Submitted:
09 August 2023
Posted:
11 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Study Design and Participants
2.3. Data Collection
2.3.1. Data of Participants
2.3.2. Ambient Air Pollution Parameters
2.4. Ethical Approval
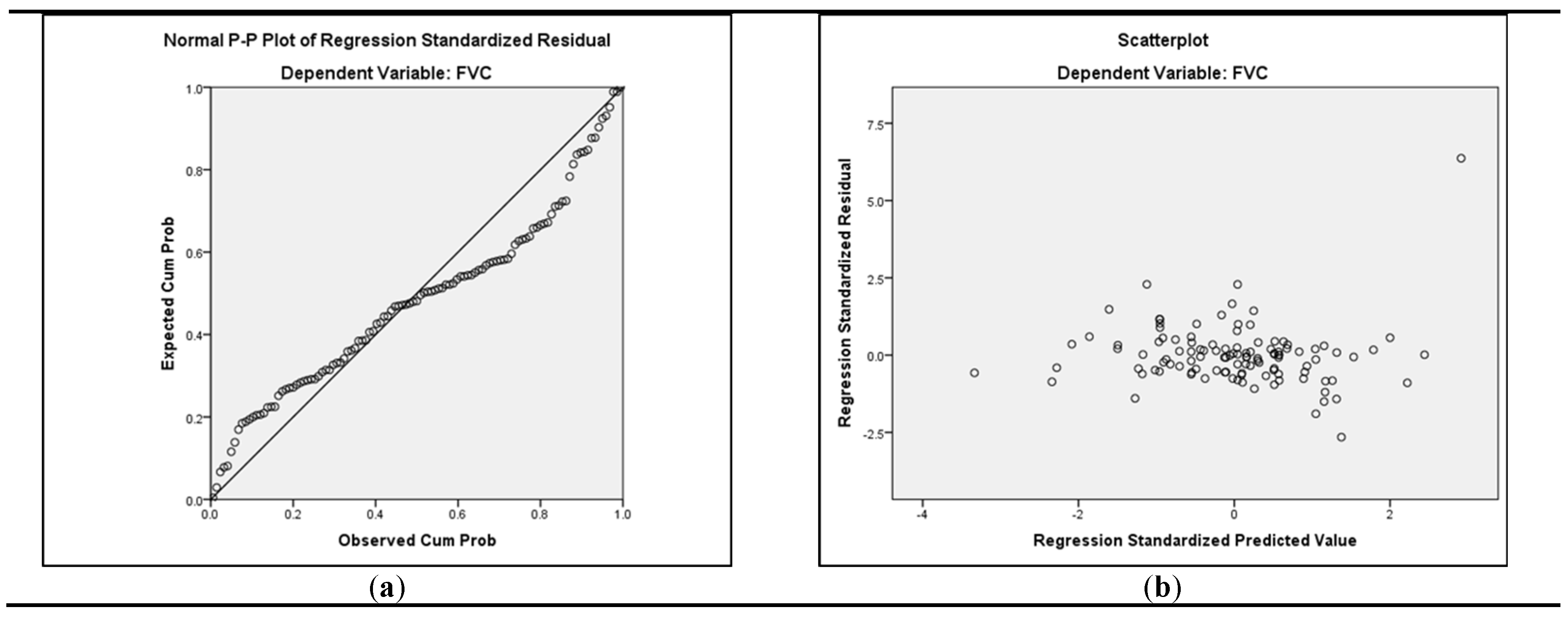
2.5. Data Analysis
3. Results
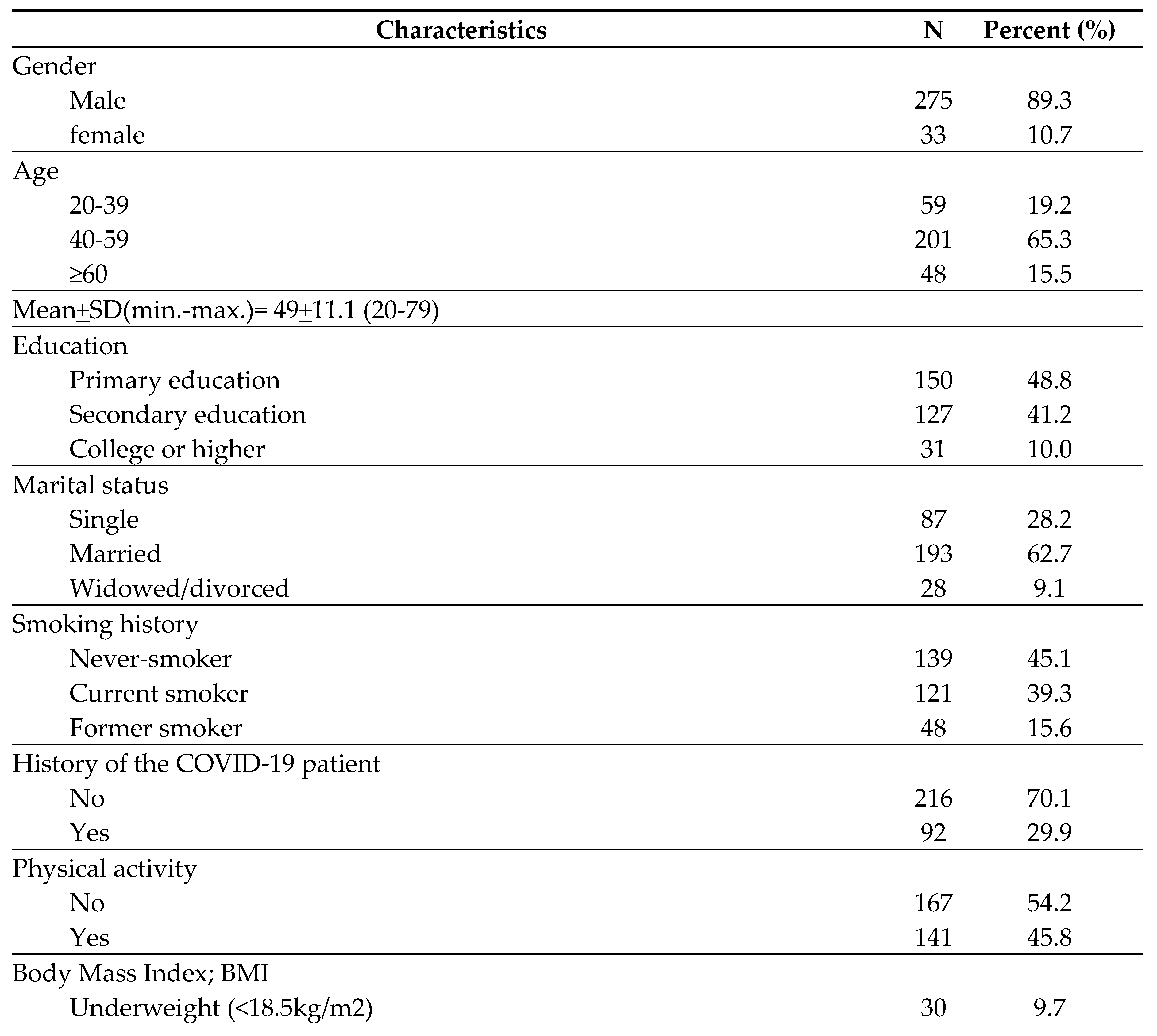
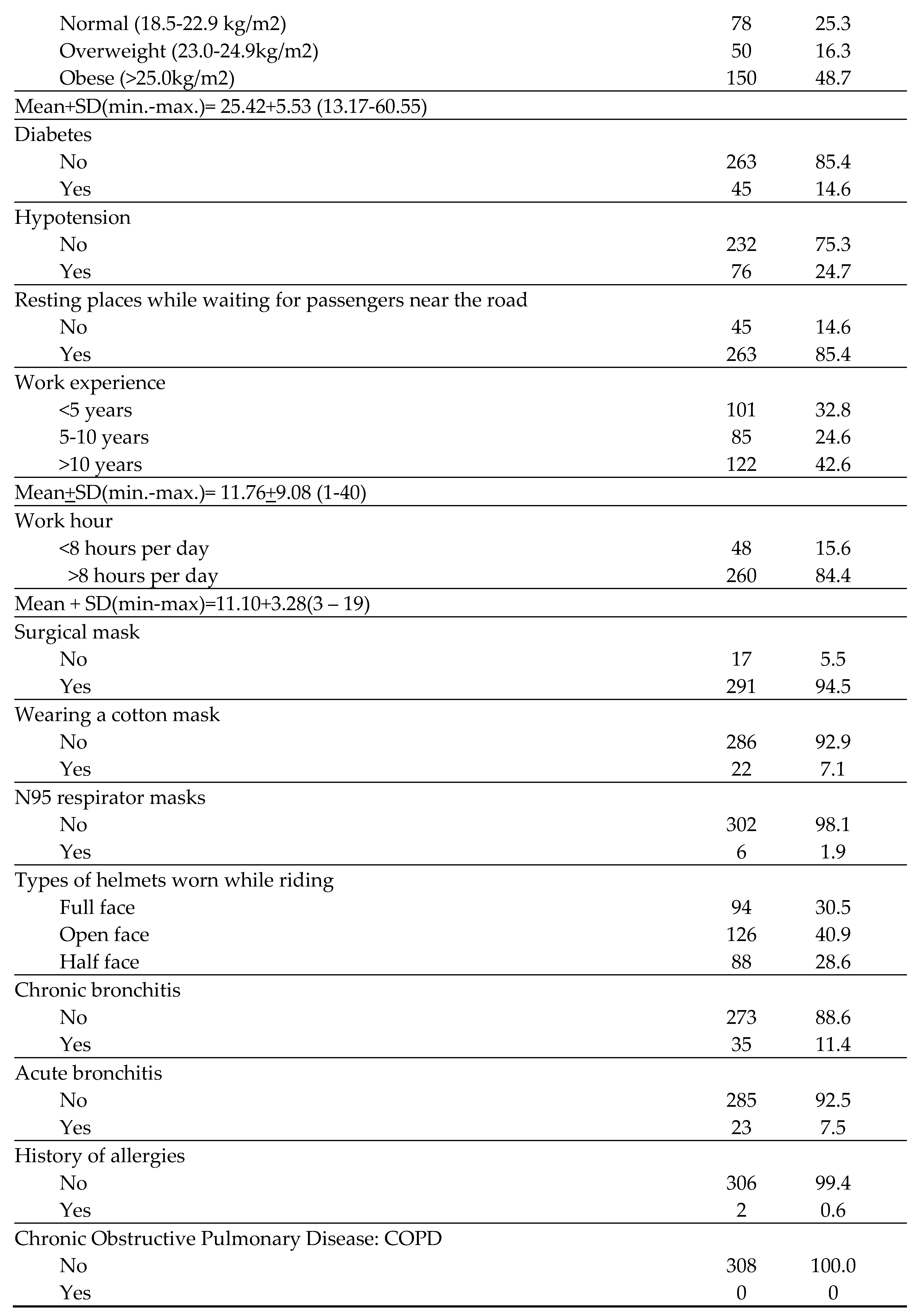
3.1. Demographic, Work Characteristics, and Respiratory Symptoms of Participants
3.2. The 24 Hours Average Concentration of PM2.5 and PM10 in Bangkok and Adjacent Provinces
3.3. Exposure to Respirable Dust Concentration while Performing Tasks
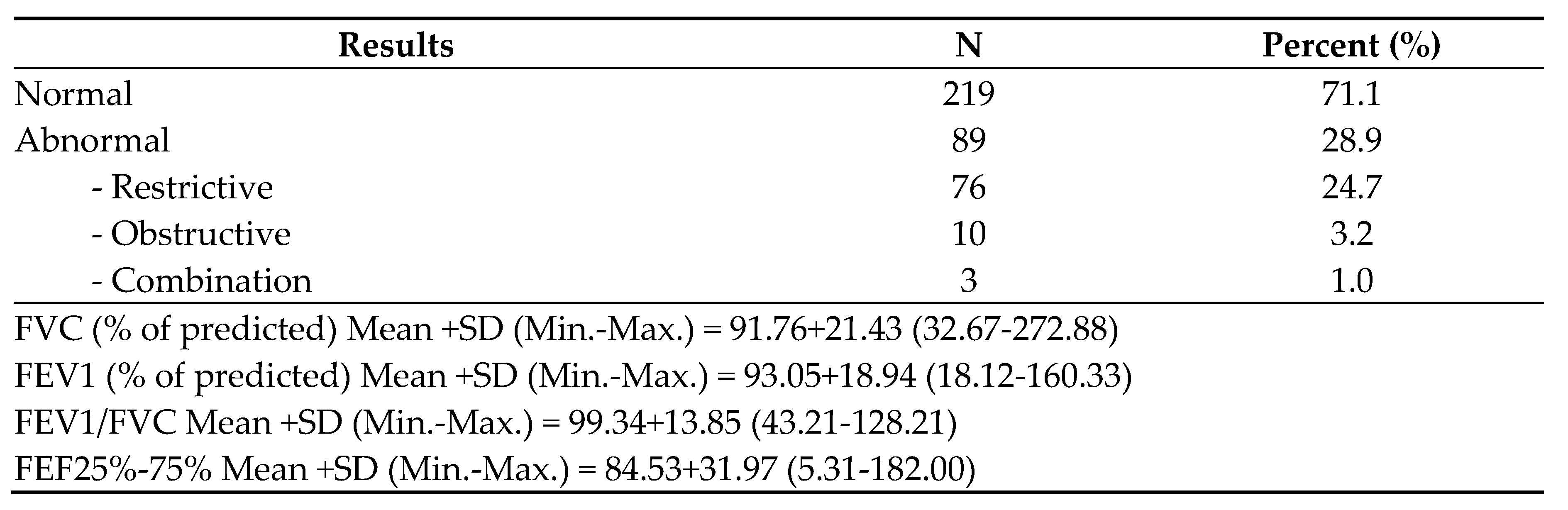
3.4. Lung Function Tests (LFTs)
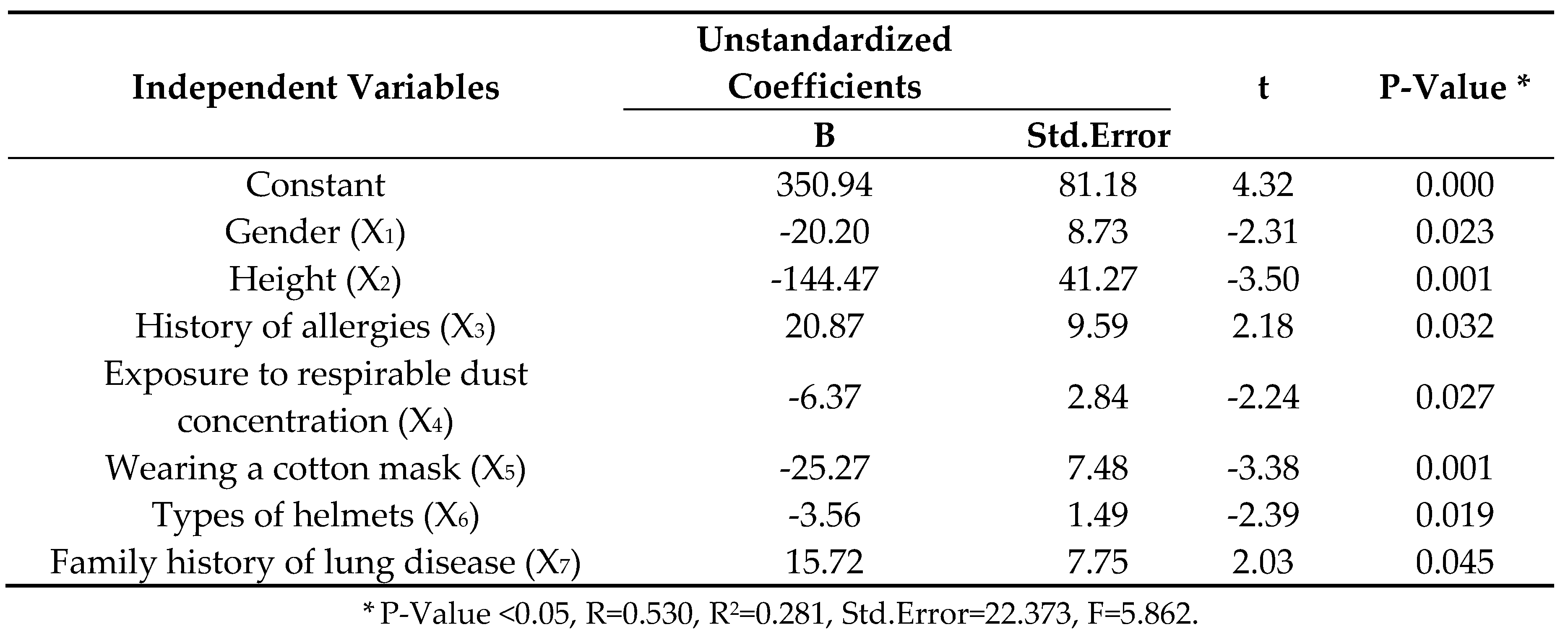
3.5. Association between Independent Variables and Lung Function Impairment
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- American Thoracic Society. What constitutes an adverse health effect of air pollution? American journal of respiratory and critical care medicine 2000, 161, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Aretz, B., Janssen, F., Vonk, J. M., Heneka, M. T., Boezen, H. M., & Doblhammer, G. (2021). Long-term exposure to fine particulate matter, lung function and cognitive performance: A prospective Dutch cohort study on the underlying routes. Environmental Research, 201, 111533. [CrossRef]
- Barry S. Levy, David H. Wegman, Sherry L. Baron, & Sokas, R. K. (2011). Occupational and environmental health: recognizing and preventing disease and injury (sixth ed.). Oxford university press.
- Ben Saad, H., Selmi, H., Hadj Mabrouk, K., Gargouri, I., Nouira, A., Said Latiri, H., Maatoug, C., Bouslah, H., Chatti, S., & Rouatbi, S. (2014). Spirometric “Lung Age” estimation for North African population. Egyptian Journal of Chest Diseases and Tuberculosis, 63(2), 491-503. [CrossRef]
- Bureau of Highway Safety, D. o. H. (2021). Traffic volume on highways in Bangkok Metropolitan Region. Available online: http://bhs.doh.go.th/download/traffic.
- Chaaban, O., Balanay, J. A. G., & Sousan, S. (2022). Assessment of best-selling respirators and masks: Do we have acceptable respiratory protection for the next pandemic? American Journal of Infection Control. [CrossRef]
- China, N., Vaz, D., Martins, C., Gomes, J., Ladeira, I., Lima, R., & Guimarães, M. (2020). Obtaining spirometric reference values when height is not available – comparison of alternative anthropometric measures. Pulmonology, 26(4), 198-203. [CrossRef]
- Chuang, K.-J.; Lin, L.-Y.; Ho, K.-F.; Su, C.-T. Traffic-related PM2.5 exposure and its cardiovascular effects among healthy commuters in Taipei, Taiwan. Atmospheric Environment: X 2020, 7, 100084. [Google Scholar] [CrossRef]
- Ciprandi, G., & Cirillo, I. (2006). The lower airway pathology of rhinitis. Journal of Allergy and Clinical Immunology, 118(5), 1105-1109. [CrossRef]
- Cordova, J. E. D.; Aguirre, V. T.; Apestegui, V. V.; Ibarguen, L. O.; V, B. N.; Steenland, K.; Rengifo, G. F. G. Association of PM2.5 concentration with health center outpatient visits for respiratory diseases of children under 5 years old in Lima, Peru. Environmental Health 2020, 19, 1–6. [Google Scholar]
- Daleck, A.; Wigmann, C.; Kress, S.; Altug, H.; Jirik, V. e.; Heinrich, J.; Abramson, M. J.; Schikowski, T. The mediating role of lung function on air pollution-induced cardiopulmonary mortality in elderly women: The SALIA cohort study with 22-year mortality follow-up. International Journal of Hygiene and Environmental Health 2021, 233, 113705. [Google Scholar] [CrossRef] [PubMed]
- Dauchet, L.; Hulo, S.; Cherot-Kornobis, N.; Matran, R.; Amouyel, P.; Edme, J.-L.; Giovannelli, J. Short-term exposure to air pollution: Associations with lung function and inflammatory markers in non-smoking, healthy adults. Environment International 2018, 121, 610–619. [Google Scholar] [CrossRef]
- Department of Land Transport, M. o. T. (2021). The Number of Driving Licences and Transport Personnel Licences Classified by Type. Available online: https://web.dlt.go.th/statistics/.
- Department of Provincial Administration, M. o. I. (2020). Area classified by region and province, year 2011 - 2020.
- Doungrutai Boudoung. (1999). Effect of Respirable Particulates on Lung Function among Traffic Policemen in Bangkok Chulalongkorn University].
- Guo, H., Sahu, S. K., Kota, S. H., & Zhang, H. (2019). Characterization and health risks of criteria air pollutants in Delhi, 2017. Chemosphere. [CrossRef]
- Hankinson, J. L., Kawut, S. M., Shahar, E., Smith, L. J., Stukovsky, K. H., & Barr, R. G. (2010). Performance of American Thoracic Society-recommended spirometry reference values in a multiethnic sample of adults: the multi-ethnic study of atherosclerosis (MESA) lung study. chest, 137(1), 138-145. [CrossRef]
- Hankinson, J. L., Odencrantz, J. R., & Fedan, K. B. (1999). Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med, 159(1), 179-187. [CrossRef]
- Hou, D., Ge, Y., Chen, C., Tan, Q., Chen, R., Yang, Y., Li, L., Wang, J., Ye, M., Li, C., Meng, X., Kan, H., Cai, J., & Song, Y. (2020). Associations of long-term exposure to ambient fine particulate matter and nitrogen dioxide with lung function: A cross-sectional study in China. Environment International, 144, 105977. [CrossRef]
- Jenson, D., & Unnikrishnan, V. U. (2015). Energy dissipation of nanocomposite based helmets for blast-induced traumatic brain injury mitigation. Composite Structures, 121, 211-216. [CrossRef]
- Jiang, Y., Chen, J., Wu, C., Lin, X., Zhou, Q., Ji, S., Yang, S., Zhang, X., & Liu, B. (2020). Temporal cross-correlations between air pollutants and outpatient visits for respiratory and circulatory system diseases in Fuzhou, China. BMC Public Health, 20:1131, 1-13. [CrossRef]
- ohannson, K. A.; Vittinghoff, E.; Morisset, J.; Wolters, P. J.; Noth, E. M.; Balmes, J. R.; Collard, H. R. Air Pollution Exposure Is Associated With Lower Lung Function, but Not Changes in Lung Function, in Patients With Idiopathic Pulmonary Fibrosis. Chest 2018, 154(1), 119–125. [Google Scholar] [CrossRef] [PubMed]
- Kan, H., Heiss, G., Rose, K. M., Whitsel, E., Lurmann, F., & London, S. J. (2007). Traffic exposure and lung function in adults: the Atherosclerosis Risk in Communities study. Thorax, 62, 873-879. [CrossRef]
- Kanjanasiranont, N., Prueksasit, T., & Morknoy, D. (2017). Inhalation exposure and health risk levels to BTEX and carbonyl compounds of traffic policeman working in the inner city of Bangkok, Thailand [Article]. Atmospheric Environment, 152, 111-120. [CrossRef]
- Li, J., Ma, T., Huang, C., Huang, X., Kang, Y., Long, Z., & Liu, M. (2020). Protective Mechanism of Helmet Under Far-field Shock Wave. International Journal of Impact Engineering, 143, 103617. [CrossRef]
- Loonsamrong, W., Taneepanichskul, N., Puangthongthub, S., & Tungsaringkarn, T. (2017). Health Risk Assessment and BTEX Exposure among Car Park Workers at a Parking Structure in Bangkok, Thailand [article in journal/newspaper]. Journal of Health Research; Vol 29 No 4: July - August 2015; 285-292 ; 2586-940X ; 0857-4421. Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=edsbas&AN=edsbas.4A273663&authtype=sso&custid=s4775581&site=eds-live&scope=site&custid=s4775581.
- Ma, H., Liu, F., Yang, X., Liu, Q., Wang, X., Xing, X., Lin, Z., Cao, J., Li, J., Huang, K., Yan, W., Liu, T., Fan, M., Chen, S., Lu, X., Gu, D., & Huang, J. (2021). Association of short-term fine particulate matter exposure with pulmonary function in populations at intermediate to high-risk of cardiovascular disease: A panel study in three Chinese cities. Ecotoxicology and Environmental Safety, 220, 112397. [CrossRef]
- Milanese, M., Corsico, A. G., Bellofiore, S., Carrozzi, L., Di Marco, F., Iovene, B., Richeldi, L., Sanna, A., Santus, P., Schisano, M., Scichilone, N., Vancheri, C., & Cerveri, I. (2021). Suggestions for lung function testing in the context of COVID-19. Respiratory Medicine, 177, 106292. [CrossRef]
- Ministry of Public Health. (2021, November 30,2021). Public Health practices for preventing the spread of COVID-19 safety measures for organizations. Available online: https://stopcovid.anamai.moph.go.th/attach/w774/f20211201211017_iXg45j3zsx.pdf (accessed on 19 November 2022).
- National Institute for Occupational Safety and Health. (1998). Particulates not otherwise regulated, respirable 0600. In (3 ed., pp. 1-6).
- National Statistical Office, N. (2021). Number of employed people in formal and informal workers Classified by age group, sex, region and province, 2011 - 2020. Retrieved August 16. Available online: http://statbbi.nso.go.th/staticreport/page/sector/th/02.aspx.
- Okeleji, L. O., Ajayi, A. F., Adebayo-Gege, G., Aremu, V. O., Adebayo, O. I., & Adebayo, E. T. (2021). Epidemiologic evidence linking oxidative stress and pulmonary function in healthy populations. Chronic Diseases and Translational Medicine, 7(2), 88-99. [CrossRef]
- Ongwandee, M., & Chavalparit, O. (2010). Commuter exposure to BTEX in public transportation modes in Bangkok, Thailand [Article]. Journal of Environmental Sciences, 22(3), 397-404. [CrossRef]
- Pannipa, Suebsuk; Pongnumkul, Autchariya; Leartsudkanung, Darunee; Sareewiwatthana, Penchun. Predicting Factors of Lung Function Among Motorcycle Taxi Drivers in the Bangkok Metropolitan Area. Journal of Public Health 2014, 44(1), 79–92. [Google Scholar]
- Paranthaman, M. P., Peroutka-Bigus, N., Larsen, K. R., Phadke, K. S., Summers, T., Theodore, M., Hensley, D. K., Levine, A. M., Lee, R. J., & Bellaire, B. H. (2022). Effective antiviral coatings for deactivating SARS-CoV-2 virus on N95 respirator masks or filters. Materials Today Advances, 14, 100228. [CrossRef]
- Pollution Control Department. (2022). Overall air quality reporting. Available online: www.air4thai.pcd.go.th (accessed on 22 October 2022).
- Quanjer, P. H., Stanojevic, S., Cole, T. J., Baur, X., Hall, G. L., Culver, B. H., Enright, P. L., Hankinson, J. L., Ip, M. S. M., Zheng, J., & Stocks, J. (2012). Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. European Respiratory Journal, 40(6), 1324-1343. [CrossRef]
- Raphiphan, P., Zaslavsky, A., & Indrawan-Santiago, M. (2014). Building Knowledge from Social Networks on What is Important to Drivers in Constrained Road Infrastructure. Procedia Computer Science, 35, 720-729. [CrossRef]
- Redlich, C. A.; Tarlo, S. M.; Hankinson, J. L.; Townsend, M. C.; Eschenbacher, W. L.; Essen, S. G. V.; Sigsgaard, T.; Weissman, D. N. Official American Thoracic Society Technical Standards: Spirometry in the Occupational Setting. American journal of respiratory and critical care medicine 2014, 189, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Simaporn, promsarn; lertritwimanman, P. New normal in spirometric procedures. Thai Journal of Tuberculosis Chest Disease and Critical Care 2020, 39(2), 76–81. [Google Scholar]
- Simaporn, Promsarn; Lertritwimarnman, P. New normal in Spirometric Procedures. Thai Journal of Tuberculosis Chest Disease and Critical Care 2020, 39, 76–81. [Google Scholar]
- Siriorn, Sindhu; Kamlungdee, Umaporn; Konggumnerd, R. Effect of smoke exposure on lung function among adults in communities. Thai Journal of Nursing Council 2011, 26(3), 93–106. [Google Scholar]
- Summacheeva Foundation. (2018). Guideline for Standardization and Interpretation of Pulmonary Function Test by Spirometry in Occupational Health Setting.
- Syahira, M. P. A., Karmegam, K., Diyana, M. Y. N. A., Irniza, R., Bahri, M. T. S., Vivien, H., Maizura, H. N., & Sivasankar, S. (2020). Impacts of PM2.5 on respiratory system among traffic policemen. 25-29. [CrossRef]
- Warkentin, T.M.; Lam, S.; Hung, R. J. Determinants of impaired lung function and lung cancer prediction among never-smokers in the UK Biobank cohort. EBioMedicine 2019, 47, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Tanawat, Rakkamon; Na-songkhla, Thitima; Chuchuag, Varintip; Issara, O. Factors associated with pulmonary function among workers exposing ammonia from fresh natural latex purchasing process at rubber holder cooperative in Southern, Thailand. Disease Control Journal 2015, 41(4), 285–296. [Google Scholar]
- Thanapon Lertchittasakul, Arun Laoarun, & Boonsong, P. (2019, 26-28 June 2019). Quality of life of public motorcycle riders in Bangkok a case study in Thungkru, Rat Burana, Phasi Charoen, Bangkok Noi, Bang Khae district. The 4th National RMUTR Conference and The 1st International RMUTR Conference, Bangkok. 28 June.
- Thayyezhuth, D., Venkataram, R., Bhat, V. S., & Aroor, R. (2021). A study of Spirometric parameters in non asthmatic allergic rhinitis. Heliyon, 7(11), e08270. 11. [CrossRef]
- The National Environment Board. (2022, July 8, 2022). The standard for particulate matter less than 2.5 microns in the ambient air. Available online: http://www.ratchakitcha.soc.go.th/DATA/PDF/2565/E/163/T_0021.PDF (accessed on 13 November 2022).
- Thurston, G. D., Kipen, H., Annesi-Maesano, I., Balme, J., Brook, R. D., Cromar, K., Matteis, S. D., Forastiere, F., Forsberg, B., Frampton, M. W., Grigg, J., Heederik, D., Kelly, F. J., Kuenzli, N., Laumbach, R., Peters, A., Rajagopalan, S. T., Rich, D., Ritz, B., . . . Brunekreef, B. (2017). A joint ERS/ATS policy statement: what constitutes an adverse health effect of air pollution? An analytical framework. Eur Respir J, 49, 1-19. [CrossRef]
- Traffic, T. L. V. R. (2022). Number of registered motorcycles in Thailand from 2012 to the first eight months of 2021. Retrieved April13. Available online: https://www.statista.com/statistics/1179962/thailand-number-of-registered-motorcycles/.
- Tunsaringkarn, T., Siriwong, W., Rungsiyothin, A., & Nopparatbundit, S. (2012). Occupational Exposure of Gasoline Station Workers to BTEX Compounds in Bangkok, Thailand [article]. The International Journal of Occupational and Environmental Medicine, 3(3), 117-125. Available online: https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=edsdoj&AN=edsdoj.3c553ee2a08748358625c2010fa3f3a6&authtype=sso&custid=s4775581&site=eds-live&scope=site&custid=s4775581.
- Ueyama, M., Hashimoto, S., Takeda, A., Maruguchi, N., Yamamoto, R., Matsumura, K., Nakamura, S., Terada, S., Inao, T., Kaji, Y., Yasuda, T., Hajiro, T., Tanaka, E., Taguchi, Y., & Noma, S. (2021). Prediction of forced vital capacity with dynamic chest radiography in interstitial lung disease. European Journal of Radiology, 142, 109866. [CrossRef]
- Uma Sawetskulanont. (1997). Effects of particulate matter on Tc-99m DTPA lung clearance in traffic policemen in Bangkok Metropolis Chulalongkorn University].
- Wang, Y.; Wang, T.; Xu, M.; Yu, H.; Ding, C.; Wang, Z.; Pan, X.; Li, Y.; Niu, Y.; Yan, R.; et al. Independent effect of main components in particulate matter on DNA methylation and DNA methyltransferase: A molecular epidemiology study. Environment International 2020, 134, 105296. [Google Scholar] [CrossRef] [PubMed]
- World health organization. (2016). Air pollution. Available online: https://www.who.int/health-topics/air-pollution#tab=tab_2.
- world Health Organization. (2021, 22 September 2021). Ambient (outdoor) air pollution. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 13 November 2022).
- Yamane, T. (1973). Statistics. An introductory analysis. Third edition. Harper & Row. Available online: https://books.google.co.th/books?id=sl75MgEACAAJ.
- Yang, M.; Guo, Y.-M.; Bloom, M. S.; Dharmagee, S. C.; Morawska, L.; Heinrich, J.; Jalaludin, B.; Markevychd, I.; Knibbsf, L. D.; Lin, S.; et al. Is PM1 similar to PM2.5? A new insight into the association of PM1 and PM2.5 with children’s lung function. Environment International 2020, 145, 106092. [Google Scholar] [CrossRef] [PubMed]
- Yang, T., Chen, R., Gu, X., Xu, J., Yang, L., Zhao, J., Zhang, X., Bai, C., Kang, J., Ran, P., Shen, H., Wen, F., Huang, K., Chen, Y., Sun, T., Shan, G., Lin, Y., Wu, S., Zhu, J., . . . Wang, C. (2021). Association of fine particulate matter air pollution and its constituents with lung function: The China Pulmonary Health study. Environment International, 156, 106707. [CrossRef]
- Zaharia, C. (2014). Particulate matter (settled particles, coarse PM10, fine PM2.5 or PM1, ultrafine particles) in urban atmosphere: characteristics, quality control and health effects. In (pp. 221-244).
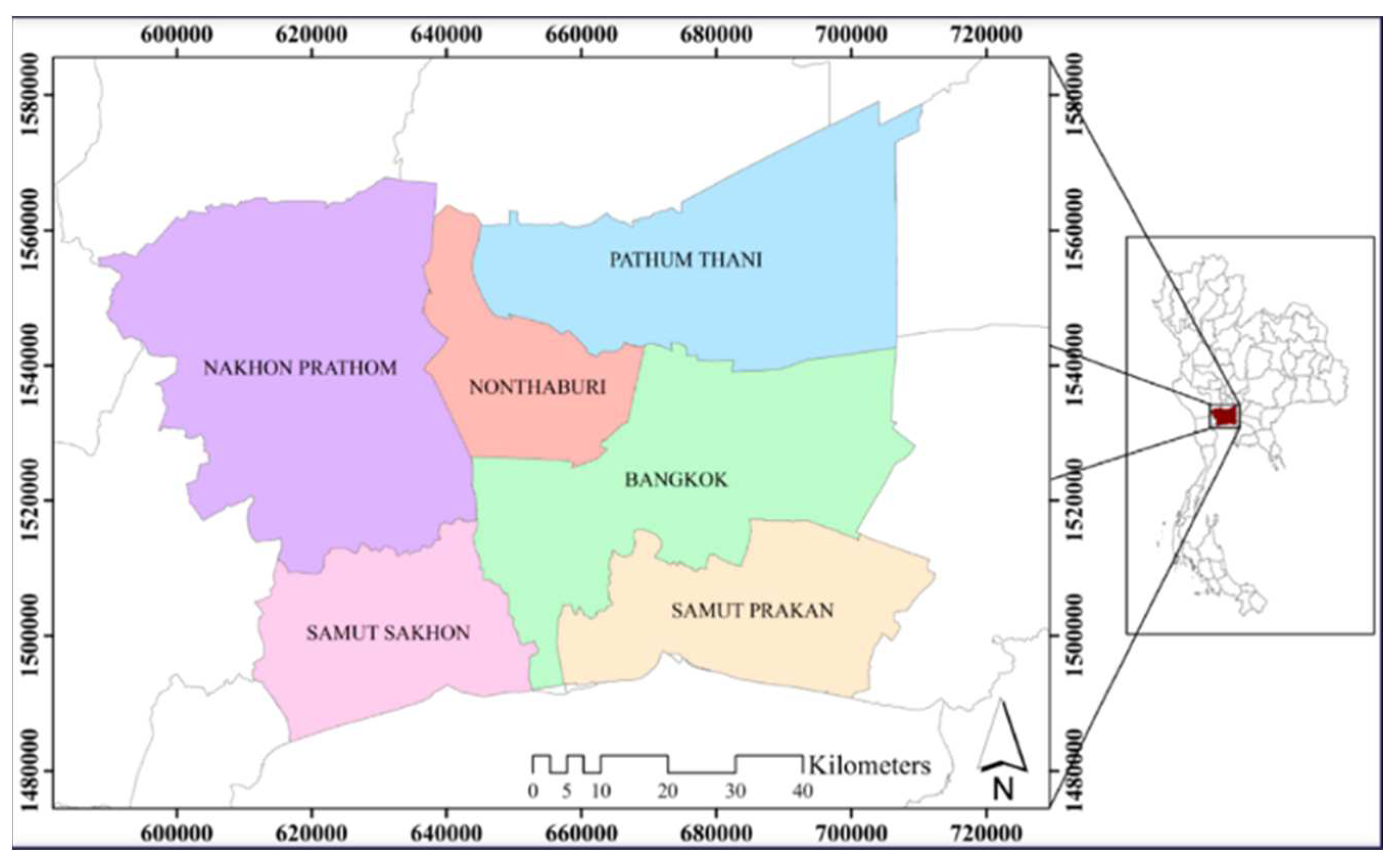
| Province | Number of Motorcycle Taxi Drivers 1 | Sample Size |
|---|---|---|
| Bangkok | 84,889 | 152 |
| Nonthaburi | 10,346 | 33 |
| Pathum Thani | 11,543 | 32 |
| Samut Prakan | 17,218 | 44 |
| Samut Sakhon | 4,949 | 35 |
| Nakhon Pathom | 6,286 | 12 |
| Total | 135,231 | 308 |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| - Over 20 years of age | - Diagnosis of chronic respiratory disease or any other chronic respiratory disease. |
| - Motorcycle taxi drivers who worked in ambient outdoor more than one year in Bangkok and adjacent provinces. | - Any acute or chronic condition that would limit the ability of the subject to participate in the study. |
| - Thai nationality and able to speak Thai language. | - Having an intermittent period working outdoor such as a stopping to work for other jobs outdoor and moving to indoor for doing work. |
| - Refusal to give informed consent. |
| Activity | Length of Time to Stop before Lung Function Testing |
|---|---|
| Drinking alcohol | 4 hours |
| Eating a large meal | 2 hours |
| Vigorous exercise | 30 minutes |
| Smoking | >1 hour |
| For reversibility testing | |
| Taking short-acting bronchodilators | 6 hours |
| Taking long-acting bronchodilators (including combination inhalers) or twice-daily preparations | 24 hours |
| Taking tiotropium or once-daily preparations | 48 hours |
| Province | Station | PM2.5 (µg/m3) | PM10 (µg/m3) | ||||
|---|---|---|---|---|---|---|---|
| rangea | meanb | >stdc | rangea | meanb | >stdc | ||
| Bangkok | Din Daeng Community Housing | 17-33 | 23 | 0/30 | 38-70 | 51 | 0/30 |
| Pathum Thani | Bangkok University | 5-21 | 12 | 0/28 | 17-53 | 31 | 0/28 |
| Nonthaburi | Sukhothai Thammathirat Open University | 5-20 | 10 | 0/30 | - | - | - |
| Samut Prakan | Disabled and Handicapped Vocational Rehabilitation Center Station | 5-22 | 11 | 0/30 | 11-34 | 20 | 0/30 |
| Samut Sakhon | Samut Sakhon Highway District | 12-30 | 17 | 0/30 | - | - | - |
| Nakhon Prathom | Water supply reservoir | 6-21 | 10 | 0/30 | 13-40 | 21 | 0/30 |
| SEG | Work Performing Area | Number of Workers | Personal Air Samplings (Psoint) | Respirable Dust Concentration (mg/m3) | ||
|---|---|---|---|---|---|---|
| Max. | Min. | Mean | ||||
| SEG1 | Bangkok- Din Daeng District | 152 | 57 | 0.365 | Not detected | 0.029 |
| SEG2 | Pathum Thani- Khlong Nueng Subdistrict, Khlong Luang District | 32 | 21 | 0.094 | 0.003 | 0.024 |
| SEG3 | Nonthaburi- Sukhothai Thammathirat Open University | 33 | 15 | 0.018 | 0.002 | 0.006 |
| SEG4 | Samut Prakan- Song Khanong Subdistrict, Phra Pradaeng District | 44 | 34 | 0.025 | Not detected | 0.009 |
| SEG5 | Samut Sakhon- Om Noi Subdistrict, Krathum Baen District | 35 | 16 | 0.027 | 0.001 | 0.008 |
| SEG6 | Nakhon Prathom- Nakhon Pathom Subdistrict, Mueang District | 12 | 10 | 0.018 | Not detected | 0.008 |
| Independent Variables | Pearson’s Correlation | P-Value * |
|---|---|---|
| Province | -0.18 | 0.002 |
| Gender | -0.13 | 0.028 |
| Distance from resting places while waiting for passengers with real-time air quality index (AQI) station | 0.20 | 0.001 |
| Family history of lung disease | -0.15 | 0.011 |
| Height | -0.13 | 0.028 |
| Hypertension | -0.13 | 0.021 |
| Types of helmet | -0.12 | 0.035 |
| Wearing a cotton mask | -0.15 | 0.009 |
| History of allergies | 0.15 | 0.007 |
| Exposure to respirable dust concentration | -0.11 | 0.047 |
| PM2.5 | 0.14 | 0.017 |
| SO2 | 0.17 | 0.003 |
| Wind direction | -0.14 | 0.015 |
| Temperature | 0.02 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





