Submitted:
03 August 2023
Posted:
07 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
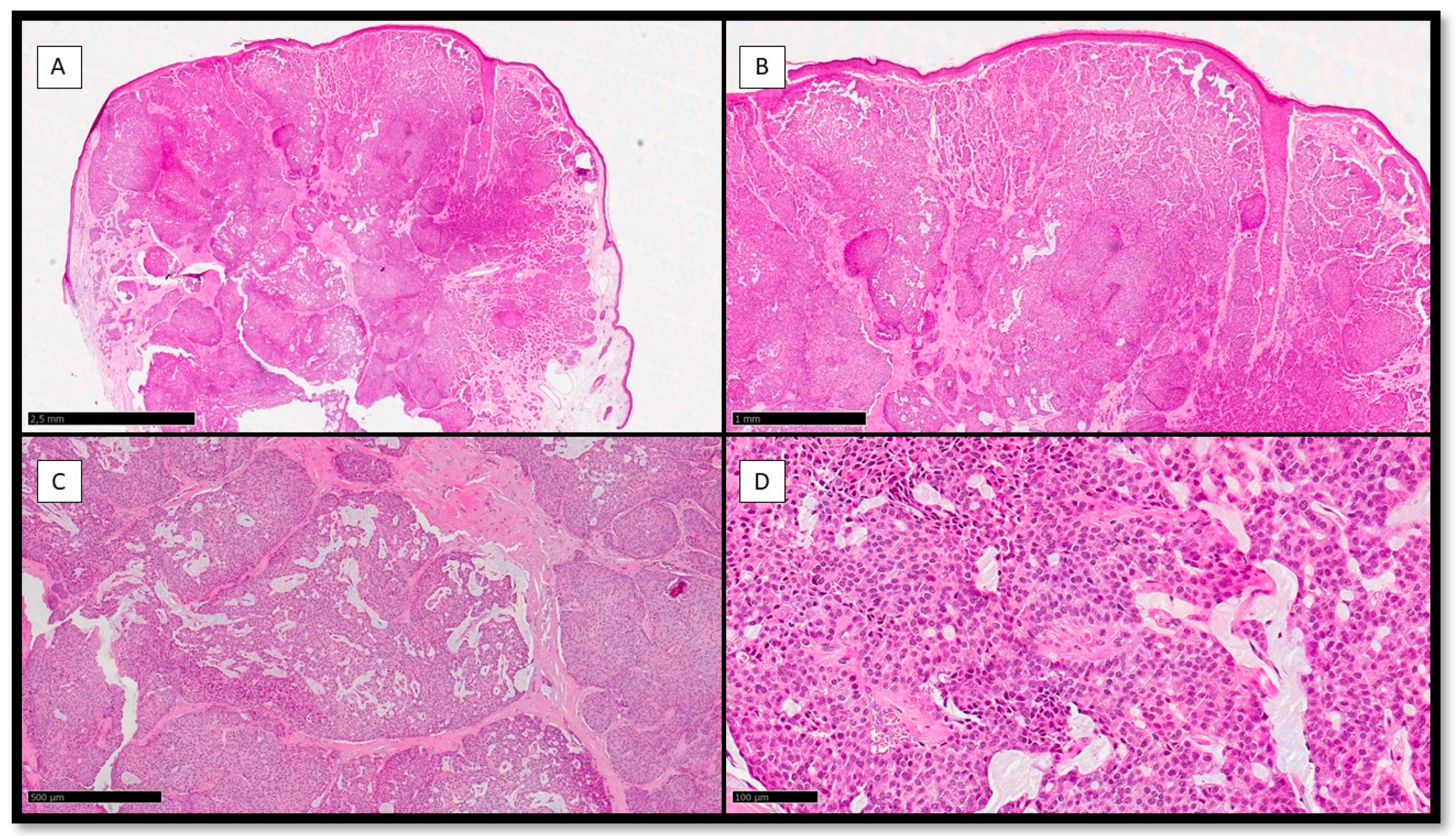
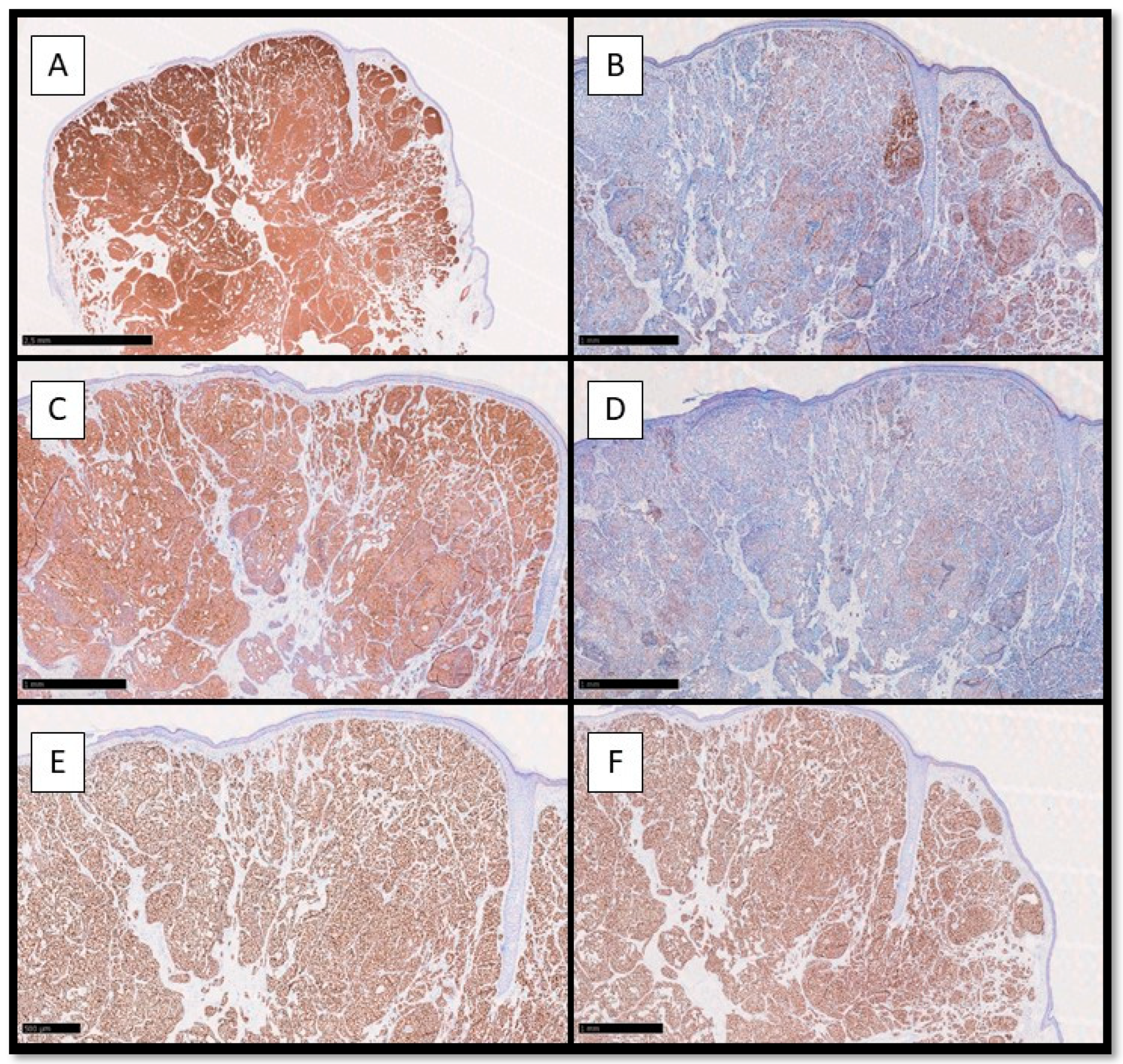
2. Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
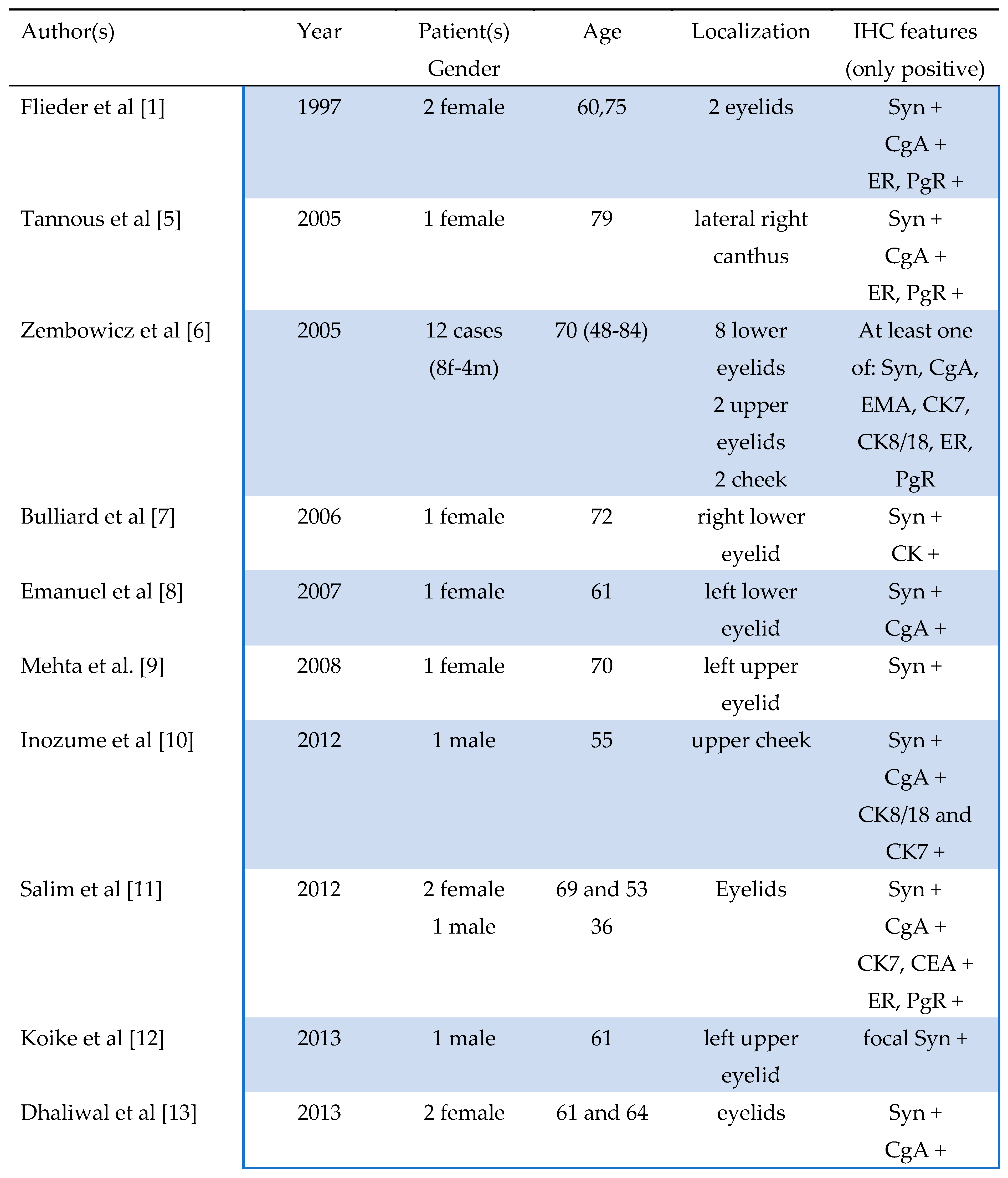
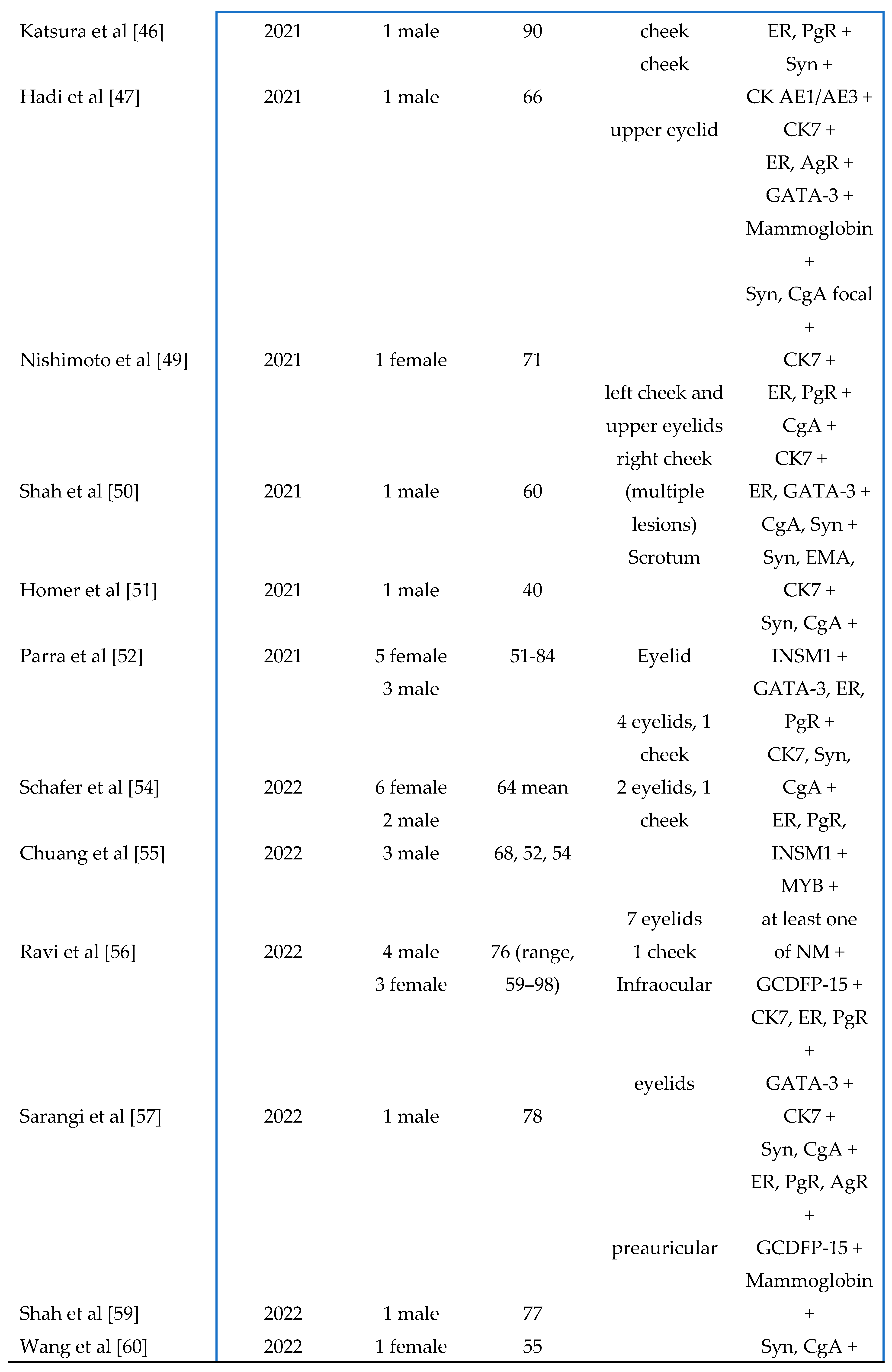
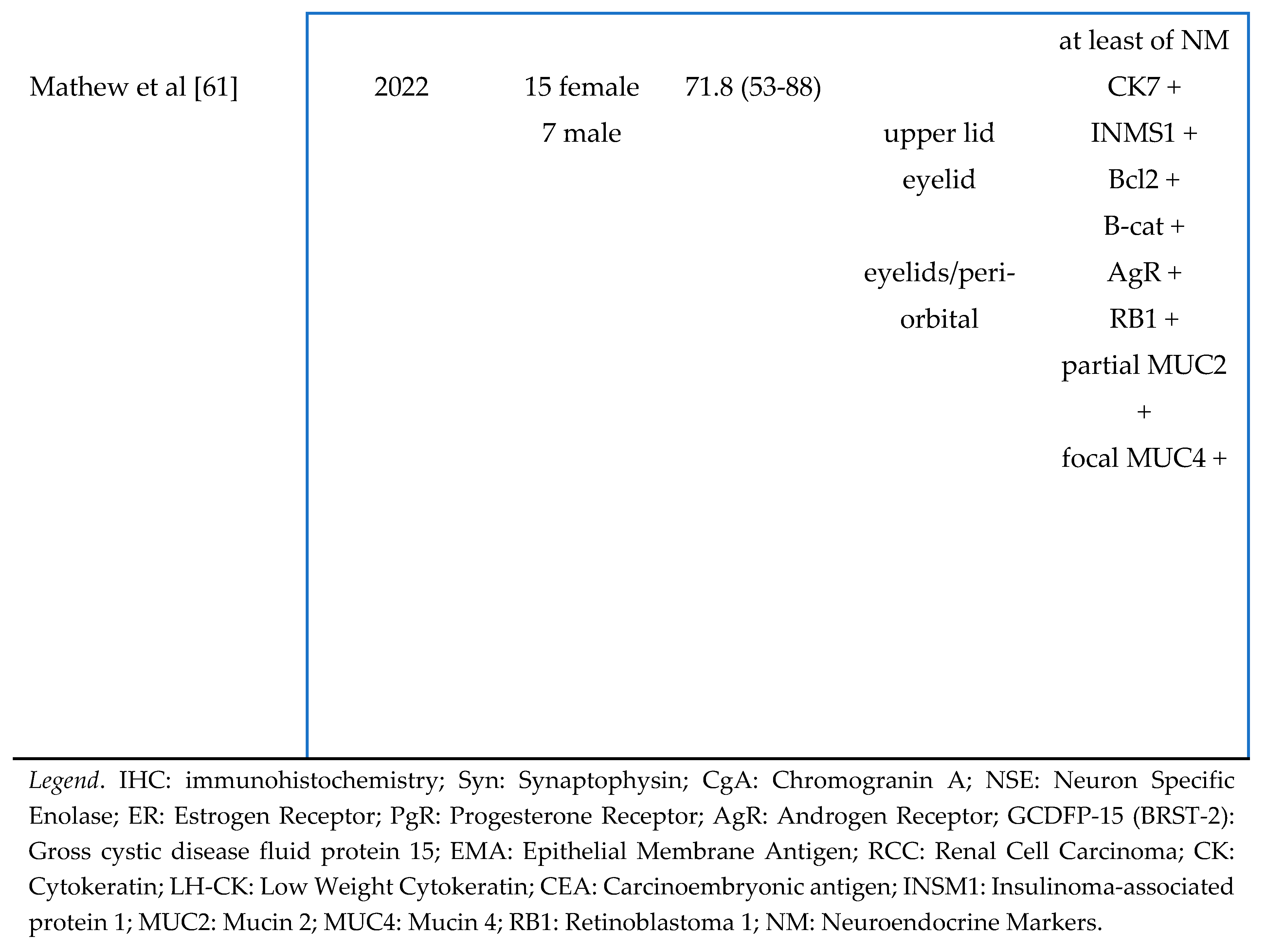
- Flieder, A.; Koerner, F.C.; Pilch, B.Z.; Maluf, H.M. Endocrine Mucin-Producing Sweat Gland Carcinoma. Am. J. Surg. Pathol. 1997, 21, 1501–1506. [Google Scholar] [CrossRef]
- Elder, D.; Massi, D.; Scolyer, A.; Willemze, R. WHO Classification of Skin Tumours, 2018, IARC, (pp. 168-169).
- Requena, L.; Sangueza, O. Cutaneous Adnexal Neoplasms, 2017, Springer International Publishing Switzerland.
- Tsai, J.-H.; Hsiao, T.-L.; Chen, Y.-Y.; Hsiao, C.-H.; Liau, J.-Y. Endocrine mucin-producing sweat gland carcinoma occurring on extra-facial site: a case report. J. Cutan. Pathol. 2014, 41, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Tannous, Z.S.; Avram, M.M.; Zembowicz, A.; Mihm, M.C.; Liteplo, M.; Kwan, T.; Olbricht, S.M. Treatment of Synchronous Mucinous Carcinoma and Endocrine Mucin-Producing Sweat Gland Carcinoma with Mohs' Micrographic Surgery. Dermatol. Surg. 2006, 31, 364–367. [Google Scholar] [CrossRef] [PubMed]
- Zembowicz, A.; Garcia, C.F.; Tannous, Z.S.; Mihm, M.C.; Koerner, F.; Pilch, B.Z. Endocrine Mucin-Producing Sweat Gland Carcinoma. Am. J. Surg. Pathol. 2005, 29, 1330–1339. [Google Scholar] [CrossRef]
- Bulliard, C.; Murali, R.; Maloof, A.; Adams, S. Endocrine mucin-producing sweat gland carcinoma: report of a case and review of the literature. J. Cutan. Pathol. 2006, 33, 812–816. [Google Scholar] [CrossRef]
- Emanuel, P.O.; de Vinck, D.; Waldorf, H.A.; Phelps, R.G. Recurrent endocrine mucin–producing sweat gland carcinoma. Ann. Diagn. Pathol. 2007, 11, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Thiagalingam, S.; Zembowicz, A.; Hatton, M.P. Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid. Ophthalmic Plast. Reconstr. Surg. 2008, 24, 164–165. [Google Scholar] [CrossRef]
- Inozume, T.; Kawasaki, T.; Harada, K.; Tanaka, K.; Kawamura, T.; Shibagaki, N.; Katoh, R.; Shimada, S. A case of endocrine mucin-producing sweat gland carcinoma. Pathol. Int. 2012, 62, 344–346. [Google Scholar] [CrossRef]
- Salim, A.A.; Karim, R.Z.; McCarthy, S.W.; Scolyer, R.A. Endocrine mucin producing sweat gland carcinoma: a clinicopathological analysis of three cases. Pathology 2012, 44, 568–571. [Google Scholar] [CrossRef]
- Koike, T.; Mikami, T.; Maegawa, J.; Iwai, T.; Wada, H.; Yamanaka, S. Recurrent endocrine mucin-producing sweat gland carcinoma in the eyelid. Australas. J. Dermatol. 2012, 54, e46–e49. [Google Scholar] [CrossRef]
- Dhaliwal, C.A.; Torgersen, A.; Ross, J.J.; Ironside, J.W.; Biswas, A. Endocrine Mucin-Producing Sweat Gland Carcinoma. Am. J. Dermatopathol. 2013, 35, 117–124. [Google Scholar] [CrossRef] [PubMed]
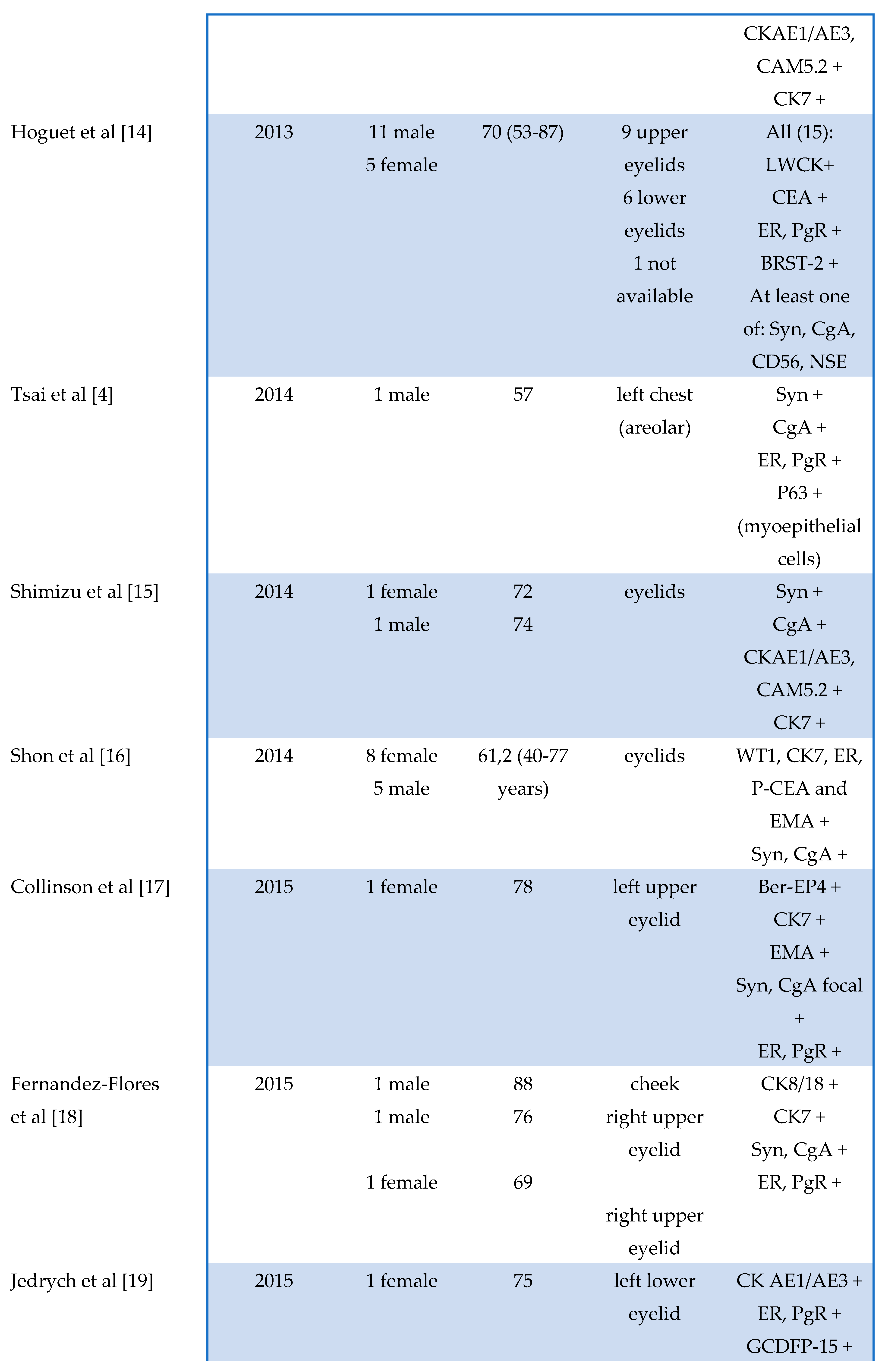
- Hoguet, A.; Warrow, D.; Milite, J.; McCormick, S.A.; Maher, E.; DellaRocca, R.; DellaRocca, D.; Goldbaum, A.; Milman, T. Mucin-producing Sweat Gland Carcinoma of the Eyelid: Diagnostic and Prognostic Considerations. Arch. Ophthalmol. 2013, 155, 585–592. [Google Scholar] [CrossRef]
- Shimizu, I.; Dufresne, R.; Robinson-Bostom, L. Endocrine mucin-producing sweat gland carcinoma. Cutis 2014, 93. [Google Scholar]
- Shon, W.; Salomão, D.R. WT1 expression in endocrine mucin-producing sweat gland carcinoma: a study of 13 cases. Int. J. Dermatol. 2014, 53, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
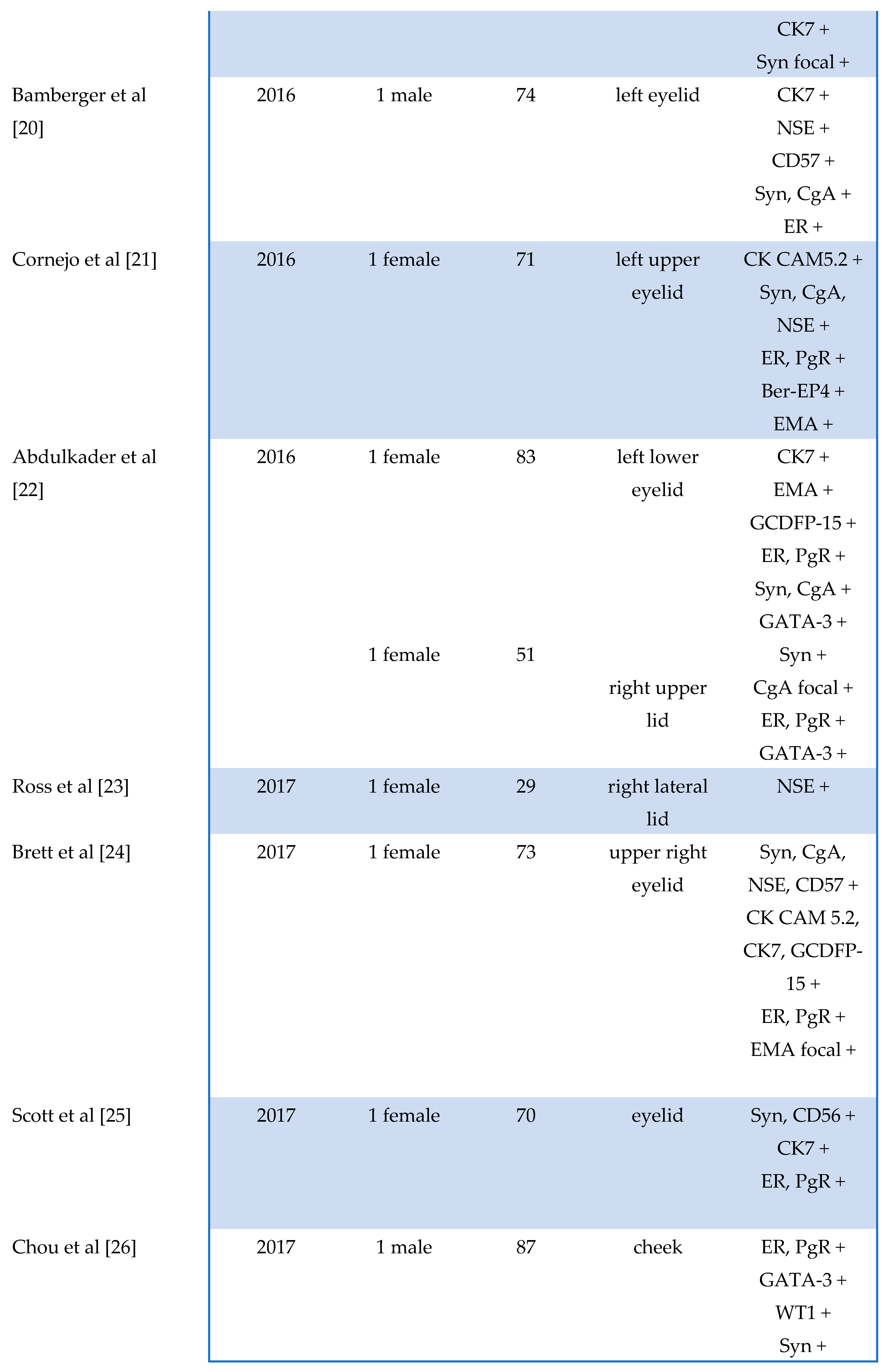
- Collinson, A.C.; Sun, M.T.; James, C.; Huilgol, S.C.; Selva, D. Endocrine mucin-producing sweat gland carcinoma of the eyelid. Int. Ophthalmol. 2015, 35, 883–886. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Flores, A.; Cassarino, D.S. Endocrine mucin-producing sweat gland carcinoma: a study of three cases and CK8, CK18 and CD5/6 immunoexpression. J. Cutan. Pathol. 2015, 42, 578–586. [Google Scholar] [CrossRef]
- Jedrych, J.; Jones, M.; Seethala, R.; Ho, J. Primary Cutaneous Endocrine Mucin–Producing Sweat Gland Carcinoma Co-occurring Simultaneously With Low-Grade Ductal Mucinous Breast Cancer. Am. J. Dermatopathol. 2015, 37, 425–427. [Google Scholar] [CrossRef]
- Bamberger, M.; Medline, P.; Cullen, J.B.; Gill, H. Histopathology of endocrine mucin-producing sweat gland carcinoma of the eyelid. Can. J. Ophthalmol. 2016, 51, e72–e75. [Google Scholar] [CrossRef]
- Cornejo, K.M.; Hutchinson, L.; Meng, X.; O'Donnell, P.; Deng, A. Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid: A Report of a Case With Molecular Analysis. Am. J. Dermatopathol. 2016, 38, 636–638. [Google Scholar] [CrossRef]
- Abdulkader, M.; Kuhar, M.; Hattab, E.; Linos, K. GATA3 Positivity in Endocrine Mucin-Producing Sweat Gland Carcinoma and Invasive Mucinous Carcinoma of the Eyelid: Report of 2 Cases. Am. J. Dermatopathol. 2016, 38, 789–791. [Google Scholar] [CrossRef]
- Ross, A.G.; Chan, A.A.; Mihm, M.C.; Yu, J.Y. Endocrine Mucin-Producing Sweat Gland Carcinoma: An Uncommon Presentation. Semin. Ophthalmol. 2016, 32, 511–513. [Google Scholar] [CrossRef] [PubMed]
- Brett, M.A.; Salama, S.; Gohla, G.; Alowami, S. Endocrine Mucin-Producing Sweat Gland Carcinoma, a Histological Challenge. Case Rep. Pathol. 2017, 2017, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.L.; Anyanwu, C.O.; Vandergriff, T.; Nijhawan, R.I. Endocrine Mucin–Producing Sweat Gland Carcinoma Treated With Mohs Micrographic Surgery. Dermatol. Surg. 2017, 43, 1498–1500. [Google Scholar] [CrossRef] [PubMed]
- Chou, Y.-H.; Chang, Y.-C.; Huang, Y.-L.; Wu, C.-T. Endocrine mucin-producing sweat gland carcinoma with GATA3 expression: report of two cases. Pathology 2017, 49, 805–808. [Google Scholar] [CrossRef]
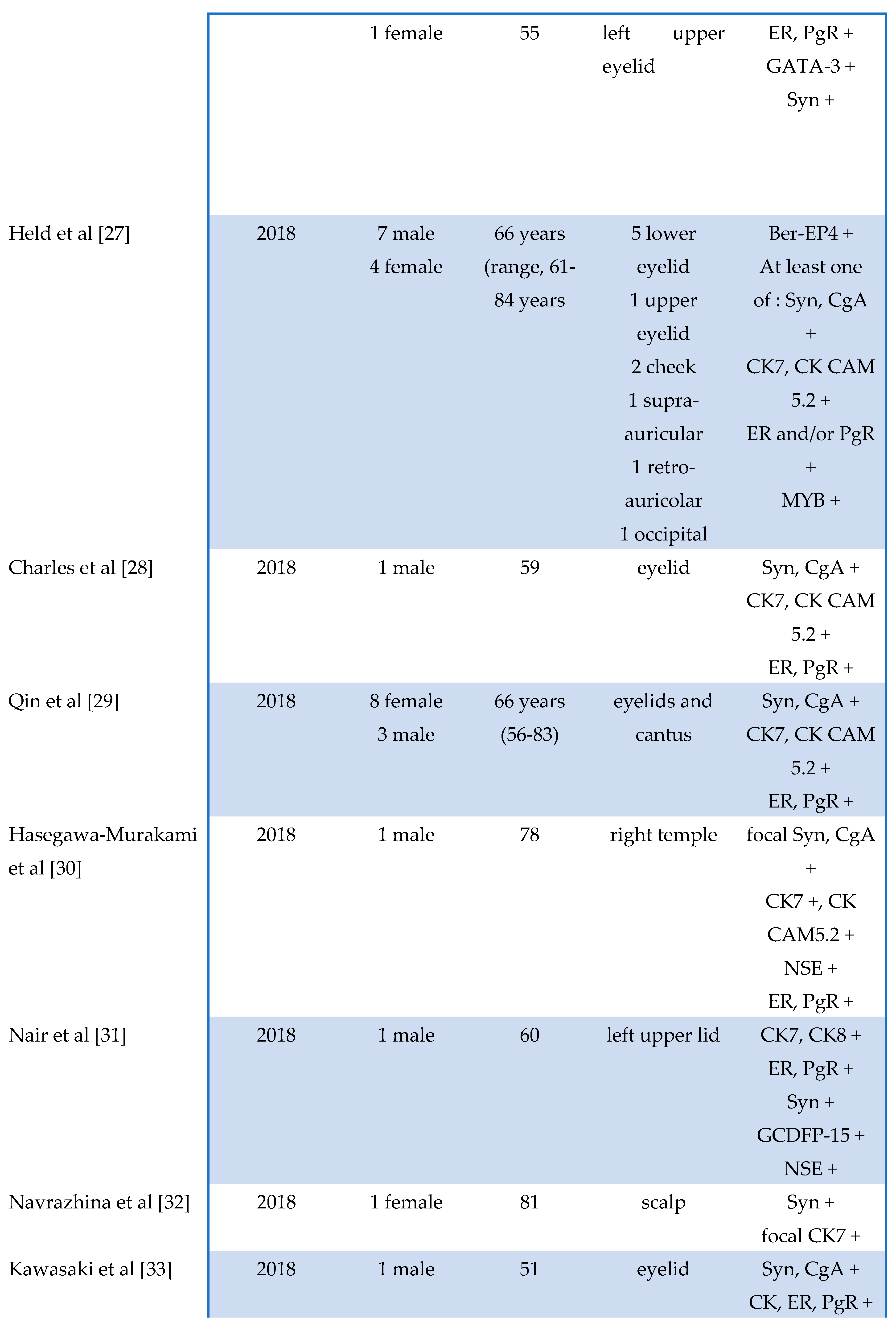
- Held, L.; Ruetten, A.; Kutzner, H.; Palmedo, G.; John, R.; Mentzel, T. Endocrine mucin-producing sweat gland carcinoma: Clinicopathologic, immunohistochemical, and molecular analysis of 11 cases with emphasis on MYB immunoexpression. J. Cutan. Pathol. 2018, 45, 674–680. [Google Scholar] [CrossRef]
- Charles, N.C.; Proia, A.D.; Lo, C. Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid Associated With Mucinous Adenocarcinoma. Ophthalmic Plast. Reconstr. Surg. 2018, 34, e37–e38. [Google Scholar] [CrossRef]
- Qin, H.; Moore, R.F.; Ho, C.-Y.; Eshleman, J.; Eberhart, C.G.; Cuda, J. Endocrine mucin-producing sweat gland carcinoma: A study of 11 cases with molecular analysis. J. Cutan. Pathol. 2018, 45, 681–687. [Google Scholar] [CrossRef]
- Hasegawa-Murakami, Y.; Kono, M.; Yokota, K.; Inaba, H.; Fukumoto, T.; Akiyama, M. Dermoscopic features of endocrine mucin-producing sweat gland carcinoma. J. Dermatol. 2017, 45, 353–356. [Google Scholar] [CrossRef]
- Nair, A.G.; Bhargava, R.; Furniturewala, A.U. Endocrine mucin-producing sweat gland carcinoma of the eyelid: A clinical and histological conundrum. Indian J. Ophthalmol. 2018, 66, 1042–1044. [Google Scholar] [CrossRef]
- Navrazhina, K.; Petukhova, T.; Wildman, H.F.; Magro, C.M.; Minkis, K. Endocrine mucin-producing sweat gland carcinoma of the scalp treated with Mohs micrographic surgery. JAAD Case Rep. 2018, 4, 887–889. [Google Scholar] [CrossRef]
- Kawasaki, T.; Kubota, T.; Ichihara, S.; Horibe, K.; Hasebe, T. Neuroendocrine cells associated with endocrine mucin-producing sweat gland carcinoma: a potential precursor lesion? Pathology 2018, 50, 573–575. [Google Scholar] [CrossRef] [PubMed]
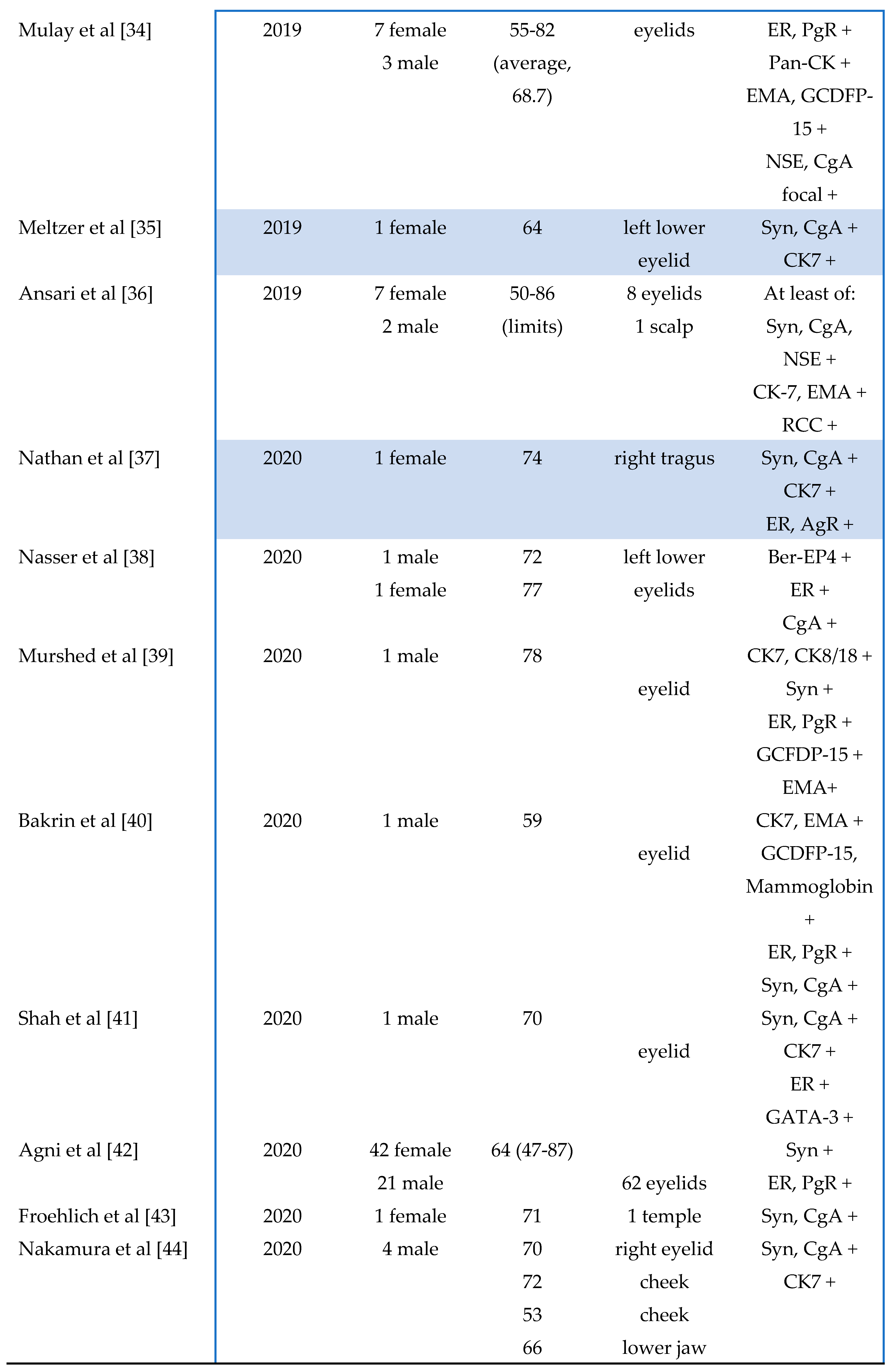
- Mulay, K.; Menon, V.; Lahane, S.; Sharma, M.; Honavar, S. Endocrine mucin-producing sweat gland carcinoma (EMPSGC) of the eyelid: Clinicopathologic features, immunohistochemical findings and review of literature. Indian J. Ophthalmol. 2019, 67, 1374–1377. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, O.A.; Joseph, J.M. Delayed treatment of endocrine mucin–producing sweat gland carcinoma initially diagnosed as a chalazion. JAAD Case Rep. 2019, 5, 789–791. [Google Scholar] [CrossRef] [PubMed]
- Ansari, A.N.; Bobos, M.; Shih, S.; Chen, M.C.-C.; Ardakani, N.M.; Rosales, C.M.; Chen, C.-J.; Savage, C.; Bracey, T.; McKee, P.H.; et al. Renal Cell Carcinoma Antigen Expression in Primary Cutaneous Endocrine Mucinous Carcinomas: A Case Series of 14 Patients and Review of the Literature. Am. J. Dermatopathol. 2019, 41, 571–577. [Google Scholar] [CrossRef]
- Nathan, N.R.; Emerick, K.S.; Hoang, M.P.; Smith, G.P.; Yancovitz, M. Perineural and Vascular Invasion in an Endocrine Mucin-Producing Sweat Gland Carcinoma of the Ear with Associated Mucinous Carcinoma. Dermatopathology 2020, 6, 271–274. [Google Scholar] [CrossRef]
- Nasser, H.; Siddiqui, S. Endocrine Mucin–Producing Sweat Gland Carcinoma: Two New Eyelid Cases and Review of the Literature. Int. J. Surg. Pathol. 2020, 28, 653–657. [Google Scholar] [CrossRef]
- Murshed, K.A.; Ben-Gashir, M. A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma: Is it Still an Under-Recognized Entity? Case Rep. Dermatol. 2020, 12, 255–261. [Google Scholar] [CrossRef]
- Bakrin, I.H.; Rajaintharan, P.S.; Tawil, Z.; Mahayidin, H. Endocrine mucin-producing sweat gland carcinoma - newly described skin appendageal tumours. . 2020, 42, 111–114. [Google Scholar]
- Shah, S.; Parekh, P.; Rodriguez, M. Endocrine Mucin-Producing Sweat Gland Carcinoma in an Elderly Man. Am. J. Dermatopathol. 2020, 42, 153–155. [Google Scholar] [CrossRef]
- Agni, M.; Raven, M.L.D.; Bowen, R.C.; Laver, N.V.; Chevez-Barrios, P.; Milman, T.; Eberhart, C.G.; Couch, S.; Bennett, D.D.; Albert, D.M.; et al. An Update on Endocrine Mucin-producing Sweat Gland Carcinoma. Am. J. Surg. Pathol. 2020, 44, 1005–1016. [Google Scholar] [CrossRef]
- Froehlich, M.B.; Cook, J.; Bruner, E.; Stalcup, S.; Patel, K.; Day, T. Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid With Locoregional Metastasis to the Parotid Gland. Dermatol. Surg. 2020, 46, 1116–1118. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Sakurai, M.; Ozawa, H.; Morita, A. Four male cases of endocrine mucin-producing sweat gland carcinoma: Specific gender differences in East Asia. Kaohsiung J. Med Sci. 2020, 36, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Au, R.T.M.; Bundele, M.M. Endocrine mucin-producing sweat gland carcinoma and associated primary cutaneous mucinous carcinoma: Review of the literature. J. Cutan. Pathol. 2021, 48, 1156–1165. [Google Scholar] [CrossRef]
- Katsura, Y.; Sasaki, A.; Minagawa, D.; Kato, I.; Ueda, T. Endocrine mucin-producing sweat gland carcinoma of the cheek. Dermatol. Online J. 2021, 27. [Google Scholar] [CrossRef]
- Hadi, R.; Xu, H.; Barber, B.R.; Shinohara, M.M.; Moshiri, A.S. A case of endocrine mucin-producing sweat gland carcinoma with distant metastasis. J. Cutan. Pathol. 2021, 48, 937–942. [Google Scholar] [CrossRef] [PubMed]
- Saggini, A.; Cota, C. Local invasion in endocrine mucin-producing sweat gland carcinoma: Still an open issue. J. Cutan. Pathol. 2019, 47, 192–194. [Google Scholar] [CrossRef]
- Nishimoto, A.; Kuwahara, H.; Ohashi, R.; Ansai, S. Multicentric endocrine mucin-producing sweat gland carcinoma and mucinous carcinoma of the skin: A case report. J. Cutan. Pathol. 2020, 48, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Aman, A.; Srinivaas, K.; Gudipati, A.; Chavali, P. Endocrine mucin-producing sweat gland carcinoma of the peno-scrotum with systemic metastases: A rare case report. . 2021, 64, 180–182. [Google Scholar]
- Homer, N.A.; Hoesly, P.M.; Durairaj, V.D. Atypical presentation of an endocrine mucin-producing sweat gland carcinoma of the eyelid. Orbit 2020, 40, 81–82. [Google Scholar] [CrossRef]
- Parra, O.; Linos, K.; Yan, S.; Lilo, M.; LeBlanc, R.E. Comparative performance of insulinoma-associated protein 1 (INSM1) and routine immunohistochemical markers of neuroendocrine differentiation in the diagnosis of endocrine mucin-producing sweat gland carcinoma. J. Cutan. Pathol. 2020, 48, 41–46. [Google Scholar] [CrossRef]
- Froehlich, M.H.; Conti, K.R.; Norris, I.I.; Allensworth, J.J.; Ufkes, N.A.; Nguyen, S.A.; Bruner, E.T.; Cook, J.; Day, T.A. Endocrine mucin-producing sweat gland carcinoma: a systematic review and meta-analysis. J. Dermatol. Treat. 2022, 33, 2182–2191. [Google Scholar] [CrossRef] [PubMed]
- Schafer, C.N.; Hurst, E.A.; Rosman, I.S.; Council, M.L. Endocrine Mucin-Producing Sweat Gland Carcinoma Treated With Mohs Micrographic Surgery. Dermatol. Surg. 2021, 48, 362–364. [Google Scholar] [CrossRef] [PubMed]
- Chuang, I.-C.; Jang, C.-S. Endocrine mucin-producing sweat gland carcinoma: Reappraisal of patient demographics and tumour immunophenotypes. Indian J. Dermatol. Venereol. Leprol. 2022, 88, 544–547. [Google Scholar] [CrossRef]
- Ravi, P.Y.; Walsh, N.M.; Archibald, C.; Pasternak, S. Endocrine Mucin-Producing Sweat Gland Carcinoma: Emerging Evidence of Multicentric Cutaneous Origin and Occasional Concurrence With Analogous Breast Tumors. Am. J. Dermatopathol. 2022, 44, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Sarangi, J.; Konkimalla, A.; Kaur, K.; Sikka, K.; Sen, S.; Kakkar, A. Endocrine Mucin Producing Sweat Gland Carcinoma with Metastasis to Parotid Gland: Not as Indolent as Perceived? Head Neck Pathol. 2021, 16, 331–337. [Google Scholar] [CrossRef]
- Quattrochi, B.; Russell-Goldman, E. Utility of Insulinoma-Associated Protein 1 (INSM1) and Mucin 2 (MUC2) Immunohistochemistry in the Distinction of Endocrine Mucin-Producing Sweat Gland Carcinoma From Morphologic Mimics. Am. J. Dermatopathol. 2021, 44, 92–97. [Google Scholar] [CrossRef]
- Shah, D.S.; Homer, N.A.; Epstein, A.; Durairaj, V.D. Simultaneous presentation of orbital mantle cell lymphoma and endocrine mucin-producing sweat gland carcinoma. Orbit 2021, 41, 509–513. [Google Scholar] [CrossRef]
- Wang, D.; Deng, W.B.; LoBue, S.; Giovinazzo, K.; Rosen, M.; Heilman, E.M.; Hodgson, N.M.M. Bilateral Concurrent Endocrine Mucin-Producing Sweat Gland Carcinoma and Mucinous Carcinoma of the Eyelids. Ophthalmic Plast. Reconstr. Surg. 2022, 38, e96–e99. [Google Scholar] [CrossRef]
- Mathew, J.G.; Bowman, A.S.; Saab, J.; Busam, K.J.; Nehal, K.; Pulitzer, M. Next-generation sequencing analysis suggests varied multistep mutational pathogenesis for endocrine mucin-producing sweat gland carcinoma with comments on INSM1 and MUC2 suggesting a conjunctival origin. J. Am. Acad. Dermatol. 2021, 86, 1072–1079. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





