1. Introduction
In endodontic treatment, maintaining the original shape and path of the root canal is of paramount importance for a successful outcome [
1,
2]. However, one of the challenges often encountered in clinical practice is the creation of a "ledge" – a deviation from the original pathway of the root canal [
3]. This procedural error has been identified as one of the most common complications in endodontics, significantly impacting the course of treatment and potentially altering the long-term prognosis of the tooth being treated [
4].
A ledge is formed when the endodontic instrument deviates from the natural canal path, typically in curved or narrow canals, resulting in an artificial barrier on the canal wall [
3,
5]. The development of a ledge can prevent the instrument from reaching the apical stop, obstructing shaping, disinfection, and the subsequent filling of the canal system to its working length. As a result, the uneliminated infection may contribute to the continuation of periapical periodontitis [
6,
7]. A more grave concern is that the presence of a ledge can potentially misdirect root canal instrumentation, leading to a possible lateral perforation of the tooth [
8]. This erroneous path taken by the instruments not only compromises the integrity of the root structure but also poses a significant risk to the overall success of the endodontic procedure.
A clinical investigation performed by Greene et al. indicated that 46% of the root canals shaped by dental students had been ledged [
5]. Similarly, Kapalas et al. reported that 52% of the canals treated by dental students resulted in ledge formation [
9]. In comparison, when endodontists performed the procedure, the incidence of ledge creation reduced substantially to 33% [
9]. This highlights the crucial role of a dentist's experience and technical skill in preventing ledge formation. In addition to prevention, ledge management also holds significant importance [
3]. Dental students should be trained to recognize, evaluate, bypass, and correct ledges once formed to avoid severe iatrogenic accidents. Although dental students can gain experience and make progress from their mistakes in clinical work, patients should not be the subject of practice with their health interests at stake. Currently, dental students' understanding of ledges mostly comes from descriptions in textbooks and endodontic literature, highlighting a significant gap in the availability of highly realistic education tools for pre-clinical practice.
The burgeoning landscape of digital technology unfolds novel avenues for the evolution and enhancement of dental education. Additive manufacturing, also known as 3D printing, is a cutting-edge technique that creates physical objects from digital designs by depositing material layer by layer until the final product is formed [
10,
11]. This process fundamentally differs from traditional subtractive manufacturing methods that remove material, allowing complex and intricate designs to be created with minimal material waste and great precision [
12]. At present, 3D printed training models have showcased promising prospects in enhancing the quality of dental education [
13,
14,
15], but training models for ledge management are still lacking.
The present study aimed to establish a digital workflow to fabricate realistic 3D printed tooth models with a root canal ledge for hands-on endodontic training. The benefits of the 3D printed tooth models were evaluated by postgraduate students and endodontic experts using a Likert scale questionnaire. These models were expected to help dental students and practitioners gain experience in ledge management, thus filling the gap in endodontic education.
2. Materials and Methods
2.1. Model Fabrication
2.1.1. Tooth Preparation
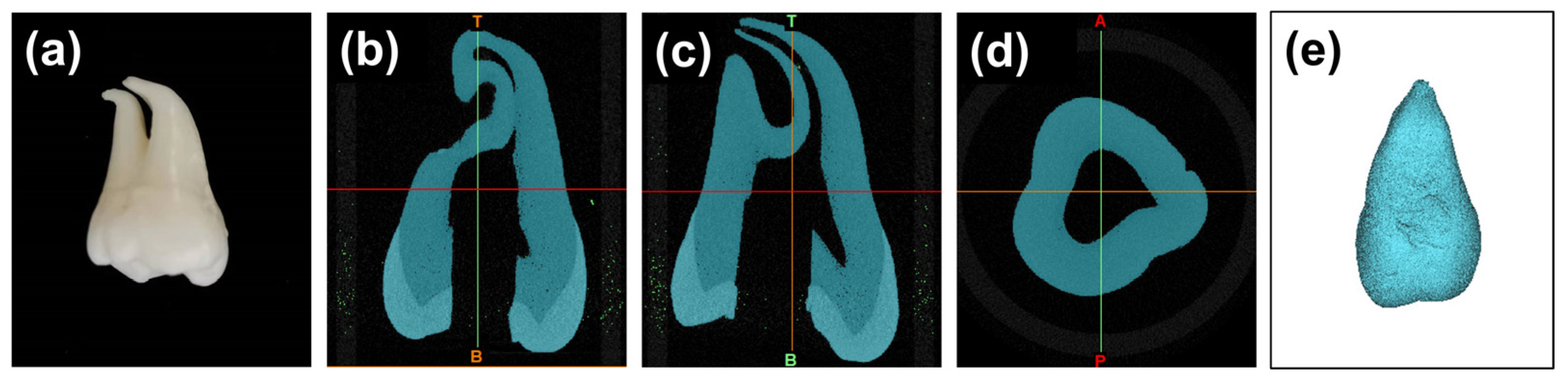
With approval from the Medical Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-D-2021-211), an extracted healthy mandibular molar with curved roots was collected for scientific use. After tooth extraction, the residual periodontal tissues were carefully removed from the root by a sharp scalpel. The teeth were then soaked in 3% hydrogen peroxide for three days. After endodontic cavity preparation, the location of the root canal orifice was carefully detected, and the pulp was removed using a barbed broach (MANI Inc, Tochigi, Japan). Subsequently, the root canals were initially negotiated to their working length with a No. 10 K-file (Dentsply Maillefer, Ballaigues, Switzerland), and then enlarged and shaped with a No. 15 K-file (Dentsply Maillefer). A 3% sodium hypochlorite solution (Longly, Wuhan, China) was intermittently used for irrigation to clear the debris (
Figure 1a).
2.1.2. Micro-Computed Tomography (μCT) Scanning
The prepared tooth was subjected to high-resolution micro-computed tomography (μCT) scanning using a μCT scanner (μCT45, Scanco Medical, Brüttisellen, Switzerland). The scanner was set up to capture images with a voxel size of 10 μm. To obtain a comprehensive view of the tooth's internal structures, the scanning protocol included 250 projections over a 180° rotation. The tube diameter was set at 9/8 mm. After the scanning process, the resulting Digital Imaging and Communications in Medicine (DICOM) data was imported into Materialise Mimics (21.0, Materialise, Leuven, Belgium) and 3D reconstructed. Specifically, A grayscale threshold range between 1637 Hounsfield Units (HU) and 15024 HU was applied to segment the tooth from the background. To further refine the model, a region-growing algorithm with 6-connectivity was utilized to select and aggregate voxels with similar density values. After ensuring the accuracy of the 3D model, it was exported in the standard tessellation language (STL) format for further use (
Figure 1b–d).
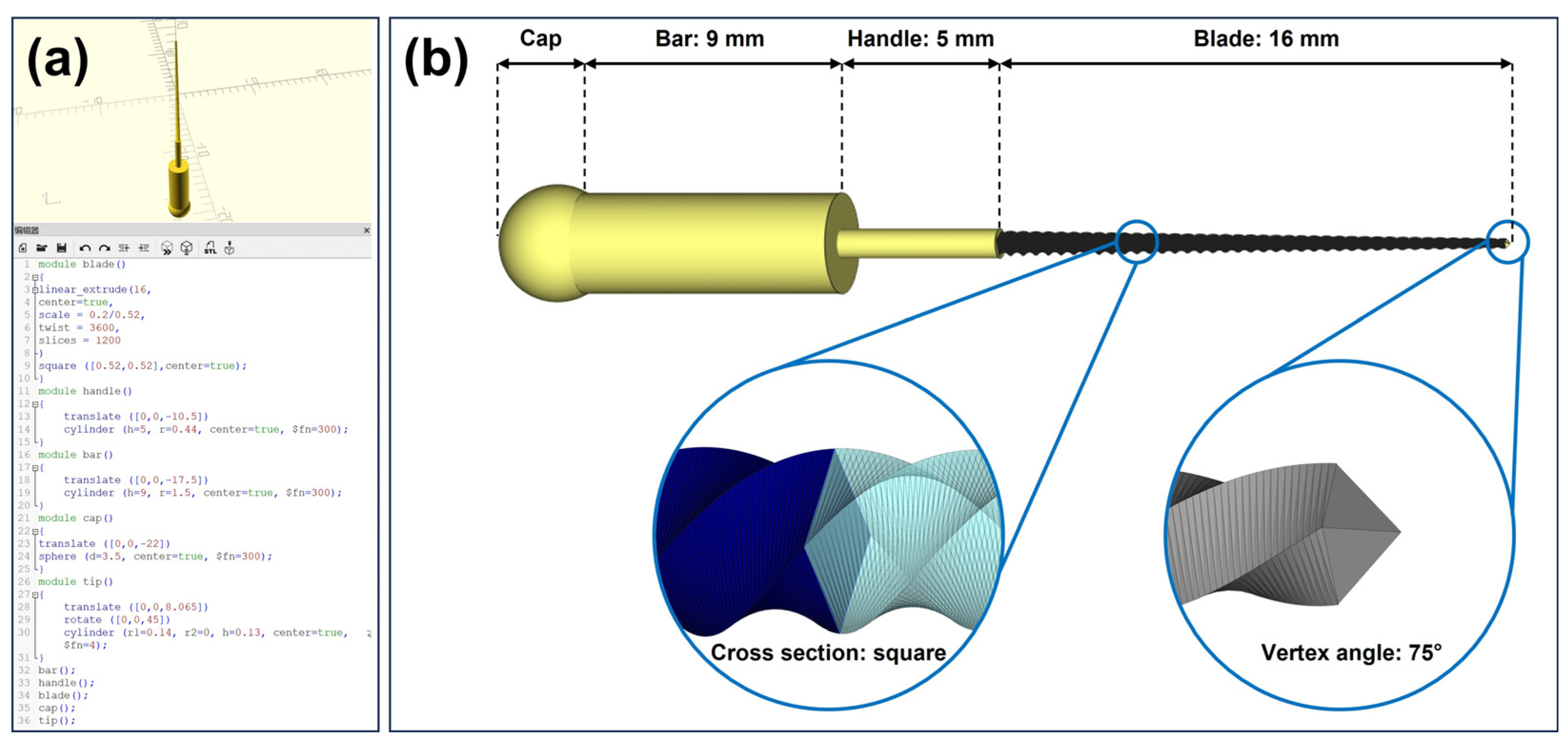
2.1.3. Computer-Aided Design (CAD) of a K File
A No. 20 K-file was designed using CAD software (OpenSCAD, 2021.01,
http://www.openscad.org/). The K file design was divided into four main parts: blade, handle, bar, and cap. Briefly, the blade design was achieved by linearly extruding a square with a side length of 0.52 mm over a distance of 16 mm, with a 3600-degree twist, and uniformly scaled down to a square with a side length of 0.2 mm. The tip of the blade was designed as a four-sided pyramid with a vertex angle of 75°. The handle of the K file was created as a cylinder with a height of 5 mm and a radius of 0.44 mm. The bar was designed similarly to the handle, as a cylinder with a height of 9 mm and a radius of 1.5 mm. The cap, designed as a sphere with a diameter of 3.5 mm, was positioned to partially overlap with the bar. The completed CAD design of the K-file was saved in STL format for subsequent use (
Figure 2). The programming code is provided in
Appendix A.
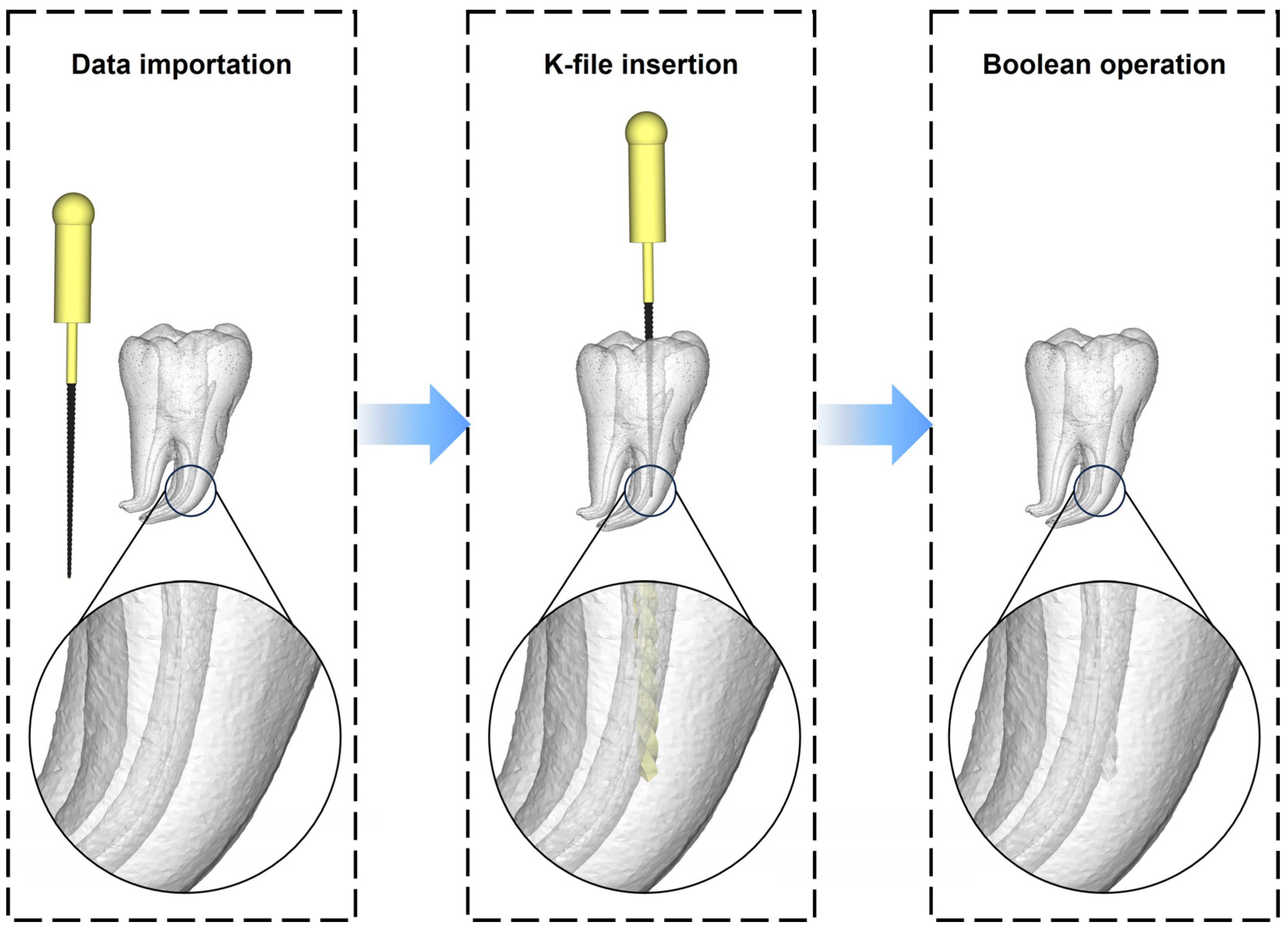
2.1.4. CAD of the Tooth Model with Root Canal Ledge
The STL files of the 3D-reconstructed tooth in section 2.1.2 and the K-file in section 2.1.3 were both imported into the Materialise Magics software (25.0, Materialise, Leuven, Belgium). Subsequently, the K-file was positioned in one of the curved root canals of the 3D-reconstructed tooth using the translate and rotate functions. The tip of the K-file was partly inserted into the outer wall of the curved section of the root canal, mimicking the formation of a ledge. Following this, Boolean operations were applied to subtract the K-file model from the 3D-reconstructed tooth, resulting in a tooth model with a root canal ledge. The model was then saved in STL format for subsequent additive manufacturing (
Figure 3).
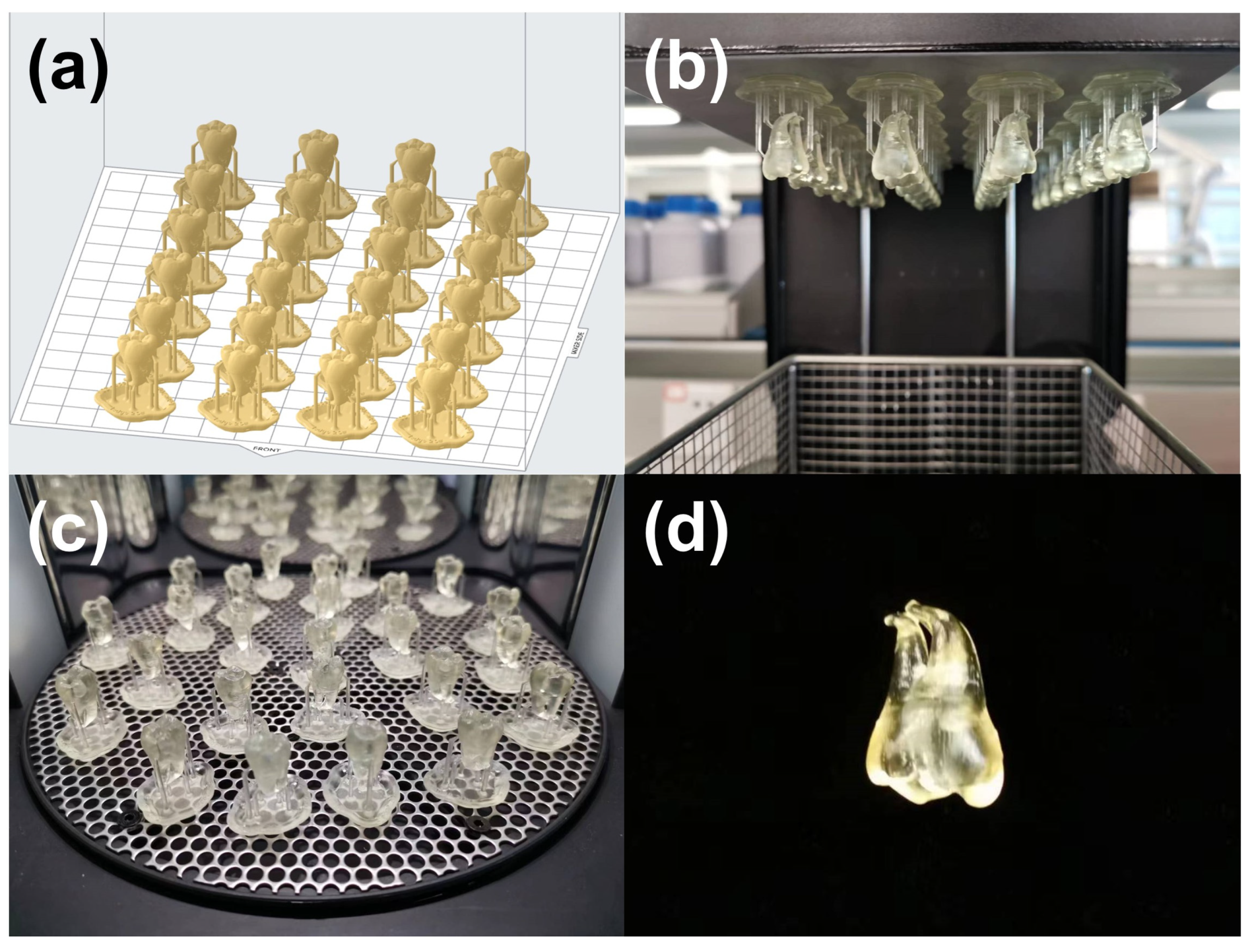
2.1.5. Additive Manufacturing
The model obtained in section 2.1.4 was 3D printed on a 1.5x scale by a stereolithography (SLA) printer (Form 3B, Formlabs, Somerville, MA, USA) with a 50 μm layer thickness using a semitransparent photopolymer resin (SG V1, Formlabs). The printing direction and layout are shown in
Figure 4a. 24 models were printed at one time for 9 h and 30 min. Following the printing process, the models were cleansed with isopropyl alcohol (IPA, Chron chemicals, Chengdu, China) for a duration of 20 min using a post-cleaning device (Form Wash, Formlabs). Afterward, the models underwent a post-curing process under a 405 nm blue light at a temperature of 60 °C for a period of 30 minutes in a post-curing device (Form Cure, Formlabs). Upon completion of the post-curing, the support structures were carefully detached using a specialized finishing kit provided by Formlabs. Any remnants of the support structures were meticulously trimmed using a sharp scalpel to ensure a clean and precise final model.
2.2. Model Evaluation
To evaluate the fabricated training models, we organized a hands-on workshop with voluntary participation. According to the minimum sample size determined by the n-Star method [
16], 30 individuals, including 20 postgraduate students and 10 endodontists, participated in this hands-on course. The students had already completed their basic theoretical study in endodontic treatment and performed at least 10 root canal treatments on patients. To maintain objectivity of the evaluation, students were assured that their performance during the evaluation would not have any influence on their academic scores.
At the outset of the workshop, we conducted a brief review for the students on the concept of ledge formation and the reasons for its occurrence. Subsequently, the techniques for ledge management were outlined, which focused on: 1) Recognizing ledges - characterized by the loss of the typical tactile sensation of the endodontic instrument's tip as the feeling of being held by the canal walls transitions into a sensation of hitting against a canal wall; 2) Bypassing ledges - achieved by pre-bending the endodontic instrument to facilitate the tip's gentle slide along the inner surface of the curved canal, thereby assisting in bypassing the ledge and reaching the working length; 3) Correcting ledges - this technique involves positioning and maintaining the file tip apical to the ledge, applying gentle pressure with the file against the outer wall where the ledge is located, and then moving the file in and out over a short distance.
Next, the participants were asked to practice the techniques mentioned above using the 3D printed models. The benefits of the model were assessed by a questionnaire (
Table 1) made by the Teaching and Research Section of Preventive Dentistry at the university using SurveyStar (Ranxing Information Technology Co., Ltd., Changsha, Hunan, China). Participants were asked to rate 7 items on a Likert scale from 1 to 5 in the questionnaire (1 = excellent, 2 = good, 3 = satisfactory, 4 = adequate, 5 = poor). The first four items pertained to the quality of the model, while the remaining three items assessed the educational effect of the tooth model. In addition, free comment from the participants was also collected. The internal consistency among the items in the questionnaire was examined by Cronbach’s alpha test using SPSS statistics software (26.0, IBM, New York, NY, USA). An obtained Cronbach's alpha value greater than 0.7 was considered indicative of good reliability. We also calculated the frequencies and mean values (Ø) of ratings. The differences in ratings between the students and experts were examined by Mann-Whitney U test using GraphPad Prism (9.5.1, GraphPad Software, San Diego, CA, USA). A p-value of 0.05 was used to determine statistical significance.
3. Results
3.1. D Printed Model for Endodontic Training
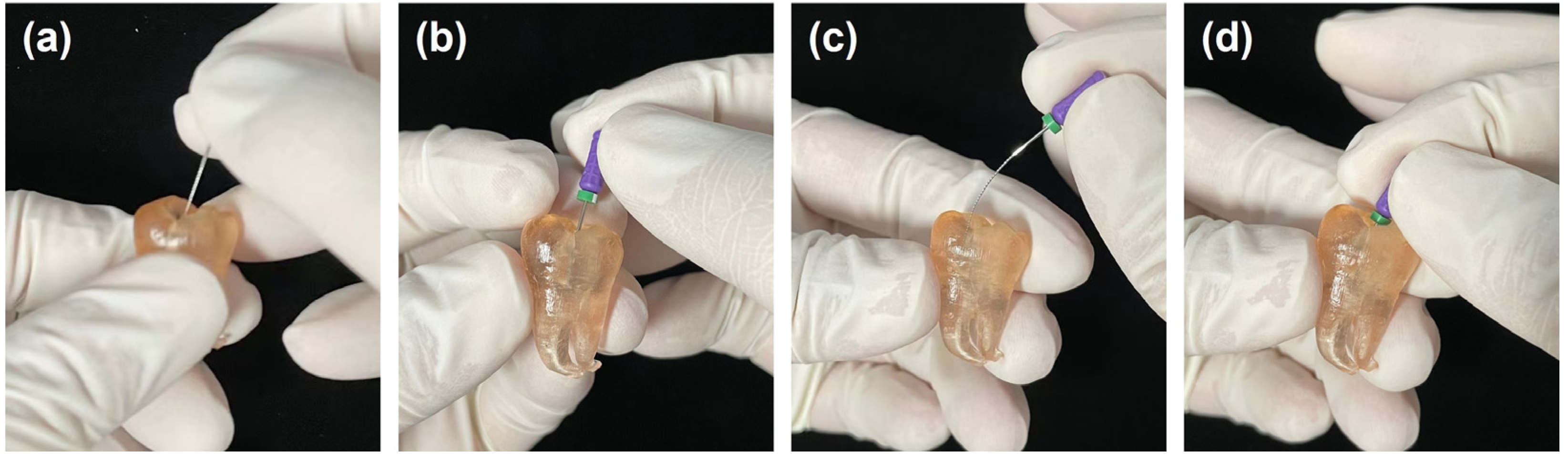
As shown in
Figure 5, the 3D printed tooth model could be successfully applied in endodontic training. The model incorporated a highly realistic root canal system for endodontic practice (
Figure 5a). When a straight K-file was inserted into the curve portion of the root canal, resistance force and tactile change caused by the ledge could be experienced (
Figure 5b). By pre-bending, the instrument could bypass the ledge and reach the working length (
Figure 5c,d).
3.2. Evaluation of the Model
All participants completed the questionnaire, resulting in a 100% response rate. The questionnaire demonstrated good internal consistency, with a Cronbach's alpha value of 0.85. For all 7 items in the questionnaire, students and experts provided similar ratings. Accordingly, no statistically significant differences were found between the student and expert groups according to the results of the Mann-Whitney U test (p > 0.05,
Table 2).
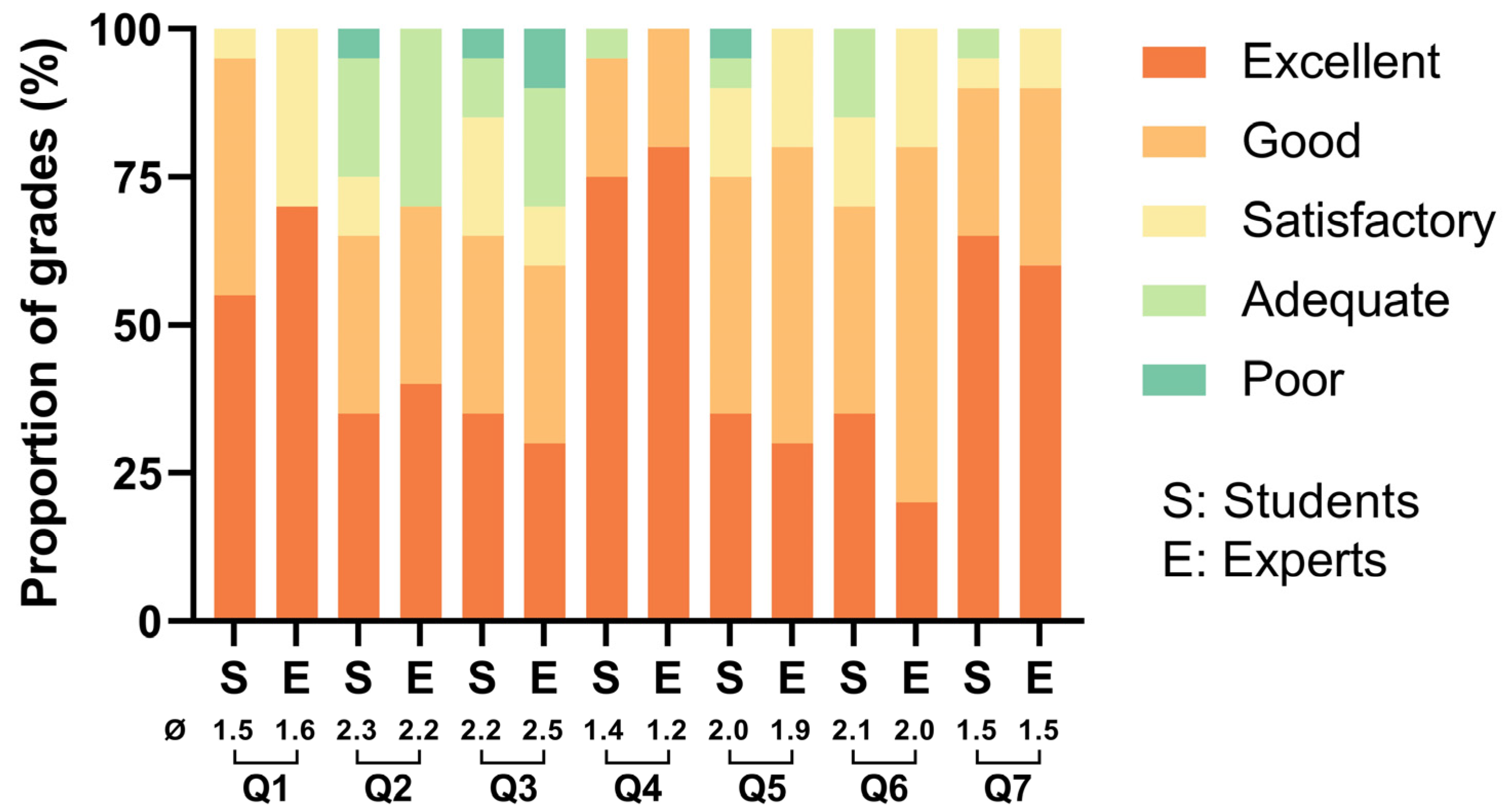
As illustrated in
Figure 6, both experts and students gave relatively positive evaluations concerning the quality of the model. They rated the fidelity of the 3D printed model in simulating the anatomical structure of a natural tooth as good to excellent (Q1: Ø = 1.5 for students and Ø = 1.6 for experts), the realism of the model in simulating a root canal ledge as satisfactory to good (Q2: Ø = 2.3 for students and Ø = 2.2 for experts), and the material texture replication of a natural tooth as satisfactory to good (Q3: Ø = 2.2 for students and Ø = 2.5 for experts). Both students and experts concurred that the semitransparent material used for fabricating the model significantly contributes to endodontic training, rating it as Good to Excellent (Q4: Ø = 1.4 for students and Ø = 1.2 for experts).
Concerning the educational effect of the model, both students and experts agreed that practicing with the 3D printed model was beneficial for preventing ledge formation (Q5) and managing existing ledges (Q6). The associated ratings were predominantly "good" with mean values (Ø) around 2. Lastly, both groups of participants believed that incorporating the 3D printed model into future endodontic training could potentially achieve "good" to "excellent" educational outcomes (Q7: Ø = 1.5 for students and experts).
Table 2.
Comparative analysis of ratings between students and experts using the Mann-Whitney U test.
Table 2.
Comparative analysis of ratings between students and experts using the Mann-Whitney U test.
| |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
| P-value1
|
0.86 |
0.87 |
0.63 |
0.90 |
0.95 |
1.00 |
0.91 |
| S/E2
|
313/152 |
315/150 |
299/166 |
316/149 |
311.5/153.5 |
309/156 |
306/159 |
| U statistic |
97 |
95 |
89 |
94 |
98.5 |
99 |
96 |
4. Discussion
Ledge formation is one of the most common and prevalent complications in endodontic treatment [
17]. Failure in preventing ledge formation and managing existing ledges may lead to more serious complications, such as persistent apical periodontitis and lateral perforation of the root [
3,
18]. These complications can significantly diminish the prognosis of endodontic treatment, and may even result in the eventual extraction of the treated tooth [
19,
20]. To date, a wealth of textbooks and literature has comprehensively and meticulously discussed the causes of ledge formation and the techniques to manage them. These resources are undoubtedly crucial for enhancing the theoretical knowledge of dental students. However, dentistry remains a practice-based discipline, which means that substantial hands-on training is required to translate theoretical knowledge into clinical skills. In the journey of a student to become an expert, patients should not be regarded as subjects for practice, and their health interests should not be sacrificed. However, there remains a conspicuous absence of highly realistic endodontic training models specifically designed for ledge management practice. To fill this gap, the present study aimed to create a tooth model with a root canal ledge for preclinical endodontic training.
Undeniably, extracted teeth have been a significant source for preclinical practice by providing dental students with highly realistic clinical simulations [
21]. However, extracted teeth might be limited in their reproducibility. In other words, an extracted tooth can only be used one time in hands-on practice. This characteristic makes extracted teeth insufficient to meet the vast demand for preclinical practice among dental students. Moreover, disinfection and storage of extracted teeth may also be tricky [
22]. With the rapid advancement of digital dental technologies in recent years, 3D printed tooth models have shown prospect in resolving this issue, thus driving forward the progression of dental education. To date, a number of 3D printed tooth models have been developed for preclinical practice, but most of them focused on the aspects of primary dental education, such as models for crown preparation [
14], caries removal [
15,
23], and root canal therapy [
24,
25]. The models that enable the practice of more challenging techniques (such as removing fractured instrument and repairing lateral perforation) are still in great need by both dental students and experts.
In this study, additive manufacturing serves as the pivotal technology for model fabrication. This is due to the working principle of 3D printing allows for the fabrication of complex structures. The root canal system is one of such examples, especially when the roots are significantly curved [
25,
26]. However, the fabrication process in this study still faces challenges because the root canal near the apex is extremely narrow. Even though we adopted a relatively accurate 3D printing technology (SLA) [
27], blockage at the apical part of the root canal was prone to occur. Utilizing other 3D printing technologies with higher precision, such as Polyjet [
28,
29], or using resins available for smaller layer thickness, such as Model V3 provided by Formlabs (25 μm), might solve this issue. In this study, we employed SG V1 (Formlabs) resin to print the model with a minimum layer thickness of 50 μm. Although SG V1 is not the most accurate material offered by Formlabs, its semitransparent nature could greatly aid in observing, understanding, and learning ledge management (questionnaire Q4). Students could check the position of instruments when necessary, thus providing essential feedback on their operations. To address the issue of apical blockage, we slightly magnified the model. This modification did not significantly impact the realism of the 3D printed model (questionnaire Q1).
The two relatively lower-rated items in the questionnaire were Q2 and Q3. We have analyzed the potential reasons to guide further improvements to the model. Regarding Q2, the reason might be related to the ledge being set too small and shallow. In real root canal treatment, the formation of a ledge is usually caused by repeated enlargement with a file, so the actual size of the ledge may be larger than the diameter of the file tip. In this study, the size of the ledge equaled to the diameter of a No. 20 K-file tip, which may slightly differ from the real situation. For further improvement, enlarging and deepening the ledge to increase the difficulty of ledge bypassing can be considered. In terms of Q3, the relatively lower rating could be due to the photopolymer resin's hardness and wear resistance being inferior to that of natural teeth [
30], thus potentially lessening the challenge of correcting and eliminating ledges. For future enhancements, we could consider using more durable 3D printing resins for model fabrication.
The limitation of this study is the absence of a control group utilizing a "traditional training model". As previously mentioned, there are currently no commercially available models designed specifically for ledge management training. Given the considerable incidence (33%) of ledge formation among endodontists [
9], this study included 10 such experts and assessed any differences in model evaluation compared to students. The results of this study show that both groups had similar perceptions about the 3D printed training model, which is worth promoting in future endodontic education (Q7) to benefit dental practitioners in preventing ledge formation (Q5) and managing existing ledges (Q6).
5. Conclusions
By utilizing μCT scanning, CAD, and additive manufacturing, this study developed a digital workflow for fabricating a tooth model specifically designed for practicing ledge management in endodontic education. Both students and experts provided positive feedback regarding the quality of the model and its effectiveness in endodontic training. This novel model is expected to fill the gap in endodontic education, thus offering substantial benefits to dental practitioners.
Author Contributions
Conceptualization, Tao Hu and Yichen Xu; methodology, Yichen Xu; software, Yichen Xu; validation, Tao Hu and Yichen Xu; formal analysis, Rui Zhang and Renjie Tang; investigation, Rui Zhang and Renjie Tang; resources, Tao Hu and Yichen Xu; data curation, Yuting Tian and Yong Xiang; writing—original draft preparation, Rui Zhang; writing—review and editing, Yichen Xu, Sebastian Spintzyk; visualization, Yichen Xu; supervision, Tao Hu; project administration, Tao Hu; funding acquisition, Tao Hu and Yichen Xu. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Natural Science Foundation of China (No. 32201096), Research and Development Program of West China Hospital of Stomatology Sichuan University (No. RD-03-202002 and No. RD-02-202114), and Research Funding from West China School/Hospital of Stomatology Sichuan University (No. RCDWJS2021-13).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Medical Ethics Committee of West China Hospital of Stomatology, Sichuan University (No. WCHSIRB-D-2021-211).
Acknowledgments
The authors would like to acknowledge the students and endodontists who participated in the hands-on workshop.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A Programming Code of a No. 20 K-File in OpenSCAD Software
module blade()
{
linear_extrude(16,
center=true,
scale=0.2/0.52,
twist=3600,
slices=1200
)
square ([0.52,0.52], center=true);
}
module handle()
{
translate ([0,0,-10.5])
cylinder (h=5, r=0.44, center=true, $fn=300);
}
module bar()
{
translate ([0,0,-17.5])
cylinder (h=9, r=1.5, center=true, $fn=300);
}
module cap()
{
translate ([0,0,-22])
sphere (d=3.5, center=true, $fn=300);
}
module tip()
{
translate ([0,0,8.065])
rotate ([0,0,45])
cylinder (r1=0.14, r2=0, h=0.13, center=true, $fn=4);
}
bar();
handle();
blade();
cap();
tip();
References
- Çelik, G.; Özdemir Kısacık, F.; Yılmaz, E.F.; Mersinlioğlu, A.; Ertuğrul, İ.F.; Orhan, H. A Comparative Study of Root Canal Shaping Using Protaper Universal and Protaper next Rotary Files in Preclinical Dental Education. PeerJ 2019, 7, e7419. [Google Scholar] [CrossRef]
- Hamid, H.R.; Gluskin, A.H.; Peters, O.A.; Peters, C.I. Rotary Versus Reciprocation Root Canal Preparation: Initial Clinical Quality Assessment in a Novice Clinician Cohort. J Endod 2018, 44, 1257–1262. [Google Scholar] [CrossRef]
- Jafarzadeh, H.; Abbott, P.V. Ledge Formation: Review of a Great Challenge in Endodontics. Journal of Endodontics 2007, 33, 1155–1162. [Google Scholar] [CrossRef]
- Berutti, E.; Alovisi, M.; Moccia, E.; Carossa, M.; De Caro, G.; Roccuzzo, A.; Pasqualini, D.; Scotti, N. Micro-Computed Tomographic Evaluation of Endodontic Ledge Position in Relation to Canal Curvatures. BMC Oral Health 2022, 22, 482. [Google Scholar] [CrossRef]
- Greene, K.J.; Krell, K.V. Clinical Factors Associated with Ledged Canals in Maxillary and Mandibular Molars. Oral Surg Oral Med Oral Pathol 1990, 70, 490–497. [Google Scholar] [CrossRef]
- Friedman, S.; Abitbol, S.; Lawrence, H.P. Treatment Outcome in Endodontics: The Toronto Study. Phase 1: Initial Treatment. J Endod 2003, 29, 787–793. [Google Scholar] [CrossRef]
- de Chevigny, C.; Dao, T.T.; Basrani, B.R.; Marquis, V.; Farzaneh, M.; Abitbol, S.; Friedman, S. Treatment Outcome in Endodontics: The Toronto Study--Phase 4: Initial Treatment. J Endod 2008, 34, 258–263. [Google Scholar] [CrossRef]
- Hargreaves, K.M. , Cohen, S., Berman, L.H. (Eds.) Cohen’s Pathways of the Pulp, 10th ed.; Mosby Elsevier: St. Louis, Mo, USA, 2011; ISBN 978-0-323-06489-7. [Google Scholar]
- Kapalas, A.; Lambrianidis, T. Factors Associated with Root Canal Ledging during Instrumentation. Endod Dent Traumatol 2000, 16, 229–231. [Google Scholar] [CrossRef] [PubMed]
- van Noort, R. The Future of Dental Devices Is Digital. Dental Materials 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Xepapadeas, A.B.; Koos, B.; Geis-Gerstorfer, J.; Li, P.; Spintzyk, S. Effect of Post-Rinsing Time on the Mechanical Strength and Cytotoxicity of a 3D Printed Orthodontic Splint Material. Dent Mater 2021, 37, e314–e327. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Huang, H.; Wu, M.; Tian, Y.; Wan, Q.; Shi, B.; Hu, T.; Spintzyk, S. Rapid Additive Manufacturing of a Superlight Obturator for Large Oronasal Fistula in Pediatric Patient. The Laryngoscope 2022, lary.30352. [Google Scholar] [CrossRef]
- Hanisch, M.; Kroeger, E.; Dekiff, M.; Timme, M.; Kleinheinz, J.; Dirksen, D. 3D-Printed Surgical Training Model Based on Real Patient Situations for Dental Education. Int J Environ Res Public Health 2020, 17, 2901. [Google Scholar] [CrossRef]
- Höhne, C.; Schwarzbauer, R.; Schmitter, M. 3D Printed Teeth with Enamel and Dentin Layer for Educating Dental Students in Crown Preparation. J Dent Educ 2019, 83, 1457–1463. [Google Scholar] [CrossRef] [PubMed]
- Höhne, C.; Schmitter, M. 3D Printed Teeth for the Preclinical Education of Dental Students. J Dent Educ 2019, 83, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Louangrath, P. Minimum Sample Size Method Based on Survey Scales. Int. J. Res. Methodol. Soc. Sci 2017, 3, 44–52. [Google Scholar] [CrossRef]
- Aung, N.; Watanabe, S.; Kouno, A.; Hongo, T.; Yao, K.; Satake, K.; Okiji, T. Fluid Movement in the Apical Area Beyond the Ledge During Er:YAG Laser-Activated Irrigation: A Particle Image Velocimetry Analysis. Photobiomodul Photomed Laser Surg 2020, 38, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Harty, F.J.; Parkins, B.J.; Wengraf, A.M. Success Rate in Root Canal Therapy. A Retrospective Study of Conventional Cases. Br Dent J 1970, 128, 65–70. [Google Scholar] [CrossRef]
- Ingle, J.I.; Bakland, L.K.; Baumgartner, J.C. Ingle’s Endodontics 6, 6th ed.; BC Decker; McGraw-Hill Education [distributor]: Hamilton, ON, Maidenhead, 2008; ISBN 978-1-60795-068-4. [Google Scholar]
- Walton, R.E.; Torabinejad, M. Philadelphia, PA, 2002; ISBN 978-0-7216-9160-2, 3rd ed.; Walton, R.E., Torabinejad, M., Eds.; In Principles and Practice of Endodontics, Saunders: Philadelphia, PA, USA, 2002; ISBN 978-0-7216-9160-2. [Google Scholar]
- Decurcio, D.A.; Lim, E.; Chaves, G.S.; Nagendrababu, V.; Estrela, C.; Rossi-Fedele, G. Pre-Clinical Endodontic Education Outcomes between Artificial versus Extracted Natural Teeth: A Systematic Review. Int Endod J 2019, 52, 1153–1161. [Google Scholar] [CrossRef]
- Chandki, R.; Maru, R.; Gunwal, M.; Garg, A.; Mishra, A. A Comparison of Different Methods for Disinfection or Sterilization of Extracted Human Teeth to Be Used for Dental Education Purposes. World J Dent 2013, 4, 29–31. [Google Scholar]
- Ballester, B.; Pilliol, V.; Allaerd, P.; Jacquot, B.; Guivarc’h, M. Evaluation of a New 3D-Printed Tooth Model Allowing Preoperative ICDAS Assessment and Caries Removal. Eur J Dent Educ 2023. [Google Scholar] [CrossRef]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D Printed Replicas for Endodontic Education. Int Endod J 2019, 52, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.; Wealleans, J.; Ray, J. Endodontic Applications of 3D Printing. Int Endod J 2018, 51, 1005–1018. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J Clin Med 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Németh, A.; Vitai, V.; Czumbel, M.L.; Szabó, B.; Varga, G.; Kerémi, B.; Hegyi, P.; Hermann, P.; Borbély, J. Clear Guidance to Select the Most Accurate Technologies for 3D Printing Dental Models – A Network Meta-Analysis✰. Journal of Dentistry 2023, 134, 104532. [Google Scholar] [CrossRef] [PubMed]
- Layani, M.; Wang, X.; Magdassi, S. Novel Materials for 3D Printing by Photopolymerization. Adv Mater 2018, 30, e1706344. [Google Scholar] [CrossRef]
- Patpatiya, P.; Chaudhary, K.; Shastri, A.; Sharma, S. A Review on Polyjet 3D Printing of Polymers and Multi-Material Structures. Proceedings of the Institution of Mechanical Engineers, Part C: Journal of Mechanical Engineering Science 2022, 236, 7899–7926. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Espera, A.H.; Chen, Q.; Advincula, R.C. Mechanical Characterization of 3D-Printed Polymers. Additive Manufacturing 2018, 20, 44–67. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).