1. Introduction
Tuberculosis (TB) continues to pose a significant global health challenge, despite being a preventable and treatable disease [
1]. It remains the leading cause of death from an infectious disease, claiming the lives of over one million people annually. The World Health Organization (WHO) reported an estimated 10 million cases of TB and 1.6 million TB-related deaths worldwide in 2021 [
1]. While the magnitude of the disease varies across countries, low and middle-income countries account for the highest burdens of the disease. Remarkably, around 87% of TB cases occur within the 30 high TB burden countries [
2]. The African continent accounts for a quarter (25%) of the global TB cases and has the highest incidence of TB and HIV co-infection [
1].
Ethiopia is one of the 30 designated high TB burden countries in the world, with an estimated 170,000 cases and 25,000 deaths due to TB in 2022 [
1]. To combat the disease, the country has been implementing the Directly Observed Treatment Short-course (DOTS) strategy since 1994 and achieved 100% national coverage in 2006 [
3]. Additionally, Ethiopia has adopted global end-TB targets aimed at reducing the TB burden. However, TB continues to be a major challenge in the country [
1,
4].
To accelerate progress and tailor effective interventions, it is crucial to have accurate and up-to-date information regarding areas with the highest TB burden. Previous studies conducted in Ethiopia have reported spatial or spatiotemporal clustering of TB at the sub-national level and identified ecological factors associated with TB clustering [
5,
6,
7,
8,
9,
10]. However, these studies were limited to pre-COVID-19 pandemic data and did not assess the impact of health service coverage, including TB diagnosis services, and climatic factors on TB clustering. Furthermore, there is a lack of recent information regarding the spatial distribution and temporal patterns of TB case notifications in the Oromia region of Ethiopia.
Therefore, the objective of this study is to assess the spatiotemporal patterns of notified TB cases at the district level in the Oromia region, employing a Bayesian statistical framework. Additionally, this study aims to investigate the influence of environmental, socio-demographic, and health service coverage factors on the distribution of TB in the region. By showing the spatial and temporal distribution and underlying factors associated with TB distribution, this study can inform targeted interventions and guide preventive and treatment measures in the Oromia region of Ethiopia.
2. Materials and Methods
Study setting
The study was conducted in the Oromia region of Ethiopia, one of the largest regions in the country by area with a total area of 0.2 million square kilometers. According to the most recent estimates, the population of the Oromia region was 40 million people in 2022 [
11]. Climate conditions in the Oromia region are very diverse from highland (cold), midland (temperate), and lowland (hot) areas. The climate in the region experiences four distinct seasons with hot and dry summers and mild and rainy winters. Average annual rainfall varies across the region. The districts are the lowest administrative divisions with legal autonomy.
Data sources
We used different data sources for the primary outcome and exposure variables. Our primary outcome measure was the number of reported pulmonary TB cases at the district level for the period between 2018 and 2022. The TB data along with HIV data were obtained from the Health Management Information System (HMIS) [
12,
13] and a web-based District Health Information System (DHIS). In HMIS and DHIS, TB cases are registered daily as the patients diagnosed and start treatment but are reported quarterly in each of the health facilities that provide TB diagnosis and treatment. The data set comprises sociodemographic information on age and sex along with clinical data about the classification of TB cases [
14]. Data for climatic variables such as temperature, precipitation, humidity, and wind speed were obtained from the power database [
15].
Population data for the five-year study period (the number of people in each district), health service coverage, and laboratory diagnostic coverage were obtained from the Oromia region health bureau (Oromia health bureau 2021/22 annual report). A polygon ESRI shapefile for the Oromia region at the district level was obtained from the Oromia Regional Land Bureau. The dependent variables (TB cases) were geo-referenced, and covariates were linked to the dependent variable using ArcGIS (ESRI, Redlands, CA) geographical information system (GIS) software.
Measurement
The spatial-specific population density was calculated by dividing the total number of people in each district by the land area of the district in square kilometers.
Health service coverage: dividing the number of health centers (a primary healthcare unit) by the catchment population in a specific year. The Ethiopian Ministry of Health suggests that one health center should cater to a population of 25,000 [
16].
Laboratory diagnostic coverage is the proportion of health facilities providing TB diagnosis to the total number of health facilities in the district.
Data analysis
TB case notification: As a descriptive analysis, the TB TB case notification for the Oromia region was calculated by sex and year. TB case notifications were calculated by dividing the total number of new TB cases, by the population of the same year and sex in the corresponding district, multiplied by 100,000 to obtain a rate per 100,000 population.
Standardized incidence ratio: Standardized incidence ratios (SIR) were calculated for each district by year. For each district
,
=1…n, the SIR was calculated as the ratio of the observed number of TB cases in the district (
) to the expected number of TB cases (
) in the district across the study period,
t = 2018,…., 2022:
he expected count
represented the total number of TB cases that one would expect if the population of district
had the same risk as the regional population during the same year. The expected number of TB cases for each district (
) was computed as:
Where is the overall crude TB TB case notification for the Oromia region (i.e., the total number of TB cases in a specific year divided by the total population of the region during the same year), and is the population of each district during a year.
Spatial autocorrelation analysis: The global Moran’s I and the Getis-Ord statistic were used to identify clusters of high TB incidence at the district level across all regions of Oromia. The global Moran’s I statistic was used to assess the presence, strength, and direction of spatial autocorrelation over the Oromia region and to test the assumption of spatial independence in implementing the spatial pattern analysis. The Getis-Ord statistic was used to detect the local clustering of TB infection. Maps produced from Moran’s I statistics and the Getis-Ord statistics show the existence of TB clusters and identify the locations of potential hotspot areas.
Bayesian spatiotemporal analysis: The spatiotemporal model was constructed using covariates. The observed numbers of TB cases
in the district
for the five-year observation period were modeled using a Poisson distribution with mean
, where
is the expected number of TB cases and
is the relative risk in the district
for a given year. The logarithm of the relative risk
was expressed as the sum of an intercept, a vector of covariates and their coefficients, and random effects to account for extra-Poisson variability. The model for the spatiotemporal data is expressed as follows:
Here,
represents the coefficient vector of the covariates,
is the vector of
covariates corresponding to the district
during a year, T corresponds to the year,
is a measure of the significance of the regional trend in TB notification rate,
is a measure of space-time interaction,
represents the population size of districts during a year,
is a random effect specific to the district
to model spatiotemporal dependence between the relative risks, and
is an unstructured exchangeable component that models uncorrelated noise. The unstructured component
was modeled as independent and identically distributed normal variables with zero mean and variance
[
17,
18].
Before fitting the model, all covariates were checked for multi-collinearity using variance inflation factors (VIF) (
Table S1). Those variables with a VIF greater than 6 were excluded from the final model. Variables with a p-value less than 0.2 in the bivariate regression model were selected for the final model. Health service coverage, population density, temperature, precipitation, and wind speed were eligible covariates to be included in the final model. Since these independent variables had different units and scales of measurement that would have unknown threshold effects, the variables were normalized using their mean and standard deviation ([X-mean]/SD). This method also helped with identifiability in the estimation of the posterior distribution of the coefficients. All the analyses were conducted using R and ArcGIS Pro software.
Ethical considerations
The Ethics Review Committees of the Public Health Emergency Directorate at Oromia Regional Health Bureaus reviewed and approved the study protocol. As the data obtained from the DHIS were aggregated at a district level without any personal information, informed consent was not required.
3. Results
Table 1 shows the summary statistics of notified TB in the Oromia region reported from 337 districts to the regional TB surveillance system through the HMIS for the period January 2018 to December 2022. A total of 206,278 pulmonary TB cases were reported during the study period. Of these TB cases, 114,458 (55.5%) were males. During the study period, a total of 65,372 people tested positive for HIV, crude HIV positivity rate of five years was found to be 0.38 %. The positivity rate of HIV among tested people decreased from 0.61% in 2018 to 0.34% in 2022.
TB TB case notification
The overall TB case notification of notified TB across the study years in the Oromia region was 117.8 (95% CI 107.3 - 128.4) per 100,000 population. The annual TB case notification of notified TB was higher in males (ranging from 16.5 to 1201.9 per 100,000) than in females (ranging from 14.9 to 746.6 per 100,000 for females). The TB case notification of TB also varied by year, with the lowest TB case notification (96.93 per 100,000 population) reported in 2020 (i.e., during the COVID-19 pandemic) and the highest TB case notification (106.19 per 100,000 population) reported in 2019 (
Table 1).
TB cases displayed seasonal variations with the highest number of cases reported between January to March (n=53,689; 26%) and the lowest number of TB reported from July to September (n=49,206; 23%). The notified TB case by year and season as a region is presented in the appendix (
Table S3). The TB case notification of notified TB varied substantially at the zonal level, ranging from 304.71 in the Horo Guduru zone to 2,069.70 in Dukem town per 100,000 population. The TB case notification of notified TB at the zone level is presented in the appendix (
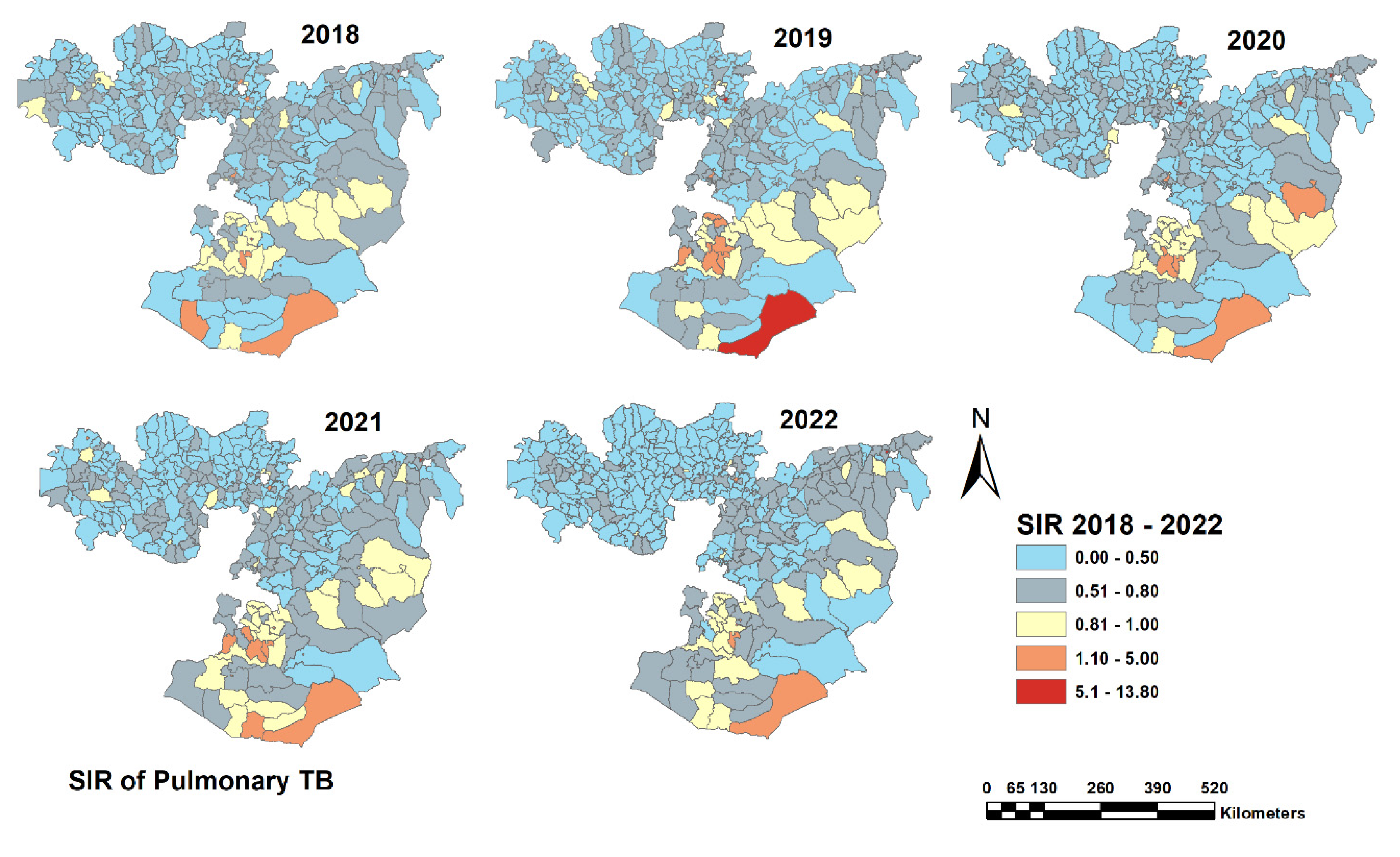
Table S4). Spatial variation in the notified TB TB case notification was also observed at the district levels with a standardized incidence ratio (SIR) varying from 0.16 in Horro district in Horro Guduru Wollega Zone to 9.6 in Kercha District in the West Guji zone.
Figure 1 shows the distribution of TB SIR at the district level in the Oromia region. The highest SIR of TB was found in districts located in the southern part of the region, and in districts near the Somali region. The SIR of notified TB was relatively low in the western part of the region.
Spatial clustering of TB
The global Moran’s index statistic value for PTB notifications in each year between 2018 and 2022 was consistently positive ranging from 0.0657 to 0.1604 (p-value < 0.001), furthermore, a significant spatial autocorrelation (Z= 5·785, P< 0·001) was observed in the average annual PTB notification indicating the presence of significant, positive spatial autocorrelation in TB notification rate over the whole study area (
Table 2). These findings suggest that the distribution of TB in the Oromia region was not random but exhibited significant spatial autocorrelation over the five years.
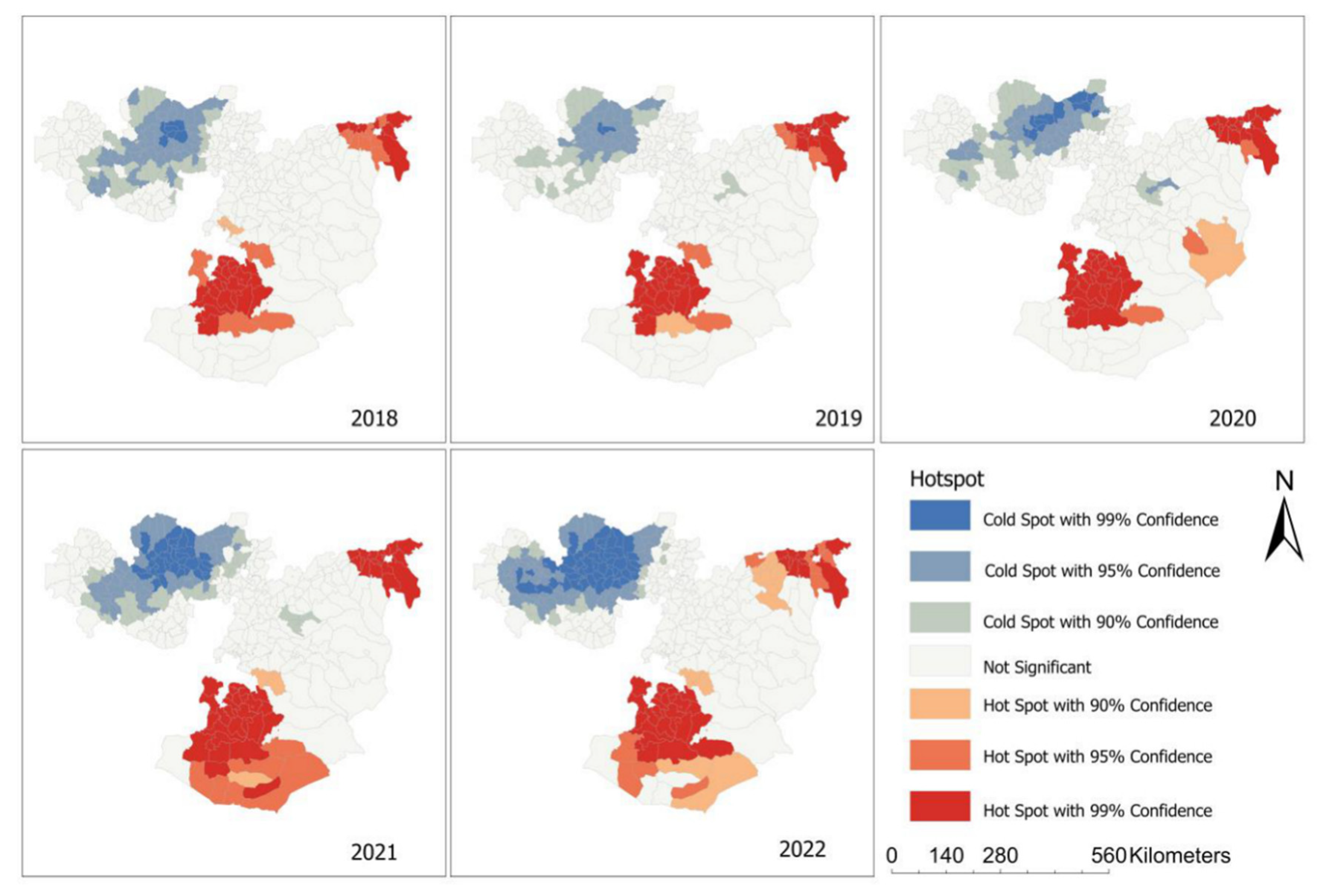
Based on our clustering analyses using the Getis–Ord G statistic, some districts were identified as hot spots and cold spots (
Figure 2).
The hot spot districts, indicating a higher-than-expected TB case notification compared to the regional average, were in the northern and southern parts of the region, while the cold spot districts were located in the western parts of the region. Over five years, the hotspots in the southern parts of the region experienced significant expansion, resulting in the spread of TB to neighboring districts.
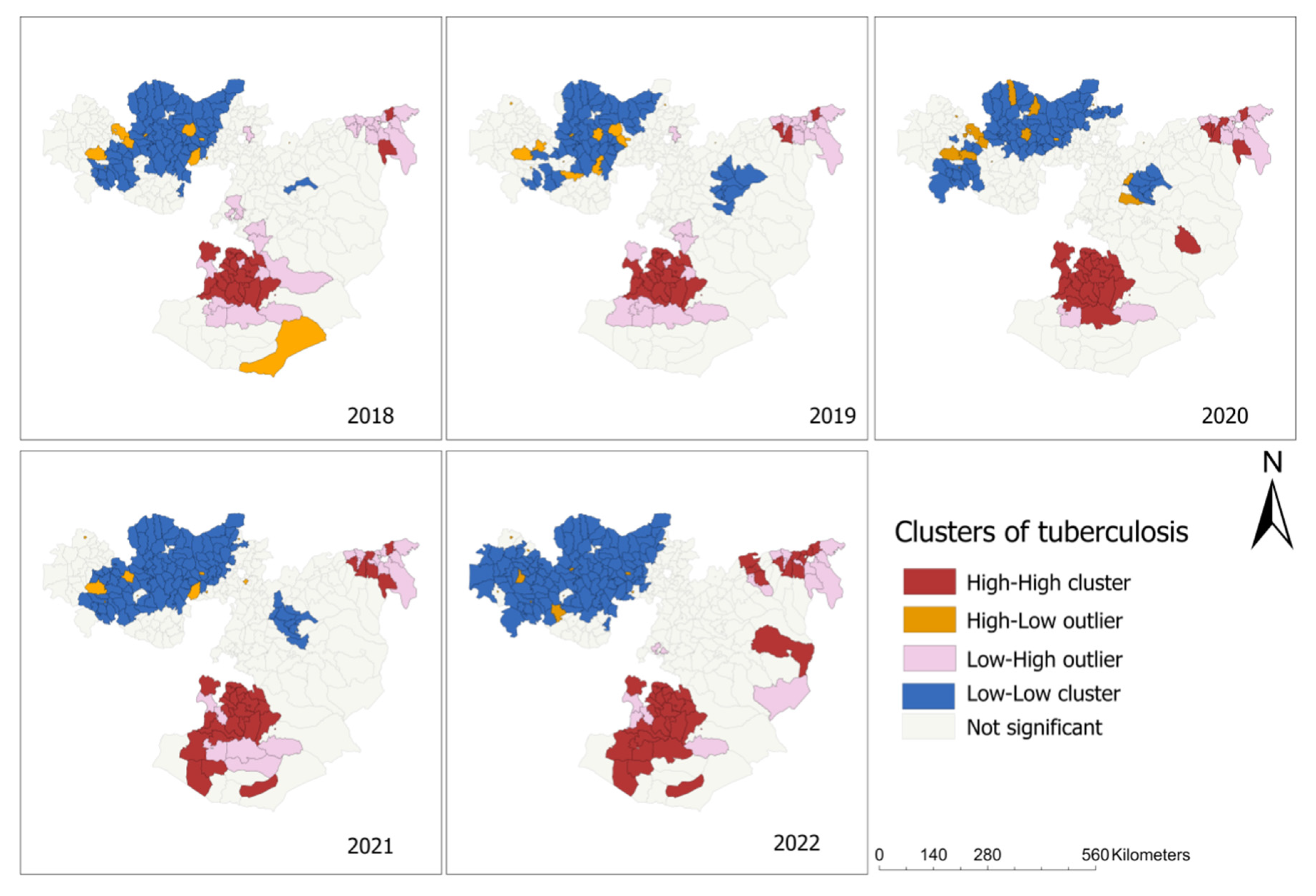
In the local Moran’s I analysis, districts located in the south and north parts of the region such as Bule Hora town in West Guji zones showed a high-high type of relationship, meaning that these districts had a high notification of TB cases and the surrounding district also had high TB case notification (
Figure 3). Some districts in the western part of the region had a high-low type of relationship which indicated that there was a high TB case notification in these districts, surrounded by districts with a low TB case notification. Low-low clusters of TB were found in Begi districts in the West Wollega zone (
Figure 3).
The result from the non-spatial univariate Bayesian regression model
According to the result of univariate analysis, all the variables examined in this study exhibited a significant association with TB notification (
Table S2). However, to address the issue of multicollinearity among covariates, the variable humidity was excluded from the final model since its VIF value exceeded 6.
The result from the Spatiotemporal Bayesian regression model
Table 3 shows the Bayesian multivariable Poisson regression model of ecological-level factors associated with TB in the Oromia region. Variables of HIV positivity rate and wind speed were negatively associated with notified TB.
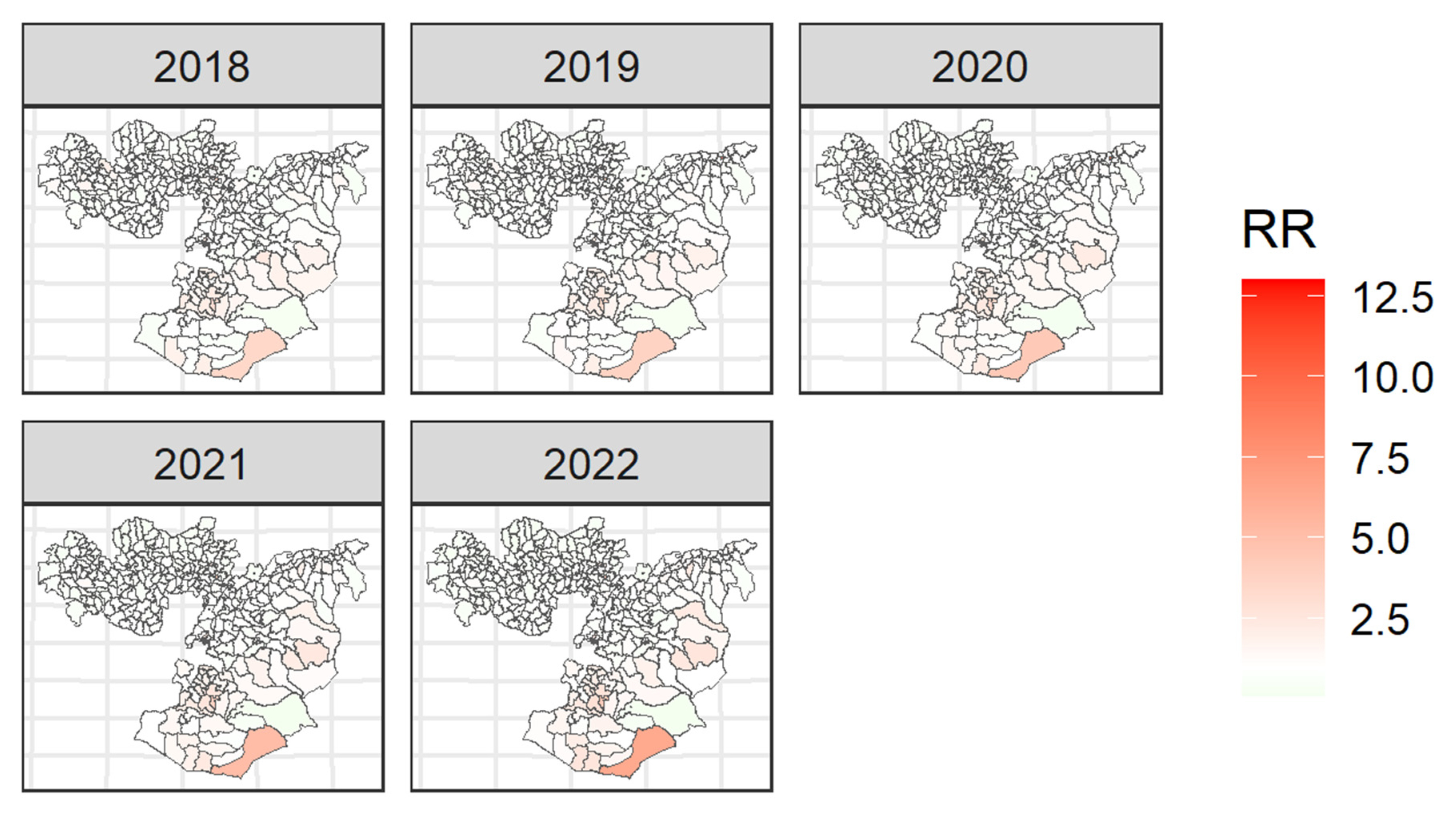
All variables included in the final model were significantly associated with TB incidence in the Oromia region except the annual mean precipitation. After accounting for the ecological-level factors in the model, the posterior mean of spatially structured random effects was found to be clustered in the region (
Figure 4). This indicates that a substantial amount of district-level heterogeneity in TB remained unexplained by the ecological level factors included in our models.
4. Discussion
The study conducted a comprehensive analysis of the spatiotemporal trend of TB notification within districts in the Oromia region. Its primary objectives included identifying clusters of hotspots and trends in TB case notification, evaluating the influence of socio-demographic characteristics and environmental conditions on TB prevalence, and exploring the impact of health-related factors on the distribution of the disease. By examining these factors, the study aimed to provide valuable insights into the dynamics of TB distribution within the region.
In our current study, we reported several significant findings regarding the distribution of pulmonary TB in the Oromia region. Firstly, we observed distinct trends in TB occurrences over the study period, noting changes and patterns in both annual and seasonal occurrences. Secondly, we identified hot spot areas with concentrated TB cases, providing valuable insights for targeted interventions and resource allocations. Thirdly, we identified a cluster of TB cases, indicating areas with higher transmission rates and shared risk factors. Lastly, our study revealed an association between ecological factors and TB notification, highlighting potential drivers of transmission and risk factors within the studied population in districts of the Oromia region.
The spatial clustering of TB showed a trend: Our study also showed that TB was found to be clustered in the southern parts of the region consistently for five years. This clustering can be attributed to several factors. Firstly, the presence of numerous mining shafts in select districts of the southern part contributes to this phenomenon. Moreover, these districts share a border with Kenyan districts as there is geographical proximity and population movements across the border increasing the likelihood of cross-border transmission of TB, which further reinforces the clustering of TB cases in this particular area. This finding emphasized the need for coordinated efforts and strengthened collaboration between Ethiopia and neighboring countries to effectively control TB transmission in a cross-border context.
TB notification rates varied before and after the COVID-19 pandemic with the lowest TB case notification reported during the COVID-19 pandemic in 2020. Similar findings were reported in recent studies in which TB notification rates were decreased during the COVID-19 pandemic, partly due to the collapse of the health systems to diagnose and report TB cases and due to patients' fear to visit health facilities [
19]. As in many other countries, COVID-19 has put a negative impact on TB control programs in Ethiopia which affected TB case detection, interrupted community-based interventions, and resulted in the diversion of resources including human resources, from the TB control program to the COVID-19 response [
1,
20].
We observed notable seasonal variations in the notification of TB, specifically, our findings indicated a peak in TB cases between January and March (dry season) with troughs from July to September (rainy season). The findings in this study corroborate with a study conducted in Ethiopia which showed higher and lower TB case notifications during the dry and rainy seasons, respectively [
21,
22,
23,
24]. In Ethiopia, the dry season occurs from January to March, immediately following the harvest season in most rural societies. During these periods, agricultural activities become less demanding, allowing individuals in rural societies to experience the freedom to visit health facilities, and the probability of TB diagnosis during this time frame will be high. Conversely, the rainy season, specifically from July to September is characterized by intensive agricultural activities among the rural population whose livelihoods are heavily dependent on farming. In addition, during these months, individuals in rural communities dedicate extensive hours to working in their fields, while the healthcare-seeking tendency is restricted due to heavy rainfall and agricultural commitments. These situations could potentially contribute to a decreased number of TB cases. These findings suggest the need to investigate season-specific strategies for TB case finding in Ethiopia.
Densely populated districts were highly vulnerable to TB distribution: The spatiotemporal distribution of TB was positively associated with demographic factors. Accordingly, our present study revealed an association between TB notification and population density. This aligns with previous studies, which consistently indicate relatively a higher prevalence of TB in areas characterized by higher population density, particularly in urban settings when compared to less densely populated rural areas [
10,
25,
26,
27]. In areas with high population density, where overcrowded living conditions are common, there is an increased risk of TB transmission due to the proximity of individuals [
28]. Moreover, the limited access to quality healthcare services and poor sanitation exacerbate the situation. The combination of these factors, along with a higher prevalence of HIV and other risk factors, contributes to the occurrence of high TB prevalence [
4,
10]. By addressing the unique challenges posed by population density, health authorities can work towards reducing the prevalence of TB in these areas and improving overall health outcomes.
Our study also showed that TB case notification was higher in males than females. Similar studies conducted in different parts of the world including Ethiopia revealed that a higher TB case notification of TB was observed in males than in females [
7,
9,
29,
30]. This might be attributed to their strong social interactions, staying in overcrowded situations, and the high drinking and smoking habits of males, all of which contribute to the development of TB [
31,
32]. Immunological differences between males and females (which favors women), and the impact of sex hormones on TB susceptibility and progression [
33] might also contribute to the occurrence of higher TB in males. On the other hand, health-seeking behavior, stigma, socioeconomic determinants and barriers, and misdiagnosis (such as poor quality of TB screening during pregnancy), [
32] might be associated with lower TB case notification of notified TB in females. Efforts aimed at mitigating gender disparities in TB incidence should prioritize the promotion of gender equity, enhancing healthcare accessibility, and fostering disease awareness among individuals of all genders.
Metrological factors should be considered in TB control and prevention strategies: Our current study revealed a significant correlation between metrological factors and the notification of TB cases. Specifically, we found a positive relationship between temperature and TB case notification. These findings are consistence with many studies conducted globally, including Ethiopia, which also reported the link between temperature and TB notification, particularly in the case of pulmonary TB [
23,
34,
35,
36,
37]. The association between temperature and TB notification has been widely acknowledged and assumed in the scientific community. However, extremely high or low temperatures can elevate the likelihood of growth and transmission of
M. tuberculosis which is the causative agent for TB [
38,
39]. Thus our study further reinforces the understanding that temperature plays a crucial role in influencing the occurrence or distribution of TB cases.
Additionally, in our present study, the variable wind speed was found to have the opposite effect on TB notifications. A similar finding was reported in a study conducted in mainland China [
40,
41]. The transmission of
M. tuberculosis may be hindered by low wind speed [
42,
43,
44]. Further explorations are necessary to fully comprehend the mechanism underlying the negative correlation observed between wind speed and TB distribution.
District-level primary health care service strongly affected TB case notification
In our present study, district-level health service coverage was positively associated with TB case notification. Many studies revealed a direct association between TB case notification and health service coverage. Based on this, increased TB case notification can be justified by improved health service coverage [
28,
36,
45]. As part of health service coverage, community-level health extension workers carry out the identification of TB suspects and referral of the suspects for diagnosis, this might lead to higher levels of case identification, resulting in increased TB case notification [
46]. Enhanced district-level health service coverage and investing in community-level health extension workers can improve TB case notification.
As part of health service coverage increased TB case notification can be justified by laboratory diagnostic coverage [
47]. In our present study, laboratory diagnostic coverage is positively associated with TB case notification. Many studies revealed the direct relationship between TB notification and laboratory diagnostic coverage or access. When there is wider access to laboratory diagnostic services for TB, more cases can be accurately diagnosed and confirmed. This leads to an increased number of TB cases being notified to the health system.
The variable HIV positivity ratio was found to be negatively associated with TB case notification in our current study. This type of finding is not common as there is a direct relationship between HIV and TB [
1,
48,
49,
50]. The negative association observed in this study may be attributed to several factors, including the provision of TB preventive therapy, the prompt or the same-day initiation of antiretroviral therapy (ART), and clinical evaluation for individuals diagnosed with HIV. These interventions, such as rapid ART initiation and the same-day service along with strong TB/HIV collaborative activities, potentially play a significant role in influencing the observed negative association. Further studies are needed to explore additional factors that could contribute to the observed negative association to gain a more comprehensive understanding of the phenomenon.
This study made significant contributions to the spatiotemporal analysis of TB case notification in the Oromia region of Ethiopia. All districts in the region were included in the analysis. However, there are some limitations. Firstly, the data used in the study was extracted from a centralized HMIS. This raises the possibility of under-reporting of TB cases in some districts. In other words, the low TB case notification rates in many districts may not accurately reflect the actual burden of the disease in those districts as the extrapulmonary TB case category was not included in the analysis. A wide range of data was employed as independent variables, sourced from different outlets, such as -non-HMIS or parallel reports and websites, which were compiled by different organizations. Consequently, the analysis of the relationship between data from these diverse sources may introduce certain biases that can impact the obtained results.
5. Conclusions
Substantial spatial variations in the distribution of notified TB TB case notifications were observed at zonal and district levels with most of the hotspot areas detected in the northern and southern parts of the region. The spatiotemporal distribution of notified TB incidence was positively associated with population density. Efforts aimed at combating TB should extend beyond simply halting its transmission. It is important to proactively assess the potential distribution of diseases by analyzing past occurrences concerning diverse ecological factors. Implementing preventive measures that account for socio-demographic, meteorological, and health system factors can be strategically focused on areas at high risk, resulting in effective control in the Oromia region.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Figure S1: title; Table S1: title; Video S1: title.
Author Contributions
Conceptualization, D.B., Methodology, D.B., T.D., and K.A.A.; Software, D.B., T.D., K.A.A., and S.W.; Formal analysis, D.B., T.D., K.A.A., and S.W., Investigation, D.B., K.T., S.A., T.D., K.A.A., S.W. M.M., G.G., B.D., D.A., T.K., A.B., B.K., D.G. B.A., D.M., D.H., and G.M., Data curation, D.B., K.T., S.A., T.D., K.A.A., S.W. M.M., G.G., B.D., D.A., T.K., A.B., B.K., D.G. B.A., D.M., D.H., K.G., and G.M., Writing original draft preparation, D.B., K.T., S.A., T.D., K.A.A., S.W. M.M., G.G., and B.D.; Writing review and editing, D.B., K.T., S.A., T.D., K.A.A and M.M., Supervision, K.T., S.A., G.S., D.A., T.K., A.B., and K.G., Project administration, K.T., S.A., G.S., D.A., T.K., A.B., and K.G. All authors have read the manuscript and agreed on the journal to which the manuscript submitted.
Funding
This research received no external funding.
Informed Consent Statement
Since the data obtained from the DHIS were aggregated and did not contain any personal information, obtaining informed consent was not necessary. Oromia Regional Health Bureau’s Ethical Review Committees reviewed and approved the study protocol.
Data Availability Statement
The information presented in this study is available on request from the corresponding author.
Acknowledgments
Addis Ababa University, College of Natural and Computational Science, Department of Microbial, Cellular, and Molecular Biology. Oromia region health bureau. We are also grateful in extending our thanks to Mr. Sisay and Mr. Nigusie from the Oromia region land bureau for providing us with the regional shapefile.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviation
| CrI |
Credible interval |
| DIC |
Devian Information Criterea |
| DHIS |
District Health Information System |
| DOTS |
Directly Observed Treatment Short-course |
| GIS |
Geographical information system |
| HIV |
Human Immunodeficiency Virus |
| HMIS |
Health Management Information System |
| RR |
Relative risk |
| SIR |
Standardized Incidence Ratio |
| SD |
Standard deviation |
| TB |
Tuberculosis |
| VIF |
Variance inflation factors |
| WHO |
World Health Organization |
References
- WHO World Health Organization (WHO). Global Tuberculosis Report; 2022; ISBN 9789240061729.
- WHO World Health Organization (WHO). Global Tuberculosis Report; Geneva, 2021; ISBN 9780415475976.
- Titosse, A.C.; Pimenta Rodrigues, M.V.; Marques Ramos, A.P.; Prado Osco, L.; Giuffrida, R.; Da Silva Fonseca, E.; Azevedo Arana, A.R. Tuberculosis Space-Temporal Distribution from 2011 to 2016 in the Municipality of Maputo, Mozambique. Población y Salud en Mesoamérica 2020, 18. [CrossRef]
- Woldeyohannes, S.M. Worldwide Spatial and Temporal Distribution of Tuberculosis (TB). J. AIDS Clin. Res. 2015, 06. [Google Scholar] [CrossRef]
- Asemahagn, M.A.; Alene, G.D.; Yimer, S.A. Spatial-Temporal Clustering of Notified Pulmonary Tuberculosis and Its Predictors in East Gojjam Zone, Northwest Ethiopia. PLoS One 2021, 16, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Xu, C.; Hu, M.; Qiao, J.; Chen, W.; Li, T.; Qian, S.; Yan, M. Spatio-Temporal Variation in Tuberculosis Incidence and Risk Factors for the Disease in a Region of Unbalanced Socio-Economic Development. BMC Public Health 2021, 21, 1–11. [Google Scholar] [CrossRef]
- Tadesse, S.; Enqueselassie, F.; Hagos, S. Spatial and Space-Time Clustering of Tuberculosis in Gurage Zone, Southern Ethiopia. PLoS One 2018, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Dangisso, M.H.; Datiko, D.G.; Lindtjørn, B. Spatio-Temporal Analysis of Smear-Positive Tuberculosis in the Sidama Zone, Southern Ethiopia. PLoS One 2015, 10, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Shaweno, D.; Shaweno, T.; Trauer, J.M.; Denholm, J.T.; McBryde, E.S. Heterogeneity of Distribution of Tuberculosis in Sheka Zone, Ethiopia: Drivers and Temporal Trends. Int. J. Tuberc. Lung Dis. 2017, 21. [Google Scholar] [CrossRef] [PubMed]
- Alene, K.A.; Clements, A.C.A. Spatial Clustering of Notified Tuberculosis in Ethiopia : A Nationwide Study. 2019, 1–11.
- OIC Oromia Region, Investment Commission. May 20, 2021. Available online: http://oromiainvest.com/oromia_at_a_glance/# (accessed on 20 May 2021).
- FMoH Health Management Information System (HMIS)/Monitoring and Evaluation (M&E). 2008, 26–29.
- Bogale, A. Implementation Status of Health Management Information System in Hospitals of South West Shoa Zone, Oromia, Central Ethiopia. Clin. Outcomes Res. 2021, 13, 1–8. [Google Scholar] [CrossRef]
- FMOH Guidelines for Management of TB, DR-TB and Lerosy in Ethiopia Sixth Edition August 2018 Addis Ababa; 2018; ISBN 9781626239777.
- NASA NASA Prediction Of Worldwide Energy Resources. Available online: https://power.larc.nasa.gov/ (accessed on 10 April 2023).
- FMOH HMIS Indicators Reference Guide Technical Standards : 2017, 1.
- Zhang, K.; Liu, J.; Liu, Y.; Zhang, P.; Carroll, R.J. Bayesian Adjustment for Measurement Error in an Offset Variable in a Poisson Regression Model. Stat. Modelling 2022, 22, 509–526. [Google Scholar] [CrossRef]
- Moraga, P. Geospatial Health Data; 2019; ISBN 9780367357955.
- Togun, T.; Kampmann, B.; Stoker, N.G.; Lipman, M. Anticipating the Impact of the COVID-19 Pandemic on TB Patients and TB Control Programs. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 1–6. [Google Scholar] [CrossRef]
- Arega, B.; Negesso, A.; Taye, B.; Weldeyohhans, G.; Bewket, B.; Negussie, T.; Teshome, A.; Endazenew, G. Impact of COVID-19 Pandemic on TB Prevention and Care in Addis Ababa, Ethiopia: A Retrospective Database Study. BMJ Open 2022, 12, 1–6. [Google Scholar] [CrossRef]
- Tadesse, T.; Demissie, M.; Berhane, Y.; Kebede, Y.; Abebe, M. Incidence of Smear-Positive Tuberculosis in Dabat, Northern Ethiopia. Int. J. Tuberc. Lung Dis. 2013, 17, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Gashu, Z.; Jerene, D.; Datiko, D.G.; Hiruy, N.; Negash, S.; Melkieneh, K.; Bekele, D.; Nigussie, G.; Suarez, P.G.; Hadgu, A. Seasonal Patterns of Tuberculosis Case Notification in the Tropics of Africa: A Six-Year Trend Analysis in Ethiopia. PLoS One 2018, 13, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Alene, K.A.; Viney, K.; McBryde, E.S.; Clements, A.C.A. Spatiotemporal Transmission and Socio-Climatic Factors Related to Paediatric Tuberculosis in North-Western Ethiopia. Geospat. Health 2017, 12, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Wubuli, A.; Li, Y.; Xue, F.; Yao, X.; Upur, H.; Wushouer, Q. Seasonality of Active Tuberculosis Notification from 2005 to 2014 in Xinjiang, China. PLoS One 2017, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Alene, K.A.; Viney, K.; McBryde, E.S.; Clements, A.C.A. Spatial Patterns of Multi-Drug Resistant Tuberculosis and Relationships to Socioeconomic, Demographic and Household Factors in Northwest Ethiopia. PLoS One 2017, 12, 1–14. [Google Scholar] [CrossRef]
- Wubuli, A.; Xue, F.; Jiang, D.; Yao, X.; Upur, H. Socio-Demographic Predictors and Distribution of Pulmonary Tuberculosis ( TB ) in Xinjiang, China : A Spatial Analysis. 2015, 2013, 1–22. [CrossRef]
- Clark, M.; Nowgesic, E. The Association of Housing Density, Isolation, and Tuberculosis in Canadian First Nations Communities. 2002, 940–945.
- Dangisso, M.H.; Datiko, D.G.; Lindtjørn, B. Accessibility to Tuberculosis Control Services and Tuberculosis Programme Performance in Southern Ethiopia. Glob. Health Action 2015, 8, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Wu, B.; Wu, C.; Wang, Q.; Hu, D.; Chen, W. Spatial-Temporal Analysis of Tuberculosis in Chongqing, China 2011-2018. BMC Infect. Dis. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Li et al Spatial-Temporal Analysis of Pulmonary Tuberculosis in the Northeast of the Yunnan Province, People’s Republic of China. BioMed Cent. 2017, 35–44.
- Jagielski, T.; Minias, A.; van Ingen, J.; Rastogi, N.; Brzostek, A.; Żaczek, A.; Dziadek, J. Methodological and Clinical Aspects of the Molecular Epidemiology of Mycobacterium Tuberculosis and Other Mycobacteria. Clin. Microbiol. Rev. 2016, 29, 239–290. [Google Scholar] [CrossRef]
- Zhu, Q.Q.; Wu, Q.; Wang, A.M.; Bao, F.J.; Zhang, Y.Z.; Liu, J.; Yan, J.W.; Fang, X.H.; Li, L.; Zhang, Z.K.; et al. Epidemiological Characteristics of Pulmonary Tuberculosis in Anhui Province, Eastern China from 2013 to 2018. PLoS One 2020, 15, 1–11. [Google Scholar] [CrossRef]
- Bini, E.I.; Mata Espinosa, D.; Marquina Castillo, B.; Barrios Payán, J.; Colucci, D.; Cruz, A.F.; Zatarain, Z.L.; Alfonseca, E.; Pardo, M.R.; Bottasso, O.; et al. The Influence of Sex Steroid Hormones in the Immunopathology of Experimental Pulmonary Tuberculosis. PLoS One 2014, 9, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Gelaw, Y.; Yu, W.; Magalha, R.; Assefa, Y.; Williams, G. Effect of Temperature and Altitude Difference on Tuberculosis Notification: A Systematic Review. J. Glob. Infect. Dis. 2019, 11, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Hao, Y.; Fei, Z.Y.; He, J. Effect of Meteorological Factors on Incidence of Tuberculosis: A 15-Year Retrospective Study Based on Chinese Medicine Theory of Five Circuits and Six Qi. Chin. J. Integr. Med. 2015, 21, 751–758. [Google Scholar] [CrossRef]
- Li, X.X.; Wang, L.X.; Zhang, J.; Liu, Y.X.; Zhang, H.; Jiang, S.W.; Chen, J.X.; Zhou, X.N. Exploration of Ecological Factors Related to the Spatial Heterogeneity of Tuberculosis Prevalence in P. R. China. Glob. Health Action 2014, 7. [Google Scholar] [CrossRef]
- Kiani, B.; Raouf Rahmati, A.; Bergquist, R.; Hashtarkhani, S.; Firouraghi, N.; Bagheri, N.; Moghaddas, E.; Mohammadi, A. Spatio-Temporal Epidemiology of the Tuberculosis Incidence Rate in Iran 2008 to 2018. BMC Public Health 2021, 21, 1–20. [Google Scholar] [CrossRef]
- Li, H.; Ge, M.; Zhang, M. Spatio-Temporal Distribution of Tuberculosis and the Effects of Environmental Factors in China. BMC Infect. Dis. 2022, 22, 1–13. [Google Scholar] [CrossRef]
- Keerqinfu, *!!! REPLACE !!!*; Zhang, Q.; Yan, L.; He, J. Keerqinfu; Zhang, Q.; Yan, L.; He, J. Time Series Analysis of Correlativity between Pulmonary Tuberculosis and Seasonal Meteorological Factors Based on Theory of Human-Environmental Inter Relation. J. Tradit. Chinese Med. Sci. 2018, 5, 119–127. [CrossRef]
- Guo, C.; Du, Y.; Shen, S.Q.; Lao, X.Q.; Qian, J.; Ou, C.Q. Spatiotemporal Analysis of Tuberculosis Incidence and Its Associated Factors in Mainland China. Epidemiol. Infect. 2017, 145, 2510–2519. [Google Scholar] [CrossRef] [PubMed]
- Cao, K.; Yang, K.; Wang, C.; Guo, J.; Tao, L.; Liu, Q.; Gehendra, M.; Zhang, Y.; Guo, X. Spatial-Temporal Epidemiology of Tuberculosis in Mainland China: An Analysis Based on Bayesian Theory. Int. J. Environ. Res. Public Health 2016, 13, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; He, L.; Chen, Y.; Wang, Q.; Meng, Q.; Chang, W.; Xiong, L.; Yu, Z. The Influence of Meteorological Factors on Tuberculosis Incidence in Southwest China from 2006 to 2015. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, M.; Wu, S.S.; Jiang, H.; Zhang, J.; Wang, S.; Ma, W.; Li, Q.; Ma, Y.; Liu, Y.; et al. Spatial Distribution of Tuberculosis and Its Association with Meteorological Factors in Mainland China. BMC Infect. Dis. 2019, 19, 1–7. [Google Scholar] [CrossRef]
- Li, Z.; Liu, Q.; Zhan, M.; Tao, B.; Wang, J.; Lu, W. Meteorological Factors Contribute to the Risk of Pulmonary Tuberculosis: A Multicenter Study in Eastern China. Sci. Total Environ. 2021, 793, 148621. [Google Scholar] [CrossRef] [PubMed]
- Van Gurp, M.; Rood, E.; Fatima, R.; Joshi, P.; Verma, S.C.; Khan, A.H.; Blok, L.; Mergenthaler, C.; Bakker, M.I. Finding Gaps in TB Notifications: Spatial Analysis of Geographical Patterns of TB Notifications, Associations with TB Program Efforts and Social Determinants of TB Risk in Bangladesh, Nepal and Pakistan. BMC Infect. Dis. 2020, 20, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Datiko, D.G.; Yassin, M.A.; Theobald, S.J.; Blok, L.; Suvanand, S.; Creswell, J.; Cuevas, L.E. Health Extension Workers Improve Tuberculosis Case Finding and Treatment Outcome in Ethiopia: A Large-Scale Implementation Study. BMJ Glob. Heal. 2017, 2, 1–8. [Google Scholar] [CrossRef] [PubMed]
- MOH Tbl-Nsp July 2021 – June 2026 August 2020. 2021. 26 August.
- Kulldorff, M. A Spatial Scan Statistic. Biometry Branch, DCP, Natl. Cancer Inst. 1997, 1848–1848.
- Waters, N. A Review of “Handbook of Applied Spatial Analysis: Software Tools, Methods and Applications”; 2012; Vol. 102; ISBN 9783642036460.
- Approach, P.H.; On, C.G. Guidelines Hiv Prevention, Testing, Treatment, Service Delivery and Monitoring:; 2021; ISBN 9789240031593.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).