1. Introduction
Research on microvascular complications of diabetes mellitus (DM), including diabetic retinopathy (DR) and cataracts (CA), is currently shifting its focus towards early detection and therapy
[1,2]. This is a departure from what is now regarded as the standard method, which primarily focuses on late-phase treatment. These strategies are painful, with limited curative ability for DR, and significant economic burden for CA. Moreover, CA surgery, despite being a customary practice, was found to be associated with an increased risk of DR development in diabetic patients
[3]. The transition from advanced-stage management to early-stage prevention is being made possible, firstly by advancements in screening
[4,5].
Numerous studies have emphasized the pressing issue of timely detection at subclinical stages, defined by the presence of morphophysiological alterations with limited characteristic symptoms. One study on diabetic patients
[2] described peripheral spoke-like lesions on the eye lens through slit-lamp examination, typically associated with cortical CA (a type often linked to diabetes). These lesions only became symptomatic with accumulation in the center of the lens, leading to impaired vision, correctable by surgery. Likewise, subclinical abnormalities in DR resulting from early microvascular and neuronal degeneration were measured using spectral domain optical coherence tomography and optical coherence tomography angiography
[6].
Thus, the impact of subclinical diagnosis by various screening methods could be increased by subsequent treatment. At present, lifestyle changes are primarily recommended, specifically blood glucose management. A metanalysis study
[7] found that, despite being guideline advocated, strict glycemic control could not be correlated to significant benefits against microvascular complications. To address this research gap, recent studies have postulated the use of plant-derived antioxidants as effective remedies for diabetes-induced complications. This can be justified by the existing understanding of pathophysiology. According to Brownlee’s hypothesis
[8], there is a singular common mechanism that causes both diabetes and its complications – increased production of reactive oxygen species (ROS). This model states that the typical diabetes-linked reduced amount of insulin and/or its effects trigger a systematic chain of events. Firstly, the ensuing hyperglycemia stimulates an increased flux through the major pathways responsible for diabetes damage – polyol, hexosamine, protein kinase C (PKC), advanced glycation end-product formation (AGEs) and activation of Poly(ADP-ribose) polymerase. Secondly, vulnerable glial cells, such as astrocytes, Müller cells and microglia, enter a state of oxidative stress, which is coupled with an increase in the secretion of proinflammatory cytokines, TNF-α, IL-1β, IL-6
[9]. Furthermore, it has been proposed
[10] that the retinal glia hosts a resident renin-angiotensin system (RAS), which produces local Angiotensin II (Ang II). Intraocular levels of Ang II have been shown to rise in diabetes and were associated with an increased inflammatory and oxidative stress response. Ang II has also been found to stimulate the retinal microglia through the Angiotensin type 1 receptor (AT1), leading to a decrease in retinal blood flow, independent of systemic changes
[11]. Similarly, RAS modulators have demonstrated anticataract properties, possibly by inhibiting the AT1-mediated production of ROS
[12].
A variety of antioxidant plant compounds have been suggested as potential treatments for diabetic ocular complications, each presenting individual strengths and weaknesses. Among these compounds, Rutin, a flavonol from the flavonoid subclass of dietary polyphenols, shows promising properties for managing DM. Rutin is known for its antioxidant and anti-inflammatory abilities
[13]. Additionally, a recent study has demonstrated that Rutin can act as an inhibitor of AT1 receptors
[14]. Moreover, it can lower glycemia by inhibiting carbohydrate absorption and gluconeogenesis, and it can promote insulin secretion and the cellular uptake of glucose
[13]. This compound has also been shown to decrease serum triglycerides, LDL, and VLDL, with high HDL levels in experimental models
[13].
The main disadvantage of Rutin is its low bioavailability, attributed to its highly hydrophilic nature, which hinders diffusion through cell membranes. After ingestion, Rutin is hydroxylated to quercetin, a compound quickly metabolized in the body, resulting in limited bioavailability
[15].
Delivering therapeutic agents to the eye poses an additional challenge. As such, barriers exist for both topical administration, the tear layer and corneal epithelium with tight junctions, and systemic delivery, including the blood-aqueous layer and blood-retina barrier
[16].
Considering the systemic nature of diabetes, and Rutin's multiorgan action, oral administration, together with a nanotechnology-based formulation, were proposed to overcome delivery and bioavailability issues. Nanoparticles are accepted as efficient drug delivery systems for both lens and retinal pathologies. Gold nanoparticles (AuNPs) have been used in previous medical studies due to their ease of functionalization with various active molecules
[17]. A recent study
[18] demonstrated significant uptake of AuNPs functionalized with resveratrol, a stilbene from the subclass of dietary polyphenols, in ocular lens epithelial cells, in both
in vitro and
in vivo models of CA, with no dose dependent toxicity. Similarly, improvements were demonstrated in a Wistar rat model of diabetic retinopathy when treated with AuNPs phytoreduced with resveratrol
[19]. Other authors
[20] revealed increased
in vitro glucose uptake by adipocytes using AuNPs prepared with vicenin-2, a compound from the same flavonoid subclass as Rutin.
In the present study, we hypothesized that the administration of gold nanoparticles conjugated with Rutin (AuNPsR) in an early rat model of DR and CA may present beneficial therapeutic effects. The effects were evaluated by oxidative stress investigation in serum and ocular tissues, and inflammatory cytokines levels in eye homogenates. Eye fundus assessment of retinal arterioles, transmission electron microscopy (TEM) of eye lenses, and histopathological examination of retinas were also performed.
2. Materials and Methods
2.1. Reagents
Tetrachloroauric acid trihydrate, 2-thiobarbituric acid, Bradford reagent, sodium hydroxide, Folin-Ciocalteu reagent were obtained from Merck (Darmstadt, Germany). O-phthalaldehyde was purchased from Sigma–Aldrich (Taufkirchen, Germany). IL1β, TNFα and IL6 were measured in eye homogenates by ELISA assays using the Elabscience ELISA kits (Houston, Texas, USA), according to the producer instructions. Results were expressed as pg/mg protein.
2.2. Gold Nanoparticles Synthesis and Characterization
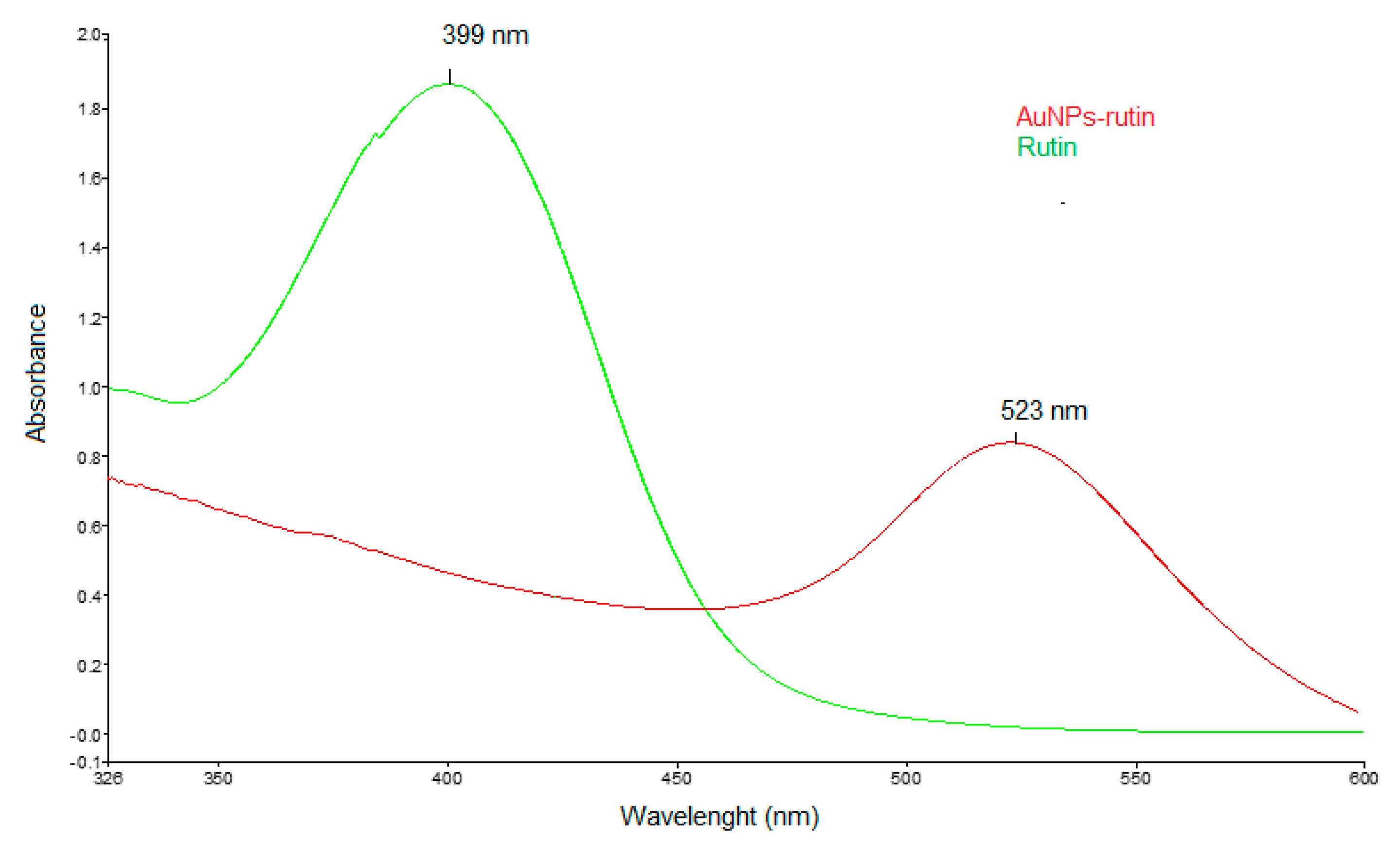
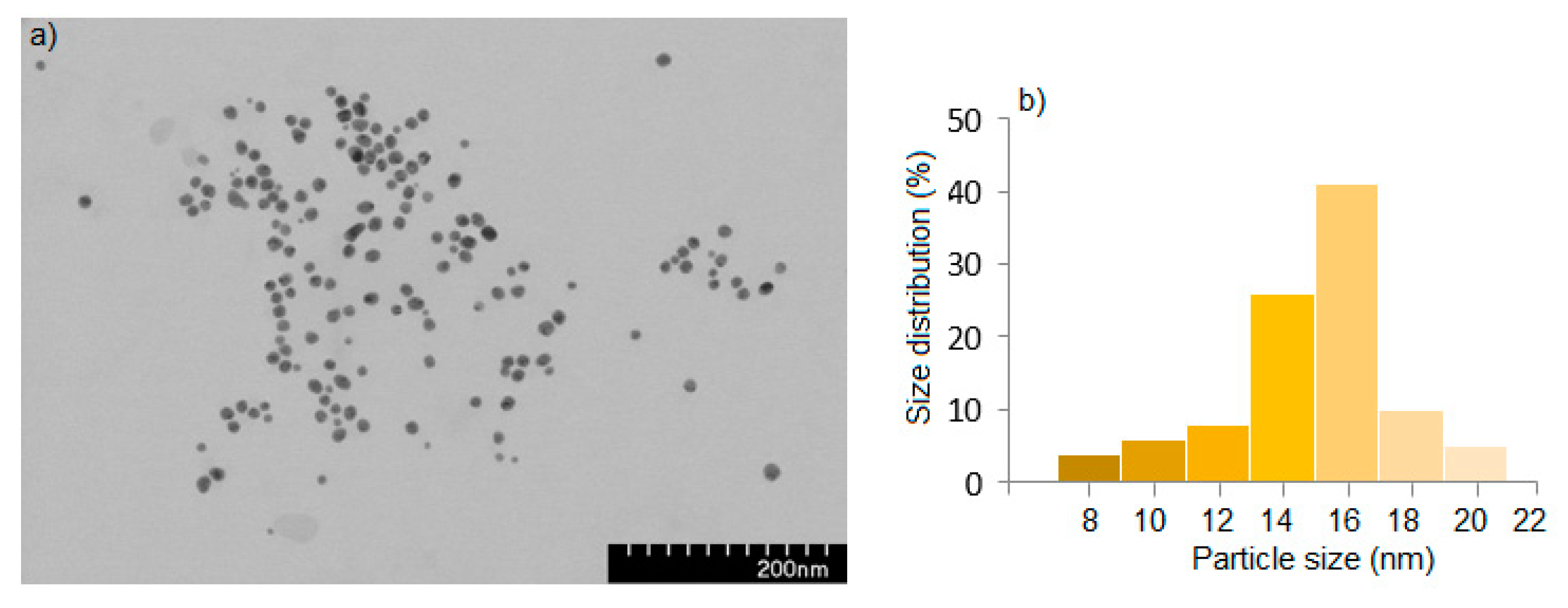
The synthesis of AuNPsR was carried out as follows: to a mixture of 61 mg Rutin and 100 mL distilled water, 2 M aqueous solution of NaOH was added dropwise (approximately 4 mL), until Rutin was totally dissolved, and the color of the obtained solution turned yellow-orange. One hundred mL of 1mM tetra chloroauric solution was added over the Rutin solution and the mixture was stirred at room temperature for one hour. The obtained AuNPsR were purified by centrifugation at 10,000 rpm followed by washing of the resulted pellet twice with distilled water. The pellet was resuspended and used for biological determination. The obtained AuNPsR were characterized using classical methods. UV-Vis spectroscopy was applied to follow the progress of the reaction; to this end, a Perkin Elmer Lambda 25 spectrometer was used. The absorbance of gold colloidal solution was scanned between 300 and 800 nm, in one cm quartz cuvette, distilled water being used as blank. Transmission electron microscopy (TEM), by using a Hitachi H-7650 transmission microscope, made possible the morphological characterization of AuNPsR. The ImageJ 1.53t [
21] software was used to determine the mean size of the synthesized AuNPsR, from at least 100 AuNPsR. The zeta potential and hydrodynamic diameter of AuNPsR were assessed using a Malvern Zetasizer Nanoseries compact scattering spectrometer.
2.3. Experimental design
The study adhered to the ethical standards regarding animal research and received approval from the University Ethical Board and the Veterinary and Food Safety Direction (project authorization no. 294/09.03.2022). Fifty-five Wistar albino female rats, three months old, weighing 300 ± 10 g, were provided by the Experimental Animal Facility of Iuliu Hatieganu University of Medicine and Pharmacy in Cluj-Napoca, Romania. Rats were housed in cages under standard environmental conditions, with a temperature of 21 ± 2◦C, a relative humidity of 55% ± 5, and a 12-hour light/12-hour dark cycle. Conventional food and water were provided ad libitum.
The experiment consisted of three stages: induction of diabetes, development of incipient ocular complications, and administration of treatment.
Prior to the induction of DM, blood samples were drawn to assess glycemic levels, which were found to be within the normal range for all animals (average of 110 ± 10 mg/dL). To induce DM, two doses of streptozotocin (STZ) were administered by intraperitoneal injection: 30 mg/kg STZ on day zero and 30 mg/kg STZ after 72 hours. Animals were included in the study if their blood glucose levels exceeded 250 mg/dL on the seventh days after the last dose of STZ. The average value obtained was 300 ± 20 mg/dL.
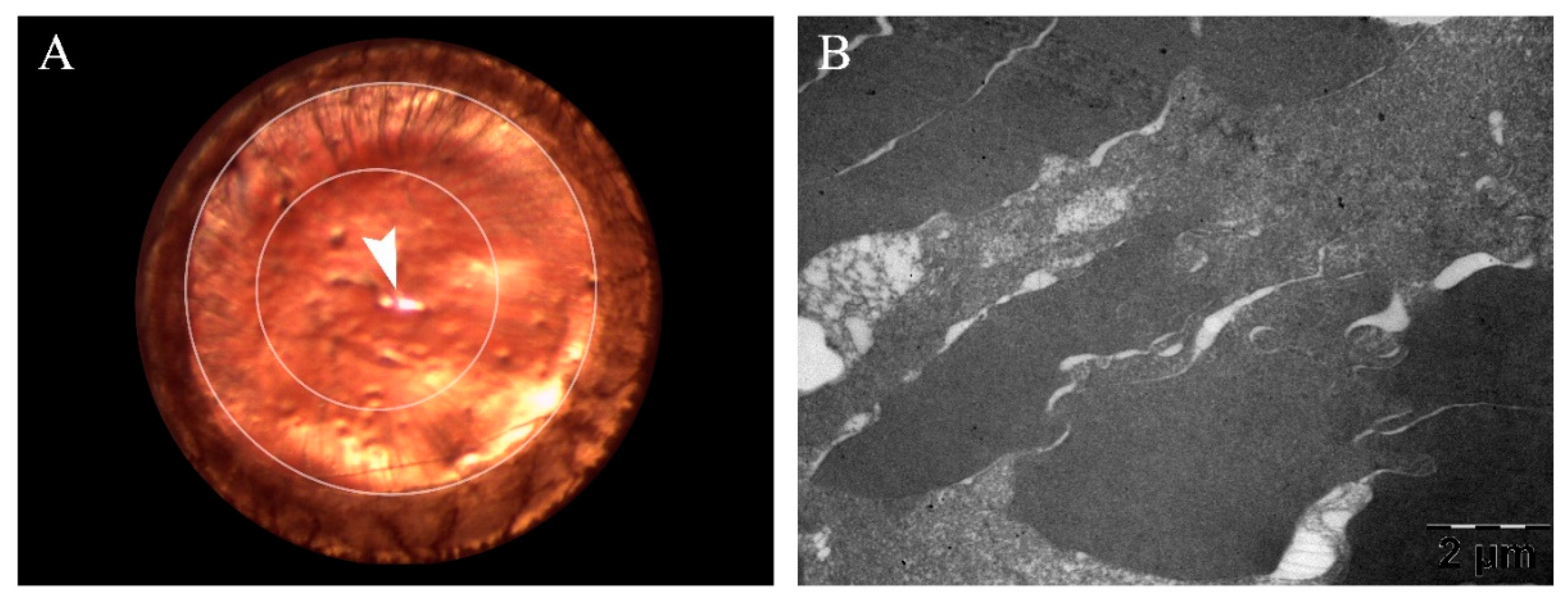
In the following six weeks after induction of DM, weekly anterior segment examination and funduscopy were performed to assess the incipient development of CA and DR. On the last day of the sixth week, animals exhibited the first signs of CA formation, including swollen fibers and subcapsular opacities, according to a previously described grading system of lens opacity [
22]. In order to confirm CA development, TEM morphological evaluation was performed for ten randomly selected diabetic animals. A side-by-side view of the anterior segment photography and the corresponding TEM micrograph is presented in
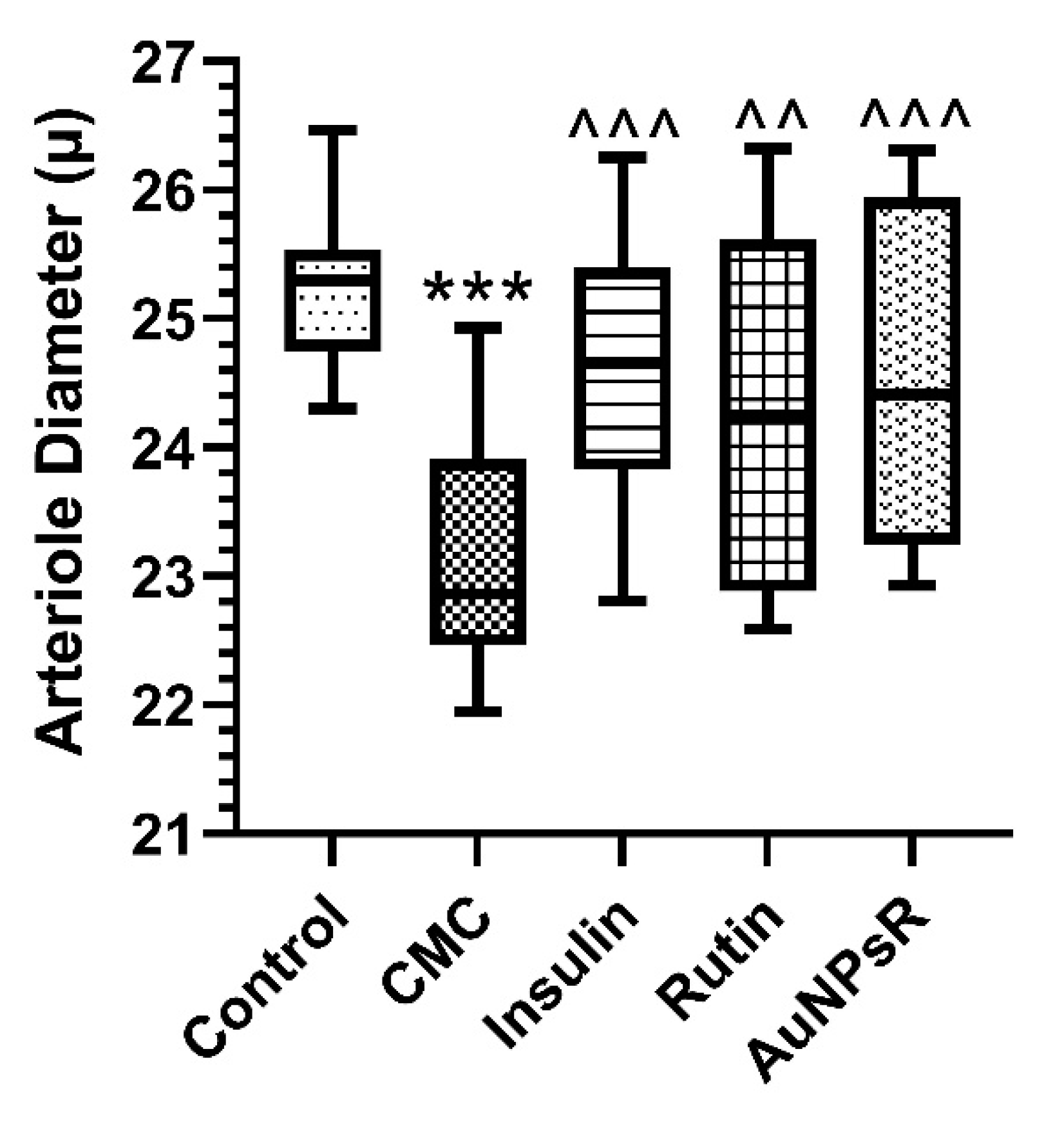
Figure 1. Subsequently, early DR was detected and defined through variations in retinal arteriole diameter.
Thirty-six animals with signs of incipient diabetic ocular complications were included in the study and were randomly divided in the following four treatment groups (nine animals/group): CMC group (0.6 mL/day of 1% carboxymethylcellulose vehicle solution), Rutin group (10 mg/kg/day), Insulin group (0.1 mg/kg of insulin), and AuNPsR group (0.6 mL/day of AuNPsR). A fifth group with nine healthy age-matched animals, without DM and treated only with CMC, was considered the Control group. Treatments were administered daily for seven days, via oral gavage, between 7 a.m. and 8 a.m., except for insulin, which was administered subcutaneously.
After seven days of treatment, animals were completely sedated in order to perform funduscopy and image collection. Then, from five animals/group, blood was used to assess oxidative stress levels, whilst the eyes were collected for biochemical analysis. Additionally, eyes from four animals/group were used for histological examination and TEM. All specimens were euthanized by overdose as to not damage the eye from the increased pressure.
All eyes were collected using a technique specifically developed to maintain structural integrity. The soft tissues overlaying the skull were removed. Then, an incision was made along the frontonasal suture, and the dorsal part of the skull was gently lifted. This exposed the ocular globes and their respective optic nerves, which were easily enucleated and further processed.
2.4. Funduscopy Examination
Fundus photographs were captured using a Leica Microsystems M320 T Surgical Training Microscope. Pupils were dilated with a drop of 1% tropicamide and the vibrissae were trimmed, to prevent them from obstructing the photographs. During the procedure, eyelids were completely retracted and a mound of propylene glycol water-based viscous gel was applied to the external portion of the rodent's eye. A glass microscope slide was placed on top of the gel, and gentle pressure was exerted to flatten the cornea. The gel prevents the image from distorting and provides a practical alternative to liquid oil in this situation. The position of the specimen and the pressure applied to the glass slide were permanently adjusted to achieve the proper focus. The specimen's position and angle were altered accordingly to examine different areas of the fundus. All photographs were captured using the built-in camera of the surgical microscope.
2.5. Fundus Photography Processing and Analysis
Fundus photographs were analyzed using ImageJ version 1.53k [
21]. Firstly, arterioles were differentiated from venules based on the anatomical model described by McLenachan et al [
23]. Thus, an alternating pattern was observed, with each arteriole being situated next to a venule. Following the approach outlined by Miri et al [
24], the darker red vessels were considered as venous in nature.
To facilitate the visualization of red color variance, all photographs were imported into ImageJ, converted to the RGB format and then split into grayscale color channels. For the red channel, brighter grays indicated higher red amounts, while darker grays meant lower red amounts or no red. As a result, arterioles, associated with a bright red color due to oxygenated blood, appeared as washed-out brighter gray, while venules, associated with a dark red color due to deoxygenated blood, appeared as clearly distinguishable dark gray. This allowed successful arteriole isolation.
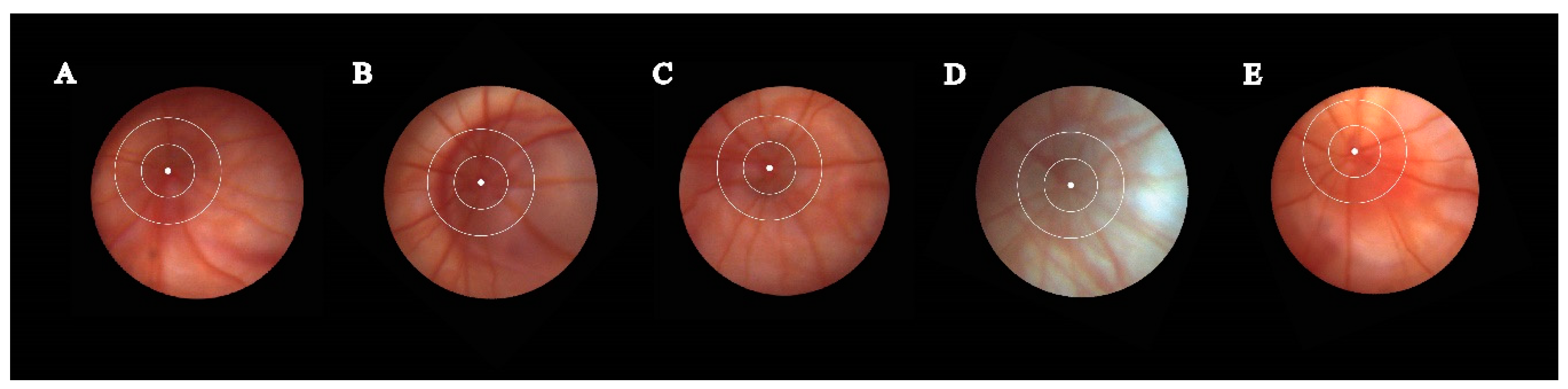
For measurements, the raw fundus photographs were used, as depicted in
Figure 2. Fundus photographs were obtained from both eyes of five randomly selected animals. For each eye, three arterioles were measured, resulting in 30 measurements for every group (three arterioles × two eyes per animal × five animals per group). The selected measurement area was within a 0.5 to 0.25 disc diameter from the edge of the funduscopy disc margin. This area was chosen to account for the curvature of the eye and to ensure measurement consistency across photographs. A centerline was drawn following the long axis of the vessel. To assess diameter, five distinct measurement lines perpendicular to the centerline were created. The width of each measurement line was calculated, and the five values were averaged.
2.6. Oxidative Stress Investigation and inflammation assessment
Oxidative stress was evaluated in serum and eye homogenates by quantification of malondialdehyde (MDA), as a marker of lipid peroxidation, using Conti’s method [
25]. Additionally, catalase (CAT) activity was measured through Pippenger’s method [
26]. Superoxide dismutase (SOD) activity was assessed through the method described by Beauchamp and Fridovich [
27]. Inflammation from eye homogenates was evaluated by ELISA tests and the results were expressed as pg/mg protein.
2.7. Retina Histopathological Examination
Extraocular tissues were excised immediately after enucleation, to ensure proper penetration of the fixative. Then, the eyes underwent a two-step fixation process. For this purpose, a 10% formaldehyde solution was utilized, at ten times the volume of the tissue being studied. For the first 24 hours, the ocular globes were submerged in the fixation solution, as a whole. Subsequently, they were briefly removed from the fixative, and sectioned in half, along the anatomical sagittal plane (with the blade placed perpendicular to the superior and inferior rectus muscles). Then, the obtained halves were fixed for a second 24-hour period, in the same solution. Through employing a preliminary fixation of the entire globe, collapse upon halving was avoided. Ultimately, samples were embedded in paraffin and sectioned at 5 μ, then stained with hematoxylin-eosin and examined using an Olympus BX43F light microscope (Olympus, Tokyo, Japan). Pictures of representative areas were captured using the microscope mounted camera (Olympus UC30 camera with the Olympus U-CMAD3 adapter).
2.8. Eye Lens Transmission Electron Microscopy
Following enucleation, eye lenses were removed as swiftly as possible. The ocular globe was held in place with toothed microsurgical forceps whilst the cornea was removed along the limbus, by gliding two surgical blades against each other and in opposing directions. After extraction, eye lenses were first fixed in a 2.7% glutaraldehyde solution in 0.1 M phosphate buffer, and then they were cut in halves. Afterward, samples were washed four times, in the same buffer. Subsequent to postfixation with 1.5% osmium tetroxide (OsO4) in 0.15 M phosphate buffer, eye lenses underwent dehydration in a series of acetone solutions of increasing concentrations (from 30%, up to 100%), infiltration and embedding in EMbed 812. Using a Diatome A382 diamond knife (Diatome, Hatfield, USA), 70-80 nm thick ultrathin sections were obtained on a Bromma 8800 ULTRATOME III (LKB, Stockholm, Sweden). These sections were then collected on 300 mesh copper grids, contrasted with uranyl acetate and lead citrate, and examined at 80kV using a JEOL JEM-100CX II transmission electron microscope (JEOL, Tokyo, Japan). Images were captured with a MegaView G3 camera, equipped with a Radius 2.1 software (both from Emsis, Münster, Germany).
2.9. Eye Lens TEM Photography Processing and Analysis
To assess opacity modifications in eye lenses using TEM micrographs, an adapted protocol based on Wirahadikesuma et al. was implemented [
28]. Micrographs were analyzed using ImageJ version 1.53k [
21].
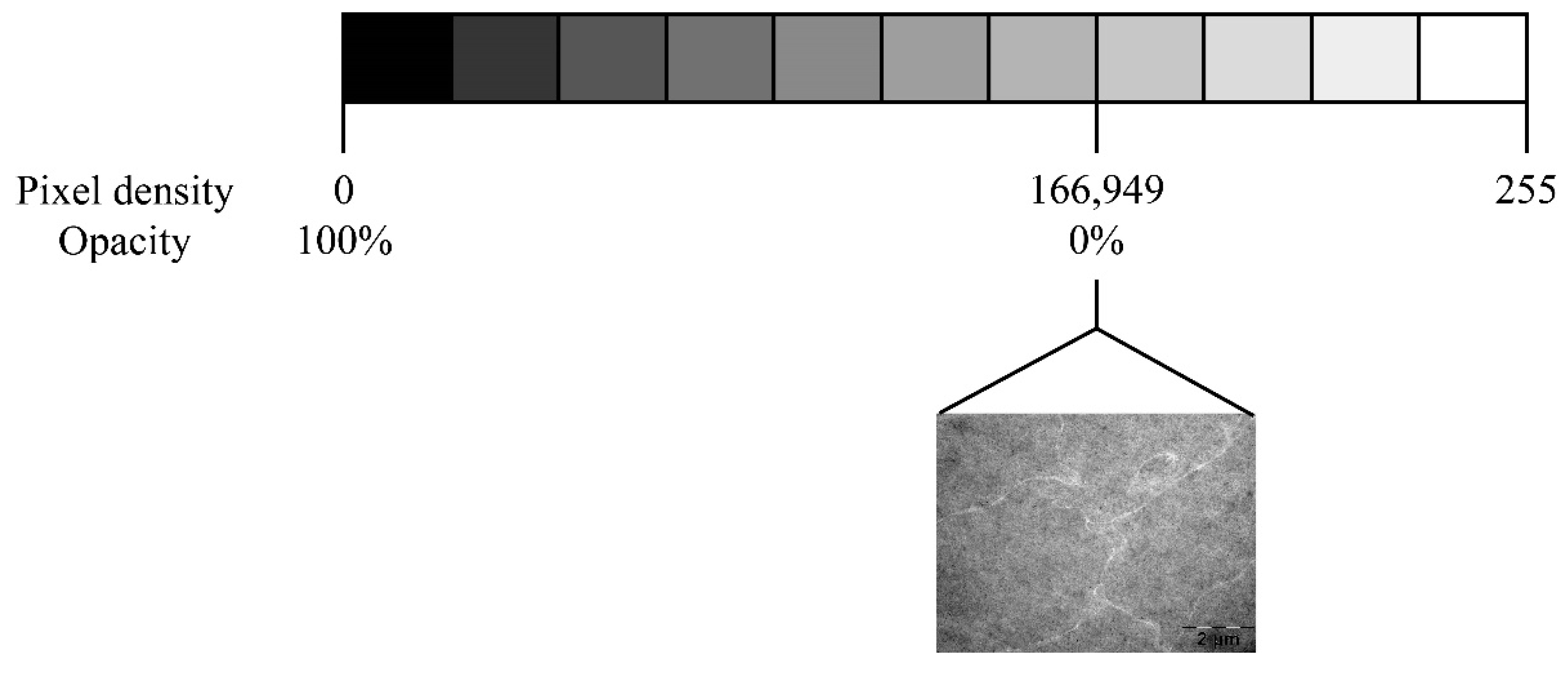
Twenty micrographs from each group were examined. For each micrograph, 20 regions of interest were measured by two blinded researchers, resulting in a total of 800 measurements for each group (20 photos per group × 20 measurements per micrograph × two independent researchers). Regions of interest were selected based on the homogeneity of lens tissue and were defined as a square area, with the calculated side length of 365 pixels, which would allow for 95% coverage of each micrograph. As the measurement unit was not significant to our outcome, the standard pixel unit was utilized.
To measure pixel density, the .tif micrographs were converted to the commonly used 8-bit integer format, yielding a possible range of pixel densities from zero to 255. Following Ansel Adam's Zone System, zero represents pure black and 255 represents pure white. Considering that the images are micrographs, where pure black corresponds to complete electron density, such as a perfect saturation of the employed dye (OsO4), zero was considered the maximum opacity achievable by our tissue. Measurements from the control group were used as a reference. Hence, the maximum pixel density obtained in the control group was considered the transparency standard, with a value of 166.949 pixels/area. To facilitate visualization of opacity measurements, the following formula was applied to convert pixel density to a percentage of opacity,
Consequently, 100% opacity would correspond to zero pixels/area (maximum opacity), and 0% opacity would correspond to 166.949 pixels/area (minimum opacity or maximum transparency achievable). This conversion is depicted in
Figure 3.
Any heterogeneity caused by CA-induced morphological modifications would be indicated by higher electron density and consequently a tendency towards increased opacity.
2.10. Statistical Analysis
Data was analyzed using GraphPad Prism version 9.0.0 for Windows, GraphPad Software, San Diego, California USA,
www.graphpad.com. All multi-group assessments were performed using the Kruskal-Wallis test for not normally distributed data. Outliers of TEM micrographs were identified using Robust regression and Outlier removal (ROUT) with Q set at the default 1%. To describe the quantitative data from arteriole diameter and eye lens opacity investigations, the minimum and maximum values, median, and interquartile range (Q1–Q3, the range between the 25th percentile and the 75th percentile) were graphed. Additionally, quantiative data from serum oxidative stress, eye tissue oxidative stress and inflammation examinations, was described through mean and standard deviation. A p-value equal to or lower than 0.05 was considered statistically significant. Photos were analyzed using ImageJ 1.53k [
21].
4. Discussion
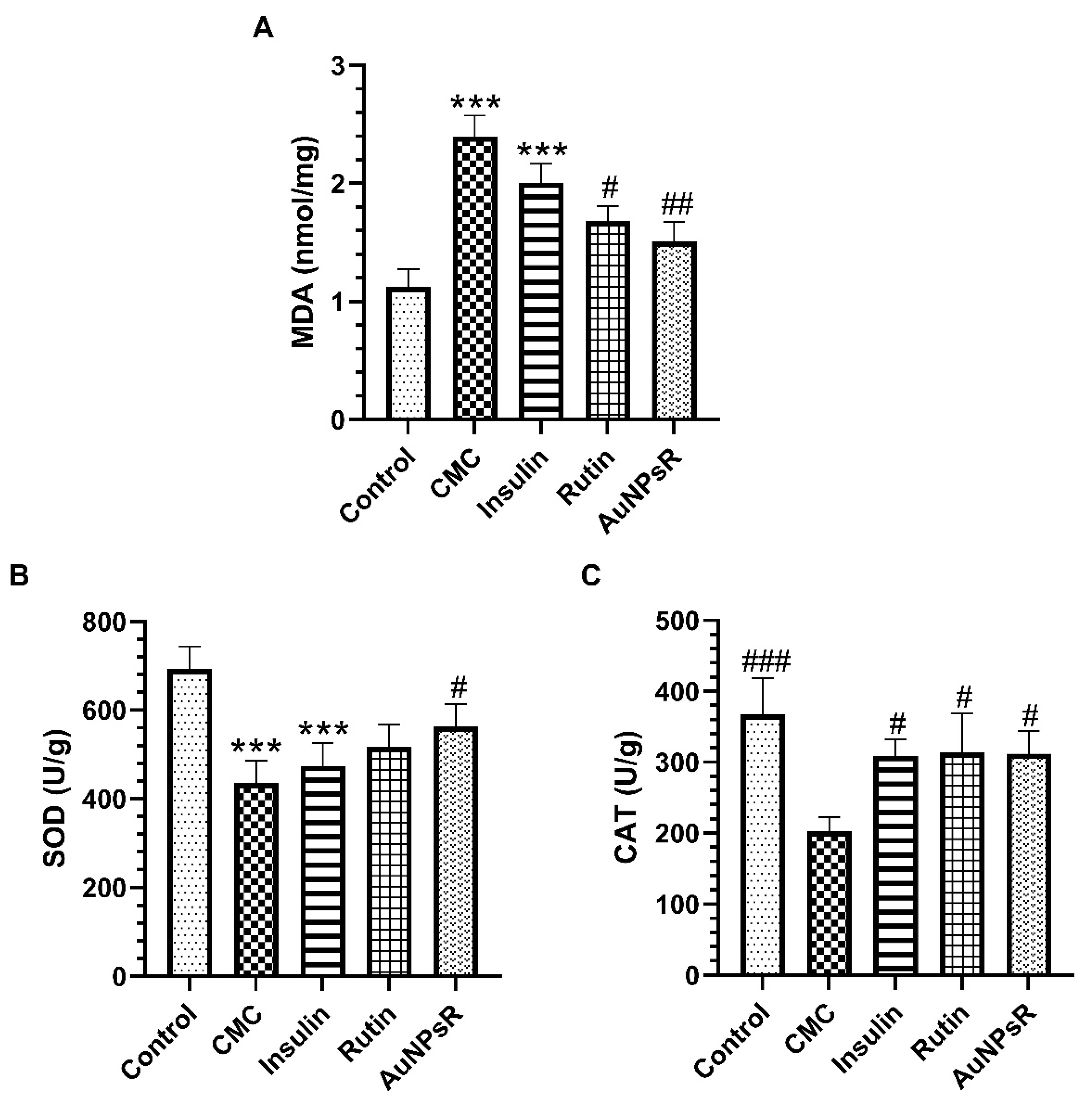
Diabetes is a chronic metabolic disorder associated with endothelial dysfunction and altered vascular contractility. Its various complications, which are of clinical importance, include diabetic retinopathy and cataracts. The underlying pathophysiology is related to hyperglycemia, oxidative stress imbalance and inflammation of the vascular wall, with the accompanying activation of the major pathways responsible for diabetes related damage. The present study demonstrated that DM induced the vasoconstriction of retinal arterioles, with a marked reduction in diameter. Additionally, DM increased the lipid peroxidation in eye tissues and in serum, decreased the antioxidant defense, and triggered an inflammatory response. These findings were also associated with a decrease in retinal wall thickness, and a reduction in the width of retinal layers. Additionally, DM increased lens opacity and caused marked lens fiber disorganization. Treatment with Rutin improved the retinal arteriolar diameter, increased the antioxidant enzymatic activity and reduced the ocular levels of TNF alpha and IL-6. Consequently, Rutin administration reduced the retinal edema and preserved eye lens structure. The administration of AuNPsR improved the appearance of retinal vessels upon fundus examination, decreased MDA formation and increased the overall antioxidant capacity. However, retinal edema and a degree of disorganization in the eye lens fibers were observed.
This study brings a new perspective regarding the early detection and treatment of ocular complications in DM. Additionally, this work proposed a solution to the gap in research delineated in previous articles – that despite its beneficial effects in diabetic microvascular complications, rutin has poor bioavailability and delivery, and thus lowered potency. Therefore, it was hypothesized that using gold nanoparticles as a delivery system would yield, together with an increase in systemic concentration and better ocular uptake, superior antihyperglycemic, antioxidant, and anti-inflammatory effects.
Diabetes was induced by administration of STZ, a substance widely used due to its time and dose dependent induction of apoptosis in pancreatic beta-cells [
32]. The early development of CA and DR were closely monitored through serial examination of eye structures, using relevant literature as a guide.
Firstly, CA was considered to be in its incipient stage at the six-week mark, when, according to Muranov et al [
22], the formation of peripheral opacities on anterior segment evaluation was noted. Similarly, Aung et al evaluated the development of CA in a rat model of post-STZ induced diabetes, and found that subcapsular CA, with characteristic spoke-like lesions, was developed only after six weeks of hyperglycemia [
33]. Moreover, they observed a gradual decline in visual acuity even before statistically significant CA formation, yet contrast sensitivity only began to decrease after nine weeks of diabetes. Thus, the studied hypothesis is further delineated, with a significant need for therapeutic strategies aimed at early-stage CA, before evident vision loss. Additionally, incipient CA development was evaluated by TEM analysis at the six-week mark, to reassure anterior segment examination findings. Similar to our results, Majaw et al observed a more severe disorder of lens fibers in four-week diabetic mice, compared to healthy controls, upon TEM examination [
34].
The development of DR was monitored in parallel. Therefore, weekly fundus examination was used to compare diabetic subjects and healthy animals. Arteriole diameter modifications, indicative of early DR, were noted at the six-week mark. Accordingly, Lai et al described a reduction in blood flow through the retinal arterioles between the fourth and sixth week of hyperglicemia, in a goto-Kakizaki rat model, a species derived from the Wistar family [
35].
Furthermore, the therapeutic agent was chosen based on the pathophysiology of ocular diabetic complications. The mechanisms involved in incipient CA are related to lipid peroxidation, a process significantly increased in diabetes due to the imbalance between prooxidant and antioxidant systems [
36]. This pathophysiological substrate justifies the use of TEM micrographs to study lens opacity. The compounds that form in the eye lens due to lipid peroxidation include dienes, a subclass of alkenes, chemical group readily reacted by OsO4, the employed TEM dye [
37,
38].
Early DR has been associated with reduced retinal blood flow, as observed in an experimental model by Muir et al [
39]. This mechanism is currently explained through the hyperactivation of retinal glia by diabetes caused oxidative stress [
10]. This then triggers the synthesis of Ang II by the intraocular RAS, which in turn leads to a decrease in retinal blood flow by acting on AT1 microglial receptors. Additionally, the same study found that Ang II increases the production of proinflammatory cytokines through its binding onto AT1 microglial receptors. This pathophysiological explanation of incipient DR is further supported by Eshaq et al [
40]. Their study demonstrated that the administration of candesartan, an AT1 receptor blocker, to diabetic Wistar rats, decreased the angiotensin converting enzyme (ACE) level, and increased the retinal blood flow. Moreover, they concluded that candesartan reduced ROS production through a decrease in p22phox levels.
In terms of treatment, insulin was utilized as a positive control because STZ destroys pancreatic beta-cells and induces type 1 diabetes (T1D). On funduscopy examination of retinal arteriole diameter, insulin showed favorable results, restoring normal width parameters. This is an accepted action of insulin, a known vasodilator agent [
41]. However, vessel diameter could be altered immediately after treatment administration, and swiftly reverted. On TEM investigation of lens opacity induced by diabetes, insulin returned results that require a more in-depth discussion, as it increased the opacity in eye lenses, similar to vehicle administration. The discrepancy between the worsening of CA with insulin administration and its beneficial effects upon fundus examination require further detailed investigations.
The mechanism through which insulin might worsen early CA is not well known. However, Papadimitriou et al highlighted a possible direction of research, as they presented a T1D patient under an intense insulin regime, that had an elevated insulin autoantibody count at the time of bilateral CA formation [
42]. Additionally, a widely accepted hypothesis is related to the early worsening of DR (EWDR) by severe insulin therapy. Meng et al explained this phenomenon by the overexpression of NADPH oxidase 4 enzyme activity, and thus, by the overproduction of ROS, as a result of high doses of insulin [
43]. Furthermore, a possible link could exist between EWDR and early lens opacification, based on the reasoning that both CA and DR develop in the same intraocular medium, frequently
in tandem [
44]. The EWDR can be explained by the osmotic force theory, which states that a forceful reduction in glucose, an osmotically active molecule, by insulin use, can lead to a shift in intraocular pressure [
45]. Okamoto et al correlated this process to an aggravated eye lens state, where a series of patients developed hyperopia because of a rapid decrease in glycemia after insulin administration [
46]. This latter explanation was consistent with the changes seen in the present study upon TEM analysis and histopathological examination. Thus, the increased interfibrillar space observed through TEM, after insulin treatment, could be caused by an alteration of intraocular pressure. This could also be correlated with the edema observed upon the retinal histopathological investigation of diabetic rats treated with insulin. Moreover, the histopathological examination yielded a smaller width of both outer nuclear and photoreceptor layers, findings which have not been previously reported, as to our knowledge. An alternative explanation for edema formation in insulin treated rats could be related to the increased production of IL-6. It is known that IL6 mediates retinal inflammation and vascular leakage, with significant
in vivo effects as early as four-weeks of hyperglycemia, as shown by Rojas et al in a DR model of IL-6 deficient mice [
47]. Moreover, anti-IL-6 antibodies have been demonstrated to have beneficial effects in the treatment of diabetic macular edema [
48].
In terms of the target therapeutic agent, an evident pattern that supports the initial claim can be observed. In terms of incipient CA, results confirmed the present hypothesis as best outcomes were attributed to AuNPsR treatment. On TEM investigation of lens opacity induced by diabetes, AuNPsR restored the transparency and improved the arteriolar diameter in fundoscopy. This outcome was similar to that obtained by Rutin administration alone. In fact, it can be concluded that all treatments induced vasodilation and restored the retinal arteriole diameter in DM. Moreover, Rutin and AuNPsR showed a wide range of beneficial effects, additional to those produced by insulin. Thus, upon histopathological investigation, AuNPsR restored the width of all retinal layers, lowered MDA levels and increased SOD and CAT activities.
To our knowledge, no previous study has described the benefits of AuNPsR on DR and CA. However, a similar compound, resveratrol, from the same dietary polyphenol family has been examined. Chen et al demonstrated a statistically significant
in vitro eye lens epithelial cell uptake of gold nanoparticles functionalized with resveratrol (AuNPsRes) with high biocompatibility and reduced citotoxicity [
18]. Furthermore, this study showcased the anticataractogen abilities of AuNPsRes, as it delayed the eye lens opacification upon slit-lamp examination of the studied rats. In terms of restoring transparency, present study results are consistent with those described by Chen et al, as AuNPsR treatment showed promising benefits. This can be correlated to the favorable antioxidant effect observed in both serum and homogenized eye tissue, where AuNPsR significantly decreased MDA formation, a factor responsible for early CA occurence. However, an additional focal disarray of Lf was observed upon TEM structural examination. To our knowledge, no previous study highlighted this modification after administration of gold nanoparticles. Additionally, Cosert et al underlined the significant discrepancies between
in vivo and
in vitro effects of gold engineered nanomaterials, offering supplementary reasoning for the conflicting results [
49]. Nonetheless, Zhang et al reported vacuolization of eye lenses in developing zebrafish embryos after silver nanoparticles administration, which could imply a lens deterioration by a metal-based drug delivery system [
50]. Notably, this study underlined no morphological modifications in the retinas of the same specimens. Subsequently, Dong et al highlighted the implications of AuNPsRes in treatment of DR in a Wistar albino rat mode [
19]. They noticed a decrease in retinal vessels permeability compared to vehicle treated diabetic rats. This would be physiologically correlated to the effect of gold nanoparticles on arteriolar vasoconstriction. Notably, they associated these findings with low levels of vascular endothelial growth factor (VEGF), a molecule that, when targeted in early DR, yielded no significant results in restoring vision, in a recently published clinical trial [51]. Probably, the involvement of VEGF in early DR is limited and there are multiple other factors with a vasodilator role in the retina. It is worth noting that Dong et al evaluated retinal changes after 14 weeks of hyperglicemia, compared to the seven weeks in our study. Thus, VEGF-related mechanisms may be characteristic for more advanced DR. This supposition is further supported by Shi et al and Xiao et al, who found that retinal vessel permeability was significantly increased only after the eighth week of diabetes [52,53]. Furthermore, upon histopathological examination of the retina, a characteristic of early DR was noticed, neural degeneration [54]. Retinal layers showed a decrease in width in rats with DM treated with CMC in alignment with existing literature. Thus, Lai et al reported lowered cellularity in both the ganglion cell layer and outer nuclear layer, coupled with a reduction in total retinal width [
35]. The retinal thickness and width of all individual layers, were most significantly restored in the rats treated with AuNPsR. This could be explained by the levels of ocular IL-1 beta, which were highest in the AuNPsR group. Baptista and Alveleira et al found that IL-1 beta plays a significant role in the proliferation of retinal microglia [55]. The size of the nanoparticles studied in the present work was a considerably small, 15 nm. Therefore, a high penetrability in the ocular tissues was obtained. Despite their benefits against neural deterioration, administration of AuNPsR induced the accumulation of retinal edema, more severe than the other treatments administered. This finding could be correlated to an IL-6 induced edema formation.
Based on the presented data, further toxicological studies are needed in order to assess the safe use of gold nanoparticles and the real benefits for the management of early ocular diabetes complications. The present study investigated the effects of a lower dose, as to maintain feasibility to human treatment extrapolation. However, varying doses should be examined, as to determine the ideal therapeutic cutoff.
Author Contributions
Conceptualization, M.Moldovan and G.A.F.; methodology, M.Moldovan and G.A.F; software, M.Moldovan and A.-M.P.; validation, M.Moldovan, M. Muntean, R.M.B, B.M., G.K.; formal analysis, M.Moldovan and A.-M.P.; investigation, M.Moldovan, A.-M.P., M.Muntean, R.M.B, D.G, B.M, G.K., L.D.; resources, D.G., L.D., A.F., G.A.F.; data curation, M.Moldovan and A.-M.P.; writing—original draft preparation, M.Moldovan; writing—review and editing, G.A.F.; visualization, M.Moldovan, A.-M.P.; supervision, G.A.F., A.F.; project administration, M.Moldovan; funding acquisition, M.Moldovan and G.A.F. All authors have read and agreed to the published version of the manuscript.
Figure 1.
Side-by-side images obtained from the same randomly selected animals; (A) anterior segment photography depicting peripheral spoke-like opacities of incipient cataracts; the larger oval outlines the internal limit of the iris, while the smaller oval outlines the internal border of cataracts lesions, more visibile in the upper left quadrant (from eleven to one clockwise); arrowhead points towards microscope reflection, not to be confused with central opacity; (B) Transmission electron microscopy (TEM) micrograph of eye lens with notable lens fiber disorganization, characteristic of incipient cataracts.
Figure 1.
Side-by-side images obtained from the same randomly selected animals; (A) anterior segment photography depicting peripheral spoke-like opacities of incipient cataracts; the larger oval outlines the internal limit of the iris, while the smaller oval outlines the internal border of cataracts lesions, more visibile in the upper left quadrant (from eleven to one clockwise); arrowhead points towards microscope reflection, not to be confused with central opacity; (B) Transmission electron microscopy (TEM) micrograph of eye lens with notable lens fiber disorganization, characteristic of incipient cataracts.
Figure 2.
A representative fundus photography from each group, in controls (A), and rats with six weeks of diabetes and one week of treatment as follows: CMC (carboxymethylcellulose) (B), Insulin (C), Rutin (D), AuNPsR (gold nanoparticles phytoreduced with Rutin) (E). .
Figure 2.
A representative fundus photography from each group, in controls (A), and rats with six weeks of diabetes and one week of treatment as follows: CMC (carboxymethylcellulose) (B), Insulin (C), Rutin (D), AuNPsR (gold nanoparticles phytoreduced with Rutin) (E). .
Figure 3.
Depiction of Ansel Adam's Zone System by a grayscale gradient, which ranges from zero pixels, or the equivalent of pure black, to 255 pixels, or the equivalent of pure white. For our experimental purpose of evaluating eye lens opacity using transmission electron microscopy micrographs, 100% opacity was attributed to zero pixels, and 0% opacity, or standard transparency, to 166.949 pixels. This value corresponds to the presented micrograph of a subject from the control group, which demonstrated the highest transparency.
Figure 3.
Depiction of Ansel Adam's Zone System by a grayscale gradient, which ranges from zero pixels, or the equivalent of pure black, to 255 pixels, or the equivalent of pure white. For our experimental purpose of evaluating eye lens opacity using transmission electron microscopy micrographs, 100% opacity was attributed to zero pixels, and 0% opacity, or standard transparency, to 166.949 pixels. This value corresponds to the presented micrograph of a subject from the control group, which demonstrated the highest transparency.
Figure 4.
UV-Vis spectra of Rutin and gold nanoparticles phytoreduced with Rutin (AuNPsR).
Figure 4.
UV-Vis spectra of Rutin and gold nanoparticles phytoreduced with Rutin (AuNPsR).
Figure 5.
TEM image (a) and size distribution (b) of gold nanoparticles phytoreduced with Rutin (AuNPsR).
Figure 5.
TEM image (a) and size distribution (b) of gold nanoparticles phytoreduced with Rutin (AuNPsR).
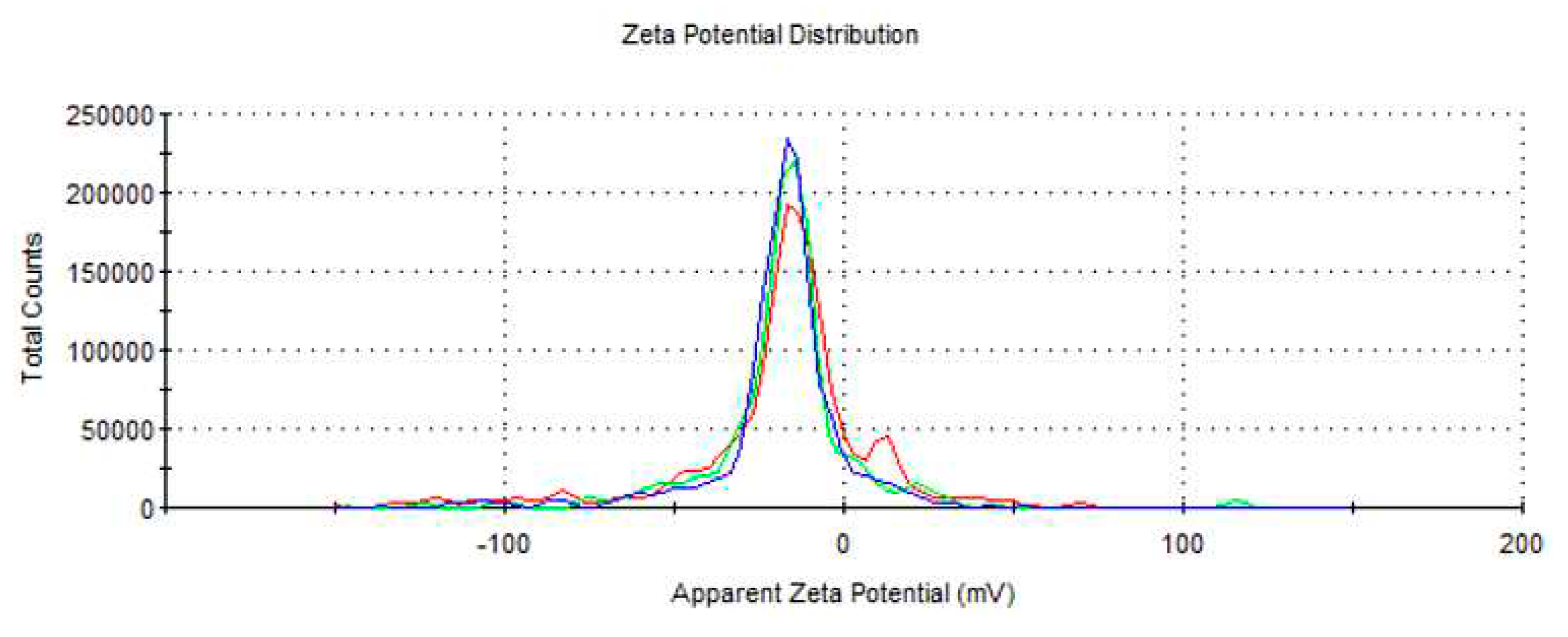
Figure 6.
Zeta potential of gold nanoparticles phytoreduced with Rutin (AuNPsR).
Figure 6.
Zeta potential of gold nanoparticles phytoreduced with Rutin (AuNPsR).
Figure 7.
Retinal arterioles variation of diameter in Control group, and in rats with six-week diabetes, followed by one week of treatments: carboxymethylcellulose (CMC), insulin, Rutin, and gold nanoparticles phytoreduced with Rutin (AuNPsR). Parameters are expressed as minimum and maximum values, median, and interquartile range (Q1–Q3, the range between the 25th percentile and the 75th percentile), with *** p < 0.001 compared to Control group; ^^ p < 0.01, ^^^ p < 0.001 compared to CMC group.
Figure 7.
Retinal arterioles variation of diameter in Control group, and in rats with six-week diabetes, followed by one week of treatments: carboxymethylcellulose (CMC), insulin, Rutin, and gold nanoparticles phytoreduced with Rutin (AuNPsR). Parameters are expressed as minimum and maximum values, median, and interquartile range (Q1–Q3, the range between the 25th percentile and the 75th percentile), with *** p < 0.001 compared to Control group; ^^ p < 0.01, ^^^ p < 0.001 compared to CMC group.
Figure 8.
Blood oxidative stress assessment. (A) Malondialdehyde (MDA) levels, (B) Superoxide dismutase (SOD) and (C) Catalase (CAT) activities in controls, and in diabetic animals treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as mean and standard deviation, with * p < 0.05, *** p < 0.001 compared to Control group; # p < 0.05, ## p < 0.01, and ### p < 0.001 compared to CMC group.
Figure 8.
Blood oxidative stress assessment. (A) Malondialdehyde (MDA) levels, (B) Superoxide dismutase (SOD) and (C) Catalase (CAT) activities in controls, and in diabetic animals treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as mean and standard deviation, with * p < 0.05, *** p < 0.001 compared to Control group; # p < 0.05, ## p < 0.01, and ### p < 0.001 compared to CMC group.
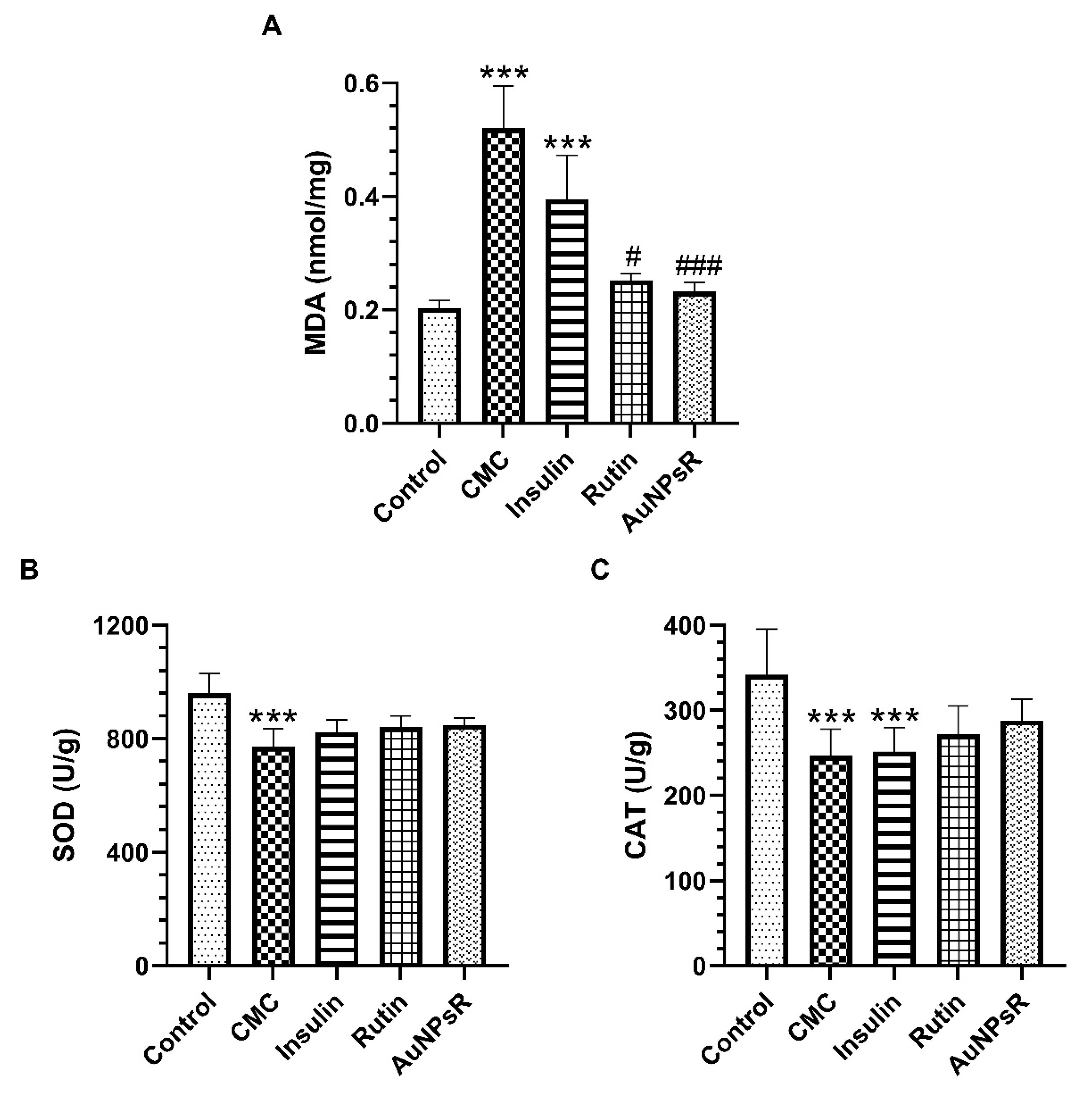
Figure 9.
Oxidative stress parameters in eye tissues homogenates. (A) Malondialdehyde (MDA) levels, (B) Superoxide dismutase (SOD), and (C) Catalase (CAT) activities, in controls and in rats with DM (diabetes mellitus) and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). The parameters are expressed as mean and standard deviation, with *** p < 0.001 compared to Control group; # p < 0.05, and ### p < 0.001 compared to CMC group.
Figure 9.
Oxidative stress parameters in eye tissues homogenates. (A) Malondialdehyde (MDA) levels, (B) Superoxide dismutase (SOD), and (C) Catalase (CAT) activities, in controls and in rats with DM (diabetes mellitus) and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). The parameters are expressed as mean and standard deviation, with *** p < 0.001 compared to Control group; # p < 0.05, and ### p < 0.001 compared to CMC group.
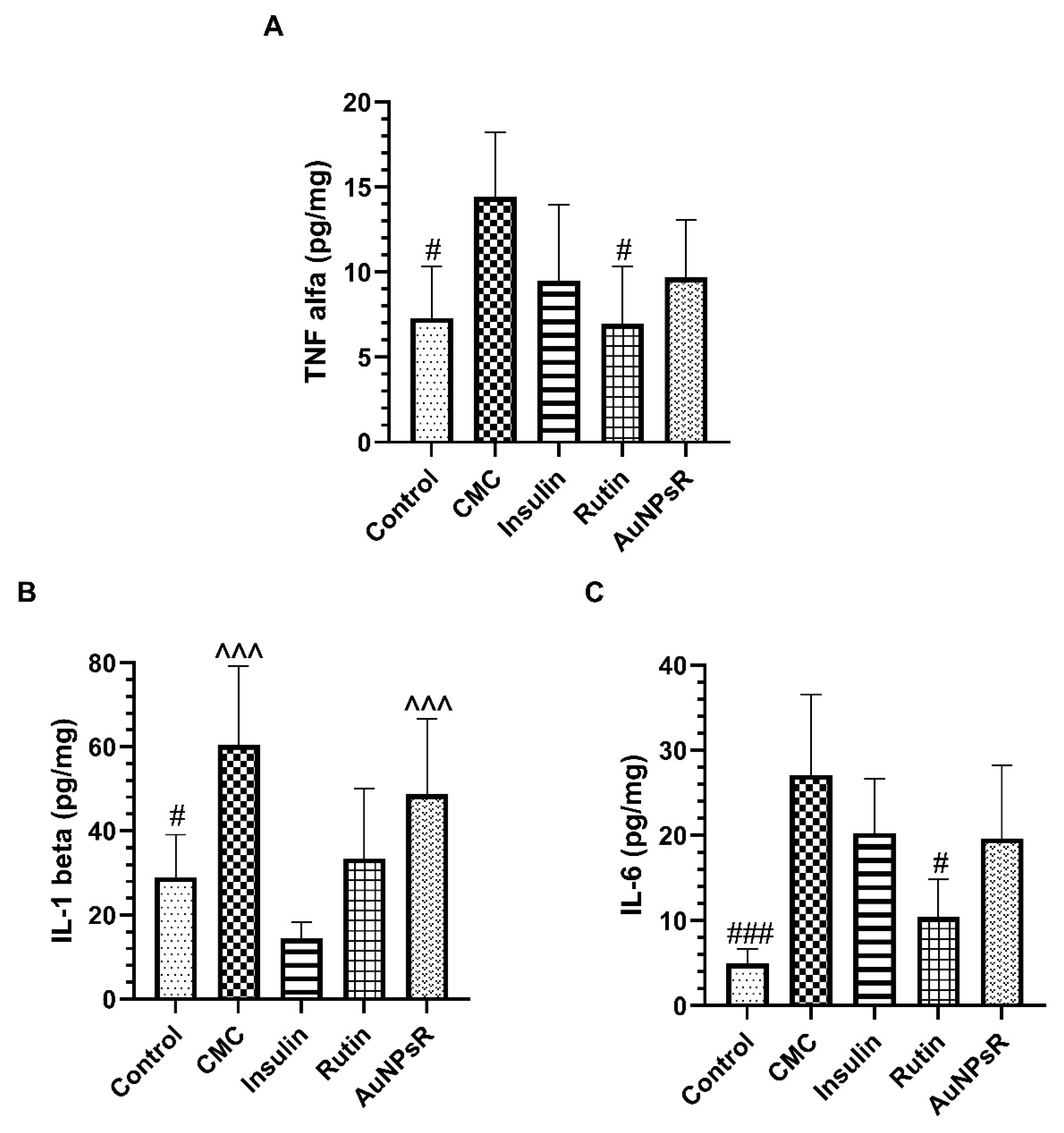
Figure 10.
Proinflammatory cytokines levels in eye homogenates, (A) TNF alfa, (B) IL-1 beta, and (C) IL-6, in controls and in rats with DM and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as mean and standard deviation, with # p < 0.05, ### p < 0.001 compared to CMC group; ^^^ p < 0.001 compared to Insulin group.
Figure 10.
Proinflammatory cytokines levels in eye homogenates, (A) TNF alfa, (B) IL-1 beta, and (C) IL-6, in controls and in rats with DM and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as mean and standard deviation, with # p < 0.05, ### p < 0.001 compared to CMC group; ^^^ p < 0.001 compared to Insulin group.
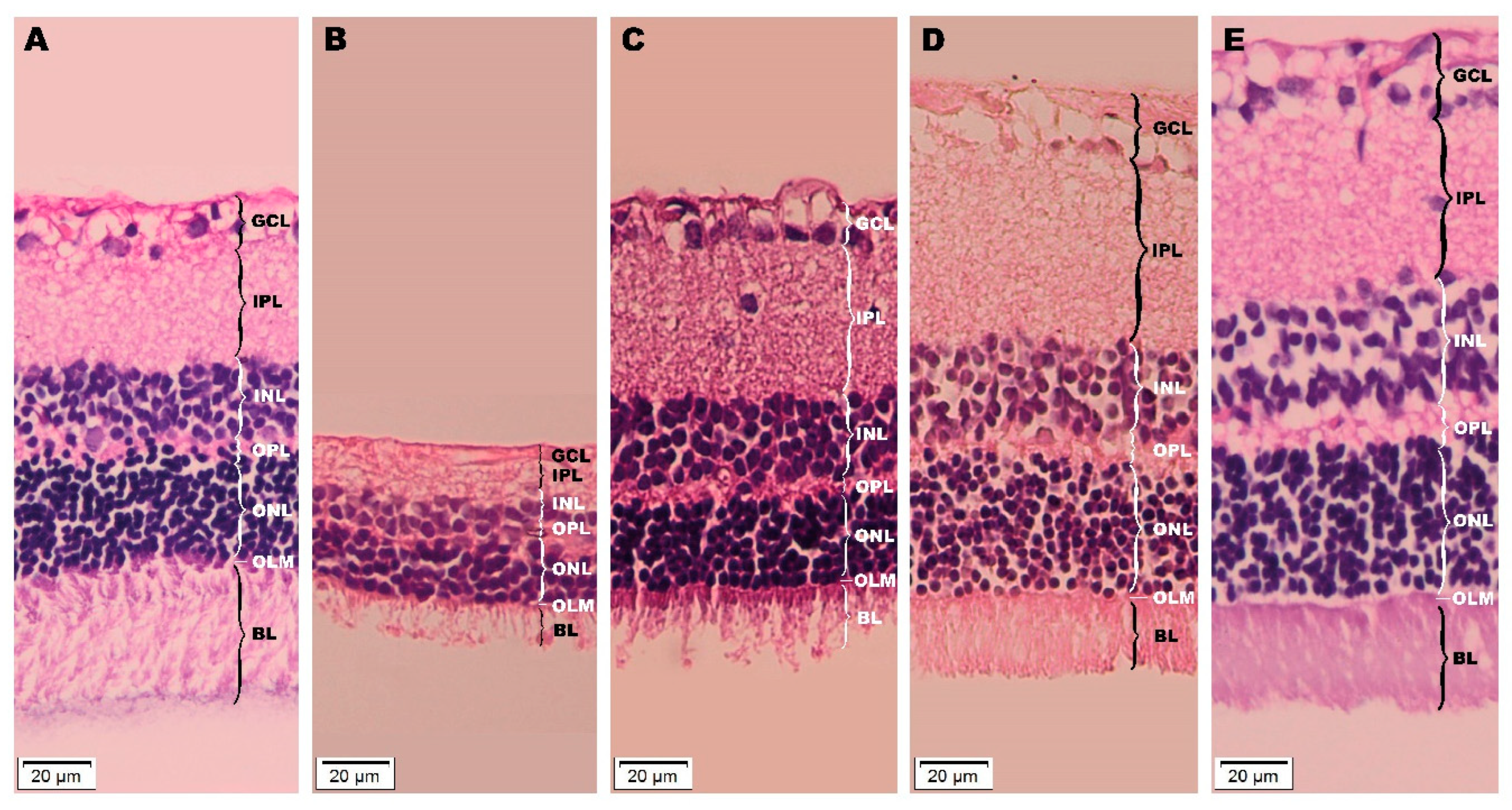
Figure 11.
Histopathological investigation of retinas from (A) healthy specimens, and from six-week diabetic animals, with a subsequent one week of the following treatments: (B) CMC (carboxymethylcellulose), (C) insulin, (D) Rutin, (E) AuNPsR (gold nanoparticles phytoreduced with Rutin); a significant difference in overall retinal thickness is visible, with varying width for each individual layer; increasing levels of edema are perceptible, minimal for insulin (C), moderate for Rutin (D), and advanced for AuNPsR (E); layers of retinas from each group are delineated, GCL (ganglion cell layer), IPL (inner plexiform layer), INL (inner nuclear layer), OPL (outer plexiform player), ONL (outer nuclear layer), OLM (outer limiting membrane), BL (bacillary layer).
Figure 11.
Histopathological investigation of retinas from (A) healthy specimens, and from six-week diabetic animals, with a subsequent one week of the following treatments: (B) CMC (carboxymethylcellulose), (C) insulin, (D) Rutin, (E) AuNPsR (gold nanoparticles phytoreduced with Rutin); a significant difference in overall retinal thickness is visible, with varying width for each individual layer; increasing levels of edema are perceptible, minimal for insulin (C), moderate for Rutin (D), and advanced for AuNPsR (E); layers of retinas from each group are delineated, GCL (ganglion cell layer), IPL (inner plexiform layer), INL (inner nuclear layer), OPL (outer plexiform player), ONL (outer nuclear layer), OLM (outer limiting membrane), BL (bacillary layer).
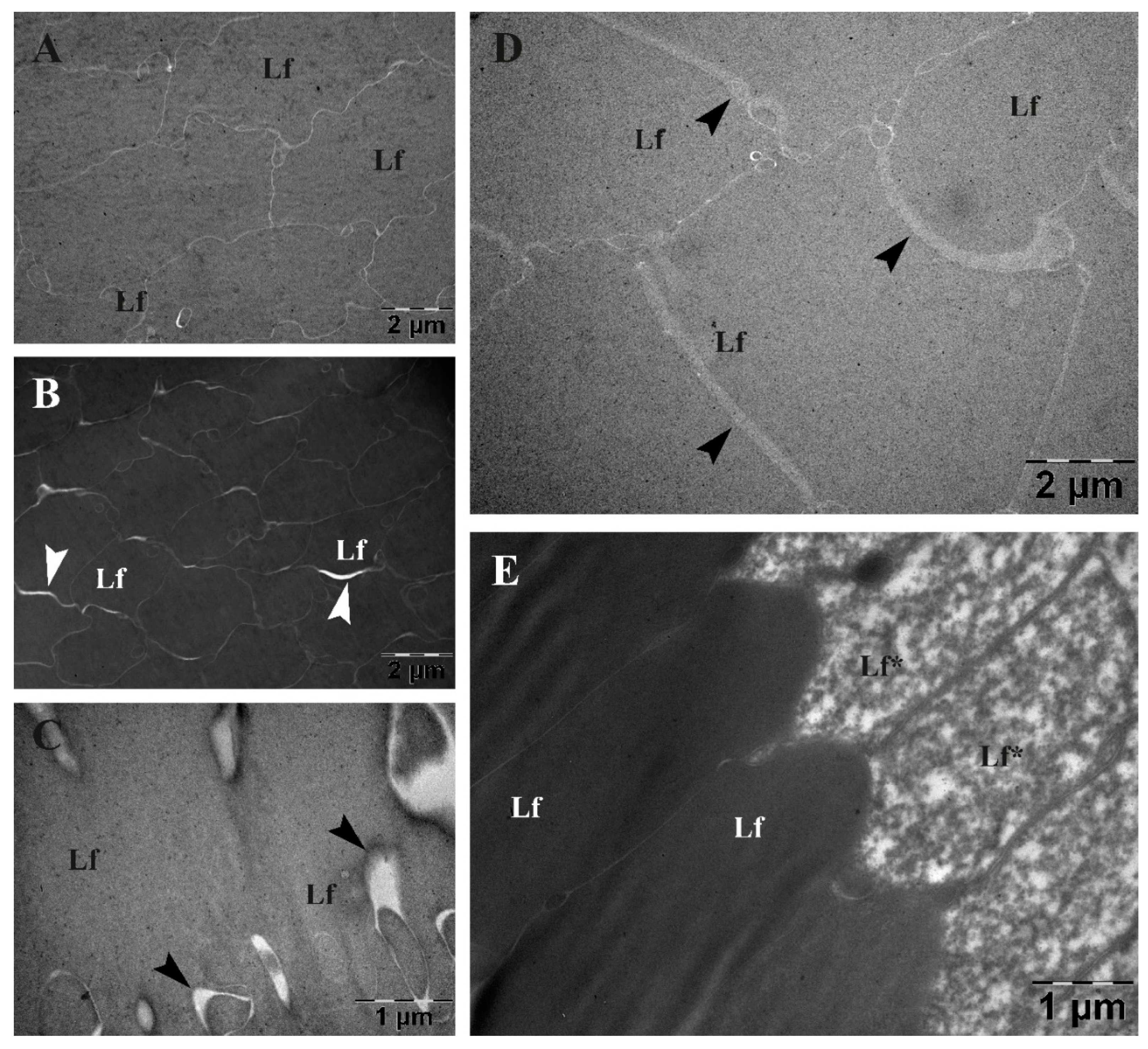
Figure 12.
Transmission electron microscopy investigation of eye lenses from (A) age-matched controls, and from six-week diabetic specimens, followed by one week administration of treatments: (B) CMC (carboxymethylcellulose), (C) insulin, (D) Rutin, (E) AuNPsR (gold nanoparticles phytoreduced with Rutin); a superior electron density was observed in diabetic specimens from CMC group (B), and in diabetic subjects treated with insulin (C); diabetic animals treated with AuNPsR (E) showed focal lens fiber disorganization; arrowhead points towards enlarged interfibrillar spaces (Lf, lens fibers; Lf* disorganized lens fibers).
Figure 12.
Transmission electron microscopy investigation of eye lenses from (A) age-matched controls, and from six-week diabetic specimens, followed by one week administration of treatments: (B) CMC (carboxymethylcellulose), (C) insulin, (D) Rutin, (E) AuNPsR (gold nanoparticles phytoreduced with Rutin); a superior electron density was observed in diabetic specimens from CMC group (B), and in diabetic subjects treated with insulin (C); diabetic animals treated with AuNPsR (E) showed focal lens fiber disorganization; arrowhead points towards enlarged interfibrillar spaces (Lf, lens fibers; Lf* disorganized lens fibers).
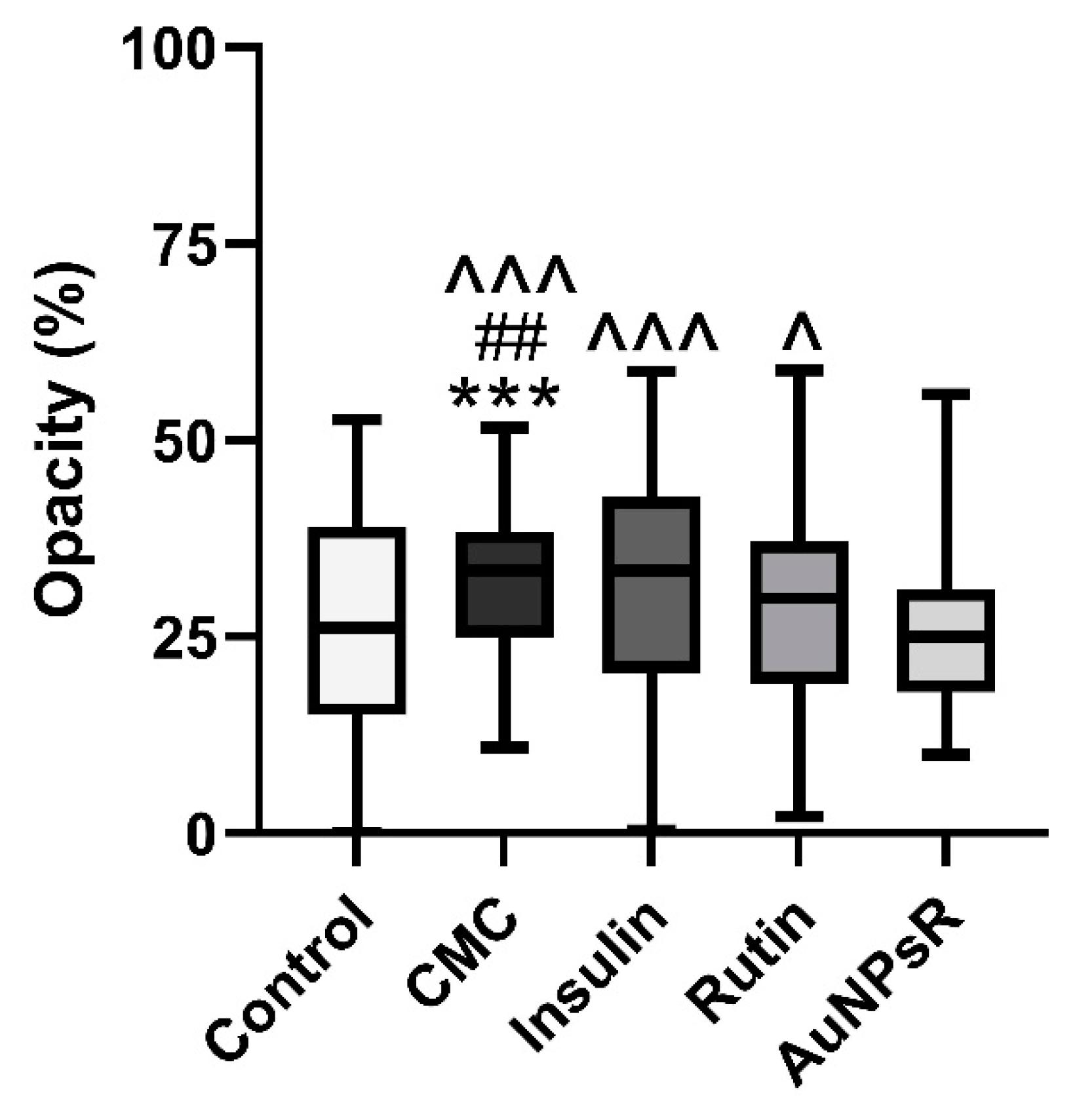
Figure 13.
Lens opacity variation assessed through transmission electron microscopy micrographs, in controls and in rats with diabetes and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as minimum and maximum values, median, and interquartile range (Q1–Q3, the range between the 25th percentile and the 75th percentile), with *** p < 0.001 compared to Control group; ## p < 0.01 compared to Rutin group; ^ p < 0.05, ^^^ p < 0.001 compared to AuNPsR group.
Figure 13.
Lens opacity variation assessed through transmission electron microscopy micrographs, in controls and in rats with diabetes and treated with CMC (carboxymethylcellulose), insulin, Rutin, and AuNPsR (gold nanoparticles phytoreduced with Rutin). Parameters are expressed as minimum and maximum values, median, and interquartile range (Q1–Q3, the range between the 25th percentile and the 75th percentile), with *** p < 0.001 compared to Control group; ## p < 0.01 compared to Rutin group; ^ p < 0.05, ^^^ p < 0.001 compared to AuNPsR group.