Submitted:
31 July 2023
Posted:
02 August 2023
Read the latest preprint version here
Abstract
Keywords:
1. Introduction
2. History of Telemedicine
- Functional diagnoses are made based on short-time examinations, which have little to do with the proper working environment regarding the temporal aspect [40].
- Studies are mostly conducted with a few persons with limited statistical power. In addition, "idealized persons" are recruited, i.e., mostly young men aged between 20 and 30 years, sporty, with normal weight, etc. However, the results are then extrapolated and transferred to all other persons. But the transfer can neither be applied to all age groups (age physiology) nor both genders (gender physiology).
- In the real human environment, numerous additional influences significantly impact performance capability and resilience [54]. In this context, the combination of temperature, altitude (oxygen pressure), wind, radiation, precipitation, pressure changes, noise disturbances, etc., must be mentioned [55]. The complexity of these factors is not taken into account in the laboratory.
- In the future, more reliable indices will have to include more parameters on the one hand and take into account intra-individual dynamic factors, e.g., sleep deficit, inadequate food intake, beginning or healing infectious diseases, or influences due to the unique environment (family, friends, etc.) [56]. “Dynamic” in this context primarily means weighting the individual parameters, which may sometimes impact the person in the respective situation, sometimes more or less intensively [57].
3. Physiological Monitoring in the Military Area
4. Occupational Fields of High Responsibility in a Stressful Environment
- No impairment of flight safety and the activities of flying personnel
- Small dimensions and low weight
- No changes concerning aircraft engineering (except for attachment of the transmitter and the antenna as well as the power supply from the aircraft electrical system for the transmitter)
- Low operating and servicing effort
- No disturbing influences on airborne equipment and no corresponding disturbances of the biotelemetry device
- High stability with regard to flight and environmental factors
- Relatively high transmitter power to bridge long distances, with high constancy of the transmission frequency
5. Current Technologies
5.1. Sensors for Field Use
5.2. Smart Textiles
5.3. Electronic Transfer Routes
6. Current Systems
6.1. Mobile Medical Terminals - Wearables
6.1.1. POLAR®
6.1.2. Vitaport
6.1.3. SenseWear
6.1.4. Equivital Hidalgo
6.1.5. Zephyr
6.1.6. Sensor Mobile SM 100
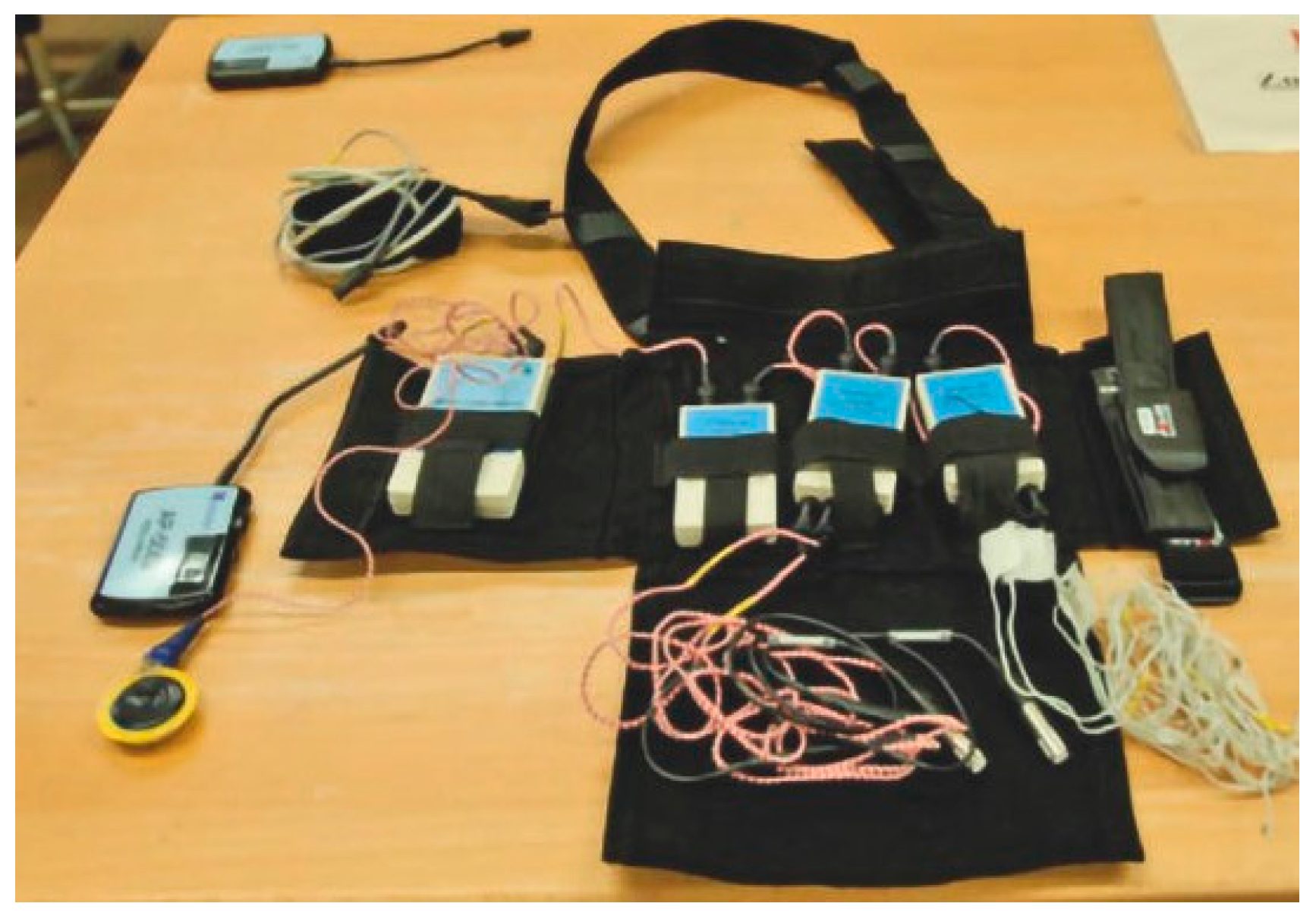
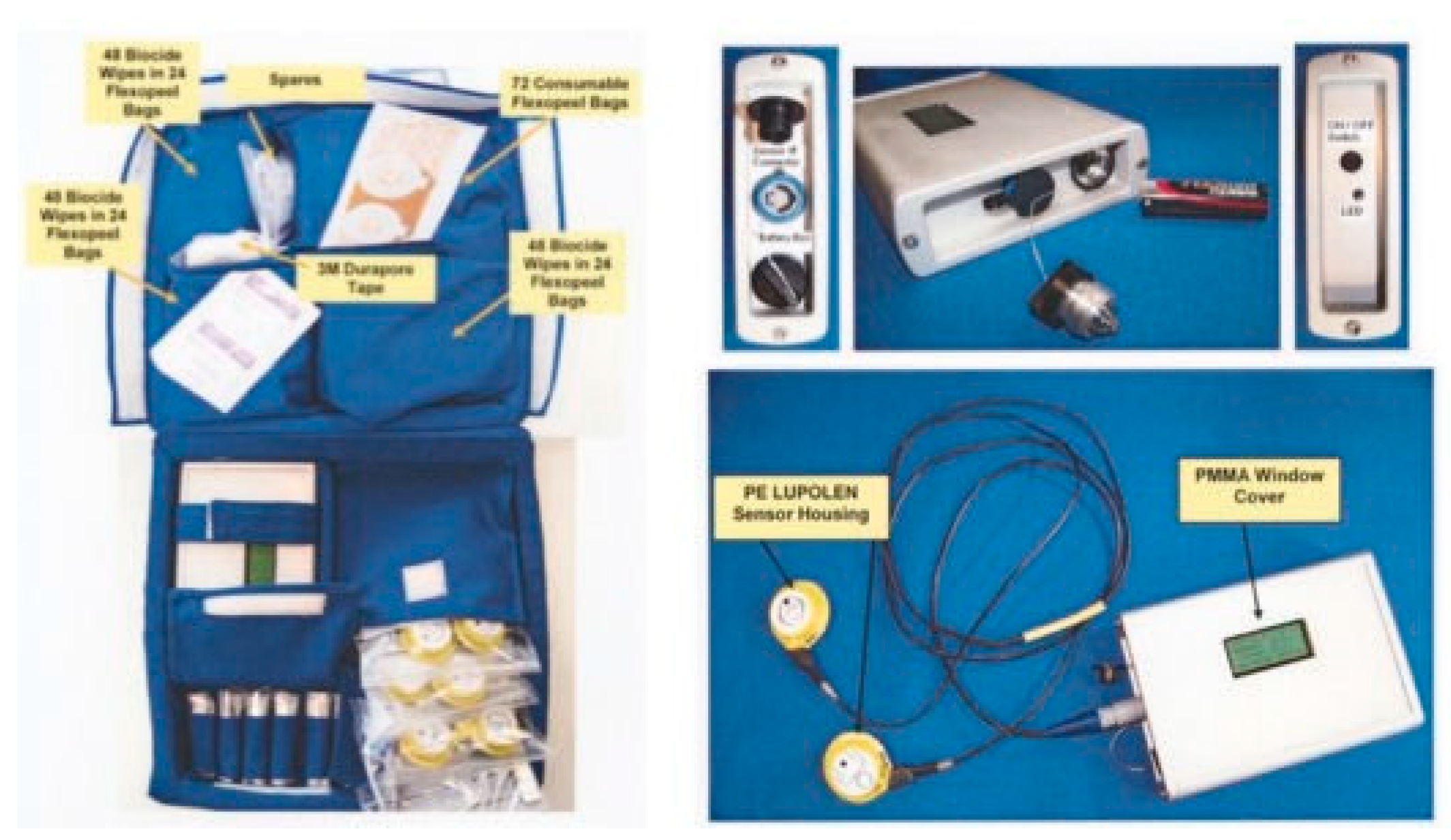
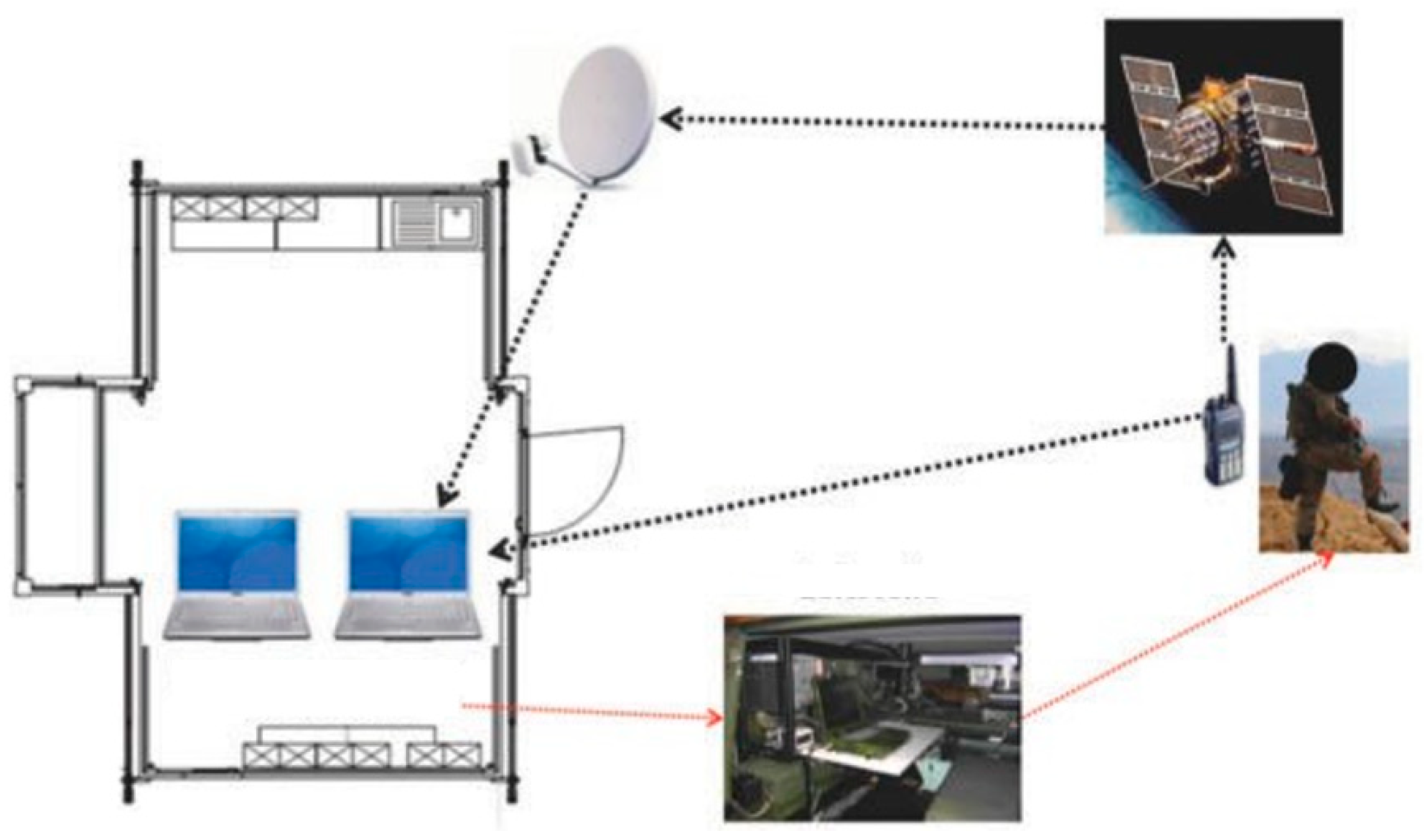
7. Recent Developments: The Mobile Physiological Laboratory
- The analog and digital measuring techniques are distributed among several small units and can, for example, be placed in a vest.
- The connection of unique measuring methods (e.g., core body temperature, heart rate, fundamental vocal frequency, etc.) is possible due to the development of a corresponding satellite, which can be used directly on the system without any further settings.
- The central processing unit automatically recognizes the respective satellites and immediately records the data with the satellite's signal-specific parameters.
- With the help of the software and hardware provided, users can also develop satellites and programs of their own.
- Moreover, the system can monitor the data online and thus already evaluate them.
- Metabolic and Physiological Changes in the Human Organism during Overwintering in the Antarctic [133]
- Monitoring of Vital Parameters in a Real-World Environment Using a Flexible Modular Telephysiological System [134]
- Oxygen Supply for Parachutists at Operational Altitudes – Laboratory Studies and their Benefits in an Extreme and a Real-World Environment [135]
- Heat Exposure of Jet Pilots during Air Traffic [136]
- Mars500 Project – Circadian Rhythm and Body Core Temperature in Humans during Long-Term Isolation and Confinement [137]
- The Role of Exercise in Synchronizing the Circadian Timing System during 60 Days of Bed-Rest [138]
- Core Body Temperature Changes during Long-Duration Space Flights [139]
- Provision of emergency functions and algorithms [140]
- Development of built-in-test (BIT) functions to ensure operation through monitoring of all necessary functions, including power supply
- Algorithms regarding the trend statement of vital parameters during missions
- Recording of system parameters
- Safety functions for the mission duration (reliability)
- Unique algorithms for processing large and complex data quantities with low demand for computing power, yielding a valid diagnostic value
- Data safety (especially for military use) and person’s privacy
8. Discussion & Conclusions
Author Contributions
Funding
Declaration of conflicting interests
Ethical approval
Guarantor
Acknowledgment
Author Statement
References
- World Health Organization. The Challenge of Obesity – Quick Statistics. Available online: www.euro.who.int/en/health-topics/ noncommunicable-diseases/obesity/data-and-statistics (accessed on 20 May 2023).
- The State of Obesity. Available online: http://stateofobesity.org (accessed on 20 May 2023).
- Rohde, U.; Sievert, A.; Rüther, T.; Witzki, A.; Leyk, D. Concept for a Predeployment Assessment of Basic Military Fitness in the German Armed Forces. J. Strength Cond. Res. 2015, 29, S211–S215. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Campbell, A.S.; de Ávila, B.E.-F.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef] [PubMed]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable Sensors for Remote Health Monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- E-HEALTH-COM. Available online: www.e-health.com.eu/ (accessed on 20 May 2023).
- Stetter BJ, Buckeridge E, Nigg SR, Sell S, Stein T. Towards a wearable monitoring tool for in-field ice hockey skating performance analysis. Eur J Sport Sci 2019, 19, 893–901.
- Ajana, B. Digital health and the biopolitics of the Quantified Self. Digit. Heal. 2017, 3. [Google Scholar] [CrossRef]
- Allouch SB, van Velsen L. Fit by Bits: An Explorative Study of Sports Physiotherapists' Perception of Quantified Self Technologies. Stud Health Technol Inform 2018, 247, 296–300.
- Heyen, N.B. From self-tracking to self-expertise: The production of self-related knowledge by doing personal science. Public Underst. Sci. 2020, 29, 124–138. [Google Scholar] [CrossRef]
- Baron KG, Abbott S, Jao N, Manalo N, Mullen R. Orthosomnia: Are Some Patients Taking the Quantified Self Too Far? J Clin Sleep Med 2017, 13, 351–354.
- Fehrenbacher, K.; Apel, C.; Bertsch, D.; van der Giet, M.S.; van der Giet, S.; Grass, M.; Gschwandtl, C.; Heussen, N.; Hundt, N.; Kühn, C.; et al. Temporary threshold shift after noise exposure in hypobaric hypoxia at high altitude: results of the ADEMED expedition 2011. Int. Arch. Occup. Environ. Heal. 2021, 84, 1191–1199. [Google Scholar] [CrossRef]
- Kupper, T. [Workload and professional requirements for alpine rescue], Professoral Thesis, Dept. of Aerospace Medicine, RWTH Aachen Technical University, Aachen.
- Kupper, T. High altitude, hypoxia, and human performance (editorial). Med Sport 2010; 14: 1.
- Kupper, T. Occupational Health in Mountain rescue, in: Brugger, H., Zafren, K., Festi, L. (Eds.), Mountain Emergency Medicine. Edra, Milano 2021: pp。 599–608.
- Occupational Aspects of Alpine Helicopter Rescue Operations. Recommendation of the UIAA Medical Commission Vol.23. Union Internationale des Associations d'Alpinisme (Medical Commission), Bern / Switzerland, 2015.
- Küpper, T.; Hillebrandt, D.; Steffgen, J.; Schöffl, V. Safety in Alpine Helicopter Rescue Operations—Minimal Requirements of Alpine Skills for Rescue Personnel. Ann. Occup. Hyg. 2013, 57, 1180–1188. [Google Scholar] [CrossRef] [PubMed]
- Küpper, T.; Milledge, J.S.; Hillebrandt, D.; Kubalová, J.; Hefti, U.; Basnyat, B.; Gieseler, U.; Pullan, R.; Schöffl, V. Work in Hypoxic Conditions-Consensus Statement of the Medical Commission of the Union Internationale des Associations d'Alpinisme (UIAA MedCom). Ann. Occup. Hyg. 2011, 55, 369–386. [Google Scholar] [CrossRef] [PubMed]
- Küpper, T.; Steffgen, J.; Jansing, P. Cold Exposure During Helicopter Rescue Operations in the Western Alps. Ann. Occup. Hyg. 2003, 47, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Küpper T, Milledge JS, Hillebrandt D, Kubalová J, Hefti U, Basnyat B, Gieseler U, Pullan R, Schöffl V. Work in hypoxic conditions--consensus statement of the Medical Commission of the Union Internationale des Associations d'Alpinisme (UIAA MedCom). Ann Occup Hyg 2011, 55, 369–386.
- Küpper, T.; Steffgen, J.; Jansing, P. Cold Exposure During Helicopter Rescue Operations in the Western Alps. Ann. Occup. Hyg. 2003, 47, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Küpper, T.E.A.H.; Steffgen, J.; Jansing, P. Noise Exposure During Alpine Helicopter Rescue Operations. Ann. Occup. Hyg. 2004, 48, 475–481. [Google Scholar] [CrossRef]
- Lehmacher, E.J.; Jansing, P.; Küpper, T. Thermophysiological Responses Caused by Ballistic Bullet-Proof Vests. Ann. Occup. Hyg. 2004, 51, 91–96. [Google Scholar] [CrossRef]
- Einthoven, W. Le Télécardiogramme. Arch Int de Physiol 1906, 4, 132–164. [Google Scholar]
- Licklider JCR. Man-Computer Symbiosis. IRE Transactions of Human Factors in Electronics 1960; HFE-1: 4–11.
- Seising, R. Frühe Visionen der Telemedizin: Technische Möglichkeiten und gesellschaftliche Wirklichkeit [Early Visions of Telemedicine: Technical Possibilities and Social Reality]. INFORMATIK 2003 – Innovative Informatikanwendungen. 33. Jahrestagung der Gesellschaft für Informatik 2003 [Innovative informatics applications. 33rd Annual Conference of the German Informatics Society 2003], Frankfurt a.M.
- Gabriel, MR. Guide to the Literature of Electronic Publishing. London: Jai Pr; 1989.
- Alfred-Wegener-Institut. Neumayer Station III. Available online: www.awi.de/en/expedition/stations/neumayer-station-iii.html (accessed on 16 May 2023).
- Ivanova, T.; Sapunova, S.; Dandolov, I.; Ivanov, Y.; Meleshko, G.; Mashinsky, A.; Berkovich, Y. 'SVET' space greenhouse onboard experiment data received from 'MIR' station and future prospects. Adv. Space Res. 1994, 14, 343–346. [Google Scholar] [CrossRef]
- Shephard RJ, Aoyagi Y. Measurement of human energy expenditure, with particular reference to field studies: a historical perspective. Eur J Appl Physiol. 2012, 112, 2785–2815.
- Gunga, HC. Nathan Zuntz. His Life and Work in the Fields of High-Altitude Physiology and Aviation Medicine. American Physiological Society, Elsevier, ISBN 978-1-4614-7575-0, 2009.
- Zuntz N, Lehmann C, Hagemann O. Der Stoffwechsel des Pferdes bei Ruhe und Arbeit [The Metabolism of the Horse at Rest and Work]. Berlin: Parey; 1889.
- Zuntz N, Schumburg W. Studien zu einer Physiologie des Marsches [Studies on the Physiology of Marching]. Berlin: Hirschwald; 1901.
- Zuntz N, Loewy A, Müller F, Caspari W. Höhenklima und Bergwanderungen in ihrer Wirkung auf den Menschen [High Altitude Climate and Mountain Walks in their Effect on Humans]. Berlin: Bong; 1906.
- Zuntz, N. Zur Physiologie und Hygiene der Luftfahrt [On the Physiology and Hygiene of Aviation]. Berlin: Springer; 1912.
- Zuntz, N. Zur Methodik der Klimaforschung [On the Methodology of Climate Research]. Med Klin 1911, 22, 855–856. [Google Scholar]
- Johnston, D.W.; Anastasiades, P.; Wood, C. The Relationship Between Cardiovascular Responses in the Laboratory and in the Field. Psychophysiology 1990, 27, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Langewitz W, Rüddel H, Schächinger H et al. Standardized Stress Testing in the Cardiovascular Laboratory: Has It Any Bearing on Ambulatory Blood Pressure Values? J Hypertens Suppl 1989; 7: S41–S48.
- Pollak, M.H. Heart rate reactivity to laboratory tasks and ambulatory heart rate in daily life. Psychosom. Med. 1991, 53, 25–35. [Google Scholar] [CrossRef]
- Fahrenberg J, Heger R, Foerster F et al. Differentielle Psychophysiologie von Befinden, Blutdruck und Herzfrequenz im Labor-Feld-Vergleich [Differential Psychophysiology of Well-Being, Blood Pressure and Heart Rate in laboratory-field comparison]. Zeitschrift für Differentielle und Diagnostische Psychologie [Journal of Differential and Diagnostic Psychology] 1991, 12, 1–25.
- Jain A, Schmidt T, Johnson D et al. Cardiovascular Reactivity in the Laboratory and in the Field: Comparing Different Methods to Assess Reactivity in Real Life. J Psychophysiol 1994, 8, S44.
- Bassan, L. Über die Notwendigkeit einer Übereinstimmung zwischen der prinzipiellen und technischen Methodik bei der arbeitsphysiologischen Forschung [On the Necessity of Agreement between the Principle and Technical Methodology in Occupational Physiological Research]. Savremena Medizina 1955, 1, 77–85. [Google Scholar]
- Rosenblat VV. Verwendung der Radiotelemetrie in der Arbeits- und Sportphysiologie und einige Schlußfolgerungen aus der Arbeit der Sverdlovsker biotelemetrischen Gruppe [Use of Radiotelemetry in Work and Sport Physiology and Some Conclusions from the Work of the Sverdlovsk Biotelemetric Group]. In: Die Radiotelemetrie in der Physiologie und Medizin [Radiotelemetry in Physiology and Medicine]. Sverdlovsk 1963, 14–23.
- Bassan L. Forderungen des Physiologen und Arztes an die Biotelemetrie [Demands of Physiologist and Physician to Biotelemetry]. Z ges Hyg 1966; 12: 755.
- Fahrenberg J, Myrtek M. Ambulantes Monitoring [Ambulatory Monitoring]. In: Rösler F, Hrsg. Enzyklopädie der Psychologie: Bereich Psychophysiologie [Encyclopedia of Psychology: Section Psychophysiology] Band 1. Göttingen: Hogrefe; ISBN 3801705544, 1994.
- Thomas, O.; E Shipman, K.; Day, K.; Thomas, M.; Martin, U.; Dasgupta, I. Prevalence and determinants of white coat effect in a large UK hypertension clinic population. J. Hum. Hypertens. 2016, 30, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Johnston, D.W.; Anastasiades, P. The relationship between heart rate and mood in real life. J. Psychosom. Res. 1990, 34, 21–27. [Google Scholar] [CrossRef]
- Hocking Schuler JL, O‘Brien WH. Cardiovascular Recovery from Stress and Hypertension Risk Factors: A Meta-Analytic Review. Psychophysiology 1997; 34: 649−659.
- Deter HC, Blecher A. First Results of a Psychophysiological Comparative Study of Patients with Essential Hypertension and Normal Subjects in a Psychoanalytic Interview. 12th World Congress of Psychosomatic Medicine 1993, Bern.
- Sokolov M, Werdegar D, Perloff DB, Cowan RM, Bienenstuhl H. Preliminary Studies Relating Portably Recorded Blood Pressure to Daily Life Events in Patients with Essential Hypertension. In: Koster M, Musaph H, Visser P, eds. Psychosomatics in Essential Hypertension. Basel: Karger; 1970: 164−189.
- Rumo, M.; Amft, O.; Tröster, G.; Mäder, U. A stepwise validation of a wearable system for estimating energy expenditure in field-based research. Physiol. Meas. 2011, 32, 1983–2001. [Google Scholar] [CrossRef]
- Moran, D.; Shapiro, Y.; Epstein, Y.; Burstein, R.; Stroschein, L.; Pandolf, K.B. Validation and adjustment of the mathematical prediction model for human rectal temperature responses to outdoor environmental conditions. Ergonomics 1995, 38, 1011–1018. [Google Scholar] [CrossRef]
- Fahrenberg, J.; Foerster, F.; Schneider, H.-J.; Müller, W.; Myrtek, M. Predictability of Individual Differences in Activation Processes in a Field Setting Based on Laboratory Measures. Psychophysiology 1986, 23, 323–333. [Google Scholar] [CrossRef]
- Templer, KJ. Blutdruck, Verhalten und Persönlichkeit [Blood Pressure, Behavior and Personality]. Huber; 1993.
- Shapiro, D.; Jamner, L.D.; Goldstein, I.B. Ambulatory stress psychophysiology: the study of “compensatory and defensive counterforces” and conflict in a natural setting. Psychosom. Med. 1993, 55, 309–323. [Google Scholar] [CrossRef]
- Kirsch KA, Gunga HC. Extreme Umwelten: Leben und Mobilität in Kälte [Extreme Environments: Life and Mobility in Cold]. Flug u Reisemed 1999; 6: 36−38.
- Olsen, C.H.; Ottesen, J.T.; Smith, R.C.; Olufsen, M.S. Parameter subset selection techniques for problems in mathematical biology. Biol. Cybern. 2019, 113, 121–138. [Google Scholar] [CrossRef] [PubMed]
- Pernin, CG, Axelband E, Drezner JA, Dille BB, Gordon IV J, Held B, McMahon KS, Perry WL, Rizzi C, Shah AR, Wilson PA, Sollinger JM, Lessons from the Army's Future Combat Systems Program. Santa Monica, CA: RAND Corporation, 2012.
- U.S. Army. Researchers Test Warfighter Physiological Statuts Monitor. July 26, 2007. Available online: www.army.mil/ article/4157/researchers-test-warfighter-physiological-status-monitor/ (accessed on 20th May 2023).
- Hoyt, R.W.; Reifman, J.; Coster, T.S.; Buller, M.J. Combat medical informatics: present and future. Proceedings. AMIA Symp. 2002, 335–339. [Google Scholar]
- Cyber Security & Information Systems Information Analysis Center. The DoD Cybersecurity Policy Chart. July 23, 2019. Available online: http://iac.dtic.mil/csiac/ia_policychart.html (accessed on 20th May 2023).
- European Defence Agency. Soldier Modernization Harmonization. 2012-11-22. Available online: www.eda.europa.eu/docs/ default-source/news/biosensors.pdf (accessed on 20 May 2023).
- Ley, S. Infanterist der Zukunft – Erweitertes System: Die Kampfausstattung auf dem Weg zur Realisierung [Infantryman of the Future - Advanced System: Combat Equipment on the Way to Realization]. Strategie und Technik [Strategy and Technology]. 2010: 18–23.
- Gesetz über die Rechtsstellung der Soldaten (Soldatengesetz - SG) [Law on the Legal Status of Soldiers (Soldiers Act)], zuletzt geändert am [last amended on] 20. 08. 2021.
- Weber T, Wickenhöfer R, Lülsdorf P, et al. Telemedizin in der Bundeswehr [Telemedicine in the Bundeswehr]. Wehrmedizinische Monatsschrift [Monthly journal of military medicine] 2000, 3, 64–69.
- Seidel, M. Telemedizin bei der Bundeswehr: Einsatz zwischen Bonn und Koblenz [Telemedicine in the German Armed Forces: Deployment between Bonn and Koblenz]. Dtsch Ärztebl 1997; 94: A-2383/B-2017/ C-1912.
- Thomas, G. Stressed out? May 29, 2015. Available online: www. airlineratings.com/news.php?id=502 (accessed on 20 May 2023).
- Schumm, J.A.; Monson, C.M.; O'Farrell, T.J.; Gustin, N.G.; Chard, K.M. Couple Treatment for Alcohol Use Disorder and Posttraumatic Stress Disorder: Pilot Results From U.S. Military Veterans and Their Partners. J. Trauma. Stress 2015, 28, 247–252. [Google Scholar] [CrossRef]
- Leino, T.K.; Leppäluoto, J.; Ruokonen, A.; Kuronen, P. Neuroendocrine responses and psychomotor test results in subjects participating in military pilot selection. Aviat. Space, Environ. Med. 1999, 70, 571–576. [Google Scholar]
- Herbison, C.E.; Henley, D.; Marsh, J.; Atkinson, H.; Newnham, J.P.; Matthews, S.G.; Lye, S.J.; Pennell, C.E. Characterization and novel analyses of acute stress response patterns in a population-based cohort of young adults: influence of gender, smoking, and BMI. Stress 2016, 19, 139–150. [Google Scholar] [CrossRef]
- Tomei, F.; De Sio, S.; Tomao, E.; Anzelmo, V.; Baccolo, T.P.; Ciarrocca, M.; Cherubini, E.; Valentini, V.; Capozzella, A.; Rosati, M.V. Occupational exposure to noise and hypertension in pilots. Int. J. Environ. Heal. Res. 2005, 15, 99–106. [Google Scholar] [CrossRef]
- Wang, J.; Lin, P.-C.; Li, S.-C. Measuring the ability of military aircrews to adapt to perceived stressors when undergoing centrifuge training. J. Appl. Meas. 2014, 15, 200–212. [Google Scholar] [PubMed]
- Truszczynski, O.; Wojtkowiak, M.; Lewkowicz, R.; Biernacki, M.P.; Kowalczuk, K. Reaction Time in Pilots at Sustained Acceleration of +4.5 Gz. Aviat. Space, Environ. Med. 2013, 84, 845–849. [Google Scholar] [CrossRef] [PubMed]
- Simonov, P.V.; Frolov, M.V.; A Ivanov, E. Psychophysiological monitoring of operator's emotional stress in aviation and astronautics. Aviat. Space, Environ. Med. 1980, 51, 46–49. [Google Scholar] [PubMed]
- Sekiguchi, C.; Handa, Y.; Gotoh, M.; Kurihara, Y.; Nagasawa, A.; Kuroda, I. Evaluation method of mental workload under flight conditions. Aviat. Space, Environ. Med. 1978, 49, 920–925. [Google Scholar] [PubMed]
- Die Leistungsgrenzen des Menschen beim Tragen von Atemschutz und Schutzanzug [Human Performance Limits when Wearing Respiratory Protection and Protective Suits]. Arbeitsmedizin Sozialmedizin Präventivmedizin [Occupational Medicine Social Medicine Preventive Medicine]. 1985, 20, 173–176.
- Internationale Nachrichtenagentur [International News Agency] Rossiya Segodnya. Pentagon kürzt Drohnenflüge wegen Piloten-Stress [Pentagon Cuts Drone Flights because of Pilot Stress]. 17.06.2015. Available online: http://de.sputniknews.com/militar/ 20150617/302795904.html (accessed on 20 May 2023).
- Werner, A.; Kreutzmann, U.; Glowka, S.; Schinkel, C. The New Quality of Aviation Unmanned Aerial Vehicles (UAV) Prevent Psychological Stress of Military Drone Operators. Clin. Med. Res. 2020, 9, 25–30. [Google Scholar] [CrossRef]
- Deutsche Luftwaffe. Konzept für Human Performance Enhancement (HPE) im fliegerischen Dienst der Bundeswehr [German Air Force. Concept for Human Performance Enhancement (HPE) in the Flying Service of the Bundeswehr.]. 18September 2012.
- Litovchenko VV, Malinin ID, Mnatsikan’ian AZ. [Operative Medical Control of the Status of the Pilot in Flight]. Voen Med Zh 1981: 71–73.
- Fritze H, Kollande G, Mocker R. Die Komplexanalyse – eine Methodik zur ergonomischen Untersuchung der fliegerischen Tätigkeit in der Militärluftfahrt [The Complex Analysis - a Methodology for Ergonomic Examination of Flying Activities in Military Aviation [Biotelemetry Device for Aeromedical Examinations]. Zeitschrift für Militärmedizin [Journal of Military Medicine]. 1974, 5, 339–343.
- Otto K. Entwicklung einer 1/3-Telemetrieanlage für die drahtlose Übertragung der Herzfrequenz, der Atemfrequenz und der Bewegungsfrequenz von freibeweglichen Probanden. Kurzdokumentation [Development of a 1/3 Telemetry Device for Wireless Transmission of Heart Rate, Respiratory Rate, and Exercise Rate of Free-Moving Subjects. Brief Documentation], TMA 74.1/3, Vertrag Nr.: FE/68- 71/40 434, Berlin, 1971.
- Kessel R, Lang E, Denkl P. [Stress and Electrocardiogram. Telemetric Investigations during a Stunt Flight Program (Telemetric Circulatory Observations in Jet Pilots. In: Graul EH. Current Problems in Aerospace Medicine]. MMW - Münch Med Wochenschr. 1976, 118, 1001–1006.
- Pircher, Hardmeier. Telemetrische Kreislaufbeobachtungen bei Jetpiloten [Telemetric Circulatory Observations in Jet Pilots]. In: Graul EH. Aktuelle Probleme der Luft- und Raumfahrtmedizin [Current Problems in Aerospace Medicine]. Gießen: Eli Lilly GmbH; 1967: 73.
- Rice, G.M.; VanBrunt, T.B.; Snider, D.H.; Hoyt, R.E. Wearable Accelerometers in High Performance Jet Aircraft. Aerosp. Med. Hum. Perform. 2016, 87, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.H.; Marko, A.; Kissen, A.T.; McGuire, D.W. A new, miniaturized, multichannel, personal radiotelemetry system. J. Appl. Physiol. 1968, 24, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Calton, B.; Abedini, N.; Fratkin, M. Telemedicine in the Time of Coronavirus. J. Pain Symptom Manag. 2020, 60, e12–e14. [Google Scholar] [CrossRef]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-Provider Clinical Engagement During the COVID-19 Pandemic and Beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef]
- Vevere, A.; Oks, A.; Katashev, A.; Terlecka, G.; Saiva, L.; Jansons, M.; Dyachenko, N.; Seglina, P. Smart textile device for shooter’s fingers movement monitoring. Technol. Heal. Care 2022, 30, 217–229. [Google Scholar] [CrossRef]
- van Doornen LJ, van Blokland RW. The Relationship between Cardiovascular and Catecholamine Reactions to Laboratory and Real-Life Stress. Psychophysiology 1992, 29, 173–181.
- Ardenne, M. Der verschluckbare Intestinalsender – ein Beispiel für den Einsatz moderner Technik in der Medizin [The Swallowable Intestinal Transmitter - an Example of the Use of Modern Technology in Medicine]. Die Technik [The Technology] 1961; 12: 9.
- O'Brien, C.; Hoyt, R.W.; Buller, M.J.; Castellani, J.W.; Young, A.J. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med. Sci. Sports Exerc. 1998, 30, 468–472. [Google Scholar] [CrossRef]
- Hoskins, S.; Sobering, T.; Andresen, D.; Warren, S. Near-field wireless magnetic link for an ingestible cattle health monitoring pill. Conf Proc IEEE Eng Med Biol Soc 2009, 2009, 5401–5404. [Google Scholar] [CrossRef]
- Tolles, WE. Short Range Telemetry of Ingested or Implanted Sensors. In: Slater LE. Bio-Telemetry, Pergamon Press; 1963, 330–340.
- Tortora, G.; Fontana, R.; Argiolas, S.; Vatteroni, M.; Dario, P.; Trivella, M.G. A dynamic control algorithm based on physiological parameters and wearable interfaces for adaptive ventricular assist devices. Conf Proc IEEE Eng Med Biol Soc 2015, 2015, 4954–4957. [Google Scholar] [CrossRef]
- Scheit L, Werner A. „Wearable Sensors“ zur Unterstützung eines medizinischen Monitorings für militärische Zwecke ["Wearable Sensors" to Support Medical Monitoring for Military Purposes]. WMM. 2021, 65, 225–235.
- Goncalvas, C.; da Silva, A.F.; Gomes, J.; Simoes, R. Wearable E-Textile Technologies: A Review on Sensors, Actuators and Control Elements. Inventions 2018, 3, 14. [Google Scholar] [CrossRef]
- Sayem, A.S.M.; Haider, J. An Overview on the Development of Natural Renewable Materials for Textile Applications. In Reference Module in Materials Science and Materials Engineering; Science Direct; Elsevier: Amsterdam, The Netherlands, 201983.
- Muhammad Sayem AS, Hon Teay S, Shahariar H, Fink PL, Albarbar A. Review on Smart Electro-Clothing Systems (SeCSs). Sensors (Basel). 2020, 20, 587.
- Fernández-Caramés, T.M.; Fraga-Lamas, P. Towards The Internet of Smart Clothing: A Review on IoT Wearables and Garments for Creating Intelligent Connected E-Textiles. Electronics 2018, 7, 405. [Google Scholar] [CrossRef]
- Consumer Products Inventory. Sensatex™ SmartShirt System. Available online: www.nanotechproject.org/cpi/products/ sensatextm-smartshirt-system/ (accessed on 20 May 2023).
- Alwis, L.S.M.; Bremer, K.; Roth, B. Fiber Optic Sensors Embedded in Textile-Reinforced Concrete for Smart Structural Health Monitoring: A Review. Sensors 2021, 21, 4948. [Google Scholar] [CrossRef]
- Georgia Tech Wearable Motherboard™. Available online: www. gtwm.gatech.edu/ (accessed on 20 May 2023).
- Khundaqji, H.; Hing, W.; Furness, J.; Climstein, M. Smart Shirts for Monitoring Physiological Parameters: Scoping Review. JMIR mHealth uHealth 2020, 8, e18092. [Google Scholar] [CrossRef]
- Weber T, Lindlar M. Im Alltag der Telemedizin: Entwicklung aus der Luft- und Raumfahrtmedizin im weltweiten Einsatz [In everyday telemedicine: development from aerospace medicine in worldwide use]. DLR Nachrichten [DLR News] 2006, 113, 76–79.
- Otto, C. Telemedizin im Sanitätsdienst der Bundeswehr: Das Ziel ist ein Telematikverbund [Telemedicine in the Bundeswehr Medical Service: The goal is a Telematics Network]. Dtsch Ärztebl 2003; 100: A 99–102 / B-90 / C-88.
- Padeken D, Weber TP, Wilke D, et al. Telemedizin im Sanitätsdienst der Bundeswehr. Conference: Präsentation vor dem Inspekteur der Bundeswehr [Telemedicine in the Medical Service of the German Armed Forces. Conference: Presentation to the Chief of Staff of the German Armed Forces] DLR, Köln, 20. Januar 1999.
- Spaite, D.W.; Valenzuela, T.D.; Meislin, H.W. Physician In-field Observation of Prehospital Advanced Life Support Personnel: A Statewide Evaluation. Prehospital Disaster Med. 1993, 8, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Isakadze N, Martin SS. How useful is the smartwatch ECG? Trends Cardiovasc Med. 2020, 30, 442–448.
- Harst, L.; Lantzsch, H.; Scheibe, M. Theories Predicting End-User Acceptance of Telemedicine Use: Systematic Review. J. Med Internet Res. 2019, 21, e13117. [Google Scholar] [CrossRef]
- Available online:. Available online: https://www.polar.com/en (accessed on 20 May 2023).
- A Tiller, W.; McCraty, R.; Atkinson, M. Cardiac coherence: a new, noninvasive measure of autonomic nervous system order. Altern. Ther. Heal. Med. 1996, 2, 52–65. [Google Scholar]
- Achmon, J.; Granek, M.; Golomb, M.; Hart, J. Behavioral treatment of essential hypertension: a comparison between cognitive therapy and biofeedback of heart rate. Psychosom. Med. 1989, 51, 152–164. [Google Scholar] [CrossRef]
- Available online:. Available online: https://healthmanagement.org/products/view/ambulatory-polysomnograph-with-eeg-vitaport-4-natus-medical-incorporated?channel=all (accessed on 20 May 2023).
- BodyMedia. SenseWear Manual. Pittsburgh: BodyMedia Inc. 2007.
- Available online: http://www.fitness-tracker24.com/sensewear/9-bodymedia (accessed on 20 May 2023).
- Weeß H-G. Diagnostische Methoden [Diagnostic Methods]. In: Stuck BA, Maurer JT, Schredl M, Weeß H-G. Praxis der Schlafmedizin [Practice of Sleep Medicine]. Heidelberg: Springer 2009; 23–78.
- O’driscoll, D.M.; Turton, A.R.; Copland, J.M.; Strauss, B.J.; Hamilton, G.S. Energy expenditure in obstructive sleep apnea: validation of a multiple physiological sensor for determination of sleep and wake. Sleep Breath. 2013, 17, 139–146. [Google Scholar] [CrossRef]
- Conradt, R.; Brandenburg, U.; Ploch, T.; Peter, J.H. [Actigraphy: methodological limits for evaluation of sleep stages and sleep structure of healthy probands]. Pneumologie 1997, 51 (Suppl. 3), 721–724. [Google Scholar]
- Available online:. Available online: https://www.equivital.com/ (accessed on 20 May 2023).
- Equivital™. Media Centre. Available online: www.equivital.co.uk/ media-center (accessed on 20 May 2023).
- Welles, A.P.; Buller, M.J.; Margolis, L.; Economos, D.; Hoyt, R.W.; Richter, M.W. Thermal-Work Strain During Marine Rifle Squad Operations in Afghanistan. Mil. Med. 2013, 178, 1141–1148. [Google Scholar] [CrossRef] [PubMed]
- Equivital™. EQ02 LifeMonitor. Available online: www.equivital. co.uk/assets/common/SEM_Data_Sheet_General_HI- DA3330-DSG-02.2_.2_.pdf (accessed on 20 May 2023).
- Available online:. Available online: https://www.zephyranywhere.com/ (accessed on 20 May 2023).
- Kim JH, Roberge R, Powell JB et al. Measurement Accuracy of Heart Rate and Respiratory Rate during Graded Exercise and Sustained Exercise in the Heat Using the Zephyr BioHarness. Int J Sports Med. 2013, 34, 497–501.
- Vitasystems GmbH. Available online: www.vitagroup.ag/de_DE/ Ueber-uns/vitasystems (accessed on 20 May 2023).
- Available online:. Available online: https://www.kie-hb.de/en/healthlab-mobphysiolab.html (accessed on 20 May 2023).
- Available online:. Available online: https://www.draeger.com/de_de/Products/Tcore-Temperature-Monitoring-System (accessed on 20 May 2023).
- Kimberger, O.; Saager, L.; Egan, C.; Sanchez, I.P.; Dizili, S.; Koch, J.; Kurz, A. The accuracy of a disposable noninvasive core thermometer. Can. J. Anaesth. 2013, 60, 1190–1196. [Google Scholar] [CrossRef] [PubMed]
- Gunga, H.-C.; Sandsund, M.; Reinertsen, R.E.; Sattler, F.; Koch, J. A non-invasive device to continuously determine heat strain in humans. J. Therm. Biol. 2008, 33, 297–307. [Google Scholar] [CrossRef]
- Masè, M.; Werner, A.; Putzer, G.; Avancini, G.; Falla, M.; Brugger, H.; Micarelli, A.; Strapazzon, G. Low Ambient Temperature Exposition Impairs the Accuracy of a Non-invasive Heat-Flux Thermometer. Front. Physiol. 2022, 13, 830059. [Google Scholar] [CrossRef]
- Gunga, H.-C.; Werner, A.; Stahn, A.; Steinach, M.; Schlabs, T.; Koralewski, E.; Kunz, D.; Belavý, D.; Felsenberg, D.; Sattler, F.; et al. The Double Sensor—A non-invasive device to continuously monitor core temperature in humans on earth and in space. Respir. Physiol. Neurobiol. 2009, 169 (Suppl. 1), S63–S68. [Google Scholar] [CrossRef]
- Tiedemann, J. Physiologische Veränderungen des menschlichen Organismus während einer fünfzehnmonatigen Überwinterung in der Antarktis [Physiological Changes in Human Organism during a Fifteen-Month Hibernation in Antarctica]. Doctoral Thesis 2012. Refubium – Repositorium der Freien Universität Berlin [Refubium - Repository of the Free University Berlin].
- Steinach, M. Physiologische Langzeitveränderungen bei Überwintern in der Antarktis unter besonderer Berücksichtigung von Aktivitätsparametern [Long-Term Physiological Changes during Hibernation in the Antarctic with Special Consideration of Activity Parameters]. Doctoral Thesis 2013. Institut für Physiologie, Zentrum für Weltraummedizin Berlin, Bibliothek der [Institute of Physiology, Center for Space Medicine Berlin and extreme Environments, Library of the] Charité.
- Michael, S. Human Performance von Fallschirmspringern in großen Höhen mit den Sprungverfahren High Altitude High Opening (HaHo) und High Altitude Low Opening (HaLo) in der realen Umgebung im Vergleich zur Ausbildung in der Höhen-Klima-Simulationsanlage (HKS). [Human Performance of Skydivers at High Altitudes using the High Altitude High Opening (HaHo) and High Altitude Low Opening (HaLo) Jumping Procedures in the Real Environment compared to Training in the High-Altitude Climate Simulation Chamber (HAC)]. Doctoral Thesis 2020. Institut für Physiologie, Zentrum für Weltraummedizin und extreme Umwelten, Berlin, [Institute of Physiology, Center for Space Medicine and extreme Environments Berlin, Library of the] Bibliothek der Charité.
- Werner A, Lang V, Brix B et al. Heat Exposure of Jet Pilots during Air Traffic. 82nd Annual Scientific and Human Performance Meeting, AsMA, Anchorage, USA, 2011.
- Werner, A. Mars500 Project – Circadian Rhythm and Body Core Temperature in Humans during Long-Term Isolation and Confinement. Flight Surgeon Conference USAF, Ramstein, 2013.
- Stahn A, Mendt S, Steinach M, Opatz O, Werner A, Kunz D, Belavy DL, Felsenberg D, Sattler F, Koch J, Gunga HC. The Role of Exercise in Synchronizing the Circadian Timing System during 60 Days of Bed-Rest Using Rectal Recordings and a New Non-Invasive Heatflux Technology. Proceedings of the 62nd International Astronautical Congress 2011.
- Stahn, A.C.; Werner, A.; Opatz, O.; Maggioni, M.A.; Steinach, M.; von Ahlefeld, V.W.; Moore, A.; Crucian, B.E.; Smith, S.M.; Zwart, S.R.; et al. Increased core body temperature in astronauts during long-duration space missions. Sci. Rep. 2017, 7, 16180. [Google Scholar] [CrossRef]
- Scheuermann C, Binderberger T, von Frankenberg N, Werner A. Digital twin: a machine learning approach to predict individual stress levels in extreme environments. , Sep 2020. Pages 657–664.
- Cesarelli, G.; Donisi, L.; Coccia, A.; Amitrano, F.; D’addio, G.; Ricciardi, C. The E-Textile for Biomedical Applications: A Systematic Review of Literature. Diagnostics 2021, 11, 2263. [Google Scholar] [CrossRef]
- Dolez, P.I. Energy Harvesting Materials and Structures for Smart Textile Applications: Recent Progress and Path Forward. Sensors 2021, 21, 6297. [Google Scholar] [CrossRef] [PubMed]
- Alwis, L.S.M.; Bremer, K.; Roth, B. Fiber Optic Sensors Embedded in Textile-Reinforced Concrete for Smart Structural Health Monitoring: A Review. Sensors 2021, 21, 4948. [Google Scholar] [CrossRef] [PubMed]
- Stylios, GK. Novel Smart Textiles. Materials 2020, 13, 950. [Google Scholar] [CrossRef] [PubMed]
- Marsch, L.A. Digital health data-driven approaches to understand human behavior. Neuropsychopharmacology 2020, 46, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.; Anderson, M.; Albala, S.; Casadei, B.; Franklin, B.D.; Richards, M.; Taylor, D.; Tibble, H.; Mossialos, E. Health information technology and digital innovation for national learning health and care systems. Lancet Digit. Heal. 2021, 3, e383–e396. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




