1. Introduction
An epidural hematoma, which is an accumulation of blood in the spinal canal that puts pressure on the spinal cord, thecal sac, or cauda equina, can lead to neurological issues [
1]. Even though spinal surgeries are the most common cause, epidural hematomas can also arise spontaneously due to injury, blood thinning medication, bleeding from abnormal blood vessels in the spinal cord (like an arteriovenous malformation), epidural steroid injections, or spinal or epidural anesthesia [
2,
3,
4]. Given their potentially disastrous long-term effects, epidural hematomas warrant the attention of all spinal surgeons.
Epidural hematomas, although rare, can be a severe postoperative complication after spinal surgery. The reported incidence of a symptomatic epidural hematoma is less than 1% ranging from 0.10% to 0.69% [
5,
6]. While asymptomatic epidural hematomas are relatively more common postoperatively, symptomatic epidural hematoma mandates immediate attention and appropriate management to avoid untoward long-term complications. Various studies looking into the pharmacological prophylaxis for deep vein thrombosis and pulmonary embolism have reported epidural hematoma rates of less than 1% [
7]. Further, utilization of wound drains has been shown not to prevent the occurrence of epidural hematomas [
8].
The diagnosis of symptomatic postoperative epidural hematoma necessitates a high index of suspicion and is made based on clinical symptoms such as evolving sudden postoperative axial pain in the area of surgery with neurological deficit and urinary retention [
9]. Once such hematoma is suspected, an emergency magnetic resonance imaging (MRI) is done to confirm the diagnosis followed by emergency evacuation of the hematoma within 6-12 hours [
10]. Here, we present the case of post-operative epidural hematoma that was quickly reversed with the help of a conservative technique that prevented revision surgery.
2. Case report
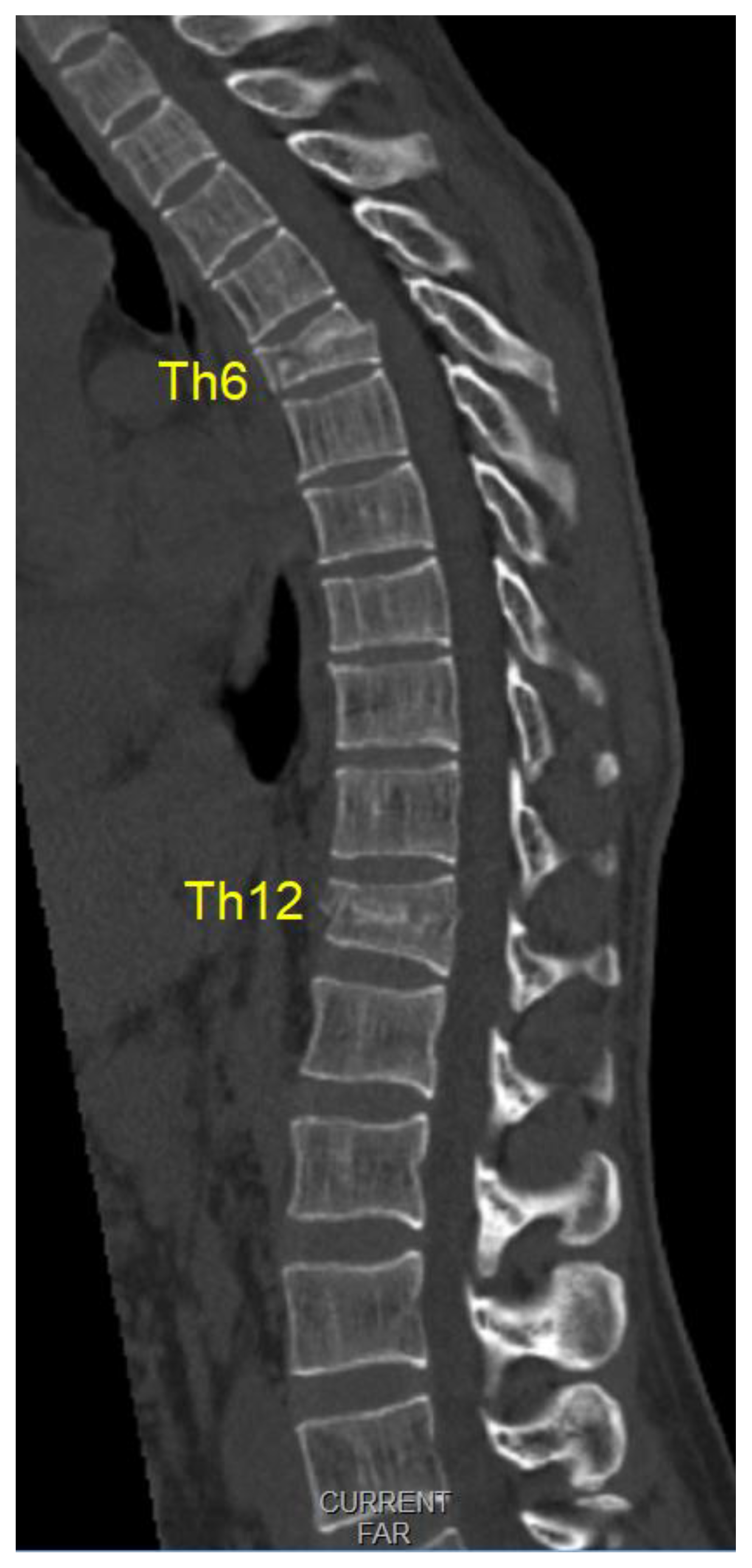
A 36-year-old male patient was admitted to our emergency trauma department with compressive Th6 and Th12 fractures as shown in
Figure 1 sustained from a fall on the head and upper spine onto a soft surface. The initial examination ruled out accompanying head or any organ injury. There were no rib fractures or injuries to the extremities. The patient was neurologically normal upon admission.
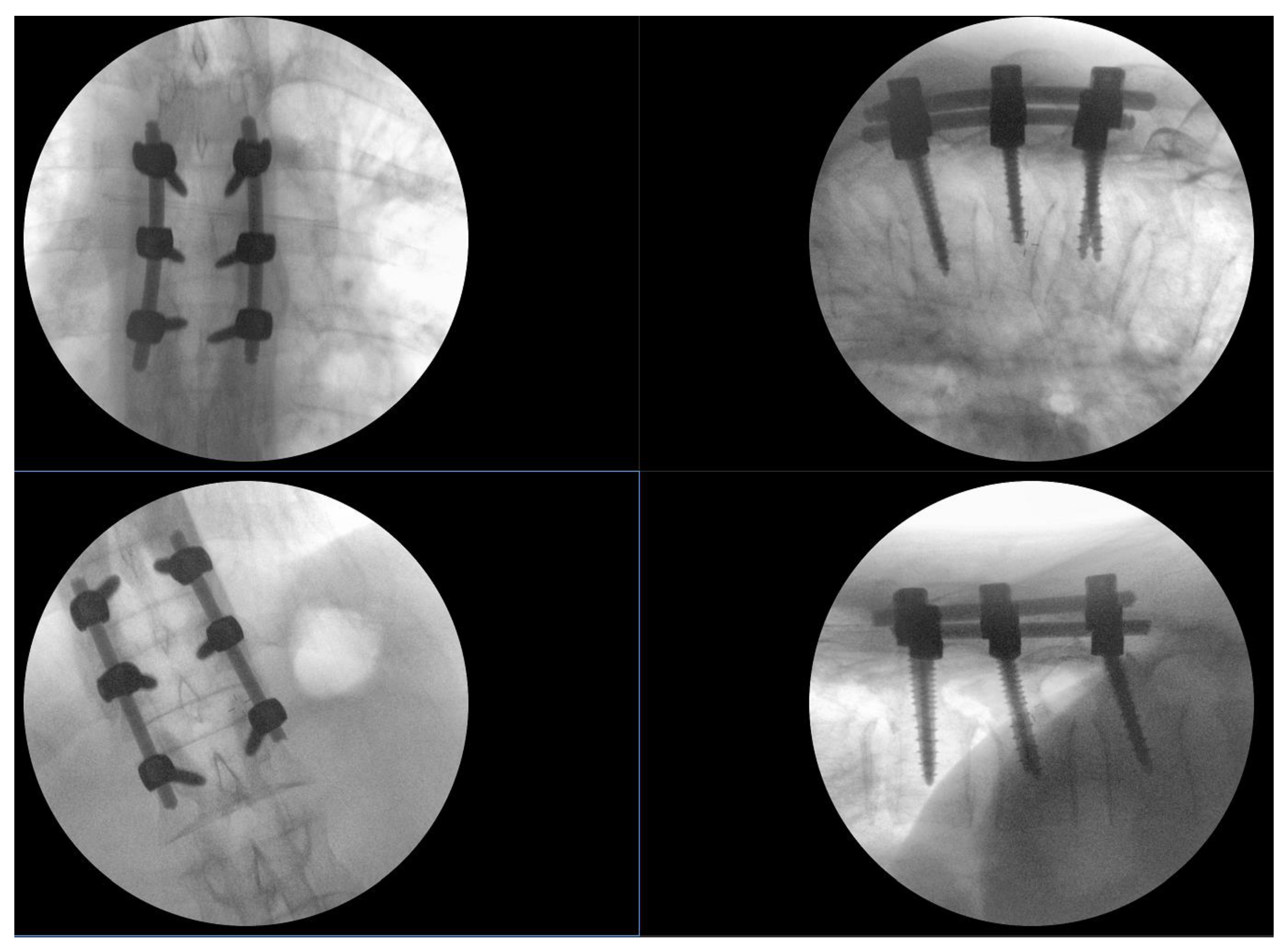
There were no fracture lines through the posterior elements or indirect signs of rupture of the tension band. Low-molecular-weight heparin was routinely applied in the evening before surgery. Spinal stabilization surgery was performed the day after admission after a brief period of preoperative preparation. Intraoperatively, no disturbance of the posterior tension band was observed (interspinous ligaments were intact, and the laminar bone showed no subtle fractures). All transpedicular screws were placed under fluoroscopic guidance in 2 planes as shown in
Figure 2. There was no breach of the medial pedicular walls, and no laminectomy was performed primarily since there was no need initially. Intraoperatively, there was minimal blood loss, and the anesthesiologist did not report any significant changes in blood pressure or pulse.
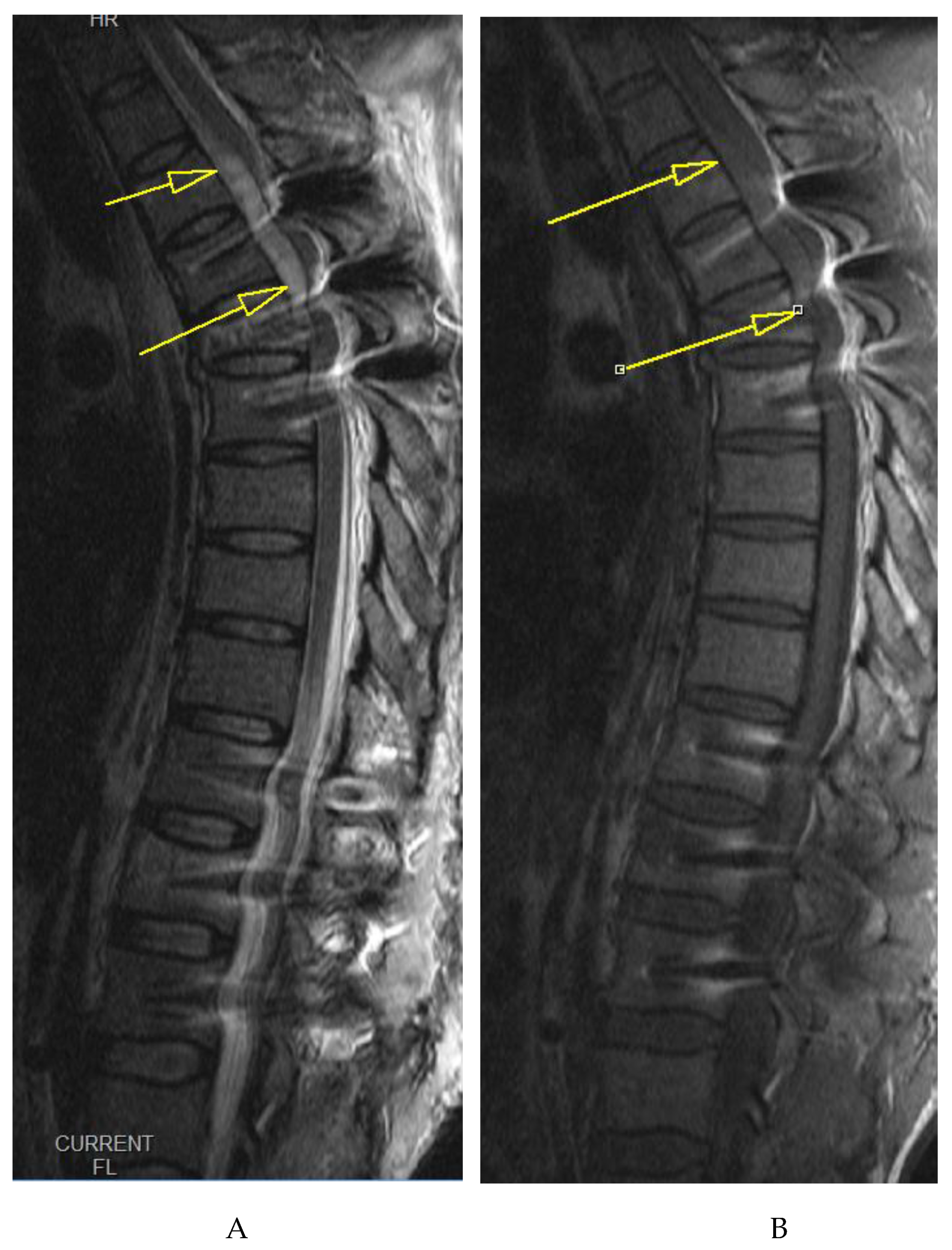
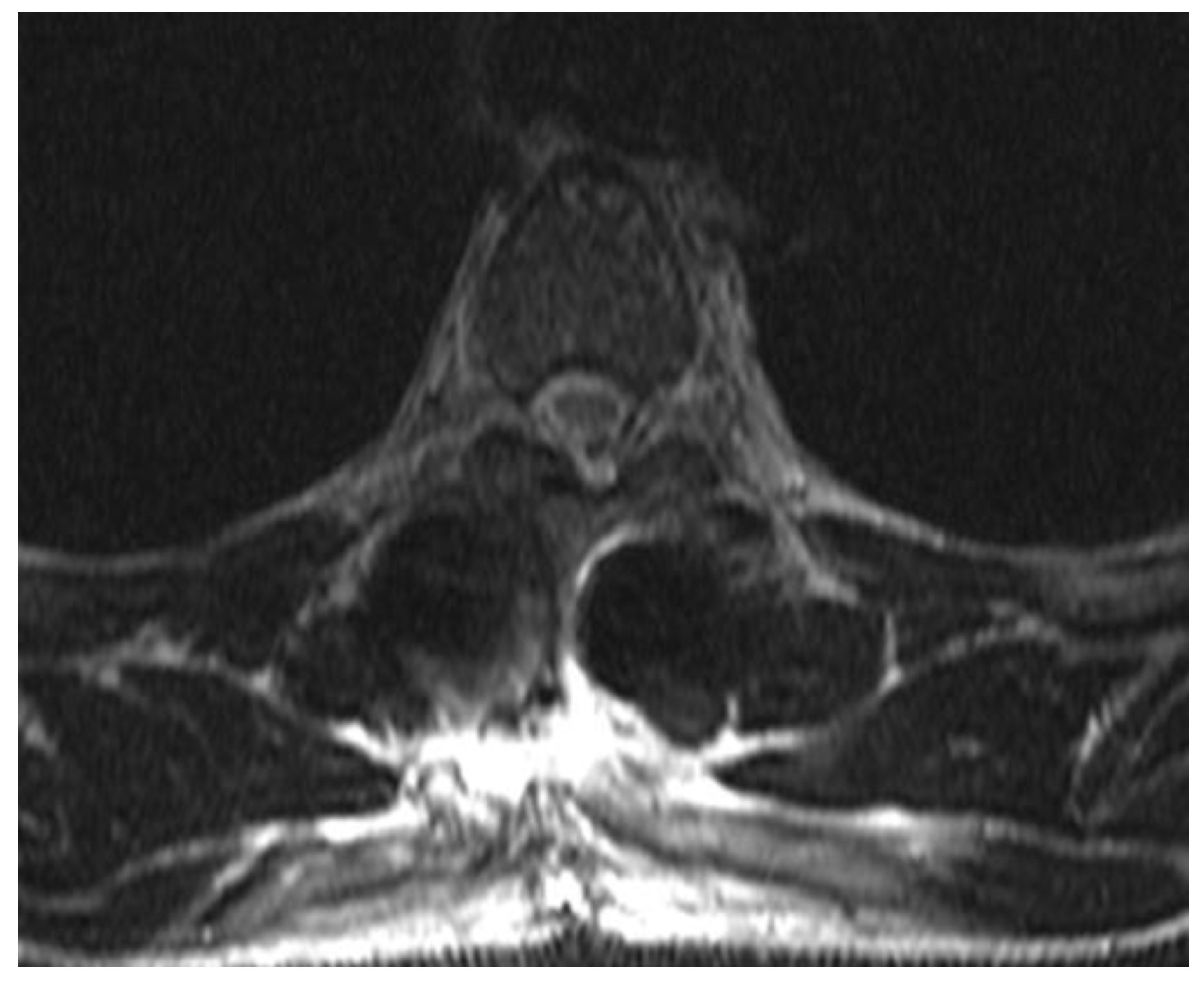
On awakening from general anesthesia, the initial postoperative neurological state was without any impairment, and he was able to urinate spontaneously. Approximately 45 minutes after surgery, he began to develop signs of hypesthesia in the lower extremities, weakness in the legs, an unsettling sensation in the abdomen, and was covered with cold sweat. Due to neurological worsening, an emergency MRI of the thoracic spine was performed, which revealed a hyperacute epidural hematoma that developed at the level of the Th6 fracture and spread cranially to Th4 as shown in
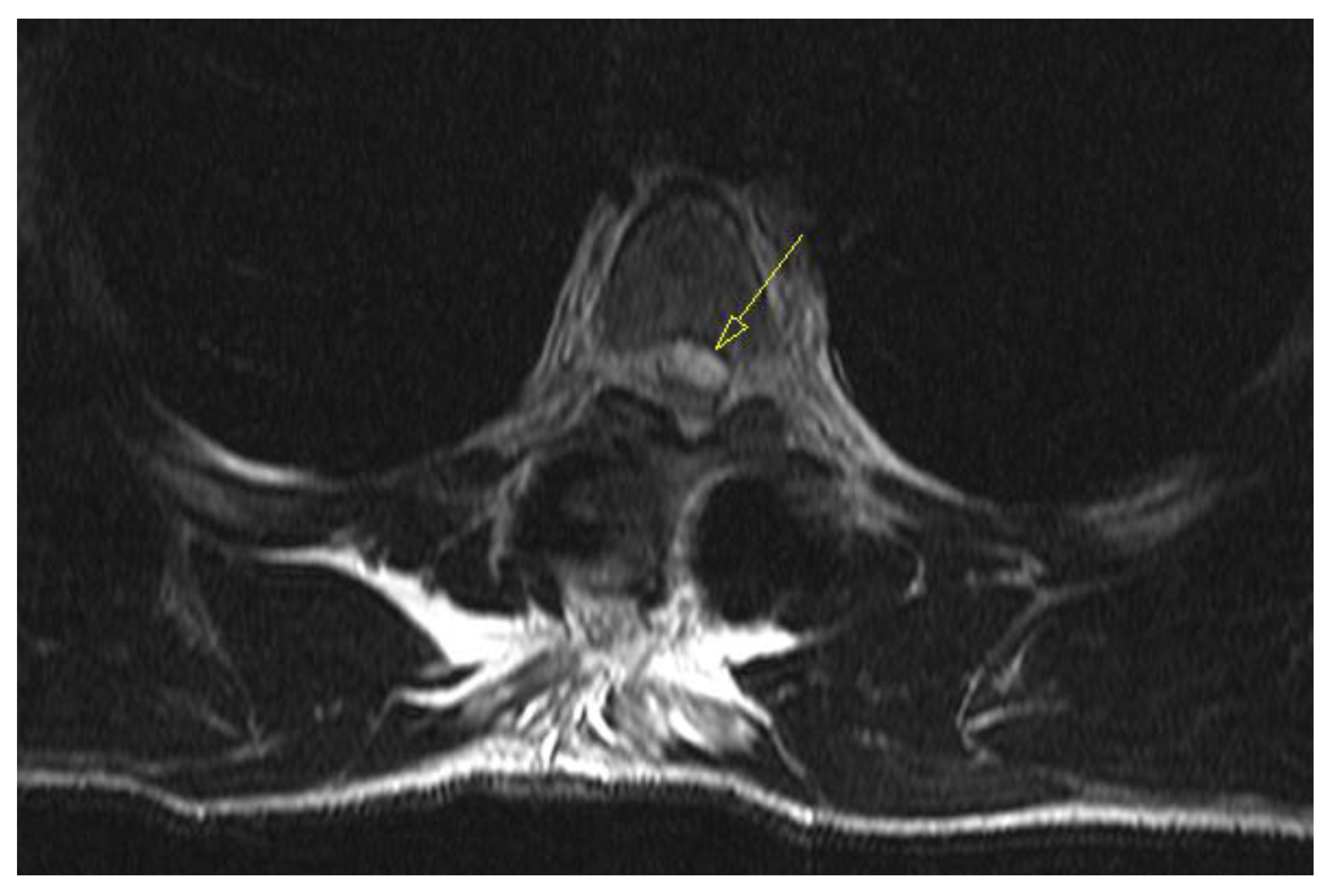
Figure 3. The width was measured at 7mm and compressed the spinal cord against the laminae as shown in
Figure 4. Most likely the bleeding occurred from the fracture itself.
Upon completion of the MRI, total paralysis was observed in the legs and skin anesthesia up to the level of the lower ribcage (roughly corresponding to the Th7 dermatome). Emergency revision surgery was immediately planned, and he was placed in a semi-seated position while awaiting entry into the operating room. During the roughly 45-minute waiting time (while another surgery was finishing up), rapid and complete resolution of loss of sensation and motor recovery was observed over 30 minutes. The need for emergency surgery was revised and postponed due to the observation of spontaneous neurological recovery.
Serial neurological exams were conducted every 30 minutes, during which there was no worsening of neurological status. The daily dose of low molecular weight heparin was skipped on the day of the incident to avoid any potential ongoing minor epidural bleeding, and the patient was encouraged to frequently test his muscle strength by isometric contractions of the groups of the leg muscle while recovering in bed.
Due to spontaneous resolution in a short period, emergency revision surgery was avoided. Emergency revision is no guarantee of neurological recovery as the procedure may require extensive decompression, costotransversectomy, and slight cord manipulation to access the anteriorly located hematoma – maneuvers that can cause further injury to the fragile mid-thoracic spinal cord. The assumption is that the slight elevation of the upper part of the body to a semi-seated position of approximately 20 ° (initially conducted to avoid further cranial migration of the hematoma) allowed caudal diversion (under gravity alone) of the hyperacute hematoma to the lumbar epidural space, where there is significantly more space to accommodate the few milliliters of blood.
Normal bladder function was restored 2 days after surgery. Repeat MRI evaluation was done on 3
rd postoperative day demonstrating significant resolution of hematoma as shown in
Figure 5, and
Figure 6. The subsequent hospital stay was uneventful. The patient was mobilized the day after surgery, pain medication tapered in 2 days, the wound healed primarily without signs of inflammation or dehiscence, and he is fully independent of daily tasks that do not require much stress on the spine.
3. Discussion
A symptomatic epidural hematoma can occur post-surgery when decompressive methods expose neural components and persistent bleeding under the fascia creates pressure, leading to neural compression and dysfunction [
11]. The bleeding can come from various places, such as epidural veins, muscle surfaces, or bone surfaces disrupted during fusion. Particularly, Batson's plexus, a vein network, can bleed profusely, especially during posterior interbody fusion procedures. It's often challenging to manage when occurred in obese patients [
12]. Small arteries near facet joints or injured during exposure may also contribute. Injuries in paraspinal blood vessels can become active post-retraction. It's crucial to achieve hemostasis throughout and reassess before closing. Addressing a significant bleed during the initial operation is preferable to needing to return to the operative room due to hematoma-induced symptoms.
An epidural hematoma that presents with symptoms following spine surgery is an uncommon occurrence, yet it has the potential to cause irreversible nerve damage and lasting serious disability. Factors that increase the likelihood of developing an epidural hematoma are age, the use of blood-thinning medication before or after surgery, or a procedure involving the removal of multiple laminae [
13]. If clinical symptoms suggest a hematoma, an urgent MRI is essential, with a CT-myelogram used when MRI isn't possible due to implants. An MRI helps confirm the diagnosis, showing fluid causing thecal sac compression. While some compression is normal and accepted, severe compression demands attention. The differential diagnosis for postoperative weakness includes tumor, infection, epidural hematoma, and disc herniation. An MRI serves as a confirmatory test, and it's crucial to correlate its findings with patient symptoms.
Sokolowski and colleagues created a "critical ratio" for evaluating thecal sac compression severity, but it's not an absolute criterion to decide the management [
14]. After diagnosing a symptomatic epidural hematoma, immediate evacuation within 6 to 12 hours is necessary. The existing incision can be used or extended for access. Potential bleeding sources need to be identified and eliminated, using techniques such as coagulation and bone wax. Subfascial drains are typically employed during closure. Coagulation profiles should be conducted, and anticoagulants are paused if used as done in our case. Time delay to evacuation and pre-evacuation neurologic impairment are key factors in prognosis. Neurologic recovery is maximized when deficits occur gradually, are incomplete, and when evacuation is undertaken within 6 to 12 hours [
15]. After diagnosis, prompt surgical intervention should be prioritized.
To date, there is scant material in the literature on such simple spontaneous resolutions of an otherwise potentially devastating complication. The reported cases were mostly cervical spinal epidural hematomas with spontaneous resolution without any known identifiable reason for the spontaneous resolution in them [
16,
17]. To the authors' knowledge, this is the first case report of the spontaneous resolution of a thoracic postoperative spinal epidural hematoma with a simple conservative measure following thoracic stabilization surgery.
Continued passive observation for an extended period is not recommended, and patients should be prepared for the possibility of a follow-up surgical intervention if early indications of swift recovery are not apparent. This is to suggest that while it is crucial to give the body some time to heal and show signs of improvement after initial surgery, an excessively long period of inaction or "watchful waiting" may not be in the patient's best interest. If the patient does not show signs of rapid recovery in the initial stages following the procedure, they should be mentally and physically prepared for a potential secondary surgery or revision surgery. This secondary surgery aims to rectify issues that have not been resolved with the initial operation. By being prepared for this possibility, patients can ensure they receive the necessary treatment promptly, increasing the likelihood of successful treatment outcomes thereby preventing untoward complications.5.
4. Conclusion
Although in our case this was sudden and most unexpected, there may be a rationale to attempt similar simple maneuvers when spontaneous or postoperative epidural hematomas are encountered as a cause of acute neurological deterioration. Prolonged watchful waiting should still be discouraged, and patients should remain ready for revision surgery if there are no early signs of rapid recovery.
Author Contributions
Conceptualization, S.D., and S.Ć.; methodology, J.P. and Z.L.; writing—original draft preparation, M.Š., G.E., B.B. and, S.I.; writing—review and editing, S.D., S.Ć. and, S.M..; visualization, S.D., K.P. and, S.I.; supervision, S.M., S.D. and, S.Ć. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from the patient.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Glotzbecker, M.; Bono, C.; Wood, K.; Harris, M. Postoperative Spinal Epidural Hematoma: A Systematic Review. 2010. [Google Scholar] [CrossRef]
- Bhosle, R.; Raju, D.; Patel, S.S.; Aditya, G.; Shukla, J.; Ghosh, N.; Krishnan, P. Spinal Subdural Hematoma Following Epidural Anesthesia. Asian J Neurosurg 2023, 18, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.W.; Yilmaz, T.S.; Kasper, E.M. Iatrogenic Spinal Hematoma as a Complication of Lumbar Puncture: What Is the Risk and Best Management Plan? Surg Neurol Int 2016, 7, S581–S589. [Google Scholar] [CrossRef] [PubMed]
- Benyaich, Z.; Laghmari, M.; Lmejjati, M.; Aniba, K.; Ghannane, H.; Ait Benali, S. Acute Lumbar Spinal Subdural Hematoma Inducing Paraplegia After Lumbar Spinal Manipulation: Case Report and Literature Review. World Neurosurg 2019, 128, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Amiri, A.R.; Fouyas, I.P.; Cro, S.; Casey, A.T.H. Postoperative Spinal Epidural Hematoma (SEH): Incidence, Risk Factors, Onset, and Management. The Spine Journal 2013, 13, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Aono, H.; Ohwada, T.; Hosono, N.; Tobimatsu, H.; Ariga, K.; Fuji, T.; Iwasaki, M. Incidence of Postoperative Symptomatic Epidural Hematoma in Spinal Decompression Surgery. J Neurosurg Spine 2011, 15, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, A.M.; Porto, G.B.F.; Wessell, J.; Buchholz, A.L.; Arnold, P.M. Venous Thromboprophylaxis in Spine Surgery. Global Spine J 2020, 10, 65S–70S. [Google Scholar] [CrossRef] [PubMed]
- Muthu, S.; Ramakrishnan, E.; Natarajan, K.K.; Chellamuthu, G. Risk-Benefit Analysis of Wound Drain Usage in Spine Surgery: A Systematic Review and Meta-Analysis with Evidence Summary. Eur Spine J 2020, 29, 2111–2128. [Google Scholar] [CrossRef]
- Modi, H.N.; Lee, D.Y.; Lee, S.-H. Postoperative Spinal Epidural Hematoma after Microscopic Lumbar Decompression: A Prospective Magnetic Resonance Imaging Study in 89 Patients. J Spinal Disord Tech 2011, 24, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Domenicucci, M.; Mancarella, C.; Santoro, G.; Dugoni, D.E.; Ramieri, A.; Arezzo, M.F.; Missori, P. Spinal Epidural Hematomas: Personal Experience and Literature Review of More than 1000 Cases. J Neurosurg Spine 2017, 27, 198–208. [Google Scholar] [CrossRef]
- Butler, A.J.; Mohile, N.; Phillips, F.M. Postoperative Spinal Hematoma and Seroma. J Am Acad Orthop Surg 2023. [CrossRef] [PubMed]
- Kao, F.-C.; Tsai, T.-T.; Chen, L.-H.; Lai, P.-L.; Fu, T.-S.; Niu, C.-C.; Ho, N.Y.-J.; Chen, W.-J.; Chang, C.-J. Symptomatic Epidural Hematoma after Lumbar Decompression Surgery. Eur Spine J 2015, 24, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Djurasovic, M.; Campion, C.; Dimar, J.R.; Glassman, S.D.; Gum, J.L. Postoperative Epidural Hematoma. Orthop Clin North Am 2022, 53, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Sokolowski, M.J.; Garvey, T.A.; Perl, J.; Sokolowski, M.S.; Akesen, B.; Mehbod, A.A.; Mullaney, K.J.; Dykes, D.C.; Transfeldt, E.E. Postoperative Lumbar Epidural Hematoma: Does Size Really Matter? Spine (Phila Pa 1976) 2008, 33, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, N.; Todd, N. Spinal Epidural Haematoma; Factors Influencing Outcome. Br J Neurosurg 2013, 27, 712–717. [Google Scholar] [CrossRef] [PubMed]
- Fattahi, A.; Taheri, M. Spontaneous Resolved Cervical Spine Epidural Hematoma: A Case Report. Surg Neurol Int 2017, 8, 183. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.-W.; Lee, J.-K.; Seo, B.-R.; Kim, S.-H. Spontaneous Resolution of Tetraparesis Because of Postoperative Cervical Epidural Hematoma. Spine J 2010, 10, e1–e5. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).