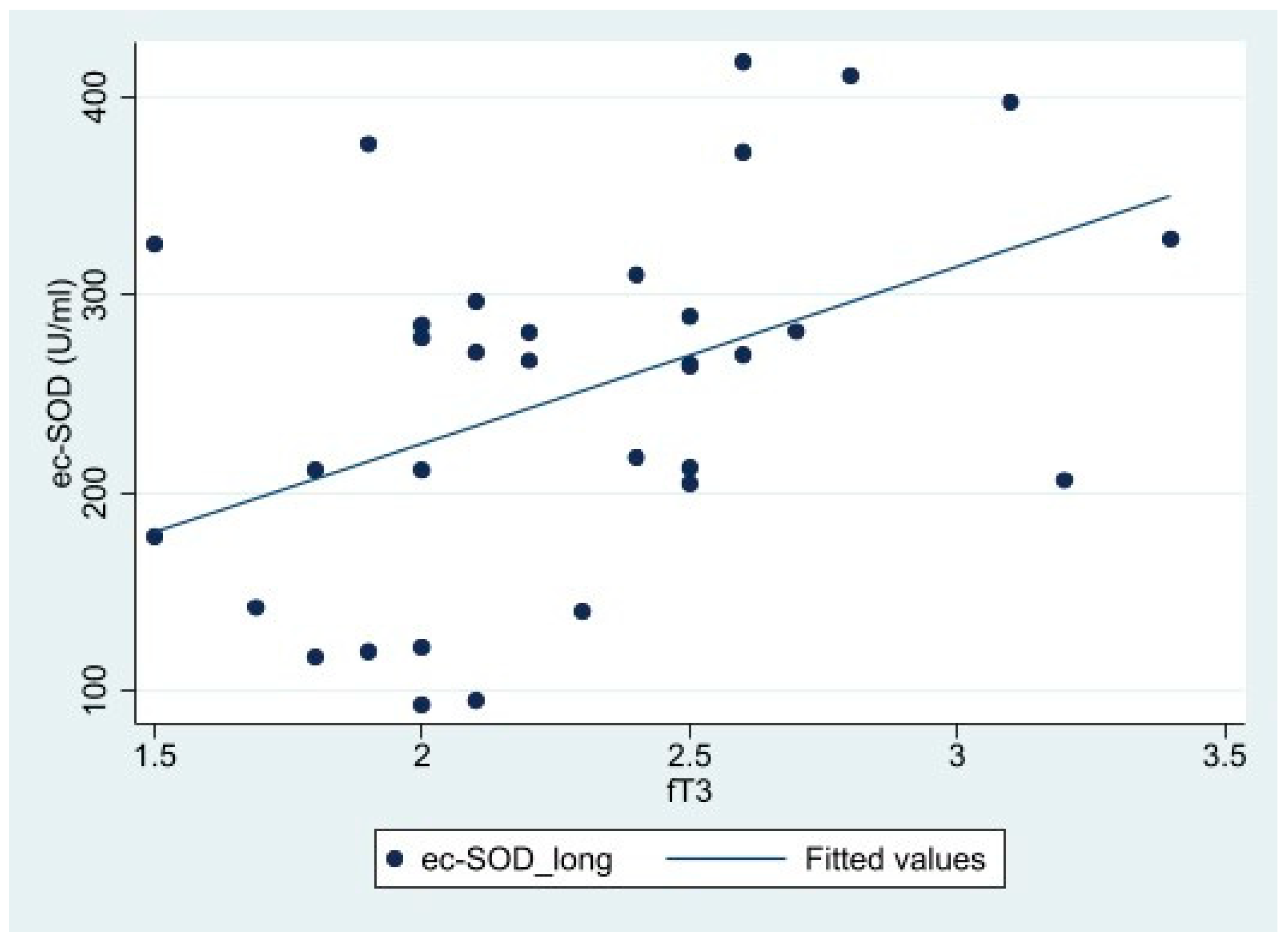
Considering the total fT3 distribution, the Pearson correlation analysis reported a significant correlation with ec-SOD basal 1 (long) (r=0.443, p=0.01) (
Table 4). The scatterplot of the significant correlation, along with the fitted model, is represented in
Figure 3.
In the AH group, comparing changes in ec-SOD levels over time until the end of treatment, there is an average increase of 26.36% (SD 10.3%) at 5 minutes, 21.85% (SD 10.09%) at 10 minutes and 8.80% (SD 21.45%) at the end. In the CH group, the increases from baseline are 28.01% (SD 34.77%) at 5 minutes, 26.50% (SD 34.63%) at 10 minutes and 4.24% (SD 31.24%) at the end.
Table 5 shows the crude increase and statistical difference by group from baseline values (baseline 2 short). We also performed the same analysis on the low-/ normal- fT3 level subgroups of the CH group.
The intragroup comparison highlighted significant increase in the ec-SOD activities at five (p=0.004) and ten minutes (p=0.004) from injection, for the AH group. Similar results were obtained for the CH group (p<0.001 at both five and ten minutes versus basal ec-SOD activities).
Considering fT3 levels in the CH group, the increase was statistically significant at five and ten minutes after injection. In the low fT3 subgroup, the p values are both <0.001. In the normal fT3 subgroup, the p-values are 0.002 and 0.001 for the two times, respectively.
Comparison of ec-SOD levels at the end of hemodialysis versus baseline was not significant in each group or subgroup analyzed.
Finally, we observed significantly higher ec-SOD values in the sub-groups with normal fT3 levels in comparison with the sub-groups with low FT3 levels (Fig. 4).
4. Discussion
NTIS is a condition considered adaptive to many acute and chronic diseases and related to their prognosis. The mechanisms are complex, including primarily deiodinases deregulation, but other factors can be operative and tissue specific [
12]. In mice, TH expression is decreased in sepsis and acute inflammation but does not seem to be affected in chronic inflammation. The same scenario is observed in humans since the expression of monocarboxylate transported 8 (MCT8) is lower after acute surgical stress than in prolonged illness, however, a compensatory increase in MCT8 has been described in chronic diseases in rabbits [
25]. We have previously described the relationship between inflammation and OS including thyroid involvement in cardio-pulmonary diseases [
26,
27].
Several study reports the occurrence of OS in chronic hemodialysis. In fact, lower enzymatic antioxidants (e.g. GPX, SOD) and higher MDA levels in comparison with controls have been described [
28]. Interestingly, a correlation with selenium deficiencies has been evidenced, and a supplementation of this element increase SOD and CAT activities [
29]. Moreover, an association between hypo-albuminemia biomarkers of inflammation and of oxidative stress has been reported [
30].
As ec-SOD is concerned it has been shown that hemodialytic patients are more prone to endothelial cell damage and elevated ec-SOD values [
31]. Shimomura et al. reported that an increase of ec-SOD in diabetic-nephrotic subjects especially in the sub-group with macro-albuminuria [
32]. The same researcher evaluated ec-SOD levels with an ELISA method in hemodialytic patients describing a correlation between the enzyme and FFA and LPL underling the role of insulin resistance. The same study reported little changes between pre and post dialysis procedure the last datum was in contrast with other paper showing a significant increase in post dialytic values [
33].
Our preliminary data suggest that low fT3 levels can negatively influence endothelial antioxidant defenses. The relationships of this datum with cardiovascular complications and prognostic usefulness remain to be established.
The ec-SOD, discovered by Marklund and co-workers in 1982 [
18,
34], is a different enzyme from the two forms of intracellular superoxide dismutases, namely CuZn-SOD and Mn-SOD. The ec-SOD isoform is predominant isozyme in extracellular fluids, in particular in plasma. It is a tetramer containing one copper and one zinc atom per subunit, which are required for enzymatic activity; the location of the ec-SOD gene in humans is chromosome 4q21 and shows a 60% homology with CuZn-SOD but minimal homology with Mn-SOD [
35]. The human mRNA for the enzyme is highly expressed in the heart, placenta, pancreas, and lung, and lower levels in the kidney, skeletal muscle, and liver.
The primary location of ec-SOD in tissues is in the extra-cellular matrix and on cell surfaces, where its concentration is 20 times higher than in plasma. The association of ec-SOD with the tissue is accomplished by a heparin-binding domain, which recognizes heparansulfate proteoglycans on the cell surface and in the matrix. Intravenous injections of heparin in humans and other species lead to an immediate increase in plasma ec-SOD content [
31], allowing the determination of endothelium-bound ec-SOD in humans in vivo [
36]. The highest tissue concentrations are found in blood vessels, lungs, kidneys, and uterus [
37].
The physiopathological role of ec-SOD has been examined in vascular-related diseases, atherosclerosis, hypertension, diabetes, ischaemia-reperfusion injury, lung disease, various inflammatory conditions, and neurological diseases [
35]. The administration of the lipid antioxidant Coenzyme Q10 can induce an improvement of endothelium-bound ec-SOD, presumably by counteracting nitric oxide oxidation [
38].
Few papers explored the role of ec-SOD in kidney disease. In a model of ADR nephropathy characterized by proteinuria and kidney failure, it has been shown that ec-SOD decreased during the illness, together with an increase in NADPH oxidase and oxidative stress index [
39]; interestingly, ec-SOD null mice, with non-proteinuric kidney injury induced by unilateral ureteral obstruction did not differ from wild-type, the same animals, when sensitized to ADR injury, exhibited augmented NADPH and β-catenin levels. Therefore, it was hypothesized a protective role of ec-SOD against proteinuria and the progression of the disease. In the same study, also human biopsies of chronic kidney disease showed a similar reduction in ec-SOD.
A protective role in humans has also been suggested in patients in hemodialytic treatment by Yamada & coll. [
40], who found that a single-base substitution of the ec-SOD gene, causing a decrease of the binding capability to endothelial cells and therefore an increased serum concentration. The percentage of patients harboring this mutation rapidly decreased in the group of patients with diabetes mellitus; a prognostic use was suggested based on patients who died from ischemic heart disease or cerebrovascular accidents.
To the best of our knowledge, we have provided, for the first time evidence that reports the ec-SOD activity in hemodialytic patients concerning thyroid hormones; it suggests that low fT3 concentration can influence ec-SOD levels; according to other chronic conditions, the data seem to point toward real hypothyroidism at the tissue level. Therefore, future research is needed to understand the present observation that could be the basis for a longitudinal study, to evaluate the impact of low fT3 on cardiovascular risk, and for a treatment study. Thus, we can speculate that if fT3 exerts a protective role, it could also be useful in chronic kidney insufficiency in delaying dialytic treatment.
Author Contributions
Conceptualization, A.M. and L.T.; methodology, A.S., E.C., N.P.; software, F.B. and N.N..; validation, N.N., and S.S.; formal analysis, F.B. S.S., P.O. and A.S.; investigation, A.S., F.B. ; resources, L.T.; data curation, A.M., N.N. F.B.; writing—original draft preparation, A.M. and A.S. ; writing—review and editing, A.S. and L.T.; visualization, E.L., P.O; supervision, N.P.; project administration, A.M.; funding acquisition, A.S. All authors have read and agreed to the published version of the manuscript
Funding
The publication of this article was supported by Università Cattolica del Sacro Cuore “Linea D1 2022” fund n. R4124501287 to A.S..
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Catholic University (protocol code 15291/18 approval on 06/20/2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
All the authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Chopra, J. Euthyroid sick syndrome: is it a misnomer? J. Clin. Endocrinol. Metab. 1997, 82, 329–334. [Google Scholar] [CrossRef]
- De Groot, L. Non-thyroidal illness syndrome is a manifestation of hypothalamic-pituitary dysfunction, and in view of current evidence, should be treated with appropriate replacement therapies. Crit. Care Clin. 2006, 22, 57–86. [Google Scholar] [CrossRef] [PubMed]
- McIver, B.; Gorman, C.A. Euthyroid sick syndrome: an overview. Thyroid 1997, 7, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Bartalena, L.; Brogioni, S.; Grasso, L.; Velluzzi, F.; Martino, E. Relationship of the inctìreased serum interleukin-6 concentration to changes of thyroid function in nonthyroidal illness. J. Endocrinol. Invest. 1994, 17, 269–274. [Google Scholar] [CrossRef]
- Silvestrini, A.; Mordente, A.; Martino, G.; Bruno, C.; Meucci, E.; Vergani, E.; Mancini, A. The Role of Selenium in Oxidative Stress and in Nonthyroidal Illness Syndrome (NTIS): An Overview. Curr. Med. Chem. 2020, 27, 423–449. [Google Scholar] [CrossRef] [PubMed]
- Chopra, I.J.; Huang, T.S.; Boado, R.; Solomon, D.H.; Teco, G.N.C. Evidence against benefit from replacement doses of thyroid hormones in non-thyroidal illness (NTI): studies using turpentine oil-injected rat. J. Endocrinol. Invest. 1987, 10, 559–564. [Google Scholar] [CrossRef]
- Wartofsky, L.; Burman, K.D. Alterations in thyroid function in patients with systemic illness: the “euthyroid sick syndrome”. Endocr. Rev. 1982, 3, 164–217. [Google Scholar] [CrossRef]
- Mancini, A.; Corbo, G.M.; Gaballo, A.; Raimondo, S.; Di Segni, C.; Gigliotti, P.; Silvestrini, A.; Valente, S.; Pontecorvi, A.; Meucci, E. Relationship between plasma antioxidants and thyroid hormones in chronic obstructive pulmonary disease. Exp. Clin. Endocrinol. Diabetes 2012, 120, 623–628. [Google Scholar] [CrossRef]
- Mancini, A.; Raimondo, S.; Di Segni, C.; Persano, M.; Pontecorvi, A. Non-Thyroidal illness: physiopathology and clinical implications. In “Current topics in hypothyroidism with focus on development”; E. Potlukova (ed), Intech, Rijeka; 2013; pp. 183–202. [Google Scholar]
- St Germain, D.L.; Galton, V.A.; Hernandez, A. Defining the roles of the iodothyronine deiodinases: current concepts and challenges. Endocrinology 2009, 150, 1097–1107. [Google Scholar] [CrossRef]
- Mancini, A.; Di Segni, C.; Raimondo, S.; Olivieri, G.; Silvestrini, A.; Meucci, E.; Currò, D. Mediators Inflamm. 2016, 6757154. [Google Scholar] [CrossRef]
- Fliers, E.; Boelen, A. An update on non-thyroidal illness syndrome. J. Endocrinol. Invest. 2021, 44, 1597–1607. [Google Scholar] [CrossRef]
- Arrojo, R.; Drigo, E.; Bianco, A.C. Type 2 deiodinase at the crossroads of thyroid hormone action. Int. J. Biochem. Cell Biol. 2011, 43, 1432–1441. [Google Scholar] [CrossRef]
- Mancini, A.; Capobianco, E.; Bruno, C.; Vergani, E.; Nicolazzi, M.; Favuzzi, A.M.R.; Panocchia, N.; Meucci, E.; Mordente, A.; Silvestrini, A. Non-thyroidal illness syndrome in chronic diseases: role of irisin as modulator of antioxidants. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 1582–1591. [Google Scholar] [CrossRef]
- Aronis, K.N.; Moreno, M.; Polyzos, S.A.; Moreno-Navarrete, J.M.; Ricart, W.; Delgado, E.; de la Hera, J.; Sahin-Efe, A.; Chamberland, J.P.; Berman, R.; Spiro, A. 3rd; Vokonas, P.; Fernandez-Real, J.M.; Mantzoros, C.S. Circulating irisin levels and coronary heart disease: association with future acute coronary syndrome and major adverse cardiovascular events. Int. J. Obes. 2015, 39, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.Y.; Panaglotu, G.; Mouglos, V.; Brinkoetter, M.; Vamvini, M.T.; Scneider, B.E.; Mantzoros, C.S. FNDC5 and irisin in humans: I. Predictors of circulating concentrations in serum and plasma and II. mRNA expression and circulating concentrations in response to weight loss and exercise. Metabolism 2012, 61, 1725–1738. [Google Scholar] [CrossRef]
- Silvestrini, A.; Meucci, E.; Ricerca, B.M.; Mancini, A. Total Antioxidant Capacity: biochemical aspects and clinical significance. Int. J. Mol. Sci. 2023, 24, 10978. [Google Scholar] [CrossRef]
- Marklund, S.L.; Hellner, L. Superoxide dismutase in extracellular fluids. Clin. Chim. Acta 1982, 126, 41–51. [Google Scholar] [CrossRef]
- Shimomura, H.; Maekata, E.; Takamiya, T.; Adachi, T.; Komoda, T. Blood extracellular superoxide dismutase levels in hemodialysis patients pre- and post-hemodialysis and its association with lipoprotein lipase mass and free fatty acid. Clin. Chim. Acta 2003, 328, 113–119. [Google Scholar] [CrossRef]
- Nakamura, M.; Ando, Y.; Sasada, K.; Haraoka, K.; Ueda, M.; Okabe, M.; Motomiya, Y. Role of extracellular Superoxide Dismutase in patients under maintenance hemodialysis. Nephron Clin. Pract. 2005, 101, c109–c115. [Google Scholar] [CrossRef]
- Bossola, M.; Laudisio, A.; Antocicco, M.; Panocchia, N.; Tazza, L.; Colloca, G.; Tosato, M. : Zuccalà, G. Intradialytic hypotension is associated with dialytic age in patients on chronic hemodialysis. Ren. Fail. 2013, 35, 1260–1263. [Google Scholar] [CrossRef]
- Rice-Evans, C.; Miller, N.J. Total antioxidant status in plasma and body fluids. Methods Enzymol. 1994, 234, 279–293. [Google Scholar]
- Mancini, A.; Leone, E.; Festa, R.; Grande, G.; Di Donna, V.; De Marinis, L.; Pontecorvi, A.; Tacchino, R.M.; Littarru, G.P.; Silvestrini, A.; Meucci, E. Evaluation of antioxidant systems (coenzyme Q10 and total antioxidant capacity) in morbid obesity before and after biliopancreatic diversion. Metab. Clin. Exp. 2008, 57, 1384–1389. [Google Scholar] [CrossRef]
- Belardinelli, R.; Tiano, L.; Littarru, G.P. Oxidative stress, endothelial function and coenzyme Q10. Biofactors 2008, 32, 129–133. [Google Scholar] [CrossRef]
- Mebis. L.; Paletta, D.; Debaveye, Y.; Ellger, B.; Langouche, L.; D’Hoore, A.; Darras, V.M.; Visser, T.J., Van den Berghe, G. Expression of thyroid hormone transporters during critical illness. Eur. J. Endocrinol. 2009, 161, 243–250. [Google Scholar] [CrossRef]
- Mancini, A.; Raimondo, S.; Di Segni, C.; Persano, M.; Gadotti, G.; Silvestrini, A.; Festa, R.; Tiano, L.; Pontecorvi, A.; Meucci, E. Thyroid hormones and antioxidant systems: focus on oxidative stress in cardiovascular and pulmonary diseases. Int. J. Mol. Sci. 2013, 14, 23893–909. [Google Scholar] [CrossRef]
- Mancini, A.; Vergani, E.; Bruno, C.; Olivieri, G.; Di Segni, C.; Silvestrini, A.; Venuti, A.; Favuzzi, A.; Meucci, E. Oxidative stress as a possible mechanism underlying multi-hormonal deficiency in chronic heart failure. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3936–3961. [Google Scholar] [CrossRef]
- Montazerifa, F.; Hashemi, M.; Karajibani, M.; Sanadgol, H.; Dikshit, M. Evalutation of lipid peroxidation and erythrocyte glutathione peroxidase and superoxide dismutase in hemodialysis patients. Saudi J. Kidney. Dis. Transpl. 2012, 23, 274–279. [Google Scholar]
- Koening, J.S.; Fischer, M.; Bulant, E.; Tiran, B.; Elmadfa, I.; Druml, W. Antioxidant status in patients on chronic hemodialysis therapy: impact of parenteral selenium supplementation. Wien Klin. Wochenschr. 1997, 109, 13–19. [Google Scholar]
- Danielsky, M.; Alp kizler, T.; McMonagle, E.; Conner Kane, J.; Pupim, L.; Morrow, J.; Himmelfarb, J. Linkage of hypoalbuminemia, inflammation, and oxidative stress in patients receiving maintenance hemodialysis therapy. Am. J. Kidney Dis. 2003, 42, 286–294. [Google Scholar] [CrossRef]
- Adachi, T.; Ohta, H.; Futemna, A.; Kato, K.; Hirano, K. Quantitative analysis of extracellular-superoxide dismutase in serum and urine by ELISA with monoclonal antibody. Clin. Chim. Acta 1992, 212, 89–102. [Google Scholar] [CrossRef]
- Maehata, E.; Adachi, T.; Inoue, M.; Yano, M.; Shiba, T. High blood superoxide dismutase (SOD) states in patients with diabetes mellitus-dependence on extracellular (EC)-SOD. J. Jpn. Diabetes Soc. 2001, 44, 935–991. [Google Scholar]
- Futemna, A.; Kitano, M.; Hara, T.; Miyai, H.; Yamada, H.; Kato, K. Extracellular superoxide dismutase level in chronic hemodialysis patients. J. Jpn. Soc. Dial. Ther. 1993, 26, 519–23. [Google Scholar] [CrossRef]
- Marklund, S.L.; Bjelle, A.; Almqvist, L.G. Superoxide dismutase isoenzymes of the sinovial fluid in rheumatoid arthritis and in reactive arthritides. Ann. Rheum. Dis. 1986, 45, 847–851. [Google Scholar] [CrossRef]
- Fattman, C.L.; Schaefer, L.M.; Oury, T.D. Extracellular superoxide dismutase in biology and medicine. Free Rad. Biol. Med. 2003, 35, 236–256. [Google Scholar] [CrossRef]
- Landmesser, U.; Merten, R.; Spiekermann, S.; Buttner, K.; Drexler, H.; Hornig, B. Vascular extracellular superoxide dismutase activity in patients with coronary artery disease: relation to endothelium-dependent vasodilation. Circulation 2000, 101, 2264–2270. [Google Scholar] [CrossRef]
- Marklund, S.L. Exracellular superoxide dismutase and other superoxide dismutases in tissues from nine mammalian species. Biochem. J. 1984, 222, 649–655. [Google Scholar] [CrossRef]
- Tiano, L.; Belardinelli, R.; Carnevali, P.; Principi, F.; Seddaiu, G.; Littarru, G.P. Effect of coenzyme Q10 administration on endothelial function and extracellular superoxide dismutase in patients with ischaemic heart disease: a double-blind, randomized controlled study. Eur. Heart J. 2007, 28, 2249–2255. [Google Scholar] [CrossRef]
- Tan, R.J.; Zhou, D.; Xiao, L.; Zhou, L.; Li, Y.; Bastacky, S.I.; Oury, T.D. , Liu, Y.Extracellular Superoxide Dismutase Protects against Proteinuric Kidney Disease. Am. Soc. Nephrol. 2015, 26, 2447–2459. [Google Scholar] [CrossRef]
- Yamada, H.; Yamada, Y.; Adachi, T.; Fukatsu, A.; Sakuma, M.; Futemna, A.; Kakumu, S. Protective role of extracellular superoxide dismutase in hemodialysis patients. Nephron 2000, 84, 218–223. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).