1. Introduction
Obstructive Sleep Apnea (OSA) is a growing health concern involving about one billion people worldwide; it is characterized by episodes of vibration and collapse of upper airways during sleep resulting in noise production (snoring), airflow decreasing (hypopnea) or cessation (apnea), oxygen desaturations, fragmentation of sleep, daytime sleepiness [
1]. The first-line treatments that are frequently employed in moderate and severe OSA are continuous positive airway pressure (CPAP) and/or mandibular advancement device (MAD) [
2,
3]; however failure in long-term adherence to both treatments was reported in 25–50% of cases [
4].These factors led to significant advances in OSA and snoring surgery management over the past few years. In patients who do not tolerate or do not have good results with first lines treatments, OSA surgery is now a viable solution, thanks to newer, less invasive, or morbid treatments that also increase patient compliance [
5]. Among the surgical procedures for OSA treatment, palatopharyngeal surgery is one the most common performed [
6]. To preserve pharyngeal function and improve breathing space, oropharyngeal surgery for OSA has progressed from a significant removal of "redundant" soft tissue (resection techniques) to less invasive reconstruction techniques.
To reduce surgical procedures' invasiveness and increase oropharyngeal stiffness in the last years Vicini et al. [
7] made popular a new suturing technique known as Barbed sutures Pharyngoplasty (BP), which allows a knot-free tissue closure and an uniform distribution of tensile closure force [
8].
BP requires more surgical precision from the surgeon, following precise vectors in a submucosal plane during the procedure [
9].
Generally, the surgeon illuminates the operating field with his conventional headlight (photophore), but often this is not enough to achieve an optimal and uniform illumination of the entire surgical area. In addition, due to the depth of the oral cavity and often the narrow mouth of patients, it is difficult for trainees to correctly view all the steps of surgical procedures performed by the first surgeon.
In transoral surgical procedures the surgeon is often forced to assume uncomfortable positions for a long time [
10], with difficult exposure of the operating field and poor sharing of the procedure with assistants and trainees [
11].
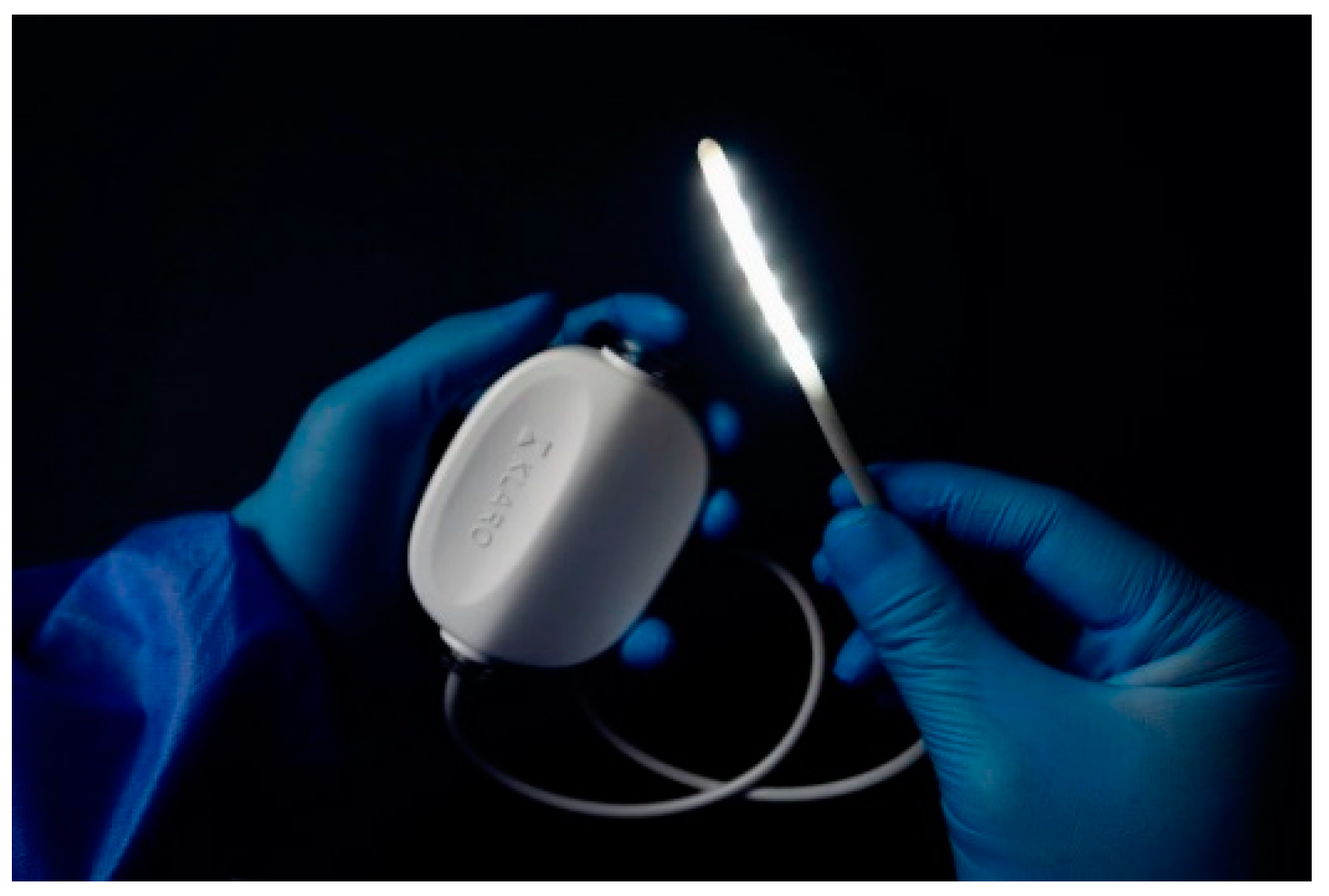
A new device called Klaro
TM (
Figure 1) has been recently introduced to the market for the illumination of anatomical cavities during surgical operations. The Klaro
TM (Vivo Surgical Private Limited, Singapore) is a sterile and disposable surgical lighting device for deep cavities.
This work aims to describe our experience using KlaroTM as an additional illumination tool, especially in BP for OSA, to facilitate surgeon’s work and residents’ learning curve.
2. Materials and Methods
2.1. Patients’ selection
We used the Klaro™ device in 15 consecutives patients (13 males, 2 females; median age 49,1±9,87 years old) affected by moderate-severe obstructive OSA, who underwent BP at the Unit of Integrated Therapies in Otolaryngology at Campus Bio-Medico University Hospital Foundation from January to May 2022.
The inclusion criteria were OSA patients older than 18 years old, with a confirmed circular palatal collapse at drug-induced sleep endoscopy assessment, who refused or did not tolerate nasal CPAP therapy as first-line treatment. Furthermore, all the patients enrolled in the study showed good nasal patency, small tonsils (tonsil size 1 and 2 according to Friedman Staging System), BMI less than 30 kg/m2, and ASA < 2. Patients with age more than 70-year-old, with severe medical comorbidities, Mallampati grade IV were excluded from the study.
2.2. Surgical Procedure
The surgical technique used was Alianza Barbed Pharyngoplasty. It is performed under general anesthesia with orotracheal intubation; the patient is placed in supine position, and a Boyle-Davis mouth gag is used to expose the oropharynx.
It uses barbed absorbable sutures that allow suspending palato-pharyngeal structures to anatomical non-collapsible landmarks (posterior nasal spine, pterigoideal hamulus, pterigomandibular raphe) [
12].
We used two interlaced unidirectional barbed threads (Medtronic V-Loc™ 180, size 2–0 or 3–0, length 30 cm, mounted on taper-pointed 26-mm semicircular needle, absorption in 180 days, tensile strength 65% at 21 days) to obtain a bidirectional suture: each needle is passed in the looped-end of the other suture, then gentle traction is applied to tighten a “flat knot.”
To prevent the two looped ends left protruding in the oral cavity a tiny (3 mm) incision in the mucosa over the Posterior Nasal Spine (PNS) is made sink them in.(8)
2.3. The illumination device
The Klaro™ consists of a flexible high-intensity LEDs bar that can be bent by the user so that it conforms to the shape of the retractor blade to provide optimum stability during the procedure.
It is powered by a battery pack that can be attached to the surgical drapes and guarantees autonomy of 4 hours. The Klaro™ is characterized by four lighting intensity adjustable levels, wide-angle lighting (from 155° when it is unbent to 340° when bent), and it maintains a safe working temperature under 38°C throughout the 4 hours of use. The Klaro™ is registered and approved in several international territories, including the US FDA, European Union’s (EU) CE Mark, and Singapore’s Health Science Authority (HSA).
2.4. Mounting the KlaroTM device on tongue retractor
The device is provided with 4 Retractor Loops and 2 Mini Retractor Loops that enable the user to fasten the Klaro™ LED strip easily and quickly onto most surgical retractors in the market (
Figure 2).
2.5. Study Design
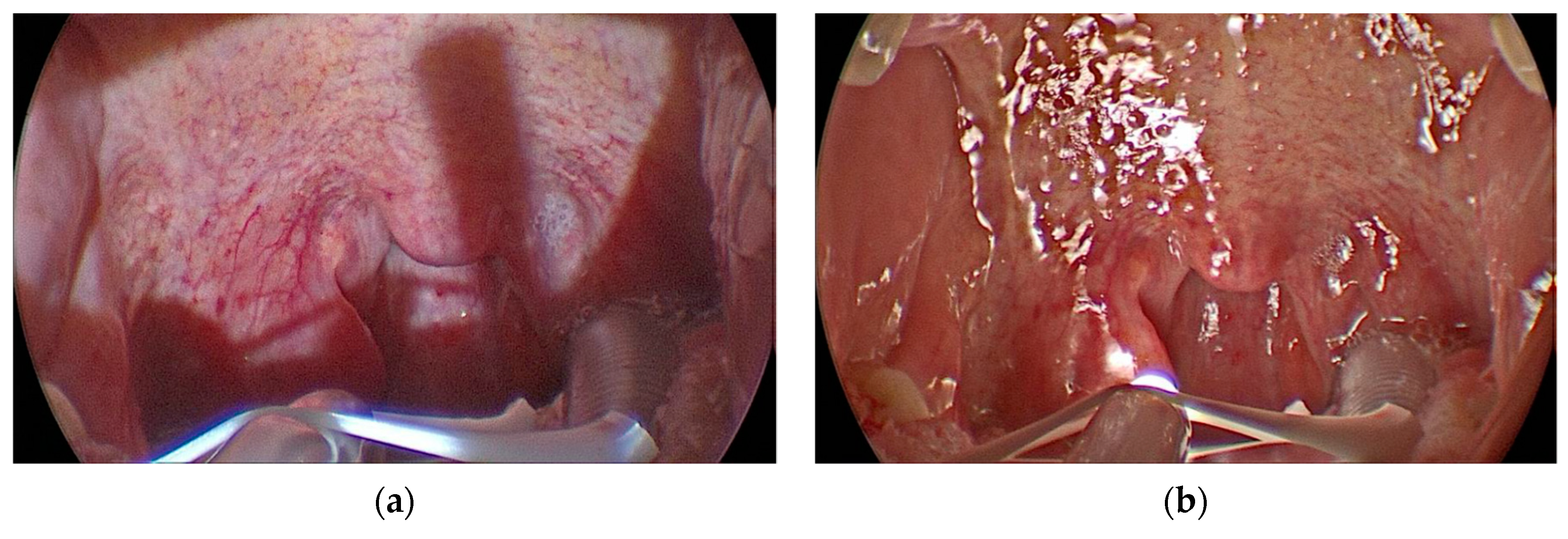
On each patient, the procedure was performed by an expert surgeon: on one half of the palate with the headlamp and the other half with Klaro
TM illumination system; the residents attended the surgical procedures, which were filmed with a 70° rigid endoscope and transmitted on the screen (
Figure 3A,B).
For the illumination system evaluation, we asked both the first surgeon and residents about the quality of vision of critical structures (Uvula, Posterior Pharyngeal Wall, Palatopharyngeus muscle, penetration and exit point of the needle, and Needle tip), grading it with a score from 1 to 3 (1 = poor vision, 2 = moderate vision, 3 = good vision).
2.6. Statistical analysis
The comparison between KlaroTM and headlamp was made using a Wilcoxon’s signed rank sum test. Statistical significance was set at a p-value < 0.05, and the data were analysed using R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Intraoperative quality of visualization of anatomical structures according to the surgeon: headlamp vs KlaroTM
The quality of visualization was statistically significantly better with Klaro
TM versus Headlamp identifying the palatopharyngeal muscle fibers at the bottom of the tonsillar fossa, allowing to perform delicate manoeuvres such as entry and exit with the needle at the same point. No significant differences were reported for the visualization of the posterior pharyngeal wall and uvula (
Table 1).
3.2. Intraoperative quality of visualization of anatomical structures according to the residents: headlamp vs KlaroTM
The quality of visualization on the screen was statistically significantly better with Klaro
TM versus Headlamp to identify the fibres of the palatopharyngeal muscle and to recognize the entrance and exit point of the sutures and the needle tip (
Table 2). The uniformity of vision and the absence of shadows on the screen during the use of Klaro
TM made the image more uniform and enjoyable (Fig 3 A,B). Also, the residents did not report significant differences for the visualization of posterior pharyngeal wall and uvula.
4. Conclusions
The KLAROTM lighting system is a good and comfortable illumination device for oropharyngeal surgery that improves the surgeon’s ergonomics, providing a better visualization for observers learning of surgical procedures; the uniform illumination device allows to identify the anatomical landmarks performing barbed pharyngoplasty accurately.
The KLAROTM lighting system is easily adaptable to the retractors thanks to its flexibility and adequate hooking systems, even if sometimes, especially in patients with Mallampati IV and/or reduced mouth opening can be cumbersome. Our experience with KLAROTM is focused on barbed pharyngoplasty for OSA, but we encourage to use of KlaroTM in all oral and pharyngeal surgeries, including tonsillectomy and oncological surgery.
Author Contributions
Conceptualization, M.C. and L.S.; methodology, L.S, A.M., F.I; formal analysis, L.G., F.I.; investigation, F.I., A.M, S.D.G., L.S., L.D.B.; data curation, L.G, F.I..; writing—original draft preparation, A.M., F.I., L.S.; writing—review and editing, L.D.B., L.S., A.D.V., P.B.; visualization, A.D.V., P.B., C.V., M.C.; supervision, A.D.V., P.B., C.V., M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Not applicable
Data Availability Statement
All data generated or analysed during this study are included in this published article.
Acknowledgments
The KLAROTM was presented at the 3rd and 4th editions of the “Course on surgical innovations and new technologies in obstructive sleep apnea and snoring in the era of precision medicine” organized by the Unit of Integrated Therapies in Otolaryngology of Fondazione Policlinico Campus Bio-Medico of Rome. It was also used during the live surgeries of the same course.
Conflicts of Interest
The authors declare no conflict of interest
References
- Mantovani, M., Minetti, A., Torretta, S., Pincherle, A., Tassone, G., and Pignataro, L.: ‘The "Barbed Roman Blinds" technique: a step forward’, Acta Otorhinolaryngol Ital, 2013, 33, (2), pp. 128.
- Patil, S.P., Ayappa, I.A., Caples, S.M., Kimoff, R.J., Patel, S.R., and Harrod, C.G.: ‘Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline’, J Clin Sleep Med, 2019, 15, (2), pp. 335-343. [CrossRef]
- Ramar, K., Dort, L.C., Katz, S.G., Lettieri, C.J., Harrod, C.G., Thomas, S.M., and Chervin, R.D.: ‘Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015’, J Clin Sleep Med, 2015, 11, (7), pp. 773-827. [CrossRef]
- Chiu, F.H., Chen, C.Y., Lee, J.C., and Hsu, Y.S.: ‘Effect of Modified Uvulopalatopharyngoplasty without Tonsillectomy on Obstructive Sleep Apnea: Polysomnographic Outcome and Correlation with Drug-Induced Sleep Endoscopy’, Nat Sci Sleep, 2021, 13, pp. 11-19. [CrossRef]
- Kent, D., Stanley, J., Aurora, R.N., Levine, C., Gottlieb, D.J., Spann, M.D., Torre, C.A., Green, K., and Harrod, C.G.: ‘Referral of adults with obstructive sleep apnea for surgical consultation: an American Academy of Sleep Medicine clinical practice guideline’, J Clin Sleep Med, 2021, 17, (12), pp. 2499-2505. [CrossRef]
- Sheen, D., and Abdulateef, S.: ‘Uvulopalatopharyngoplasty’, Oral Maxillofac Surg Clin North Am, 2021, 33, (2), pp. 295-303. [CrossRef]
- Vicini, C., Meccariello, G., Montevecchi, F., De Vito, A., Frassineti, S., Gobbi, R., Pelucchi, S., Iannella, G., Magliulo, G., and Cammaroto, G.: ‘Effectiveness of barbed repositioning pharyngoplasty for the treatment of obstructive sleep apnea (OSA): a prospective randomized trial’, Sleep Breath, 2020, 24, (2), pp. 687-694. [CrossRef]
- Casale, M., Moffa, A., Giorgi, L., Sabatino, L., Pierri, M., Lugo, R., Baptista, P., and Rinaldi, V.: ‘No-cutting remodelling intra-pharyngeal surgery can avoid CPAP in selected OSA patients: myth or reality?’, Eur Arch Otorhinolaryngol, 2022, 279, (10), pp. 5039-5045. [CrossRef]
- Gulotta, G., Iannella, G., Meccariello, G., Cammaroto, G., Visconti, I.C., de Vincentiis, M., Greco, A., Pelucchi, S., Magliulo, G., Ruoppolo, G., Maniaci, A., Cocuzza, S., La Mantia, I., De Vito, A., Abita, P., and Vicini, C.: ‘Barbed suture Extrusion and Exposure in palatoplasty for OSA: What does it mean?’, Am J Otolaryngol, 2021, 42, (4), pp. 102994. [CrossRef]
- Sahni, D.: ‘Is there an Increased Incidence of Cervical Degenerative Disease in Surgeons who use Loupes and a Headlight?’, Journal of spine surgery 2015, 4, (5). [CrossRef]
- Festa, B.M., Zuppardo, J., Costantino, A., Ferreli, F., Spriano, G., Mercante, G., and De Virgilio, A.: ‘High-definition 3D exoscope-assisted tonsillectomy’, Am J Otolaryngol, 2022, 44, (1), pp. 103674. [CrossRef]
- Moffa, A., Rinaldi, V., Mantovani, M., Pierri, M., Fiore, V., Costantino, A., Pignataro, L., Baptista, P., Cassano, M., and Casale, M.: ‘Different barbed pharyngoplasty techniques for retropalatal collapse in obstructive sleep apnea patients: a systematic review’, Sleep Breath, 2020, 24, (3), pp. 1115-1127.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).